Key Points
Question
Are there differences in long-term clinical outcomes between patients who received skeletonized or pedicled internal thoracic arteries (ITAs) for coronary artery bypass grafting in the Arterial Revascularization Trial (ART)?
Findings
In this post hoc analysis of the ART trial including 2161 patients, skeletonized ITA harvesting was associated with similar survival but higher rates of adverse cardiovascular events at 10-year follow-up compared with pedicled ITA harvesting. This difference was larger for patients operated on by surgeons who enrolled 50 patients or less in the trial.
Meaning
Further evaluation of the safety and effectiveness of the skeletonized ITA harvesting technique, with particular regard to surgeon experience, is necessary.
This post hoc analysis of the Arterial Revascularization Trial compares the long-term clinical outcomes of skeletonized and pedicled internal thoracic artery harvesting for coronary artery bypass surgery.
Abstract
Importance
Recent evidence has suggested that skeletonization of the internal thoracic artery (ITA) is associated with worse clinical outcomes in patients undergoing coronary artery bypass surgery (CABG).
Objective
To compare the long-term clinical outcomes of skeletonized and pedicled ITA for CABG.
Design, Setting, and Participants
The Arterial Revascularization Trial (ART) was a 2-group, multicenter trial comparing the use of a bilateral ITA vs a single ITA for CABG at 10 years. Patients in the ART trial were stratified by ITA harvesting technique: skeletonized vs pedicled. Data were collected from June 2004 to December 2017, and data were analyzed from June to July 2021.
Interventions
In this analysis, the 10-year clinical outcomes were compared between patients who received skeletonized vs pedicled ITAs.
Main Outcomes and Measures
The primary outcome was all-cause mortality. The secondary outcomes were a composite of major adverse cardiac events (MACE) including all-cause mortality, myocardial infarction, and repeated revascularization and a composite including MACE and sternal wound complication (SWC). Cox regression and propensity score matching were used.
Results
Of 2161 included patients, 295 (13.7%) were female, and the median (interquartile range) age was 65.0 (58.0-70.0) years. At 10 years, the risk of all-cause mortality was not significantly different between the pedicled and skeletonized groups (hazard ratio [HR], 1.12; 95% CI, 0.92-1.36; P = .27). However, the long-term risks of the secondary outcomes were significantly higher in the skeletonized group compared with the pedicled group (MACE: HR, 1.25; 95% CI, 1.06-1.47; P = .01; MACE and SWC: HR, 1.22; 95% CI, 1.05-1.43; P = .01). The difference was not seen when considering only patients operated on by surgeons who enrolled 51 patients or more in the trial (MACE: HR, 1.07; 95% CI, 0.82-1.39; P = .62; MACE and SWC: HR, 1.04; 95% CI, 0.80-1.34; P = .78).
Conclusions and Relevance
While the long-term survival of patients was not different between groups, the rate of adverse cardiovascular events was consistently higher in the skeletonized group and the difference was associated with surgeon-related factors. Further evidence on the outcome of skeletonized ITA is needed.
Introduction
The use of the internal thoracic artery (ITA) to graft the left anterior descending artery is the cornerstone of the modern coronary artery bypass grafting (CABG) operation and a class I recommendation in contemporary myocardial revascularization guidelines.1,2 The use of 2 ITAs has been associated with improved outcomes in observational studies but not in randomized trials.3
The ITA can be harvested as a pedicled or as a skeletonized conduit: in the first case, the artery is harvested together with the surrounding fat, the satellite veins, and part of the endothoracic fascia (en bloc), while with the skeletonized technique, only the artery is separated from the chest wall.4 The skeletonized technique is technically more complex and more time consuming5 but has been associated with relevant technical and clinical benefits, most importantly a reduction in the risk of postoperative sternal wound complications (SWCs).6,7
Previous studies have suggested that the 2 harvesting techniques were similar in term of ITA patency and cardiovascular outcomes, and the skeletonized technique was generally recommended to reduce the risk of sternal complications or allow more complex grafting strategies.8 However, recently, a post hoc analysis of the Cardiovascular Outcomes for People Using Anticoagulation Strategies (COMPASS) trial reported a significantly higher rate of graft occlusion and adverse cardiovascular events for patients who received skeletonized vs pedicled ITAs.9
Because of the key role that the ITA plays in modern CABG surgery and the potentially important implications of the findings of an increased risk of graft failure and clinical events with the skeletonized technique, we performed an unplanned post hoc analysis of the Arterial Revascularization Trial (ART)—to our knowledge, the largest CABG trial with long-term follow-up to date—aimed at comparing the long-term clinical outcomes of patients who received skeletonized vs pedicled ITAs.10
Methods
The ART trial rationale and results have been previously published.10,11,12,13 In brief, the ART trial is the largest CABG trial to date with 10-year follow-up and investigated the difference in survival between patients receiving single ITA and bilateral ITA for CABG. Ethical approval was obtained at all 28 participating centers, and written informed consent to participation and data utilization was provided by all participants.
Present Analysis: Patient Population and Outcomes
This is an unplanned post hoc analysis that was designed by the ART Steering Committee after the publication of a post hoc analysis of the COMPASS trial showing higher failure rate for skeletonized vs pedicled ITAs.9 Patients in the ART trial with available details of the ITA harvesting technique were included in this analysis. Information on harvesting technique was not recorded from the beginning of the ART trial and was available for 2161 of 3102 patients (69.7%). Patients were stratified by ITA harvesting technique: skeletonized vs pedicled.
As surgeon experience is known to affect the outcomes of ITA grafting,14 surgeons in the ART trial were categorized based on the number of patients included in the trial using the same cutoff used in previous analyses from the ART trial (50 patients or less vs 51 patients or more).10,15 In addition, individual surgeon volume (as a continuous variable) was added to the main Cox model in a sensitivity analysis.
In a secondary analysis, we limited the comparison to patients with a single ITA to the left anterior descending artery (385 in the skeletonized group and 469 in the pedicled group); this was done to reduce heterogeneity and because the clinical consequences of failure of the ITA to the left anterior descending artery are known to be more important than those of failure of ITA grafts to other coronary territories.16 In another exploratory analysis, we limited the comparison to the events that occurred in the first 2 years of follow-up; this was done because graft failure is mostly due to technical causes and surgical factors during the first years after surgery and to atherosclerosis in the late follow-up period, and failure owing to the harvesting technique is more likely to occur in the first 2 years.17
For all the analyses, the primary outcome was all-cause mortality at 10-year follow-up; the secondary outcomes were a composite of major adverse cardiac events (MACE) at 10 years including all-cause mortality, myocardial infarction, and repeated revascularization and a composite including MACE and SWC, as defined in previous publications from the ART trial.10,12 All outcomes were centrally adjudicated; individual outcome definitions are provided in the eMethods in Supplement 1.
Statistical Analysis
Categorical variables were reported as counts and percentages and compared among groups using χ2 or Fisher exact test, as appropriate. Continuous variables were reported as means and standard deviations or medians and interquartile ranges (IQRs) and compared using t test or Mann-Whitney U test, respectively, after checking for normality.
In the main analysis, Cox regression was used to compare the skeletonized and pedicled groups. Variables included in the model were age, sex, New York Heart Association (NYHA) heart failure class, diabetes, chronic obstructive pulmonary disease, peripheral vascular disease, prior stroke, prior myocardial infarction, left ventricular ejection fraction, bilateral vs single ITA, use of the radial artery graft, off-pump vs on-pump CABG, and skeletonized vs pedicled ITA harvesting; collinearity was tested using variance inflation factor.
In a sensitivity analysis, we used propensity score matching (PSM) rather than Cox regression for statistical adjustment. PSM was done using the nearest-neighbor method (1:1; caliper, 0.2). Standardized mean difference and balance plots were used to assess balance among matched variables, with a standardized mean difference less than 10 considered as a proper matching. PSM included the same variables included in the Cox model.
A 2-tailed P value threshold of .05 was used. Adjustment for multiplicity was not used as this is a post hoc analysis and results must be seen only as hypothesis generating. All analyses were performed using R version 3.6.2 (The R Foundation) with the following R packages: Publish, survminer, and tableone.
Results
Of the 3102 patients enrolled in the ART trial, 2161 (69.7%) had available information on the ITA harvesting technique (995 in the skeletonized group and 1166 in the pedicled group) and were included in the present analysis. Of 2161 included patients, 295 (13.7%) were female, and the median (IQR) age was 65.0 (58.0-70.0) years. Baseline characteristics of patients with and without information on the ITA harvesting technique are shown in eTable 1 in Supplement 1. All patients included in the present analysis had complete 10-year follow-up data. Compared with the pedicled group, patients in the skeletonized group were older (median [IQR] age of 65.0 [58.0-71.0] years vs 64.0 [58.0-70.0] years), more often female (161 of 995 [16.2%] vs 134 of 1166 [11.5%]), had a lower NYHA class (NYHA class III or IV in 202 of 995 [20.3%] vs 300 of 1166 [25.7%]), received off-pump CABG more often (593 of 995 [59.6%] vs 514 of 1166 [44.2%]), and received a higher number of grafts (more than 3 grafts in 380 of 995 [38.2%] vs 383 of 1166 [32.8%]) (Table 1).
Table 1. Baseline Characteristics of the Patients.
| Characteristic | No. (%) | P value | |
|---|---|---|---|
| Pedicled ITA (n = 1166) | Skeletonized ITA (n = 995) | ||
| Age, median (IQR), y | 64.0 (58.0-70.0) | 65.0 (58.0-71.0) | .01 |
| Female | 134 (11.5) | 161 (16.2) | .002 |
| BMI, median (IQR)a | 28.1 (25.6-30.7) | 27.7 (25.3-31.0) | .50 |
| NYHA class of III to IV | 300 (25.7) | 202 (20.3) | .004 |
| Diabetes | 264 (22.6) | 261 (26.2) | .06 |
| Smoking | 153 (13.1) | 144 (14.5) | .40 |
| COPD | 91 (7.8) | 58 (5.8) | .09 |
| PVD | 86 (7.4) | 77 (7.7) | .81 |
| Prior stroke | 31 (2.7) | 33 (3.3) | .44 |
| Prior MI | 487 (41.8) | 392 (39.4) | .28 |
| LVEF <50% | 279 (25.7) | 236 (23.7) | .32 |
| Race and ethnicityb | |||
| African | 0 | 4 (0.4) | <.001 |
| Afro-Caribbean | 1 (0.1) | 0 | |
| East Asian | 3 (0.3) | 2 (0.2) | |
| Southeast Asian | 95 (8.2) | 24 (2.4) | |
| White | 1052 (90.3) | 919 (92.4) | |
| Other | 14 (1.2) | 46 (4.6) | |
| No. of graftsc | |||
| ≤3 | 780 (66.9) | 615 (61.8) | .003 |
| ≥4 | 383 (32.8) | 380 (38.2) | |
| Off-pump CABG | 514 (44.2) | 593 (59.6) | <.001 |
| Use of MAG | 671 (58.9) | 601 (61.0) | .35 |
| Use of RA | 303 (26.1) | 248 (24.9) | .56 |
Abbreviations: BMI, body mass index; CABG; coronary artery bypass grafting; COPD, chronic obstructive pulmonary disease; IQR, interquartile range; ITA, internal thoracic artery; LVEF, left ventricular ejection fraction; MAG, multiple arterial grafting; MI, myocardial infarction; NYHA, New York Heart Association; PVD, peripheral vascular disease; RA, radial artery.
Calculated as weight in kilograms divided by height in meters squared.
Racial and ethnic group was self-reported.
For 3 patients, data on number of grafts used were not available.
Primary and secondary outcomes in the main analysis are reported in Table 2. At 10-year follow-up, 226 patients (22.7%) in the skeletonized group and 225 (19.3%) in the pedicled group had died. The rates of the secondary outcomes were also higher in the skeletonized group (MACE, 340 [34.2%] vs 333 [28.6%]; MACE and SWC, 358 [36.0%] vs 361 [31.0%]). On multivariable analysis, the long-term risk of all-cause mortality was not significantly different between the pedicled and skeletonized groups (HR, 1.12; 95% CI, 0.92-1.36; P = .27) (Figure, A). However, the long-term risks of the secondary outcomes were significantly higher in the skeletonized group compared with the pedicled group (MACE: HR, 1.25; 95% CI, 1.06-1.47; P = .01; MACE and SWC: HR, 1.22; 95% CI, 1.05-1.43; P = .01) (Figure, B and C; eTable 2 in Supplement 1).
Table 2. Postoperative Outcomes.
| Outcome | No. (%) | HR (95% CI) | P value | |
|---|---|---|---|---|
| Pedicled ITA (n = 1166) | Skeletonized ITA (n = 995) | |||
| All-cause mortality | 225 (19.3) | 226 (22.7) | 1.12 (0.92-1.36)a | .27 |
| MACE | 333 (28.6) | 340 (34.2) | 1.25 (1.06-1.47)a | .01 |
| MACE and SWC | 361 (31.0) | 358 (36.0) | 1.22 (1.05-1.43)a | .01 |
| MI | 44 (3.8) | 41 (4.1) | 1.12 (0.73-1.72) | .60 |
| RR | 116 (9.9) | 134 (13.5) | 1.42 (1.11-1.82) | .01 |
| SWC | 53 (4.5) | 33 (3.3) | 0.61 (0.40-0.94) | .03 |
Abbreviations: HR, hazard ratio; ITA, internal thoracic artery; MACE, major adverse cardiac events; MI, myocardial infarction; RR, repeated revascularization; SWC, sternal wound complications.
Adjusted for age, female sex, New York Heart Association class of III to IV, diabetes, chronic obstructive pulmonary disease, peripheral vascular disease, prior stroke, prior MI, left ventricular ejection fraction less than 50%, use of bilateral ITA, use of radial artery, and use of off-pump coronary artery bypass grafting.
Figure. Kaplan-Meier Curves of All-Cause Mortality, Major Adverse Cardiac Events (MACE), and MACE and Sternal Wound Complication (SWC) Among the Entire Cohort.
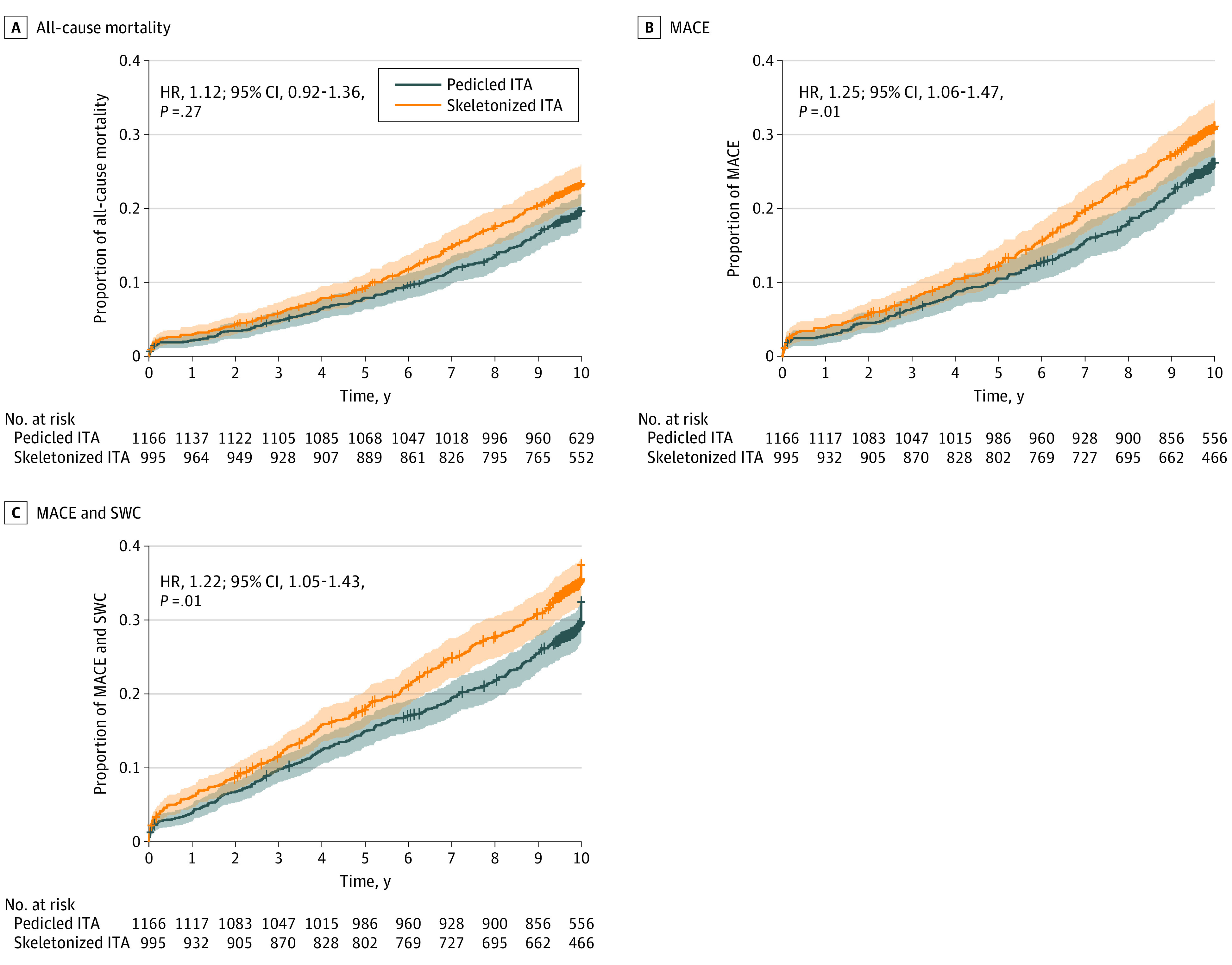
HR indicates hazard ratio; ITA, internal thoracic artery.
In the analysis based on the number of patients that surgeons enrolled in the trial, the long-term risk of all-cause mortality was not significantly different between the pedicled and skeletonized groups for both groups of surgeons (50 or less: HR, 1.28; 95% CI, 0.96-1.72; P = .09; 51 or more: HR, 1.01; 95% CI, 0.73-1.39; P = .95) (Table 3; eTables 3 and 4 in Supplement 1). However, the long-term risks of the secondary outcomes were significantly higher in the skeletonized group compared with the pedicled group for surgeons who enrolled 50 patients or less (MACE: HR, 1.30; 95% CI, 1.03-1.65; P = .03; MACE and SWC: HR, 1.33; 95% CI, 1.06-1.67; P = .01) but not for surgeons who enrolled 51 patients or more (MACE: HR, 1.07; 95% CI, 0.82-1.39; P = .62; MACE and SWC: HR, 1.04; 95% CI, 0.80-1.34; P = .78). When individual surgeon volume (as a continuous variable) was added to the main Cox model, the differences between the 2 ITA harvesting groups became not statistically significant for all the considered outcomes (all-cause mortality: HR, 1.15; 95% CI, 0.92-1.44; P = .21; MACE: HR, 1.18; 95% CI, 0.99-1.42; P = .07; MACE and SWC: HR, 1.18; 95% CI, 0.99-1.40; P = .07).
Table 3. Postoperative Outcomes Stratified by Number of Patients Enrolled in the Trial by Surgeon.
| Outcome | ≤50 Patients | ≥51 Patients | ||
|---|---|---|---|---|
| HR (95% CI)a | P value | HR (95% CI)a | P value | |
| All-cause mortality | 1.28 (0.96-1.72) | .09 | 1.01 (0.73-1.39) | .95 |
| MACE | 1.30 (1.03-1.65) | .03 | 1.07 (0.82-1.39) | .62 |
| MACE and SWC | 1.33 (1.06-1.67) | .01 | 1.04 (0.80-1.34] | .78 |
Abbreviations: HR, hazard ratio; MACE, major adverse cardiac events; SWC, sternal wound complications.
Adjusted for age, female sex, New York Heart Association class of III to IV, diabetes, chronic obstructive pulmonary disease, peripheral vascular disease, prior stroke, prior myocardial infarction, left ventricular ejection fraction less than 50%, use of bilateral ITA, use of radial artery, and use of off-pump coronary artery bypass grafting.
When limiting the analysis to patients with a single ITA to the left anterior descending artery, the long-term risk of all-cause mortality was not significantly different between the pedicled and skeletonized groups (HR, 1.25; 95% CI, 0.93-1.68; P = .14). However, the long-term risks of the secondary outcomes were significantly higher in the skeletonized group compared with the pedicled group (MACE: HR, 1.52; 95% CI, 1.18-1.95; P = .001; MACE and SWC: HR, 1.46; 95% CI, 1.15-1.87; P = .002) (eFigure 1 and eTable 5 in Supplement 1).
When limiting the analysis to the first 2 years of follow-up, the long-term risks of all-cause mortality and the composite of MACE and SWC were not significantly different between the pedicled and skeletonized groups (all-cause mortality: HR, 1.12; 95% CI, 0.90-1.39; P = .31; MACE and SWC: HR, 1.19; 95% CI, 1.00-1.42; P = .05). However, the long-term risk of MACE was significantly higher in the skeletonized group compared with the pedicled group (HR, 1.22; 95% CI, 1.02-1.47; P = .03).
The matched population consisted of 859 pairs for the main comparison and 304 pairs for the single ITA to the left anterior descending artery comparison; good balance was achieved among groups (eFigure 2 and eTable 6 in Supplement 1). The results using PSM were consistent with the results of the main analysis (eFigures 3 and 4 in Supplement 1).
Discussion
In this post hoc analysis of the ART trial, we found that there were no differences in 10-year survival among patients who received skeletonized vs pedicled ITAs. However, the adverse event rates were consistently higher among patients who received skeletonized ITAs, and the difference between groups did reach statistical significance for the composite outcome of adverse cardiac events. The difference was not seen when considering only patients operated on by surgeons who enrolled 51 patients or more in the trial.
Skeletonization of the ITA has been associated with better preservation of sternal perfusion in at least 2 small randomized trials,18,19 and observational studies and meta-analyses have generally reported a reduction in the risk of sternal complications with the skeletonized compared with the pedicled technique.7,20 In an analysis of the Society of Thoracic Surgeons National Database, Schwann et al20 found a lower incidence of SWC among patients who received skeletonized rather than pedicled ITAs, and similar results were reported in a meta-analysis of 8 observational studies7 and in a post hoc analysis of the ART trial (and also in this analysis).21 This is important because sternal wound infection is associated with ITA use20 and is a strong risk factor for early and late mortality after CABG as well as adverse postoperative events and prolonged in-hospital stay.22,23 Skeletonization has also been associated with superior ITA length and higher free flow that can potentially facilitate CABG24 and is currently recommended in expert consensus documents and professional societies guidelines.8,25
On the other hand, ITA skeletonization requires direct surgical manipulation of the artery and may potentially be more traumatic for the vessel wall. However, histologic and functional studies have reported comparable endothelial integrity and function with the 2 techniques.26,27 Also, individual studies and meta-analysis of observational studies have reported similar clinical outcomes and patency rates for skeletonized and pedicled ITAs.24,28
Recently, a post hoc analysis of the COMPASS trial reported significantly higher occlusion rate and MACE at 1 year in patients who received skeletonized vs pedicled ITAs, eliciting a strong debate in the surgical community on the best technique for ITA harvesting.9 Our data cannot settle the skeletonization question but add important information on the topic. We found that there was no statistically significant difference between groups in long-term survival, and this is reassuring in regard to the safety of both techniques. However, the adverse event rate was higher in the skeletonization group and reached statistical significance for the composite outcome of MACE. The consistency of this finding in all the sensitivity and exploratory analyses is concerning and indicates that further evidence is needed.
We found also that the difference between groups was larger (and statistically significant) when considering only patients operated on by surgeons who enrolled 50 patients or less in the trial and that, when accounting for individual surgeon volume in the main analysis, the differences between groups became not statistically significant. This is consistent with the known volume-outcome effect that has been shown by us and others for bilateral ITA CABG.29,30 No information on surgeon experience was reported in the COMPASS report,9 but one could speculate that surgeon comfort with the more delicate skeletonized technique may have been an important confounder even in the COMPASS analysis.
It must be noted that data derived from the study of saphenous vein grafts (the most commonly used CABG conduits) suggest that less traumatic harvesting techniques (no-touch technique, open technique) are generally associated with better patency rates compared with potentially more traumatic techniques (traditional harvesting, endoscopic harvesting)30,31; this may probably also apply to the ITA and be the biologic rationale for the worse results of the skeletonized technique.
Limitations
This study must be viewed in light of its limitations. This was a nonprespecified post hoc analysis, and confounding related to differences in baseline characteristics and power limitations may have affected the reported comparisons. There were statistically significant differences in age, diabetes, and sex between groups, which could contribute to the differences in outcomes independently from the use of a skeletonized or pedicle ITA. Skeletonization was associated with off-pump CABG, which may be an important confounder. We have no data on long-term graft patency. Details of ITA harvesting were available only in 2161 of 3102 patients (69.7%), and as the ART trial was not designed to compare the 2 ITA harvesting techniques, technical details and reporting may have varied substantially among participating centers. Results were not adjusted for multiplicity and must be seen as hypothesis generating. The cutoff used to define surgeon experience is arbitrary, and the number of patients enrolled in the ART trial may or may not correlate with surgeon experience with skeletonization.
Conclusions
In conclusion, in the ART trial, skeletonized ITA harvesting was associated with similar survival but higher rates of adverse cardiovascular events at 10-year follow-up compared with pedicled ITA harvesting; the difference was associated with the number of patients enrolled by individual surgeons in the trial. Further evaluation of the safety and effectiveness of the skeletonized technique, with particular regard to surgeon experience, is necessary.
eMethods. Definitions of the outcomes.
eTable 1. Baseline characteristics of patients with and without information on the internal thoracic artery harvesting technique.
eTable 2. Variables associated with all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among the entire cohort.
eTable 3. Variables associated with all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among patients whose surgery was performed by surgeons who enrolled 50 patients or less in the trial.
eTable 4. Variables associated with all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among patients whose surgery was performed by surgeons who enrolled 51 patients or more in the trial.
eTable 5. Variables associated with all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among the SITA-only cohort.
eTable 6. Baseline characteristics in the matched cohort.
eFigure 1. Kaplan Meier curves of all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among the SITA-only cohort.
eFigure 2. Balance plot for assessment of standardized mean difference before and after propensity score matching among the entire cohort and the SITA-only cohort.
eFigure 3. Kaplan Meier curves of all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among the entire cohort after propensity matching.
eFigure 4. Kaplan Meier curves of all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among the SITA-only cohort after propensity matching.
Nonauthor Collaborators. ART Investigators.
References
- 1.Neumann F-J, Sousa-Uva M, Ahlsson A, et al. ; ESC Scientific Document Group . 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87-165. doi: 10.1093/eurheartj/ehy394 [DOI] [PubMed] [Google Scholar]
- 2.Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124(23):e652-e735. [DOI] [PubMed] [Google Scholar]
- 3.Gaudino M, Bakaeen FG, Benedetto U, et al. ; ATLANTIC (Arterial Grafting International Consortium) Alliance Members . Arterial grafts for coronary bypass: a critical review after the publication of ART and RADIAL. Circulation. 2019;140(15):1273-1284. doi: 10.1161/CIRCULATIONAHA.119.041096 [DOI] [PubMed] [Google Scholar]
- 4.Keeley SB. The skeletonized internal mammary artery. Ann Thorac Surg. 1987;44(3):324-325. doi: 10.1016/S0003-4975(10)62088-7 [DOI] [PubMed] [Google Scholar]
- 5.Cunningham JM, Gharavi MA, Fardin R, Meek RA. Considerations in the skeletonization technique of internal thoracic artery dissection. Ann Thorac Surg. 1992;54(5):947-950. doi: 10.1016/0003-4975(92)90656-O [DOI] [PubMed] [Google Scholar]
- 6.Iddawela S, Mellor SL, Zahra SA, Khare Y, Harky A. Pedicled or skeletonized bilateral internal mammary artery harvesting—a meta- analysis and trial sequential analysis. Expert Rev Cardiovasc Ther. 2021;19(7):647-654. doi: 10.1080/14779072.2021.1939684 [DOI] [PubMed] [Google Scholar]
- 7.Sá MPBO, Cavalcanti PEF, de Andrade Costa Santos HJ, et al. Skeletonized versus pedicled bilateral internal mammary artery grafting: outcomes and concerns analyzed through a meta-analytical approach. Int J Surg. 2015;16(pt B):146-152. [DOI] [PubMed] [Google Scholar]
- 8.Aldea GS, Bakaeen FG, Pal J, et al. ; Society of Thoracic Surgeons . The Society of Thoracic Surgeons clinical practice guidelines on arterial conduits for coronary artery bypass grafting. Ann Thorac Surg. 2016;101(2):801-809. doi: 10.1016/j.athoracsur.2015.09.100 [DOI] [PubMed] [Google Scholar]
- 9.Lamy A, Browne A, Sheth T, et al. ; COMPASS Investigators . Skeletonized vs pedicled internal mammary artery graft harvesting in coronary artery bypass surgery: a post hoc analysis from the COMPASS trial. JAMA Cardiol. Published online Jun 16, 2021. doi: 10.1001/jamacardio.2021.1686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taggart DP, Benedetto U, Gerry S, et al. ; Arterial Revascularization Trial Investigators . Bilateral versus single internal-thoracic-artery grafts at 10 years. N Engl J Med. 2019;380(5):437-446. doi: 10.1056/NEJMoa1808783 [DOI] [PubMed] [Google Scholar]
- 11.Taggart DP, Lees B, Gray A, Altman DG, Flather M, Channon K; ART Investigators . Protocol for the Arterial Revascularisation Trial (ART). a randomised trial to compare survival following bilateral versus single internal mammary grafting in coronary revascularisation [ISRCTN46552265]. Trials. 2006;7:7. doi: 10.1186/1745-6215-7-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taggart DP, Altman DG, Gray AM, et al. ; ART Investigators . Randomized trial to compare bilateral vs. single internal mammary coronary artery bypass grafting: 1-year results of the Arterial Revascularisation Trial (ART). Eur Heart J. 2010;31(20):2470-2481. doi: 10.1093/eurheartj/ehq318 [DOI] [PubMed] [Google Scholar]
- 13.Taggart DP, Altman DG, Gray AM, et al. ; ART Investigators . Randomized trial of bilateral versus single internal-thoracic-artery grafts. N Engl J Med. 2016;375(26):2540-2549. doi: 10.1056/NEJMoa1610021 [DOI] [PubMed] [Google Scholar]
- 14.Gaudino M, Bakaeen F, Benedetto U, et al. Use rate and outcome in bilateral internal thoracic artery grafting: insights from a systematic review and meta-analysis. J Am Heart Assoc. 2018;7(11):e009361. doi: 10.1161/JAHA.118.009361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gaudino M, Kappetein AP, Di Franco A, et al. Randomized trials in cardiac surgery: JACC Review Topic of the Week. J Am Coll Cardiol. 2020;75(13):1593-1604. doi: 10.1016/j.jacc.2020.01.048 [DOI] [PubMed] [Google Scholar]
- 16.Gaudino M, Di Franco A, Bhatt DL, et al. The association between coronary graft patency and clinical status in patients with coronary artery disease. Eur Heart J. 2021;42(14):1433-1441. doi: 10.1093/eurheartj/ehab096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gaudino M, Antoniades C, Benedetto U, et al. ; ATLANTIC (Arterial Grafting International Consortium) Alliance . Mechanisms, consequences, and prevention of coronary graft failure. Circulation. 2017;136(18):1749-1764. doi: 10.1161/CIRCULATIONAHA.117.027597 [DOI] [PubMed] [Google Scholar]
- 18.Boodhwani M, Lam BK, Nathan HJ, et al. Skeletonized internal thoracic artery harvest reduces pain and dysesthesia and improves sternal perfusion after coronary artery bypass surgery: a randomized, double-blind, within-patient comparison. Circulation. 2006;114(8):766-773. doi: 10.1161/CIRCULATIONAHA.106.615427 [DOI] [PubMed] [Google Scholar]
- 19.Kamiya H, Akhyari P, Martens A, Karck M, Haverich A, Lichtenberg A. Sternal microcirculation after skeletonized versus pedicled harvesting of the internal thoracic artery: a randomized study. J Thorac Cardiovasc Surg. 2008;135(1):32-37. doi: 10.1016/j.jtcvs.2007.09.004 [DOI] [PubMed] [Google Scholar]
- 20.Schwann TA, Gaudino MFL, Engelman DT, et al. Effect of skeletonization of bilateral internal thoracic arteries on deep sternal wound infections. Ann Thorac Surg. 2021;111(2):600-606. doi: 10.1016/j.athoracsur.2020.05.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Benedetto U, Altman DG, Gerry S, et al. ; Arterial Revascularization Trial investigators . Pedicled and skeletonized single and bilateral internal thoracic artery grafts and the incidence of sternal wound complications: insights from the Arterial Revascularization Trial. J Thorac Cardiovasc Surg. 2016;152(1):270-276. doi: 10.1016/j.jtcvs.2016.03.056 [DOI] [PubMed] [Google Scholar]
- 22.Kaspersen AE, Nielsen SJ, Orrason AW, et al. Short- and long-term mortality after deep sternal wound infection following cardiac surgery: experiences from SWEDEHEART. Eur J Cardiothorac Surg. 2021;60(2):233-241. doi: 10.1093/ejcts/ezab080 [DOI] [PubMed] [Google Scholar]
- 23.Sears ED, Wu L, Waljee JF, Momoh AO, Zhong L, Chung KC. The impact of deep sternal wound infection on mortality and resource utilization: a population-based study. World J Surg. 2016;40(11):2673-2680. doi: 10.1007/s00268-016-3598-7 [DOI] [PubMed] [Google Scholar]
- 24.Kusu-Orkar T-E, Kermali M, Masharani K, et al. Skeletonized or pedicled harvesting of left internal mammary artery: a systematic review and meta-analysis. Semin Thorac Cardiovasc Surg. 2021;33(1):10-18. doi: 10.1053/j.semtcvs.2020.09.010 [DOI] [PubMed] [Google Scholar]
- 25.Gaudino MFL, Sandner S, Bonalumi G, Lawton JS, Fremes SE; Coronary Task Force of the European Association for Cardio-Thoracic Surgery . How to build a multi-arterial coronary artery bypass programme: a stepwise approach. Eur J Cardiothorac Surg. 2020;58(6):1111-1117. doi: 10.1093/ejcts/ezaa377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gaudino M, Toesca A, Nori SL, Glieca F, Possati G. Effect of skeletonization of the internal thoracic artery on vessel wall integrity. Ann Thorac Surg. 1999;68(5):1623-1627. doi: 10.1016/S0003-4975(99)00664-5 [DOI] [PubMed] [Google Scholar]
- 27.Gaudino M, Trani C, Glieca F, et al. Early vasoreactive profile of skeletonized versus pedicled internal thoracic artery grafts. J Thorac Cardiovasc Surg. 2003;125(3):638-641. doi: 10.1067/mtc.2003.106 [DOI] [PubMed] [Google Scholar]
- 28.Sá MPB de O, Ferraz PE, Escobar RR, et al. Patency of skeletonized versus pedicled internal thoracic artery in coronary bypass graft surgery: a systematic review, meta-analysis and meta-regression. Int J Surg. 2014;12(7):666-672. doi: 10.1016/j.ijsu.2014.05.071 [DOI] [PubMed] [Google Scholar]
- 29.Schwann TA, Habib RH, Wallace A, et al. Operative outcomes of multiple-arterial versus single-arterial coronary bypass grafting. Ann Thorac Surg. 2018;105(4):1109-1119. doi: 10.1016/j.athoracsur.2017.10.058 [DOI] [PubMed] [Google Scholar]
- 30.Gaudino M, Hameed I, Robinson NB, et al. Angiographic patency of coronary artery bypass conduits: a network meta-analysis of randomized trials. J Am Heart Assoc. 2021;10(6):e019206. doi: 10.1161/JAHA.120.019206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li G, Zhang Y, Wu Z, Liu Z, Zheng J. Mid-term and long-term outcomes of endoscopic versus open vein harvesting for coronary artery bypass: a systematic review and meta-analysis. Int J Surg. 2019;72:167-173. doi: 10.1016/j.ijsu.2019.11.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Definitions of the outcomes.
eTable 1. Baseline characteristics of patients with and without information on the internal thoracic artery harvesting technique.
eTable 2. Variables associated with all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among the entire cohort.
eTable 3. Variables associated with all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among patients whose surgery was performed by surgeons who enrolled 50 patients or less in the trial.
eTable 4. Variables associated with all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among patients whose surgery was performed by surgeons who enrolled 51 patients or more in the trial.
eTable 5. Variables associated with all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among the SITA-only cohort.
eTable 6. Baseline characteristics in the matched cohort.
eFigure 1. Kaplan Meier curves of all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among the SITA-only cohort.
eFigure 2. Balance plot for assessment of standardized mean difference before and after propensity score matching among the entire cohort and the SITA-only cohort.
eFigure 3. Kaplan Meier curves of all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among the entire cohort after propensity matching.
eFigure 4. Kaplan Meier curves of all-cause mortality, major adverse cardiac events, and major adverse cardiac events and sternal wound complication among the SITA-only cohort after propensity matching.
Nonauthor Collaborators. ART Investigators.


