Abstract
AIM
To investigate the association of peripheral anterior synechiae (PAS) with intraocular pressure (IOP) and glaucomatous optic neuropathy (GON) in primary angle closure (PAC) and primary angle-closure glaucoma (PACG).
METHODS
Totally 355 eyes (238 PAC and 117 PACG) of 181 patients were included in this retrospective analysis of baseline data from a randomized clinical trial. All patients had undergone a comprehensive ophthalmic examination. The extent of PAS in clock hours as determined on gonioscopy was documented. The independent effect of the extent of PAS on IOP and the prevalence of GON were determined using multivariable generalized estimating equation (GEE) models.
RESULTS
The frequency of GON increased with the extent of PAS and a higher IOP. PAS were more extensive (8 vs 1 clock hour, P<0.001) and IOP higher (28.01 vs 18.00 mm Hg, P<0.001) in PACG compared to PAC. The prevalence of GON among the PAS quartiles were 10.2% (PAS<0.5 clock hours), 16.9% (PAS≥0.5 and PAS<3 clock hours), 29.6% (PAS≥3 and PAS<7 clock hours), and 74.4% (PAS≥7 clock hours), respectively. After adjusting for IOP, age, gender, spherical equivalent, average Shaffer score and number of medications, the odds ratio (OR) for GON was 4.4 (95%CI: 1.5-13.0; P=0.007) with PAS≥3 clock hours and 13.8 (95%CI: 4.3-43.6; P<0.001) with PAS≥7 clock hours as compared to eyes with PAS<0.5 clock hours. The frequency of GON increased linearly with the extent of PAS. Extent of PAS was also associated with higher IOP. Eyes with both PAS≥6 clock hours and IOP≥21 mm Hg had the highest risk of GON compared to eyes with both PAS<6 clock hours and IOP<21 mm Hg (OR=18.0, 95%CI: 7.5-43.4; P<0.001).
CONCLUSION
The extent of PAS in PAC and PACG is an important predictor of higher IOP and is linearly associated with GON independent of IOP, suggesting other factors related to PAS formation may be involved in the development of GON in PACG.
Keywords: primary angle-closure glaucoma, peripheral anterior synechiae, intraocular pressure
INTRODUCTION
Glaucoma is the leading cause of irreversible blindness worldwide[1]. Primary angle-closure glaucoma (PACG) causes more blindness than primary open angle glaucoma (POAG)[2]. It is estimated that by 2020 there will be 23.4 million cases of PACG worldwide with 17.96 million in Asia[3]. In China, PACG was estimated to be the predominant subtype of glaucoma, and the prevalence was about at the level of 1.4%, expected to increase to 2.01% until 2050[4].
Primary angle-closure diseases (PACD) comprises primary angle closure (PAC) and PACG[5]. The increase in intraocular pressure (IOP) in PACD is secondary to closure of the angle of the anterior chamber; this closure can be appositional or synechial[6]. A higher IOP in PACG is associated with a narrower width of the angle as well as the presence of peripheral anterior synechiae (PAS)[7]–[8]. While it is intuitive that higher IOP would be associated with extent of PAS and consequently more serious glaucomatous optic neuropathy (GON), this relationship is not well defined.
The aim of our study was to determine the association of PAS with raised IOP and the prevalence of GON in PACD.
SUBJECTS AND METHODS
Ethical Approval
This was a retrospective analysis of baseline data obtained from a randomized controlled trial (RCT) conducted at the Handan Eye Hospital between October 1, 2005 and October 31, 2006 (registration number: ChiCTR-TRC-00000034, www.chictr.org). The study was conducted in accordance with the principles of the Declaration of Helsinki. The informed consents were obtained from the patients.
The purpose of this RCT was to investigate the role of laser peripheral iridotomy (LPI) with or without argon laser peripheral iridoplasty (ALPI) in patients with PACD; the methodology has been described in detail elsewhere[9]. As part of the RCT, all eligible subjects underwent a comprehensive ophthalmic examination including visual acuity, refraction, IOP (Goldmann applanation tonometry), slit-lamp examination, static and dynamic gonioscopy, fundus examination, and visual field (VF) testing (Humphrey Field Analyzer 750i, SITA fast strategy, 24-2 threshold test; Humphrey Instrument, San Leandro, California, USA).
Inclusion criteria were: 1) Eyes defined as PAC or PACG based on the International Society of Geographical and Epidemiological Ophthalnology (ISGEO) classification[10]. PAC was defined as non-visibility of the trabecular meshwork for ≥180° on gonioscopy with PAS and/or an IOP ≥21 mm Hg in the absence of GON. PACG was defined as PAC with evidence of GON. 2) Ability to undergo an ophthalmic examination.
Exclusion criteria were: 1) unwillingness or inability to provide consent; 2) prior intraocular surgical treatment; 3) history or signs of trauma to the eye; 4) any ocular disorders such as uveitis that could impact the structure or function of the drainage angle.
PAS was defined as adhesion of the iris stroma to the trabecular meshwork or higher that was at least half a clock hour in width. The presence and extent of PAS as determined by dynamic indentation gonioscopy was recorded. The examination of PAS was carried out at the lowest level of ambient illumination using a Goldmann-type two-mirror lens (Model OG3MS, Ocular instruments. Inc., USA). A 1-mm beam of light was reduced to a very narrow slit and was offset horizontally for assessing superior and inferior angles and vertically for nasal and temporal angles.
Gonioscopic angle width was graded in five categories (0=closed to 4=wide open) based on Shaffer's classification. The average Shaffer score width was determined by dividing the sum of all four quadrants by 4[11]. The ophthalmologist (Fan SJ) had a good agreement with (Liang YB) to determine the extent of PAS: 83.3% of 30 subjects with PAC or PACG were assessed between the 2 investigators as having less than 1 clock hour of PAS.
PAS was confirmed by good clinical ophthalmologist agreement as well as GON although with no anterior segment imaging device. GON was diagnosed on the basis of abnormality of the vertical cup-disc ratio (vCDR) of 0.7 or more and VF abnormalities present in the same eye. An abnormal VF, was defined as VF damage consistent with retinal nerve fiber layer (RNFL) damage or VF defects consistent with glaucomatous optic nerve damage[12]–[13].
Statistical Analysis
The predictor variable PAS was evaluated both as a continuous variable as well as a categorical variable in quartiles (Qs). If a subject's visual acuity and function precluded reliable VF testing, the diagnosis was made on the basis of an abnormal vCDR[10]. The association of PAS with IOP and prevalence of GON was first examined with smoothing plots (Proc Loess). As both eyes of each participant were eligible for inclusion, the independent effect of extent of PAS category on IOP and the probability of GON was determined using multivariable generalized estimating equation (GEE) models.
Covariates were selected based on the published literature. Adjustment for IOP assessed the independent effect of PAS on the prevalence of GON. Adjustments were performed for age, gender, spherical equivalent, average Schaffer score and the number of medications to determine the combined effects of PAS and IOP on GON. All statistical analyses were performed using SAS version 9.4 for Windows (SAS Institute, Cary, North Carolina, USA). P<0.05 was defined as the significant level.
RESULTS
A total of 355 eyes (238 PAC and 117 PACG) of 181 patients fulfilled the inclusion and exclusion criteria. The mean age was 63.4±8.2y and 67.6% were female.
The baseline characteristics in PAC patients and PACG patients are summarized in Table 1. Extent of PAS, IOP, mean defect (MD), spherical equivalent, average Shaffer score, and number of medications were significantly different between PAC and PACG. PAS was more extensive (8 vs 1 clock hour, P<0.001) and IOP higher (28.01 vs 18.00 mm Hg, P<0.001) in PACG compared to PAC.
Table 1. Characteristics of study eyes.
| Characteristics | PAC (n=238) | PACG (n=117) | P |
| Spherical equivalent (D) | 1.50 (0.75, 2.25) | 1.00 (-0.50, 2.00) | 0.001 |
| PAS (No. of clock hours) | 1.00 (0.00, 4.00) | 8.00 (3.50, 10.50) | <0.001 |
| IOP (mm Hg) | 18.00 (15.00, 24.00) | 28.01 (20.00, 46.00) | <0.001 |
| MD (dB) | 5.48 (4.61, 6.34) | 17.71 (15.35, 20.08) | <0.001 |
| Average Shaffer score | 1.00 (1.00, 1.63) | 1.00 (1.00, 1.00) | 0.010 |
| No. of medications, n (%) | 0.010 | ||
| 0 | 171 (71.85) | 90 (76.92) | |
| 1 | 28 (11.76) | 2 (1.71) | |
| 2 | 16 (6.72) | 8 (6.84) | |
| 3+ | 23 (9.66) | 17 (14.53) |
PAC: Primary angle closure; PACG: Primary angle-closure glaucoma; IOP: Intraocular pressure; PAS: Peripheral anterior synechia.
mean (95%CI)
The results of the multivariable GEE models are shown in Table 2. The prevalence of GON among the PAS quartiles were 10.2% (PAS<0.5 clock hours), 16.9% (PAS≥0.5 and PAS<3 clock hours), 29.6% (PAS≥3 and PAS<7 clock hours) and 74.4% (PAS≥7 clock hours), respectively. Compared to PAS<0.5 clock hours, the crude prevalence of GON was 3.7 (95%CI: 1.6-8.4) in eyes with PAS≥3 clock hours and 25.7 (95%CI: 11.0-60.0) with PAS≥7 clock hours. After adjusting for age, gender, eyes, spherical equivalent, average Shaffer score and number of medications, the prevalence was 5.4 (95%CI: 1.9-15.7) in eyes with PAS ≥3 clock hours and 22.7 (95%CI: 7.4-69.1) with PAS≥7 clock hours. After adjusting for IOP as well as the characteristics mentioned above the probability of GON remained significantly increased: OR=4.4 (95%CI: 1.5-13.0; P=0.007) for PAS≥3 clock hours and OR=13.8 (95%CI: 4.3-43.6; P<0.001) for PAS≥7 clock hours.
Table 2. Effect of peripheral anterior synechia (quartile) on GON.
| PAS (clock hours) | Eyes | GON, n (%) | Crude |
Model 1 |
Model 2 |
|||
| OR (95%CI) | P | OR (95%CI) | P | OR (95%CI) | P | |||
| Left eyea | ||||||||
| Q1 (0-0.5) | 56 | 2 (3.6) | 1.0 (1.0, 1.0) | Ref. | 1.0 (1.0, 1.0) | Ref. | 1.0 (1.0, 1.0) | Ref. |
| Q2 (0.5-3.0) | 35 | 7 (20.0) | 6.8 (1.3, 34.7) | 0.022 | 8.2 (0.8, 78.8) | 0.069 | 8.4 (0.8, 87.1) | 0.074 |
| Q3 (3.0-7.0) | 43 | 13 (30.2) | 11.7 (2.5, 55.4) | 0.002 | 15.9 (1.8, 139.5) | 0.013 | 13.3 (1.5, 120.8) | 0.022 |
| Q4 (7.0-12.0) | 45 | 31 (68.9) | 59.8 (12.7, 280.6) | <0.001 | 58.1 (6.2, 540.8) | <0.001 | 32.4 (3.3, 321.2) | 0.003 |
| Trend test | <0.001 | <0.001 | 0.001 | |||||
| Right eyea | ||||||||
| Q1 (0-0.5) | 52 | 9 (17.3) | 1.0 (1.0, 1.0) | Ref. | 1.0 (1.0, 1.0) | Ref. | 1.0 (1.0, 1.0) | Ref. |
| Q2 (0.5-3.0) | 24 | 3 (12.5) | 0.7 (0.2, 2.8) | 0.595 | 1.7 (0.3, 9.4) | 0.538 | 1.5 (0.2, 8.6) | 0.676 |
| Q3 (3.0-7.0) | 55 | 16 (29.1) | 2.0 (0.8, 4.9) | 0.154 | 3.7 (1.0, 13.3) | 0.048 | 2.9 (0.8, 11.1) | 0.115 |
| Q4 (7.0-12.0) | 45 | 36 (80.0) | 19.1 (6.9, 53.2) | <0.001 | 21.9 (5.2, 91.7) | <0.001 | 12.5 (2.8, 56.6) | 0.001 |
| Trend test | <0.001 | <0.001 | 0.001 | |||||
| Pooledb | ||||||||
| Q1 (0-0.5) | 108 | 11 (10.2) | 1.0 (1.0, 1.0) | Ref. | 1.0 (1.0, 1.0) | Ref. | 1.0 (1.0, 1.0) | Ref. |
| Q2 (0.5-3.0) | 59 | 10 (16.9) | 1.8 (0.7, 4.8) | 0.236 | 2.9 (0.9, 9.7) | 0.079 | 3.0 (0.9, 9.8) | 0.070 |
| Q3 (3.0-7.0) | 98 | 29 (29.6) | 3.7 (1.6, 8.4) | 0.002 | 5.4 (1.9, 15.7) | 0.002 | 4.4 (1.5, 13.0) | 0.007 |
| Q4 (7.0-12.0) | 90 | 67 (74.4) | 25.7 (11.0, 60.0) | <0.001 | 22.7 (7.4, 69.1) | <0.001 | 13.8 (4.3, 43.6) | <0.001 |
| Trend test | <0.001 | <0.001 | <0.001 | |||||
PAS: Peripheral anterior synechia; GON: Glaucomatous optic neuropathy; Model 1: Adjusted for age, gender, eyes, spherical equivalent, average Shaffer score and number of medications; Model 2: Model 1 and additional adjustment for IOP. aMultivariable generalized linear regression models were performed to assess the associations; bMultivariable generalized estimating equation models were applied to evaluate the associations.
The association between PAS and IOP with GON is shown in Table 3. Adjusting for age, gender, eyes, spherical equivalent, average Shaffer score and number of medications, the rate was 18.0 times higher (95%CI: 7.5-43.4; P<0.001) in eyes with both PAS≥6 clock hours and IOP≥21 mm Hg compared to eyes with PAS<6 clock hours and IOP<21 mm Hg. The OR was 8.2 for PAS≥6 clock hours compared to PAS<6 clock hours (95%CI: 4.4-15.3; P<0.001) and 5.2 for IOP≥21 mm Hg compared to IOP<21 mm Hg (95%CI: 2.6-10.4; P<0.001).
Table 3. Effect of peripheral anterior synechia, intraocular pressure, and their combined effect on the probability of GON.
| PAS≥6 | IOP≥21 (mm Hg) | Eyes | GON, n (%) | Crude |
Adjusted |
||
| OR (95%CI) | P | OR (95%CI) | P | ||||
| No | 239 | 40 (16.7) | 1.0 (1.0, 1.0) | Ref. | 1.0 (1.0, 1.0) | Ref. | |
| Yes | 116 | 77 (66.4) | 9.8 (5.8, 16.7) | <0.001 | 8.2 (4.4, 15.3) | <0.001 | |
| No | 189 | 35 (18.5) | 1.0 (1.0, 1.0) | Ref. | 1.0 (1.0, 1.0) | Ref. | |
| Yes | 166 | 82 (49.4) | 4.3 (2.6, 7.1) | <0.001 | 5.2 (2.6, 10.4) | <0.001 | |
| No | No | 161 | 21 (13.0) | 1.0 (1.0, 1.0) | Ref. | 1.0 (1.0, 1.0) | Ref. |
| No | Yes | 78 | 19 (24.4) | 2.1 (1.0, 4.5) | 0.040 | 2.7 (1.0, 6.8) | 0.034 |
| Yes | No | 28 | 14 (50.0) | 6.7 (3.1, 14.4) | <0.001 | 4.7 (2.0, 10.8) | 0.001 |
| Yes | Yes | 88 | 63 (71.6) | 16.8 (8.5, 33.4) | <0.001 | 18.0 (7.5, 43.4) | <0.001 |
PAS: Peripheral anterior synechia; IOP: Intraocular pressure; GON: Glaucomatous optic neuropathy. Adjusted for age, gender, eyes, spherical equivalent, average Shaffer score and the number of medications.
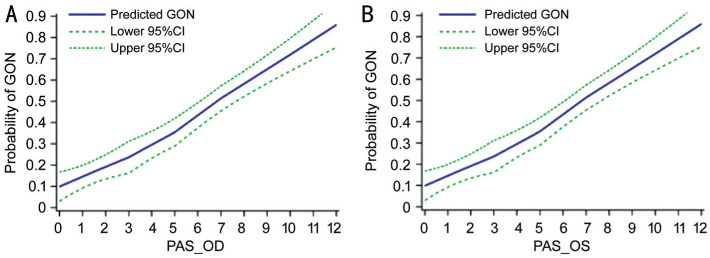
After adjusting for age, gender, spherical equivalent, average Shaffer score, number of medications and IOP, the prevalence of GON increased linearly with increase in extent of PAS; this was true for both right and the left eyes (Figure 1).
Figure 1. Association between PAS and the prevalence of GON in PACD.
A: The graph displays the crude association between PAS and the prevalence of GON in right eyes; B: The graph displays the crude association between PAS and the prevalence of GON in left eyes. The curves (95%CI indicated by dotted lines) were derived from smoothing plots (Proc Loess).
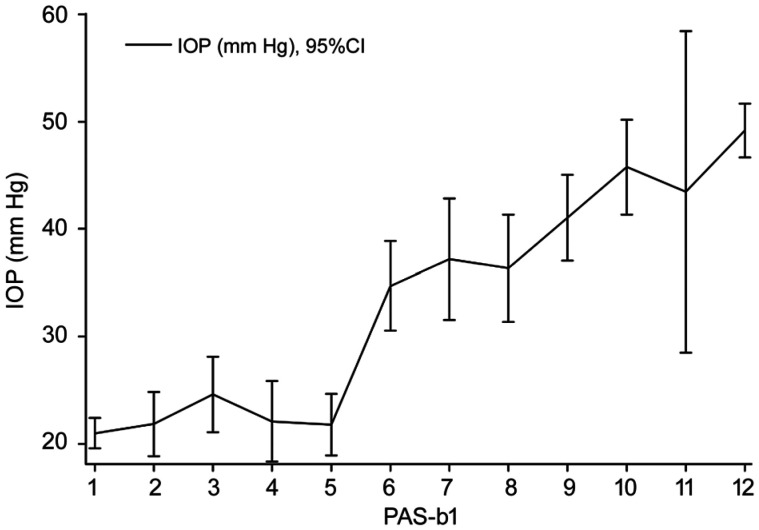
Figure 2 demonstrates that extent of PAS is related to higher IOP. The presence of 5 clock hours to 6 clock hours of PAS seems to be a turning point of IOP.
Figure 2. Distribution of IOP with clock hours of PAS.
PAS=6 seems the cut-off point for increase in pressure.
DISCUSSION
Our research demonstrated PAS is significantly more extensive in PACG patients than in PAC patients and the probability of GON is linearly associated with PAS. It is of great clinical significance that PAS could be a surrogate of PACG prevention or a predicator of GON development. There were a few surveys demonstrating that PAS were significantly associated with IOP and GON in PACG[6]–[7]. In a population based survey of Mongolian people, 16.7% with PAS had GON compared with 0.9% without PAS[14]. There was a 0.39 mm Hg increase in untreated IOP for each unit increase in clock hours of PAS. Odds of GON increased 1.2 times per 1-mm Hg increase in screening IOP. Choi and Kim[15] suggested that the extent of PAS may be regarded as a reliable indicator of the severity of GON in PACG, and especially in chronic PACG. Spearman's correlation coefficient between the severity of VF defects and the extent of PAS was 0.348[15].
It is noteworthy that PAS was found to be independently associated with GON in our study, although with IOP as well as other characteristics such as age, gender, eyes, spherical equivalent, average Shaffer score, and the number of medications had been adjusted, which confirms that PAS is an important risk factor for the development of GON independent of IOP. Comparing with PAS<0.5 clock hours, probability of GON significantly increased while PAS≥3 clock hours (adjusted OR=4.4; 95%CI, 1.5-13.0), especially while PAS≥7 clock hours (adjusted OR=13.8; 95% CI, 4.3-43.6). The finding implied there may be some other mechanisms which have not been discovered previously where PAS can lead to GON solely and not because of higher IOP, emphasizing the need for careful examination of PAS in PAC diseases. It may be that the extent of PAS indicates the importance of the duration, in relation to GON, since the duration of PACG was not available. The more extensive the PAS was, the more chronic the disease process in PACG patients might have been and higher the probability of developing GON[15]. Inflammation factors such as tumor necrosis factor-α (TNF-α), interleukins (ILs), nuclear factor-kappa B (NF-κB) and various cytokines which may increase the susceptibility of optic nerve by leading to the death of the retinal ganglion cells (RGCs) are also considered to be associated with the development of PAS[16]–[17].
There seems to be no doubt that PAS is a risk factor for increased IOP and GON in PACG. To the best of our knowledge, PAS leads to permanent blockage of the access to the trabecular meshwork, while intermittent blockage happens in appositional angle closure. If untreated, PAS will extend and become confluent. In addition, the decrease of PAS signifies long-term well controlled IOP and GON. It was recorded that in eyes with synechial PAC or PACG, both LPI alone or combined with ALPI provided a significant and equivalent reduction in IOP, but combined laser technique released more of the PAS rather than LPI alone[18]. Goniosynechialysis (GSL) was demonstrated effective in eyes with broad PAS as a surgical technique to strip the PAS from the trabecular surface in the angle so that aqueous can regain access to the meshwork[19]–[20]. In PACG patients with concomitant cataract, phacoemulsification plus GSL or phacoemulsification alone may suffice to achieve medically well-controlled eyes with minimal PAS, and if not then trabeculectomy should be considered.
The approach to management of PACG varies greatly in different parts of the world. In most parts of the world, LPI is the preferred standard first-line treatment for PACG[21]–[23]. In China, trabeculectomy is a mainstay of initial treatment for PACG and that decision was mainly based on the degree of PAS. LPI is only reserved for PAC with PAS<180°[24]. Nevertheless, this threshold of PAS was based on the experiences of clinicians. Figure 2 of distribution of IOP with PAS showed that 5 to 6 clock hours of PAS seemed to be an obvious turning point for higher IOP. Furthermore, eyes with both PAS≥6 clock hours and IOP≥21 mm Hg had the highest risk of GON compared to eyes both with PAS<6 clock hours and IOP<21 mm Hg (OR=18.0, 95%CI: 7.5-43.4; P<0.001). This result was consistent with the viewpoint of Lai et al[25] that the main objectives of a surgical treatment in PACG were the reduction of the IOP, the reopening of the closed angle, and the prevention of a progressive angle closure or reclosure. It is worth mentioning that this study may offered some evidence for threshold of 180° of PAS, which seemed to be a guide to the likely success or failure of treatment in PAC diseases that IOP was more likely to be successful after LPI, or phacoemulsification alone if the PAS<180°[23],[26]–[28].
Our study has some limitations. PAS was documented by gonioscopy and the total clock hours of PAS were recorded. We didn't record the adhesiveness of the PAS to the trabeculum and the trabecular function, which may also affect IOP. The duration, which was usually difficult to retrospect accurately for PAC patients, especially for chronic PACG patients, can't be adjusted in these models. But still, this study demonstrated that PAS was obviously associated with GON independent of IOP, which was considered as the medium of PAS and GON previously.
The presence of 5 to 6 clock hours of PAS seemed to be a turning point of IOP. PAS can be considered as an important predictor of high IOP for PAC diseases, and the turning point seemed to be 5 to 6 clock hours.
In conclusion, PAS was significantly associated with IOP and GON in PAC diseases. There may be some other mechanisms have not been discovered previously that PAS can lead to GON independent of IOP.
Acknowledgments
Foundations: Supported by Health Innovation Talents in Zhejiang Province (No.2016025); Wenzhou Medical University R&D Fund (No.QTJ13009).
Conflicts of Interest: Zhang M, None; Mao GY, None; Ye C, None; Fan SJ, None; Liang YB, None; Wang NL, None.
REFERENCES
- 1.Lewis CJ, Hedberg-Buenz A, DeLuca AP, Stone EM, Alward WLM, Fingert JH. Primary congenital and developmental glaucomas. Hum Mol Genet. 2017;26(R1):R28–R36. doi: 10.1093/hmg/ddx205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sun XH, Dai Y, Chen YH, Yu DY, Cringle SJ, Chen JY, Kong XM, Wang XL, Jiang CH. Primary angle closure glaucoma: what we know and what we don't know. Prog Retin Eye Res. 2017;57:26–45. doi: 10.1016/j.preteyeres.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 3.Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–2090. doi: 10.1016/j.ophtha.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 4.Song PG, Wang JW, Bucan K, Theodoratou E, Rudan I, Chan KY. National and subnational prevalence and burden of glaucoma in China: a systematic analysis. J Glob Health. 2017;7(2):020705. doi: 10.7189/jogh.07.020705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Y, Li SZ, Li L, He MG, Thomas R, Wang NL. Dynamic iris changes as a risk factor in primary angle closure disease. Invest Ophthalmol Vis Sci. 2016;57(1):218–226. doi: 10.1167/iovs.15-17651. [DOI] [PubMed] [Google Scholar]
- 6.Thomas R, George R, Parikh R, Muliyil J, Jacob A. Five year risk of progression of primary angle closure suspects to primary angle closure: a population based study. Br J Ophthalmol. 2003;87(4):450–454. doi: 10.1136/bjo.87.4.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee JY, Kim YY, Jung HR. Distribution and characteristics of peripheral anterior synechiae in primary angle-closure glaucoma. Korean J Ophthalmol. 2006;20(2):104–108. doi: 10.3341/kjo.2006.20.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Foster PJ, Machin D, Wong TY, Ng TP, Kirwan JF, Johnson GJ, Khaw PT, Seah SK. Determinants of intraocular pressure and its association with glaucomatous optic neuropathy in Chinese Singaporeans: the Tanjong Pagar Study. Invest Ophthalmol Vis Sci. 2003;44(9):3885–3891. doi: 10.1167/iovs.03-0012. [DOI] [PubMed] [Google Scholar]
- 9.Sun X, Liang YB, Wang NL, Fan SJ, Sun LP, Li SZ, Liu WR. Laser peripheral iridotomy with and without iridoplasty for primary angle-closure glaucoma: 1-year results of a randomized pilot study. Am J Ophthalmol. 2010;150(1):68–73. doi: 10.1016/j.ajo.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 10.Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86(2):238–242. doi: 10.1136/bjo.86.2.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaffer RN. A suggested anatomic classification to define the pupillary block glaucomas. Invest Ophthalmol. 1973;12(7):540–542. [PubMed] [Google Scholar]
- 12.Melgarejo JD, Lee JH, Petitto M, et al. Glaucomatous optic neuropathy associated with nocturnal dip in blood pressure: findings from the Maracaibo aging study. Ophthalmology. 2018;125(6):807–814. doi: 10.1016/j.ophtha.2017.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hood DC, De Moraes CG. Efficacy of a deep learning system for detecting glaucomatous optic neuropathy based on color fundus photographs. Ophthalmology. 2018;125(8):1207–1208. doi: 10.1016/j.ophtha.2018.04.020. [DOI] [PubMed] [Google Scholar]
- 14.Foster PJ, Aung T, Nolan WP, Machin D, Baasanhu J, Khaw PT, Alsbirk PH, Lee PS, Seah SK, Johnson GJ. Defining “occludable” angles in population surveys: drainage angle width, peripheral anterior synechiae, and glaucomatous optic neuropathy in east Asian people. Br J Ophthalmol. 2004;88(4):486–490. doi: 10.1136/bjo.2003.020016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Choi JS, Kim YY. Relationship between the extent of peripheral anterior synechiae and the severity of visual field defects in primary angle-closure glaucoma. Korean J Ophthalmol. 2004;18(2):100–105. doi: 10.3341/kjo.2004.18.2.100. [DOI] [PubMed] [Google Scholar]
- 16.Almasieh M, Wilson AM, Morquette B, Cueva Vargas JL, Di Polo A. The molecular basis of retinal ganglion cell death in glaucoma. Prog Retin Eye Res. 2012;31(2):152–181. doi: 10.1016/j.preteyeres.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Husain R, Do T, Lai J, Kitnarong N, Nongpiur ME, Perera SA, Ho CL, Lim SK, Aung T. Efficacy of phacoemulsification alone vs phacoemulsification with goniosynechialysis in patients with primary angle-closure disease: a randomized clinical trial. JAMA Ophthalmol. 2019;137(10):1107–1113. doi: 10.1001/jamaophthalmol.2019.2493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wright C, Tawfik MA, Waisbourd M, Katz LJ. Primary angle-closure glaucoma: an update. Acta Ophthalmol. 2016;94(3):217–225. doi: 10.1111/aos.12784. [DOI] [PubMed] [Google Scholar]
- 19.Lee JY, Berrocal AM, Grajewski AL, Chang TC. Juvenile angle closure management: the role of lens extraction and goniosynechialysis. Am J Ophthalmol Case Rep. 2020;19:100808. doi: 10.1016/j.ajoc.2020.100808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rodrigues IA, Alaghband P, Beltran Agullo L, Galvis E, Jones S, Husain R, Lim KS. Aqueous outflow facility after phacoemulsification with or without goniosynechialysis in primary angle closure: a randomised controlled study. Br J Ophthalmol. 2017;101(7):879–885. doi: 10.1136/bjophthalmol-2016-309556. [DOI] [PubMed] [Google Scholar]
- 21.Elisa B. Glaucoma treatment. La Revue Du Praticien. 2016;66(5):508–513. [PubMed] [Google Scholar]
- 22.Liebmann JM, Ritch R. Laser surgery for angle closure glaucoma. Semin Ophthalmol. 2002;17(2):84–91. doi: 10.1076/soph.17.2.84.14720. [DOI] [PubMed] [Google Scholar]
- 23.Thomas R, Walland MJ. Management algorithms for primary angle closure disease. Clin Exp Ophthalmol. 2013;41(3):282–292. doi: 10.1111/j.1442-9071.2012.02885.x. [DOI] [PubMed] [Google Scholar]
- 24.Chinese Glaucoma Society. Glaucoma Practice Guideline (2005) Chin J Ophthalmol. 2005;41:1140–1143. [Google Scholar]
- 25.Lai J, Choy BN, Shum JW. Management of primary angle-closure glaucoma. Asia Pac J Ophthalmol (Phila) 2016;5(1):59–62. doi: 10.1097/APO.0000000000000180. [DOI] [PubMed] [Google Scholar]
- 26.Zhou WB. Stages of primary pupil-block chronic angle-closure glaucoma. Zhonghua Yan Ke Za Zhi. 1993;29(2):114–116. [PubMed] [Google Scholar]
- 27.Tham CC, Kwong YY, Leung DY, Lam SW, Li FC, Chiu TY, Chan JC, Lam DS, Lai JS. Phacoemulsification versus combined phacotrabeculectomy in medically uncontrolled chronic angle closure glaucoma with cataracts. Ophthalmology. 2009;116(4):725–731. 731.e1–3. doi: 10.1016/j.ophtha.2008.12.054. [DOI] [PubMed] [Google Scholar]
- 28.Nolan WP, Foster PJ, Devereux JG, Uranchimeg D, Johnson GJ, Baasanhu J. YAG laser iridotomy treatment for primary angle closure in east Asian eyes. Br J Ophthalmol. 2000;84(11):1255–1259. doi: 10.1136/bjo.84.11.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]