Abstract
The burden of morbidity among privately insured transgender people is largely unknown. We identified transgender people enrolled in private insurance (using claims from 2001–19) and compared their rates of selected chronic conditions, using the Elixhauser Comorbidity Index, with claims for a matched cisgender cohort. We documented disparities between transgender and cisgender people across most conditions and found that transgender people were at elevated risk for nearly all chronic conditions compared with their cisgender counterparts. We also found that trans masculine and nonbinary people had the highest predicted average number of chronic conditions compared with all other gender groups. Our findings highlight key gender differences in morbidity between and within transgender and cisgender populations, and they underscore the importance of collecting gender identity information in national surveillance efforts to increase understanding of the health disparities among transgender and cisgender populations. In addition, these findings underscore the need for nondiscrimination protections for transgender people in the US.
Some US health surveillance systems have begun to collect gender identity information that allows for the identification of transgender populations. However, the collection of gender identity information is often limited to specific states1 or focused on specific health conditions such as HIV/AIDS.2 Without robust surveillance systems, researchers are left with a dearth of resources to understand the risk for morbidity in transgender populations and have turned to alternative data sources, such as insurance claims data, to characterize the health of transgender populations.3 Building on original work by John Blosnich and colleagues4 and Kimberly Proctor and colleagues,5 researchers have advanced algorithms using insurance claims to identify transgender people in national data sets. Most often, these algorithms have been used to identify transgender people in federal insurance programs such as Medicare5–7 and the Department of Veterans Affairs,4,8 which represent disproportionably older and disabled people and veterans, respectively.
Given that the majority of transgender people in the US are privately insured,9 commercial insurance data provide an opportunity to understand the health of large segments of the transgender population. Recently, Alex McDowell and colleagues10 drew on the algorithms from Proctor and colleagues5 and Blosnich and colleagues4 to identify privately insured transgender people in the IBM MarketScan Commercial database and found higher rates of mental health diagnoses, substance use disorders, and hypertension among transgender populations compared with their cisgender counterparts. In 2020 Guneet Jasuja and colleagues3 used a private insurance database to study health conditions, developing an algorithm that allowed for the exploration of conditions among trans feminine and nonbinary people (those assigned a male sex at birth who may identify along the nonbinary-to-feminine gender spectrum and who have received feminizing hormones or surgery) and trans masculine and nonbinary people (those assigned a female sex at birth who may identify along the nonbinary-to-masculine gender spectrum and who have received masculinizing hormones or surgery). Across transgender people in particular, Jasuja and colleagues found that compared with trans masculine and nonbinary people, trans feminine and nonbinary people had a higher prevalence of nearly every chronic health condition, including diabetes, alcohol and drug use disorders, and HIV/AIDS. In this study we extended the work of Jasuja and colleagues3 by exploring the morbidity of transgender people relative to that of cisgender people and the differences across subgroups (for example, trans feminine and nonbinary or trans masculine and nonbinary versus cisgender men or cisgender women). Such data are needed to fully understand disparities among transgender people and their cisgender counterparts.
In this article we document the morbidity of transgender populations relative to cisgender populations and compare within- and between-group differences according to gender subgroup in private insurance claims from the period 2001–19. Findings from this study can provide important information on the burden of chronic health conditions for a sizeable portion of the US transgender population9 and can help identify specific health conditions that should be addressed in future intervention efforts.
Study Data And Methods
We conducted a retrospective analysis of administrative data from Optum’s Clinformatics Data Mart Database, which included deidentified insurance claims for privately insured people and Medicare Advantage (Medicare managed care) enrollees from the period 2001–19.
SAMPLE
We identified transgender people using an augmented version of the algorithm from Jasuja and colleagues3 that was adapted by Jaclyn Hughto and colleagues for use in Medicare and Medicaid data.11 Transgender people were identified using common diagnoses (gender dysphoria and gender identity disorder) and procedures (using Current Procedural Terminology, or CPT, codes), as well as claims for gender-affirming care during 2001–19. This algorithm included people who received a diagnosis of endocrine disorder not otherwise specified in conjunction with hormone prescriptions or transgender-specific surgeries. “Endocrine disorder not otherwise specified” is often used to bill for transgender-affirming services instead of gender identity disorder to avoid the stigma of labeling the person as transgender or to avoid denials of payment;3 thus, the use of this code enables the identification of transgender people who would not otherwise be identified via the algorithms from Proctor and colleagues,5 Blosnich and colleagues,4 or McDowell and colleagues10 In addition, by incorporating the use of hormones and procedures, the algorithm we used allows for the stratification of gender subgroups (that is, trans feminine and nonbinary and trans masculine and nonbinary people). The observed period included October 2015, when medical claims coding changed from International Classification of Diseases, Ninth Revision (ICD-9), to International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10), codes.
All people identified as transgender were included in the analyses, and a 10 percent random sample of the remaining people was pulled for analyses and labeled as “cisgender.” We required that all people included in our analyses have at least one inpatient or outpatient claim. Race/ethnicity, age, and census region have been associated with rates of morbidity in the US;12,13 therefore, we matched the transgender cohort to a cisgender cohort by race/ethnicity, census region, and year of birth. We also matched on the number of years with at least one inpatient or outpatient claim to ensure that the cisgender sample was similarly engaging with care compared with the transgender cohort. As a result of improved diagnostic tools or increasing prevalence, the rates for specific morbid conditions varied during the period;14,15 to control for these time-varying confounds, we also matched on the year of enrollment and the year that enrollment ended to ensure that the observed period was the same between the two cohorts. All matches were forced to be exact.
CHRONIC CONDITIONS
Diagnoses were identified using ICD-9 and ICD-10 codes from the period 2001–19. Codes used for each condition were calculated using the Elixhauser Comorbidity Index.12,16 Several conditions were combined for ease of interpretation (for example, complicated and uncomplicated hypertension, complicated and uncomplicated diabetes, deficiency and blood loss anemia, and cancer diagnoses). If a person was diagnosed with any of the ICD codes falling under an Elixhauser category during the study period, they were counted as having that condition. A summarized measure of morbidity, or total morbidity score, was created by summing the totals for each of the twenty-six categories for each person. Thus, the lowest possible score a person may have was 0 and the highest was 26.
COVARIATES
Information on birth year and gender was collected via an enrollment questionnaire completed by participants or their guardians at the start of their enrollment period. For protected health information purposes, Optum reported birth year instead of specific dates. Gender was used to classify cisgender people as either cisgender women or cisgender men, with those selecting “female” being classified as cisgender women and those selecting “male” being classified as cisgender men. Using the modified algorithm outlined by Hughto and colleagues,11 gender among transgender people was determined on the basis of the use of feminizing and masculinizing procedures and the gender marker at enrollment. For transgender people, gender was categorized as trans masculine and nonbinary, trans feminine and nonbinary, or unknown. Race/ethnicity data were collected via self-report or derived from a combination of public records, transactions, and consumer surveys. Race/ethnicity was coded into five categories: Asian, Black, Hispanic, unknown, or White. Membership files provided by Optum included the coverage start and end dates as well as the state of residence for each person. Enrollment start year was coded as the year a person began their insurance coverage and enrollment end year was the year in which their coverage ended. Census region was coded using state of residence and coded as Midwest, Northeast, South, or West.
STATISTICAL ANALYSES
Statistical analyses were conducted using Stata/MP, version 14.2. Cisgender people were matched to transgender people using exact matching on the covariates mentioned above. The number of cisgender people was reweighted to reflect the number of transgender people to whom they were matched and the number of cisgender people per transgender match. Therefore, the weighted number of cisgender people matched the actual number of transgender people.
We tested whether the transgender and cisgender groups were statistically different on the demographic characteristics, using regression techniques (linear for continuous outcomes and logistic for dichotomous outcomes) to apply the matched weights. In comparisons of the predicted probability of specific morbidities between the transgender and cisgender cohorts, logistic regression models were fit, predicting the likelihood of each condition by transgender status and applying the matched weights. Predicted probabilities were calculated using Stata’s margins command by transgender status. A similar approach was used to examine the difference between transgender and cisgender cohorts on the Elixhauser Comorbidity Index, reported as the total morbidity score, except linear regression was used instead of logistic.
For analyses of chronic conditions by gender, logit models were fit predicting the likelihood of each condition by gender and age while applying the matched weights. Predicted probabilities were calculated using Stata’s margins command by gender. A similar approach was used to examine the total morbidity score, with linear regression used instead of logistic.
LIMITATIONS
Findings must be interpreted in light of several limitations. Algorithms used to identify transgender people in insurance data have been validated as highly specific in work by Proctor and colleagues,5 but they are likely insensitive because not all transgender people seek gender-affirming health care, gender-affirming health care is heterogenous within transgender populations, in some cases gender-affirming health care is indistinguishable from routine health care, and not all transgender people with insurance access gender-affirming care because of a lack of availability or trust in medical care systems. Given this limitation, we cannot guarantee that this sample is fully representative of transgender people who were insured during the study period; rather, it represents a subset of insured transgender people who were engaged in a particular set of gender-affirming health care practices. Furthermore, transgender populations are more likely to be uninsured than the general population;9 thus, these findings are not representative of the total transgender population.
The standards of care for accessing gender-affirming medical care require transgender people to meet with a mental health practitioner before accessing hormones and surgeries. Therefore, the elevated rates of mental health conditions among the transgender cohort maybe driven by this requirement rather than by actual prevalence.17 Researchers have found that transgender people are likely to experience discrimination, harassment, and violence within medical settings that may incentivize going without care or accessing care outside of traditional sources.9,18,19 Therefore, our sample may represent a healthier subset of transgender people than all privately insured transgender people, biasing our findings in favor of the null.
Last, misclassification of the transgender and cisgender cohort may have occurred. We took steps to minimize this occurrence; regardless, in light of the fact that the size of the US transgender population is estimated to be 0.6 percent,20 the inclusion of some transgender people in the cisgender sample is unlikely to meaningfully affect estimates of reported chronic conditions within our cisgender sample.
Study Results
Exhibit 1 displays the weighted means and percentages of the cohorts’ characteristics. Given our matching process, there are no significant differences between the cohorts on age at enrollment, years with at least one claim, race/ethnicity, and census region. Our cohort is mostly White (64 percent), followed by uncategorized race (20 percent), Hispanic (7 percent), Black (7 percent), and Asian (2 percent). A plurality of the sample lives in the South (41 percent), followed by the West, Midwest, and Northeast. The average age at the time of enrollment was thirty-two. Among the transgender sample, 89 percent were enrolled in private coverage, and 11 percent were enrolled in a Medicare Advantage plan. Among the cisgender sample, 91 percent were enrolled in private coverage, and 9 percent were enrolled in a Medicare Advantage plan (data not shown). As shown in exhibit 2, we identified more transgender people per year, on average, in the years post-2015, similar to the findings of Erin Ewald and colleagues,21 indicating that, on average, more transgender people were identified in the years after the implementation of ICD-10.
EXHIBIT 1:
Characteristics of matched transgender and cisgender cohorts in US commercial insurance plans, weighted, 2001–19
| Transgender (n = 36,069) | Cisgender (n = 1,263,420) | |
|---|---|---|
| Enrollment timing and claims (weighted mean) | ||
| Age at enrollment, years | 32 | 32 |
| Years enrolled | 4.9 | 4.9 |
| Years with at least 1 claim | 5 | 5 |
| Race (weighted %) | ||
| Asian | 1.8 | 1.8 |
| Black | 6.8 | 6.8 |
| Hispanic | 7.2 | 7.2 |
| Unknown | 20.3 | 20.3 |
| White | 64.0 | 64.0 |
| Census region at enrollment (weighted %) | ||
| Midwest | 24.1 | 24.1 |
| Northeast | 9.6 | 9.6 |
| South | 40.8 | 40.8 |
| West | 25.4 | 25.4 |
source Authors’ analysis derived from administrative data from Optum’s Clinformatics Data Mart Database, 2001–19. note The data source included deidentified insurance claims for privately insured and Medicare Advantage enrollees.
EXHIBIT 2. Number of transgender enrollees in US commercial insurance plans, by enrollment start year, 2001–19.
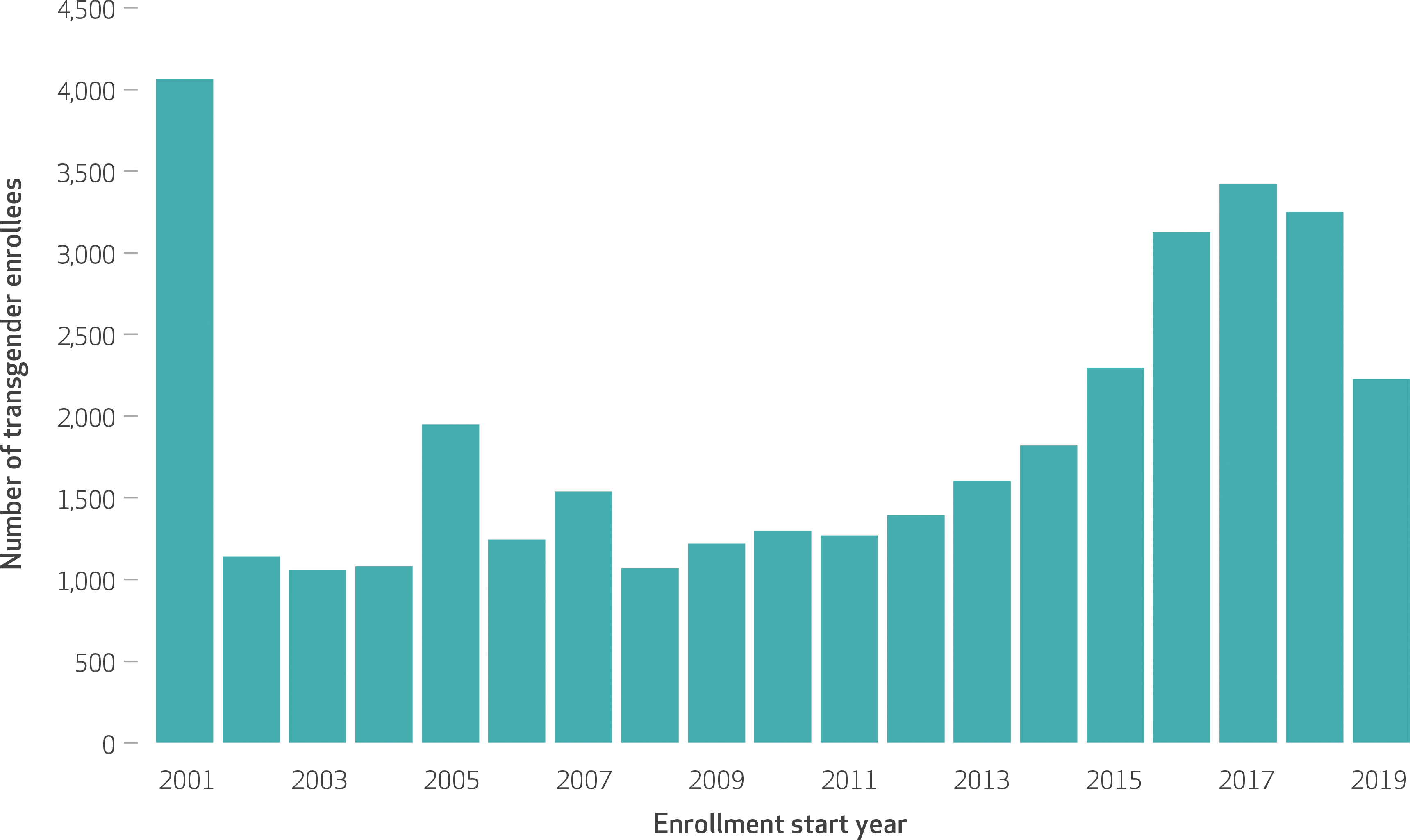
source Authors’ analysis derived from administrative data from Optum’s Clinformatics Data Mart Database, 2001–19. note The data source included deidentified insurance claims for privately insured and Medicare Advantage enrollees.
Exhibit 3 presents the weighted predicted means and probabilities of chronic conditions by transgender status. Overall, transgender people are at a greater risk for morbidity, as measured by their total morbidity score, than their cisgender counterparts (3.0 versus 2.0). Furthermore, we found that transgender people were at a significantly greater risk (p < 0.001) for nearly all chronic conditions studied. Comparing cardiovascular conditions, transgender people had a higher rate of cardiac arrhythmia (17.3 percent versus 12.6 percent) and congestive heart failure (5.0 percent versus 3.7 percent) than the matched cisgender cohort. Regarding the rates of neurological conditions, the transgender cohort experienced greater risk for paralysis (1.3 percent versus 1.0 percent) and other neurological disorders (8.1 percent versus 5.3 percent) than their cisgender counterparts.
EXHIBIT 3:
Predicted means and probabilities of chronic conditions among enrollees in US commercial insurance plans, by transgender status, weighted, 2001–19
| Transgender | Cisgender | |
|---|---|---|
| Total morbidity score (mean) | 3.00 | 1.99 |
| Cardiovascular conditions (%) | ||
| Hypertension | 27.27 | 32.64 |
| Cardiac arrhythmia | 17.25 | 12.56 |
| Valvular disease | 8.96 | 7.50 |
| Peripheral vascular disorders | 7.31 | 8.06 |
| Congestive heart failurea | 4.95 | 3.68 |
| Coagulopathy | 4.44 | 3.03 |
| Pulmonary circulation disorders | 2.88 | 2.24 |
| Neurological conditions (%) | ||
| Other neurological disorders | 8.09 | 5.34 |
| Paralysis | 1.30 | 0.97 |
| Weight, diabetic, and thyroid conditions (%) | ||
| Obesity | 21.87 | 15.62 |
| Fluid and electrolyte disorders | 15.54 | 10.16 |
| Hypothyroidism | 19.13 | 12.90 |
| Diabetes | 12.88 | 13.90 |
| Abnormal weight loss | 7.80 | 4.35 |
| Mental health and substance use (%) | ||
| Depression | 56.46 | 19.86 |
| Drug use disorder | 8.12 | 3.21 |
| Psychoses | 5.81 | 1.44 |
| Alcohol use disordera | 5.25 | 3.20 |
| Other chronic conditions (%) | ||
| Chronic pulmonary disease | 26.29 | 18.13 |
| Blood loss or deficiency anemia | 10.75 | 6.54 |
| Liver diseasea | 9.22 | 5.97 |
| Renal failurea | 5.61 | 4.06 |
| Rheumatoid arthritis/collagen | 7.88 | 5.30 |
| Cancerb | 5.12 | 5.05 |
| AIDS/HIV | 1.51 | 0.29 |
| Peptic ulcer disease excluding bleeding | 2.13 | 1.25 |
source Authors’ analysis derived from administrative data from Optum’s Clinformatics Data Mart Database, 2001–19. notes The data source included deidentified insurance claims for privately insured and Medicare Advantage enrollees. Total morbidity score was determined using the Elixhauser Comorbidity Index. The underlying transgender numbers vary as a result of our transgender identification criteria, as some chronic condition and transgender exclusion codes overlap with those of the Elixhauser Comorbidity Index. So as to not bias our estimates downward, we removed people from our calculations who were identified as transgender only because they fell into an inclusion category that required that they did not have the condition being analyzed. See Jasuja GK, et al., note 3 in text, for more detail. Sample sizes are in exhibit 1 except where noted. p < 0.001 for all variables.
Transgender n = 35,631.
Transgender n = 31,124.
Across most weight, diabetic, and thyroid conditions, the transgender cohort experienced greater rates of morbidity than their cisgender comparisons. Of particular note, transgender people were at a greater risk for obesity (21.9 percent versus 15.6 percent) and abnormal weight loss (7.8 percent versus 4.4 percent) than their cisgender counterparts. Some of the greatest disparities between the transgender and cisgender cohorts were found when analyzing the rates of mental health and substance use conditions. Transgender cohorts were much more likely to experience depression (54.5 percent versus 19.9 percent), psychoses (5.8 percent versus 1.4 percent), and drug use disorder (8.1 percent versus 3.2 percent) than their cisgender counterparts. Comparing other chronic conditions, transgender people were at a greater risk for all measured conditions than their cisgender counterparts. In particular, transgender people were at a greater risk for chronic pulmonary disease (26.3 percent versus 18.1 percent), AIDS/HIV (1.5 percent versus 0.3 percent), and renal failure (5.6 percent versus 4.1 percent) compared with their cisgender counterparts. Furthermore, transgender people were at higher risk for blood loss or deficiency anemia (10.8 percent versus 6.5 percent) than their cisgender counterparts.
Exhibit 4 presents the weighted and age-adjusted predicted means and probabilities of chronic conditions by gender. Online appendix exhibit 1 shows the statistical significance of differences between the predicted means and probabilities of conditions among the transgender and cisgender gender groups.22 Overall, trans masculine and nonbinary people had a significantly higher total morbidity score (3.5) than all other gender groups. Trans feminine and nonbinary people had higher total morbidity scores than both cisgender men and cisgender women (2.6,1.9, and 2.1, respectively). Trans masculine and nonbinary people were at the greatest risk for nineteen of the twenty-six conditions, with the greatest relative disparity being rheumatoid arthritis when compared with the other groups. When we compared cardiovascular conditions, both trans feminine and nonbinary people and trans masculine and nonbinary people were at greater risk for hypertension than cisgender men and women. Trans masculine and nonbinary people were at more risk for peripheral vascular disorders but at less risk for congestive heart failure than cisgender men. When we compared rates of neurological conditions, both trans feminine and nonbinary people and trans masculine and nonbinary people were at a higher risk for other neurological disorders than both cisgender men and women (6.4, 8.0, 4.9, and 5.0, respectively).
EXHIBIT 4:
Predicted means and probabilities of chronic conditions among enrollees in US commercial insurance plans, by gender spectrum, weighted and age adjusted, 2001–19
| TFN (n = 5,796) | TMN (n = 10,682) | Cisgender men (n = 547,771) | Cisgender women (n = 715,501) | |
|---|---|---|---|---|
| Total morbidity score (mean) | 2.62 | 3.50 | 1.89 | 2.08 |
| Cardiovascular conditions (%) | ||||
| Hypertension | 28.50 | 29.93 | 22.90 | 27.89 |
| Cardiac arrhythmia | 13.96 | 19.83 | 12.25 | 11.68 |
| Valvular disease | 6.45 | 12.22 | 6.30 | 6.69 |
| Peripheral vascular disorders | 6.09 | 6.53 | 5.97 | 5.22 |
| Congestive heart failure® | 3.04 | 3.38 | 4.18 | 3.28 |
| Coagulopathy | 4.05 | 4.86 | 2.90 | 2.81 |
| Pulmonary circulation disorders | 2.16 | 2.27 | 1.75 | 1.78 |
| Neurological conditions (%) | ||||
| Other neurological disorders | 6.40 | 8.00 | 4.86 | 5.04 |
| Paralysis | 1.05 | 1.07 | 1.01 | 0.86 |
| Weight, diabetic, and thyroid conditions (%) | ||||
| Obesity | 19.17 | 26.68 | 14.73 | 17.50 |
| Fluid and electrolyte disorders | 13.89 | 17.95 | 9.20 | 10.70 |
| Hypothyroidism | 12.51 | 30.82 | 7.40 | 16.34 |
| Diabetes | 12.09 | 13.24 | 11.69 | 9.97 |
| Abnormal weight loss | 5.99 | 8.59 | 4.40 | 5.01 |
| Mental health and substance use (%) | ||||
| Depression | 51.85 | 53.54 | 18.68 | 27.85 |
| Drug use disorder | 8.66 | 7.02 | 4.56 | 3.22 |
| Psychoses | 5.04 | 4.12 | 1.73 | 1.79 |
| Alcohol use disordera | 5.49 | 4.17 | 4.35 | 2.29 |
| Other chronic conditions (%) | ||||
| Chronic pulmonary disease | 20.79 | 31.92 | 19.73 | 21.57 |
| Blood loss or deficiency anemia | 6.28 | 15.58 | 4.39 | 8.61 |
| Liver diseasea | 6.85 | 13.31 | 6.18 | 5.79 |
| Renal failurea | 4.22 | 3.57 | 4.50 | 3.72 |
| Rheumatoid arthritis/collagen | 3.93 | 13.83 | 3.89 | 6.87 |
| Cancerb | 4.95 | 3.04 | 5.03 | 5.06 |
| AIDS/HIV | 3.00 | 0.35 | 0.58 | 0.14 |
| Peptic ulcer disease excluding bleeding | 1.17 | 3.31 | 1.21 | 1.38 |
source Authors’ analysis derived from administrative data from Optum’s Clinformatics Data Mart Database, 2001–19. notes The data source included deidentified insurance claims for privately insured and Medicare Advantage enrollees. Total morbidity score was determined using the Elixhauser Comorbidity Index. The underlying transgender numbers vary as a result of our transgender identification criteria, as some chronic condition and transgender exclusion codes overlap with those of the Elixhauser Comorbidity Index. So as to not bias our estimates downward, we removed people from our calculations who were identified as transgender only because they fell into an inclusion category that required that they did not have the condition being analyzed. See Jasuja GK, et al., note 3 in text, for more detail. p values for these regressions are in appendix exhibit 1 (see note 22 in text). TFN is trans feminine and nonbinary. TFM is trans masculine and nonbinary.
TFN n = 5,658.
TMN n = 4,660.
When we analyzed weight, diabetic, and thyroid conditions, trans masculine and nonbinary people were at the greatest risk for diabetes (13.2 percent) compared with all other groups. Both trans feminine and nonbinary people and trans masculine and nonbinary people were at a much higher risk for obesity (19.2 percent and 26.7 percent, respectively) than both cisgender men (14.7 percent) and cisgender women (17.5 percent). Cisgender men were at the lowest risk for hypothyroidism compared with all other groups (7.4 percent).
When we analyzed mental health and substance use conditions, the trans feminine and nonbinary and trans masculine and nonbinary cohorts had similar risk for depression (51.9 percent and 53.5 percent, respectively) and psychoses (5.0 percent and 4.1 percent, respectively) and were at much higher risk than both cisgender men and cisgender women. Trans masculine and nonbinary people and trans feminine and nonbinary people were at a greater risk for drug use disorder (7.0 percent and 8.7 percent, respectively) than both cisgender men (4.6 percent) and cisgender women (3.2 percent). Trans feminine and nonbinary people were also at a greater risk for alcohol use disorder (5.5 percent) than both cisgender men (4.4 percent) and cisgender women (2.3 percent).
Comparing other chronic conditions, cisgender men were at the lowest risk for chronic pulmonary disease (19.7 percent), whereas trans masculine and nonbinary people had the greatest risk (31.9 percent). Trans masculine and nonbinary people were at the greatest risk for liver disease (13.3 percent) compared with all other cohorts. Trans feminine and nonbinary people also were at a greater risk for AIDS/HIV (3.0 percent) compared with all other cohorts.
Discussion
The purpose of this study was to expand understanding of morbidities in transgender populations relative to cisgender populations with commercial insurance. Our findings showed not only that transgender people had a significantly elevated risk for most health conditions relative to their cisgender counterparts12 but also that there were significant differences in the health status of transgender subgroups, with trans masculine and nonbinary people having a significantly elevated risk for nineteen of the twenty-six health conditions relative to trans feminine and nonbinary people. These findings underscore the need for clinical and policy interventions aimed at achieving health equity for transgender populations, with a particular focus on subgroups that are most at risk for chronic conditions, such as trans masculine and nonbinary people.
The predicted probabilities of nearly all conditions were significantly higher among transgender people relative to their cisgender counterparts. When examining physical health conditions by gender subgroup, we found that the predicted probability of hypertension was elevated among cisgender women compared with cisgender men, yet similar between trans feminine and nonbinary people and trans masculine and nonbinary people. This similarity between transgender subgroups may be in part a result of the physiologic effects of gender-affirming estrogen for trans feminine and nonbinary people, which has been shown to be associated with cardiovascular disease.23 However, compared with trans feminine and nonbinary people, cisgender men, and cisgender women, trans masculine and nonbinary people had the highest burden for more than half of the other physical health conditions, including hypertension and most other cardiovascular outcomes, which is consistent with prior research comparing the cardiovascular health of cisgender people with that of trans masculine and nonbinary people receiving gender-affirming hormones.24,25 Chronic pulmonary disease was significantly elevated among trans masculine and nonbinary people compared with trans feminine and nonbinary people. Consistent with prior research,26 cisgender women had a greater predicted probability of chronic pulmonary disease relative to cisgender men. Furthermore, we found a slight disparity in renal disease such that trans feminine and nonbinary people had a greater risk for renal failure compared with trans masculine and nonbinary people. Although renal failure was slightly higher among cisgender men than cisgender women in our sample, prior research has found that males are nearly twice as likely as females to reach end-stage renal failure.27 Finally, we found that the largest disparity among the chronic conditions across gender groups was observed for AIDS/HIV. Trans feminine and nonbinary people had 8.7, 5.2, and 21.3 times the predicted probability of AIDS/HIV compared with trans masculine and nonbinary people, cisgender men, and cisgender women, respectively—a finding that is highly consistent with surveillance data.9,28
Large disparities were also observed in the predicted probability of mental health and substance use conditions, with transgender people having approximately 4.0, 2.7, 2.5, and 1.6 times the predicted probability of psychoses, depression, drug use disorder, and alcohol use disorder, respectively, relative to cisgender people. However, given that the standards of care for accessing gender-affirming medical care require transgender people to meet with a mental health practitioner before accessing hormones and surgeries, increased rates of mental health conditions among the transgender cohort may be driven by this requirement rather than by actual prevalence.17
Furthermore, consistent with the literature,29 we found that the predicted probability of drug and alcohol use disorders was 42–90 percent higher among cisgender men than cisgender women. However, the predicted probability of substance abuse was greater among trans feminine and nonbinary than among trans masculine and nonbinary people. Prior research has linked these disparities in AIDS/HIV and mental health to minority stress and stigma, which restrict access to health-promoting resources and contribute to poor physical and mental health outcomes for this population relative to cisgender people.30–32 Multilevel interventions are needed to prevent stigma, which contributes to health inequities at the policy and service delivery level, to improve health outcomes for transgender populations.
In addition, rates of morbidity appear elevated in our matched cisgender sample compared with in the similar-age general population,33,34 which indicates that the prevalence of morbidities among our cisgender cohort is not representative of a randomly selected cisgender cohort and that these findings may understate the disparities in morbidity between transgender and cisgender populations.
Research And Policy Implications
Claims analyses provide a useful means to understand transgender health and allow for comparisons across a host of chronic conditions that are not possible using small convenience samples. Furthermore, using algorithms to stratify by gender or sex assigned at birth allows for comparisons to be made both within and across transgender and cisgender groups. This stratification provides a meaningful insight into health disparities unique to certain subpopulations of transgender people and is a strategy that should be leveraged in future research.
Although claims analysis provides a mechanism to explore a host of previously unexplored or underexplored health conditions, the inclusion of sex and gender questions in national surveillance data, such as the National Health Interview Survey and the National Health and Nutrition Examination Survey, is greatly needed to increase understanding of the prevalence of these conditions among US transgender populations that are uninsured, as well as the structural, social, and behavioral drivers of the disparities described here. Policy change is needed to ensure the inclusion of gender identity data in future census data and other national surveys. In light of the health disparities observed here and prior research documenting discrimination as a driver of poor health,30–32 there is an ongoing need to ensure that state and federal nondiscrimination policies ensure protections against discrimination on the basis of gender identity and expression.
Conclusion
Our findings documenting an elevated risk for morbidity among transgender people underscore the importance of future research that does not simply focus on a single chronic condition but considers the prevalence of multiple conditions that have ramifications for the health and well-being of transgender populations. Our work also highlights the importance of gender subgroups within transgender populations, such as transgender men, transgender women, and gender nonbinary people, in understanding the distributions of chronic conditions within transgender cohorts, and it stresses the need for interventions that address the health of trans masculine and nonbinary people in particular. Ultimately, insurance administrators and national surveillance systems should collect self-reported gender identity information inclusive of transgender identities to increase understanding of the health of transgender people relative to cisgender people across nationally representative data sets. In the context of research documenting discrimination as a contributing factor to poor health outcomes among transgender populations, these findings highlight the need for federal and state nondiscrimination protections for transgender people.
Supplementary Material
Acknowledgments
Landon Hughes was supported by the Rackham Merit Fellowship, the National Institute on Aging (Grant No. T32 AG000221), and the Eunice Kennedy Shriver National Institute of Child Health and Development (Grant No. T32 HD00733931). The authors especially thank the University of Michigan’s Institute for Social Research for the funds to access these data and the Institute for Healthcare Policy and Innovation for providing the technical assistance needed to access these data. Prior to the September 2021 journal issue embargo date, the authors discovered an error in the Optum data used for the study that affected the distribution of their identified transgender and cisgender cohorts. The article has been corrected online, but the version that appears in the print volume (volume 40, issue 9) presents the uncorrected analysis.
Contributor Information
Landon Hughes, Department of Health Behavior and Health Education and a predoctoral trainee in the Population Studies Center, Institute for Social Research, University of Michigan, in Ann Arbor, Michigan..
Theresa I. Shireman, Department of Health Services, Policy, and Practice and director of the Center for Gerontology and Healthcare Research, Brown University School of Public Health, in Providence, Rhode Island..
Jaclyn Hughto, Departments of Behavioral and Social Sciences and Epidemiology and the Center for Health Promotion and Health Equity, Brown University School of Public Health. She is also an adjunct investigator at the Fenway Institute, Fenway Health, in Boston, Massachusetts..
NOTES
- 1.Downing JM, Przedworski JM. Health of transgender adults in the U.S., 2014–2016. Am J Prev Med. 2018;55(3):336–44. [DOI] [PubMed] [Google Scholar]
- 2.Rich AJ, Scheim AI, Koehoorn M, Poteat T. Non-HIV chronic disease burden among transgender populations globally: a systematic review and narrative synthesis. Prev Med Rep. 2020;20:101259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jasuja GK, de Groot A, Quinn EK, Ameli O, Hughto JMW, Dunbar M, et al. Beyond gender identity disorder diagnoses codes: an examination of additional methods to identify transgender individuals in administrative databases. Med Care. 2020; 58(10):903–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blosnich JR, Brown GR, Shipherd Phd JC, Kauth M, Piegari RI, Bossarte RM. Prevalence of gender identity disorder and suicide risk among transgender veterans utilizing Veterans Health Administration care. Am J Public Health. 2013; 103(10):e27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Proctor K, Haffer SC, Ewald E, Hodge C, James CV. Identifying the transgender population in the Medicare program. Transgend Health. 2016;1(1):250–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dragon CN, Guerino P, Ewald E, Laffan AM. Transgender Medicare beneficiaries and chronic conditions: exploring fee-for-service claims data. LGBT Health. 2017; 4(6):404–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Progovac AM, Cook BL, Mullin BO, McDowell A, Sanchez RMJ, Wang Y, et al. Identifying gender minority patients’ health and health care needs in administrative claims data. Health Aff (Millwood). 2018;37(3): 413–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown GR, Jones KT. Mental health and medical health disparities in 5135 transgender veterans receiving healthcare in the Veterans Health Administration: a case-control study. LGBT Health. 2016;3(2):122–31. [DOI] [PubMed] [Google Scholar]
- 9.James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anaf M. The report of the 2015 U.S. Transgender Survey [Internet]. Washington (DC): National Center for Transgender Equality; 2016. [cited 2021 Jul 12]. Available from: https://transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf [Google Scholar]
- 10.McDowell A, Progovac AM, Cook BL, Rose S. Estimating the health status of privately insured gender minority children and adults. LGBT Health. 2019;6(6):289–96. [DOI] [PubMed] [Google Scholar]
- 11.Hughto JW, Shireman TI. Health Equity Data Access Program: newly funded HEDAP projects: characterizing disparities in the HIV prevention and care continuum among transgender and cisgender Medicaid and Medicare beneficiaries [Internet]. Baltimore (MD): Centers for Medicare and Medicaid Services; 2018[last updated 2021 Mar 4; cited 2021 Jul 12]. Available from: https://www.cms.gov/About-CMS/Agency-Information/OMH/equity-initiatives/advancing-health-equity/health-equity-data-access-program [Google Scholar]
- 12.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. [DOI] [PubMed] [Google Scholar]
- 13.Johnson-Lawrence V, Zajacova A, Sneed R. Education, race/ethnicity, and multimorbidity among adults aged 30–64 in the National Health Interview Survey. SSM Popul Health. 2017;3:366–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weinberger AH, Gbedemah M, Martinez AM, Nash D, Galea S, Goodwin RD. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol Med. 2018; 48(8):1308–15. [DOI] [PubMed] [Google Scholar]
- 15.Okunrintemi V, Tibuakuu M, Virani SS, Sperling LS, Volgman AS, Gulati M, et al. Sex differences in the age of diagnosis for cardiovascular disease and its risk factors among US adults: trends from 2008 to 2017, the Medical Expenditure Panel Survey. J Am Heart Assoc. 2020;9(24): e018764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying increased risk of read mission and in-hospital mortality using hospital administrative data: the AHRQ Elixhauser Comorbidity Index. Med Care. 2017;55(7):698–705. [DOI] [PubMed] [Google Scholar]
- 17.Streed CG Jr, Arroyo H, Goldstein Z. Gender minority patients’ mental health care. Health Aff (Millwood). 2018;37(6):1014. [DOI] [PubMed] [Google Scholar]
- 18.Stroumsa D, Crissman HP, Dalton VK, Kolenic G, Richardson CR. Insurance coverage and use of hormones among transgender respondents to a national survey. Ann Fam Med. 2020;18(6):528–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seelman KL, Colon-Diaz MJP, LeCroix RH, Xavier-Brier M, Kattari L. Transgender noninclusive healthcare and delaying care because of fear: connections to general health and mental health among transgender adults. Transgend Health. 2017; 2(1):17–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flores AR, Herman JL, Gates GJ, Brown TNT. How many adults identify as transgender in the United States? [Internet]. LosAngeles (CA): Williams Institute; 2016June [cited 2021 Jul 12]. Available from: https://williamsinstitute.law.ucla.edu/publications/trans-adults-united-states/ [Google Scholar]
- 21.Ewald ER, Guerino P, Dragon C, Laffan AM, Goldstein Z, Streed C Jr. Identifying Medicare beneficiaries accessing transgender-related care in the era of ICD-10. LGBT Health. 2019;6(4):166–73. [DOI] [PubMed] [Google Scholar]
- 22.To access the appendix, click on the Details tab of the article online.
- 23.Iwamoto SJ, Defreyne J, Rothman MS, Van Schuylenbergh J, Van de Bruaene L, Motmans J, et al. Health considerations for transgender women and remaining unknowns: a narrative review. Ther Adv Endocrinol Metab. 2019;10:2042018819871166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nota NM,Wiepjes CM, de Blok CJM, Gooren LJG, Kreukels BPC, den Heijer M. Occurrence of acute cardiovascular events in transgender individuals receiving hormone therapy. Circulation. 2019;139(11): 1461–2. [DOI] [PubMed] [Google Scholar]
- 25.Getahun D, Nash R, Flanders WD, Baird TC, Becerra-Culqui TA, Cromwell L, et al. Cross-sex hormones and acute cardiovascular events in transgender persons: a cohort study. Ann Intern Med. 2018;169(4):205–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lisspers K, Larsson K, Janson C, Stâllberg B, Tsiligianni I, Gutzwiller FS, et al. Gender differences among Swedish COPD patients: results from the ARCTIC, a real-world retrospective cohort study. NPJ Prim Care Respir Med. 2019;29(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Institutes of Health, National Institute of Diabetes and Digestive and Digestive and Kidney Diseases. Précis: an introduction to end-stage renal disease in the U.S. Am J Kidney Dis. 2014;63(1): e169–92. [Google Scholar]
- 28.Centers for Disease Control and Prevention. HIV and transgender communities [Internet]. Atlanta (GA): CDC; 2019April [cited 2021 Jul 12]. Available from: https://www.cdc.gov/hiv/pdf/policies/cdc-hiv-transgender-brief.pdf [Google Scholar]
- 29.Hughto JMW, Quinn EK, Dunbar MS, Rose AJ, Shireman TI, Jasuja GK. Prevalence and co-occurrence of alcohol, nicotine, and other substance use disorder diagnoses among US transgender and cisgender adults. JAMA Netw Open. 2021; 4(2):e2036512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: a critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med. 2015;147: 222–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the Minority Stress Model. Prof Psychol Res Pr. 2012;43(5):460–7. [Google Scholar]
- 32.Hatzenbuehler ML, Pachankis JE. Stigma and minority stress as social determinants of health among lesbian, gay, bisexual, and transgender youth: research evidence and clinical implications. Pediatr Clin North Am. 2016;63(6):985–97. [DOI] [PubMed] [Google Scholar]
- 33.Ostchega Y, Fryar CD, Nwankwo T, Nguyen DT. Hypertension prevalence among adults aged 18 and over: United States, 2017–2018 [Internet]. Hyattsville (MD): National Center for Health Statistics; 2020April [cited 2021 Jul 12]. (NCHS Data Brief No. 364). Available from: https://www.cdc.gov/nchs/products/databriefs/db364.htm [Google Scholar]
- 34.Mendola ND, Chen T-C, Gu Q, Eberhardt MS, Saydah S. Prevalence of total, diagnosed, and undiagnosed diabetes among adults: United States, 2013–2016 [Internet]. Hyattsville (MD): National Center for Health Statistics; 2018September [cited 2021 Jul 12]. (NCHS Data Brief No. 319). Available from: https://www.cdc.gov/nchs/data/databriefs/db319.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


