Abstract
Global trends in the incidence and mortality rates of colorectal cancer show a steady increase with significant predilection to western developed countries, possibly linking it to westernized lifestyles among other risk factors. This study aims to investigate the incidence and trends of colorectal cancer in Lebanon, a country in the Middle East and North Africa region, and to compare these rates to those in regional and western countries. Colorectal cancer incidence data were extracted from the Lebanese National Cancer Registry for the currently available years 2005 to 2016. The calculated age-standardized incidence rates and age-specific rates were expressed as per 100,000 population. The age-standardized incidence rates of colorectal cancer in Lebanon increased from 16.3 and 13.0 per 100,000 in 2005 to 23.2 and 20.2 per 100,000 in 2016, among males and females, respectively. The incidences were higher for males, and they increased with age. The annual percent change was +4.36% and +4.45%, in males and females respectively (p-value < 0.05). There was a non-statistically significant trend of decrease in recent years (since 2012 in males and since 2011 in females). The age-standardized incidence rates in Lebanon were higher than those in the majority of the regional countries, but lower than the rates in developed western countries. There were high age-specific incidence rates at age groups 40-44 and 45-49 years in Lebanon in both males and females (with significant rising temporal trend) compared to other countries, including the ones reported to have the highest colorectal cancer age-standardized incidence rate worldwide. Therefore, the burden of colorectal cancer is significant in Lebanon. This raises the necessity to develop national strategies tailored to reduce colorectal cancer incidence through promoting healthy lifestyles, raising awareness, and early detection as of 40 years of age.
Keywords: colorectal cancer, epidemiology, incidence, cancer Prevention, risk factors, cancer screening
Introduction
Colorectal cancer (CRC) is the third most commonly diagnosed cancer in men and the second in women globally, with an increasing incidence reaching over 1.8 million new cases in 2018 (10.2% of all new cancer cases) as compared to 1.4 million in 2012.1,2 CRC is also the fourth most common cause of cancer-related mortality in both sexes worldwide, leading to around 880,792 deaths in 2018 (9.2% of all cancer-related deaths).1,2 The projected age-standardized incidence rate among the world population (ASRw) per 100,000 person-years was reported to be 19.7 in 2018 with higher rates among males (23.6 in 2018) as compared to females (16.3 in 2018).1 The global trend in the incidence of CRC shows a steady increase in the incidence rates with significant geographic variation.1,3 The estimated incidence of CRC in 2018 is reported to be the highest in countries with a high or very high human development index (HDI) such as parts of Europe (Hungary, Slovakia, Slovenia, The Netherlands, and Norway), Australia, New Zealand, Northern America, and Eastern Asia (Japan and South Korea).1
The epidemiology of CRC and the current evidence suggest that its pathogenesis is not only genetic or hereditary, but it is also strongly linked to western lifestyles with risk factors including diet rich in processed meat and red meat, alcohol consumption, lack of physical activity, excess body fat and smoking.3-6 This link suggests that the incidence of CRC would continue to increase in westernized developing countries, adding more burden on governments.
Lebanon is a small developing country in the Middle East (population ≈ 6 million in 2016) with health indices close to the western world.7 CRC is one of the most prevalent cancers in both sexes, and it accounted for 8.9% and 8.6% of cancer-related mortality in males and females, respectively in 2014.8 The national cancer registry (NCR) was officially restarted in 2002 in the country, after several years of being inactive due to war. This registry is believed to be an almost absolute count of all incident cases in Lebanon with data capture and recapture systems, i.e. data collected passively from physicians’ reports (capture system) and actively from histopathological and hematological laboratories (recapture system).9 The recapture system validates and complements the capture approach.10 The NCR covers more than 90% of cancer cases in Lebanon,9 excluding in situ lesions. The NCR publishes its cancer incidence data on the official website of the Ministry of Public Health (MoPH); the currently available data covers the period extending from 2005 to 2016.10
This study aims to analyze the 12-year incidence rates and temporal trends for CRC in Lebanon and to compare these rates to the ones in the Middle East and North Africa (MENA) region, as well as to the rates in Western and Eastern countries. This study will also discuss the different factors leading to increased CRC incidence and conclude with practice and policy recommendations.
Materials & Methods
Twelve-Year Trend Analysis From 2005 Until 2016
In this study, CRC data include all codes from C18 to C21 in the International Classification of Diseases, tenth revision (ICD-10). The age-standardized (ASRw) and the age-specific incidence rates, expressed per 100,000 population, were calculated based on figures published by the Lebanese NCR on the MoPH website10 for 12 consecutive years from 2005 to 2016. The age-standardized incidence rate is a weighted average of the age-specific incidence rates per 100,000 persons, where the weights are the proportions of persons in the corresponding age groups of a standard population. Standardization is essential when comparing different populations with different age structures. The most commonly used standard population is the world standard population, which is drawn from a pooled population of several countries. In this study, the age-standardized incidence rate was computed using the modified world standard population by Doll as the reference population.11 The age-specific incidence rate is the number of new cancer cases occurring during a specific period, in a population of a specific age and sex group, divided by the number of mid-year population of that age and sex group.12
Stratified by sex, the annual percent change (APC) and the average annual percent change (AAPC) of CRC incidence rates over the years were computed using the joinpoint regression program (JRP) 4.7.0.0 with a statistical significance level defined at p-value < 0.05. The APC is based on the hypothesis that cancer rates change at a constant percentage of the previous year’s rate.13
Comparison of Trends Between Sexes
Trend variations in CRC ASRw between sexes were compared using 2 tests, parallelism and coincidence. Parallelism determines if the 2 regression mean functions are parallel allowing different intercepts and examines the similarity in their direction (i.e., the slope of trend’s change) between males and females, while coincidence determines whether 2 joinpoint regression mean functions are identical (i.e., similar overall incidence) between males and females.13
Projections of the CRC Incidence in Lebanon for the Year 2025
Projections were estimated using the currently available CRC data over the 12 years (2005-2016). Linear and log-linear regression models were found to be the best fit models in this study (almost similar), and they were used to estimate the future patterns of cancer incidence. These 2 models, which assume a Poisson distribution for the observed number of incident cases, have been reported to be the most practical methods that can be used to estimate future patterns of cancer incidence for periods of up to 10 years while assuming that there is no change in underlying trends.14,15
The new sex and CRC incidence coefficients were generated, along with the forecasted incidence and the corresponding lower and upper confidence limits (LCL and UCL). R square and p-value were used to assess the goodness-of-fit of the model. The R square permits to measure how well the model explains the total variations and a p-value less than 0.05 is considered significant.
Comparison to Regional and Western Countries
The calculated ASRw and age-specific rates were subsequently compared with age-standardized and age-specific incidence rates from selected regional, Western, and Eastern countries as published online in Cancer Incidence in Five Continents Time Trends (CI5plus),16 Cancer Incidence in Five Continents Volume XI (CI5 XI),11,17 or from the Country National Cancer Registry.18-24 The rates mentioned in CI5plus and CI5 XI are built on high-quality population-based cancer registries. For comparison, we included countries that surround Lebanon geographically, as well as randomly selected countries from the MENA region and other Western and Eastern countries.
Results
Incidence Trends (2005-2016) and Average Annual Percent Change (AAPC)
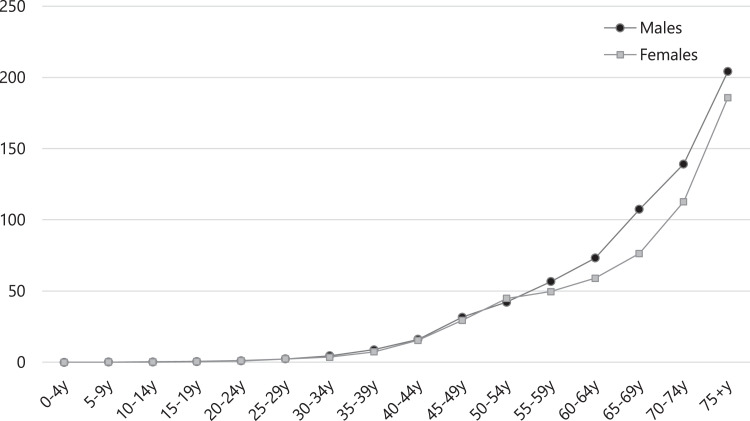
In Lebanon, CRC was found to be the fourth and second most common cancer in males (after prostate, lung and trachea, and bladder) and females (after breast) respectively, over the studied 12-year period (2005-2016). A total of 10284 incident cases of CRC were reported during this period, with 53% of cases being in males (5450 cases) and 77.4% occurring in patients aged 50 years and above (7959 cases). The average number of new CRC cases per year was 454 in males and 403 in females. The age-specific incidence rate was found to increase with age in both sexes, reaching its maximum in the age group 75 years and above (Figure 1).
Figure 1.
Age-specific incidence rates (per 100,000 population) for colorectal cancer, Lebanon 2005-2016. Source: Lebanese Ministry of Public Health, Epidemiological Surveillance Program, National Cancer Registry, 2020.
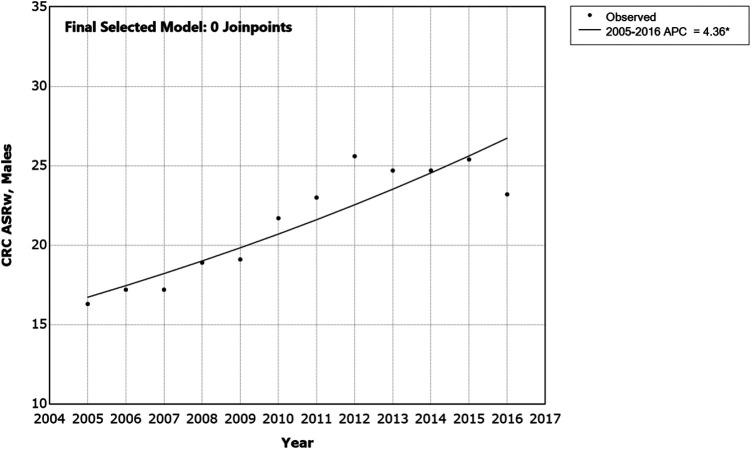
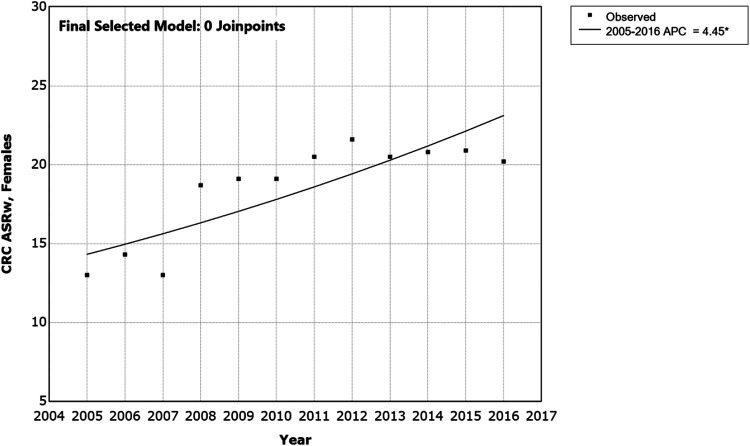
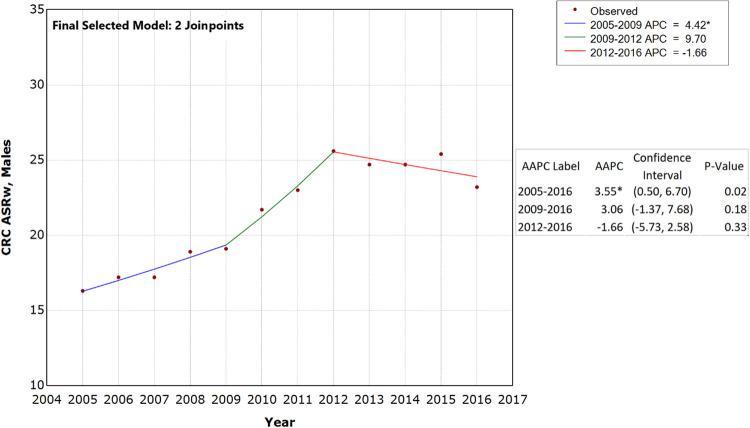
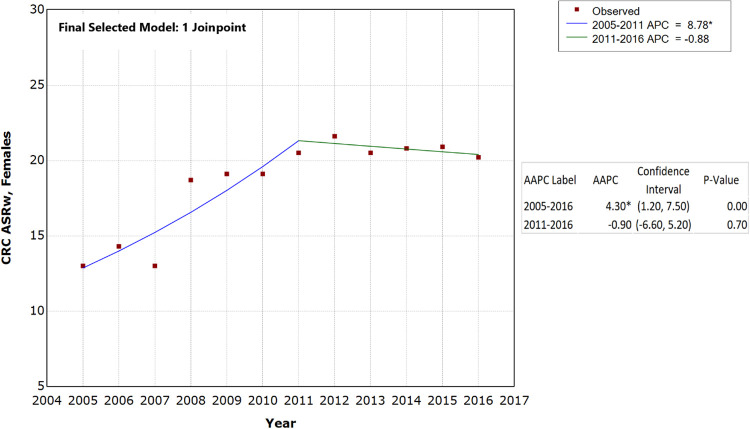
Stratified by sex, the APC and AAPC were computed to reflect the trends in CRC rates over the 12-year study period in general and in each age group (Tables 1 and 2). With 0 joinpoint models, which is a straight line indicating the minimum number of joinpoints, the APC (equal to AAPC) of CRC was +4.36% (p-value < 0.05) and + 4.45% (p-value < 0.05) in males and females respectively (Figures 2 and 3), and significantly different than zero. With 2 joinpoints model in males and 1 joinpoint model in females, the AAPC of CRC was +3.55% (P < 0.05) and + 4.30% (P < 0.05) in males and females respectively (Figures 4 and 5). There was a non-statistically significant trend of decrease in recent years (since 2012 in males and 2011 in females). The age-standardized incidence rates of CRC over the past years were higher in males than females (including the average ASRw), however the increasing trends were slightly but significantly higher in females than males.
Table 1.
CRC Age-Specific Rates’ Trend Analysis in Males by Age Group per Year—Lebanon (2005-2016).
| Year | ASRw^ | Age-Specific Rates (per 100,000) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0-4y | 5-9y | 10-14y | 15-19y | 20-24y | 25-29y | 30-34y | 35-39y | 40-44y | 45-49y | 50-54y | 55-59y | 60-64y | 65-69y | 70-74y | 75+y | ||
| 2005 | 16.3 | 0 | 0 | 0.5 | 0.5 | 2 | 2.7 | 5.5 | 8.8 | 13.3 | 15.2 | 31.6 | 48.3 | 73.0 | 81.2 | 89.1 | 128.5 |
| 2006 | 17.2 | 0 | 0 | 0 | 0.5 | 0 | 2.5 | 2.0 | 5.6 | 14.7 | 19.0 | 30.0 | 50.4 | 55.1 | 88.2 | 71.4 | 230.7 |
| 2007 | 17.2 | 0 | 0 | 0 | 1.0 | 2 | 1.9 | 7.1 | 6.7 | 6.5 | 19.8 | 35.3 | 60.2 | 74.2 | 78.9 | 101.4 | 141.9 |
| 2008 | 18.9 | 0 | 0 | 0 | 0.5 | 1.5 | 0.6 | 3.2 | 10.5 | 11.7 | 29.7 | 34.4 | 48.4 | 50.1 | 82.0 | 139.9 | 216.2 |
| 2009 | 19.1 | 0 | 0 | 0 | 0 | 0.5 | 1.6 | 6.6 | 6.9 | 12.6 | 30.1 | 43.2 | 64.1 | 54.1 | 90.7 | 120.2 | 179.4 |
| 2010 | 21.7 | 0 | 0 | 0 | 0 | 1.5 | 1.8 | 4.9 | 7.0 | 18.8 | 34.4 | 36.9 | 69.5 | 75.3 | 111.2 | 152.2 | 177.6 |
| 2011 | 23.0 | 0 | 0 | 0.4 | 0 | 1.0 | 2.3 | 5.5 | 11.5 | 18.5 | 35.0 | 43.5 | 42.0 | 88.1 | 117.8 | 157.0 | 214.5 |
| 2012 | 25.6 | 0 | 0 | 0 | 1.8 | 1.0 | 3.9 | 3.6 | 9.8 | 22.8 | 53.2 | 57.1 | 52.9 | 88.0 | 128.2 | 144.8 | 214.2 |
| 2013 | 24.7 | 0 | 0 | 0.7 | 0 | 0.4 | 3.5 | 2.6 | 5.9 | 17.7 | 46.7 | 45.8 | 67.0 | 56.9 | 135.4 | 177.9 | 247.0 |
| 2014 | 24.7 | 0 | 0.6 | 0 | 0.7 | 0.8 | 2.6 | 5.6 | 12.4 | 22.0 | 27.3 | 44.7 | 59.6 | 81.1 | 153.9 | 161.6 | 231.5 |
| 2015 | 25.4 | 0 | 0 | 0 | 1.4 | 1.2 | 3.3 | 3.1 | 10.3 | 14.8 | 33.3 | 57.2 | 60.4 | 99.6 | 127.0 | 171.3 | 244.6 |
| 2016 | 23.2 | 0 | 0 | 0.3 | 0 | 1.2 | 1.4 | 3.8 | 10.6 | 19.6 | 35.3 | 47.1 | 55.9 | 81.6 | 92.9 | 183.3 | 224.2 |
| APC | 4.36* | . | . | . | . | . | 8.41 | −2.89 | 2.37 | 5.98 | 6.67* | 9.34* | 2.88 | 1.43 | 4.55* | 2.9 | 5.97* |
^ASRw: Age Standardized Rate (world); * APC significantly different from zero.
Table 2.
CRC Age-Specific Rates’ Trend Analysis in Females by Age Group per Year—Lebanon (2005-2016).
| Year | ASRw^ | Age-Specific Rates (per 100,000) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0-4y | 5-9y | 10-14y | 15-19y | 20-24y | 25-29y | 30-34y | 35-39y | 40-44y | 45-49y | 50-54y | 55-59y | 60-64y | 65-69y | 70-74y | 75+y | ||
| 2005 | 13.0 | 0 | 0.6 | 0 | 0.5 | 2.1 | 1.2 | 4.0 | 4.7 | 13.5 | 14.8 | 18.1 | 35.3 | 59.4 | 49.7 | 94.9 | 111.8 |
| 2006 | 14.3 | 0 | 0 | 0 | 0.5 | 0.5 | 0.6 | 6.0 | 6.6 | 6.7 | 19.1 | 30.1 | 49.0 | 53.1 | 63.7 | 89.0 | 140.8 |
| 2007 | 13.0 | 0 | 0 | 0 | 1.2 | 1.6 | 3.0 | 2.0 | 6.1 | 10.7 | 18.5 | 29.4 | 37.9 | 55.6 | 49.1 | 63.5 | 103.7 |
| 2008 | 18.7 | 0 | 0 | 0 | 0 | 1.0 | 2.2 | 3.4 | 11.5 | 9.7 | 35.6 | 32.3 | 48.1 | 50.2 | 80.0 | 148.9 | 181.8 |
| 2009 | 19.1 | 0 | 0.5 | 0 | 0.5 | 0 | 1.6 | 2.8 | 2.8 | 15.5 | 28.5 | 68.5 | 39.6 | 57.9 | 70.8 | 112.8 | 214.3 |
| 2010 | 19.1 | 0 | 0 | 0 | 0 | 0.5 | 1.6 | 6.6 | 6.9 | 12.6 | 30.1 | 43.2 | 64.1 | 54.1 | 90.7 | 120.2 | 179.4 |
| 2011 | 20.5 | 0 | 0 | 0 | 0 | 0.5 | 2.6 | 2.7 | 11.5 | 21.6 | 26.5 | 34.3 | 66.7 | 66.9 | 85.5 | 102.0 | 243.6 |
| 2012 | 21.6 | 0 | 0 | 0 | 0 | 0.5 | 3.0 | 4.2 | 6.7 | 26.9 | 40.5 | 49.9 | 48.6 | 67.0 | 78.5 | 152.6 | 211.1 |
| 2013 | 20.5 | 0 | 0 | 0 | 0.4 | 1.2 | 4.4 | 1.9 | 6.6 | 18.5 | 42.1 | 49.8 | 49.5 | 46.6 | 105.7 | 105.4 | 215.4 |
| 2014 | 20.8 | 0 | 0.3 | 1.0 | 0.4 | 1.5 | 2.4 | 3.3 | 9.0 | 18.7 | 31.0 | 56.9 | 46.8 | 70.8 | 75.2 | 143.1 | 199.5 |
| 2015 | 20.9 | 0 | 0 | 0 | 0 | 0.4 | 2.6 | 2.8 | 7.8 | 18.9 | 39.4 | 64.3 | 51.0 | 57.9 | 83.7 | 106.3 | 215.6 |
| 2016 | 20.2 | 0 | 0 | 0 | 1.1 | 1.5 | 2.0 | 3.2 | 5.7 | 11.2 | 26.9 | 59.6 | 58.2 | 67.0 | 82.9 | 113.3 | 212.4 |
| APC | 4.45* | . | . | . | . | . | 3.27 | –1.57 | 3.74 | 6.01* | 7.45* | 5.12* | 1.31 | 3.35 | 4.67* | 7.57* | 4.09* |
^ASRw: Age Standardized Rate (world); * APC significantly different from zero.
Figure 2.
Age Standerized Incidence Rates (ASRw) for Colorectal Cancer (CRC) in Males, Lebanon 2005-2016. *Indicates that the Annual Percent Change (APC) is significantly different from zero at the alpha = 0.05 level.
Figure 3.
Age Standerized Incidence Rates (ASRw) for Colorectal Cancer (CRC) in Females, Lebanon 2005-2016. *Indicates that the Annual Percent Change (APC) is significantly different from zero at the alpha = 0.05 level.
Figure 4.
Age Standerized Incidence Rates (ASRw) for Colorectal Cancer (CRC) in Males, Lebanon 2005-2016. *Indicates that the Annual Percent Change (APC) or Average APC(AAPC) is singnificantly different from Zero at the alpha = 0.05 level.
Figure 5.
Age Standerized Incidence Rates (ASRw) for Colorectal Cancer (CRC) in Females, Lebanon 2005-2016. *Indicates that the Annual Percent Change (APC) or Average APC(AAPC) is singnificantly different from Zero at the alpha = 0.05 level.
The p-value on the parallelism test was > 0.05 (p-value: 0.88), indicating that the trends’ slopes between males and females are not significantly different. However, the p-value on the coincidence test was < 0.05 (p-value < 0.001), indicating that the difference in the rates (position of trend lines) between males and females is significantly different (higher in females).
Projected CRC Rates in 2025
Employing linear-regression models, the ASRw of CRC in 2025 is expected to approach 28.8 (LCL:19.2, UCL: 38.5) cases per 100,000 males and 26.1 (LCL: 13.4, UCL: 38.8) cases per 100,000 for females. The R squares showed that the best-fitted models (R2 ≥ 0.8) were in males (R2 = 0.81; p-value <0.001) and to a lesser extent in females (R2 = 0.71; p-value: 0.001).
Comparison to Regional and Western Countries
The CRC ASRw among males in Lebanon (25.6 in 2012 and 21.4 in 2005-2016) was found to be much higher than that in other MENA countries except for Israeli Jews and Non-Jews, while it was lower than the rates recorded in France and the United States of America (USA), and significantly lower than in countries with the highest rates of CRC among males in 2018 (i.e., South Korea and Slovakia) (Table 3).
Table 3.
CRC ASRw and Age-Specific Rates in Males—Lebanon Compared to MENA and non-MENA Countries.
| Country | Year(s) | Annual Incidence per 100,000 by Age Group: Males | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ASRw^ | 20-24y | 25-29y | 30-34y | 35-39y | 40-44y | 45-49y | 50-54y | 55-59y | 60-64y | 65-69y | 70-74y | 75+y | |||
| MENA Countries | Lebanon | 2012 | 25.6 | 1.0 | 3.9 | 3.6 | 9.8 | 22.8 | 53.2 | 57.1 | 52.9 | 88.0 | 128.2 | 144.8 | 214.2 |
| Israeli Non-Jews | 2012 | 31.6 | 1.2 | – | 5.8 | 11.6 | 18.4 | 13.6 | 37.2 | 78.1 | 102.9 | 242.9 | 252.5 | 350.6 | |
| Israeli Jews | 2012 | 33.5 | – | 1.8 | 5.3 | 7.5 | 7.6 | 27.4 | 47.0 | 70.1 | 136.4 | 185.0 | 294.4 | 416.3 | |
| Algeria (Setif) | 2008-2011 | 10.7 | 1.9 | 1.8 | 4.3 | 5.9 | 10.2 | 6.6 | 22.6 | 31.4 | 43.4 | 62.9 | 72.4 | 57.8 | |
| Algeria (Batna) | 2008-2012 | 9.6 | 1.5 | 1.5 | 4.6 | 4.0 | 7.1 | 13.9 | 21.8 | 21.5 | 50.5 | 43.4 | 60.4 | 54.6 | |
| Jordan | 2012 | 16.1 | 0.3 | 1.3 | 3.9 | 7.1 | 11.0 | 22.0 | 32.2 | 35.8 | 56.8 | 97.1 | 116.0 | 135.5 | |
| Minia Governorate, Egypt, | 2009 | 5.5 | 2.2 | 1.7 | 6.4 | 4.0 | 4.8 | 9.0 | 16.7 | 10.2 | 34.7 | 10.4 | 21.3 | 17.6 | |
| Aswan Governorate, Egypt, | 2010 | 4.8 | 1.4 | 1.8 | 4.6 | 2.4 | – | 3.2 | – | 20.7 | 20.3 | 26.1 | 34.8 | 34.7 | |
| Damietta Governorate, Egypt | 2012 | 7.6 | 1.5 | 1.9 | – | 2.3 | 5 | 5.8 | 24.5 | 37.5 | 36.7 | 18 | 43.5 | 47.7 | |
| Kuwait | 2012 | 21.9 | – | 3.7 | – | 4.7 | 5 | 9 | 24.5 | 58.2 | 57 | 44.1 | 78.3 | 82.4 | |
| Saudi Arabia | 2013 | 11.9 | 0.8 | 1.2 | 4.0 | 3.0 | 7.9 | 14.0 | 21.4 | 42.5 | 50.3 | 49.5 | 94.7 | 96.3 | |
| Malta | 2012 | 29.4 | – | 19 | 6.3 | 6.7 | 7.7 | 7.5 | 39.6 | 60.7 | 100.7 | 208.7 | 264.8 | 307.0 | |
| Non-MENA Countries | Cyprus | 2012 | 33.2 | – | 2.7 | 3.0 | 7.0 | 18.4 | 18.4 | 39.2 | 109.4 | 86.0 | 207.7 | 308.3 | 393.1 |
| Turkey (2 registries) | 2012 | 23.1 | 2.1 | 3.6 | 4.3 | 5.0 | 13.4 | 22.7 | 34.8 | 59.6 | 135.1 | 132.8 | 139.9 | 176.9 | |
| Iran (Golestan) | 2008-2011 | 16.0 | 0.9 | 2.6 | 3.6 | 15.4 | 15.2 | 17.5 | 48.4 | 60.2 | 55.1 | 62.5 | 82.4 | 100.2 | |
| USA, SEER (9 registries) | 2012 | 28.3 | 1.6 | 3.3 | 5.0 | 10.6 | 19.3 | 36.0 | 67.9 | 76.7 | 102.6 | 146.2 | 182.7 | 255.6 | |
| Denmark | 2012 | 42.3 | 2.2 | 1.9 | 4.2 | 4.8 | 11.2 | 26.0 | 58.2 | 89.7 | 158.3 | 286.1 | 345.0 | 544.5 | |
| Norway | 2012 | 44.2 | 4.1 | 1.8 | 7.1 | 6.1 | 11.9 | 25.6 | 42.6 | 95.3 | 157.3 | 290.5 | 402.1 | 586.0 | |
| Sweden | 2012 | 31.6 | 2.2 | 3.3 | 4.8 | 19.4 | 20.5 | 42.2 | 70.1 | 127.5 | 183.7 | 264.1 | 363.9 | 378.0 | |
| England | 2012 | 38.6 | 1.6 | 3.1 | 7.0 | 7.6 | 11.9 | 26.2 | 49.7 | 90.1 | 165.7 | 214.5 | 324.3 | 461.4 | |
| Spain (9 registries) | 2010 | 48.3 | 0.4 | 1.8 | 3.0 | 6.1 | 13.4 | 31.6 | 74.3 | 131.9 | 217.5 | 314.3 | 377.7 | 513.5 | |
| France (9 registries) | 2011 | 36.4 | 1.2 | 2 | 3.7 | 4.3 | 12.7 | 27.6 | 58.0 | 98.7 | 136.4 | 220.4 | 302.9 | 412.4 | |
| Italy (8 registries) | 2010 | 40.3 | – | 1.8 | 3.2 | 5.8 | 13.5 | 27.8 | 59.1 | 121.3 | 184.7 | 230.6 | 290.5 | 466.0 | |
| Belgium | 2012 | 44.8 | 2.0 | 2.9 | 5.5 | 6.8 | 13.3 | 31.6 | 56.7 | 102.4 | 184.8 | 293.5 | 369.3 | 515.0 | |
| Germany (2 registries) | 2012 | 35.4 | 1.2 | 5.2 | 3.0 | 11.1 | 15.3 | 27.4 | 44.2 | 90.0 | 157.7 | 213.0 | 269.9 | 362.4 | |
| Slovakia | 2010 | 60.4 | 1.4 | 1.7 | 3.4 | 5.6 | 23.0 | 42.6 | 77.7 | 153.3 | 270.2 | 385.2 | 550.5 | 623.5 | |
| Korea (5 registries) | 2012 | 52.3 | 0.8 | 2.9 | 6.6 | 16.7 | 29.2 | 46.4 | 92.5 | 151.0 | 226.6 | 317.7 | 378.6 | 452.9 | |
^ASRw: Age Standardized Rate (world): age-standardized incidence rates (world population). References: Lebanon (10); Israeli Non-Jews (16); Israeli Jews (16); Algeria (17); Jordan (18); Egypt (19); Kuwait (16); Saudi Arabia (20-21); Malta (16); Cyprus (16); Turkey (16); Iran (17); USA (16); Denmark (22); Norway (22); Sweden (22); England (16); Spain (16); France (16); Italy (16); Belgium (23); Germany (16); Slovakia (24); Korea (16).
Similarly, the CRC ASRw among females in Lebanon (21.6 in 2012 and 18.5 in 2005-2016) was much higher than in other MENA countries except for Israeli Jews and Non-Jews, slightly lower than in France and USA, and it was considerably less than in countries reported to have the highest rates of CRC among females in 2018 (i.e., Norway and Denmark) (Table 4).
Table 4.
CRC ASRw and Age-Specific Rates in Females—Lebanon Compared to MENA and non-MENA Countries.
| Country | Year(s) | Annual Incidence per 100,000 by Age Group: Females | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ASRw^ | 20-24y | 25-29y | 30-34y | 35-39y | 40-44y | 45-49y | 50-54y | 55-59y | 60-64y | 65-69y | 70-74y | 75+y | |||
| MENA countries | Lebanon | 2012 | 21.6 | 0.5 | 3.0 | 4.2 | 6.7 | 26.9 | 40.5 | 49.9 | 48.6 | 67.0 | 78.5 | 152.6 | 211.1 |
| Israeli Non-Jews | 2012 | 24.5 | - | 2.8 | 2.8 | 7.1 | 12.8 | 33.6 | 58.6 | 64.9 | 92.3 | 137.7 | 180.3 | 198.0 | |
| Israeli Jews | 2012 | 25.3 | - | 1.9 | 3.9 | 12.5 | 14.3 | 26.1 | 55.8 | 67.7 | 80.7 | 115.5 | 192.6 | 271.9 | |
| Algeria (Setif) | 2008-2011 | 11.4 | 0.3 | 1.8 | 4.8 | 8.9 | 8.7 | 17.9 | 21.5 | 34.2 | 52.9 | 83.6 | 43.7 | 35.1 | |
| Algeria (Batna) | 2008-2012 | 8.5 | 0.3 | 0.8 | 3.3 | 3.9 | 11.8 | 10.5 | 21.6 | 20.3 | 29.5 | 40.4 | 55.5 | 59.4 | |
| Jordan | 2012 | 16.7 | 0.9 | 1.1 | 2.1 | 6.2 | 20.5 | 19.3 | 42.9 | 36.0 | 61.9 | 85.6 | 148.0 | 94.9 | |
| Minia Governorate, Egypt | 2009 | 4.6 | 1.4 | 3.4 | 3.3 | 3.7 | 9.8 | 7.2 | 12.9 | 10.1 | 13.7 | 17.7 | 19.5 | 12.5 | |
| Aswan Governorate, Egypt | 2010 | 6.9 | - | - | - | - | 2.9 | - | 15.4 | 49.7 | 42.3 | 23 | 53.8 | 26.8 | |
| Damietta Governorate, Egypt | 2012 | 9.1 | - | - | 2.3 | 2.3 | 5.2 | 15.5 | 14.8 | 33 | 22.2 | 32.5 | 81.3 | 100.1 | |
| Kuwaiti | 2012 | 18.5 | - | 4 | 7.1 | 7.7 | 11.8 | 34.3 | 34.4 | 58.8 | 92.2 | 74.3 | 109.8 | 116.2 | |
| Saudi Arabia | 2013 | 10.2 | 0.3 | 2.3 | 2.5 | 4.6 | 8.3 | 15.7 | 27.7 | 33.8 | 38.8 | 48.7 | 63.0 | 53.9 | |
| Malta | 2012 | 23.1 | - | 6.9 | 13.5 | 7.1 | - | 30.7 | 6.6 | 61.3 | 105.3 | 149.4 | 140.9 | 261.4 | |
| Non-MENA Countries | Cyprus | 2012 | 18.3 | - | - | 2.7 | 5.9 | 15.5 | 23.1 | 27.2 | 39.6 | 83.4 | 88.6 | 121 | 195.9 |
| Turkey (2 registries) | 2012 | 13.8 | 1.3 | 1.2 | 2.8 | 5.1 | 10.9 | 16.5 | 29.6 | 42.8 | 43.3 | 63.7 | 122.5 | 110.3 | |
| Iran (Golestan) | 2008-2011 | 12.5 | 1.3 | 2.8 | 4.3 | 6.7 | 12.8 | 20.3 | 36.4 | 31.9 | 46.4 | 63.1 | 55.5 | 74.8 | |
| USA, SEER (9 registries) | 2012 | 22.2 | 1.8 | 2.9 | 6.0 | 9.2 | 16.7 | 33.2 | 54.7 | 51.9 | 70.9 | 95.6 | 143.7 | 228.6 | |
| Denmark | 2012 | 33.7 | 2.9 | 2.5 | 4.2 | 8.5 | 13.5 | 31.9 | 50.3 | 100.7 | 123.7 | 188.5 | 266 | 369.6 | |
| Norway | 2012 | 36.3 | 1.8 | 3.7 | 11.8 | 5.3 | 11.0 | 29.7 | 59.4 | 94.3 | 131.9 | 209.0 | 281.0 | 419.4 | |
| Sweden | 2012 | 24.4 | 0.6 | 1.0 | 1.4 | 8.3 | 11.4 | 20.1 | 36.1 | 66.6 | 99.7 | 128.3 | 190.5 | 282.0 | |
| England | 2012 | 26.2 | 2.7 | 4.4 | 6.3 | 7.5 | 13.7 | 22.4 | 39.8 | 66.6 | 98.5 | 134.4 | 200.9 | 296.8 | |
| Spain (9 registries) | 2010 | 24.5 | 0.8 | 0.3 | 2.7 | 6.1 | 12.6 | 23.8 | 45.9 | 72.8 | 100.6 | 134.1 | 181.4 | 244.2 | |
| France (9 registries) | 2011 | 23.4 | 1.6 | 1.7 | 5.5 | 10.5 | 14.2 | 18.4 | 41.6 | 61.2 | 86.3 | 127.7 | 159.3 | 265.2 | |
| Italy (8 registries) | 2010 | 27.3 | 1.4 | 1.2 | 4.6 | 7.8 | 11.4 | 29.0 | 59.6 | 79.8 | 109.5 | 155.7 | 162.7 | 273.2 | |
| Belgium | 2012 | 30.0 | 2.9 | 3.4 | 7.7 | 8.9 | 17.1 | 27.5 | 45.6 | 75.0 | 116.0 | 174.2 | 203.6 | 321.5 | |
| Germany (2 registries) | 2012 | 26.3 | 2.3 | 1.0 | 4.0 | 12.5 | 12.9 | 25.7 | 51.2 | 75.9 | 101.5 | 126.0 | 190.8 | 283.9 | |
| Slovakia | 2010 | 29.7 | 1.0 | 1.9 | 3.5 | 8.7 | 13.9 | 35.2 | 50.5 | 75.8 | 123.8 | 167.4 | 209.3 | 299.0 | |
| Korea (5 registries) | 2012 | 28.2 | 0.8 | 2.4 | 6.2 | 11.5 | 20.3 | 37.5 | 59.8 | 75 | 112.6 | 146.3 | 187.4 | 233.3 | |
^ASRw: Age Standardized Rate (world): age-standardized incidence rates (world population). References: Lebanon (10); Israeli Non-Jews (16); Israeli Jews (16); Algeria (17); Jordan (18); Egypt (19); Kuwait (16); Saudi Arabia (20-21); Malta (16); Cyprus (16); Turkey (16); Iran (17); USA (16); Denmark (22); Norway (22); Sweden (22); England (16); Spain (16); France (16); Italy (16); Belgium (23); Germany (16); Slovakia (24); Korea (16).
There were high age-specific incidence rates in the age groups 40-44 and 45-49 years in Lebanon in both males and females (with significant rising temporal trend as shown in Tables 1 and 2) compared to other countries including the ones reported to have the highest CRC ASRw worldwide (Tables 3 and 4).
Discussion
CRC is one of the most common cancers in Lebanon, with an ASRw higher than that in other MENA countries except for Israeli Jews and Non-Jews, and lower than that in developed non-MENA countries. These rates suggest a possible influence of sociological and lifestyle patterns, which are transitioning from regional norms to global trends. It is worth noting that there is a wide international variation in CRC incidence rates (up to 10-fold). This variation has been attributed to the differences in population size and age structure, differences in risk factors, namely modifiable ones, and availability of early detection services.4,5 Despite the high incidence rates of CRC in Lebanon, little research has been done regarding CRC and its associated risk factors. The following factors can be considered to affect the high incidence of CRC in Lebanon:
Sociological Factors: The demographic shifts that Lebanon has experienced over the last few decades indicate that it has the fastest growing older adult population in the Arab region. This is attributed to 3 factors; the decreased fertility rates to around 1.9,25 the longer life expectancy at birth (76.3 years in general compared to 69.1 years in the WHO Eastern Mediterranean Region in 2016),26 and the high rates of youth out-migration.27 The proportion of elderly citizens aged 65 and above was estimated at approximately 10% of the population in Lebanon.25 This demographic shift toward a growing proportion of elderly people, along with higher CRC age-specific incidence rates after the age of 50 years, may partially explain the significant increase in CRC ASRw in Lebanon from 2005 to 2016. However, demographic shifts do not play a role when the ASRw using the world standard population are compared among countries.
Lifestyle Factors: Modifiable lifestyle factors, namely smoking, alcohol consumption, red meat and processed meat consumption, sedentary lifestyle, and excess body weight, play a crucial role in increasing CRC risk.4,5,6,28-32 Other reported risk factors include advancing age, male sex, ethnicity (African American), genetic predisposition, family or personal history of CRC, presence of certain medical conditions (inflammatory bowel diseases namely ulcerative colitis, diabetes mellitus, insulin resistance, history of abdominal radiation, acromegaly, renal transplant with use of immunosuppressive medications, androgen deprivation therapy, cholecystectomy, coronary artery disease, and ureterocolic anastomosis), and environmental factors.4,5,6,28-32
Nutrition plays both a causal and protective role in CRC. Pro-inflammatory food components (e.g., energy, carbohydrates, proteins, total fat, trans fat, cholesterol, and saturated fatty acids) are reported to increase the risk of CRC.31 Whereas anti-inflammatory food components (e.g., fiber, omega 3, omega 6, niacin, thiamin, riboflavin, vitamin B6, B12, zinc, magnesium, selenium, vitamin A, vitamin C, vitamin D, vitamin E, folic acid, and beta carotene) are found to protect against CRC.31 Mediterranean diet is reported to protect against different types of neoplasms including large bowel, and a minimal adherence to a healthy Mediterranean diet is expected to increase CRC incidence by 2% in both males and females.33 Physical activity also plays a protective effect, particularly high physical activity, which is expected to have an average of 15% protection rate on CRC.33 On the contrary, a positive association was found between colon cancer and alcohol consumption.28,31 Smoking was also found to be strongly associated with CRC whereby a significant trend of increasing CRC risk was seen with longer smoking duration, higher smoking intensity, and with increasing pack-years.6,28,30,34 Passive smoking was also found to be associated with an increased risk of CRC.35
In Lebanon, consumption of unhealthy diet, physical inactivity, obesity, diabetes mellitus, and smoking are becoming more prominent.36-38 While 60-70% of the Lebanese population were found to moderately adhere to a healthy Mediterranean diet,33 studies showed the prevalence of unhealthy eating behaviors among Lebanese. In fact, the consumption of vegetables and fruits among the adult Lebanese population is found to be moderately low, consisting of 1.8 servings per day.39 Moreover, a study conducted in the capital city showed a high energy intake per capita resulting from increased consumption of meat, namely, beef, saturated fat, and refined carbohydrates, and a decreased intake of fresh fruits and vegetables.36 The level of physical inactivity is considerable among the adult population in Lebanon with 34.8% (40.9% of men and 29.3% of women) reporting having more than 12 sedentary hours per day37 and 61% of adults aged 18 to 69 years reporting having low levels of physical activity.39 Alcohol consumption in Lebanon is the highest in the Arab region,40 with 40.3% (51.9% of men and 29.6% of women) of adult population reporting drinking alcohol.37 The consequence of these lifestyle changes was highlighted again over a 12-year study period showing an alarming rise in obesity prevalence in the Lebanese population.38 Another study conducted in 2016 showed that 27% of adults aged 18-69 years are obese, and 37.9% are overweight.39 Moreover, 18% of adults aged 50 years and above are suffering from diabetes mellitus (20.6% in men and 15.0% in women).37 The prevalence of tobacco smoking among adults in Lebanon has been rising over the years, increasing from 34% (43% in men and 26% in women) in 2009 to 38% (48% in men and 29% in women) in 2016.37,39 Another study showed a high consumption of cigarette packs (12.4 packs per person per month) among adult Lebanese.41 It is important to note that Lebanon has one of the weakest tobacco control regulatory environments where smoking is prevalent in youth. Moreover, unsafe levels of indoor air pollution due to smoking were found in several public places in Lebanon,42 putting people at risk of passive smoking.
Environmental Factors: Several studies have shown an association between pollution and chlorinated water and CRC.43,44 The risk level is dependent on the frequency of exposure to, and the levels of trihalomethanes in drinking water.44 Furthermore, chronic exposure to low-dose persistent organic pollutants was found to be associated with an increased risk of colorectal polyps and cancer.45 In Lebanon, drinking water is chlorinated, and it was found to include some levels of pesticides and high concentrations of heavy metals.46
Genetic Factors: There are no published studies at this stage regarding the prevalence of genetic predisposition to CRC in Lebanese population.
Availability of CRC Screening Tests: Screening tests for CRC, including colonoscopy, flexible sigmoidoscopy, fecal occult blood testing (FOBT), and fecal immunochemistry testing (FIT) are available in Lebanon but not widely at the public primary health care level.8 It can be assumed that this rise in CRC incidence can be due to the widespread availability of these tests, since the introduction of early detection screening tests might increase CRC incidence rates during the first few years due to the detection of undiagnosed disease.5 However, this might not be the case in Lebanon since only 14.2%, and 15% of eligible adults reported having undergone CRC screening in different studies.47,48 Actually, there is a major gap in the knowledge about CRC screening, risk factors, and warning signs in the country.48,49 In a study conducted in a tertiary health care center regarding the awareness of CRC and attitudes toward its screening guidelines among patients, 83% and 67% of participants were not aware of CRC risk factors and warning signs, respectively.48 Only 55% of participants were aware of the necessity for screening.48 Another study conducted among the public showed that 59% of participants never heard of CRC.49
It is worth noting as well that the mean global total cost for the treatment of metastatic CRC in Lebanese hospitals was found to be USD 64,805 per patient.50 This is significant, knowing that 21.9% of CRC cases studied in a tertiary care center in Lebanon were metastatic at the time of diagnosis.51 Also, the medications used for CRC are among the 4 cancer types consuming up to 67% of the MoPH oncology drug budget in 2008-2013 (breast cancer followed by chronic myeloid leukemia, CRC, and lung cancer).52
Taking all the above into consideration and knowing that sporadic cases of CRC account for 70% of all cases,53 it is essential to have national CRC raising awareness and screening campaigns in the country. Indeed, a national CRC awareness campaign was launched in 2019 by the MoPH. The campaign included launching CRC screening guidelines and educational materials on the importance of screening, as well as providing free FIT testing at a limited scale.54 The guidelines included offering FIT testing yearly for all individuals at average risk for CRC and those aged 50 years and above, while for those at increased risk, the guidelines advise using colonoscopy starting 50 years of age or earlier as indicated. However, the campaign stopped shortly afterward for economic reasons.
Different CRC screening programs are available worldwide, yet the rate of global CRC screening is less than 40%.30 This unsatisfactory screening rate is probably due to lack of CRC programs in some countries, and to several barriers affecting the available programs (e.g. financial coverage, access to primary care, costs, logistical challenges, lack of provider involvement, cultural beliefs and lack of awareness of CRC screening).30 A national CRC awareness and screening program in Lebanon is highly recommended and it should tackle both preventive measures as well as early detection at nominal fees. Re-launching the national campaign and ensuring its sustainability and integration in primary care is important. Using innovative ways to raise awareness can be beneficial; this includes for example sending short invitation SMS-text message for screening,55 which was adopted in the latest breast cancer campaigns in the country; and using educational inflatable colon for raising awareness, which was shown to increase participants’ knowledge regarding CRC and their willingness to screen.47
Recent studies suggest that the incidence of CRC might be increasing in individuals younger than 50 years.31,56 Another important finding in our study is the presence of relatively high age-specific incidence rates at age groups 40-44 and 45-49 years in both males and females compared to other countries, including those reported to have the highest CRC ASRw worldwide. This finding is in favor of changing the starting age for the CRC screening in average-risk individuals to 40 years instead of 50 years, or at least to 45 years as per the recommendation of the American Cancer Society.57 It is worth noting though that the majority of third-party payers, including private insurances in Lebanon, do not cover tests requested for screening purposes. This should be taken into consideration when developing national screening guidelines for CRC.
Our study is based on NCR data published by the MoPH on its official website. In this respect, few limitations can be mentioned. Although tremendous improvements were done to the NCR in terms of case counting during the last years, the information about the collected cases is still incomplete. The inconsistency in including in-situ cancers might lead to a bias when age-standardized incidence rates are compared. Moreover, the information about the mortality or survival rates is lacking.
Conclusion
Colorectal cancer is a major public health problem in Lebanon. This review could serve as a blueprint to raise awareness about the need for earlier screening for CRC and the necessity for promoting healthier lifestyle choices as primary prevention. A national CRC prevention program needs to be developed to address this problem, while taking into consideration necessary measures to overcome the different challenges that might face such programs in developing countries like Lebanon. It is suggested to integrate the national CRC prevention program at the primary care level i.e. through the 240 primary health care centers distributed all over the country. The main components of this program include increasing community awareness on CRC risk factors, strengthening healthy lifestyle education programs, improving CRC screening practices by primary care physicians as well as provision of supported or free FIT testing to individuals aged 40 years and above. Moreover, advocating for the coverage of screening tests by private insurances and other third-party payers in the country, would lead to improvements in the screening of CRC and other types of cancer. Finally, it is important to join efforts among relevant stakeholders to develop a more comprehensive and complete cancer database.
List of Abbreviations
- APC - Annual Percent Change
- AAPC - Average Annual Percent Change
- ASRw - Age-Standardized Incidence Rate
- C15 Plus - Cancer Incidence in Five Continents Time Trends
- C15 XI - Cancer Incidence in Five Continents Volume XI
- CRC - Colorectal Cancer
- FIT - Fecal Immunochemistry Testing
- FOBT - Fecal Occult Blood Testing
- HDI - Human Development Index
- ICD10 - International Classification of Diseases, tenth revision
- JRP - Joinpoint Regression Program
- LCL - Lower Confidence Limit
- MENA - Middle East and North Africa
- MoPH - Ministry of Public Health
- NCR - National Cancer Registry
- SMS - Short Message Service
- UCL - Upper Confidence Limit
- USA - United States of America
- WHO - World Health Organization
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics Approval and Consent to Participate: Ethical approval is not applicable for this article. There are no human subjects in this article and informed Colorectal Cancer in Lebanon: Incidence, Temporal Trends, and Ethics approval and consent to participate: Ethical approval is not applicable for this article. There are no human subjects in this article and informed consent is not applicable.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ola El-Kibbi  https://orcid.org/0000-0002-5538-1694
https://orcid.org/0000-0002-5538-1694
Mona H. Osman, MD, MPH, MBA  https://orcid.org/0000-0002-6364-6541
https://orcid.org/0000-0002-6364-6541
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A.Global Cancer Statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492. The online GLOBOCAN 2018 database is accessible at http://gco.iarc.fr/, as part of IARC’s Global Cancer Observatory. Accessed July 14, 2019. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, Estimated Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. International Agency for Research on Cancer (IARC); 2013. Accessed August 11, 2020. http://globocan.iarc.fr [Google Scholar]
- 3.Center MM, Jemal A, Smith RA, Ward E. Worldwide variations in colorectal cancer. CA Cancer J Clin. 2009;59(6):366–378. doi:10.3322/caac.20038 [DOI] [PubMed] [Google Scholar]
- 4.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi:10.3322/caac.20107 [DOI] [PubMed] [Google Scholar]
- 5.Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66(4):683–691. doi:10.1136/gutjnl-2015-310912 [DOI] [PubMed] [Google Scholar]
- 6.Finlay A, Macrae RMG, Seres D, Savarese DMF. Colorectal Cancer: Epidemiology, Risk Factors, and Protective Factors. 2018. Accessed August 11, 2020.https://www.uptodate.com/contents/colorectal-cancer-epidemiology-risk-factors-and-protective-factors
- 7.World Health Organization (WHO). Lebanon: country profiles, 2017. Accessed October 10, 2020. https://www.who.int/tobacco/surveillance/policy/country_profile/lbn.pdf?ua=1; https://www.who.int/substance_abuse/publications/global_alcohol_report/profiles/lbn.pdf?ua=1
- 8.World Health Organization. Cancer country profiles. 2014. Lebanon. Accessed October 10, 2020. https://www.who.int/cancer/country-profiles/lbn_en.pdf
- 9.Adib S, Daniel J.Cancer in Lebanon 2004 With an Update of Cancer 2003. Ministry of Public Health, National Cancer Registry; 2008. Accessed October 11, 2020. https://www.moph.gov.lb/DynamicPages/download_file/571 [Google Scholar]
- 10.National Cancer Registry. Lebanon. Ministry of Public Health Web site; 2020. Accessed August 11, 2020. https://www.moph.gov.lb/en/Pages/8/19526/national-cancer-registry
- 11.Bray F, Ferlay J. Age Standardization (chapter 7). In: Bray F, Colombet M, Mery L, Piñeros M, Znaor A, Zanetti R, Ferlay J, eds. Cancer Incidence in Five Continents, Vol. XI(electronic version); 2017. International Agency for Research on Cancer (IARC). Accessed August 11, 2020. http://ci5.iarc.fr/CI5-XI/Pages/Chapter7.aspx [Google Scholar]
- 12.United States Cancer Statistics (USCS). Centers for Disease Control and Prevention (CDC) Web site. Updated August 20, 2014. Accessed August 11, 2020. https://www.cdc.gov/cancer/npcr/uscs/technical_notes/stat_methods/rates.htm
- 13.Joinpoint Help System 4.7.0.0 (online)- Surveillance Research Program. National Cancer Institute (NCI), Division of cancer control and population sciences, USA. Accessed October 11, 2020. https://surveillance.cancer.gov/help/joinpoint/setting-parameters/method-and-parameters-tab
- 14.Dyba T, Hakulinen T. Comparison of different approaches to incidence prediction based on simple interpolation techniques. Stat Med. 2000;19(13):1741–1752. doi:10.1002/1097-0258(20000715)19:13<1741: aid-sim496>3.0.co;2-o [DOI] [PubMed] [Google Scholar]
- 15.O’Lorcain P, Deady S, Comber H. Mortality predictions for colon and anorectal cancer for Ireland, 2003-17. Colorectal Dis. 2006;8(5):393–401. doi:10.1111/j.1463-1318.2006.00951.x [DOI] [PubMed] [Google Scholar]
- 16.Ferlay J, Colombet M, Bray F.Cancer Incidence in Five Continents Time Trends (CI5plus): IARC CancerBase No. 9 [Internet]. International Agency for Research on Cancer (IARC); 2018. Accessed August 11, 2020. http://ci5.iarc.fr/CI5plus/Pages/table4_sel.aspx [Google Scholar]
- 17.Bray F, Colombet M, Mery L, et al. eds. Cancer Incidence in Five Continents, Vol. XI (CI5 XI) [electronic version]. International Agency for Research on Cancer (IARC); 2017. Accessed August 11, 2020. http://ci5.iarc.fr/CI5-XI/Pages/registry_summary.aspx [Google Scholar]
- 18.Jordan Cancer Registry. Cancer Incidence in Jordan 2012. Accessed October 30, 2020. http://www.moh.gov.jo/Echobusv3.0/SystemAssets/a05a084b-3781-4979-a217-2184d5d57ede.pdf
- 19.National Cancer Registry Program of Egypt (NCRPE). Accessed August 11, 2020. http://cancerregistry.gov.eg/
- 20.Bazarbashi S, Al Eid H, Minguet J. Cancer Incidence in Saudi Arabia: 2012 Data from the Saudi Cancer Registry. Asian Pac J Cancer Prev. 2017;18(9):2437–2444. doi:10.22034/APJCP.2017.18.9.2437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kingdom of Saudi Arabia Saudi Health Council Saudi Cancer Registry. Cancer Incidence Report Saudi Arabia 2013. Accessed August 11, 2020. https://nhic.gov.sa/eServices/Documents/2013.pdf
- 22.The NORDCAN project. Accessed August 11, 2020. http://www-dep.iarc.fr/NORDCAN/english/frame.asp
- 23.Belgium Cancer Registry. Published November 27, 2014. Accessed August 11, 2020. https://kankerregister.org/Annual%20Tables
- 24.European Cancer Information System (ECIS). Accessed August 11, 2020. https://ecis.jrc.ec.europa.eu/index.php.
- 25.Central Administration of Statistics. Population and housing characteristics in Lebanon, Statistics in Focus (SIF), Beirut, Lebanon, Issue number 2. 2012. Accessed October11, 2020.http://www.cas.gov.lb/images/PDFs/SIF/CAS_Population_and_housing_In_Lebanon_SIF2.pdf
- 26.World Health Organization. Life expectancy and Healthy life expectancy Data by WHO region. Accessed October 20, 2020. https://apps.who.int/gho/data/view.main.SDG2016LEXREGv?lang=en
- 27.Abdulrahim S, Ajrouch KJ, Antonucci TC. Aging in Lebanon: challenges and opportunities. Gerontologist. 2015;55(4):511–518. doi:10.1093/geront/gnu095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.International Agency for Research on Cancer (IARC); Personal Habits and Indoor Combustions; Tobacco Smoking. IARC Monographs, Volume100E, 2012. Accessed October 11, 2020. http://publications.iarc.fr/122
- 29.Johnson CM, Wei C, Ensor JE, et al. Meta-analyses of colorectal cancer risk factors. Cancer Causes Control. 2013;24(6):1207–1222. doi:10.1007/s10552-013-0201-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laubey-Secretan B, Vilahur N, Bianchini F, Guha N, Straif K. International Agency for Research on Cancer Handbook Working Group. The IARC Perspective on Colorectal Cancer Screening. N Engl J Med. 2018;378(18):1734–1740. doi:10.1056/NEJMsr1714643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thanikachalam K, Khan G. Colorectal Cancer and Nutrition. Nutrients. 2019;11(1):164. Published January 14, 2019. doi:10.3390/nu11010164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laubey-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. International Agency for Research on Cancer Handbook Working Group. Body Fatness and Cancer—Viewpoint of the IARC Working Group. N Engl J Med. 2016;375(8):794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Charafeddine MA, Olson SH, Mukherji D, Sally N., Temraz SN, Abou-Alfa GK, Shamseddine AI. Proportion of cancer in a Middle Eastern country attributable to established risk factors. BMC Cancer. 2017;17:337. doi:10.1186/s12885-017-3304-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karahalios A, English DR, Simpson JA. Weight change and risk of colorectal cancer: a systematic review and meta-analysis. Am J Epidemiol. 2015;181(11):832–845. Epub 2015 Apr 16. [DOI] [PubMed] [Google Scholar]
- 35.Yang C, Wang X, Huang CH, Yuan WJ, Chen ZH. Passive smoking and risk of colorectal cancer: a meta-analysis of observational studies. Asia Pac J Public Health. 2016;28(5):394–403. doi:10.1177/1010539516650724 [DOI] [PubMed] [Google Scholar]
- 36.Nasreddine L, Hwalla N, Sibai A, Hamzé M, Parent-Massin D.Food consumption patterns in an adult urban population in Beirut, Lebanon. Public Health Nutr. 2006;9(2):194–203. [DOI] [PubMed] [Google Scholar]
- 37.Sibai A, Tohme RA, Mahfoud Z, Chaaya M, Hwalla N.Noncommunicable Diseases and Behavioral Risk Factor Survey Comparison of Estimates Based on Cell Phone Interviews With Face to Face Interviews. American University of Beirut; 2009. Accessed October 10, 2020. https://www.moph.gov.lb/DynamicPages/download_file/563 [Google Scholar]
- 38.Nasreddine L, Naja F, Chamieh MC, Adra N, Sibai AM, Hwalla N. Trends in overweight and obesity in Lebanon: evidence from two national cross-sectional surveys (1997 and 2009). BMC Public Health. 2012;12:798. doi:10.1186/1471-2458-12-798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.WHO Stepwise Approach for Non-Communicable Diseases Risk Factor Surveillance. World Health Organization, Ministry of Public Health. Lebanon, 2016-2017. Accessed October 28, 2020.https://www.who.int/ncds/surveillance/steps/Lebanon_STEPS_report_2016-2017.pdf?ua=1
- 40.Ghandour L, Chalak A, El-Aily A, et al. Alcohol consumption in the Arab region: what do we know, why does it matter, and what are the policy implications for youth harm reduction? Int J Drug Policy. 2016;28:10–33. doi:10.1016/j.drugpo.2015.09.013 [DOI] [PubMed] [Google Scholar]
- 41.Salti N, Chaaban J, Naamani N. The economics of tobacco in Lebanon: an estimation of the social costs of tobacco consumption. Subst Use Misuse. 2014;49(6):735–742. doi:10.3109/10826084.2013.863937 [DOI] [PubMed] [Google Scholar]
- 42.Saade G, Seidenberg AB, Ree VW, Otrock Z, Connolly GN. Indoor secondhand tobacco smoke emission levels in six Lebanese cities. Tobacco Control 2010;19:138e–142. doi:10.1136/tc.2009.030460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.El-Tawil AM. Colorectal cancer and pollution. World J Gastroenterol. 2010;16(28):3475–3477. doi:10.3748/wjg.v16.i28.3475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.El-Tawil AM. Colorectal cancers and chlorinated water. World J Gastrointest Oncol. 2016;8(4):402–409. doi:10.4251/wjgo.v8.i4.402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee Y-M, Kim S-A, Choi G-S, et al. Association of colorectal polyps and cancer with low-dose persistent organic pollutants: a case-control study. PLoS ONE. 2018;13(12):e0208546. doi:10.1371/journal.pone.0208546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ministry of Environment/LEDO. Lebanon State of the Environment Report: Chapter 8 Water [Online]. Ministry of Environment. 2001. Accessed November 10, 2020. http://www.moe.gov.lb/getattachment/The-Ministry/Reports/State-Of-the-Environment-Report-2001/Chap-8-Water.pdf.aspx
- 47.Baassiri A, El-Harakeh M, Itani A, et al. Giant inflatable colon model enhances Lebanese community knowledge and intention for colorectal cancer screening. JCO Glob Oncol. 2020;6:JGO.19.00274. doi:10.1200/JGO.19.00274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tfaily MA, Naamani D, Kassir A, et al. Awareness of colorectal cancer and attitudes towards its screening guidelines in Lebanon. Ann Glob Health. 2019;85(1). pii: 75. doi:10.5334/aogh.2437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nemer HA, Hejase AJ, Hussin J, et al. Colorectal cancer: exploring awareness in Lebanon. J Middle East North Afr Sci. 2016;2(10). Accessed November 10, 2020. http://www.jomenas.org. doi:10.12816/0032694 [Google Scholar]
- 50.Henaine AM, Chahine G, Massoud M, et al. Management of patients with metastatic colorectal cancer in Lebanese hospitals and associated direct cost: a multicentre cohort study. East Mediterr Health J. 2019;25(7):481–494. doi:10.26719/emhj.18.063 [DOI] [PubMed] [Google Scholar]
- 51.Nehmeh WA, Rassy M, Ghorra C, Abdayem P, Tohmé C.Sporadic colon cancer in Lebanon: a clinicopathological study. Gulf J Onc. 2018;1(27):19–22. [PubMed] [Google Scholar]
- 52.Elias F, Khuri FR, Adib SM, et al. Financial Burden of Cancer Drug Treatment in Lebanon. Asian Pac J Cancer Prev. 2016;17(7):3173–3177. [PubMed] [Google Scholar]
- 53.Mármol I, Sánchez-de-Diego C, Pradilla Dieste A, Cerrada E, Rodriguez Yoldi MJ. Colorectal carcinoma: a general overview and future perspectives in colorectal cancer. Int J Mol Sci. 2017;18(1):197. Published January 2019, 2017. doi:10.3390/ijms18010197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.National guidelines for colorectal cancer early detection. Republic of Lebanon; Ministry of Public Health. 2019. Accessed November 10, 2020. https://www.moph.gov.lb/userfiles/files/AwarenessCampaign/National%20Colon%20Cancer%20Awareness%20Campaign%202019/colorectal%20cancer-guidelines%20%20%202019.pdf [Google Scholar]
- 55.Lakkis NA, Atfeh AM, El-Zein YR, Mahmassani DM, Hamadeh GN. The effect of two types of sms-texts on the uptake of screening mammogram: a randomized controlled trial. Prev Med. 2011;53(4-5):325–327. doi:10.1016/j.ypmed.2011.08.013 [DOI] [PubMed] [Google Scholar]
- 56.Araghi M, Soerjomataram I, Bardot A, et al. Changes in colorectal cancer incidence in seven high-income countries: a population-based study. Lancet Gastroenterol Hepatol. Published online May 16, 2019. doi:10.1016/S2468-1253(19)30147-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Smith RA, Andrews KS, Brooks D, et al. Cancer screening in the United States, 2018: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. 2018;68(4):297–316. doi:10.3322/caac.21446 [DOI] [PubMed] [Google Scholar]