Abstract
The COVID-19 pandemic has seen an unusually high proportion of the population suffering from mental health difficulties, but of particular concern is the disproportionate increase in psychological distress among younger adults. In this article, we exploit an explanatory sequential mixed-methods design to examine which aspects of the COVID-19 pandemic 18-25-year-olds found most challenging. We report analyses of American Voices Project (AVP) qualitative in-depth interview data, a MyVoice text-message open-ended survey, and Census Bureau Household Pulse Survey (HPS) data, all collected in 2020. Our interview and text-message results show that young adults were distressed about the effects of COVID-19 on the health of loved ones and older Americans. Young adults expressed concerns that the pandemic was not being treated sufficiently seriously by some politicians and the general public. The policy response was seen to be inadequate to the task of containing the disease, and some feared that the pandemic would never end. Statistical analyses of the HPS confirm that young adults’ scores on the HPS’s anxiety scale were significantly negatively associated with state-level policy responses. Overall, our results show that young adults found virus mitigation strategies challenging, but that a strong policy response was associated with reduced levels of psychological distress. Our results suggest that public health policy might have also operated as mental health policy during the COVID-19 pandemic.
Keywords: Young adults, Psychological distress, COVID-19, Policy response
1. Introduction
The period of young or “emerging” adulthood – from around 18 to 25 years old – is a time of great potential (National Research Council, 2015), but it is also a period of heightened vulnerability to poor mental health. The COVID-19 pandemic has seen an unusually high proportion of the population suffering from mental health difficulties, but of particular concern is the disproportionate increase in psychological distress among younger adults. Young adults have borne many of the costs of the pandemic – through job loss, school closures, a loss of important milestones, and social isolation – and have also experienced the largest increases in adverse mental and behavioral health conditions.
Prior research on the United States has largely focused on changes in rates or levels of psychological distress between the pandemic and the months and years prior. This literature has documented substantial increases in rates of anxiety disorders, depressive disorders, and suicidal ideation, increases in substance use and overdose, and increases in the number of emergency room visits related to psychological distress (Czeisler, 2020; Daly, Sutin, & Robinson, 2021; Holingue et al., 2020; Holland et al., 2021; Vahratian, 2021). Young adults have experienced particularly large increases in levels of psychological distress and loneliness, alongside decreases in positive affect (Daly et al., 2021; Ellwardt & Präg, 2021; Giuntella, Hyde, Saccardo, & Sadoff, 2021; Golberstein, Wen, & Miller, 2020; Hoyt, Cohen, Dull, Maker Castro, & Yazdani, 2021; Hu & Qian, 2021; Lee, Cadigan, & Rhew, 2020; Rogers, Ha, & Ockey, 2021). There is some evidence for heterogeneity among young adults in their psychological responses to the pandemic: gender identity, sexual orientation, and income have all been shown to be associated with psychological distress (Fish et al., 2020; Hoyt et al., 2021; Tetreault et al., 2021).
The causes of poor mental health among young adults during the pandemic are not fully understood, although young adults are more likely to have been exposed to potential stressors than older adults. Difficult social and economic experiences during the pandemic appear to have been particularly strong predictors of psychological distress, and in an analysis of data collected in June 2020, Ganson et al. report that half of young adults in the United States had either experienced job loss or expected to lose their jobs soon (2021). Younger people were also more likely to experience food insecurity and food insufficiency during 2020 (Nagata, Ganson, Whittle, et al., 2021). Both job loss and food insecurity are associated with poor mental health in young adults (Bartelink, Zay Ya, Guldbrandsson, & Bremberg, 2020; Nagata et al., 2019), suggesting that exposure to economic precarity might account for at least part of the disproportionate increase in psychological distress in the young adult population during the pandemic. Notwithstanding, research on college students also shows a take-off in mental health difficulties during the pandemic (Giuntella et al., 2021; Hoyt et al., 2021). This would imply that a range of other factors – including pandemic-induced changes in stress, physical activity, sleep patterns, and lifestyle – may be important in accounting for the rise of psychological distress (Birditt, Turkelson, Fingerman, Polenick, & Oya, 2021; Giuntella et al., 2021). Although young adults were at low risk from COVID-19 disease, mitigation policies aimed toward reducing spread of the disease, such as “stay at home” orders, school closures, and social distancing requirements, have had disproportionate impacts on younger people. Alongside increases in exposure to stressors, psychological distress is likely to have been further exacerbated by reduced access to mental health care (Nagata, Ganson, Bonin, et al., 2021).
Thriving cohorts of young adults are vital to a strong workforce, economy, and collective wellbeing. Positive mental health is foundational for individual and community resilience, and investments that support mental health are vital (National Academies of Sciences, Engineering, and Medicine, 2019; Spera & Monnat, 2020). Professional treatment of psychological distress is known to be effective in young people (National Research Council, 2015), but it is underutilized (Harvey & Gumport, 2015; National Academies of Sciences, Engineering, and Medicine, 2019), meaning that population-based initiatives are also required. Family-, community, and school-based interventions have shown promise (National Academies of Sciences, Engineering, and Medicine, 2019; National Research Council, 2015; Spera & Monnat, 2020), and internet-based therapies are likely to be an area of special focus following their mainstream adoption during the pandemic (Aminoff et al., 2021; Carlo et al., 2021). Policies designed to ameliorate those problems that the pandemic has exacerbated, including economic precarity and job loss, have also been shown to be associated with reduced rates of psychological distress in the population (Donnelly & Farina, 2021).
In this paper, we examine psychological distress in young adults in the United States during 2020. Rather than treating the pandemic as a straightforward “event,” the effects of which can be judged by comparing pandemic data with non-pandemic data, we examine changes in psychological distress during the pandemic in 2020. We employ a mixed methods design to describe young adults’ experiences of psychological distress during 2020, and to identify their sources of distress. We find evidence of substantial volatility in psychological distress over the course of 2020, and identify a set of pandemic-related stressors alongside the standard correlates of psychological distress. We argue that during 2020, clear and decisive COVID-19 containment policy might have simultaneously operated as mental health policy, by offering hope and reassurance to young adults that the COVID-19 pandemic and the resulting economic crisis might be brought under control.
2. Material and methods
We draw upon data from three different sources: in-depth interviews, a text-message survey, and the Census Bureau’s Household Pulse Survey. Using an explanatory sequential mixed-methods design (Creswell & Creswell, 2018), we use the qualitative data to identify common themes and develop hypotheses, and test these hypotheses using the quantitative data.
Our in-depth interview data come from the American Voices Project (AVP), a nationally representative study that was in the field for much of the COVID-19 pandemic (Alexander et al., 2017; Freese, Johnson, & Garcia, 2021; Jackson, Lee Williams, Dahir, & Edelman, 2021; Stanford Center on Poverty and Inequality, 2021). The sampling frame is Census tracts and block groups, with an oversample of low- and middle-income sites. Within each block group, a representative address-based sample of households is drawn. From the AVP sample we select all 18-25-year-olds who were interviewed between May and December 2020, giving a final sample size of 52 (descriptive statistics for all data sources are included in Table 1 ). We used a combination of inductive and deductive coding to identify the main themes that emerged in the interview data (Gerson & Damaske, 2020). We initially designed the coding frame to capture the pandemic’s effects on developmentally-important milestones and activities, and added further categories for unanticipated themes after a first round of coding. A team of coders (five undergraduate and two graduate students) went through initial rounds of practice coding (i.e., coding the same transcript) followed by discussion for clarification and verification of the coding frame. The trained coders then used this coding frame to code the interviews, and met regularly to discuss emergent themes.
Table 1.
Descriptive statistics for the analysis samples.
| Sociodemographic characteristic | AVP interviews |
MyVoice text messages |
HPS data |
|---|---|---|---|
| May–Dec 2020 |
Oct–Nov 2020 |
April–Dec 2020 |
|
| No. (%) | No. (%) | Weighted % | |
| Gender | |||
| Female | 33 (63) | 311 (54.1) | 51.6 |
| Male | 19a (37) | 220 (38.3) | 48.4 |
| Other | 44 (7.6) | ||
| Hispanic/Latinx | 12 (23) | 64 (11.1) | 16.9 |
| Race | |||
| Asian | 12a (23) | 100 (17.4) | 5.6 |
| Black | 60 (10.4) | 12.5 | |
| White | 26 (50) | 336 (58.4) | 75.7 |
| Other | 14 (27) | 79 (13.7) | 6.2 |
| Age, mean, SD of young adults | 21.9, 2.1 | 20.5, 2.1 | 21.8, s.e. 0.02 |
| Total n | 52 | 575 | 1,864,102 (including 77,414 18-25-year-olds) |
Cell counts merged in line with AVP disclosure guidelines to preserve respondent confidentiality.
Next, we carried out a text-message survey of youth and young adults using the MyVoice platform (DeJonckheere et al., 2017; Waselewski, Waselewski, & Chang, 2020). MyVoice maintains an ongoing panel of young people, ages 14–24, who receive a small payment for participating in weekly SMS text-message surveys over a 3-month period. Panel members are recruited using targeted social media messaging based on age, gender, race and ethnicity, and region (MyVoice, 2020). Panel members receive a series of five text message questions and reply with their answers. Our survey went into the field on October 30th 2020, and data collection continued to November 6th. The response rate was 78%, and we selected respondents aged 18–24 for our analyses. We asked respondents:
-
1.
Reflecting on your experiences since March, what have you found most difficult about the COVID-19 pandemic?
-
2.
What are you most worried about as the pandemic continues?
The first question was answered by 575 respondents and the second by 536 respondents. We again used a combination of inductive and deductive coding to identify the emergent themes from the data. The authors read all responses and developed initial codes, then met regularly to develop a final codebook. Both authors then coded responses into the broad categories reported below.
Finally, we conduct statistical analyses of the Census Bureau’s Household Pulse Survey (HPS). The HPS is a repeated cross-sectional survey, first fielded in April 2020, which aims to collect time-sensitive data on the impact of the COVID-19 pandemic on U.S. households. The sample is drawn from the Census Bureau’s Master Address File, and households are contacted via email and text (Census Bureau, 2020a). We use the first 21 waves of the HPS, collected between late-April and December 2020. The sample size for each cross-section is very large, but response rates are very low, averaging 5.1% (Census Bureau, 2020b). Weights are included to allow researchers to provide population-level estimates; in a study of non-response bias, the Census Bureau reports that the HPS weights help to mitigate bias (Peterson, Toribio, Farber, & Hornick, 2021). Because Little’s test indicated that data were not MCAR (Little, 1988), we also conducted multiple imputation using chained equations to impute values for those who had not responded to all questions (Little, 1988). Details of the imputation model are included in the Appendix.
We link the HPS data to weekly data on COVID-19 case counts (per 100,000 state residents) and state policy responsiveness, measured on scales of 0–100, where higher scores indicate a more robust policy response (Hale et al., 2021; The New York Times, 2021). We include two separate policy indexes in our model: a containment and health index and an economic support index. Our primary research interest is in the containment and health index, as this captures the policy response with respect to virus mitigation. The containment and health index contains fourteen indicators, including school and workplace closures, restrictions on gathering, and mask mandates (see Appendix: Methods for a list of all items included in the scales; see figs.A1&A2 for over-time variation in case counts and containment policy responses by state).
Our analyses examine variation in psychological distress over time, and associations among psychological distress, COVID-19 case counts, and the state-level policy response, controlling for a set of standard sociodemographic characteristics and state fixed effects. Our primary response variable captures psychological distress via the Generalized Anxiety Disorder (GAD) scale, a validated measure of anxiety that was adapted for use in the HPS (Census Bureau, 2020a; Vahratian, 2021). The scale runs from 0 to 6, and is constructed by adding the scores from two separate items in the HPS. The items are of the format: “Over the last 7 days, how often have you been bothered by the following problems ...[item-specific phrase] Would you say not at all, several days, more than half the days, or nearly every day?” The first item elicits responses to the phrase “Feeling nervous, anxious, or on edge?” and the second elicits responses to “Not being able to stop or control worrying?” Although our primary measure of psychological distress is the GAD scale, the HPS also includes similar items that can be used to construct a measure of depression (the Patient Health Questionnaire (PHQ) scale), and in the Appendix we replicate our analyses for the depression measure, showing similar results.
We fit pooled multivariate OLS models of the form:
Standard errors account for clustering at the state and household level (Gu & Yoo, 2019). Our analysis code is available at OSF (https://osf.io/kzfqh/).
Our model allows us to isolate the associations between psychological distress and case counts and psychological distress and virus containment policy (i.e., the bolded coefficients) after controlling for individual-level confounders, economic policy response, and the state-level correlates of psychological distress. At the individual level, we control for gender, race, Hispanic ethnicity, recent job loss and income. We do not control for educational attainment, as the young adults in our sample are too young to have completed their educational career, and the variable is therefore endogenous to age. All individual-level variables are interacted with the age-group variable. The state of residence fixed effects capture geographical context and allow us to model the association between GAD scores and case numbers/policy response net of state characteristics. This approach is demanding with respect to statistical power, but the state fixed effects allow us to hold constant all of those aspects of state context that are constant over time and are associated with psychological distress. The state fixed effects are also an important tool for mitigating non-response bias. Although our models use the HPS weights, which have been shown to mitigate bias, the Census Bureau noted that additional non-response bias might remain with respect to geography (Peterson et al., 2021). It is also important to acknowledge that selection on unobservables – such as political partisanship – might be a source of non-response.
We interact the policy response variable with age-group, thereby testing the hypothesis that the association between psychological distress and policy response is stronger for young adults than for older adults. Given that our research interest was in policy interventions related to virus control, we included a control for economic policy, captured by the economic support index (see Appendix: Methods). Prior research has shown that economic policy is more strongly associated with psychological distress for those who have experienced recent job loss (Donnelly & Farina, 2021), and we therefore include an interaction between the economic support index and the job loss variable. There was no interaction between the economic support index, job loss, and age-group. We also tested for interaction between case numbers and age-group, but the interaction coefficient was extremely small and insignificant, and for reasons of parsimony we excluded it from our final model.
3. Results
Psychological distress was acknowledged by almost all of the young adults who were interviewed. AVP respondents described feelings consistent with standard operationalization of anxiety and depression, characterizing their emotional state with words like “stressed,” “worried,” “frightened,” “bad,” and “sad.” Many identified their feelings explicitly as “anxiety,” “stress,” or “depression.” Interviewees freely described difficult psychological experiences, and highlighted the effects of external factors in explaining the intensity of their psychological distress. For example, in an AVP interview from July 2020, one respondent described:
“It’s been a roller coaster… I started 2020 off on a pretty high note…and then like all of a sudden all this COVID news starts bubbling around. And I’m like, “Okay, cool, wait; we’re America, we’ve dealt with big problems before. We will deal with it as we’ve always dealt with things.” Like in a nice American way and we’ll all join together and it will be fine and then, March rolls around and they lock everything down… all of a sudden, just like overnight. And that’s where I guess some problems started coming in…There were some moments…where it was hard to accept that this is the way things are…and it got pretty dark sometimes.”
We see in this quote three themes that we build upon in the following sections: high volatility in mental health, worries that the country’s pandemic policy was inadequate to the task, and the potential for clear and decisive policy to reassure young people that problems can be solved (i.e., “we’re America, we’ve dealt with big problems before”). In the following sections, we pull together evidence from the interviews, text-messages, and survey data, to describe young adult psychological distress during the COVID-19 pandemic.
3.1. Volatility in psychological distress during the COVID-19 pandemic
AVP interviewees reported substantial volatility in their psychological distress over the course of 2020. In the interviews from late-spring and early-summer, young adults compared their mental wellbeing favorably to the early phase of the pandemic. For example, this young man recalled,
“I guess, levels of stress and worry have gone down, I mean, there’s just less to be stressed and worried about honestly, as far as like the day-to-day. When it was first ramping up, it definitely was more stressful and just, what is the extent of this going to be?”
Fall and winter AVP interviewees similarly highlighted the early months of the pandemic as a particularly difficult time, although among these respondents we see varying descriptions of their wellbeing; some respondents focused on their adaptation to the pandemic and relatively good mental health, while others described still being troubled by symptoms of psychological distress. Notably, a common theme among the AVP interviewees was that the beginning of 2020 was a happy time, which COVID-19 interrupted. Current experiences of mental distress are thus counter-posed against the pre-pandemic period.
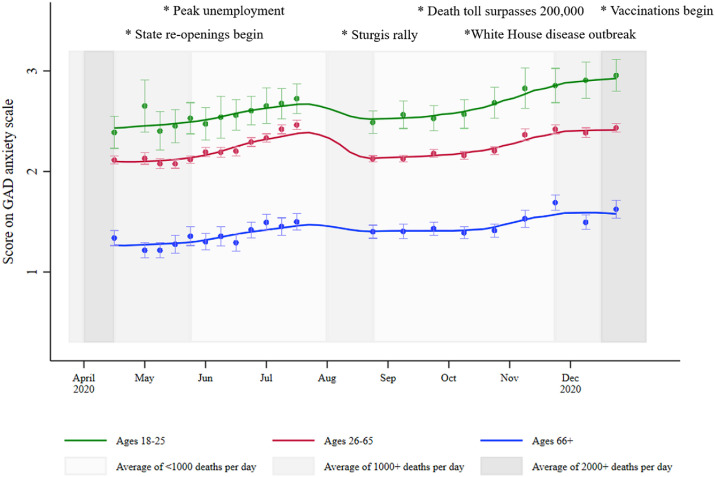
The HPS data allow us to examine whether or not the individual-level volatility in psychological distress picked up qualitatively in our AVP interviews is also observed at the population level with quantitative data. In Fig. 1 we show mean GAD scores for young adults, with mean levels for older adults for comparison. We also include in the figure contextual information on the average number of daily deaths from COVID-19, and some of the key events from 2020.
Fig. 1.
Score on the HPS GAD anxiety scale; mean scores by age-group, with 95% confidence intervals. Shading represents average deaths per day; key dates and events are marked. Trend lines are fitted using local polynomial smoothing (all bandwidths set at 2).
We see evidence in Fig. 1 for volatility in levels of psychological distress over the course of 2020. Mean scores on the GAD scale show a small increase between April and July, and a subsequent decrease over the summer months. The fall and winter months see a gradual increase in mean GAD scores, exceeding the levels reached during the prior peaks. At all points in the time series, mean scores for young adults exceed those for older groups, although the gap between young and older adults increases after the summer months. The changes in mean GAD scores observed for the whole population align with the volatility highlighted in the qualitative interview data, although unfortunately, the first HPS wave was not administered until April 23rd, so we do not have quantitative measures of psychological distress for March and early-April, when AVP respondents noted feeling particularly distressed.
Changes in mean GAD scores by gender and race/ethnicity are included in the Appendix as figs.A4&A5. Similar results are found for the PHQ measure of depression (figs.A6-A8). We also include in the appendix details of an analysis based on a finer-grained measure of age-group (fig.A3). In this analysis, we find that there is variation within the 26-65-year-old age-group consistent with an age effect: older age-groups generally display lower GAD scores than younger groups. However, as the finer-grained measure of age produces less precise estimates, to preserve power for the regression analyses presented below we use the three-category age-group measure (the alternative measure of age-group is included in our OSF syntax).
3.2. Young adults’ reflections on the causes of their psychological distress
When prompted to consider the sources of their psychological distress, the responses from young adults in our AVP interview and MyVoice text-message data coalesced around a few key themes: concerns about health and risk from the virus, the economic and educational repercussions of the pandemic and profound social isolation, and a lack of reassurance that “someone is in charge” and that the virus will ultimately be defeated. We elaborate below on these three sources of worry by reviewing the distribution of the main themes found in the MyVoice text-message study (see Table 2 ).
Table 2.
Distribution of themes found in MyVoice text message study; no. (%) respondents mentioning theme, and representative direct quotations.a
| Theme | No. (%) | Representative quotation |
|---|---|---|
| What have you found most difficult about the COVID-19 pandemic? n = 575 | ||
| Health: | ||
| Own health | 13 (2.2) | The fear. I used to be really sick lung wise and I’d been healthy for less than six months when it started. Im barely rebuilding my life. Im terrified to be that sick again |
| Others’ health | 18 (3.1) | worrying about being asymptomatic and spreading covid around |
| Bad health behavior | 24 (4.2) | What’s the most difficult about the pandemic is people not taking precautions to keep them and others safe |
| Mental health/wellbeing | 57 (9.9) | A general feeling of hopelessness and that very little we do actually matters |
| Other health/virus concerns | 61 (10.6) | the fear of it spreading |
| Economy and education: | ||
| Economic and employment | 48 (8.4) | Honestly employment. I’ve never had a problem getting a job and now not a single company will get back to me |
| Education | 89 (15.5) | Studying remotely. Feeling lonely and no help |
| Other: | ||
| Lockdown restrictions | 129 (22.4) | Being stuck inside all the time with nothing to do and nowhere to go |
| Isolation and relationships | 221 (38.4) | Not socially hanging out with friends because I am alone and don't know where to start |
| Politics | 19 (3.3) | False info from trump |
| Uncertainty | 30 (5.2) | Not knowing what the future holds |
| Nothing | 10 (1.7) | Nothing really. Life is pretty normal |
| What are you most worried about as the pandemic continues? n = 536 | ||
| Health: | ||
| Own health | 60 (11.2) | Getting sick |
| Family’s health | 72 (13.4) | The safety of my family. It might not be as fatal in younger people but we can still get it and spread it to our parents. |
| Disease spread | 77 (14.4) | People not caring and more people dying |
| Bad health behavior | 31 (5.8) | I’m worried that no one is taking it seriously |
| Mental health/wellbeing | 37 (6.9) | myself going insane |
| Economy and education: | ||
| Economic recession | 41 (7.7) | i am most worried about the economy tanking |
| Own economic situation | 49 (9.1) | That I won’t be able to find work |
| Education | 41 (7.7) | Not experiencing college for what it’s supposed to be |
| Other: | ||
| Pandemic not ending | 103 (19.2) | I’m afraid that it won’t ever go away. |
| Isolation and lockdown | 55 (10.3) | Continued isolation |
| Politics | 34 (6.3) | political turmoil coming this Tuesday |
| Nothing | 15 (2.8) | literally nothing |
All messages are rendered with original spelling and punctuation. Numbers (%) do not add up to total no. (%), as messages can be coded into more than one theme.
In the MyVoice text-message data, the hardships of lockdown and isolation stood out as the most difficult experiences of the pandemic, while concerns about health and risk from the virus dominated the set of worries about the future. Although for each prompt a very small proportion of respondents reported that “nothing” about the pandemic was difficult or worrying, the vast majority of respondents identified one or more sources of concern.
With respect to the particular concerns raised in the MyVoice text-message study, worries about COVID-19 disease loomed large. The risk of serious disease associated with COVID-19 is relatively low for young adults (Marin et al., 2021), but many respondents shared worries about sickness in family, friends, and the general population. Notably, young adults expressed more concern about the health of others than about themselves. Similar responses were found in the AVP interview study, summarized in one young adult’s statement from October: “I’m terrified for my grandparents right now.” Concern about virus spread and empathy for others, then, was a prominent feature of both the interview and text-message data, despite negative media attention at the height of the pandemic that was focused on young adults’ “misbehavior” and “irresponsible” conduct (The New York Times, 2020).
When sharing fears about the future, our MyVoice text-message respondents were concerned about the consequences of a prolonged pandemic. Although virus mitigation efforts had been a source of difficulty – with around half of the sample identifying lockdown-related factors as their most difficult experience – when looking to the future, the large majority of our respondents pointed to the health and economic consequences of the pandemic not being brought under control. Just under a fifth of respondents shared concerns that the pandemic would never end, while others worried about continuing virus spread, a lack of mitigation practices, and continued economic distress. Notably, young people’s concerns were largely directed at the general public and leaders, with respondents variously observing, “nothing being done to help,” “people being stupid,” and “how many more people will die before trump gets his shit together.” AVP interviewees similarly described a loss of faith in politicians and fellow Americans, such as this young man interviewed in May:
“I would say that there is quite a significant amount of worry that I have just around the whole pandemic in general, based on how I see people treating the situation. It’s made me lose faith in a lot of Americans in general. That’s where the majority of my worry comes from.”
Both AVP interviewees and MyVoice text-message respondents expressed disbelief and disappointment that the pandemic had hit the United States so hard, and that there was not a robust policy response with respect to virus mitigation and ongoing economic support.
It is important to emphasize that we are here summarizing the main themes found in the responses. There was, of course, variation with respect to political attitudes in our samples. A handful of respondents expressed concerns that the pandemic was being taken too seriously by some. For example, our MyVoice text-message responses include, “I think the pandemic is a political move although I don’t the reasons though,” “Government abuse of powers, over valuing lives, infringements of my right to live and enjoy life, people being afraid of life’s natural cycles,” and “A false man made virus with the survivability of 99.99% taking away people’s rights and killing more due to lockdowns and mental issues than the amount of people the virus has directly killed” (all quotes presented as provided by respondents). But only around 1.5% of responses to the second text-message prompt expressed views of this type.
Alongside concerns about the health effects of the virus, both AVP interviewees and MyVoice text-message respondents shared concerns about the pandemic’s effects on education, employment, and finances. Around 40% of young adults are enrolled in postsecondary education (National Center for Education Statistics, 2020), so changes in educational provision during the pandemic have disproportionately affected young adults: just over 15% of our MyVoice text-message respondents found educational issues to be the most difficult issues that they had faced during the pandemic. Notably, however, while respondents recalled finding online schooling difficult, education was not of primary concern as young adults looked toward the future. As 2020 progressed, more and more AVP interviewees described economic pressure as a source of psychological distress. By the end of the year, those AVP interviewees without a secure income were in a desperate situation:
“I’m currently facing eviction. I’m about to lose my car. I supposed to be out of my place like five days ago, so I don’t have anywhere to go… I guess it don’t really matter what I do. It just doesn’t really matter anymore…I’m just at the end of my rope with everything.”
In our MyVoice text-message data, collected in November, around 15% of our sample identified economic concerns when asked what they were most worried about.
In highlighting the separate sources of distress in young adults it is important to emphasize that many young people were dealing with multiple problems. As one young woman recounted in an October AVP interview,
“Lately times have been getting really hard. My stepfather was laid off from work and we had two deaths in the family back-to-back from COVID-19 …. It’s really, really hard to keep afloat so that adds even more stress onto the stress that you’ve already had.”
Given the unequal distribution of COVID-19 and unemployment risks (Dyke, 2021; Grusky et al., 2021; Rossen, 2020), young people of color and those originating in poorer households were the most likely to have been contending with multiple stressors.
3.3. The association between psychological distress, virus rates, and government policy response
We have described volatility in rates of psychological distress over the course of 2020, and we have identified the sources of distress in the economic, health, and social consequences of the pandemic. Here, we use the HPS data to examine whether the volatility is associated with changes in virus risk and policy response. Based on the qualitative data, we hypothesize that psychological distress will be higher when the number of COVID-19 cases is higher (Holingue et al., 2020), and that a strong virus containment policy response will lead to reductions in distress.
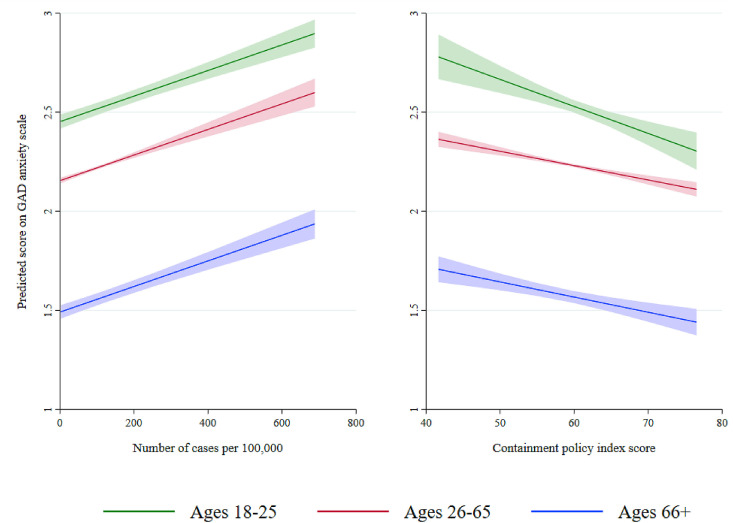
In Fig. 2 , we present predicted scores on the GAD anxiety scale for the three age-groups as a function of COVID-19 cases and policy response, with controls for a range of individual-level sociodemographic factors and state fixed effects. The predicted scores allow us to examine the effects of COVID-19 cases and policy response as their values change across the range observed in the data; the predicted values are calculated from the model outlined in “Material and methods,” and full model tables are presented in table.A1. In table.A2 we present a comparison of imputed and complete-case analyses; this analysis shows that the imputed analysis is conservative, and that the effects of policy response are stronger in the complete-case analysis.
Fig. 2.
Predicted scores on the HPS GAD anxiety scale by case counts and policy responsiveness, for the three age-groups, with 95% confidence intervals.
As COVID-19 cases rise in a state, mean GAD scores also rise. As we described in the methods section above, we found no evidence of interaction between age-group and COVID-19 cases: all age-groups see similar increases in mean GAD scores as COVID-19 cases rise. In contrast, we see evidence of interaction between age-group and containment policy response: GAD scores are more strongly associated with policy response in young adults than in older adults (for young adults, GAD b = -0.0137, s.e. 0.0027; interaction term for adults aged 26–65, GAD b = 0.0064, s.e. 0.0027). When state governments mount a strong response to the virus, mean GAD scores are lower, and age-group differences are markedly reduced. Weak government responses are associated with higher GAD scores, and larger age-group differences.
In additional models, we examined the components of the government policy response in greater detail. Our interest was in whether those policies that had been most difficult for young adults to bear – in particular, the lockdowns, restrictions on gathering, and school closings – were associated with higher levels of psychological distress. Rather, we find the opposite: stay-at-home requirements, restrictions on gatherings, and school closings are all negatively associated with mean GAD scores (see table.A3). The quantitative analyses, then, are consistent with the same dynamic that we saw in the AVP interview and MyVoice text-message data: young adults found COVID-19 mitigation strategies difficult, but at the same time, they yearned for an end to the pandemic and the economic and social disruption that accompanied it.
4. Discussion and conclusions
We have presented evidence on psychological distress in young adults during the COVID-19 pandemic. Our qualitative and quantitative data are consistent in revealing volatility in psychological distress over the course of 2020, and in revealing the sources of distress in the pandemic’s consequences for health, economic security, and diminished social interaction. Young adults expressed concern about the consequences of the pandemic continuing, and a substantial proportion feared that the pandemic would never end.
Strong COVID-19 containment policies at the state level were associated with lower levels of psychological distress for state residents, and this association was stronger for younger adults than for older adults. Taking the qualitative and quantitative findings together, our interpretation of this result is that stringent COVID-19 containment policy offered young adults two important sources of respite. First, the consequences of the pandemic for young adult lives were severe. Young adulthood is ordinarily a time of exploration and increased independence, but the pandemic reduced the opportunities for young people to benefit from these freedoms. Lockdowns, social distancing, and other containment measures were widely acknowledged as key sources of distress, and young adults expressed fears that the future would hold further restrictions on their freedom. However, they saw this risk to be higher if the pandemic were to proceed unchecked. Stringent containment policy was challenging for young adults to experience, but it held out the possibility that COVID-19 might be defeated, and that life would return to normal. Second, young adults interpreted the lack of a strong policy response as a signal that the pandemic was not being treated sufficiently seriously, and that no-one was in control of the situation. The signaling effect of implementing stringent COVID-19 containment policy may have been particularly strong for young adults, as young people routinely require increased reassurance and additional supports as they navigate the transition to independent adulthood (National Research Council, 2015).
Unfortunately, data constraints preclude a statistical test of the mechanisms underlying the association between COVID-19 containment policy and psychological distress. Our statistical analyses were conducted on observational, cross-sectional, survey data with a low response rate, and we must therefore exercise caution in imposing a causal interpretation on the statistical results. We must also acknowledge the very narrow focus of the HPS measures when compared against the rich and contextually-grounded descriptions in the qualitative data. Nevertheless, we do find a high degree of consistency between the expressed feelings of young adults in the MyVoice text-message and AVP interview data, and the patterns of association in the HPS data. Triangulation across data sources is helpful in confirming that similar findings arise via three different methodological approaches, and on three different samples of the U.S. young adult population.
COVID-19 containment policies have been the focus of both political contestation and public unrest. Although most American adults are broadly supportive of COVID-19 mitigation policies (Barry, Anderson, Han, Presskreischer, & McGinty, 2021; Gollust, 2021), these policies have largely been understood to be a “necessary evil” in the face of a dangerous threat to public health. Here, we find evidence consistent with positive mental health benefits of containment policies, particularly for young adults. Prior research has indicated that economic policies introduced during the pandemic reduced the psychological distress associated with unemployment and income shocks (Donnelly & Farina, 2021), and we similarly find that policies designed to buffer the economic impact of the pandemic are associated with lower levels of psychological distress. Nevertheless, our analysis demonstrates a negative association between mitigation policies and psychological distress that persists even after taking account of changes in economic policy.
Strong partisan differences in response to COVID-19 containment policy have been a feature of recent political discourse at both the state and federal levels (Gollust, 2021; Parmet & Paul, 2020). One potential explanation for why young adults have had generally positive responses to containment policy is that young adults are substantially more likely to support the Democratic party than older adults (Center for Information and Research on Civic Learning & Engagement, 2020). Unfortunately, the HPS does not include a measure capturing political partisanship, which would have allowed us to test this hypothesis. But it is important to consider whether stringent COVID-19 mitigation policies would have still been associated with reduced psychological distress had President Trump been enthusiastically promoting such policies, in the face of opposition from Democratic politicians. This counterfactual is, of course, unobservable, but our qualitative evidence would suggest that young adults saw a stringent policy response as offering a route out of the pandemic, and that this policy benefit would obtain regardless of which party was responsible for promoting the response.
As the country’s attention turns to recovery, it will be important to acknowledge the distress that young adults have experienced during the pandemic, and put supports into place that will promote mental wellbeing. Young people have a high degree of resilience, but there is a clear danger that the psychological distress experienced during the pandemic might have longer-lasting effects. In analyzing the qualitative data it is hard to avoid the conclusion that many young adults felt that they had missed out on opportunities that will never be repeated, and that they were let down by their governments and compatriots. Acknowledging those losses, and rebuilding trust, will be important in this period of recovery. While statewide COVID-19 mitigation strategies were not targeted towards young adults specifically, the unintended benefits for mental health warrant further consideration of policy levers that can support strong mental health during critical points of the life-course.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We thank the American Voices Project team for access to the interview data reported in this study, and Tammy Chang, Marika Waselewski, and the MyVoice team for collaboration on the text-message study. We thank David Cox and David Grusky for useful comments on an earlier version of this paper. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmmh.2021.100027.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Alexander J.T., Andersen R., Cookson P.W., Edin K., Fisher J., Grusky D.B., et al. A qualitative Census of rural and urban poverty. The Annals of the American Academy of Political and Social Science. 2017;672:143–161. doi: 10.1177/0002716217714156. [DOI] [Google Scholar]
- Aminoff V., Sellén M., Sörliden E., Ludvigsson M., Berg M., Andersson G. Internet-based cognitive behavioral therapy for psychological distress associated with the COVID-19 pandemic: A pilot randomized controlled trial. Frontiers in Psychology. 2021;12 doi: 10.3389/fpsyg.2021.684540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry C.L., Anderson K.E., Han H., Presskreischer R., McGinty E.E. Change over time in public support for social distancing, mask wearing, and contact tracing to combat the COVID-19 pandemic among US adults, April to November 2020. American Journal of Public Health. 2021;111:937–948. doi: 10.2105/AJPH.2020.306148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartelink V.H.M., Zay Ya K., Guldbrandsson K., Bremberg S. Unemployment among young people and mental health: A systematic review. Scandinavian Journal of Public Health. 2020;48:544–558. doi: 10.1177/1403494819852847. [DOI] [PubMed] [Google Scholar]
- Birditt K.S., Turkelson A., Fingerman K.L., Polenick C.A., Oya A. Age differences in stress, life changes, and social ties during the COVID-19 pandemic: Implications for psychological well-being. The Gerontologist. 2021;61:205–216. doi: 10.1093/geront/gnaa204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlo F.D., Sociali A., Picutti E., Pettorruso M., Vellante F., Verrastro V., et al. Telepsychiatry and other cutting-edge technologies in COVID-19 pandemic: Bridging the distance in mental health assistance. International Journal of Clinical Practice. 2021;75 doi: 10.1111/ijcp.13716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Census Bureau . 2020. 2020 Household Pulse Survey. Interagency federal statistical rapid response survey to measure effects of the Coronavirus (COVID-19) pandemic on the United States household population. [Google Scholar]
- Census Bureau . 2020. https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/Source-and-Accuracy-Statement-July-16-July-21.pdf (Source of the data and accuracy of the estimates for the 2020 Household Pulse Survey). [Google Scholar]
- Center for Information and Research on Civic Learning & Engagement . 2020. Election week 2020: Young people increase turnout, lead Biden to Victory.https://circle.tufts.edu/latest-research/election-week-2020 [WWW Document]. URL. accessed 6.7.21. [Google Scholar]
- Creswell J.W., Creswell J.D. 5th ed. SAGE Publications, Inc; Los Angeles: 2018. Research design: Qualitative, quantitative, and mixed methods approaches. [Google Scholar]
- Czeisler M.É. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Sutin A.R., Robinson E. Depression reported by US adults in 2017–2018 and March and April 2020. Journal of Affective Disorders. 2021;278:131–135. doi: 10.1016/j.jad.2020.09.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeJonckheere M., Nichols L.P., Moniz M.H., Sonneville K.R., Vydiswaran V.V., Zhao X., et al. MyVoice national text message survey of youth aged 14 to 24 Years: Study protocol. JMIR Research Protocols. 2017;6 doi: 10.2196/resprot.8502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly R., Farina M.P. How do state policies shape experiences of household income shocks and mental health during the COVID-19 pandemic? Social Science & Medicine. 2021;269:113557. doi: 10.1016/j.socscimed.2020.113557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyke M.E.V. Racial and ethnic disparities in COVID-19 incidence by age, sex, and period among persons aged 25 Years — 16 U.S. Jurisdictions, January 1–December 31, 2020. MMWR Morb Mortal Wkly Rep. 2021;70 doi: 10.15585/mmwr.mm7011e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellwardt L., Präg P. Heterogeneous mental health development during the COVID-19 pandemic in the United Kingdom. Scientific Reports. 2021;11:15958. doi: 10.1038/s41598-021-95490-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish J.N., McInroy L.B., Paceley M.S., Williams N.D., Henderson S., Levine D.S., et al. “I’m kinda stuck at home with unsupportive parents right now”: LGBTQ youths’ experiences with COVID-19 and the importance of online support. Journal of Adolescent Health. 2020;67:450–452. doi: 10.1016/j.jadohealth.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freese J., Johnson A.L., Garcia M. Stanford Center on Poverty&Inequality; 2021. ‘What’s weighing heaviest’ Indirect health consequences of the Covid-19 crisis.https://inequality.stanford.edu/sites/default/files/research/articles/covid-indirect-health-consequences.pdf [Google Scholar]
- Ganson K.T., Tsai A.C., Weiser S.D., Benabou S.E., Nagata J.M. Job insecurity and symptoms of anxiety and depression among U.S. young adults during COVID-19. Journal of Adolescent Health. 2021;68:53–56. doi: 10.1016/j.jadohealth.2020.10.008. [DOI] [PubMed] [Google Scholar]
- Gerson K., Damaske S. 1st ed. Oxford University Press; New York: 2020. The science and art of interviewing. [Google Scholar]
- Giuntella O., Hyde K., Saccardo S., Sadoff S. Lifestyle and mental health disruptions during COVID-19. Proceedings of the National Academy of Sciences. 2021;118 doi: 10.1073/pnas.2016632118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein E., Wen H., Miller B.F. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174:819. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Gollust S.E. Partisan and other gaps in support for COVID-19 mitigation strategies require substantial attention. American Journal of Public Health. 2021;111:765–767. doi: 10.2105/AJPH.2021.306226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grusky D.B., Carpenter A., Graves E., Kallschmidt A., Mitnik P., Nichols B., et al. Stanford Center on Poverty&Inequality; 2021. The rise of the noxious contract. Job safety in the Covid-19 crisis.https://inequality.stanford.edu/sites/default/files/research/articles/covid-noxious-contract.pdf [Google Scholar]
- Gu A., Yoo H.I. Social Science Research Network; Rochester, NY: 2019. Vcemway: A one-stop solution for robust inference with multi-way clustering (SSRN scholarly paper No. ID 3409489) [DOI] [Google Scholar]
- Hale T., Angrist N., Goldszmidt R., Kira B., Petherick A., Phillips T., et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker) Nature Human Behaviour. 2021:1–10. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- Harvey A.G., Gumport N.B. Evidence-based psychological treatments for mental disorders: Modifiable barriers to access and possible solutions. Behaviour Research and Therapy. 2015;68:1–12. doi: 10.1016/j.brat.2015.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holingue C., Kalb L.G., Riehm K.E., Bennett D., Kapteyn A., Veldhuis C.B., et al. Mental distress in the United States at the beginning of the COVID-19 pandemic. American Journal of Public Health. 2020;110:1628–1634. doi: 10.2105/AJPH.2020.305857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland K.M., Jones C., Vivolo-Kantor A.M., Idaikkadar N., Zwald M., Hoots B., et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry. 2021;78:372–379. doi: 10.1001/jamapsychiatry.2020.4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyt L.T., Cohen A.K., Dull B., Maker Castro E., Yazdani N. “Constant stress has become the new normal”: Stress and anxiety inequalities among U.S. College students in the time of COVID-19. Journal of Adolescent Health. 2021;68:270–276. doi: 10.1016/j.jadohealth.2020.10.030. [DOI] [PubMed] [Google Scholar]
- Hu Y., Qian Y. COVID-19 and adolescent mental health in the United Kingdom. Journal of Adolescent Health. 2021;69:26–32. doi: 10.1016/j.jadohealth.2021.04.005. [DOI] [PubMed] [Google Scholar]
- Jackson M., Lee Williams J., Dahir N., Edelman A. Stanford Center on Poverty&Inequality; 2021. Having to stay still. Youth and young adults in the Covid-19 crisis.https://inequality.stanford.edu/sites/default/files/research/articles/Covid-Youth-Young-Adults.pdf [Google Scholar]
- Lee C.M., Cadigan J.M., Rhew I.C. Increases in loneliness among young adults during the COVID-19 pandemic and association with increases in mental health problems. Journal of Adolescent Health. 2020;67:714–717. doi: 10.1016/j.jadohealth.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little R.J.A. A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association. 1988;83:1198–1202. doi: 10.1080/01621459.1988.10478722. [DOI] [Google Scholar]
- Marin B.G., Aghagoli G., Lavine K., Yang L., Siff E.J., Chiang S.S., et al. Predictors of COVID-19 severity: A literature review. Reviews in Medical Virology. 2021;31:e2146. doi: 10.1002/rmv.2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MyVoice Transparency | MyVoice. 2020. https://hearmyvoicenow.org/research/transparency/ URL. accessed 9.24.21.
- Nagata J.M., Ganson K.T., Bonin S.L., Twadell K.L., Garcia M.E., Langrock O., et al. 2021. Prevalence and sociodemographic correlates of unmet need for mental health counseling among adults during the COVID-19 pandemic Psychiatric Services. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagata J.M., Ganson K.T., Whittle H.J., Chu J., Harris O.O., Tsai A.C., et al. Food insufficiency and mental health in the U.S. during the COVID-19 pandemic. American Journal of Preventive Medicine. 2021;60:453–461. doi: 10.1016/j.amepre.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagata J.M., Palar K., Gooding H.C., Garber A.K., Whittle H.J., Bibbins-Domingo K., et al. Food insecurity is associated with poorer mental health and sleep outcomes in young adults. Journal of Adolescent Health. 2019;65:805–811. doi: 10.1016/j.jadohealth.2019.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine . The National Academies Press; Washington, DC: 2019. The promise of adolescence: Realizing opportunity for all youth. [DOI] [PubMed] [Google Scholar]
- National Center for Education Statistics . 2020. The condition of education 2020.https://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2020144 [WWW Document]. URL. accessed 3.13.21. [Google Scholar]
- National Research Council . National Academies Press (US); Washington (DC): 2015. Investing in the health and well-being of young adults. [PubMed] [Google Scholar]
- Parmet W.E., Paul J. COVID-19: The first posttruth pandemic. American Journal of Public Health. 2020;110:945–946. doi: 10.2105/AJPH.2020.305721. [DOI] [Google Scholar]
- Peterson S., Toribio N., Farber J., Hornick D. 2021. Nonresponse bias report for the 2020 Household Pulse Survey. [Google Scholar]
- Rogers A.A., Ha T., Ockey S. Adolescents’ perceived socio-emotional impact of COVID-19 and implications for mental health: Results from a U.S.-based mixed-methods study. Journal of Adolescent Health. 2021;68:43–52. doi: 10.1016/j.jadohealth.2020.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossen L.M. Excess deaths associated with COVID-19, by age and race and ethnicity — United States, January 26–October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6942e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spera S., Monnat S. Syracuse University Lerner Center for Public Health Promotion; 2020. Adolescent and young adult mental health is better in states that mandate more school mental health policies. [Google Scholar]
- Stanford Center on Poverty and Inequality American Voices Project methodology - Stanford Center on Poverty & Inequality. 2021. https://inequality.stanford.edu/avp/methodology [WWW Document]. URL. accessed 9.16.21.
- Tetreault E., Teferra A.A., Keller-Hamilton B., Shaw S., Kahassai S., Curran H., et al. Perceived changes in mood and anxiety among male youth during the COVID-19 pandemic: Findings from a mixed-methods study. Journal of Adolescent Health. 2021;69:227–233. doi: 10.1016/j.jadohealth.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The New York Times . 2020. Colleges try and fail to stop campus partying to slow Covid spread. [Google Scholar]
- The New York Times . 2021. Coronavirus (Covid-19) data in the United States. [Google Scholar]
- Vahratian A. Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID-19 pandemic — United States, August 2020–February 2021. MMWR Morb Mortal Wkly Rep. 2021;70 doi: 10.15585/mmwr.mm7013e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waselewski E.A., Waselewski M.E., Chang T. Needs and coping behaviors of youth in the U.S. during COVID-19. Journal of Adolescent Health. 2020;67:649–652. doi: 10.1016/j.jadohealth.2020.07.043. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.