Abstract
Background
Vaccine hesitancy has affected COVID-19 adult vaccination programs in many countries. Data on hesitancy amongst child and adolescent populations is largely confined to parent opinion. We investigated the characteristics of vaccine hesitant children and adolescents using results from a large, school-based self-report survey of the willingness to have a COVID-19 vaccination in students aged 9 –18 years in England.
Methods
Data from the OxWell Student Survey on mental health, life experiences and behaviours were used, collected from four counties across England. Local authority partners recruited schools. The vaccine hesitancy question gave six response options and were clustered to inform delivery: eager and willing were categorised as vaccination ‘opt-in’, don't know and not bothered categorised as ‘undecided’, and unwilling and anti-vaccination categorised as ‘opt-out’. We conducted a multinomial regression to determine associations between vaccine hesitancy and sociodemographic, health behaviour and social connection variables.
Findings
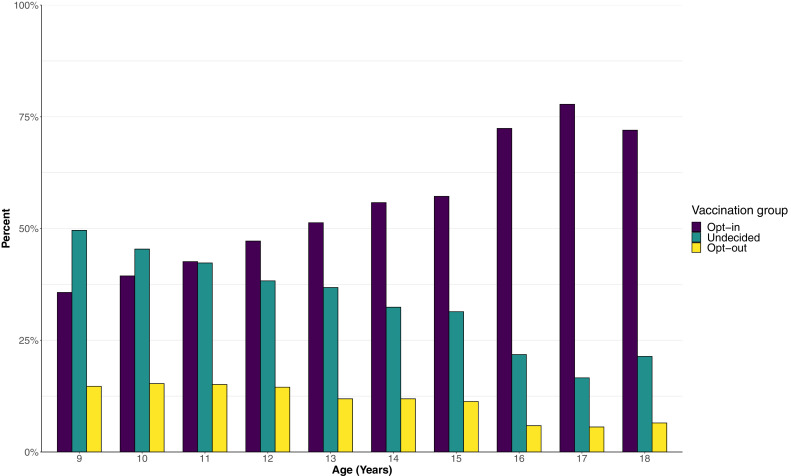
27,910 students from 180 schools answered the vaccine hesitancy question between 14th May and 21st July 2021, of whom 13984 (50.1%) would opt-in to take a vaccination, 10322 (37.0%) were undecided, and 3604 (12.9%) would opt-out. A lower percentage of younger students reported that they would opt-in to vaccination, for example, 35.7% of 9-year-olds and 51.3% of 13-year-olds compared to 77.8% of 17-year-olds would opt-in to take a vaccination. Students who were ‘opt-out’ or ‘undecided’ (a combined ‘vaccine hesitant’ group) were more likely to come from deprived socioeconomic contexts with higher rates of home rental versus home ownership and their school locations were more likely to be in areas of greater deprivation. They were more likely to smoke or vape, spend longer on social media, feel that they did not belong in their school community but had lower levels of anxiety and depression. The vaccine hesitant students- the undecided and opt-out groups- were similar in profile, although the opt-out students had higher reported confirmed or probable previous COVID-19 infection than the opt-in group, whereas those undecided, did not.
Interpretation
If government vaccination strategies move towards vaccinating younger school-aged students, efforts to increase vaccination uptake may be necessary. Compared with students who would opt-in, those who were vaccine hesitant had greater indicators of social deprivation and felt a lack of community cohesion by not feeling a sense of belonging at their school. There were indications that those students who would opt-out had higher levels of marginalisation and mistrust. If programmes are rolled out, focus on hesitant younger students will be important, targeting more marginalised and deprived young people with information from trusted sources utilising social media; improving access to vaccination centres with provision both in and outside school; and addressing fears and worries about the effects of the vaccine. The main limitation of this study is that the participant group may not be wholly representative of England or the UK, which may bias population-level estimates of willingness to be vaccinated.
Funding
The Westminster Foundation, the National Institute for Health Research (NIHR) Applied Research Collaboration Oxford and Thames Valley at Oxford Health NHS Foundation Trust and the NIHR Oxford Health Biomedical Research Centre.
Keywords: COVID19, Vaccination, Vaccine hesitancy, Child and adolescent, School, Mental health, Public health
Research in context.
Evidence before this study
We conducted a search on Ovid EMBASE and Scopus on young peoples’ opinions of COVID-19 vaccination, using a combination of terms related to: COVID-19; vaccinations; children and adolescents; and hesitancy. Very few studies report on populations under the age of 18 years with more reporting on parental intentions. The findings highlight how attitudes towards the COVID-19 vaccination in adolescent populations as well as parents follow many similar patterns to those in studies of adult populations. A UK household survey of 920 16-24 year-olds reported a vaccine hesitancy rate of 27% which was higher than for their adult counterparts. For the six studies reporting on over 7500 parents questioned on intentions to vaccinate their children, 45%–62% reported that they would vaccinate their children.
Added value of this study
To our knowledge, this is the largest study to date examining attitudes to COVID-19 vaccination in children and adolescents with 27,910 students from four counties in England, aged nine to 18 years. This study identifies the importance of focusing on the younger age range with regards to hesitancy and that negative perceptions of school inclusion and trust are associated with hesitancy. The school role can be seen as crucial, not only as an established location that has a record of successful vaccination delivery in a number of high- and low-income nations, but also where potential interventions can be targeted to enhance social cohesion.
Implications of all the available evidence
COVID-19 vaccination has so far been shown to reduce transmission somewhat and limit the severity of COVID-19 disease. The unvaccinated populations, especially subpopulations at higher risk as a result of comorbidities, are becoming an important focus of public health campaigns. This study highlights that - if the decision is taken by countries to vaccinate younger populations - there is a majority of older school-aged students that are willing to be vaccinated but there is substantial variation with age that may affect acceptance rates. Those who are vaccine hesitant show markers of social deprivation, mistrust, and less social cohesion, and increasing rates of vaccine uptake might benefit from focusing on the concerns of this group and information presented in the media most accessed by the age group being targeted.
Alt-text: Unlabelled box
1. Introduction
As many countries enter a new stage of management in the shifting sands of the COVID-19- pandemic, the emphasis of the spread of the disease and its prevention is moving to the younger generations. This emphasis reflects the downshift in average age of those becoming infected with the virus, with it being described as becoming a ‘disease of the young’ [1]. The role of vaccination for adolescents is now taking centre stage in many higher resource countries, particularly as older and more vulnerable populations have been vaccinated and severe illness is largely a vaccine-preventable outcome. A number of countries have in the first half of 2021 started to offer the vaccination to their adolescent populations, most notably Israel, the USA and recently the UK, where those over the age of 16, and younger adolescents with certain co-morbidities, have been offered the vaccine [[2], [3], [4]].
Vaccinations for adolescent populations for most infectious diseases have been offered relatively late in many of the global vaccination drives but now are of increasing prominence. Adolescence marks an important time when either primary vaccinations can be given, such as in the introduction more than a decade ago of the human papillomavirus (HPV) vaccine to prevent future cancer; or as a key time to booster immunity for many infectious diseases such as diphtheria, polio and tetanus (DpT), meningococcus and in some parts of the globe- hepatitis B [5–7].
School-based delivery of these vaccination programmes have made a substantial contribution [8], especially as adolescent populations in general have low rates of visits to primary care [6]. For example, with the HPV roll-out, the UK statistics of pre-pandemic uptake for both doses was between 82 and 87% [9], likely to be significantly higher than if delivered in other locations [10]. Most school-based programmes rely on the consent of a competent child and/or the consent of one parent, and providers will usually be reluctant to immunise if either party refuses [11].
The risks of COVID-19 in children and adolescents include a low risk of multisystemic inflammatory syndrome (MIS-C) [12] and long COVID [13,14] as well as educational disruptions. Adolescent COVID-19 vaccination data highlight the relative safety of the COVID-19 vaccines so far administered [15]. There have been reports of side effects after vaccination, especially common are pain at the injection site and some mild flu-like symptoms. There have been reports of rare cases of myocarditis and pericarditis in adolescents, mostly males, mainly following the second vaccination dose [16]. Early vaccine data from Israel, for example, have demonstrated the relative safety and efficacy of the vaccination since those over the age of 16 have been vaccinated. For example, from January to May 2021 no severe morbidity was identified in vaccinated adolescents (12-15 years), whilst there were 15 un-vaccinated adolescents hospitalised following COVID-19 infection, in the same period [17].
The patterns of vaccine hesitancy are constantly changing, even within nations, influenced by reports of vaccine safety, the variant of coronavirus that might be circulating, and current rates of infection. Understandably, studies of COVID-19 vaccine hesitancy have focussed on adults, with very few reports on children and adolescents. The aim of this study was to estimate the prevalence of vaccine hesitancy across the age range of UK school children. A secondary aim was to examine the hypotheses that previous COVID-19 infection, socioeconomic position, mental health, social connectedness and healthy behaviours were associated with vaccine hesitancy amongst children and adolescents (for this study adolescents were aged 12-18 years).
2. Methods
2.1. Design
This study uses data from the 2021 OxWell Student Survey, an annual cross‐sectional survey of schools and further education colleges (FECs) in England. The OxWell survey has three age-appropriate versions (divided into English school years 5 to 7, 8 to 11, and 12 and 13 covering ages 9 to 18 years old) and asks students a range of questions on mental health and wellbeing, life experiences and behaviours. Here we report on all year groups tested on willingness to have the vaccination, but use only the surveys sent to those aged 12 years and above (school years 8 to 13 to) in our regression models as the surveys for the adolescent population were more detailed (for example including questions on paranoia) which allowed us to include more conceptually relevant predictors of vaccine hesitancy. The study was approved by the University of Oxford Research Ethics Committee (Ref: R62366).
2.2. Participants and recruitment
All students aged approximately 9 years and older (school years 5 and above) attending mainstream state-maintained and independent primary schools (school years 5-6), secondary schools (school years 7-13), and further education colleges (FEC) (school years 12 and 13) in ten local authority areas in four English counties (Berkshire, Buckinghamshire, Merseyside and Oxfordshire) were eligible to participate. Between May and July 2021, local authorities invited schools in their catchment area to participate, following parental opt-out and adolescent assent and consenting procedures as described in previous studies [18]. Most students completed the survey as part of in-school activities and all questions within the survey were optional so that students could proceed to the next part of the survey if they did not want to answer a particular question, without needing to give a reason.
2.3. Measures and outcomes
2.3.1. Vaccine hesitancy
For the 2021 OxWell survey, students answered a single question from the Oxford COVID-19 Vaccine Hesitancy Scale[19]: “Would you take a COVID-19 vaccine (approved for use in the UK) if offered?”. All students had the following six response options with 'I would describe myself as':
-
-
Eager to get a COVID-19 vaccine
-
-
Willing to get a COVID-19 vaccine
-
-
Not bothered about getting a COVID-19 vaccine
-
-
Unwilling to get a COVID-19 vaccine
-
-
Anti-vaccination for COVID- 19
-
-
Don't know
A ‘Don't know what this means’ response option was available for the youngest students, aged 9 to 12 years (school years 5 to 7) which for the purpose of this analysis we coded as part of the ‘don't know’ category.
We conceptualised and therefore categorised responses to the question on vaccine hesitancy according to how delivery of the vaccination might be informed. We considered ‘eager’ and ‘willing’ responses to be those who would opt-in to taking a vaccination, those who were ‘not bothered’ and ‘don't know’ as being undecided, and those who responded ‘unwilling’ and ‘anti-vaccination’ as those who would opt-out. We defined vaccine hesitancy as those who would opt-out or were undecided.
We hypothesized that the variables described below would be associated with vaccine hesitancy.
2.3.2. Sociodemographic characteristics
Full details of the survey measures used in the study are provided in Supplementary Methods 1. Students were asked their age in years and gender (categorised as male, female, and other/prefer not to answer), and whether both their parents were born in the UK (answered yes, no, or would rather not answer). Students were asked about parental home ownership as a proxy for deprivation. School postcode was used as a proxy for calculating neighbourhood-level Index of Multiple Deprivation. This uses data from the National Census and combines seven domains (including income, employment and health deprivation) to give an overall deprivation score for 32,844 distinct geographical areas in England, divided into quintiles [20].
2.3.3. Previous COVID-19 infection
Students were asked whether they thought that they had previously contracted COVID-19, with responses: “Yes (confirmed by test)”; "probably"; “possibly"; “no”.
2.3.4. Health behaviours
We included three health behaviours as a proxy for healthiness of behaviours. These were whether students exercised for more or less than one hour a week (in term time, both in and out of school); if they smoked cigarettes and/or e-cigarettes/vaped (never/not often versus sometimes/quite often/most days); and time they spent on social media (as reported below in the ‘Social connection’ section).
2.3.5. Social connection
We included four questions as proxies for a students’ sense of social connection and social safety, namely: if they spent more or less than four hours daily on social media; whether they felt a sense of school belonging; how often they felt lonely; and if they had been bullied and how often.
2.3.6. Mental health
Measurement of depression and anxiety was from the 25‐item Revised Children's Anxiety and Depression Scales (RCADS) [21]. We measured paranoid thoughts using the 18-item Bird Checklist of Adolescent Paranoia (B-CAP) [22].
2.4. Analysis
We describe attitudes to taking the COVID-19 vaccine using plots and absolute and relative frequencies by age group. A multinomial regression model was used to assess the relationship between our predictor variables and vaccine hesitancy only in adolescent respondents – aged 12-18 years (school years 8–13). We report our results from the multinomial model as odds ratios and report them alongside 95% confidence intervals and p-values. All analyses were conducted using R version 4.05. We considered missing responses to the question on vaccine hesitancy as missing at random (details of our decision making described in Supplementary Methods 2) and excluded these students from our analysis. We imputed other missing data using multiple imputation via chained equations [23]. We imputed missing continuous data using predictive mean matching, categorical data using polytomous regression, and binary data using logistic regression. We produced 500 imputations and pooled our estimates across imputations according to Rubin's rules [24]. We conducted two sensitivity analyses; one using only complete cases and a second using only those who self-reported that they did not think they had had a COVID-19 infection and compared both results with our full imputed datasets.
2.5. Role of the funding source
The funding source had no role in the study design, collection, analysis and interpretation of the data, writing of the report and in the decision to submit the paper for publication.
3. Results
A total of 33,556 students from 117 primary schools, 62 secondary schools, and 1 further education college accessed the survey (Supplementary Figure 1). Of those, the survey administrators removed 2283 survey responses due to students spending less than 5 minutes on a survey (considered as survey non-starters) or survey response times falling in non-consistent extremes (all surveys were conducted during term time, mostly within the school day, a minority were set as homework). Of the 31,273 remaining responses, we included all students who responded to the question on willingness to take the vaccination (n = 27,910), leaving 12,811 aged approximately 9-12 years (school years 5–7); 13,481 aged 12-16 years (in school years 8-11) and 1,618 aged 16-18 years (in school years 12 and 13). Our participant group characteristics are described in Table 1.
Table 1.
Sample characteristics for students who answered the question “Would you take a COVID-19 vaccine (approved for use in the UK) if offered? “ (n = 27, 910).
| Characteristic | N | n (%); Median (IQR) |
|---|---|---|
| Gender | 27,859 | |
| Male | 11,900 (43%) | |
| Female | 14,566 (52%) | |
| Other/Prefer not to answer | 1,393 (5.0%) | |
| Age, years | 27,685 | 13.00 (11.00, 14.00) |
| Born in the UK | 27,812 | |
| Both parents born in UK | 15,997 (58%) | |
| Neither parent born in UK | 10,802 (39%) | |
| Would rather not say | 1,013 (3.6%) | |
| Deprivation quintile1 | 26,923 | |
| 1 | 7,875 (29%) | |
| 2 | 4,662 (17%) | |
| 3 | 2,834 (11%) | |
| 4 | 2,981 (11%) | |
| 5 | 8,571 (32%) | |
| Housing Status | 27,842 | |
| Home is rented | 5,708 (21%) | |
| Home is owned | 16,441 (59%) | |
| Don't know | 5,693 (20%) | |
| Covid Status | 27,457 | |
| Yes had COVID (confirmed by test) | 1,871 (6.8%) | |
| Probably had COVID | 2,307 (8.4%) | |
| Possibly had COVID | 5,604 (20%) | |
| No not had COVID | 17,675 (64%) | |
| Willingness to be vaccinated | 27,910 | |
| Opt-in | 13,984 (50%) | |
| Undecided | 10,322 (37%) | |
| Opt-out | 3,604 (13%) |
Quintile 1 is most deprived – quintile 5 least deprived
To make an estimate of the response rate, we compared the number of Liverpool students that responded to the survey to the actual headcount per school year group in Liverpool primary and secondary schools. Of the total possible 112 primary schools, 63 (56.3%) participated. In these schools, 4038 of a total of 5289 students were recruited to the survey (76.3%). Of the 31 secondary schools in Liverpool, 20 (64.5%) schools participated. In these schools, 7639 of a possible 14812 students responded to the survey (51.6%). Response rates per class varied across year groups in the analysis sample, from 76.9% in year 5, 86.6% in year 6, 58.3% in year 7, 60.5% in year 8, 64.5% in year 9, 48.1% in year 10, 3.7% in year 11 and 25.7% for combined years 12 and 13, as only this was available.
Of the students who responded to the question on whether they would take a COVID-19 vaccination, 13984 (50.1%) would opt-in to take a vaccination, of the vaccine hesitant group, 10322 (37.0%) were undecided, and 3604 (12.9%) would opt-out. Responses differed by age, with a larger percentage in the younger age groups being undecided or opting-out of a COVID-19 vaccination (Fig. 1). In comparison with those opting-in to a COVID-19 vaccination, each added year in age was associated with a decrease in the odds of students describing themselves as undecided (OR = 0.80, 95%CI: 0.78-0.83, p < 0.001) or opting-out (OR=0.80, 95%CI: 0.77-0.84, p < 0.001). Table 2 describes responses by sociodemographic variables, previous COVID-19 infection, health behaviours, social connectedness and mental health measures (Supplementary Fig. 2 and Supplementary Table 1 describe these results according to the full six option response to the vaccine hesitancy question).
Fig. 1.
Percentages of students by age in response to question: “Would you take a COVID-19 vaccine (approved for use in the UK) if offered?” (n = 27910).
Table 2.
Sample characteristics by response to the question: Would you take a COVID-19 vaccine (approved for use in the UK) if offered?.
| Characteristic | Opt-in, N = 13,9841 | Undecided, N = 10,3221 | Opt-out, N = 3,6041 |
|---|---|---|---|
| Age group | |||
| Age 9 - 11 | 3,499 (41%) | 3,817 (44%) | 1,307 (15%) |
| Age 12 - 16 | 9,003 (52%) | 6,056 (35%) | 2,164 (13%) |
| Age 16 and over | 1,396 (76%) | 338 (18%) | 105 (5.7%) |
| (Missing) | 86 | 111 | 28 |
| Deprivation quintile2 | |||
| 1 | 3,467 (44%) | 3,143 (40%) | 1,265 (16%) |
| 2 | 1,924 (41%) | 1,968 (42%) | 770 (17%) |
| 3 | 1,365 (48%) | 1,110 (39%) | 359 (13%) |
| 4 | 1,578 (53%) | 1,085 (36%) | 318 (11%) |
| 5 | 5,165 (60%) | 2,629 (31%) | 777 (9.1%) |
| (Missing) | 485 | 387 | 115 |
| Gender | |||
| Male | 5,883 (49%) | 4,592 (39%) | 1,425 (12%) |
| Female | 7,349 (50%) | 5,212 (36%) | 2,005 (14%) |
| Other/Prefer not to answer | 734 (53%) | 493 (35%) | 166 (12%) |
| (Missing) | 18 | 25 | 8 |
| Born in the UK | |||
| Both parents born in UK | 8,306 (52%) | 5,602 (35%) | 2,089 (13%) |
| Neither parent born in UK | 5,305 (49%) | 4,163 (39%) | 1,334 (12%) |
| Would rather not say | 334 (33%) | 511 (50%) | 168 (17%) |
| (Missing) | 39 | 46 | 13 |
| Housing Status | |||
| Home is rented | 2,467 (43%) | 2,283 (40%) | 958 (17%) |
| Home is owned | 9,494 (58%) | 5,227 (32%) | 1,720 (10%) |
| Don't know | 1,994 (35%) | 2,783 (49%) | 916 (16%) |
| (Missing) | 29 | 29 | 10 |
| Covid Status | |||
| Yes had COVID (confirmed by test) | 905 (48%) | 675 (36%) | 291 (16%) |
| Probably had COVID | 1,140 (49%) | 774 (34%) | 393 (17%) |
| Possibly had COVID | 2,914 (52%) | 1,977 (35%) | 713 (13%) |
| No not had COVID | 8,835 (50%) | 6,699 (38%) | 2,141 (12%) |
| (Missing) | 190 | 197 | 66 |
| Characteristic (School years 8 and above) | Opt-in, N = 85373 | Undecided, N = 48743 | Opt-out, N = 16883 |
|---|---|---|---|
| Exercise Frequency3 | |||
| 1 hour or less | 767 (48%) | 633 (39%) | 210 (13%) |
| more than 1 hour | 7,328 (58%) | 3,960 (31%) | 1,395 (11%) |
| (Missing) | 442 | 281 | 83 |
| Smoking status ( tobacco or e-cigarettes)3 | |||
| Never or rarely | 7,015 (59%) | 3,648 (31%) | 1,246 (10%) |
| Sometimes or often | 334 (47%) | 266 (37%) | 116 (16%) |
| (Missing) | 1,188 | 960 | 326 |
| Time spent on social media3 | |||
| less than 4 hours | 5,067 (63%) | 2,269 (28%) | 735 (9.1%) |
| 4 hours or more | 2,342 (50%) | 1,718 (37%) | 635 (14%) |
| (Missing) | 1,128 | 887 | 318 |
| Identifies with school community3 | |||
| Fully agree | 390 (64%) | 151 (25%) | 69 (11%) |
| Agree | 1,698 (66%) | 677 (26%) | 216 (8.3%) |
| Somewhat agree | 1,580 (62%) | 719 (28%) | 268 (10%) |
| Neither agree nor disagree | 2,477 (54%) | 1,666 (36%) | 476 (10%) |
| Somewhat disagree | 737 (58%) | 399 (31%) | 144 (11%) |
| Disagree | 592 (54%) | 346 (31%) | 163 (15%) |
| Fully disagree | 464 (48%) | 340 (36%) | 153 (16%) |
| (Missing) | 599 | 576 | 199 |
| Frequency of bullying3 | |||
| Not bullied | 7,979 (57%) | 4,451 (32%) | 1,519 (11%) |
| Bullied | 485 (50%) | 341 (35%) | 150 (15%) |
| (Missing) | 73 | 82 | 19 |
| Feeling lonely3 | |||
| Not lonely | 6,901 (57%) | 3,915 (32%) | 1,367 (11%) |
| Lonely | 1,528 (57%) | 865 (32%) | 297 (11%) |
| (Missing) | 108 | 94 | 24 |
| RCADS score3,4 | 51 (41, 65) | 50 (40, 64) | 51 (40, 64) |
| (Missing) | 916 | 660 | 238 |
| Paranoia score3,5 | 5 (1, 14) | 5 (0, 15) | 6 (1, 18) |
| (Missing) | 2,191 | 1,637 | 573 |
n (%); Median (IQR)
Based on English Indices of Deprivation quintile derived from school postcode, where 5 is least deprived
Only included in survey for school years 8 and above (age 12 and above)
RCADS = Revised Children's Anxiety and Depression Scale, total score higher scores are more severe
B-CAP = The Bird Checklist of Adolescent Paranoia
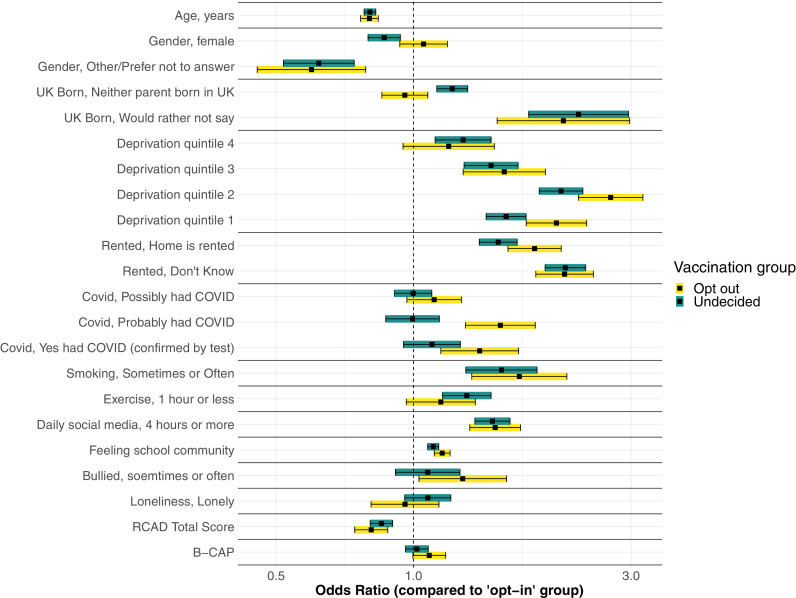
Full results from the multinomial regression model, adjusted for multiple covariates, are presented in Table 3 and Fig. 2. For sociodemographic variables, in comparison with those opting-in to a COVID-19 vaccination, students with neither parent born in the UK (in comparison with both parents born in the UK) had increased odds of describing themselves as being undecided (OR=1.22, 95%CI: 1.12-1.32, p < 0.001) but not opting-out (OR=0.96, 95%CI: 0.85-1.08, p = 0.461). In comparison with those in the highest deprivation quantile (i.e. those least deprived), those in quintile 4 (OR=1.28, 95%CI: 1.12-1.48, p < 0.001), quintile 3 (OR=1.48, 95%CI: 1.29-1.70, p < 0.001), quintile 2 (OR=2.11, 95%CI: 1.89-2.35, p < 0.001), and quintile 1 (OR=1.60, 95%CI: 1.45-1.77, p < 0.001) all had higher odds of describing themselves as undecided about a vaccination in comparison with opting-in to a vaccination. For those opting-out, students in quintile 4 schools were not significantly different from those opting-in (OR=1.19, 95%CI: 0.95-1.50, p = 0.130), but were for the other quintiles: quintile 3 (OR=1.58, 95%CI: 1.28-1.95, p < 0.001), quintile 2 (OR=2.71, 95%CI: 2.30-3.18, p < 0.001), and quintile 1 (OR=2.06, 95%CI: 1.77-2.40, p < 0.001).
Table 3.
Multinomial regression of predictors of response to the question “Would you take a COVID-19 vaccine (approved for use in the UK) if offered?” in students in years 8–13, with the reference group as those who described themselves as opting-in to getting a vaccine (n = 150991).
| Undecided (N = 1688) |
Opt-out (N = 4874) |
||||||
|---|---|---|---|---|---|---|---|
| Variablereference category | Category | OR | 95%CI | p-value5 | OR | 95%CI | p-value5 |
| Age, years | 0.80 | 0.78-0.83 | <0.001 | 0.80 | 0.77-0.84 | <0.001 | |
| Gender, male | Female | 0.86 | 0.8-0.94 | <0.001 | 1.05 | 0.93-1.19 | 0.405 |
| Other/Prefer not to answer | 0.62 | 0.52-0.74 | 0<.001 | 0.60 | 0.45-0.79 | <0.001 | |
| UK Born,both parents born in the UK | Neither parent born in UK | 1.22 | 1.12-1.32 | <0.001 | 0.96 | 0.85-1.08 | 0.461 |
| Would rather not say | 2.30 | 1.79-2.96 | <0.001 | 2.13 | 1.53-2.98 | <0.001 | |
| Deprivation quintile, 5th quantile (least deprived) | Quintile 4 | 1.28 | 1.12-1.48 | 0.001 | 1.19 | 0.95-1.5 | 0.130 |
| Quintile 3 | 1.48 | 1.29-1.7 | <0.001 | 1.58 | 1.28-1.95 | <0.001 | |
| Quintile 2 | 2.11 | 1.89-2.35 | <0.001 | 2.71 | 2.3-3.18 | <0.001 | |
| Quintile 1 | 1.60 | 1.44-1.77 | <0.001 | 2.06 | 1.77-2.4 | <0.001 | |
| Accommodation, parents’ home is owned | Don't know | 2.15 | 1.94-2.39 | <0.001 | 2.14 | 1.85-2.48 | <0.001 |
| Home is rented | 1.53 | 1.39-1.69 | <0.001 | 1.84 | 1.61-2.11 | <0.001 | |
| Covid status,No not had Covid | Possibly had COVID | 1.00 | 0.91-1.1 | 0.977 | 1.11 | 0.97-1.27 | 0.137 |
| Probably had COVID | 1.00 | 0.87-1.14 | 0.947 | 1.55 | 1.3-1.85 | <0.001 | |
| Yes had COVID (confirmed by test) | 1.10 | 0.95-1.27 | 0.202 | 1.40 | 1.15-1.7 | 0.001 | |
| Smoking,never smoked | Sometimes or often | 1.56 | 1.3-1.87 | <0.001 | 1.71 | 1.34-2.17 | <0.001 |
| Exercise,more than 1 h per week | 1 hour or less | 1.31 | 1.16-1.48 | <0.001 | 1.15 | 0.96-1.37 | 0.120 |
| Time on social media,less than 4 h a day | 4 hours or more | 1.49 | 1.36-1.63 | <0.001 | 1.51 | 1.33-1.72 | <0.001 |
| Feelings about school community2 | 1.10 | 1.07-1.14 | <0.001 | 1.16 | 1.11-1.2 | <0.001 | |
| Been bullied in the last year,never or once or twice | Bullied sometimes or often | 1.07 | 0.91-1.26 | 0.387 | 1.28 | 1.03-1.6 | 0.027 |
| Loneliness, never or sometimes lonely | Often lonely | 1.08 | 0.96-1.21 | 0.223 | 0.96 | 0.81-1.14 | 0.626 |
| RCADS score3 | 0.85 | 0.8-0.9 | <0.001 | 0.81 | 0.74-0.88 | <0.001 | |
| B-CAP score4 | 1.02 | 0.96-1.08 | 0.558 | 1.08 | 1-1.18 | 0.058 | |
| (Intercept) | 3.94 | 2.56-6.05 | <0.001 | 0.88 | 0.46-1.69 | 0.709 | |
Imputed sample data
Scored 1 to 7 on a likert scale, with 1 being strongly agree and 7 being strongly disagree
RCADS = Revised Children's Anxiety and Depression Scale, total score higher scores are more severe
B-CAP = The Bird Checklist of Adolescent Paranoia
p-values < 0.05 are in bold
Fig. 2.
Figure depicting Odds Ratios and 95% confidence intervals for predictors of response to the question: “Would you take a COVID-19 vaccine (approved for use in the UK) if offered?” in students in years 8 - 13, with the reference group those who described themselves as opting-in to getting a vaccine indicated as the comparator with OR = 1 (n = 15910).
In terms of health behaviours, students who exercised one hour or less a week had greater odds of describing themselves as being undecided about a vaccination (OR=1.31, 95%CI: 1.16-1.48, p < 0.001) but not opting-out of vaccination (OR=1.15, 95%CI: 0.96-1.37, p = 0.120) in comparison with those describing themselves as opting-in.
In terms of social connectedness, in comparison with those who spent less than four hours on social media a day, those who spent more than for hours had increased odds of describing themselves as being undecided about a vaccination (OR=1.49, 95%CI: 1.36-1.63, p < 0.001), or opting-out of a vaccination (OR=1.51, 95%CI: 1.33-1.72, p < 0.001). As students identified less with being part of their school community, the odds increased of describing themselves as being undecided about a vaccination (OR=1.10, 95%CI: 1.07-1.14, p < 0.001) or opting-out of a vaccination (OR=1.16, 95%CI: 1.11-1.20, p < 0.001) in comparison with describing themselves as opting-in to getting a vaccination.
Examining previous COVID-19 infection, compared to those who had not had COVID-19, those who had confirmed COVID-19 (OR=1.40, 95%CI: 1.15-1.70, p < 0.001) or probably had COVID-19 (OR=1.55, 95%CI 1.30-1.85, p < 0.001) both had higher odds of describing themselves as opting-out of vaccination in comparison with opting-in, but not for those with possible COVID-19 infection (OR=1.11, 95%CI 0.97-1.27, p = 0.137). We did not find similarly higher odds for those undecided about vaccination in comparison with those opting-in.
Finally, in relation to mental health, as RCADS total score increased, the odds of students describing themselves as undecided (OR= 0.85, 95%CI: 0.80-0.90, p < 0.001) or opting-out of a vaccination (OR=0.81, 95%CI: 0.74-0.88, p < 0.001) decreased in comparison with describing oneself as opting-in. In relation to paranoid feelings, there was no statistically significant difference in students describing themselves as undecided (OR=1.02, 95%CI: 0.96-1.08, p = 0.558) or opting-out of a vaccination (OR = 1.08, 95%CI: 1.00-1.18, p = 0.058) in comparison with describing oneself as opting-in to a COVID-19 vaccination. Results from both sensitivity analyses are largely aligned to our primary analysis and are described in Supplementary Tables 2 and 3.
4. Discussion
The data from over 27,000 UK students aged nine to 18 years show that the majority of older school-aged students are willing or eager to be vaccinated but whereas the rates for 16-,17 year-olds are as high as adults, the rates in younger students are substantially lower. Compared to students who would opt-in, those that were vaccine hesitant (undecided or opt-out) had differences primarily in indicators of social deprivation, community cohesion, and healthy behaviours. Vaccine hesitant students were more likely to come from a deprived socioeconomic context with higher rates of home rental rather than home ownership and their school locations were in areas of greater deprivation. The hesitant students were more likely to exhibit less healthy behaviours with more smoking and vaping and spend longer on social media. The vaccine hesitant students were less socially connected in other ways, being less likely to identify with their school community. Of note, the hesitant group had lower levels of anxiety and depression. There was further evidence to highlight how, for the more extreme vaccination opt-out group, the markers of social marginalisation were greater, as they were more likely to report being bullied at school and there was an indication of higher levels of paranoia. In addition, those more likely to opt-out were also more likely to have definitely or probably had COVID-19 infection. However, females were less likely than their male counterparts to be undecided about vaccination in comparison with opting-in to vaccination as well as students who had both parents born outside the UK.
It is important to note some key limitations of the study. Although we recruited a large participant group from a broad range of schools and regions, we do not know how representative our sample is of either England as a whole, or within individual regions. Furthermore, response rates differed by school and class year. We only had relevant data for one region and we do not know whether this is representative of the other regions surveyed. In this region 86.7% of year 6 students in recruiting schools participated but only 3% of year 11 students participated (who were mostly absent from in-person school because of key national examinations (GCSEs)). In addition, there were classes and ‘student bubbles’ needing to isolate throughout this period and so it is unclear what proportion of expected and unexpected absences there were at the time of testing. In terms of demographic representativeness, no information on ethnicity or free school meals were collected in the survey and current school-level data on gender by year group were not available. Furthermore 5% of the survey sample did not choose male or female as a response (either because they fell in an ‘other’ category and/or because they ‘chose not to answer’). A whole schools methodology is clearly challenged during such a disruptive time for education. A further key limitation is that all the responses were self-reported and so limited by the inherent information and social desirability biases of self-report surveys including recall bias. We prioritised use of validated questionnaires; but the self-report method might have, for example, impacted on responses to the question as to whether students had had COVID-19 infection, although our findings had face validity as the regression results highlighted how hesitancy increased as likelihood of past infection increased. In addition, we do not know the presence of physical vulnerability factors in the students and hence cannot estimate willingness to be vaccinated in what may become a greater priority group. However, when students were asked to participate in the survey they were informed that they would be asked a large number of questions on mental health and well-being but they were not informed that there would be a question on willingness to have a COVID-19 vaccination. Therefore, the presence of this question would not have impacted on a student's decision to participate in the survey. Finally, it would be essential to triangulate these findings with more qualitative data from current students about reasons behind their choices and how to address any factors or concerns that might be drivers in their decision-making, especially, for example, in those who have previously had confirmed or probable COVID-19 infection. We report on discussions with a young people's advisory group (YPAG) in Supplementary Materials, although these young people were not in the under 15 age range.
We will focus the discussion on resource, ethical and policy implications of COVID-19 vaccination for adolescents. Adolescents are an important population group with currently 1.2 billion 10-19 years olds globally, the highest proportions are living in lower resource settings [25,26]. Addressing adolescent COVID-19 vaccination must reflect resource implications as well as issues of equity, justice and prioritisation of certain population groups, especially given vaccination distribution and acceptance in lower resource settings [27]. Whether adolescents in higher resource settings should have access to the vaccination before more vulnerable groups elsewhere remains a high priority to consider. Nevertheless, as vaccination availability increases, questions remain about the relative benefit of providing COVID-19 vaccinations for adolescents.
We found that the majority of older school-aged students would opt-in to having a COVID-19 vaccination. There is, therefore, likely to be increasing prominence to the question of adolescent self-consent as at present for those under the age of 18 in many countries (under age 16 in a minority of countries including the UK, USA and Australia) parental knowledge and/or explicit consent is required. In England and Wales, the standard of Gillick competence is used to determine if a child is able to give legally effective consent [28,29]. For an adolescent to be able to consent for COVID-19 vaccination, they need to be able to understand the reason for why the vaccination has been recommended- for which a broad explanation including that it would be to protect them and others from catching an unpleasant disease is required. Secondly, they would need to understand in broad terms the nature of the procedure, for example that it would involve an injection into their arm which might result in pain at the injection site. Furthermore, it is required that health care professionals inform recipients of the risks that ‘a reasonable patient would want to know’ -known as the material risk [30] which does not require the disclosure of all risks of the vaccination but only those where harm is highly likely to occur or where there is a non-negligible risk of a serious harm.
Gillick competence is therefore a relatively low hurdle for an adolescent to jump to enable self-consent in the case of a COVID-19 vaccination. Although a health care professional is entitled in law to provide vaccination relying just on the consent of an adolescent who is Gillick competent, it is usual practice, when for example schools administer HPV, that the consent of a person with parental responsibility is also sought. However, despite legal clarity, problems can emerge if a parent does not want their child vaccinated and the adolescent wants the vaccine. For example, in July 2021, the vaccination drive in the state of Tennessee became heavily criticised for vaccinating without explicit parental consent leading to state health officials necessitating parental involvement for vaccinations for those under the age of 18 [31,32].
An additional complication might arise if a parent wants their adolescent to be vaccinated but the adolescent refuses. Although in this case parental responsibility is sufficient in law, in practice it is unlikely that the force, indignity and resultant distress from enforcing the vaccination is ever justified. The focus in these contexts could be to try and understand the drivers for the refusal.
In considering adolescent rights to privacy, as public vaccination drives take greater prominence, there is increasing discussion about the rights and privileges that might entail as a result of having been vaccinated. Although societal plans to discriminate against hesitant individuals has been argued as a risky slippery slope toward human rights encroachments [2] there remains a need to consider protection of high-risk individuals. In some countries, fully vaccinated adults can resume their pre-pandemic activities such as travel without restriction, not wear masks and congregate in social venues. This might, therefore, affect adolescents’ attendance at certain school-related activities- such as school trips, attendance at larger group events and proximity to any other students deemed health vulnerable. Any coercion to get vaccinated can reduce public trust in vaccination drives [2] whilst the prospect of gaining a “Green Pass” has been positively associated with an intention of parents to vaccinate their children [33].
We are moving to a new phase of the pandemic, from an original short-term desire to eradicate the disease to an endemic state, where the virus continues to circulate but severe disease is minimised through vaccine immunity and therefore strategies to manage risk and morbidity focussing on preventive activities, such as vaccination programmes become prominent. A prevailing view has been that vaccinating adolescents might result in a population-level reduction in infections and severe illness amongst adults, but this may not be achievable if a limited proportion opt-in, or the virus becomes increasingly able to infect vaccinated individuals. Furthermore, there is a subgroup of children with co-morbidities who are at higher risk of more severe disease [34], which at the present time seems to be preventable through vaccination. Public health bodies and governments may need to prioritise vaccination drives to those who are undecided, particularly those in risk groups.
For those who are undecided or planning to opt-out of vaccination, a three-pronged approach may be warranted: focusing on providing information; addressing worries; and improving access - in particular to populations that are more socioeconomically deprived and marginalised. This is similar to the findings in adult populations and therefore, co-producing approaches with representatives from these populations (including parents) will be essential.
Primarily, information is needed given high levels of uncertainty amongst younger children and although it is developmentally appropriate to defer to a parental figure for these types of decisions, there will be an important need to prepare these age ranges, if they are included in vaccination programmes. Given the many hours that younger, undecided school students are spending on social media, this medium seems key to try and improve awareness and understanding of the vaccination. In addition, students who had either had previously confirmed COVID-19 infection, or a probable infection, were more likely to opt-out of a vaccination and so better information needs also answer the question of immunity for those who have had the disease to ensure that as we learn more about the range of immune responses to virus exposure, that this learning is shared with younger populations. Therefore, clarifying that re-infection is possible and it is therefore not a virus such as measles, where infection often confers lifelong immunity. Furthermore, misinformation, both online and offline, has been shown to directly impact on vaccination confidence and intent [35]. Our YPAG highlighted the importance of having trusted sources to provide this information in a socially acceptable and accessible medium. Furthermore, schools could consider incorporating the role, development and effects of vaccinations as a topic to be studied in both primary and secondary school lessons.
Addressing any worries and fears are likely to be important because there might be some avoidance of the vaccination because of needle phobia [36,37] and others who have negative concerns about the vaccine due to exposure to certain information, experiences and pre-existing beliefs. Although those with greater symptoms of anxiety or depression were more willing to be vaccinated, this might reflect heightened health concerns and anxiety leading to more knowledge about the vaccination and its potential effects. It is likely that social media will continue to play an important part in forming attitudes and responses to COVID-19 and must therefore be utilised in any public health campaigns [38].
Finally, making vaccination centres as accessible as possible is important [39]. Vaccine hesitancy was higher in deprived communities who may already have barriers to access to vaccination (e.g. access to transport, time off work). Our YPAG advised that many do not like to receive their vaccinations at school, yet school locations are likely to be the most successful location for the opt-in majority. Providing access in acceptable and relevant community spaces such as football grounds and shopping centres, might enhance opportunities for those that do not feel engaged at school and who might want privacy as to their vaccination status. More research as to what the more marginalised adolescents would find useful with regards to vaccination information and access is needed, as they might be more difficult to reach through school-based and peer-based initiatives if they feel a poor connection with their school and feel bullied.
In conclusion, as adolescents are increasingly in charge of their own healthcare, and are developing their lifelong blueprint for approaches to personal and public health initiatives, attitudes to vaccination matter. The structural risk factors, primarily around deprivation and social cohesion, that the COVID-19 pandemic has dramatically exposed across high and low-income settings, remain drivers not only for severe disease but also vaccine hesitancy. The current generation of children and adolescents are likely to experience impacts on all aspects of their development due to COVID-19. Ensuring long-term engagement with the multifaceted COVID-19 preventive approaches that will need be employed to support their health and social wellbeing, as well as that of the wider community, must now be prioritised.
Authors’ contributions
MF and KLM conceived the OxWell School Survey and obtained funds. All authors worked on conceptualisation and methodology. SP and SRW designed and performed the analyses. MF and SP wrote the manuscript. MF, KLM, SP verified the data of this study. All authors critically reviewed the manuscript.
Declaration of Competing Interest
AJP is Chair of UK Dept. Health and Social Care's (DHSC) Joint Committee on Vaccination & Immunisation (JCVI), but does not participate in policy decisions on COVID19 vaccine. He is a member of the WHO's SAGE. AJP is an NIHR Senior Investigator. DF is an NIHR Senior Investigator. SRW reports grants from UKRI Medical Research Council (MC_UU_00002/2) and grants from the NIHR Cambridge Biomedical Research Centre (BRC-1215-20014) during the conduct of the study. AJP is chief investigator on clinical trials of Oxford University's COVID19 vaccine funded by NIHR. Oxford University has entered a joint COVID19 vaccine development partnership with Astra Zeneca. All other authors have nothing to declare.
The views expressed in this article do not necessarily represent the views of the DHSC, JCVI, NIHR, MRC or WHO.
Acknowledgments
Funding
This research was funded by the Westminster Foundation, the National Institute for Health Research (NIHR) Applied Research Collaboration Oxford and Thames Valley at Oxford Health NHS Foundation Trust, the NIHR Biomedical Research Centre and an MRC Mental Health Data Pathfinder award to the University of Oxford, with support from Frimley CCG, Berkshire West CCG, Buckinghamshire Council and Milton Keynes Council. The funders played no role in the writing of the manuscript, or the decision to submit for publication.
Acknowledgements
The investigators acknowledge the philanthropic support of the donors to the University of Oxford's COVID-19 Research Response Fund.
We would like to thank all the students who took the time to participate in the OxWell school survey, and the many staff at all the participating schools for the considerable time and planning they put into conducting the survey at a hectic time. We thank many colleagues in local authorities and clinical commissioning groups, including Donna Husband, Lajla Johansson, Giovanni Ferri, Chris Price, Jonathan Jones and Janette Fulwood, for their time and support in promoting the survey. We thank Katie Treherne for helping develop the research in context search strategy. We would also like to thank Pauline Foster and Elaine Purse at Foster and Brown Research Limited who provide the infrastructure for the OxWell survey.
Data sharing statement
All authors had full access to all the data in the study and accept responsibility to submit for publication.
Fully de-identified extracts of the data can be provided to academic research collaborators upon reasonable request, following a review process by the research team to ensure uses of the data fall under the remit of the intended purposes set out in the privacy information and to prevent duplication of analyses. The data are not publicly available due to ethical and information governance restrictions. The full list of questions and other details are available on a project-specific ‘OxWell’ OSF website along with publication of the study protocol (see https://osf.io/sekhr/). Full data dictionaries can be made available upon approval for access to data extracts.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2021.101144.
Appendix. Supplementary materials
References
- 1.Mallapaty Will COVID become a disease of the young? Nature. 2021;595:343–344. doi: 10.1038/d41586-021-01862-7. [DOI] [PubMed] [Google Scholar]
- 2.Gurwitz D. COVID-19 vaccine hesitancy: Lessons from Israel. Vaccine. 2021;39(29):3785–3786. doi: 10.1016/j.vaccine.2021.05.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wodi A.P., Ault K., Hunter P., McNally V., Szilagyi P.G., Bernstein H. Advisory committee on immunization practices recommended immunization schedule for children and adolescents aged 18 years or younger - United States, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(6):189–192. doi: 10.15585/mmwr.mm7006a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ledford H. Should children get COVID vaccines? What the science says. Nature. 2021;595(7869):38–639. doi: 10.1038/d41586-021-01898-9. [DOI] [PubMed] [Google Scholar]
- 5.Langley J.M. Adolescent immunization – protecting youth and preparing them for a healthy future. Int J Pediatr Adolesc Med. 2015;2(1):1–6. doi: 10.1016/j.ijpam.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ward K., Quinn H., Menzies R., McIntyre P. A history of adolescent school based vaccination in Australia. Commun Dis Intell Q Rep. 2013;37(2):E168–E174. [PubMed] [Google Scholar]
- 7.Martinón-Torres F., Banzhoff A., Azzari C. Recent advances in meningococcal B disease prevention: real-world evidence from 4CMenB vaccination: real-world effectiveness of MenB vaccination. J Infection. 2021;83(1):17–26. doi: 10.1016/j.jinf.2021.04.031. Jul. [DOI] [PubMed] [Google Scholar]
- 8.Paul P., Fabio A. Literature review of HPV vaccine delivery strategies: considerations for school- and non-school based immunization program. Vaccine. 2014;32(3):320–326. doi: 10.1016/j.vaccine.2013.11.070. [DOI] [PubMed] [Google Scholar]
- 9.Public Health England. Human papillomavirus (HPV) vaccination coverage in adolescent females and males in England: academic year 2019 to 2020. Health Protection Report Vol 14, no 19; October 2020. Public Health England, London. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/927694/hpr1920_HPV-vc.pdf [last accessed Sept 3 2021]
- 10.Flood T., Wilson I.M., Prue G., McLaughlin M., Hughes C. Impact of school-based educational interventions in middle adolescent populations (15201317 years) on human papillomavirus (HPV) vaccination uptake and perceptions/knowledge of HPV and its associated cancers: a systematic review. Prev Med. 2020 doi: 10.1016/j.ypmed.2020.106168. [DOI] [PubMed] [Google Scholar]
- 11.Zimet G.D., Silverman R.D., Bednarczyk R.A., English A. Adolescent consent for human papillomavirus vaccine: ethical, legal, and practical considerations. J Pediatr. 2021;231:24–30. doi: 10.1016/j.jpeds.2021.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feldstein L.R., Tenforde M.W., Friedman K.G. Characteristics and outcomes of US children and adolescents with multisystem inflammatory syndrome in children (MIS-C) compared with severe acute COVID-19. JAMA. 2021;325(11):1074–1087. doi: 10.1001/jama.2021.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buonsenso D., Munblit D., De Rose C. Preliminary evidence on long COVID in children. Acta Paediatr. 2021;110(7):2208–2211. doi: 10.1111/apa.15870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Osmanov I.M., Spiridonova E., Bobkova P. Risk factors for long covid in previously hospitalised children using the ISARIC Global follow-up protocol: a prospective cohort study. Eur Respir J. Jan 2021 doi: 10.1183/13993003.01341-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wallace M., Woodworth K.R., Gargano J.W. The Advisory committee on immunization practices’ interim recommendation for use of Pfizer-BioNTech COVID-19 Vaccine in Adolescents Aged 12–15 Years—United States, May 2021. MMWR Morb Mortal Wkly Rep. 2021;70(20):749. doi: 10.15585/mmwr.mm7020e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Snapiri O., Shirman N., Weissbach A. Transient cardiac injury in adolescents receiving the BNT162b2 mRNA COVID-19 Vaccine. Ped Inf Dis J. 2021 doi: 10.1097/INF.0000000000003235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glikman D., Stein M., Shinwell ES. Vaccinating children and adolescents against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)—the Israeli experience. Acta Paediatrica. 2021 doi: 10.1111/apa.15982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mansfield K.L., Newby D., Soneson E. COVID-19 partial school closures and mental health problems: a cross-sectional survey of 11,000 adolescents to determine those most at risk. JCPP Adv. 2021;1(2):e12021. doi: 10.1002/jcv2.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Freeman D., Loe B.S., Chadwick A. COVID-19 vaccine hesitancy in the UK: the oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2020:1–15. doi: 10.1017/S0033291720005188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McLennan D, Noble S, Noble M, Plunkett E, Wright G, Gutacker N. The English indices of deprivation 2019: Technical report. 2019 Ministry of Housing, Community and Local Government, London. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/833951/IoD2019_Technical_Report.pdf [last accessed Sept 19 2021]
- 21.Ebesutani C., Reise S.P., Chorpita B.F. The revised child anxiety and depression scale-short version: scale reduction via exploratory bifactor modeling of the broad anxiety factor. Psychol Assess. 2012;24(4):833–845. doi: 10.1037/a0027283. [DOI] [PubMed] [Google Scholar]
- 22.Bird J.C., Loe B.S., Kirkham M. The assessment of paranoia in young people: item and test properties of the bird checklist of adolescent paranoia. Schizophr Res. 2020;220:116–122. doi: 10.1016/j.schres.2020.03.046. [DOI] [PubMed] [Google Scholar]
- 23.Van Buuren S., Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. J Stat Softw. 2011;45(1):1–67. [Google Scholar]
- 24.Rubin DB. John Wiley & Sons Inc.; New York: 2004. Multiple imputation for nonresponse in surveys. [Google Scholar]
- 25.United Nations Department of Economics and Social Affairs; Population Dynamics. World population prospects 2019 Highlights, Online Edition. Rev. 1. 2019. United Nations, New York. https://population.un.org/wpp/Publications/Files/WPP2019_Highlights.pdf [last accessed Sept 3 2021]
- 26.You D., Beise J., Lee S., Requejo J., Strong K. Demographic challenges and opportunities for child health programming in Africa and Asia. BMJ. 2021;372:n19. doi: 10.1136/bmj.n19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Simas C., Larson HJ. Overcoming vaccine hesitancy in low-income and middle-income regions. Nat Rev Dis Primers. 2021;7(1):41. doi: 10.1038/s41572-021-00279-w. [DOI] [PubMed] [Google Scholar]
- 28.Palmer R., Gillespie G. Consent and capacity in children and young people. Arch Dis Child Educ Pract Ed. 2013 doi: 10.1136/archdischild-2013-303675. edpract-2013-303675. [DOI] [PubMed] [Google Scholar]
- 29.Kuther TL. Medical decision-making and minors: issues of consent and assent. Adolescence. 2003;38(150):343. [PubMed] [Google Scholar]
- 30.Farrell A.M., Brazier M. Not so new directions in the law of consent? Examining Montgomery v Lanarkshire health board. J Med Ethics. 2016;42(2):85–88. doi: 10.1136/medethics-2015-102861. [DOI] [PubMed] [Google Scholar]
- 31.Laughland O. New health department rules reportedly apply to inoculations against all diseases. The Guardian; 2021. Tennessee to halt vaccine outreach to teens amid conservative backlash – report. 13 July 2021. [Google Scholar]
- 32.Barajas A. Tennessee resumes vaccination outreach but with marketing emphasis on parents, not children. 2021. CNN International, Health. https://edition.cnn.com/2021/07/23/health/tennessee-teen-vaccinations-piercey/index.html [last accessed 19 Sept 2021]
- 33.Atad E., Netzer I., Peleg O. Vaccine-hesitant parents’ considerations regarding Covid-19 vaccination of adolescents. medRxiv. 2021 2021.05.25.21257780. [Google Scholar]
- 34.Molteni E., Sudre C.H., Canas L.S. Illness duration and symptom profile in symptomatic UK school-aged children tested for SARS-CoV-2. Lancet Child Adolesc Health. 2021 doi: 10.1016/S2352-4642(21)00198-X. Aug 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Loomba S., de Figueiredo A., Piatek S.J., de Graaf K., Larson HJ. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 2021;5(3):337–348. doi: 10.1038/s41562-021-01056-1. [DOI] [PubMed] [Google Scholar]
- 36.McLenon J., Rogers M.A.M. The fear of needles: a systematic review and meta-analysis. J Adv Nurs. 2019;75(1):30–42. doi: 10.1111/jan.13818. [DOI] [PubMed] [Google Scholar]
- 37.Freeman D., Lambe S., Yu L.M. Injection fears and COVID-19 vaccine hesitancy. Psychol Med. 2021:1–11. doi: 10.1017/S0033291721002609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bozzola E., Staiano A.M., Spina G. Social media use to improve communication on children and adolescent's health: the role of the Italian Paediatric Society influencers. Ital J Pediatr. 2021;47(1):171. doi: 10.1186/s13052-021-01111-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Torracinta L., Tanner R., Vanderslott S. Mmr vaccine attitude and uptake research in the united kingdom: a critical review. Vaccines. 2021;9(4):402. doi: 10.3390/vaccines9040402. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.