Abstract
Purpose:
To describe the demographic profiles, clinical characteristics, and clinical outcomes of patients presenting with glaucoma emergencies during the COVID-19 lockdown in India.
Methods:
This retrospective, cross-sectional, observational case series involved review of medical records of all patients presenting to the glaucoma service during the COVID-19 lockdown period and comparison with the previous year (March 23 to June 23, 2020 Vs 2019) in a tertiary center in India.
Results:
We found a 78.9% reduction in overall outpatient visits (54,345 vs. 257,339; P < 0.001) and 80.9% reduction in the number of glaucoma outpatient visits (4,788 vs. 25,083; P < 0.001). Additionally, the proportion of true glaucoma emergency visits significantly increased by 62.4% in 2020 Vs 2019 (1,408/4,788 (29.4%) vs. 4,542/25,083 (18.1%); P < 0.001). Lens-induced glaucomas were the most common glaucoma surgical emergency (13.4%) in 2020. Moreover, comparison of procedures demonstrated a proportionate decrease in incisional glaucoma surgeries (70/115 (60.86%) vs. 806/939 (85.83%); P < 0.001) and an increase in the proportion of emergency cataract surgeries (129/475 (27.15%) vs. 170/2715 (6.26%); P < 0.001) and transscleral cyclophotocoagulation (45/115 (39.13%) vs. 133/939 (14.16%); P = 0.0001) during 2020 vs. 2019.
Conclusion:
Our study demonstrated a 62% increase in the proportion of visits that were true glaucoma emergencies. Additionally, the proportions of emergency cataract surgeries increased by 4.3 times and the proportion of transscleral cyclophotocoagulation increased by 2.8 times during the pandemic. More nonincisional procedures and less diagnostic testing were performed to minimize postoperative visits and virus transmission. Further understanding of the profile of emergencies may help in developing novel strategies to anticipate future challenges in managing glaucoma care during subsequent waves of the pandemic.
Keywords: Coronavirus, COVID-19, SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2 emerged in December 2019 in Wuhan, China, and led to the coronavirus disease (COVID-19) pandemic. COVID-19 continues to have an unprecedented global impact, affecting more than 39 million individuals.[1] India, like nations across the world, implemented mass quarantines, travel restrictions, the closure of religious institutions, schools, and nonessential businesses, and the delay of elective surgery and routine health maintenance visits.[2,3,4] The various stages of India's lockdown included specific restrictions and privileges that may have influenced the health-seeking behavior of patients.[5,6,7,8,9,10]
India has a high prevalence of glaucoma[11,12,13] and other blinding eye diseases.[14] While access to eye care can be a substantial issue even without COVID-19, the accommodation of millions of patients in the midst of a pandemic has been challenging.[15,16,17,18] The implementation of strict social distancing protocols has limited the number of patients that could be seen in clinic and travel restrictions prevented patients in need of care from leaving their local districts and using public transport services. In turn, healthcare providers modified usual practice patterns to allow for teleconsultation and home visits in an effort to overcome barriers to healthcare access. However, these modifications led to additional challenges as resources to utilize online consultation were limited in developing countries.[19] Finally, the employment rate in India declined to 26.1% during the lockdown; this worsening economic status may have had a bearing on payment for medications and hospital visits.[20,21]
While routine follow-up visits and elective procedures such as surgery were delayed during the lockdown, emergent glaucoma care continued to be necessary in order to prevent permanent blindness. This study aimed to describe the demographic and clinical profile of patients presenting with acute glaucoma emergencies during the lockdown period (March 23, 2020 to June 23, 2020), as compared to the same period in the previous calendar year (March 23, 2019 to June 23, 2019).
Methods
This is a retrospective, cross-sectional, observational study conducted at a tertiary eye care center in Madurai district of South India between July, 2020 and September, 2020. Our time period of interest was the lockdown period (March 23, 2020 to June 23, 2020) in India and the same period in the previous calendar year (March 23, 2019 to June 23, 2019). The study was approved by the Institutional Review Board (RET202000289) and adhered to the tenets of the Declaration of Helsinki. A general consent from patients, explaining the potential exposure risk to COVID-19 during the clinic visit was obtained. We have obtained approval from the ethics committee of our hospital on 31st August 2020.
We reviewed the electronic medical records for glaucoma patients undergoing emergent or urgent care between March 23, 2020 and June 23, 2020. The following types of visits were included in this study: 1) acute emergencies or urgencies that presented to the glaucoma service, 2) scheduled postoperative visits, and 3) referrals for primary angle closure disease requiring laser peripheral iridotomy (LPI) or cataract surgery.[22] Ocular disorders were categorized as emergent, urgent, or routine categories based on the criteria published by the All India Ophthalmic Society (AIOS) – Indian Journal of Ophthalmology guidelines during the COVID-19 pandemic.[23] Additionally, our clinic followed AIOS guidelines by restricting aerosol-generating procedures and engaged in the minimum use of diagnostic tests such as automated perimetry, optical coherence tomography, and ultrasound biomicroscopy.[23,24]
We collected demographic data including age, sex, occupation, socioeconomic status, and distance from the clinic; standardized definitions were used to describe these.[14] Patients’ subjective visual perceptions were used to define defective vision. We recorded prior ophthalmic history including presenting complaints, duration of illness, time of presentation, and prior treatment as well as the examination data including best-corrected visual acuity (BCVA), intraocular pressure (IOP), pupillary function, slit-lamp biomicroscopy, gonioscopy, and fundus examination.
We classified patients’ addresses as greater than or less than 100 km from the base hospital. Out-of-state residents were classified as such. BCVA was classified according to the WHO guidelines.[25] All glaucoma clinic patients were additionally stratified according to the severity and risk of progression: risk categories (E1, E2, E3) based on BCVA, disc appearance, and the need for more frequent visits. Category E1 contained monocular patients, BCVA <6/60, IOP >30 mmHg, cup-to-disc ratio >0.85, and those requiring close IOP monitoring to avoid progression. Category E2 included moderate to advanced glaucoma patients, with CDR between 0.7 and 0.85, IOP >30 mmHg; those on multiple antiglaucoma medications requiring follow-up visits every 4 months. Category E3 included ocular hypertensives, glaucoma suspects, and stable patients on medications requiring routine or less frequent follow-up visits.
Statistical analysis
We reviewed data from electronic medical records and entered it into a Microsoft Excel spreadsheet. Statistical analysis was performed using STATA statistical software, Version 14.0 (StataCorp, College Station, Texas, USA). Continuous variables were expressed as mean ± standard deviation or median (interquartile range), and categorical variables are presented with frequency (percentage). The normality of the data is checked using Shapiro–Wilk's test. Chi-square tests/Fisher's exact tests were used to assess the association of categorical variables and for the comparison of five lockdown periods between March 23, 2020 to June 23, 2020. Two sample proportion tests are used to compare the frequencies between the groups. Two sample t-tests/Mann–Whitney U-test are applied for the comparison of visual acuity and IOP measures between 2019 and 2020. Paired t-tests/Wilcoxon signed-rank tests are applied for the comparison of BCVA before and after laser or surgery. P values < 0.05 were considered as statistically significant.
Results
Patient characteristics
Table 1 provides a comparison of demographic details of glaucoma patient visits during the lockdown and the same time period in the year prior. Comparison (3/23/2020-6/23/2020 vs. 3/23/2019-6/23/2019) revealed a similar mean age of patients seeking an emergency glaucoma consultation (52.3 ± 18.0 years vs. 50.46 ± 17.6 years; P < 0.001) and similar sex distribution with a male preponderance (64.8% males vs. 69.1% males; P = 0.003).
Table 1.
Comparison of demographic and clinical characteristics of patients presenting to the glaucoma outpatient service between March 23 and June 23, 2019 and March 23 and June 23, 2020
| Parameters | 2019 (n=4542) n (%) | 2020 (n=1408) n (%) | Mean difference (95% CI) | Percentage change (%) and P |
|---|---|---|---|---|
| Glaucoma outpatients/Total outpatients | 25083/257339 | 4788/54345 | 0.0093 (0.0067 to 0.0120) | 80.91 (D) |
| <0.0001P | ||||
| Glaucoma emergency patients | 4542/25083 (18.1) | 1408/4788 (29.4) | -0.112 (-0.126 to -0.0992) | 62.40 (I) |
| <0.001P | ||||
| Mean age, years (SD) | 50.46±17.6 | 52.3±18.0 | -1.79 (-2.85 to -0.73) | <0.0001T |
| Sex, male/female | 3139/1403 | 913/495 | - | 0.003C |
| Patient type, new/review | 430/4112 | 198/1210 | -0.045 (-0.066 to -0.025) | 48.42 (I)/5.08 (D) |
| 0.045 (0.025 to 0.066) | <0.001C | |||
| Reasons for hospital visit, Scheduled visit | 2848 (62.7) | 840 (59.6) | 0.030 (0.001 to 0.059) | 0.0398P |
| Procedures@ | 437 (9.6) | 108 (7.7) | 0.019 (0.003 to 0.035) | 0.0266P |
| Investigations$ | 108 (2.4) | 10 (0.7) | 0.016 (0.01 to 0.023) | 0.0001P |
| Others* | 1149 (25.29) | 450 (31.96) | - 0.066 (-0.094 to -0.039) | <0.001P |
| Baseline glaucoma severity | ||||
| E1-High risk for progression | 844 (18.6) | 390 (27.7) | - 0.091 (-0.117 to -0.065) | 48.92 (I) |
| E2-Moderate risk for progression | 1162 (25.6) | 279 (19.8) | 0.057 (0.033 to 0.082) | 22.65 (D) |
| E3-No risk | 2536 (55.8) | 739 (52.5) | 0.033 (0.003 to 0.063) | 5.91 (D) |
| <0.001C | ||||
| Distance to hospital from patient’s home: | ||||
| Within 100 km in Tamil Nadu | 3291 (94.3) | 1140 (81.5) | 0.127 (0.105 to 0.149) | 13.57 (D) |
| Outside 100 km in Tamil Nadu | 199 (5.7) | 258 (18.5) | - 0.127 (-0.149 to -0.105) | 224.56 (I) |
| Total | 3490 (100%) | 1398 (100%) | <0.001C |
PProportion test; CChi-square test; TTwo-sample t-test; D-Percentage decrease; I-Percentage increase; Bolded P are significant (P<0.05); *Others - Defective vision, pain, trauma, and referral; †4.3 times more in 2020; ‡1.9 times more in 2020; @Laser suturelysis, goniopuncture, iridoplasty, and suture removal; $HFA, OCT, and Fundus photo; ¦939 glaucoma surgeries in 2019; ?115 glaucoma surgeries in 2020
Proportions of patients presenting as glaucoma emergencies to the base hospital from within 100 km distance were significantly higher than those over 100 km distance during the lockdown (1140 (81.5%) vs. 258 (18.5%); P < 0.001).
When comparing the months of lockdown to the same months in the prior year (3/23/2020–6/23/2020 vs. 3/23/2019–6/23/2019), we found a 78.9% reduction in overall outpatient visits (54,345 vs. 257,339: P <0.001) and 80.9% reduction in the number of glaucoma outpatient visits (4,788 vs. 25,083; P < 0.001). Additionally, within glaucoma outpatient visits, the proportion of true emergency visits significantly increased by 62.4% during the lockdown period vs. the same period in the prior year (1,408/4,788 (29.4%) vs. 4,542/25083 (18.1%); P < 0.001), though the actual numbers were much lower than the previous year.
Reasons for hospital visit and diagnoses
Despite a decrease in the total number of patient visits, the proportion of new patients presenting with glaucoma emergencies increased during the lockdown period as compared to the year prior (198/1408 (14.1%) vs. 430/4542 (9.5%); P < 0.001). Additionally, among risk categories, a significant increase in high-risk (E1) patients was seen in 2020 vs. 2019 (390/1408 (27.87%) vs. (844/4545 (18.6%); P < 0.001). [Table 1].
There were significant decrease in office procedures (laser suturelysis, goniopuncture, iridoplasty, suture removal) (108/1408 (7.7%) vs. 437/4542 (9.6%); P < 0.001) and glaucoma testing (visual fields, optical coherence tomography) (10/1408 (0.7%) vs. 108/4542 (2.4%); P < 0.001) in 2020 vs 2019 [Table 1].
The number of patients presenting for emergency visits reached a maximum in the most recent fifth lockdown period (n = 782) with a significant difference compared to the initial phases of lockdown (L1–L3) (n = 353) (P < 0.001). A stepwise increase in emergency visits was seen since in the first lockdown, suggesting an association between various lockdowns and lockdown reversals on the patient flow [Fig. 1].
Figure 1.
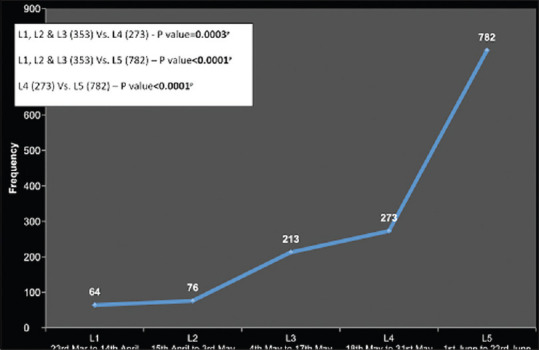
Frequency of patient visits in glaucoma clinic during the various phases of lockdown in 2020
Comparison of clinical characteristics
Table 2 provides a comparison of clinical characteristics of emergent glaucoma patient visits between the lockdown and the same time period in the year prior. During the lockdown period compared to the prior year, patients presented with worse mean uncorrected VA (logMar 1.6 ± 1.1 vs. 1.4 ± 1.0; P < 0.001) and higher mean IOP (26.9 ± 15.9 mm Hg vs. 23.0 ± 13.3 mm Hg; P < 0.001). Comparison between the two time periods revealed that the proportion of phakic people presenting with emergencies was higher during the lockdown (448/1555 (28.8%) vs. 1135/5139 (22.1%); P < 0.001).
Table 2.
Comparison of clinical evaluation findings of patients presenting with glaucoma emergencies between March 23 and June 23, 2019 and March 23 and June 23, 2020
| Parameters | 2019 n (%) | 2020 n (%) | Mean difference (95% CI) | Percentage change (%) and P |
|---|---|---|---|---|
| Presenting UCVA, Number of eyes | 5026 | 1522 | ||
| Mean (SD) in Log Mar | 1.36 (1.03) | 1.55 (1.06) | - 0.19 (-0.24 to -0.13) | <0.001M |
| Presenting BCVA, Number of eyes | 1829 | 453 | ||
| Mean (SD) in Log Mar | 1.05 (1.07) | 1.15 (1.12) | - 0.093 (-0.2 to 0.017) | 0.183M |
| Presenting IOP, Number of eyes | 4565 | 1315 | ||
| Mean (SD) | 23.01 (13.32) | 26.91 (15.86) | - 3.9 (-4.75 to -3.04) | <0.001M |
| Lens, Number of eyes | 5139 (100%) | 1555 (100%) | ||
| Pseudophakia | 1978 (38.5) | 599 (38.5) | -0.0003 (-0.27 to 0.02) | >0.99P |
| Clear lens | 1356 (26.4) | 407 (26.2) | 0.002 (-0.022 to 0.027) | 0.75 (D) and 0.875P |
| Cataract | 1135 (22.1) | 448 (28.8) | - 0.067 (-0.09 to -0.04) | 30.31 (I) and <0.001P |
| Aphakia | 657 (12.8) | 101 (6.5) | 0.062 (0.047 to 0.078) | 49.21 (D) and <0.001P |
| Subluxated | 13 (0.3) | 0 | 0.002 (0.001 to 0.0039) | 0.0471P |
| Gonioscopy, Number of eyes | 5592 (100%) | 1654 (100%) | ||
| Closed | 433 (7.7) | 169 (10.2) | - 0.024 (-0.04 to -0.008) | 32.46 (I) and 0.0014P |
| Open | 5159 (92.3) | 1485 (89.8) | 0.024 (0.008 to 0.041) | 2.7 (D) and 0.0014P |
| Fundus, Number of eyes | 4860 | 1432 | ||
| <0.85 | 1498 (30.8) | 430 (30.02) | 0.01 (-0.017 to 0.04) | 2.53 (D) and 0.4712P |
| >0.85 | 1313 (27) | 291 (20.32) | 0.07 (0.045 to 0.09) | 24.74 (D) and <0.001P |
| GOA | 160 (3.3) | 25 (1.8) | 0.015 (0.006 to 0.023) | 45.45 (D) and 0.0032P |
| No fundus view | 1889 (38.86) | 686 (47.9) | - 0.091 (-0.112 to -0.06) | 23.26 (I) and <0.001P |
MMann-Whitney U-test; PProportion test; GOA - glaucomatous optic atrophy; UCVA - Uncorrected visual acuity; BCVA - Best-corrected visual acuity; IOP - Intraocular pressure; D - Percentage decrease; I - Percentage increase; Bolded P are significant (P<0.05)
Comparison of procedures, indications for laser iridotomy, and emergency diagnosis
Comparison of procedures (3/23/2020–6/23/2020 vs. 3/23/2019–6/23/2019) revealed a decrease in the number of overall procedures (lasers and incisional surgeries) by 82.5% during the pandemic. A decrease in the proportion of LPI (231/475 (48.6%) vs. 1606/2,715 (59.2%); P < 0.001) in 2020 was seen. An increase in the proportions of transscleral diode cyclophotocoagulation (45/115 (39.13%) vs. 133/939 (14.16%); P = 0.0001) and a decrease in proportions of incisional glaucoma surgeries (70/115(60.86%)vs.806/939(85.83%); P < 0.001) were observed during the pandemic. However, the proportion of patients undergoing emergency cataract surgeries was significantly higher during the lockdown as compared to the same time period the year prior (129/475 (27.2%) vs. 170/2,715 (6.3%); P < 0.001). However, the actual numbers of these procedures was much lower than the prior year [Table 3].
Table 3.
Comparison of emergency diagnosis, laser PI, and incisional surgeries between March 23 and June 23, 2019 and March 23 and June 23, 2020
| Parameters | 2019 n (%) | 2020 n (%) | Mean difference (95% CI) | Percentage change (%) and P* |
|---|---|---|---|---|
| Emergency diagnosis, n | 4542 | 1408 | ||
| Secondary open-angle glaucoma | 2113 (46.5) | 513 (36.4) | 0.101 (0.71 to 0.13) | 21.72 (D) and <0.001 |
| Neovascular glaucoma | 1023 (22.5) | 335 (23.8) | -0.013 (0.04 to 0.01) | 5.77 (I) and 0.3211 |
| Phacomorphic glaucoma | 131 (2.9) | 114 (8.1) | -0.052 (-0.07 to -0.04) | 179.3 (I) and <0.001 |
| Secondary angle-closure glaucoma | 116 (2.6) | 78 (5.5) | -0.029 (-0.04 to -0.02) | 111.5 (I) and <0.001 |
| Phacolytic glaucoma | 129 (2.8) | 74 (5.3) | -0.025 (-0.04 to -0.01) | 89.28 (I) and <0.001 |
| Others† | 1030 (22.67) | 294 (20.88) | 0.018 (-0.01 to 0.04) | 7.89 (D) and 0.1568 |
| Procedures (Laser and surgeries), n | 2715 | 475 | 82.5 (D) | |
| Laser peripheral iridotomy, n | 1606/2715 (59.2%) | 231/475 (48.63%) | 0.104 (0.06 to 0.15) | 17.78 (D) and <0.0001 |
| Primary angle closure glaucoma | 808/1606 (50.3) | 42/231 (18.2) | 0.321 (0.27 to 0.38) | 63.81 (D) and <0.0001 |
| Primary angle closure and primary angle closure suspects | 750/1606 (46.7) | 152/231 (65.8) | -0.191 (-0.26 to -0.13) | 40.89 (I) and <0.0001 |
| Acute-angle closure glaucoma | 25/1606 (1.6) | 21/231 (9.1) | -0.74 (-0.11 to -0.04) | 468.75 (I) and <0.0001 |
| Secondary glaucoma | 19/1606 (1.2) | 14/231 (6.1) | -0.049 (-0.08 to -0.02) | 408.33 (I) and <0.0001 |
| Nanophthalmos | 4/1606 (0.3) | 2/231 (0.9) | -0.06 (-0.1 to -0.2) | 200 (I) and 0.1245 |
| Small-incision cataract surgery | 170/2715 (6.26%) | 129/475 (27.15%) | -0.208 (-0.25 to -0.17) | 333.71 (I) and <0.0001 |
| Total glaucoma surgeries (Diode and incisional surgeries), n | 939/2715 (34.58%) | 115/475 (24.2%) | 0.1 (0.06 to 0.14) | 30.02 (D) and <0.0001 |
| Transscleral cyclophotocogulation | 133/939 (14.16) | 45/115 (39.13) | -0.25 (-0.34 to -0.16) | 176.34 (I) and <0.0001 |
| Incisional surgeries | 806/939 (85.83) | 70/115 (60.86) | 0.24 (0.15 to 0.33) | 29.09 (D) and <0.0001P |
| Nonpenetrating deep sclerectomy | 15/939 (1.59) | 4/115 (3.47) | -0.19 (-0.05 to 0.12) | 118.2 (I) and 0.1525 |
| Combined trabeculectomy with cataract surgery | 505/939 (53.78) | 29/115 (25.21) | 0.28 (0.19 to 0.37) | 53.12 (D) and <0.0001 |
| Trabeculectomy | 158/939 (16.82) | 20/115 (17.39) | -0.01 (-0.08 to 0.06) | 3.38 (D) and 0.8787 |
| Glaucoma tube shunt surgery | 128/939 (13.63) | 17/115 (14.78) | -0.01 (-0.08 to 0.06) | 8.43 (D) and 0.7352 |
*Proportion test; D - Percentage decrease; I - Percentage increase; Bolded P are significant (P<0.05); †Juvenile glaucoma, traumatic glaucoma, uveitic glaucoma, steroid-induced glaucoma, acute angle-closure glaucoma, and developmental glaucoma
Small-incision cataract surgery was the most common type of emergency cataract surgery in 2020 with significant improvement in postoperative BCVA and IOP reduction (P < 0.001 for both). However, a decrease in combined triple surgery, glaucoma tubes, and trabeculectomies by 53.2, 8.4, and 3.4% with P < 0.0001, P = 0.7352, and P = 0.8787, respectively, were seen in 2020 compared to 2019, suggesting a paradigm change in glaucoma management during the pandemic [Table 3].
The most common glaucoma diagnoses seen during the lockdown were secondary open-angle glaucoma (36.4%), neovascular glaucoma (23.8%), and phacomorphic glaucoma (8.1%). During the lockdown, a higher proportion of patients received laser PI for acute-angle closure emergencies (21/231 (9.1%) vs. 25/1606 (1.6%); P < 0.0001) and secondary glaucoma (14/231 (6.1%) vs. 19/1606 (1.2%); P < 0.0001) compared to 2019 [Table 3].
Comparison of postoperative follow-up visits
Comparison (3/2020 vs. 2/2020) of scheduled postoperative follow-up visits revealed that on date follow-up (presenting on the date of scheduled postoperative follow-up visits) decreased by 43.9%, from 106 patients (65.0%) in February 2020 to 61 patients (36.5%) in March 2020 (P < 0.0001). Additionally, a 1193.9% increase was seen in loss to follow-up with four patients (2.4%) in February 2020 to 53 patients (31.7%) in March 2020 (P < 0.0001) [Fig. 2].
Figure 2.
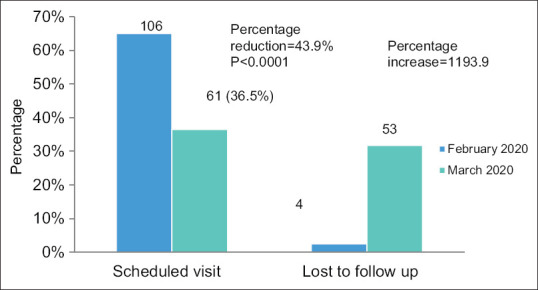
Comparison of postoperative scheduled visit and lost to follow-up between the first lock down (L1) and the previous month (February 2020)
Discussion
Our study compared glaucoma emergency care during the COVID-19 pandemic and its related 3-month shutdown in India as compared to the same time period the year prior. As compared to 2019, we observed a significant decline in overall outpatient visits during the lockdown by 78.9%, glaucoma outpatient visits by 80.9%, and the mean number of glaucoma patients seen per day also decreased by 80.7%, which corroborated with reports from other specialties.[26,27,28] However, despite an overall decline in number of emergency patient visits during the lockdown, we found an increase in the proportion of glaucoma emergencies by 62% as compared with the previous year. Additionally, we observed that the proportion of emergency cataract surgeries increased by 4.3 times and the proportion of transscleral cyclophotocoagulation increased by 2.8 times during the pandemic. We attribute these observations to the termination of all the routine outpatient visits and elective procedures, which led to overall lower total numbers during the lockdown and relatively high proportions of emergency visits and procedures.
Despite the lower frequency of surgery during the lockdown months, adherence to postoperative visits decreased by half. Additionally, out-of-state patients presented less frequently, likely related to travel restrictions. Our findings demonstrate a significant increase in emergent visits and a dramatic decline in maintenance visits, highlighting a potential increase in vision loss during these months. Our study, like others, suggest that the substantial impact of lockdown guidelines was evident by the health-seeking behavior of patients during the pandemic.[29,30,31]
We observed gender inequalities in seeking healthcare, similar to prior analyses.[29,30,31,32,33] Our cohort was predominantly male (64.8%) during the pandemic and the year prior (69.1%), with a significant increase in the disparity of men vs. women in all except the third lockdown phase (P = 0.003). Similarly, Das et al.[29] demonstrated less frequent presentation of vulnerable groups such as females (37.8%), those of low socioeconomic status (27.3%), pediatric age (22.1%), and those living more than >100 km (9.7%). These findings highlight the disparity in healthcare access, even for emergency care, during the pandemic.
Similar to our study, Das et al.[29] recently reported on the demographic and clinical profiles of 1192 patients seen during the COVID-19 pandemic. That study triaged 775 patients (65.0%) as ocular emergencies, with 97 patients (8.1%) requiring general urgent eye care, and 32 patients (4.1%) requiring medical or surgical treatment for a glaucoma emergency. Although Das et al.’s[29] rate of glaucoma emergencies was lower than ours, they demonstrated a significant increase in overall emergencies during the lockdown as compared to 1 month prior (40.3% vs. 24.7%).
Similarly, Posarelli et al.,[30] recently reported a significant increase in nondeferrable urgency visits and decrease in overall emergencies in the lockdown period when compared with the 1-month prelockdown and the same time period in 2019. In addition to the increase in glaucoma emergencies, we observed a 48.9% increase in high-risk patients (E1) and a 48.4% increase in new cases presenting as emergencies during the lockdown compared to 2019. Of patients who presented with glaucoma emergencies during the lockdown, the reasons for hospital visits varied significantly and the nature of emergencies appeared to be more severe than the year prior, as our cohort presented with greater vision loss, higher IOP, advanced cataracts, and severe optic disc damage.
Among glaucoma emergencies, lens-induced etiologies were the most common during the lockdown, with 129 patients undergoing emergency cataract surgery. Interestingly, the proportions of acute angle-closure were 5.68 times higher, phacomorphic glaucomas was 2.8 times higher, and phacolytic glaucoma was 2 times higher in 2020 as compared to 2019, though the total number of emergencies were fewer during the lockdown. Small-incision cataract surgery performed for lens-induced emergencies in both the studied periods showed significant improvement in postoperative visual acuity and IOP reduction from baseline, but IOP reduction was greater in 2019. This may have been related to the delayed presentation during the lockdown; greater lens-induced inflammation may have led to major trabecular outflow system obstruction with poor IOP response postsurgery.
Although the proportion of emergency cataract surgeries was 4.3 times higher during the lockdown, we witnessed a significant decline in the total number of glaucoma surgeries by 30% compared to the same time period the year prior (115/475 (24.2%) vs. 939/2,715 (34.58%); P < 0.001). This finding may reflect a preference for more conservative approaches requiring fewer postoperative visits during the pandemic. Accordingly, the proportions of cyclophotocoagulation procedures and nonpenetrating deep sclerectomy were increased and the proportions of office procedures and diagnostic testing were reduced. Additionally, there was a decrease in the proportions of trabeculectomies, tube shunts, and phacotrabeculectomy by 3.38, 8.43, and 53.12%, respectively, during the pandemic vs. the same time period the year prior. Similarly, a study in Italy reported fewer invasive surgeries and greater proportions of laser and nonpenetrating surgeries during the pandemic compared to the same months in 2019.[34] This reflects the conscious effort of the eye care providers to avoid recommending elective procedures and referrals and the hesitance of the patients to enter the hospital for care. The complexity of disinfecting instruments and potential restrictions may have also posed as impediments to care.
Additionally, we found a 43.9% reduction in scheduled postoperative visits with a 1193.9% increase in lost-to-follow-up rates compared to 1 month before lockdown. A substantial proportion of these postoperative patients were in critical or advanced stages of disease; possible progression during the lockdown may have greatly impacted visual status, as evidenced by prior studies.[35]
Significant challenges remain in identifying these patients and rescheduling them for follow-up visits in the future months. An option of teleconsultation was offered to our patients to address this issue; however, there was a poor response during the initial phases of lockdown.
Eye care providers will thus need to develop strategies to address the immense backlog in the postlockdown period by encouraging stable, low-risk patients and elderly patients to seek eye care locally or via telemedicine. Additionally, we could trace high-risk patients from existing databases and prioritize them for follow-up visits in an effort to offer the most vulnerable individuals optimal care. Furthermore, reinforcement of healthy practices using patient education sessions with special emphasis on both mental and eye health is warranted. Several challenges still remain, as the risk of virus transmission may persist even after the vaccination.
Conclusion
To the best of our knowledge, this is the first study reporting the demographic and clinical profile of glaucoma emergencies during the acute phase of COVID-19. Our findings suggest that patients with glaucoma emergencies sought care despite the risk of disease contraction and government-imposed restrictions. Lens-induced glaucomas were the most common glaucoma surgical emergency during the pandemic among our clinical population. Fewer glaucoma diagnostic studies and more nonincisional procedures such as transscleral cyclophotocoagulation were performed to minimize postoperative visits. Further understanding of the profile of emergencies may help in developing novel strategies to anticipate future challenges in managing glaucoma care during subsequent waves of the pandemic. A paradigm shift in eye care delivery with greater teleconsultation may help accommodate previously deferred visits and prevent unnecessary exposure for patients who can be adequately monitored from home.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Johns Hopkins University. COVID.19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) [Last accessed on 2021 Mar 13]. Available from: https://coronavirus.jhu.edu/map.html .
- 2.Boulle A, Davies MA, Hussey H, Ismail M, Morden E, Vundle Z, et al. Risk factors for COVID-19 death in a population cohort study from the Western Cape Province, South Africa? Clin Infect Dis. 2020:ciaa1198. doi: 10.1093/cid/ciaa1198. doi: 10.1093/cid/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu W, Yue XG, Tchounwou PB. Response to the COVID-19 epidemic: The Chinese experience and implications for other countries. Int J Environ Res Public Health. 2020;17:2304. doi: 10.3390/ijerph17072304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Business Insider. Our ongoing list of how countries are reopening, and which ones remain under lockdown. Business Insider. [Lastaccessed on 2021 Mar 13]. Available from: https://www.businessinsider.nl/countries-onlockdown-coronavirus-italy-2020-3?international=true and r=US .
- 5.Government of India, Ministry of Home Affairs. Guidelines on the measures to be taken by Ministries/Department of Government of India, State/Union Territory Government and State/Union Territory authorities for containment of COVID-19 epidemic in the country. Published March 24, 2020. [Last accessed on 2021 Mar 13]. Available from: https://www.mohfw.gov.in/pdf/Annexure_MHA.pdf .
- 6.Government of India, Ministry of Home Affairs. Consolidated revised guidelines on the measures to be taken by Ministries/Department of Government of India, State/UT Goverments and State/UT authorities for containment of COVID-19 in the country. Published April 15, 2020. [Last accessed on 2021 Mar 13]. Available from: https://www.mha.gov.in/sites/default/files/MHA%20order%20dt%2015.04.2020%2C%20with%20Revised%20Consolidated%20Guidelines_compressed%20%283%29.pdf .
- 7.Red, Orange, Green Zone district-wise list for coronavirus lockdown: Complete classification of areas in India. India Today 1 May 2020. [Last accessed on 2021 Mar 13]. Available from: https://www.indiatoday.in/india/story/lockdown-extended-list-of-activities-prohibited-acrosscountry-1673428-2020-05-01 .
- 8.Government of India, Ministry of Home Affairs. New guidelines on the measures to be taken by Ministries/Departments of Government of India, State/UT authorities for containment of COVID-19 in the country for the extended period of National lockdown for a further period of two weeks with effect from 4th May 2020. Published May 1, 2020. [Last accessed on 2021 Mar 13]. Available from: https://www.mha.gov.in/sites/default/files/MHA%20Order%20Dt.%201.5.2020%20to%20extend%20Lockdown%20period%20for%202%20 weeks%20w.e.f.%204.5.2020%20with%20new%20guidelines.pdf .
- 9.Government of India, Ministry of Home Affairs. Guidelines on the measures to be taken by Ministries/Departments of Government of India, State/UT Governments and State/UT authorities for containment of COVID-19 in the country upto 31st May, 2020. Published May 17, 2020. [Last accessed on 2021 Mar 13]. Available from: https://www.mha.gov.in/sites/default/files/MHAOrderextension_1752020_0.pdf .
- 10.Government of India, Ministry of Home Affairs. Guidelines for Phased Re-opening (Unlock 1). Published May 30, 2020. [Last accessed on 2021 Mar 13]. Available from: https://www.mha.gov.in/sites/default/files/MHAOrderDt_30052020.pdf .
- 11.Ramakrishnan R, Nirmalan PK, Krishnadas R, Thulasiraj RD, Tielsch JM, Katz J, et al. Glaucoma in a rural population of southern India: The Aravind comprehensive eye survey. Ophthalmology. 2003;110:1484–90. doi: 10.1016/S0161-6420(03)00564-5. [DOI] [PubMed] [Google Scholar]
- 12.Paul C, Sengupta S, Choudhury S, Banerjee S, Sleath B. Prevalence of glaucoma in Eastern India: The Hooghly River Glaucoma study. Indian J Ophthalmol. 2016;64:578–83. doi: 10.4103/0301-4738.191497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Palimkar A, Khandekar R, Venkataraman V. Prevalence and distribution of glaucoma in central India (Glaucoma Survey – 2001) Indian J Ophthalmol. 2008;56:57–62. doi: 10.4103/0301-4738.37597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Das AV, Podila S, Prashanthi GS, Basu S. Clinical profile of pterygium in patients seeking eye care in India: Electronic medical records-driven big data analytics report III. Int Ophthalmol. 2020;40:1553–63. doi: 10.1007/s10792-020-01326-3. [DOI] [PubMed] [Google Scholar]
- 15.Kullgren JT, McLaughlin CG, Mitra N, Armstrong K. Nonfinancial barriers and access to care for U.S. adults. Health Serv Res. 2012;47:462–85. doi: 10.1111/j.1475-6773.2011.01308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: Transportation barriers to health care access. J Community Health. 2013;38:976–93. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rust G, Ye J, Baltrus P, Daniels E, Adesunloye B, Fryer GE. Practical barriers to timely primary care access: Impact on adult use of emergency department services. Arch Intern Med. 2008;168:1705–10. doi: 10.1001/archinte.168.15.1705. [DOI] [PubMed] [Google Scholar]
- 18.Barik D, Thorat A. Issues of unequal access to public health in India. Front Public Health. 2015;3:245. doi: 10.3389/fpubh.2015.00245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhai Y. A call for addressing barriers to telemedicine: Health disparities during the COVID-19 pandemic. Psychother Psychosom. 2021;90:64–6. doi: 10.1159/000509000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raj V, Bahl G. Coronavirus (COVID-19) and its spillovers on Indian economy. 2020. International online Academic Conference on the Impact of the Coronavirus, June 2020. [Last accessed on 2021 Mar 13]. Available from: https://www.researchgate.net/publication/342051894_Coronavirus_COVID-19_and_its_Spillovers_on_Indian_Economy .
- 21.Gopalan HS, Misra A. COVID-19 pandemic and challenges for socio-economic issues, healthcare and National Health Programs in India. Diabetes Metab Syndr. 2020;14:757–9. doi: 10.1016/j.dsx.2020.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jiang Y, Friedman DS, He M, Huang S, Kong X, Foster PJ. Design and methodology of a randomized controlled trial of laser iridotomy for the prevention of angle closure in southern China: The Zhongshan angle closure prevention trial. Ophthalmic Epidemiol. 2010;17:321–32. doi: 10.3109/09286586.2010.508353. [DOI] [PubMed] [Google Scholar]
- 23.Sengupta S, Honavar SG, Sachdev MS, Sharma N, Kumar A, Ram J, et al. All India Ophthalmological Society-Indian Journal of Ophthalmology consensus statement on preferred practices during the COVID-19 pandemic. Indian J Ophthalmol. 2020;68:711–24. doi: 10.4103/ijo.IJO_871_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American Academy of Ophthalmology. New recommendations for urgent and nonurgent patient care. [Last accessed on 2021 Mar 13]. Available from: https://www.aao.org/headline/new-recommendationsurgent-nonurgent-patient-care .
- 25.World Health Organization. Change the Definition of Blindness. [Last accessed on 2021 Mar 13]. Available from: https://www.who.int/blindness/Change%20the%20Definition%20of%20Blindness.pdf .
- 26.Viola F, Milella P, Giuffrida FP, Ganci S, Invernizzi A. The impact of coronavirus disease (COVID-19) pandemic on intravitreal injections treatment for macular diseases: Report from a referral hospital in Milan. Retina. 2020 doi: 10.1097/IAE.0000000000002941. doi: 10.1097/IAE.0000000000002941. [DOI] [PubMed] [Google Scholar]
- 27.Lanni V, Iuliano A, Laezza MP, Uccello G, Tranfa F, Strianese D. Oculoplastic management of patients in the Covid-19 era: Experience from an Italian tertiary referral center. Orbit. 2020;39:391–3. doi: 10.1080/01676830.2020.1775264. [DOI] [PubMed] [Google Scholar]
- 28.Toro M, Choragiewicz T, Posarelli C, Figus M, Rejdak R. On Behalf of European C-CG. Early impact of covid-19 outbreak on the availability of cornea donors: Warnings and recommendations. Clin Ophthalmol. 2020;14:2879–82. doi: 10.2147/OPTH.S260960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Das A, Narayanan R. Demographics and clinical presentation of patients with ocular disorders during the COVID-19 lockdown in India: A report. Indian J Ophthalmol. 2020;68:1393–9. doi: 10.4103/ijo.IJO_1171_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Posarelli C, Maglionico MN, Covello G, Loiudice P, Cipriano A, Santini M, et al. Ophthalmological emergencies and the SARS-CoV-2 outbreak. PLoS One. 2020;15:e0239796. doi: 10.1371/journal.pone.0239796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kannan N, Kohli P, Mishra C, Sen S, Arthur D, Chhablani D, et al. To evaluate the effect of COVID-19 pandemic and national lockdown on patient care at a tertiary-care ophthalmology institute. Indian J Ophthalmol. 2020;68:1540–4. doi: 10.4103/ijo.IJO_1673_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pellegrini M, Roda M, Lupardi E, Di Geronimo N, Giannaccare G, Schiavi C. The impact of COVID-19 pandemic on ophthalmological emergency department visits. Acta Ophthalmol. 2020 doi: 10.1111/aos.14489. doi: 10.1111/aos. 14489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ye Q, Chen Y, Yan W, Wang W, Zhong J, Tang C, et al. Female gender remains a significant barrier to access cataract surgery in south Asia: A systematic review and meta-analysis. J Ophthalmol 2020. 2020 doi: 10.1155/2020/2091462. 2091462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Quaranta L, Micheletti E, Riva I. Glaucoma surgery during the covid-19 pandemic in Italy: How novel coronavirus has changed the surgical management of glaucoma patients. J Glaucoma. 2020;29:831–32. doi: 10.1097/IJG.0000000000001642. [DOI] [PubMed] [Google Scholar]
- 35.Abdelmotaal H, Ibrahim W, Sharaf M, Abdelazeem K. Causes and clinical impact of loss to follow-up in patients with proliferative diabetic retinopathy. J Ophthalmol 2020. 2020 doi: 10.1155/2020/7691724. 7691724. [DOI] [PMC free article] [PubMed] [Google Scholar]


