Abstract
Suicide is a leading cause of death for young adults, and college-enrolled students are at markedly high risk for suicide. Psychotic-like experiences (PLEs) and sleep difficulties are prevalent among college students and have been linked to increased suicidal ideation (SI). This cross-sectional study examined the relation between PLEs and SI, moderated by sleep quality, in a sample of 442 students at a university counseling center. The Behavioral Health Measure-43 (BHM-43) was used to evaluate mental health symptoms, including sleep quality and SI. The PRIME Screen-Revised was used to measure PLEs. Regression results indicated that higher PRIME scores statistically predicted greater SI. There was a significant interaction between PRIME and sleep quality in predicting SI. Among individuals with greater sleep difficulties, PLEs were positively, significantly associated with SI. The PRIME was not a significant predictor of SI at lower levels of sleep difficulties (i.e. better sleep quality). This interaction effect remained significant when controlling for age and BHM-43 depression and bipolar subscales. Findings suggest that sleep difficulties may be linked to increased SI for individuals with PLEs, and better sleep may be protective. Further research is needed to explore treatment targeting PLEs and/or sleep to mitigate suicide risk among university students.
Keywords: suicidal ideation, psychotic-like experiences, sleep disorder, college counseling
1. Introduction
In the United States, suicide rates among college students have been steadily increasing for the past several decades, and suicide is now the second leading cause of death for college-aged individuals (Duffy et al., 2019; Heron, 2019). During this transitional developmental period, it is thought that elevated stress contributes to the emergence and exacerbation of mental illness and suicidal thoughts and behaviors (STBs; Dixon et al., 1992; Rowe et al., 2013; Twenge et al., 2019). Approximately 24% of college students endorse STBs, with 2.4% of students reporting a suicide attempt in the past 12 months, and 10% reporting a lifetime attempt (American College Health Association, 2019; Center for Collegiate Mental Health, 2020). These rates indicate a critical need to bolster mental health screening and suicide risk assessment in college settings.
One important and commonly-assessed risk factor for STBs is depression, however, additive stressors may increase STBs among individuals with and without mood disorders (Dixon et al., 1992). This suggests that trans- and sub-diagnostic experiences linked to stress may uniquely contribute to suicide risk, and there is a need to expand risk screening beyond traditional screening for mood symptoms and other major psychopathology associated with suicide (e.g., psychotic or substance use disorders; Bertolote et al., 2004; Conwell et al., 1996; Huang et al., 2018). Psychotic-like experiences (PLEs), including attenuated hallucinations, delusions, and disorganized thoughts and behaviors, have been linked to STB in clinical and general population samples ( Capra et al., 2015; DeVylder et al., 2015a, 2015b; Taylor, Hutton, & Wood, 2015; Thompson et al., 2020a). Notably, recent meta-analytic results indicate that individuals experiencing PLEs may be two times more likely to have suicidal ideation (SI), three times more likely to attempt suicide, and four times more likely to die by suicide than individuals who are not experiencing PLEs (Yates et al., 2018). Given the emergence of PLEs and STB during late adolescence and emerging adulthood, and given the added distress that often accompanies PLEs, assessment of PLEs may be useful for suicide prevention efforts in the young adult age group and college settings in particular.
Sleep difficulties commonly occur with PLEs, and they often exacerbate distress and functional impairment and decrease quality of life for individuals with PLEs (Andorko et al., 2017; Davies et al., 2017; Hofstetter et al., 2005; Lee et al., 2012; Lunsford-Avery et al., 2013; Thompson et al., 2020b). Furthermore, sleep problems appear to increase presentation of PLEs, which in turn has shown to increase sleep disruption, leading to a potentially cyclic intensification of experiences (Afonso et al., 2011; Waite et al., 2016a, 2016b). Given that both PLEs and sleep difficulties are independently linked to suicide risk (Bernert et al., 2005; Sjöström et al., 2007; Yates et al., 2018) and these experiences seem to convey bidirectional effects on each other, it is hypothesized that sleep may moderate the relation between PLEs and sleep quality (e.g., poor sleep may intensify the link between PLEs and SI, and better sleep may be a protective factor).
Although prior research has supported interrelations between PLEs, sleep disturbances, and SI in community and outpatient settings, little is known about the interactive effect of sleep and PLEs on suicide risk among young adults in college campus settings. College students are at a peak age and in a prime context to develop psychotic symptomatology and STB, and they often experience sleep disruption and/or dysregulation (Lund et al., 2010). Nationwide data indicates that on average, approximately 9% of student bodies use campus counseling centers (Xiao et al., 2017), and individuals seeking help for mental health concerns are at increased risk for experiencing PLEs, sleep difficulties, and STB. Thus, exploring the relation between these PLEs and STB, moderated by sleep difficulties, may inform suicide risk screening and treatment efforts in university counseling settings.
The current study examined the relation between PLEs and SI, with sleep quality as a moderator, in a sample of help-seeking students at a large mid-Atlantic university. The Behavioral Health Measure-43 (BHM-43), a behavioral health screening tool commonly used in college counseling settings, was used to evaluate mental and behavioral health symptoms, including sleep difficulties, SI, and other clinical symptoms (e.g., depression, bipolar disorder). Mental health symptoms and demographic features (i.e. age, gender, race) previously linked to STB were used to explore the incremental value of using a PLE screening tool, the PRIME Screen- Revised, to statistically predict SI. We hypothesized that among help-seeking university students, more PLEs would be associated with greater SI. We further hypothesized that sleep quality would moderate this effect so that among individuals with greater sleep difficulties, PLEs would be more strongly linked to SI compared to those with lower levels of sleep difficulty.
2. Methods
2.1. Participants
All university students presenting for intake at the campus counseling center between 2/1/16 and 4/14/17 (N = 998) were given the opportunity to participate in the current study.
2.2. Procedures
All counseling center intake measures were administered to students electronically via tablets. Immediately after completing all standard intake forms and questionnaires, students were offered the option to consent to the study by reading the electronic consent form and indicating whether they agree to participation. Students who chose to participate were then asked to complete the PLE screen electronically and share their other intake data, including mental health symptom ratings, with the research team.
2.3. Measures
As part of the counseling center’s intake battery, all students seeking services were asked to provide demographic information including age, sex, gender, and race/ethnicity.
2.3.1. The PRIME Screen-Revised (PRIME).
The PRIME (Miller, 2004) is a brief (12-item) psychosis-spectrum screening tool that asks respondents how much they agree that they have experienced PLEs. Ratings are based on a 7-point Likert scale, from 0 (definitely disagree) to 6 (definitely agree). For screening purposes, item responses of 5 (somewhat agree) or 6 (definitely agree) are considered positive endorsements. For the current analyses, responses were summed to create a PRIME total score. Sensitivity scores range from 0.80–1.00, specificity scores range from 0.48–1.00, and positive predictive value scores range from 0.46–0.52 (Kline and Schiffman, 2014).
2.3.2. Behavioral Health Measure-43 (BHM-43).
The BHM-43 is a 44-item self-report questionnaire that assesses well-being, mental health symptomatology, and life functioning over the past two weeks (CelestHealth Solutions, 2009; Green et al., 2003). Respondents are instructed to rate their experiences and symptoms in the past two weeks from 0 (almost always) to 4 (never). The current study used the symptoms scales of the BHM-43, which includes 29 items and 12 subscales. Subscale scores are calculated by taking an average of all item responses from each subscale, and lower scores indicate more symptomatology. For clarity in terms of interpretation, all BHM-43 subscale scores were reversed so that higher scores indicate greater severity.
For the current analyses, the sleep disorder subscale was the moderator variable, used in conjunction with the PRIME to statistically predict SI. The sleep disorder score is the average score of two questions probing the frequency of 1) difficulty falling asleep, and 2) difficulty returning to sleep. The suicide monitoring scale was the main outcome variable. An SI score was calculated by taking the average of two items that ask respondents about, 1) frequency of thoughts about ending their life (never [0] to almost always [4]) and 2) their overall risk of suicide (extremely high risk [4] to no risk [0]). The first question is strongly correlated with established measures of suicide risk (Bryan et al., 2012). The second question is only asked of respondents who endorse some suicidal thoughts (scores of 1–4) on the first question. If the first question is answered “never” (0), the answer for second question is assumed to be no risk (0).
Additionally, the following symptom subscales were included due to established links between these diagnoses and suicide risk: depression, anxiety, bipolar (i.e. mania), eating disorder, obsessive-compulsive, and alcohol/drug use (Bertolote et al., 2004; De La Cruz et al., 2017; Pompili et al., 2006; Simon et al., 2007). Several of these subscales have been validated across college student samples and demonstrated utility for monitoring client progress and outcomes (Budge et al., 2013; Kopta et al., 2014; Kopta and Lowry, 2002). Notably, adjusted scores were calculated for the depression and anxiety subscales by removing items that overlap across scales and taking an average score for the remaining items. The suicidal thoughts question was removed from the depression subscale, and one question probing “difficulty concentrating” was removed from the depression and anxiety subscales because it is typically included in both.
2.4. Data Analyses
Data was analyzed using SPSS Software (IBM Corp., 2016). Data were examined to determine acceptability for analyses. Correlations were used to explore the interrelations between SI, as measured by the BHM-43, and other variables of interest (PRIME, BHM-43 subscales). Linear regressions were used to predict SI scores from the PRIME, BHM-43 scales, and demographic variables. The interaction between sleep disorder and PRIME scores was tested to determine whether the effect of PRIME experiences on SI was moderated by level of sleep disorder. Significant findings were defined by p-values below .05, and statistical trends were defined by p-values between .05 and .10. Effect sizes were reported using Cohen’s f2 to describe small (0.02), medium (0.15), and large (0.35) effects (Cohen, 1988).
3. Results
In total, 508 students consented to the study and 442 participants had complete PRIME and BHM-43 data. Participants were 17–46 years old (M = 21.78, SD = 3.84; missing n = 35). A total of 218 students (49.3%) were white, 192 (43.4%) were persons of color (POC; 75 African American/Black, 63 Asian American/Asian,30 multiracial, 14 Hispanic/Latino, 4 American Indian or Alaskan Native, 6 other racial or ethnic identity), and 32 (7.2%) had missing race/ethnicity data. A total of 260 participants (58.8%) reported being biologically female, 158 identified as male (35.7%), and 24 (5.4%) had missing data. Twenty-six students (5.9%) identified as transgender, non-binary, genderfluid, agender, or genderqueer. Due the low base-rate of gender minority students, this category was not included in analyses.
All variables of interest (PRIME, BHM subscales) were approximately normal except for the alcohol/drug use subscale (skewness = −3.69, kurtosis = 15.22). SI (M = 0.44, SD = 0.70, range 0–3.5) was significantly correlated with the PRIME (m = 13.28, SD = 13.45, range 0–56; r = .19, p < .01; see Supplement Table 1 for correlations between PRIME items and SI). SI was also significantly correlated (p < .01) with other BHM-43 subscales: sleep disorder (r = .17), depression (r = .48), anxiety (r = .25), obsessive compulsive (r = .30), bipolar (r = .33), and eating disorder (r = .14). The alcohol/drug use subscale was not correlated with SI (nonparametric rho = .01, p = .782) and was thus dropped from subsequent analyses.
As hypothesized, linear regression results indicated that SI was positively predicted by the PRIME (Beta = .19, t(441) = 3.96, p < .001; f2 = 0.04). When controlling for demographic variables (age, sex, POC status) and BHM-43 scales, results indicated that more severe depression scores (Beta = .46, t(384) = 7.28, p < .001; f2 = 0.14) and younger age (Beta = −.13, t(384) = −2.82, p < .01; f2 = 0.02) were significant predictors of higher SI. Trend-level predictors of greater SI included higher PRIME scores (Beta = .09, t(384) = 1.75, p = .082; f2 = 0.01) and bipolar scores (Beta = .09, t(384) = 1.66, p = .098; f2 = 0.01). POC status, sex, and the sleep disorder, anxiety, obsessive compulsive, and eating disorder scales did not statistically predict SI.
An independent regression model was used to test the interaction of PRIME and sleep disorder scores in predicting SI. There was an overall effect of the three variables (PRIME, sleep disorder, and the interaction) accounting for 6% of the variance in SI scores (F (3, 438) = 10.14, p < .001). PRIME scores significantly predicted SI at high levels of sleep disorder (1 SD+ above the mean, in the “severe distress” range; Beta = 0.17, t[438] = 4.08, p < .001; f2 = 0.04), and at moderate levels of sleep disorder (within 1 SD of the mean, in the “mild distress” range; Beta = 0.11, t[438] = 3.34, p < .001; f2 = 0.03). The PRIME was not a significant predictor of SI at lower levels of sleep disorder (1 SD+ below the mean, in the “normal” range; Beta = 0.05, t[438] = 0.93, p = .351; f2 < 0.01). See Figure 1.
Figure 1.
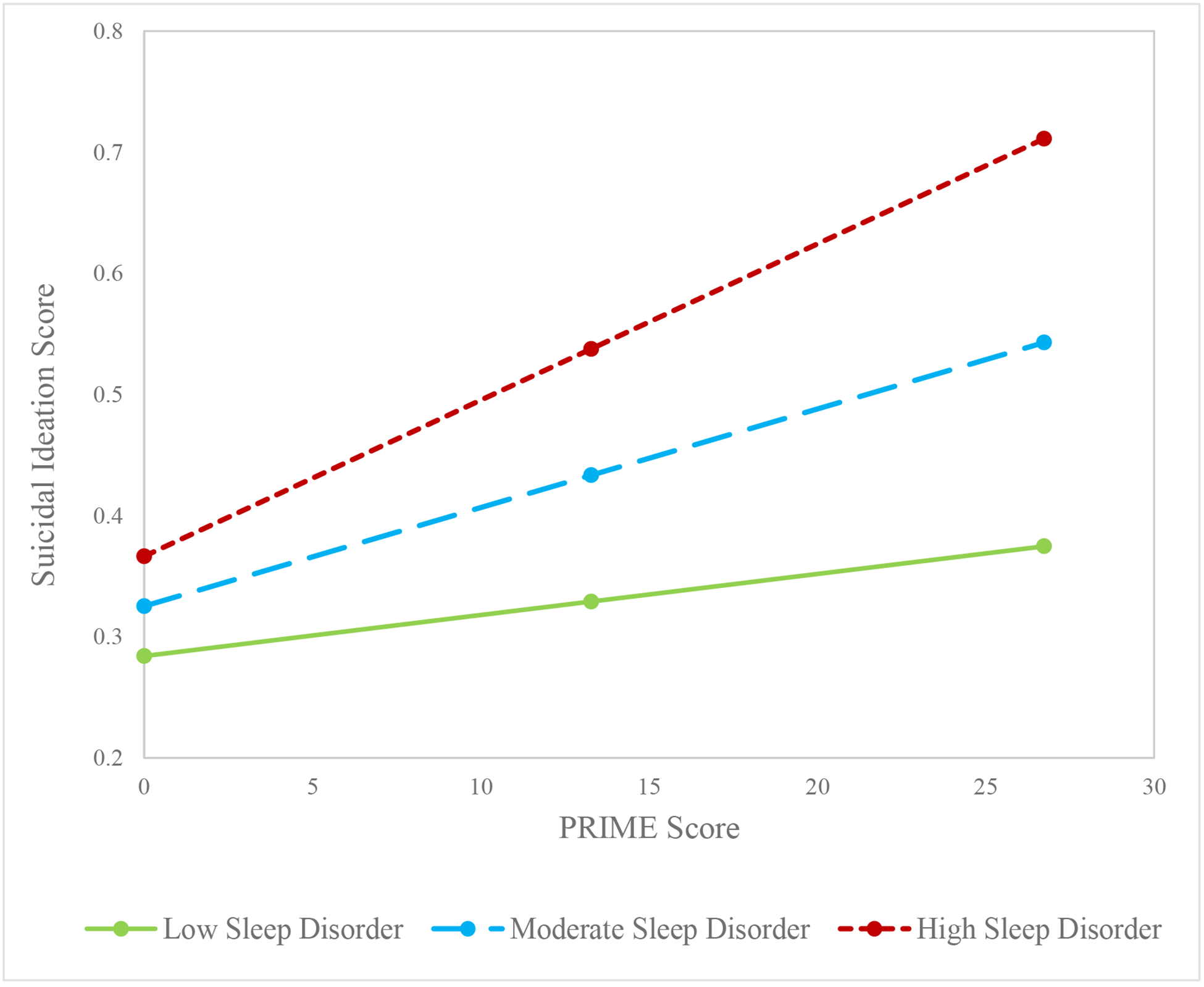
The effect of PRIME scores on suicidal ideation at high, moderate, and low levels of sleep disorder
Notably, when controlling for age and BHM-43 subscales associated with SI (i.e., depression and bipolar scores), the interaction effect was still significant. The pattern of results remained the same, except PRIME scores statistically predicted SI only at the high level of sleep disorder (Beta = 0.11, t[400] = 2.61, p < .01; f2 = 0.02), with the effect at moderate sleep disorder dropping out of significance (Beta = 0.05, t[400] = 1.67, p = .096; f2 = 0.01).
4. Discussion
The results of this study indicate that, as hypothesized, PLEs, as assessed via the PRIME, are positively, statistically predictive of SI among help-seeking college students. Small, unique effects hold beyond the significant effects of age and the BHM-43 depression scale. These regression results indicate that SI evaluations in college settings could be enhanced by assessment of PLEs.
Results also revealed an interaction effect, such that for individuals with more impaired sleep (i.e. at high and moderate levels of sleep disorder), PRIME symptoms were statistically predictive of SI. For individuals with lower levels of sleep difficulties (in the “normal” range), however, PRIME symptoms were not significant predictors of SI. These findings suggest that among individuals with PLEs, mild to severe sleep disturbances may contribute to an increased vulnerability for suicide risk, while lower levels of sleep disturbances (i.e. greater sleep quality) may act as a protective factor. Notably, the interaction between the PRIME and sleep disorder scale remained statistically significant when other clinically important covariates (i.e. depression, bipolar scores, and age) were included in the model. This finding highlights the incremental value of including PLEs, in addition to mood symptoms, in the assessment of SI, especially among university students with sleep problems.
Although the correlational design of the study prohibits causal inference and definitive conclusions, it is possible that the significant interaction observed between the PRIME and sleep quality suggests that assessing and targeting sleep hygiene among college-aged students with PLEs may lower their overall risk for suicide. Given high rates of depressive symptoms among young people with PLEs (Yung et al., 2006), the use of measures that assess both STBs and sleep in addition to mood symptoms (e.g. the Patient Health Questionnaire-9 or the Beck Depression Inventory-II) may be clinically advantageous. The likely bidirectional influence among these factors (Waite et al., 2016a) suggests that sleep interventions may also be useful for managing psychosis-spectrum experiences (Kilicaslan et al., 2017). Sleep interventions may be particularly useful in the short term or early mental health treatment, as intervention for mood symptoms and PLEs likely require more time to see clinical benefits. Additionally, mental health stigma is often a barrier to treatment engagement, and targeting sleep difficulties may be more acceptable to students during early phases of treatment (Thompson et al., 2020b). Early benefits from sleep intervention may increase client engagement while reducing stress, distress due to psychosis-related experiences and comorbid concerns, and risk for suicide (Freeman et al., 2020; Kearns et al., 2020; Reeve et al., 2019; Sheaves et al., 2019). Future research should continue to examine the effect of sleep quality on suicide risk in individuals with PLEs.
Our PRIME item-level correlational data (Supplement Table 1) are consistent with prior evidence indicating that among college students, specific types of PLEs (i.e. perceptual abnormalities and persecutory ideation) may be linked to increased SI, while other types of PLEs (i.e. bizarre experiences) may not (Capra et al., 2015; DeVylder and Hilimire, 2015). Trends such as these may be helpful to providers, as suicide risk assessment may be particularly important for students endorsing specific types of symptoms. Longitudinal research examining causal relations between specific PLEs and both sleep and suicide risk may help elucidate links between symptomatology and inform specific treatment approaches.
4.1. Limitations
Although a strong tool for screening in college settings, the BHM-43 lacks clinical depth that limits the interpretability of the scales and findings. The brief, two-item suicide monitoring scale has high face validity and likely functions adequately as an initial screening tool (Bryan et al., 2012), however, this measure neglects certain important factors to consider when evaluating and monitoring the complex and nuanced nature of the suicide risk spectrum (e.g., intensity of thoughts, suicide plan, past attempts). Similarly, the two-item sleep disorder scale measures sleep latency and maintenance insomnia to a limited extent, but it does not assess other important facets of sleep linked to suicide risk (e.g., nightmares, other types of insomnia; Li et al., 2016; Miller et al., 2019; Reeve et al., 2019). Future research would be enhanced by the use or more comprehensive measures of sleep, STB, and other risk factors, to explicitly explore the many facets of these symptom domains and their links to PLEs. Similarly, more in-depth measures of PLEs, including qualitative evaluation of clinical significance and related distress (e.g., sleep difficulties and SI), may be useful for developing targeted interventions. Despite the limited depth of the BHM-43, these screening scales may help clinicians identify areas of risk that warrant further evaluation.
4.2. Conclusions
Findings support the notion that PLEs (e.g., hallucinations and delusions) are uniquely associated with SI among help-seeking university students. Furthermore, results revealed a significant interaction between PLEs and sleep difficulties in relation to SI, such that among individuals with mild to severe sleep disturbances, PLEs were significantly associated with SI. These findings suggest a need for future research among help-seeking college students experiencing PLEs and STB, including exploration of potential interventions targeting PLEs and sleep problems to mitigate suicide risk.
Supplementary Material
Highlights.
Psychotic-like experiences (PLEs) are associated with suicidal ideation (SI)
Sleep quality moderates the relation between PLEs and SI in this university sample
For those with greater sleep difficulties, PLEs are positively associated with SI
For those with better sleep quality, PLEs are not linked to SI
Funding:
This work was supported by the Maryland Department of Health and Mental Hygiene, Behavioral Health Administration through the Maryland Center of Excellence on Early Intervention Program (MEIP) (OPASS# 14-13717G/M00B4400241to the last author.). The first author is supported by funding from the National Institute of Mental Health (K23MH119211). The funding sources had no involvement in the study design; in the collection of analysis, or interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: none. The authors do not have any conflicts of interest, including financial relationships, to disclose.
References
- Afonso P, Brissos S, Figueira ML, Paiva T, 2011. Schizophrenia patients with predominantly positive symptoms have more disturbed sleep-wake cycles measured by actigraphy. Psychiatry Res. 10.1016/j.psychres.2010.12.031 [DOI] [PubMed] [Google Scholar]
- American College Health Association (ACHA). American College Health Association-National College Health Assessment III: Reference Group Executive Summary Fall 2019., 2020. . American College Health Association, Silver Spring, MD. [Google Scholar]
- Andorko ND, Mittal V, Thompson E, Denenny D, Epstein G, Demro C, Wilson C, Sun S, Klingaman EA, DeVylder J, Oh H, Postolache TT, Reeves GM, Schiffman J, 2017. The association between sleep dysfunction and psychosis-like experiences among college students. Psychiatry Res. 248, 6–12. 10.1016/j.psychres.2016.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernert RA, Joiner TE, Cukrowicz KC, Schmidt NB, Krakow B, 2005. Suicidality and sleep disturbances. Sleep. 10.1093/sleep/28.9.1135 [DOI] [PubMed] [Google Scholar]
- Bertolote JM, Fleischmann A, De Leo D, Wasserman D, 2004. Psychiatric diagnoses and suicide: Revisiting the evidence. Crisis. 10.1027/0227-5910.25.4.147 [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Corso KA, Corso ML, Kanzler KE, Ray-Sannerud B, Morrow CE, 2012. Therapeutic Alliance and Change in Suicidal Ideation during Treatment in Integrated Primary Care Settings. Arch. Suicide Res 10.1080/13811118.2013.722055 [DOI] [PubMed] [Google Scholar]
- Budge SL, Owen JJ, Mark Kopta S, Minami T, Hanson MR, Hirsch G, 2013. Differences among trainees in client outcomes associated with the phase model of change. Psychotherapy. 10.1037/a0029565 [DOI] [PubMed] [Google Scholar]
- Capra C, Kavanagh DJ, Hides L, Scott JG, 2015. Subtypes of psychotic-like experiences are differentially associated with suicidal ideation, plans and attempts in young adults. Psychiatry Res. 10.1016/j.psychres.2015.05.002 [DOI] [PubMed] [Google Scholar]
- CelestHealth Solutions, 2009. CelestHealth Solutions Clinical Report Manual, College Counseling Version. Newburgh: CelestHealth Solutions. [Google Scholar]
- Center for Collegiate Mental Health, 2020. 2019 Annual Report (Publication No. STA 19–180) University Park, PA: CCMH. https://ccmh.psu.edu/files/2020/03/2019-CCMH-Annual-Report_3.17.20.pdf [Google Scholar]
- Cohen J, 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED, 1996. Relationships of age and axis I diagnoses in victims of completed suicide: A psychological autopsy study. Am. J. Psychiatry 10.1176/ajp.153.8.1001 [DOI] [PubMed] [Google Scholar]
- Davies G, Haddock G, Yung AR, Mulligan LD, Kyle SD, 2017. A systematic review of the nature and correlates of sleep disturbance in early psychosis. Sleep Med. Rev 10.1016/j.smrv.2016.01.001 [DOI] [PubMed] [Google Scholar]
- De La Cruz LF, Rydell M, Runeson B, D’Onofrio BM, Brander G, Rück C, Lichtenstein P, Larsson H, Mataix-Cols D, 2017. Suicide in obsessive-compulsive disorder: A population-based study of 36788 Swedish patients. Mol. Psychiatry 10.1038/mp.2016.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVylder JE, Hilimire MR, 2015. Suicide Risk, Stress Sensitivity, and Self-Esteem among Young Adults Reporting Auditory Hallucinations. Heal. Soc. Work 10.1093/hsw/hlv037 [DOI] [PubMed] [Google Scholar]
- DeVylder JE, Lukens EP, Link BG, Lieberman JA, 2015a. Suicidal ideation and suicide attempts among adults with psychotic experiences: Data from the collaborative psychiatric epidemiology surveys. JAMA Psychiatry 72, 219–225. 10.1001/jamapsychiatry.2014.2663 [DOI] [PubMed] [Google Scholar]
- DeVylder JE, Thompson E, Reeves G, Schiffman J, 2015b. Psychotic experiences as indicators of suicidal ideation in a non-clinical college sample. Psychiatry Res. 10.1016/j.psychres.2015.02.007 [DOI] [PubMed] [Google Scholar]
- Dixon WA, Rumford KG, Heppner PP, Lips BJ, 1992. Use of Different Sources of Stress to Predict Hopelessness and Suicide Ideation in a College Population. J. Couns. Psychol 10.1037/0022-0167.39.3.342 [DOI] [Google Scholar]
- Duffy ME, Twenge JM, & Joiner TE (2019). Trends in mood and anxiety symptoms and suicide-related outcomes among US undergraduates, 2007–2018: Evidence from two national surveys. Journal of Adolescent Health, 65(5), 590–598. [DOI] [PubMed] [Google Scholar]
- Freeman D, Sheaves B, Waite F, Harvey AG, Harrison PJ 2020. Sleep disturbance and psychiatric disorders. The Lancet Psychiatry, 7(7), 628–637. [DOI] [PubMed] [Google Scholar]
- Green JL, Lowry JL, Kopta SM, 2003. College students versus college counseling center clients: What are the differences? J. College Stud. Psychother 10.1300/J035v17n04_05 [DOI] [Google Scholar]
- Heron M, 2019. Deaths: Leading Causes for 2017. Natl. Vital Stat. Rep [PubMed] [Google Scholar]
- Hofstetter JR, Lysaker PH, Mayeda AR, 2005. Quality of sleep in patients with schizophrenia is associated with quality of life and coping. BMC Psychiatry. 10.1186/1471-244X-5-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang X, Fox KR, Ribeiro JD, Franklin JC, 2018. Psychosis as a risk factor for suicidal thoughts and behaviors: A meta-analysis of longitudinal studies. Psychol. Med 48, 765–776. 10.1017/S0033291717002136 [DOI] [PubMed] [Google Scholar]
- IBM Corp., 2016. IBM SPSS Statistics for Windows, Version 24.0 2016. [Google Scholar]
- Kearns JC, Coppersmith DDL, Santee AC, Insel C, Pigeon WR, Glenn CR, 2020. Sleep problems and suicide risk in youth: A systematic review, developmental framework, and implications for hospital treatment. Gen. Hosp. Psychiatry 10.1016/j.genhosppsych.2018.09.011 [DOI] [PubMed] [Google Scholar]
- Kilicaslan EE, Esen AT, Kasal MI, Ozelci E, Boysan M, & Gulec M (2017). Childhood trauma, depression, and sleep quality and their association with psychotic symptoms and suicidality in schizophrenia. Psychiatry research, 258, 557–564. [DOI] [PubMed] [Google Scholar]
- Kline E, Schiffman J, 2014. Psychosis risk screening: A systematic review. Schizophr. Res 10.1016/j.schres.2014.06.036 [DOI] [PubMed] [Google Scholar]
- Kopta SM, Lowry JL, 2002. Psychometric evaluation of the behavioral health questionnaire-20: A brief instrument for assessing global mental health and the three phases of psychotherapy outcome. Psychother. Res 10.1093/ptr/12.4.413 [DOI] [Google Scholar]
- Kopta SM, Petrik ML, Saunders SM, Mond M, Hirsch G, Kadison R, Raymond D, 2014. The Utility of an Efficient Outcomes Assessment System at University Counseling Centers. J. College Stud. Psychother 10.1080/87568225.2014.883876 [DOI] [Google Scholar]
- Lee YJ, Cho SJ, Cho IH, Jang JH, Kim SJ, 2012. The relationship between psychotic-like experiences and sleep disturbances in adolescents. Sleep Med 10.1016/j.sleep.2012.06.002 [DOI] [PubMed] [Google Scholar]
- Li SX, Lam SP, Zhang J, Yu MWM, Chan JWY, Chan CSY, Espie CA, Freeman D, Mason O, Wing Y-K, 2016. Sleep Disturbances and Suicide Risk in an 8-Year Longitudinal Study of Schizophrenia-Spectrum Disorders. Sleep. 10.5665/sleep.5852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund HG, Reider BD, Whiting AB, Prichard JR, 2010. Sleep Patterns and Predictors of Disturbed Sleep in a Large Population of College Students. J. Adolesc. Heal 10.1016/j.jadohealth.2009.06.016 [DOI] [PubMed] [Google Scholar]
- Lunsford-Avery JR, Orr JM, Gupta T, Pelletier-Baldelli A, Dean DJ, Smith Watts AK, Bernard J, Millman ZB, Mittal VA, 2013. Sleep dysfunction and thalamic abnormalities in adolescents at ultra high-risk for psychosis. Schizophr. Res 10.1016/j.schres.2013.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller BJ, Parker CB, Rapaport MH, Buckley PF, McCall WV, 2019. Insomnia and suicidal ideation in nonaffective psychosis. Sleep. 10.1093/sleep/zsy215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller T, 2004. The SIPS-Screen: a brief self-report screen to detect the schizophrenia prodrome. Schizophr. Res 70. [Google Scholar]
- Pompili M, Girardi P, Tatarelli G, Ruberto A, Tatarelli R, 2006. Suicide and attempted suicide in eating disorders, obesity and weight-image concern. Eat. Behav 10.1016/j.eatbeh.2005.12.004 [DOI] [PubMed] [Google Scholar]
- Reeve S, Sheaves B, Freeman D, 2019. Sleep Disorders in Early Psychosis: Incidence, Severity, and Association with Clinical Symptoms. Schizophr. Bull 10.1093/schbul/sby129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe C. a, Walker KL, Britton PC, Hirsch JK, 2013. The relationship between negative life events and suicidal behavior: moderating role of basic psychological needs. Crisis. 10.1027/0227-5910/a000173 [DOI] [PubMed] [Google Scholar]
- Sheaves B, Holmes EA, Rek S, Taylor KM, Nickless A, Waite F, Germain A, Espie CA, Harrison PJ, Foster R, Freeman D, 2019. Cognitive Behavioural Therapy for Nightmares for Patients with Persecutory Delusions (Nites): An Assessor-Blind, Pilot Randomized Controlled Trial. Can. J. Psychiatry 10.1177/0706743719847422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon NM, Zalta AK, Otto MW, Ostacher MJ, Fischmann D, Chow CW, Thompson EH, Stevens JC, Demopulos CM, Nierenberg AA, Pollack MH, 2007. The association of comorbid anxiety disorders with suicide attempts and suicidal ideation in outpatients with bipolar disorder. J. Psychiatr. Res 10.1016/j.jpsychires.2006.08.004 [DOI] [PubMed] [Google Scholar]
- Sjöström N, Wærn M, Hetta J, 2007. Nightmares and sleep disturbances in relation to suicidality in suicide attempters. Sleep. 10.1093/sleep/30.1.91 [DOI] [PubMed] [Google Scholar]
- Taylor PJ, Hutton P, Wood L, 2015. Are people at risk of psychosis also at risk of suicide and self-harm? A systematic review and meta-analysis. Psychol. Med 10.1017/S0033291714002074 [DOI] [PubMed] [Google Scholar]
- Thompson E, Spirito A, Frazier E, Thompson A, Hunt J, Wolff J, 2020a. Suicidal thoughts and behavior (STB) and psychosis-risk symptoms among psychiatrically hospitalized adolescents. Schizophr. Res 10.1016/j.schres.2019.12.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson EC, Fox KA, Lapomardo A, Hunt JI, Wolff JC, 2020b. Youth Self Report Thought Problems and Sleep Difficulties Are Linked to Suicidal Ideation Among Psychiatrically Hospitalized Adolescents. J. Child Adolesc. Psychopharmacol 10.1089/cap.2019.0160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG, 2019. Age, Period, and Cohort Trends in Mood Disorder Indicators and Suicide-Related Outcomes in a Nationally Representative Dataset, 2005–2017. J. Abnorm. Psychol 10.1037/abn0000410 [DOI] [PubMed] [Google Scholar]
- Waite F, Evans N, Myers E, Startup H, Lister R, Harvey AG, Freeman D, 2016a. The patient experience of sleep problems and their treatment in the context of current delusions and hallucinations. Psychol. Psychother. Theory, Res. Pract 10.1111/papt.12073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waite F, Myers E, Harvey AG, Espie CA, Startup H, Sheaves B, Freeman D, 2016b. Treating Sleep Problems in Patients with Schizophrenia. Behav. Cogn. Psychother 10.1017/S1352465815000430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H, Carney DM, Youn SJ, Janis RA, Castonguay LG, Hayes JA, Locke BD, 2017. Are we in crisis? National mental health and treatment trends in college counseling centers. Psychol. Serv 10.1037/ser0000130 [DOI] [PubMed] [Google Scholar]
- Yates K, Lång U, Cederlöf M, Boland F, Taylor P, Cannon M, McNicholas F, DeVylder J, Kelleher I, 2018. Association of Psychotic Experiences With Subsequent Risk of Suicidal Ideation, Suicide Attempts, and Suicide Deaths. JAMA Psychiatry. 10.1001/jamapsychiatry.2018.3514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yung AR, Buckby JA, Cotton SM, Cosgrave EM, Killackey EJ, Stanford C, Godfrey K, McGorry PD 2006. Psychotic-like experiences in nonpsychotic help-seekers: associations with distress, depression, and disability. Schizophrenia Bulletin, 32(2), 352–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


