Abstract
Background
Comforting behaviours, such as the use of pacifiers (dummies, soothers), blankets and finger or thumb sucking, are common in babies and young children. These comforting habits, which can be referred to collectively as 'non‐nutritive sucking habits' (NNSHs), tend to stop as children get older, under their own impetus or with support from parents and carers. However, if the habit continues whilst the permanent dentition is becoming established, it can contribute to, or cause, development of a malocclusion (abnormal bite). A diverse variety of approaches has been used to help children with stopping a NNSH. These include advice, removal of the comforting object, fitting an orthodontic appliance to interfere with the habit, application of an aversive taste to the digit or behaviour modification techniques. Some of these interventions are easier to apply than others and less disturbing for the child and their parent; some are more applicable to a particular type of habit.
Objectives
The primary objective of the review was to evaluate the effects of different interventions for cessation of NNSHs in children. The secondary objectives were to determine which interventions work most quickly and are the most effective in terms of child and parent‐ or carer‐centred outcomes of least discomfort and psychological distress from the intervention, as well as the dental measures of malocclusion (reduction in anterior open bite, overjet and correction of posterior crossbite) and cost‐effectiveness.
Search methods
We searched the following electronic databases: the Cochrane Oral Health Group Trials Register (to 8 October 2014), the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2014, Issue 9), MEDLINE via OVID (1946 to 8 October 2014), EMBASE via OVID (1980 to 8 October 2014), PsycINFO via OVID (1980 to 8 October 2014) and CINAHL via EBSCO (1937 to 8 October 2014), the US National Institutes of Health Trials Register (Clinical Trials.gov) (to 8 October 2014) and the WHO International Clinical Trials Registry Platform (to 8 October 2014). There were no restrictions regarding language or date of publication in the searches of the electronic databases. We screened reference lists from relevant articles and contacted authors of eligible studies for further information where necessary.
Selection criteria
Randomised or quasi‐randomised controlled trials in children with a non‐nutritive sucking habit that compared one intervention with another intervention or a no‐intervention control group. The primary outcome of interest was cessation of the habit.
Data collection and analysis
We used standard methodological procedures expected by The Cochrane Collaboration. Three review authors were involved in screening the records identified; two undertook data extraction, two assessed risk of bias and two assessed overall quality of the evidence base. Most of the data could not be combined and only one meta‐analysis could be carried out.
Main results
We included six trials, which recruited 252 children (aged 2 and a half to 18 years), but presented follow‐up data on only 246 children. Digit sucking was the only NNSH assessed in the studies. Five studies compared single or multiple interventions with a no‐intervention or waiting list control group and one study made a head‐to‐head comparison. All the studies were at high risk of bias due to major limitations in methodology and reporting. There were small numbers of participants in the studies (20 to 38 participants per study) and follow‐up times ranged from 1 to 36 months. Short‐term outcomes were observed under one year post‐intervention and long‐term outcomes were observed at one year or more post‐intervention.
Orthodontics appliance (with or without psychological intervention) versus no treatment
Two trials that assessed this comparison evaluated our primary outcome of cessation of habit. One of the trials evaluated palatal crib and one used a mix of palatal cribs and arches. Both trials were at high risk of bias. The orthodontic appliance was more likely to stop digit sucking than no treatment, whether it was used over the short term (risk ratio (RR) 6.53, 95% confidence interval (CI) 1.67 to 25.53; 2 trials, 70 participants) or long term (RR 5.81, 95% CI 1.49 to 22.66; 1 trial, 37 participants) or used in combination with a psychological intervention (RR 6.36, 95% CI 0.97 to 41.96; 1 trial, 32 participants).
Psychological intervention versus no treatment
Two trials (78 participants) at high risk of bias evaluated positive reinforcement (alone or in combination with gaining the child's co‐operation) or negative reinforcement compared with no treatment. Pooling of data showed a statistically significant difference in favour of the psychological interventions in the short term (RR 6.16, 95% CI 1.18 to 32.10; I2 = 0%). One study, with data from 57 participants, reported on the long‐term effect of positive and negative reinforcement on sucking cessation and found a statistically significant difference in favour of the psychological interventions (RR 6.25, 95% CI 1.65 to 23.65).
Head‐to‐head comparisons
Only one trial demonstrated a clear difference in effectiveness between different active interventions. This trial, which had only 22 participants, found a higher likelihood of cessation of habit with palatal crib than palatal arch (RR 0.13, 95% CI 0.03 to 0.59).
Authors' conclusions
This review found low‐quality evidence that orthodontic appliances (palatal arch and palatal crib) and psychological interventions (including positive and negative reinforcement) are effective at improving sucking cessation in children. There is very low‐quality evidence that palatal crib is more effective than palatal arch. This review has highlighted the need for high‐quality trials evaluating interventions to stop non‐nutritive sucking habits to be conducted and the need for a consolidated, standardised approach to reporting outcomes in these trials.
Plain language summary
Interventions for stopping dummy or finger or thumb sucking habits in children
Review question
This review has been produced to assess the effects of interventions to stop sucking habits in children, which are not linked to food. Important considerations are: which treatment or combination of treatments work most effectively, when should treatment be started, what is the optimum length of time for the intervention and what causes least upset to children and their parents?
Background
Often babies and children develop a habit of sucking objects to comfort and calm them. They frequently suck dummies (known as pacifiers in the USA), fingers, thumbs or other items like blankets. Eventually, most children grow out of the habit, or stop due to encouragement from their parents. Some children, however, continue sucking as a habit. If they continue to do so as their adult teeth start to grow through (around the age of six), there is a risk that these adult teeth will grow into the wrong position causing them to stick out too far or not meet properly when biting. As a result these children often need dental treatment to fix the problems caused by their sucking habit.
Possible treatments to help children break their sucking habits examined in studies in this review include the use of two different braces in the mouth; giving advice and incentives for changing behaviour (known as psychological advice/treatment); applying a bitter, nasty tasting substance to the children’s thumbs/fingers or combinations of these treatments. None of the studies included looked at barrier methods, for example the use of gloves or plasters or withdrawal of dummies.
Study characteristics
Review authors from the Cochrane Oral Health Group carried out this review of existing studies and the evidence is current up to 8 October 2014. The review includes six studies published from 1967 to 1997, which involved 252 children as participants (although data were supplied on only 246 of the children). Three of the studies were carried out in the USA, one in Canada, one in Sweden and one in Australia.
Not all of the studies gave the ages of children involved; in four of the studies children were aged from two and a half to 18 years old, in one study they were aged four years and over and in another nine years and over.
Results
Use of an orthodontic brace (such as a palatal crib or arch) or a psychological intervention (such as use of positive or negative reinforcement), or both, was more likely to lead to cessation of the habit than no treatment. Most of the trials that compared two different interventions were inconclusive but one study suggested that, of two different types of braces,a palatal crib is more effective than a palatal arch design.
Quality of the evidence
The evidence presented is of low quality due to the small number of participants in the few available studies and problems with the way in which the studies were conducted. There was a high risk of bias across the studies.
Conclusion
Orthodontic braces or psychological intervention seems to be effective to help children stop sucking that does not have a feeding purpose but the evidence is low quality. Further high quality clinical trials are required to guide decision making for what is a common problem that can require lengthy and expensive dental treatment to correct.
Summary of findings
Background
Description of the condition
The term 'non‐nutritive sucking habit' (NNSH) encompasses the use of pacifiers ('dummies', 'soothers'), blankets and digit sucking. Although the incidence of sucking habits varies considerably between different countries, these comforting habits are common in children in many populations. A Swedish study looked at 60 consecutive births and found the incidence of NNSH to be 82% during the first five months of life (Larsson 2001) and a USA‐based study reported the incidence as 73% for a group of 130 children between two and five years of age (Adair 1992). The incidence of NNSH reduces with age. Available data has shown that around 48% of four‐year‐olds maintain a digit or pacifier sucking habit (Modeer 1982), 12.1% of children past the age of seven years (Patel 2008), reducing to 1.9% of children by 12 years of age (Baalack 1971).
Sucking is one of the earliest reflexes exhibited and is a very strong urge in young babies. Sucking behaviours are very common in babies and young children as they give a feeling of security and many parents introduce the use of pacifiers to babies to help them settle. There are other positive effects of pacifiers in young children, which may also contribute to their widespread use. The use of pacifiers has been shown to reduce crying in children during painful experiences such as venepuncture, and has been advocated for use in paediatric emergency departments (Blass 1999; Curtis 2007). Pacifier placement for babies going to sleep has also been identified as a factor in the reduction of sudden infant death syndrome (SIDS) (Hauck 2005; Li 2006), although the mechanism behind this is currently unknown. However, the incidence of SIDS is highest at two to four months and declines towards zero at one year of age and therefore is not a reason for encouraging continuation of pacifier use in children over the age of two and a half years, when primary teeth are all present in the mouth.
Children with a history of a NNSH are more likely to develop a malocclusion compared to children with no NNSH history (Bowden 1966; Farsi 1997; Fukuta 1996; Mistry 2010; Svedmyr 1979; Vazquez‐Nava 2006). In addition, there is evidence that the more prolonged the duration of the habit, the more severe the developing malocclusion tends to be (Baalack 1971; Singh 2008; Warren 2002). However, rather than there being a direct cause‐effect relationship between NNSH and development of a malocclusion, the effects of a habit seem to be superimposed on genetic predispositions to a malocclusion. Therefore, the NNSH might worsen or, conversely, counteract an underlying malocclusion and lead to an improvement. For example, in a child who has a Class III incisor relationship, a NNSH may push the upper anterior teeth forwards and the lower ones backwards, resulting in a less severe malocclusion.
Although NNSHs do not inevitably lead to a predictable malocclusion, different sucking habits generally have different effects on the position of the teeth. A malocclusion can develop through use of a NNSH, through application of pressure by the object or digit on the teeth, interfering with their normal path of eruption. Prolonged pacifier habits are associated with the development of posterior crossbites and prolonged digit habits with increased overjet (Bishara 2006; Ogaard 1994; Warren 2002), and both are associated with an increased prevalence of reduced overbite and anterior open bite (Warren 2002). Children with an increased overjet and incompetent lips (often associated with an anterior open bite) are at greater risk of dental trauma due to the prominence of the upper teeth and lack of protection from the lips (Burden 1995; Glendor 2009; Norton 2012). Incompetent lips and prominent upper anterior teeth are both associated with poor facial aesthetics. Speech can also be affected by tooth position. Laine 1987 found a significant relationship between increased overjet and distortions of the “s” sound and Bernstein 1954 noted that speech is commonly defective where there is an anterior open bite, often presenting with a lisp. There have also been reports of digit deformities developing as a result of prolonged digit sucking requiring surgical correction (Reid 1984), although these are uncommon.
If a NNSH continues while the permanent dentition is establishing, it may be associated with a malocclusion that will require fixed orthodontic appliances (Figure 1), resulting in time consuming, complex and costly treatment required to be carried out by a specialist orthodontist (Greenlee 2011; Petren 2008; Sandler 2011).
1.

Orthodontic deterrent appliance
A number of different interventions have been described in the literature to assist the child who wishes to stop the habit and to support parents who seek advice on this. However, it is not known which is most effective, or even if they are effective, or which are favoured by children and parents.
Description of the intervention
There is no standard intervention for cessation of NNSHs. A wide variety of different approaches and interventions have been described, which range from removal of the comforting object, through fitting an orthodontic appliance to directly interfere with the habit, application of an aversive tasting substance to the digit, to behaviour modification techniques (Al‐Jobair 2004; Friman 1986). Some of the interventions are easier to apply than others, less disturbing for the child and their parent or carer and certain ones are likely to be more applicable to a particular type of habit.
The interventions are likely to differ with respect to their:
effectiveness in habit cessation;
ease for children to cope with and ease of implementation from a parent/carer perspective;
time to stop the NNSH; and,
reduction in severity of the malocclusion.
How the intervention might work
The different ways in which the interventions might work depend on the habit and the type of intervention. Where the habit involves an object (blanket, pacifier etc), its removal will stop the habit (or lead to it being replaced by another). For habits that involve digit sucking, there are a number of different types of intra‐oral appliances to prevent placement of the digit in the habit position. Other appliances prevent the sense of gratification that the child feels through carrying out the habit although the digit can still be sucked. Other approaches involve replacing the feeling of comfort with an unpleasant stimulus such as an aversive taste. Behavioural modification techniques such as cognitive behavioural therapy, reward‐based strategies or use of positive reinforcement can also be employed.
Why it is important to do this review
NNSHs are common and this is a topic of significant interest to parents. There is a need to determine the most effective and timely management option(s) for cessation of NNSHs and it is important that consideration is also given to those associated with the least distress for children and their parents or carers. There is a wide variety of treatment strategies available to help children and parents with stopping sucking habits, but a lack of clarity about relative effectiveness and side effects. The aim of this review is to draw together the evidence and identify which interventions are the most successful.
Objectives
Primary objective
To evaluate the effects of different interventions for cessation of non‐nutritive sucking habits in children.
Secondary objectives
To determine which interventions work most quickly and are the most effective in terms of child and parent‐ or carer‐centred outcomes of least discomfort and psychological distress from the intervention, as well as the dental measures of malocclusion (reduction in anterior open bite, overjet and correction of posterior crossbite) and cost‐effectiveness.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled clinical trials (RCTs) and quasi‐randomised controlled clinical trials comparing an intervention for cessation of non‐nutritive sucking habits with either a different intervention(s) or no treatment or control.
Types of participants
Children (up to age 18 years of age) who have a digit sucking habit or any other NNSH, including a pacifier habit (dummy).
Types of interventions
For the intervention group we looked at:
orthodontic appliances;
barrier techniques ‐ gloves/plasters etc.;
chemical techniques ‐ topical substances applied to pacifier or digit;
behaviour modification techniques;
non‐treated control; and
any combination of the above.
For the control group we looked at:
any combination of the above or pacifier withdrawal.
Types of outcome measures
Primary outcomes
The primary outcome was cessation of the habit.
Secondary outcomes
1. Time taken for intervention to be effective.
2. Child and parent‐ or carer‐centred outcomes of discomfort from the intervention, psychological effects of teasing associated with the intervention, and distress caused by removal of the comfort/habit.
3. Reduction in malocclusion as measured by:
reduction in anterior open bite (mm);
reduction in overjet (mm);
correction of posterior crossbite.
4. Costs of interventions.
Search methods for identification of studies
To identify studies to be included in this review, we developed detailed search strategies for each database to be searched based on the search strategy developed for MEDLINE (OVID) (see Appendix 1). This search strategy was revised appropriately for each database to take account of differences in controlled vocabulary and syntax rules. The MEDLINE search strategy combined the subject search with the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of the Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 (updated March 2011) (Higgins 2011). The searches of EMBASE, CINAHL and PsycINFO were linked to search strategies for identifying RCTs developed by the Cochrane Oral Health Group.
We contacted authors of included studies for information on unpublished studies but no further attempt was made to identify unpublished literature.
Electronic searches
The following databases were searched:
MEDLINE via OVID (1946 to 8 October 2014) (Appendix 1);
Cochrane Oral Health Group's Trials Register (to 8 October 2014) (Appendix 2);
Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2014, Issue 9) (Appendix 3);
EMBASE via OVID (1980 to 8 October 2014) (Appendix 4);
PsychINFO via OVID (1980 to 8 October 2014) (Appendix 5);
CINAHL via EBSCO (1937 to 8 October 2014) (Appendix 6).
Searching other resources
Trials Registries
We searched the following databases for ongoing trials (see Appendix 7):
US National Institutes of Health Trials Register (http://clinicaltrials.gov) (to 8 October 2014);
The WHO Clinical Trials Registry Platform (http://apps.who.int/trialsearch/default.aspx) (to 8 October 2014).
Handsearching
The following relevant journals have been handsearched as part of the Cochrane Worldwide Handsearching Programme (see the Cochrane Masterlist for further information).
American Journal of Orthodontics and Dentofacial Orthopedics, 1970‐2004
Angle Orthodontist, 1979‐2006
ASDC Journal of Dentistry for Children, 1948‐2003
British Dental Journal, 1958‐2007
European Journal of Orthodontics, 1979‐2005
International Journal of Paediatric Dentistry, 1991‐2007
Journal of Orthodontics, 1973‐2007
Trials found as a result of this handsearching have been entered into the Cochrane Oral Health Group Trials Register and relevant studies were retrieved during the electronic searches.
No additional handsearching was undertaken as part of this review.
Language
Databases were searched with no language restrictions; however, all articles found were in English or provided an English abstract.
Correspondence
We contacted the first named authors or corresponding authors of studies included in the review in an attempt to identify unpublished studies and to obtain any further information about the trials. There was a response from only one author (Dr Larsson) who was not aware of any other studies.
Reference lists
The reference lists of the 14 full text articles were checked for eligibility and were scrutinised for further relevant studies.
Data collection and analysis
Selection of studies
Two review authors (Felicity Borrie (FB) and Nicola Innes (NI)) independently assessed the titles and abstracts of all reports identified by the search strategy for relevance to the review. We obtained full copies of all relevant and potentially relevant studies that appeared to meet the inclusion criteria, or for which there was insufficient data in the title and abstract to make a clear decision. A third review author (David Bearn (DB)) assisted with study selection where there was doubt about the inclusion of a trial. Studies rejected at this or subsequent stages were recorded in the Characteristics of excluded studies tables and the reasons for exclusion recorded.
Data extraction and management
Two review authors (FB and DB) independently extracted data for all reports on a specially designed data extraction form. Consensus was reached for all data included and any disagreements were resolved by the third author (NI). For each trial, the year of publication, country of origin and source of study funding were recorded as well as the following information.
1. Trial methods
Method of allocation
Number of losses to follow‐up, and reasons by study group
2. Participants
Age
Gender
Sample size
3. Intervention
Type
Duration, and duration of follow‐up
4. Control
Type of control
Duration, and duration of follow‐up
5. Outcomes
Primary and secondary outcomes as described in the outcome measures section of this protocol.
Assessment of risk of bias in included studies
For the studies included in this review, two review authors (FB and NI) undertook assessment of risk of bias independently for all studies (Higgins 2011). An overall 'Risk of bias' judgment was obtained for each study by addressing six specific domains: sequence generation, allocation concealment, blinding (because of the nature of the interventions this was only potentially possible for the outcome assessors), completeness of outcome data, risk of selective outcome reporting and other potential sources of bias. For each entry within these domains, what the study reported was stated in the 'Risk of bias' table, and a judgment made of the risk of bias for that entry (see Figure 2). The summary assessments of the risk of bias for individual studies was guided by Table 8.7a. in Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 (Higgins 2011).
2.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Measures of treatment effect
The data were analysed by FB and DB using Review Manager (RevMan) software and reported as suggested in Chapter 9 of the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 (Higgins 2011).
For ordinal data, including patient‐centred outcomes, discomfort and psychological effects, these were, as appropriate, dichotomised and then risk ratios (RRs) were calculated.
For dichotomous data, including cessation of habit and correction of crossbite, RRs and their 95% confidence intervals and number needed to treat for an additional beneficial outcome (NNTB) would have been calculated if data had been available.
For continuous data, including reduction in habit (measured in hours per day), time to cease habit (measured in days) and overjet and overbite (measured in millimetres (mm)), we planned to calculate the mean difference (MD) and 95% confidence intervals if data were available. However, only one study (Villa 1997) had continuous outcomes; overbite, overjet and arch length (mm) and these all presented standard deviations but it was not possible to calculate the MD from the data presented (Table 3).
1. Reduction in malocclusion.
| Villa 1997 study (n = 24) | Control | Palatal Crib | Statistically significant |
| Change in mandibular arch length (mm) | 0.03 SD 0.19 | ‐1.2 SD 0.8 | Yes, P value < 0.01 |
| Change in maxillary arch length (mm) | 0.01 SD 0.33 | ‐1.4 SD 1.4 | Yes, P value < 0.05 |
| Net change in overjet (mm) | 0.02 | ‐0.2 |
SD: standard deviation P probability
For counts, including appliance breakages, we planned to calculate the rate ratio for each appliance type but there were no data available so this was not calculated.
Unit of analysis issues
We included RCTs and quasi‐RCTs.Although we had planned to analyse data presented at six months and 12 months after commencement of the intervention, this was not possible due to the lack of data and studies. For multi‐arm trials we extracted data to allow comparison between treatments as individual pairs.
Dealing with missing data
We contacted all authors of included studies by letter to obtain further information. However, none of the authors replied. We reported the proportions of participants for whom no outcome data were obtained in the 'Risk of bias' table. We used an available case analysis approach and included data only on those whose results were known, using the total number of individuals who had data recorded for each particular outcome as the denominator as in section 16.2.2 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Assessment of heterogeneity
We assessed clinical heterogeneity by examining the characteristics of the studies, the similarity between the types of participants, the interventions and the outcomes, as specified in the criteria for included studies.
We had planned to assess statistical heterogeneity using a Chi2 test and the I2 statistic where I2 values over 50% indicate substantial to considerable heterogeneity. Heterogeneity would have been considered to be significant when the P value was less than 0.10 (Higgins 2011). However, there were insufficient data for this calculation to be performed.
Assessment of reporting biases
We planned to assess publication bias according to the recommendations on testing for funnel plot asymmetry (Egger 1997) as described in section 10.4.3.1 of the Cochrane Handbook for Systematic Reviewsof Interventions 5.1.0 (Higgins 2011), but there were insufficient studies to allow this to be carried out.
Data synthesis
We followed The Cochrane Collaboration statistical guidelines and analysed the data using Review Manager software and reported according to Cochrane Collaboration criteria. If significant heterogeneity had been detected, we planned to assess the significance of treatment effects using the random‐effects model, providing that there were more than three studies. If not, we planned to use the fixed‐effect model. However, we only found sufficient data to allow one meta‐analysis with two studies with 59 patients, comparing palatal cribs versus no treatment (Haryett 1967; Larsson 1972).
Subgroup analysis and investigation of heterogeneity
We had planned subgroup analyses for age and gender of participants. However, these were not possible as there was only a single meta‐analysis involving two small studies and 59 participants. In addition, the lack of information provided in the studies with respect to gender and age distribution precluded these analyses.
Sensitivity analysis
There were insufficient data to allow the effect on the overall estimates of random sequence generation, allocation concealment or blinded outcome assessment to be investigated.
Results
Description of studies
Results of the search
We identified 195 publications from the search strategy, after removal of duplicates. From reading titles and abstracts, we rejected 181 as not being relevant to the review. No further potentially eligible studies were identified from the references checked. We obtained full text articles for the remaining 14, all of which were in English language. Of these 14 studies, we excluded eight as they were not RCTs or quasi‐RCTs (RCTs). The remaining six studies all of which were RCTs (Azrin 1980; Christensen 1987; Friman 1990; Haryett 1967; Larsson 1972; Villa 1997) met the inclusion criteria and have been included in the review (Figure 3).
3.
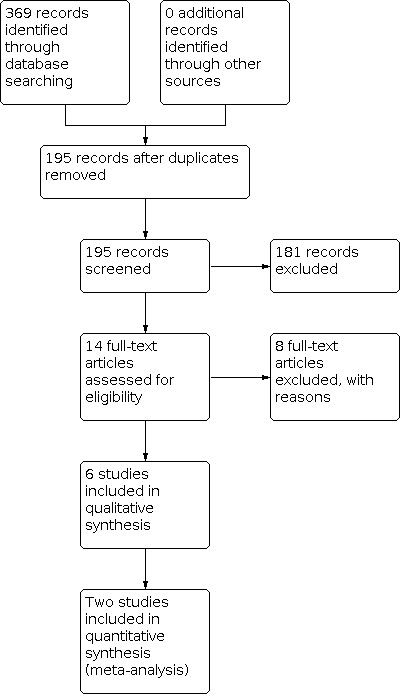
Study flow diagram
Included studies
We included six studies with 252 enrolled participants (see Characteristics of included studies). The studies dated from 1967 to 1997.
Characteristics of the trial setting and investigators
Three trials were conducted in the USA (Azrin 1980; Friman 1990; Villa 1997), one in Canada (Haryett 1967), one in Sweden (Larsson 1972) and one in Australia (Christensen 1987). The sample sizes ranged from 22 (Friman 1990) to 76 participants (Larsson 1972); however, none of the studies gave information on power calculations.
Characteristics of the participants
There were a total of 252 enrolled participants in the six trials. The NNSH assessed in all the studies was digit sucking. None of the studies reported on the use of a pacifier.
Two studies did not give clear inclusion criteria for the participants (Azrin 1980; Villa 1997).
Details of the participants’ age range were given for four studies (two and a half years to 18 years). The mean ages of the participants were:
8.3 years (range two and a half to 14 years) (Azrin 1980);
6.3 years (range four to nine years) (Christensen 1987);
6.4 years in intervention group, 6.8 years in the control group (range four to 11.6 years) (Friman 1990);
12.1 years in intervention group, 13.5 years in the control group (range eight to 18 years) (Villa 1997).
One study stated the participants were four years old and over (Haryett 1967) and another that the participants were nine years old (Larsson 1972).
Characteristics of the interventions
We expected to find interventions under the following groupings: orthodontic appliances; barrier techniques ‐ gloves/plasters etc; chemical techniques ‐ topical substances applied to pacifier or digit; behaviour modification techniques; non‐treated control; and pacifier withdrawal. There were no studies that looked at barrier techniques or pacifier withdrawal. There were a variety of intervention techniques applied and some were combined within the one intervention group.
There were variations in both the control and intervention comparisons in the trials. Two of the studies investigated a single intervention versus a control group (Friman 1990; Villa 1997); one compared two intervention groups with a control group (Christensen 1987); another had three intervention groups and a control group (Larsson 1972); and in one study there were five intervention groups and a control group (Haryett 1967). The sixth study (Azrin 1980) made a head‐to‐head comparison of two intervention groups.
In five of the studies, where the interventions were psychological in nature or an aversive tasting substance was applied, parents administered the interventions at the participants’ home (Azrin 1980; Christensen 1987; Friman 1990; Haryett 1967; Larsson 1972). For the three studies involving the use of orthodontic appliances as the sole intervention or co‐intervention, the orthodontic appliances were provided in an orthodontic clinic (Haryett 1967; Larsson 1972; Villa 1997).
The included studies are described below under headings relating to the type of intervention employed in the studies.
The interventions were grouped into psychological interventions, aversive tasting substance application to digits and orthodontic appliances. In some of the studies, combinations of interventions were applied to the same individual and the details of the interventions in the studies are detailed below as 'combination treatment'.
Orthodontic appliances
Three of the studies (Haryett 1967; Larsson 1972; Villa 1997) included in this review used two types of orthodontic appliances (palatal cribs and palatal arches) as interventions.
i. Palatal crib: Three studies used palatal cribs, the design of which differed between the studies. These minor differences were unlikely to have an effect on the way they work (Figure 4; Figure 5).
4.

Palatal crib
5.

Palatal crib with spurs
Haryett 1967 defined a palatal crib as an appliance that has bands on either the maxillary second deciduous molars or first permanent molars, with pictures showing a stainless steel wire fitted behind the upper incisors, over the palatal rugae with “vertical fencelike projections extended as deep as the lateral excursions of the mandible will allow.”
Larsson 1972 used a palatal crib with a modified design. The authors describe it as having spurs welded to bands cemented to the maxillary first molar teeth. “The crib lay a millimetre or so from the mucosa and extended just behind the maxillary incisors. The spurs were rounded in front and so adjusted that they did not disturb the occlusion.”
Villa 1997 used a “palatal crib” but did not specify the design of this appliance. The authors mention in their study that they feel that the appliance they fitted would have made sucking difficult, “if not impossible.” If this appliance had been a palatal arch some degree of sucking would likely have been possible. As there was no response from the authors to clarify the design of the palatal crib used, it has been assumed that this crib was similar to that used by Haryett 1967.
ii. Palatal arch: The palatal arch placed in Haryett 1967 had bands on the molars and a wire sitting on the gingival margins of the palatal side of the upper incisors, but had no projections. Although called a palatal arch in this study, this design is different from a standard Goshgarian palatal arch used in orthodontics, where the wire connecting the bands is situated across the middle of the palate and has an omega loop. For the purpose of this review, when a palatal arch is referred to, it is the design used by Haryett 1967.
Psychological Interventions
Five types of psychological interventions were assessed in four studies (Azrin 1980; Christensen 1987; Haryett 1967; Larsson 1972).
i. Habit reversal (HR) (Azrin 1980; Christensen 1987): The children were taught competing behaviours such as making a fist or grasping a convenient object for one to three minutes (measured by counting to 100). In Azrin 1980, parents were instructed to praise the child when sucking was absent, provide pleasant treats and surprises when sucking was absent for an extended period and stop television or bedtime stories when sucking occurred.
ii.Differential reinforcement of other behaviour (DRO): In Christensen 1987, DRO involved an increasing schedule of reinforcement using tokens as rewards when thumb sucking was avoided.
iii. A two‐part strategy; gaining child’s co‐operation to break the habit and parental reward for periods of no sucking (Haryett 1967): Co‐operation was gained by creating a desire in the child to avoid negative aesthetic effects. This was done by showing the child that digit sucking could alter the position of the teeth using both their own teeth (with mirrors) and pictures or models of other teeth with undesirable aesthetics. The second part of the strategy involved the parent rewarding the child for periods of “no sucking” by giving them their full attention and ignoring them if the habit occurred.
iv. Positive reinforcement (Larsson 1972): Participants’ mothers were given specific instructions about different forms of encouragement and reinforcement was also given by a psychologist.
v. Negative reinforcement (Larsson 1972): Children and their parents were given information about the consequences and risks of prolonged finger sucking. They were given models of the children’s teeth home with them.
Aversive tasting substance application
One study (Azrin 1980) made a head‐to‐head comparison involving aversive tasting substance (ATS) application and habit reversal. In the ATS group, the parents of the children received a single phone call informing them to apply a bitter tasting substance to the digit, morning and evening.
Combination treatment
There were three combination treatments reported in two studies (Friman 1990; Haryett 1967).
i. Psychological intervention and palatal arch (Haryett 1967): The design of the appliance is described above and the psychological component involved a two‐part strategy; gaining child’s co‐operation to break the habit and parental reward for periods of no sucking.
ii. Psychological intervention and palatal crib (Haryett 1967): The design of the appliance is described above, and the psychological component involved a two‐part strategy; gaining child’s co‐operation to break the habit and parental reward for periods of no sucking.
iii. Application of an aversive tasting substance and psychological intervention (Friman 1990): This involved both application of an aversive tasting substance to the thumb and a psychological component, a treat chosen at random from a grab bag.
Characteristics of the controls
One study compared two interventions and did not have a no‐treatment control group (Azrin 1980). In the remaining five trials (Christensen 1987; Friman 1990; Haryett 1967; Larsson 1972; Villa 1997), the control groups all consisted of no treatment, with Christensen 1987 and Friman 1990 using a waiting list control group.
Characteristics of the outcome measures
We were able to extract data for the primary outcome of habit cessation, and two of the secondary outcomes, child and parent‐ or carer‐centred outcomes detailed in Table 4 (% of children with oppositional behaviour before the intervention and at follow‐up; number upset by treatment; number reporting eating difficulty; development of mannerisms) and reduction in malocclusion. Results for more than one time point were available for two studies. These were percentage time intervals with thumb sucking immediately post treatment, and at three‐month follow‐up (Friman 1990), and cessation of habit at one month, one year, two years and three years follow‐up (Haryett 1967).
2. Child/parent/carer‐centred outcomes .
| Study | Outcome | Intervention A | Intervention B | Intervention C | Intervention D | Intervention E | Control |
| Christensen 1987 (n = 30) | Habit reversal | Differential reinforcement of other behaviour | Waiting list (no treatment) | ||||
| % of children with oppositional behaviour before intervention and at follow‐up | 3.1% to 0.2% | 2.5% to 0.6% | 2.7% to 2.7% | ||||
| Haryett 1967 (n = 66) | Psychology | Palatal arch | Palatal arch & psychology | Palatal crib | Palatal crib & psychology | No treatment | |
| Number upset by treatment | 1 | 0 | 2 | 6 | 2 | 0 | |
| No. reporting eating difficulty | 0 | 0 | 0 | 3 | 6 | 0 | |
| Development of mannerisms | 6 | 1 | 1 | 4 | 0 | 1 |
Primary outcome
Sucking cessation was measured in five studies (Azrin 1980; Christensen 1987; Friman 1990; Haryett 1967; Larsson 1972) at timepoints between five days (Friman 1990) and three years (Haryett 1967) but in a number of different ways:
four of the studies measured cessation of the habit by proportion of participants who had stopped their NNSH in each group (Azrin 1980; Christensen 1987; Haryett 1967; Larsson 1972);
one of these studies (Christensen 1987) additionally measured the proportion of time spent digit sucking before and after the intervention; and
one study (Friman 1990) only measured the percentage intervals of time with observed thumb sucking immediately after the intervention.
Sucking cessation was measured and reported at <12 months (short term) or ≥12 months (long term).
Secondary outcomes
Time taken for sucking habit to cease was not reported by any of the included studies.
No study reported adverse events. However, adverse outcomes were reported in one study (Haryett 1967); reported upset, speech and eating difficulties and development of mannerisms (Table 5).
3. Adverse outcomes after one month.
| Haryett 1967 | Psychological treatment | Orthodontic treatment | Both Psychological and Orthodontic treatment | Control |
| Reported upset | 1/11 (9%) | 6/22 (27%) | 4/22 (18%) | 0/50 (0%) |
| Speech difficulty | 0/11 (0%) | 9/22 (41%) | 6/22 (27%) | 0/50 (0%) |
| Eating difficulty | 0/11 (0%) | 3/22 (14%) | 6/22 (27%) | 0/45 (0%) |
| Developing mannerisms | 6/11 (55%) | 5/22 (23%) | 1/22 (5%) | 3/50 (6%) |
Reduction in malocclusion was reported by only one study (Villa 1997).
Costs were not measured by any of the studies.
Excluded studies
We excluded eight studies (see Characteristics of excluded studies). Two were observational, non‐intervention trials (Adair 1992; Friman 1986), three had no control group or inadequate controls (Al‐Emran 2005; Haryett 1970; Woods 1999), two were longitudinal studies (Cozza 2006; Cozza 2007), and one did not have outcomes relevant to this review (Degan 2005).
Risk of bias in included studies
A 'Risk of bias' graph (Figure 2) and summary diagram (Figure 6) were completed for the included studies (see Characteristics of included studies). All of the studies were assessed as being at overall high risk of bias although for one of the studies, this was purely on the basis of lack of blinding (Villa 1997).
6.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study
Allocation
Random sequence generation (selection bias)
Four of the studies had adequate sequence generation: coin flip (Azrin 1980; Friman 1990), sampling without replacement procedure (Christensen 1987) and random sample tables (Larsson 1972). For the other two studies, sequence generation was unclear (Haryett 1967; Villa 1997).
Allocation concealment
Allocation concealment was unclear in all studies.
Blinding
There was no blinding of participants or operators in any of the studies so we assessed all studies as at high risk of performance bias.
For the outcomes assessors, there was adequate blinding in one study (Villa 1997) where study models were assessed by an independent assessor. Blinding was unclear in two studies (Christensen 1987; Larsson 1972) and there was no blinding in three of the studies (Azrin 1980; Friman 1990; Haryett 1967) where parents acted as outcome assessors.
Incomplete outcome data
There were two studies that provided clear information about incomplete data and dropouts (Haryett 1967; Larsson 1972). They both had low dropout rates, with Haryett 1967 having one participant out of 66 lost to follow‐up at 10 months and Larsson 1972 having one participant out of 76 decline post‐intervention follow‐up. Incomplete data and follow‐up were unclear in two studies: Christensen 1987 implied that there were no dropouts in the control group but there were no figures to confirm this and for Villa 1997, dropout rates were not reported, although it was implied that all children were followed up. For two of the studies there was high risk of bias as one study (Azrin 1980) only provided information on the 50% loss to follow‐up for the intervention group with loss to follow‐up not reported for the control group. In Friman 1990, dropout rates were not reported, although it was implied that all children were followed up "posttest" and there was no detail on whether follow‐up participants had been allocated to the intervention or control group. No intention‐to‐treat analysis were performed to account for missing data.
Selective reporting
Two studies showed no signs of selective reporting (Christensen 1987; Villa 1997) in terms of outcome measures. However, data presented in Villa 1997 were insufficient to calculate mean difference. In one study (Haryett 1967), it was unclear whether individual outcomes had been prespecified and in three studies (Azrin 1980; Friman 1990; Larsson 1972), there was no prespecification of the outcomes.
Other potential sources of bias
Only two of the studies were assessed as being at low risk of other potential sources of bias (Friman 1990; Haryett 1967). One study (Villa 1997), was assessed as unclear as it was uncertain whether the sample was representative of the general population having been were recruited from an orthodontic department patient population. Three studies were assessed as being at high risk of bias for different reasons. In one study (Azrin 1980), bias may have been introduced into the sample as recruitment was through a newspaper advertisement and two children, who had been allocated to the control arm, withdrew as they had used that procedure previously without success. Christensen 1987 recruited participants through self‐referral following a newspaper article and Larsson 1972 limited recruitment to children who were judged by their parents "to be intense suckers ‐ children who sucked their fingers at least every evening...".
Effects of interventions
Summary of findings 1. Summary of findings: orthodontic appliances versus no treatment.
| Orthodontic appliances compared with no treatment for the cessation of pacifier or digit sucking habits in children | ||||||
|
Patient or population: children with pacifier or digit sucking habits Settings: home Intervention: orthodontic appliances (palatal arch/palatal crib) Comparison: no treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment | Orthodontic appliance | |||||
| Sucking cessation (short term) | 7 per 100 | 46 per 100 | RR 6.53 (1.67 to 25.53) | 70 (2) | Lowa,b | Long‐term data also show orthodontic appliances to be beneficial when compared with no treatment |
| Occlusion (changes in overbite) | MD 4.10 (2.93 to 5.27) | 24 (1) | Very lowa,b,c | Difference in mean net change in overbite between no treatment (‐0.4 mm) and orthodontic appliance (3.7 mm) = 4.1 mm | ||
| Adverse events | Insufficient information reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aDowngraded due to risk of bias. bDowngraded due to applicability (only 2 types of orthodontic appliance evaluated: palatal arch and palatal crib). cDowngraded for imprecision due to small number of participants.
Summary of findings 2. Summary of findings: psychological interventions versus no treatment.
| Psychological interventions compared with no treatment for the cessation of pacifier or digit sucking habits in children | ||||||
|
Patient or population: children with pacifier or digit sucking habits Settings: home Intervention: psychological interventions Comparison: no treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment | Pyschological interventions | |||||
| Sucking cessation (short term) | 3 per 100 | 19 per 100 | RR 6.16 (1.18 to 32.10) | 87 (2) | Lowa,b | Long‐term data also show psychological interventions to be beneficial when compared with no treatment |
| Occlusion | Not reported | |||||
| Adverse events | Insufficient information reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aDowngraded due to risk of bias. bDowngraded due to applicability.
The included studies reported on effects of the different interventions and combination of interventions on sucking cessation and occlusion. The comparisons have been summarised as follows.
Interventions versus no treatment
Orthodontic appliance versus no treatment (Analysis 1.1; Analysis 1.2; Analysis 1.3)
Psychological intervention versus no treatment (Analysis 2.1; Analysis 2.2)
Psychological intervention and orthodontic treatment versus no treatment (Analysis 3.1)
1.1. Analysis.

Comparison 1: Orthodontic appliances versus no treatment, Outcome 1: Sucking cessation (short term)
1.2. Analysis.

Comparison 1: Orthodontic appliances versus no treatment, Outcome 2: Sucking cessation (long term)
1.3. Analysis.

Comparison 1: Orthodontic appliances versus no treatment, Outcome 3: Occlusion (short term)
2.1. Analysis.

Comparison 2: Psychological intervention versus no treatment, Outcome 1: Sucking cessation (short term)
2.2. Analysis.

Comparison 2: Psychological intervention versus no treatment, Outcome 2: Sucking cessation (long term)
3.1. Analysis.

Comparison 3: Psychological intervention + orthodontic treatment versus no treatment, Outcome 1: Sucking cessation
Head‐to‐head comparisons of active interventions
Aversive taste versus psychological intervention (Analysis 4.1)
Orthodotic appliances versus alternative orthodontic appliances (Analysis 5.1)
Psychological intervention versus alternative psychological intervention (Analysis 6.1; Analysis 6.2)
Psychological intervention plus orthodontic appliance versus psychological intervention plus alternative orthodontic appliance (Analysis 7.1)
4.1. Analysis.

Comparison 4: Aversive taste versus psychological intervention, Outcome 1: Sucking cessation (short term)
5.1. Analysis.

Comparison 5: Orthodontic appliances versus alternative orthodontic appliance, Outcome 1: Sucking cessation (short term)
6.1. Analysis.

Comparison 6: Psychological intervention versus alternative psychological intervention, Outcome 1: Sucking cessation (short term)
6.2. Analysis.

Comparison 6: Psychological intervention versus alternative psychological intervention, Outcome 2: Sucking cessation (long term)
7.1. Analysis.

Comparison 7: Psycholgical+orthodontic versus psychological+alternative orthodontic, Outcome 1: Sucking cessation (short term)
We have consolidated other aspects of the studies into Additional tables to present a picture of the data more fully and show explicitly why data could not be combined for most of the interventions and outcomes.
Table 3 presents all data related to reduction in malocclusion which could only be reproduced with means and standard deviations.
Table 4 gives an overview of the child/parent/carer‐centred outcomes.
Table 5 where the adverse outcomes are detailed.
Table 6 shows the primary outcome of cessation of digit sucking after intervention for each different intervention, detailing the variety of interventions, controls, outcome measures.
4. Cessation of digit sucking after intervention .
| Study | Intervention A | Intervention B | Intervention C | Intervention D | Intervention E | Control | How cessation was measured |
Cessation of digit sucking units |
|
| Azrin 1980 (n = 30) | Habit reversal | Bitter substance | % of children with cessation of the habit | 47% HR group vs 10% control at 3 months | |||||
|
Christensen 1987 (n = 30) |
Habit reversal | Differential reinforcement of other behaviour | Waiting list (no treatment) | number of children with cessation of the habit | 2/10 HR group vs 1/10 DRO group vs 0/10 in WL control group | ||||
| Friman 1990 (n = 34) | Aversive taste treatment and reward system | Waiting list (no treatment) | % intervals of time with observed thumb sucking before and after intervention | 44% to 4% aversive taste vs 44% to 51% control (% intervals with thumb sucking) |
|||||
| Haryett 1967 (n = 66) | Psychology | Palatal arch | Palatal arch & psychology | Palatal crib | Palatal crib & psychology | No treatment | % of children with cessation of the habit | 9.1% A vs 9.1% B vs 27.3% C vs 100% D vs 100% E vs 10% no treatment | |
| Larsson 1972 (n = 76) | Positive reinforcement (pos) | Negative reinforcement (neg) | Palatal crib (crib) | No treatment | % of children with cessation of the habit | 26% pos, 53% neg, 42% crib, 5% control |
DRO: differential reinforcement of other behaviour HR: habit reversal WL: waiting list
Interventions versus no treatment
Orthodontic appliances versus no treatment
Three studies at high risk of bias reported on the effect of orthodontic appliances compared with no treatment. Outcomes reported were sucking cessation (short and long term) and occlusion.
Sucking cessation (short term)
Two studies, with data from 70 participants, compared palatal arch or palatal crib with no treatment) and reported data at one month (Haryett 1967) and two and a half months (Larsson 1972). Both studies were at high risk of bias. Pooling of data showed a statistically significant benefit in favour of the orthodontic appliances (risk ratio (RR) 6.53, 95% confidence interval (CI) 1.67 to 25.53). There was no significant heterogeneity (I2 = 0%) (Analysis 1.1).
Sucking cessation (long term)
One study comparing palatal crib with no treatment in 37 participants measured sucking cessation at 12 months (Larsson 1972). The study was at high risk of bias. Palatal crib was more likely to stop digit sucking compared to no treatment (RR 5.81, 95% CI 1.49 to 22.66) (Analysis 1.2).
Occlusion
One study, comparing palatal crib with no treatment in 24 participants, assessed changes in malocclusions at three months (Villa 1997). Although changes in mandibular and maxillary arch lengths were reported as statistically significant, the authors did not mention the clinical significance of the findings. The actual changes were less than 1.5 mm for the palatal crib intervention group, and would generally not be considered clinically important. However, the statistically significant reduction in anterior open bite of 3.7 mm in the palatal crib group (P < 0.05) is clinically important (Analysis 1.3). There was no statistically significant net change in overjet between the groups. Correction of posterior crossbite was not measured in this study despite being a well recognised feature in the malocclusion of a child with a thumb‐sucking habit.
Psychological interventions versus no treatment
Two studies at high risk of bias reported on the effect of various psychological interventions compared with no treatment on sucking cessation.
Sucking cessation (short term)
Two studies, with data from a total of 78 participants, evaluated positive reinforcement (alone or in combination with gaining the child's co‐operation) or negative reinforcement compared with no treatment (Haryett 1967; Larsson 1972). Pooling of data showed a statistically significant difference in favour of the psychological interventions (RR 6.16, 95% CI 1.18 to 32.10; I2 = 0%) (Analysis 2.1).
Sucking cessation (long term)
One study, with data from 57 participants,reported on the long‐term effect of positive and negative reinforcement on sucking cessation. A statistically significant difference was shown in favour of the psychological interventions (RR 6.25, 95% CI 1.65 to 23.65) (Analysis 2.2).
Psychological intervention plus orthodontic treatment versus no treatment
A combination of psychological intervention and orthodontic treatment was compared with no treatment in on study. The study reported on short‐term sucking cessation only.
Sucking cessation (short term)
One study, analysing 32 participants, compared psychological interventions plus orthodontic treatment (either palatal crib or palatal arch) with no treatment (Haryett 1967). The psychological intervention was a combination of positive reinforcement and cooperation. The study, at high risk of bias, found a statistically significant difference in favour of the combined intervention (RR 6.36, 95% CI 0.97 to 41.96) (Analysis 3.1).
Head‐to‐head comparisons of active interventions
Aversive taste versus psychological intervention
Sucking cessation (short term)
One study, which analysed 29 participants, compared habit reversal with aversive taste application and found that aversive taste was less likely to stop digit sucking than psychological intervention but the difference was not statistically significant (RR 0.18 (95% CI 0.03 to 1.24) (Analysis 4.1). The study was at high risk of bias.
Orthodontic appliances versus alternative orthodontic appliances
Sucking cessation (short term)
One study, at high risk of bias, compared palatal arch with palatal crib (Haryett 1967). The study evaluated 22 participants for this comparison. A statistically significant difference was shown in favour of palatal crib (RR 0.13, 95% CI 0.03 to 0.59)
Psychological interventions versus alternative psychological interventions
Sucking cessation (short term)
One study, analysing 20 participants, compared habit reversal (HR) with differential reinforcement of other behaviour (DRO) (Christensen 1987). No statistically significant difference was shown between treatment groups.
A second study compared positive reinforcement with negative reinforcement, with data from 38 participants (Larsson 1972). Again, no statistically significant difference between groups were shown.
Sucking cessation (long term)
Larsson 1972, comparing positive reinforcement with negative reinforcement, also provided long‐term data. Again, no statistically significant between group differences were shown.
Psychological interventions plus orthodontic appliance versus psychological interventions plus alternative orthodontic appliance
Sucking cessation (short term)
One study compared a combination of psychological intervention with palatal arch to psychological intervention with palatal crib (Haryett 1967). The trial evaluated 22 participants for this comparison and showed a statistically significant difference in sucking cessation (short term) in favour of the psychological intervention and palatal crib combination (RR 0.30, 95% CI [0.13 to 0.74). The trial was at a high risk of bias.
Other comparisons
These are detailed under interventions, as well as being grouped by outcomes under Table 6 for the primary outcome of cessation of the habit, Table 4 for the secondary outcome relating to child and parent/carer measures, Table 5 for adverse outcomes after one month and Table 3 for the secondary outcomes related to reduction in malocclusion.
Due to poor reporting, differences in interventions and a lack of standardisation in outcomes, no useful interpretation can be drawn from these results.
Discussion
Summary of main results
The objective of this review was twofold: to assess the effectiveness of different interventions for stopping non‐nutritive sucking habits (NNSHs), and to identify acceptability of interventions. Six trials, with 252 enrolled children, aged between two and a half and 18 years, were included. Four studies (Azrin 1980; Christensen 1987; Haryett 1967; Larsson 1972) measured the primary outcome of cessation of NNSH while two studies reported secondary outcome data related to behaviour of child and parent‐ or carer‐centred measures.
There was a range of clinical interventions, of differing duration and follow‐up, evaluated (behaviour modification, application of an aversive tasting substance to digits and use of intra‐oral orthodontic appliances). In addition, the studies were at high risk of bias. The paucity of studies for each intervention type and their high risk of bias means that the body of evidence to support clinical decision making for cessation of NNSH is low.
Orthodontic appliances (palatal arch and palatal crib) were shown to be beneficial at increasing the number of children stopping sucking in both the short and long term, in comparison to no treatment. Palatal crib was also shown to beneficial in term of effect on occlusion (short term) compared with no treatment. When palatal arch and palatal crib were compared directly in a single study, a statistically significant increase in the number of children stopping sucking was seen in favour of palatal crib. This was the same whether the palatal arch or palatal crib was used alone or in combination with a psychological intervention.
Psychological interventions, such as positive or negative reinforcement were also shown to significantly increase the number of children stopping sucking in both the short and long term, in comparison to no treatment. There was insufficient information to determine whether one psychological intervention was more effective than another.
There was insufficient information to determine whether aversive taste was more effective than psychological interventions.
Secondary outcome data for child and parent‐ or carer‐centred measure reported were ‘oppositional behaviour’ (Christensen 1987), upset during treatment, eating difficulties and development of mannerisms (Haryett 1967). However, the numbers of patients for which these were reported were small and the findings inconsistent. Given the conflicting nature of the data and the small numbers, it is not possible to draw clear conclusions.
Overall completeness and applicability of evidence
This review has highlighted that the body of evidence for this subject is weak. There are very few trials that met the inclusion criteria with small numbers of children included, a wide age range, and they are published over a 30‐year period. This review identified a wide range of interventions, with differing durations, and interventions that were aimed at children or parents or both. A range of outcomes were found along with different durations of follow‐up for participants following the interventions.
There were no studies included in the review that used removable orthodontic appliances to stop NNSHs. This method is still commonly used in the UK but is not considered good practice in the USA (Proffit 2013). None of the included studies looked at interventions for pacifier habits, but this may be due to the fact that it is easy to withdraw pacifiers and consequently eliminate the problem.
There was very little data in the studies about the duration of treatment and long‐term follow‐up regarding cessation of habit and it was not possible to determine the age at which treatment would be most effective. Furthermore, there may be a period of time when the occlusion is establishing where absence of a NNSH may be more critical than at another stage. For example, it may be that re‐uptake of a NNSH might have very little effect in a 12‐year‐old, where the occlusion is more established than in, for example, a seven‐year‐old. No conclusions could be drawn about the time taken for different interventions to be effective, as they were in place for different lengths of time and follow‐up occurred at differing time points. There was also a lack of precision in measuring outcomes regarding time taken for effective treatments. For example, in Haryett 1967 where the palatal crib was in place for 10 months and 100% success was achieved with cessation of habit, there was no information about which time point this occurred or even whether the same result would have been achieved in a shorter timeframe (Table 6),
Orthodontic appliances were used in three studies (Haryett 1967; Larsson 1972; Villa 1997). However, no information was given on ease of fitting or removing the appliances. All were fixed appliances although a removable deterrent appliance is sometimes used in the UK for managing persistent thumb sucking habits, particularly if it is a nighttime‐only occurrence and the patient is motivated to stop.
There was no information in any of the studies relating to costs of the interventions.
Quality of the evidence
The quality of the evidence ranged from low to very low due to imprecision and high risk of bias in the studies. Imprecision was as a result of very few events from the small number of participants recruited as well as wide confidence intervals that include both appreciable benefit and appreciable harm. Methodological limitations were mostly due to lack of blinding of participants and personnel involved, attrition, selective reporting and sampling bias from participant recruitment (other bias). There is little consideration of adequate controls in the studies as some individuals could potentially cease a habit without intervention. The lack of standardised measures and the low quality of these studies, may, at least in part, be a result of their age.
Potential biases in the review process
We tried to limit bias in the review process by following standard methodological procedures expected by The Cochrane Collaboration. A sensitive search strategy was used in this review with every effort made to identify all relevant studies. No studies were excluded due to language. Data collection and analyses were carried out independently with any disagreement resolved by discussion amongst the review authors or with the assistance of the Cochrane Oral Health Group to minimise/exclude bias in this review.
The post‐hoc decision to regard outcomes observed less than 12 months post‐intervention as short‐term outcomes and 12 months or more as long‐term outcomes could also be considered a potential bias.
Agreements and disagreements with other studies or reviews
There are no other studies or reviews to compare our findings with.
Authors' conclusions
Implications for practice.
This review found low‐quality evidence that orthodontic appliances (palatal arch and palatal crib) and psychological interventions (including positive and negative reinforcement) are effective at improving sucking cessation in children. There is very low‐quality evidence that palatal crib is more effective than palatal arch. There is insufficient evidence to determine the effect of other interventions evaluated for the cessation of digit sucking in children. However, although it is not possible to draw definitive conclusions from the data, in the case of a digit sucking habit, given that the use of aversive tasting substance requires no clinical input, is a non‐invasive, low‐risk procedure, is cheap and can be carried out by parents in the home setting, it is likely to continue as first line of treatment despite little evidence to support it.
Implications for research.
Clinical trials should be conducted for cessation of NNSHs using intervention groups that have a psychological input, are provided with an orthodontic appliance or have application of a bitter substance to the digit, all compared with a no‐treatment control group. These trials should be well designed and follow the Consolidated Standards of Reporting Trials (CONSORT) statement (Schulz 2010) leading to trials with low levels of bias. The trials should all have a standardised primary outcome, ideally number of participants with cessation of habit following intervention and clear time frames for both intervention and follow‐up. They should also include malocclusion as a core outcome. There was a lack of information on the impact of the interventions on the family and the child, and it is suggested that systematically reviewing qualitative information in this area might be a more appropriate way to source and synthesise these treatment‐associated outcomes.
What's new
| Date | Event | Description |
|---|---|---|
| 28 April 2021 | Review declared as stable | This Cochrane Review is currently not a priority for updating. However, if a substantial body of evidence on the topic becomes available, the review would be updated in the future. |
History
Protocol first published: Issue 9, 2010 Review first published: Issue 3, 2015
Notes
This Cochrane Review is currently not a priority for updating. However, if a substantial body of evidence on the topic becomes available, the review would be updated in the future.
Acknowledgements
The review authors would like to acknowledge the support of the Cochrane Oral Health Group.
Appendices
Appendix 1. MEDLINE (OVID) search strategy
Sucking behavior/
(suck$ and (habit$ or behav$ or routine$)).mp.
("non nutritive suck$" or "non‐nutritive suck$" or "nonnutritive suck$").mp.
or/1‐3
Pacifiers/
Fingersucking/
(pacifier$ or digit$ or dummy or dummies or soother$ or blanket$ or finger$ or thumb$).mp.
or/5‐7
4 and 8
The above subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomized trials in MEDLINE: sensitivity maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of The Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011] (Higgins 2011).
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 2. Cochrane Oral Health Group Trials Register search strategy
(suck* AND (pacif* or dumm* or digit* or finger* or thumb* or soother* or blanket* or non‐nutriti* or "non nutriti*" or nonnutriti*))
Appendix 3. The Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1 MeSH descriptor Sucking behavior this term only #2 (suck* in All Text and (habit* in All Text or behav* in All Text or routin* in All Text)) #3 (suck* in All Text and (non‐nutrit* in All Text or "non nutrit*" in All Text or nonnutrit* in All Text)) #4 (#1 or #2 or #3) #5 MeSH descriptor Pacifiers this term only #6 MeSH descriptor Fingersucking this term only #7 (pacifier* in All Text or digit* in All Text or dummy in All Text or dummies in All Text or soother* in All Text or blanket* in All Text or finger* in All Text or thumb* in All Text) #8 (#5 or #6 or #7) #9 (#4 and #8)
Appendix 4. EMBASE (OVID) search strategy
Sucking behavior/
(suck$ and (habit$ or behav$ or routine$)).mp.
("non nutritive suck$" or "non‐nutritive suck$" or "nonnutritive suck$").mp.
or/1‐3
Pacifiers/
Fingersucking/
(pacifier$ or digit$ or dummy or dummies or soother$ or blanket$ or finger$ or thumb$).mp.
or/5‐7
4 and 8
The above subject search was linked to the Cochrane Oral Health Group filter for EMBASE via OVID:
1. random$.ti,ab. 2. factorial$.ti,ab. 3. (crossover$ or cross over$ or cross‐over$).ti,ab. 4. placebo$.ti,ab. 5. (doubl$ adj blind$).ti,ab. 6. (singl$ adj blind$).ti,ab. 7. assign$.ti,ab. 8. allocat$.ti,ab. 9. volunteer$.ti,ab. 10. CROSSOVER PROCEDURE.sh. 11. DOUBLE‐BLIND PROCEDURE.sh. 12. RANDOMIZED CONTROLLED TRIAL.sh. 13. SINGLE BLIND PROCEDURE.sh. 14. or/1‐13 15. ANIMAL/ or NONHUMAN/ or ANIMAL EXPERIMENT/ 16. HUMAN/ 17. 16 and 15 18. 15 not 17 19. 14 not 18
Appendix 5. PsycINFO (OVID) search strategy
1. exp Sucking/ 2. (suck$ and (habit$ or behav$ or routine$)).mp. 3. ("non nutritive suck$" or "non‐nutritive suck$" or "nonnutritive suck$").mp. 4. or/1‐3 5. (pacifier$ or digit$ or dummy or dummies or soother$ or blanket$ or finger$ or thumb$).mp. 6. 4 and 5
The above subject search was linked to the Cochrane Oral Health Group filter for PsycINFO via OVID:
1. exp clinical trials/ 2. (clin$ adj25 trial$).ti,ab. 3. placebo$.ti,ab. 4. random$.ti,ab. 5. ((randomised adj controlled adj trial$) or (randomized adj controlled adj trial$)).mp. 6. (controlled adj clinical adj trial$).mp. 7. (random adj allocat$).mp. 8. ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).ti,ab. 9. (control$ adj4 trial$).mp. 10. (ANIMALS not HUMANS).sh. 11. or/1‐9 12. 11 not 10
Appendix 6. CINAHL (EBSCO) search strategy
S1 MH "Sucking Behavior" S2 (suck* and habit*) or (suck* and behav*) or (suck* and routine*) S3 "non nutritive suck*" or "nonnutritive suck*" or "non‐nutritive suck*" S4 S1 or S2 or S3 S5 MH Pacifiers S6 pacifier* or digit* or dummy or dummies or soother* or blanket* or finger* or thumb* S7 S5 or S6 S8 S4 and S7
The above subject search was linked to the Cochrane Oral Health Group filter for CINAHL via EBSCO:
S1 MH Random Assignment or MH Single‐blind Studies or MH Double‐blind Studies or MH Triple‐blind Studies or MH Crossover design or MH Factorial Design S2 TI ("multicentre study" or "multicenter study" or "multi‐centre study" or "multi‐center study") or AB ("multicentre study" or "multicenter study" or "multi‐centre study" or "multi‐center study") or SU ("multicentre study" or "multicenter study" or "multi‐centre study" or "multi‐center study") S3 TI random* or AB random* S4 AB "latin square" or TI "latin square" S5 TI (crossover or cross‐over) or AB (crossover or cross‐over) or SU (crossover or cross‐over) S6 MH Placebos S7 AB (singl* or doubl* or trebl* or tripl*) or TI (singl* or doubl* or trebl* or tripl*) S8 TI blind* or AB mask* or AB blind* or TI mask* S9 S7 and S8 S10 TI Placebo* or AB Placebo* or SU Placebo* S11 MH Clinical Trials S12 TI (Clinical AND Trial) or AB (Clinical AND Trial) or SU (Clinical AND Trial) S13 S1 or S2 or S3 or S4 or S5 or S6 or S9 or S10 or S11 or S12
Appendix 7. US National Institutes of Health Trials Register (ClinicalTrials.gov) and the WHO International Clinical Trials Registry Platform search strategy
suck AND pacifier suck AND dummy suck AND thumb suck AND finger suck AND digit
Data and analyses
Comparison 1. Orthodontic appliances versus no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Sucking cessation (short term) | 2 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.53 [1.67, 25.53] |
| 1.2 Sucking cessation (long term) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.3 Occlusion (short term) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 2. Psychological intervention versus no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Sucking cessation (short term) | 2 | 78 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.16 [1.18, 32.10] |
| 2.2 Sucking cessation (long term) | 1 | 57 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.25 [1.65, 23.65] |
Comparison 3. Psychological intervention + orthodontic treatment versus no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Sucking cessation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
Comparison 4. Aversive taste versus psychological intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Sucking cessation (short term) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 5. Orthodontic appliances versus alternative orthodontic appliance.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Sucking cessation (short term) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 6. Psychological intervention versus alternative psychological intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Sucking cessation (short term) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1.1 HR versus DRO | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1.2 Positive reinforcement versus negative reinforcement | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.2 Sucking cessation (long term) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 7. Psycholgical+orthodontic versus psychological+alternative orthodontic.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Sucking cessation (short term) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1.1 Psych+palatal arch versus psych+palatal crib | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Azrin 1980.
| Study characteristics | ||
| Methods | Location: USA Setting: Secondary care No mention of funding or ethical approval |
|
| Participants | Children with digit sucking habits, aged 2.5 to 14 yrs with mean of 8.3 yrs. Recruitment through self‐referral following a newspaper advertisement. 32 recruited and data for 30 analysed, 2 lost to follow‐up. |
|
| Interventions |
Habit reversal (HR) A single counselling session (n = 18) Part 1, the children were taught competing behaviours such as making a fist or grasping a convenient object for 1‐3 minutes (measured by counting to 100). Part 2, children described the intervention to their parent and requested parental assistance. Part 3, “annoyance review” in which the child listed all the problems created by thumb sucking and “heightened awareness” in which the child acted out the usual response sequence including the precursors of thumb sucking to identify the stimulus antecedents. Parents were instructed to provide social support by praising the child when sucking was absent and provided treats and surprises when sucking was absent for an extended period and stopping television or bedtime stories when sucking occurred. Aversive tasting substance application (ATSA) The parents of the children (n = 12) received a single phone call informing them about the use of a commercially available aversive tasting substance to be applied morning and evening. |
|
| Outcomes | 1. Percentage of children with no thumb sucking at 3 months 2. Mean number of episodes per day in each group at 3 months |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Random assignment by a coin flip." |
| Allocation concealment (selection bias) | Unclear risk | Method of concealment not described. |
| Blinding of participants and personnel (performance bias) Patient | High risk | Blinding of child patient not possible. |
| Blinding of participants and personnel (performance bias) Operator | High risk | Blinding of parents who carried out intervention not possible. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Parents acted as assessors. Blinding not possible. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Information on loss to follow‐up only given for the intervention group which had a high dropout rate of 50% at 20 months. Loss to follow‐up was not reported for control group. |
| Selective reporting (reporting bias) | High risk | No prespecification of outcomes to be assessed. |
| Other bias | High risk | There were two points at which bias may have been introduced into the sample: "Children were enlisted as subjects by a newspaper advertisement." "Two of the controls were not used since their parents declined to participate in the control procedure to which they were assigned in that they had used that procedure previously without success." |
Christensen 1987.
| Study characteristics | ||
| Methods | Location: Australia Setting: recruitment in secondary care, intervention at patients' home No mention of funding or ethical approval |
|
| Participants | Children age range 4‐9 yrs and mean 6.3 yrs, 43% female and 57% male. A newspaper article invited parents "to apply for inclusion in the programme if they were experiencing difficulty with their child's thumb‐sucking behaviour." 30 recruited and analysed, no loss to follow‐up |
|
| Interventions |
Habit reversal (HR) For the HR and DRO groups parents identified a home setting associated with high levels of thumb‐sucking (TV viewing). This setting served as the training setting. Two other settings were identified, generalising setting one with high levels of thumb sucking were seen, and generalisation setting two which was thumb sucking at bedtime. Observations of the child in the training setting were conducted at baseline and on two different days in each phase for the HR and DRO groups and follow‐up for the control group. Observations were scheduled to coincide with a time when the child usually watched TV, or was at play, depending on what had been selected by the parents as the training setting. Parents were instructed to involve their child (n = 10) in a discussion about working together for the next 10 days to overcome the habit, with the child identifying the stimulus conditions associated with thumb sucking. The parents provided feedback on how the competing response exercise was to be performed. This involved clenching both fists and counting to 20. Parents were instructed to carry out the procedures for 10 consecutive days. Differential reinforcement of other behaviour (DRO) This was an escalating schedule of reinforcement contingent upon non‐occurrence of thumb sucking and was implemented in two phases. Parents discussed with the child (n = 10) how they would be working together for the 10 days to overcome the habit and that privileges could be earned by not thumb sucking and that there would be daily rules for which tokens could be earned and exchanged for these privileges. The child selected the reward they would like to earn in exchange for the tokens that day. The training period continued for 10 consecutive days. Three months after the termination of training two further observation sessions were conducted in each setting. Waiting list control group This group received no treatment (n = 10). |
|
| Outcomes | 1. Number of children with cessation of habit ‐ post treatment and 3 months follow‐up 2. Proportion of time spent sucking ‐ pre‐test to follow‐up 3. Psychological effects ‐ oppositional behaviour ‐ pre‐test to follow‐up 4. Parents recommendation of intervention Outcomes were measured for HR and DRO at pre‐test, post‐test and 3 months after the termination of training (with 2 observation sessions in each setting) for outcomes 2 and 3. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Using a sampling‐without‐replacement procedure (Keppel, 1973)." |
| Allocation concealment (selection bias) | Unclear risk | Method of concealment was not described |
| Blinding of participants and personnel (performance bias) Patient | High risk | Blinding of child patient not possible |
| Blinding of participants and personnel (performance bias) Operator | High risk | Blinding of parents who carried out intervention not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information was given regarding whether the "trained observers" were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No explicit statement of children's follow‐up rates or completeness of data; however, both intervention groups had data presented equivalent to the number of children enrolled in the study. No follow‐up information was given on control group, although it was implied that they were retained |
| Selective reporting (reporting bias) | Low risk | All three outcomes stated in the introductory text were reported on |
| Other bias | High risk | As children were "self‐referred to the programme following a newspaper article" this may have introduced bias into the sample |
Friman 1990.
| Study characteristics | ||
| Methods | Location: USA Setting: Participants' home and secondary care Funded by the US department of health and human services |
|
| Participants | 4 years of age or older, with a chronic habit, and a high level of parental concern about the habit. Age range of 4 to 11.6 yrs 24 patients referred from the patients’ local paediatric provider met the inclusion criteria; however, 2 did not complete baseline questionnaires and were excluded |
|
| Interventions |
Aversive taste treatment and reward system The parents were instructed to coat their child’s thumbnail with a commercially available substance designed to treat thumb sucking (n = 11). It was applied once in the morning when the child awoke, once just before bed and once each time an instance of sucking was observed. A fading procedure was used to discontinue the treatment, which involved eliminating the morning application after having one week where sucking was not observed, and the evening application was discontinued after an additional week with no sucking. The reward system required the preparation of 50 to 100 slips of paper on which the parents had written a variety of treats with a value less than $10. These slips of paper were placed in a grab bag and the participants were allowed a take one when an observed instance of non thumb sucking occurred. Control group This group did not receive any treatment (n = 11) |
|
| Outcomes | 1. Percentage intervals with observed thumb sucking ‐ immediately post treatment compared with pre treatment (3‐month data were incomplete) 2. Acceptability of intervention ‐ 7‐point scale at 3 months |
|
| Notes | This study may have limited generalisability due to the stringent inclusion criteria: "Participants were referred to the study by local pediatric providers." "Five children were excluded because the children sucked their thumbs only before bed." "... the parents had to express a high level of concern about thumb sucking." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomly assigned ... based on a coin flip" |
| Allocation concealment (selection bias) | Unclear risk | Method of concealment was not described |
| Blinding of participants and personnel (performance bias) Patient | High risk | Blinding of child patient not possible |
| Blinding of participants and personnel (performance bias) Operator | High risk | Blinding of parents who carried out intervention not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Parents acted as assessors. Blinding not possible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropout rates were not reported, although it was implied that all children were followed up "posttest." At one‐year follow‐up, although it is stated that 8 children from the 21 out of 22 participants were followed up, no data are given on whether they were allocated to the intervention or control group |
| Selective reporting (reporting bias) | High risk | No prespecification of outcomes to be assessed |
| Other bias | Low risk | "Participants were referred to the study by local pediatric providers." |
Haryett 1967.
| Study characteristics | ||
| Methods | Location: Canada Setting: participants' home and secondary care No mention of funding or ethical approval |
|
| Participants | Children 4 years old and older Participants were referred by dentists Digit suckers 66 patients were recruited, one lost to follow‐up, 65 analysed |
|
| Interventions |
Control group This group received no treatment (n = 10) Psychological treatment The psychological intervention involved 2 parts: gaining the child’s co‐operation in breaking the thumb sucking habit by showing them in a mirror what the habit had done to the position of their own teeth, showing them photos and models of thumb suckers and creating a desire to break the habit; the parent, usually the mother, was given instructions to reward periods where thumb sucking did not take place. The reward was giving the child their full attention and ignoring them if the habit occurred (n = 11). Palatal arch An appliance banded to either the maxillary second deciduous molars or first permanent molars, with a stainless steel wire fitted behind the upper incisors on the gingival margins of the palatal aspect of the upper incisors (n = 11) Palatal arch and psychological treatment A combination of the two techniques described above (n = 11) Palatal crib An appliance banded to either the maxillary second deciduous molars or first permanent molars, with stainless steel wire fitted behind the upper incisors, over the palatal ruggae with “vertical fencelike projections extended as deep as the lateral excursions of the mandible will allow” (n = 11) Palatal crib and psychological treatment A combination of the palatal crib treatment and psychological treatment described (n = 11) The participants were randomly assigned to one of the 6 groups. All treatment lasted 10 months and after this, where appropriate, orthodontic appliances were removed |
|
| Outcomes | The outcomes were measured one month after the intervention had stopped. 1. Cessation of habit (expressed both as number of participants and %) at 1 month, 1 yr, 2 yrs and 3 yrs 2. Discomfort from intervention ‐ upset and eating difficulty 3. Psychological effects ‐ development of mannerisms |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information given "divided at random" |
| Allocation concealment (selection bias) | Unclear risk | Method of concealment not described |
| Blinding of participants and personnel (performance bias) Patient | High risk | Blinding of child participant not possible |
| Blinding of participants and personnel (performance bias) Operator | High risk | Blinding of parents who carried out intervention not possible. Parents were involved in the interventions for children in three of the groups which involved "psychologic treatment," and the other groups where an orthodontic appliance was used |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Parents acted as assessors. Blinding not possible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no missing outcome data. Only one patient out of 66 was lost at 10‐month follow‐up, "moved away." |
| Selective reporting (reporting bias) | Unclear risk | Unable to tell whether individual outcomes were prespecified as nonspecific "report the psychologic effects and the relative effectiveness of various methods of treating chronic thumb‐sucking." |
| Other bias | Low risk | Patients were recruited following referral by their own dentists |
Larsson 1972.
| Study characteristics | ||
| Methods | Location: Sweden Setting: Participants' home and secondary care |
|
| Participants | Children 9 years of age Patients were identified following an incidence study (Larsson 1971), which investigated pacifier and finger sucking in 920 children resident in a particular area of Sweden Digit suckers 76 recruited and analysed immediately post intervention. One lost to follow‐up at one year |
|
| Interventions |
Positive reinforcement Participants’ mothers were given specific instructions about different forms of encouragement, and reinforcement was also given by a psychologist (n = 19) Negative reinforcement Children and their parents were given information about the consequences and risks of prolonged finger sucking. They were given models of the children’s teeth home with them (n = 19) Palatal crib The palatal crib had spurs welded to bands cemented to the maxillary first molar teeth. “The crib lay a millimetre or so from the mucosa and extended just behind the maxillary incisors. The spurs were rounded in front and so adjusted that they did not disturb the occlusion” (n = 19) Control No treatment was provided to this group (n = 19) All interventions lasted 2 ½ months, following which all appliances were removed and the children were assessed by psychologists |
|
| Outcomes | 1. Cessation of habit (number and % of participants) immediately post intervention, 6 months after completion of treatment and 1 year after completion of treatment | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "divided by lot into three treatment groups and a control group," |
| Allocation concealment (selection bias) | Unclear risk | Method of concealment was not described |
| Blinding of participants and personnel (performance bias) Patient | High risk | Blinding of child participant not possible |
| Blinding of participants and personnel (performance bias) Operator | High risk | Blinding of parents who carried out intervention not possible. Parents were involved in the interventions for children in two of the groups, which involved positive and negative reinforcement, and a third group where an orthodontic appliance was used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Two psychologists "examined and tested" the children pre and post intervention, but no information is given regarding blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no missing outcome data. Only one patient out of 76 "did not wish to participate in the subsequent investigation" and therefore had no follow‐up data |
| Selective reporting (reporting bias) | High risk | No prespecification of outcomes to be assessed |
| Other bias | High risk | Recruitment was limited to children who were judged by their parents "to be intense suckers ‐ children who sucked their fingers at least every evening..." |
Villa 1997.
| Study characteristics | ||
| Methods | Location: USA Setting: secondary care No mention of funding or ethical approval |
|
| Participants | Children aged 8 to 18 yrs Participants were selected following screening "Twenty‐four patients between the ages of 6 and 18 years with digit‐sucking habits were selected within a 4‐month screening period from the patient population at Montefiore Medical Center, Division of Orthodontics, for inclusion in this study." Digit suckers 24 recruited and analysed |
|
| Interventions |
Palatal crib therapy There was no mention of the specific design of this appliance therefore it was assumed it was similar in design to that described by Haryett and Larsson (n = 12). Control This group received no treatment (n = 12) Pretreatment records were taken for the participants and included study models, OPT, lateral cephalogram radiographs, and intra and extra oral photographs. After 3 months, study models were again taken and compared with the pretreatment ones. |
|
| Outcomes | 1. Reduction in anterior open bite, in mm, calculated by comparing measurements from the pre and post intervention study models 2. Reduction in overjet, in mm, calculated by comparing measurements from the pre and post intervention study models 3. Change in arch length, in mm, calculated by comparing measurements from the pre and post intervention study models |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "assigned randomly" |
| Allocation concealment (selection bias) | Unclear risk | Method of concealment was not described |
| Blinding of participants and personnel (performance bias) Patient | High risk | Blinding of child participant not possible |
| Blinding of participants and personnel (performance bias) Operator | High risk | Blinding not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The evaluator was blinded as to group status of each study model." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Drop‐out rates were not reported, although it was implied that all children were followed up. The results section states "Overall 10 males and 14 females were studied." |
| Selective reporting (reporting bias) | Low risk | Outcomes were clearly defined and all reported. |
| Other bias | Unclear risk | Patients were recruited from an orthodontic department patient population. Unclear if sample would be representative of general population. |
yrs = years
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adair 1992 | Observational, non interventional study |
| Al‐Emran 2005 | All participants received the same intervention, no control group |
| Cozza 2006 | Longitudinal controlled study, where control group had no sucking habit |
| Cozza 2007 | No randomisation |
| Degan 2005 | No relevant outcomes reported |
| Friman 1986 | Observational, non interventional study |
| Haryett 1970 | Not an RCT |
| Woods 1999 | Includes nail biters as well as digit suckers and not able to distinguish the results from the data. Issues with randomisation as the control group pretreatment is very different from the two treatment groups. |
RCT: randomised controlled trial
Differences between protocol and review
We decided to contact the authors for any additional information on studies.
We made a post‐hoc decision to regard outcomes observed < 12 months post‐intervention as short‐term outcomes and ≥ 12 months as long‐term outcomes.
Addition of outcome ‐ costs.
Title change (Protocol: Interventions for the cessation of pacifier or digit sucking habits in children).
Contributions of authors
Felicity Borrie (FB) was responsible for co‐ordinating the review. FB, Nicola Innes (NI) and David Bearn (DB) contributed to the protocol and wrote the review. FB and NI were responsible for study selection. FB, NI and DB were responsible for data extraction. FB organised the retrieval of papers and wrote to authors of papers for additional information. FB and NI assessed the risk of bias in included studies. FB, NI, DB and ZIE were responsible for the interpretation and analysis of data. FB and NI assess the studies for risk of bias and ZIE created 'Summary of findings' (GRADE) tables.
Sources of support
Internal sources
School of Dentistry, The University of Manchester, UK
External sources
-
National Institute for Health Research (NIHR), UK
The NIHR is the largest single funder of the Cochrane Oral Health Group.
Disclaimer: The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
-
Cochrane Oral Health Group Global Alliance, Other
The production of all our reviews is assisted by funding from our Global Alliance partners (http://ohg.cochrane.org/): British Association for the Study of Community Dentistry, UK; British Association of Oral Surgeons, UK; British Orthodontic Society, UK; British Society of Paediatric Dentistry, UK; British Society of Periodontology, UK; Canadian Dental Hygienists Association, Canada; Mayo Clinic, USA; National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; and Royal College of Surgeons of Edinburgh, UK
Declarations of interest
Felicity RP Borrie: none known David R Bearn: none known Nicola PT Innes: none known Zipporah Iheozor‐Ejiofor: none known
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Azrin 1980 {published data only}
- Azrin NH, Nunn R, Frantz-Renshaw S. Habit reversal treatment of thumbsucking. Behaviour Research and Therapy 1980;18:395-9. [DOI] [PubMed] [Google Scholar]
Christensen 1987 {published data only}
- Christensen AP, Sanders MR. Habit reversal and differential reinforcement of other behaviour in the treatment of thumb-sucking: an analysis of generalization and side-effects. Journal of Child Psychology and Psychiatry and Allied Disciplines 1987;28(2):281-95. [DOI] [PubMed] [Google Scholar]
Friman 1990 {published data only}
- Friman PC, Leibowitz JM. An effective and acceptable treatment alternative for chronic thumb- and finger-sucking. Journal of Pediatric Psychology 1990;15(1):57-65. [DOI] [PubMed] [Google Scholar]
Haryett 1967 {published data only}
- Haryett RD, Hansen FC, Davidson PO, Sandilands ML. Chronic thumb-sucking: The psychologic effects and the relative effectiveness of various methods of treatment. American Journal of Orthodontics 1967;53(8):569-85. [DOI] [PubMed] [Google Scholar]
Larsson 1972 {published data only}
- Larsson E. Dummy - and finger-sucking habits with special attention to their significance for facial growth and occlusion. Swedish Dental Journal 1972;65:1-5. [PubMed] [Google Scholar]
Villa 1997 {published data only}
- Villa NL, Cisneros GJ. Changes in the dentition secondary to palatal crib therapy in digit-suckers: a preliminary study. Pediatric Dentistry 1997;19(5):323-6. [PubMed] [Google Scholar]
References to studies excluded from this review
Adair 1992 {published data only}
- Adair SM, Milano M, Dushku JC. Evaluation of the effects of orthodontic pacifiers on the primary dentitions of 24- to 59-month-old children: preliminary study. Pediatric Dentistry 1992;14:13-8. [PubMed] [Google Scholar]
Al‐Emran 2005 {published data only}
- Al-Emran S, Al-Jobair A. An assessment of a new reminder therapy technique for ceasing digit sucking habits in children.. Journal of Clinical Pediatric Dentistry 2005;30(1):35-8. [DOI] [PubMed] [Google Scholar]
Cozza 2006 {published data only}
- Cozza P, Baccetti T, Franchi L, McNamara JA. Treatment effects of a modified quad-helix in patients with dentoskeletal open bites. American Journal of Orthodontics and Dentofacial Orthopedics 2006;129:734-9. [DOI] [PubMed] [Google Scholar]
Cozza 2007 {published data only}
- Cozza P, Mucedero M, Baccetti T and Franchi L. Treatment and posttreatment effects of quad-helix/crib therapy of dentoskeletal open bite. Angle Orthodontist 2007;77(4):640-5. [DOI] [PubMed] [Google Scholar]
Degan 2005 {published data only}
- Degan VV, Puppin-Rontani RM. Removal of sucking habits and myofunctional therapy; establishing swallowing and tongue rest position [Remoção de hábitos e terapia miofuncional: restabeleciimento da deglutição e repouso lingual]. PRO-FONO: Revista de Actualizacao Cientifica 2005;17(3):375-82. [DOI] [PubMed] [Google Scholar]
Friman 1986 {published data only}
- Friman P, Barone VJ, Christophersen ER. Aversive taste treatment of finger and thumb sucking. Pediatrics 1986;78(1):174-6. [PubMed] [Google Scholar]
Haryett 1970 {published data only}
- Haryett RD, Hansen FC, Davidson PO. Chronic thumb-sucking. A second report on treatment and its psychological effects. American Journal of Orthodontics 1970;57(2):164-78. [DOI] [PubMed] [Google Scholar]
Woods 1999 {published data only}
- Woods DW, Murray LK, Fuqua W, Seif TA, Boyer LJ, Siah A. Comparing the effectiveness of similar and dissimilar competing responses in evaluating the habit reversal treatment for oral-digital habits in children. Journal of Behavior Therapy and Experimental Psychiatry 1999;30:289-300. [DOI] [PubMed] [Google Scholar]
Additional references
Al‐Jobair 2004
- Al-Jobair A, Al-Emran SES. Attitudes of Saudi Arabian mothers towards the digit-sucking habit in children. International Journal of Paediatric Dentistry 2004;14(5):347-54. [DOI] [PubMed] [Google Scholar]
Baalack 1971
- Baalack IB, Frisk AK. Finger-sucking in children. A study of incidence and occlusal conditions. Acta Odontologica Scandinavica 1971;29(5):499-512. [DOI] [PubMed] [Google Scholar]
Bernstein 1954
- Bernstein M. The relation of speech defects and malocclusion. American Journal of Orthodontics 1954;40:149-50. [Google Scholar]
Bishara 2006
- Bishara SE, Warren JJ, Broffitt B, Levy SM. Changes in the prevalence of nonnutritive sucking patterns in the first 8 years of life. American Journal of Orthodontics and Dentofacial Orthopedics 2006;130(1):31-6. [DOI] [PubMed] [Google Scholar]
Blass 1999
- Blass EM, Watt LB. Suckling- and sucrose-induced analgesia in human newborns. Pain 1999;83(3):611-23. [DOI] [PubMed] [Google Scholar]
Bowden 1966
- Bowden BD. A longitudinal study of digital and dummy sucking. Australian Dental Journal 1966;11(3):184-90. [DOI] [PubMed] [Google Scholar]
Burden 1995
- Burden DJ. An investigation of the association of overjet size, lip coverage, and traumatic injury to maxillary incisors. European Journal of Orthodontics 1995;17:513-7. [DOI] [PubMed] [Google Scholar]
Curtis 2007
- Curtis SJ, Jou H, Ali S, Vandermeer B, Klassen T . A randomized controlled trial of sucrose and/or pacifier as analgesia for infants receiving venipuncture in a pediatric emergency department. BMC Pediatrics 2007;7:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Farsi 1997
- Farsi NM, Salama FS. Sucking habits in Saudi children: prevalence, contributing factors and effects on the primary dentition. Pediatric Dentistry 1997;19(1):28-33. [PubMed] [Google Scholar]
Fukuta 1996
- Fukuta O, Braham RL, Yokoi K, Kurosu K. Damage to the primary dentition resulting from thumb and finger (digit) sucking. ASDC Journal of Dentistry for Children 1996;63(6):403-7. [PubMed] [Google Scholar]
Glendor 2009
- Glendor U. Aetiology and risk factors related to traumatic dental injuries - a review of the literature. Dental Traumatology 2009;25:19-31. [DOI] [PubMed] [Google Scholar]
Greenlee 2011
- Greenlee GM, Huang GJ, Chen SS-H, Chen J, Koepsell T, Hujoel P. Stability of treatment for anterior open-bite malocclusion: A meta-analysis. American Journal of Orthodontics and Dentofacial Orthopedics February 2011;139(2):154-69. [DOI] [PubMed] [Google Scholar]
Hauck 2005
- Hauck FR, Omojokun OO, Siadaty MS. Do pacifiers reduce the risk of sudden infant death syndrome? A meta-analysis. Pediatrics 2005;116(5):e716-23. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Laine 1987
- Laine T, Jaroma M, Linnasalo AL. Relationships between interincisal occlusion and articulatory components of speech. Folia Phoniatrica 1987;39(2):78-86. [DOI] [PubMed] [Google Scholar]
Larsson 2001
- Larsson E. Sucking, chewing, and feeding habits and the development of crossbite: a longitudinal study of girls from birth to 3 years of age. Angle Orthodontist 2001;71(2):116-9. [DOI] [PubMed] [Google Scholar]
Li 2006
- Li D, Willinger M, Petitti DB, Odouli R, Liu L, Hoffman HJ. Use of a dummy (pacifier) during sleep and risk of sudden infant death syndrome (SIDS): population based case-control study. BMJ 2006;332(7532):18-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mistry 2010
- Mistry P, Moles DR, O'Neil J, Noar J. The occlusal effects of digit sucking habits amongst school children in Northamptonshire (UK). Journal of Orthodontics 2010;37:87-92. [DOI] [PubMed] [Google Scholar]
Modeer 1982
- Modder T, Odenrick L, Lindner A. Sucking habits and their relation to posterior cross-bite in 4-year-old children. Scandinavian Journal of Dental Research 1982;90(4):323-8. [DOI] [PubMed] [Google Scholar]
Norton 2012
- Norton E, O'Connell AC. Traumatic dental injuries and their association with malocclusion in the primary dentition of Irish children. Dental Traumatology 2012;28:81-6. [DOI] [PubMed] [Google Scholar]
Ogaard 1994
- Ogaard B, Larsson E, Lindsten R. The effect of sucking habits, cohort, sex, intercanine arch widths, and breast or bottle feeding on posterior crossbite in Norwegian and Swedish 3-year-old children. American Journal of Orthodontics and Dentofacial Orthopedics 1994;106(2):161-6. [DOI] [PubMed] [Google Scholar]
Patel 2008
- Patel A. Digit sucking habits in children resident in Kettering (UK). Journal of Orthodontics 2008;35:255-61. [DOI] [PubMed] [Google Scholar]
Petren 2008
- Petren S, Bondemark L. Correction of unilateral posterior crossbite in the mixed dentition: a randomized controlled trial. American Journal of Orthodontics and Dentofacial Orthopedics 2008;133(6):790.e7-13. [DOI] [PubMed] [Google Scholar]
Proffit 2013
- Proffit WR, Fields HW, Sarver DM, Ackerman JL. Chapter 11 Moderate nonskeletal problems in preadolescent children. In: Contemporary Orthodontics. 5th edition. St Louis: Elsevier, 2013:413-6. [Google Scholar]
Reid 1984
- Reid DA, Price AH. Digital deformities and dental malocclusion due to finger sucking. British Journal of Plastic Surgery 1984;37(4):445-52. [DOI] [PubMed] [Google Scholar]
Sandler 2011
- Sandler PJ, Madahar AK, Murray A. Anterior open bite: aetiology and management. Dental Update October 2011;38(8):522-32. [DOI] [PubMed] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ (clinical research edition) 2010;340:c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Singh 2008
- Singh SP, Utreja A, Chawla HS. Distribution of malocclusion types among thumb suckers seeking orthodontic treatment. Journal of Indian Society of Pedodontics and Preventive Dentistry 2008;26 Suppl 3:S114-7. [PubMed] [Google Scholar]
Svedmyr 1979
- Svedmyr B. Dummy sucking. A study of its prevalence, duration and malocclusion consequences. Swedish Dental Journal 1979;3(6):205-10. [PubMed] [Google Scholar]
Vazquez‐Nava 2006
- Vazquez-Nava F, Quezada-Castillo JA, Oviedo-Trevino S, Saldivar-Gonzalez AH, Sanchez-Nuncio HR, Beltran-Guzman FJ, et al. Association between allergic rhinitis, bottle feeding, non-nutritive sucking habits, and malocclusion in the primary dentition. Archives of Disease in Childhood 2006;91(10):836-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Warren 2002
- Warren JJ, Bishara SE. Duration of nutritive and nonnutritive sucking behaviors and their effects on the dental arches in the primary dentition. American Journal of Orthodontics and Dentofacial Orthopedics 2002;121(4):347-56. [DOI] [PubMed] [Google Scholar]


