Abstract
We present a Coronavirus disease 2019 (COVID-19) patient who developed sudden bilateral vision loss after a bilateral occipital ischemic stroke and without a history of stroke risk factors. An 84-year-old man was admitted to the emergency room with bilateral sudden vision loss while receiving Favipiravir treatment for 5 days following a COVID-19 diagnosis. The patient had no history of stroke risk factors, such as hypertension, diabetes mellitus, coronary artery disease, or arrhythmia. Diffusion magnetic resonance imaging of the patient revealed acute ischemia in the bilateral posterior occipital lobe and bilateral cerebellar hemisphere. We conclude that COVID-19 may rarely cause bilateral ischemic stroke presented only in the form of vision loss.
Keywords: Bilateral vision loss, COVID-19, stroke
Coronavirus disease-19 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) usually occurs with pneumonia symptoms, such as fever, dry cough, and shortness of breath.[1] Rarely, more complex symptoms may accompany the disease. Published studies have demonstrated that COVID-19 can cause certain cerebrovascular events (usually ischemic stroke).[2,3,4] Studies claim that various mechanisms may be involved in the development of ischemic stroke due to COVID-19.[3,5] Recent studies show that SARS-CoV-2 causes thromboembolism secondary to hypercoagulopathy.[3] This case study reports the clinical, laboratory, and radiological findings of a COVID-19 patient who presented with sudden bilateral vision loss after bilateral occipital ischemic stroke without any stroke risk factors.
Case Report
An 84-year-old male was admitted to the Sakarya University Training and Research Hospital Emergency Department with sudden bilateral vision loss while quarantining at home and receiving Favipiravir treatment for 5 days due to COVID-19. The patient's SARS-Cov-2 reverse transcription polymerase chain reaction test, which was performed using a nasopharyngeal swab 5 days ago, was positive. Thoracic computed tomography of the patient was compatible with the COVID-19 diagnosis. During the initial examination of the patient, electrocardiography (ECG) was in normal sinus rhythm, and O2 saturation, arterial tension, and pulse were 91%, 140/90 mmHg (systolic/diastolic), and 80/min, respectively. A detailed ophthalmic examination of the patient showed his bilateral vision to be at the level of “hand motion” and the intraocular pressure to be 15/16 mmHg. Anterior and posterior segment examinations were normal. The patient's bilateral direct/indirect light reflex was normal. The patient was conscious, oriented, and cooperative during the neurological examination. Cranial nerve, motor, and cerebellar system examinations were normal in the patient. The patient did not have a history of stroke risk factors, such as hypertension, diabetes mellitus, coronary artery disease, or arrhythmia. Also, there was no history of stroke in the patient's family. Diffusion magnetic resonance imaging of the patient revealed acute ischemia in the bilateral posterior occipital lobe and bilateral cerebellar hemispheres [Figs. 1-3]. The echocardiography of the patient was evaluated as normal. The cardiologic evaluation of the patient also showed no abnormal findings that would pose a risk for stroke. Furthermore, the computed tomography angiography of the patient was normal.
Figure 1.
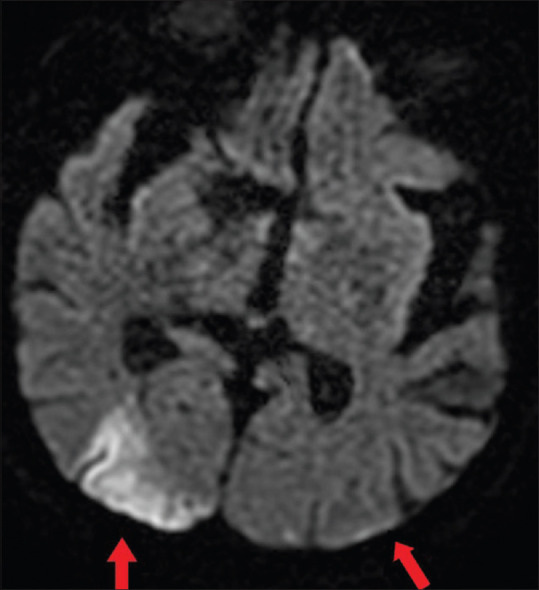
MRI section showing bilateral ischemic areas in the occipital lobe (arrows)
Figure 3.
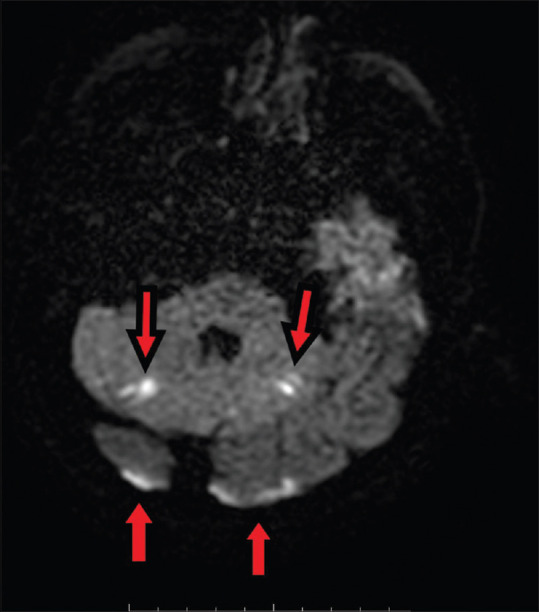
MRI section showing bilateral ischemic areas in the occipital lobe and cerebellum (arrows)
Figure 2.
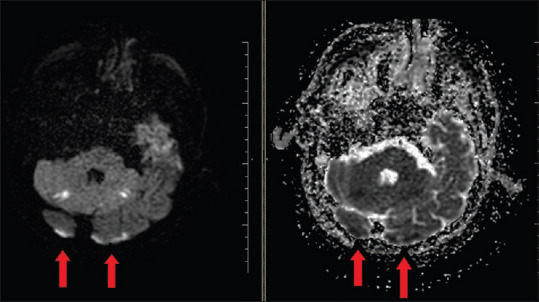
MRI section showing bilateral ischemic areas in the occipital lobe and cerebellum (arrows)
The patient's serum D-dimer, C-reactive protein, lactate dehydrogenase, and neutrophil count levels were elevated (5170 μg/L, 292.50 mg/L, 614 U/L, and 9.79 109/L, respectively). In addition, the patient's serum lymphocyte count and platelet count levels were low (0.370 and 120 109/L, respectively). Other blood serum parameters were normal. Based on the present findings, the patient was diagnosed with ischemic stroke in the basilar artery and bilateral posterior cerebral artery region and treated in the intensive care unit. Antiedema and anticoagulant therapy were added to the patient's treatment.
Discussion
According to past studies and review articles, the rate of ischemic stroke development in COVID-19 is 5%, and it develops within the first 10 days after the diagnosis of the disease.[6] Previous studies mention certain mechanisms responsible for the development of stroke associated with SARS-CoV-2 infection. These mechanisms are hypercoagulation, vasculitis secondary to intracranial cytokine storm, and atrial fibrillation (cardiomyopathy).[7] Hypercoagulation state and subsequent thromboembolism is the most accepted mechanism of stroke development.[6,8] Elevated D-dimer levels and decreased platelet levels in COVID-19 patients support this hypothesis. Our patient also exhibited high D-dimer levels and diminished platelet levels. In ischemic strokes due to COVID-19, clinical symptoms are usually accompanied by cognitive disorders and motor deficits. In the case series published by Beyrouti et al.[4] six patients who developed ischemic stroke due to COVID-19 were examined, and all of them showed motor deficits and/or cognitive disorders in their neurological examination. In the case reports published by Elkhider and his colleagues[5] all four patients who had a stroke due to COVID-19 exhibited motor deficits. Our patient presented to the emergency department because of the sudden loss of vision, and interestingly, he did not have any neurological motor deficits and his cognitive level was good. Arrhythmias such as atrial fibrillation are complications due to COVID-19.[9] Thromboembolism due to atrial fibrillation can also cause an acute ischemic stroke. However, ECG and echocardiography findings were normal in our patient. Therefore, we did not consider thromboembolism due to atrial fibrillation in our patient.
Conclusion
COVID-19 may rarely cause a bilateral ischemic stroke. Further research is needed to elucidate the mechanism of ischemic stroke development associated with COVID-19.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Pascarella G, Strumia A, Piliego C, Bruno F, Del Buono R, Costa F, et al. COVID-19 diagnosis and management: A comprehensive review. J Intern Med. 2020;288:192–206. doi: 10.1111/joim.13091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with Coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683–90. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reddy ST, Garg T, Shah C, Nascimento FA, Imran R, Kan P, et al. Cerebrovascular disease in patients with COVID-19: A review of the literature and case series. Case Rep Neurol. 2020;12:199–209. doi: 10.1159/000508958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beyrouti R, Adams ME, Benjamin L, Cohen H, Farmer SF, Goh YY, et al. Characteristics of ischaemic stroke associated with COVID-19. J Neurol Neurosurg Psychiatry. 2020;91:889–91. doi: 10.1136/jnnp-2020-323586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elkhider H, Ibrahim F, Sharma R, Sheng S, Jasti M, Lotia M, et al. COVID-19 and stroke, a case series and review of literature. Brain Behav Immun Health. 2020;9:100172. doi: 10.1016/j.bbih.2020.100172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spence JD, de Freitas GR, Pettigrew LC, Ay H, Liebeskind DS, Kase CS, et al. Mechanisms of stroke in COVID-19. Cerebrovasc Dis. 2020;49:451–8. doi: 10.1159/000509581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP, et al. Large-Vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020;382:e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ortega-Paz L, Capodanno D, Montalescot G, Angiolillo DJ. COVID-19 associated thrombosis and coagulopathy: Review of the pathophysiology and implications for antithrombotic management. J Am Heart Assoc. 2020;10:e019650. doi: 10.1161/JAHA.120.019650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rasmussen PV, Blanche P, Strange JE, Butt JH, Dalgaard F, Kragholm K, et al. Thromboembolic events related to atrial fibrillation during the COVID-19 epidemic in Denmark. Thromb Res. 2020;194:220–1. doi: 10.1016/j.thromres.2020.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]


