Abstract
Perceptual visual dysfunction (PVD) comprises a group of vision disorders resulting from dysfunction of the posterior parietal and/or temporal lobes. Often, affected children have normal/near normal visual acuities and/or visual fields, but have difficulties in activities of daily living involving the use of vision. PVDs are known to be common among children with risk factors such as a history of prematurity and/or neurodevelopmental disorders. The inferior temporal lobes and ventral stream transform visual signals into perception, while the posterior parietal lobes and dorsal stream transform visual signals to non-consciously map the scene to guide action and facilitate attention. Dysfunction of these can lead to specific visual impairments that need to be identified during history taking, triggering ascertainment of further details by a structured inventory approach. Clinical tests to elicit dorsal and ventral stream visual dysfunctions have good specificity but low sensitivity. Neuropsychologists are rarely available in the developing world to perform detailed assessments, but there are a few tests that can be used by eye care professionals with some training. Optical coherence tomography (OCT) showing thinning of the ganglion cell layer and retinal nerve fiber layer is being explored as a potential tool for rapid assessment in the clinic. The behavioral outcomes of PVD can mimic psychological conditions including autism spectrum disorder, attention deficit hyperactivity disorder, specific learning disability, and intellectual impairment, and one needs to be aware of overlap among these differential diagnoses. A practical functional approach providing working solutions for each child's set of difficulties in day-to-day activities is needed.
Keywords: Cerebral visual impairment, cognitive visual impairment, developing world, higher visual functions, perceptual visual dysfunction
Perceptual visual dysfunction (PVD) comprises a group of vision disorders resulting from anomalies of higher visual functions, affecting the higher visual centres in the posterior parietal and temporal lobes.[1] Typically, parents notice these children being unable to perform certain everyday visual tasks, yet to be functioning well in other areas of activity. When tested in the clinic, many can have normal or near-normal primary visual functions like visual acuities and visual fields, nevertheless they can be significantly visually disabled.
Epidemiology
There are no population-based data available concerning the prevalence of PVD among children owing to lack of definitive diagnostic criteria and poor awareness about the entity among eye care professionals. Mitry D et al. found that in a cohort of children with cerebral palsy (CP) in Bangladesh, 53% had PVD.[2] Macintyre-Béon C et al. reported a prevalence of 21-47% (95% confidence intervals, 15 out of 46 children) for PVD among hitherto undiagnosed prematurely born children attending mainstream schools in Scotland.[3] In another study from Scotland, Gorrie F & et al. estimated a prevalence of PVD of 23-39% among children with different diagnoses of neurodevelopmental disorders (total 535 children).[4] One of our earlier studies showed that PVD comprised 11.2% (14 out of 124) of all children with CVI seen at a tertiary level eye centre in South India over a period of one year.[5] Thus it is clear that the prevalence of PVD is high among children with risk factors such as prematurity and neurodevelopmental disorders such as CP. In response to this upcoming trend, the Government of India has already established 92 District Early Intervention centers (DEICs) as a part of the Rashtriya Bala Swasthya Karyakram (RBSK) initiative, and 366 more have been approved for different parts of the country, to ensure early diagnosis and intervention for children with brain injury. Awareness about this facility among ophthalmologists is important for appropriate referrals of children with neurodevelopmental disorders to these DEICs for them to receive the various therapies and habilitational approaches they need.[6]
Higher Visual Functions
The term higher visual function,[7] includes visual perception, visual cognition, visual attention and visual guidance of movement. Visual perception refers to becoming aware of something, through seeing.
Visual cognition concerns the mental process of interpreting incoming visual information for recognition and thinking about its significance, relating this information to known the imagery in memory. Visual attention refers to the capacity to attend visually to objects of interest within the visual scene. Visual guidance of movement encompasses mapping of visual information in the mind and using this to guide movement of the limbs and body. Disorders of these functions are called, cognitive or PVDs or higher functioning cerebral visual impairments. These can exist in the presence or absence of issues with primary processing of vision i.e., visual acuity, visual field, color vision and contrast sensitivity.
Higher Visual Processing
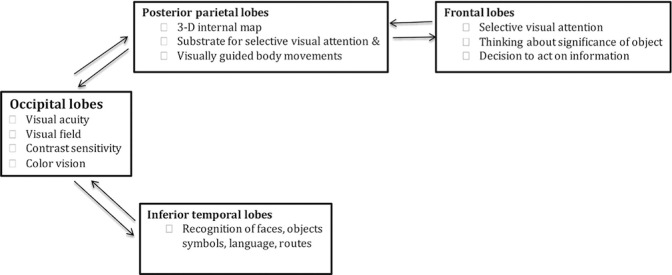
There are two broad functional divisions in our visual brains, each one with a specific task. These are called the dorsal and the ventral streams. Newcombe F and Russel WR were early reporters of the functional differences in clinical features of injuries to the parietal and temporal lobes among patients with injuries sustained during World War II.[8] The concept of two visual streams serving distinct visual functions was first published by two eminent American Neuroscientists, Leslie Ungerleider and Mort Mishkin in 1982 based on evidence gathered from experiments on monkeys[9] and later consolidated for man by Milner and Goodale.[10] Primary processing of the incoming image data for visual acuity, visual fields, color vision and contrast sensitivity takes place within the occipital lobes. After this initial processing, the visual information is carried from the occipital lobes by a connecting pathway, called the ‘dorsal stream’ (also known as the ‘vision for action’ pathway), to the intraparietal sulcus (IPS) in the posterior parietal lobes, and another connecting pathway, called the ‘ventral stream’ (also known as the ‘vision for perception’ pathway), to the inferior temporal lobes.[11]
Fig. 1 showing details of vision processing in brain, ascertained from studies of patients with focal brain injury.
Figure 1.
Showing details of vision processing in brain
Processing in the posterior parietal lobes
The posterior parietal lobes serve the following functions:
a. Non-conscious moment-to-moment synthesis of the structure of the visual scene, and passing this framework to the frontal lobes to accord attention to an object of interest: While alert, we are bombarded with a lot of visual information. Our posterior parietal lobes, without our knowing, map the overall visual scene and send this information via the superior longitudinal fasciculus to the frontal lobes, which choose a corresponding element of interest in the scene (provided by the image analysis system in the temporal lobes) to attend to at any one time.[12]
b. Creating an up to date mental virtual three-dimensional map of the external surrounding world: The posterior parietal lobes create a three dimensional map of the external world in our minds, which is refreshed from moment-to-moment. This helps us perform all our visually guided actions with precision and allows us to move efficiently through our surroundings without bumping into people or obstacles. Similar processing also takes place for sound, the direction of which is mapped in nearby areas.[13]
c. Visual guidance of body movements: As the posterior parietal lobes give us information about the locations, dimensions and distances of objects in relation to our body, these measures are used to facilitate our movement through the environment including calibration of the gap between our fingers and thumb as we reach with precision to pick up an object. Brain cells and their neurones in the posterior parietal lobes are clustered in separate regions, with each having a specialist function. For example ‘visuomotor function’ (action based on visual input) is located in the ‘lateral intraparietal area’ (LIP) linked to the frontal eye fields that direct fast eye movement to the target of interest, and the ‘parietal reach region’ (PRR) that calibrates reaching out and the ‘anterior intraparietal area’ (AIP), which brings about accurate grasp.[14]
Extensive damage to the posterior parietal lobes would therefore be expected to give rise to the following[15]:
Inability to process multiple visual objects in the surroundings - This is called ‘simultanagnostic vision’ (simultan- at the same time, agnosia- not knowing) (Video 1: Simulation of simultanagnostic vision of a child)
Impaired visual guidance of movement- This is called ‘optic ataxia’ (a term coined by Hungarian Neurologist Rudolph Balint- optische ataxie).[15]
Inability to give attention to hearing and vision at the same time- Such children tend to look away from the person talking during conversations
Inability to locate the direction of sound- If someone calls, the child cannot make out, from where the person is calling.
Inability to move the eyes from one object to another on request, despite normal eye movements. This is called apraxia of gaze. Here the eyes cannot be moved to an item specified by another person because it cannot be seen owing to the simultanagnosia.
Lower visual field impairment is a common accompaniment because upper visual pathways in the superior optic radiations serving the lower visual field pass through the posterior parietal lobes. This may lead to collision with low objects while moving around.
The combination of simultanagnosia, optic ataxia, and apraxia of gaze is called Balint syndrome.[16,17] In milder forms of the condition, known as dorsal stream dysfunction, visual guidance of the lower limbs, and less frequently the upper limbs, is inaccurate, especially when tired, the visual search is impaired and crowding of the visual scene is disabling.[16,17] Moreover, accuracy of movement of the limbs in the lower visual field can be impaired owing to impaired peripheral clarity of vision when the superior optic radiation is limited owing to periventricular white matter pathology causing enlarged receptive field sizes.[18]
The pathway between the occipital and posterior parietal lobes is referred to functionally as the dorsal stream and anatomically as the superior longitudinal fasciculus. The superior longitudinal fasciculus (SLF) is a bidirectional occipito-parietal-frontal tract connecting the occipital and the prefrontal cortices (serving visual attention) via the posterior parietal cortex. Thinning and decreased fractional anisotropy within the SLF has been shown to be a biomarker for PVD in children with cerebral palsy.[19]
Processing by the inferior temporal lobes
The inferior temporal lobes provide a storehouse for the images acquired over a lifetime. The incoming image data provided by the occipital lobes is compared with this image store and when a match takes place, an item is ‘recognized’. This is how faces, objects, shapes and routes are recognized by seeing.
Specific neurons in the inferior temporal lobes are highly selective for the kind of visual elements that they respond to. There are specialized centres for processing faces (the fusiform face area- FFA), everyday objects (the lateral occipital area- LO area), routes (the parahippocampal place area- PPA) for example. Most of these areas are clustered together on the underside of the temporal lobes near their junction with the occipital lobes.[11]
Injury to left temporal lobe may lead to symptoms of difficulty in recognizing shapes, objects, and letters. Injury to the right temporal lobe may lead to difficulty in recognizing faces (prosopagnosia- from Greek prosopon, meaning face) and the language of facial expressions, and topographic agnosia (inability to retain where things are and routes). If both temporal lobes are injured, one may experience difficulty in analyzing line length and orientation, estimation of object size, and impairment of visual memory.[20,21,22,23]
The pathway between the occipital and temporal lobes is referred to functionally as the ventral stream and anatomically as the inferior longitudinal fasciculus.
In essence, the ventral stream transforms visual signals into perception and dorsal stream transforms visual signals to automatically and non-consciously map the scene to guide action, and facilitates attention.
Motion perception
Motion perception is served anterior to the occipital lobes in the middle temporal lobes, referred to as area MT (earlier called area V5). This area primarily receives inputs from the more peripheral visual fields. Such motion detection and analysis is largely a subconscious function.[24] Bilateral damage to this area leads to inability to see moving targets, called akinetopsia, which is rare or inability to see fast moving objects or to perceive and interpret biological movement, which is now being increasingly recognized in children with prematurity and periventricular leukomalacia and is called dyskinetopsia.[24] (Video 2: Simulation of dyskinetopsia).
Though there are different centres and pathways for various higher visual functions, it is frequently not possible to correlate between the etiology of CVI, location of the brain damage and type of perceptive visual functions affected. This is largely due to the interconnectivity of different visual pathways, lesions involving multiple areas, and combinations of ocular and cerebral lesions, often seen in patients.[25]
When to suspect PVD in a child?
One should suspect PVD when a child[26]:
Seems to see well sometimes but other times not so well
Has a limited span of visual attention
Is making additional use of the other senses like hearing and touch, for various tasks
Needs more time to learn the details of an object, especially if there are multiple things around.
Needs more time to find familiar people in a busy environment, such as during a birthday party.
Has problems with eye-hand coordination e.g., placing a ring on a ring tower, putting a coin in a piggy bank.
Has difficulty in recognizing people by seeing
Has difficulty in understanding the language of facial expressions
Has difficulty seeing moving things like a ball or traffic
Has difficulty judging distances and depth: A child may find it hard to learn to climb stairs. She may prefer to sit to go down stairs, rather than walk.
Has difficulty getting orientated to new surroundings like a wedding hall
In a child with any of the above symptoms, one should seek a history of perinatal brain injury or any other neurological issues, look for the presence of optic disc pallor or cupping,[27] seek the presence any lesions on MRI brain and the presence of any neurological visual field defects. If any of these are present, the chances of the child having PVD are greater. One then needs to probe more deeply into the child's visual functioning in different areas, using a structured history taking approach as described below.
Importance of structured history taking
The clinical manifestations of PVD may go unrecognized for years despite visiting eye care professionals and parents being highly educated, because the visual origin of the child's symptoms may not have been considered. For example, inability to find one's own clothes from within a pile of clothes can be a manifestation of simultanagnosia due to dorsal stream dysfunction, but this may simply have been labeled as ‘stupidity’. The caregivers may not volunteer such behaviors during routine history taking. So it is important to have a structured way to take a detailed history, encompassing the day-to-day activities of the child. Various questionnaires have been described in the literature for this purpose.[28,29,30,31,32,33,34,35,36,37,38,39,40] Among these, we find the one developed in Scotland very useful to get an insight into the child's visual world.[30,37,38,39,40] We have adapted it slightly after administering it for many children over 10 years, removing items that are culturally inappropriate or redundant for Indian children. [Appendix 1] It comes with a set of strategies to deal with each visual difficulty, which have been contributed by several parents dealing with such children over many years.[38] [Appendix 2] Its use in Indian children has been validated.[39] This tool has been used in various studies and its value in profiling the child's visual abilities in different spheres of activity has been established.[1,2,3,32,37,38,39,40] A recent publication by Tsirca A et al. from the UK has shown significant improvement in quality of life of children below the age of 12 years, after using individualized intervention strategies as guided by the CVI Inventory over a period of 6 months follow-up (sample size 52, P = 0.058).[40]
Practical tips on the use of the CVI inventory
One should remember that it is not a diagnostic or a screening tool for PVD, but it is an inventory to profile the child's visual functioning in different spheres of day-to-day life, to identify problem areas and to come up with strategies to help with these issues.
For time management, one may take help from support staff to administer the inventory, but it is important for the ophthalmologist to confirm the positive observations made.
While interviewing parents, it is important not to guide them towards an answer but to just explain the questions and choices.
One may find multiple problem areas for a child, which may need to be prioritized and tackled one by one.
The strategies we choose for each difficulty need to be appropriate for the family's socio-economic background and available support system.
It is important to communicate these issues with all those working with the child for various issues including the parents, teachers, and all therapists, in language they all can understand.
Most families can cope with only 2 or 3 new strategies at once, so when many are needed, they are introduced gradually.
Clinical examination
Through a comprehensive eye examination, one must identify any treatable ophthalmic conditions like refractive errors, amblyopia, and any large angle constant squint needing surgery.
In addition to regular examination, one should look for the following:
Crowding ratio
The ratio between the best-corrected visual acuity (BCVA) measured with a linear optotype (multiple optotypes in each line) and BCVA measured with a single optotype, is called the crowding ratio. A crowding ratio of more than 2 can be an indicator of dorsal stream dysfunction and has been found to be a useful contributory criterion to the diagnosis of PVD.[29,41]
Apraxia of Gaze
Many children with dorsal stream dysfunction tend to have difficulty in making saccadic eye movements from one object to another nominated by the examiner, because their limited visual attention (due to dorsal stream pathology) is ‘consumed’ by the first object and prevents them from noticing the next. Yet there may be no issue with their oculomotor apparatus; hence it has also been called psychic paralysis of gaze.[16,17] When tested for saccades, such children tend to move their heads, rather than their eyes. (Video 3 showing how to test for apraxia of gaze).
Tests for cognitive visual functions
We find the following clinical tests useful for evaluation of higher visual functions in the clinic.
1. Lea puzzle[42]:
Procedure: (Video 4 showing the procedure to use for the Lea puzzle).
First explain the test to the child and start with the colored side. Give one shape at a time to place in the tray. If the child can match color and shape, this means the ventral stream is functioning normally at this level of visual analysis. The way the child reaches out and grasps the shape, and then orientates it according to its reciprocal slot on the board, and the ease with which it is placed in its slot, tells much about the way the dorsal stream is functioning. If the child can do this well, change the orientation of the puzzle to make it a more complex task and see if the child is still able to do it well. Keep an eye on whether the child puts the shape into its slot using vision or seeks additional tactile clues to do this. If the child can do this well too, then use the black and white reverse sides of the tray and shapes. Here the child has to match only shape, and there is no color clue. Again, the tray can be turned around to make the task more complex. Next, we can keep all the shapes together and ask the child to pick-up one named shape. This tests for ‘recognition of the desired symbol’ is enabled by the ventral stream, as well as the ‘visual analysis of multiple objects’ and ‘accurate reaching out and grasping for the desired symbol’, facilitated by the dorsal stream.
2. The Lea mailbox test[43]: Here the child has to post the white card through the slit in the yellow circular disc, like posting a letter into a postbox [Fig. 2]. Normative data for this test have been published.[44]
Figure 2.

Lea mailbox
Procedure: (Video 5 shows the procedure to use for the Lea mailbox test).
One should explain the procedure to the child. Then give the white card and see how she grasps it. Look for the gap between the fingers and thumb of the reaching hand, to see whether or not it matches the orientation and the thickness of the card. The pattern of picking-up the card should also be carefully observed and noted (both dorsal stream functions). There are four potential patterns of picking-up: normal in flight gap between fingers and thumb, wide in flight gap, placement of the hand on top of the item to use touch to complete the grasp, reaching beyond and gathering up. See how the child matches the orientation of the card in relation to the orientation of the slit (understanding that choosing the direction of the orientation in relation to the alignment of the slot is a ventral stream function, while the act of posting the card by means of visual guidance is a dorsal stream function). Watch how the child approaches the slit with the card. Does he post the card visually, or does he touch the yellow disc, and using tactile clues, and then manage to push the card through the slit? This behavior again suggests tactile compensation for deficient dorsal stream dysfunction.
3. Object sorting test: (Video 6 showing the procedure of object sorting test)
Here we mix-up objects of different shapes and colors in a basket and ask the child to find one of them and pick it up, ensuring first that the child knows the names of the objects and their colors. Watch to see if the child directly selects and picks-up the desired object or takes them out one by one until the requested object is found. This suggests dorsal stream dysfunction. Look for the reaction time. Does the child pick up the items reflexly, or is more time taken and more effort and attention exerted? If it is difficult for the child to find the desired object, reduce the number of objects one at a time, to see how many objects are left in the basket when the child becomes comfortable in identifying and picking-up the desired one, with the least effort and time. This is probably the threshold for the dorsal stream for being able to handle such complex visual information. And an explanation of the difficulty, and how to cater for it by limiting clutter is given to the parents.
4. Tests for motion perception:
a. Finger motion test: (Video 7 showing the procedure of the fingers in motion test) This is suitable for a school child who is familiar with finger counting. The examiner first shows the child one, two or three fingers and asks her to count them. Then the examiner rapidly moves a closed fist to and fro, perpendicular to the child's line of gaze, while extending one two or three fingers. The hand is progressively slowed until the fingers are accurately counted. This can be performed the other way round as well by asking the child to count fingers, then slowly wave the hand with increasing speed until the child cannot count the fingers.[45] If only limited movement of the hand renders the child unable to count the fingers, then the child has a severe issue with motion perception (akinetopsia). If the child can count fingers of a only the slowly moving hand, but cannot when the hand is moving more rapidly, when this is otherwise seen by all, then this is likely to be due to dyskinetopsia.
b. Pepi test: (Video 8 showing the procedure for Pepi test) This test, which investigates the ability to construct the nature of biological movement represented by moving elements on a screen, is more suitable for those who are unable to count fingers.[46] In this test, the child fixates the central red lines on a computer screen. The examiner presses key 1 or one of the arrows, and a Dalmatian dog starts to move from one corner of the screen diagonally across to the other. The examiner watches the child's eyes, to see if they are following the dog. If a child has impaired pursuit movement, one should ask the child what he/she can see. One issue with this test that we have encountered is that owing to the cluttered background being similar to the dog, a child may not be able to see the dog owing to simultanagnosia.
c. Play situations: With the child sitting on the floor, we roll a ball on the floor towards the child and watch if he/she tracks the movement of the ball. Then we throw a large ball to see if he is able to catch it. Inability to appreciate the movement of the ball may indicate dyskinetopsia.
5. Tests for simultanagnosia:
We can ask the child to describe what is he able to see around him in the examination room, without taking an unduly long time. Watch how the child moves their head and eyes while searching. We can show the child a family photograph and ask him to name the people. If he is unable to do so, we can ‘zoom in’ and show fewer faces at a time. If the child becomes better at recognizing people after zooming in, it shows that she is likely to have simultanagnostic vision and that using a cell phone with zoom in, is likely to help the child analyze her visual environment better. We can ask the child to find his parent sitting in the waiting hall among many other people. Ishihara color plates have been found to be useful as a test for simultanagnosia in adults where the patients with occipito-parietal brain damage can recognize colors but not the numbers on the plate.[47] If the examiner moves away, the patient may be able to recognize the number since the color dots become more idistinct the greater the distance, resulting in less information on the plate to process.
Note: Clinical tests that are highly sensitive and specific for PVD have yet to be developed. The tests described are helpful in the clinic, but one should keep in mind that they have low sensitivity to pick-up issues related to PVD. This means, that if a child can perform these well, it does not mean that there is no PVD, but if the child cannot perform well on these assessments, it means that the child is highly likely to have a visual perceptual problem, which needs to be recognized, understood and acted upon effectively.
Several learning resources and high-quality educational videos about PVDs are available as ‘Lessons’ on the website www.cviscotland.com and readers are recommended to refer to those.[48]
Neuropsychological evaluation
Neuropsychological evaluation is commonly carried out in some European countries as a part of the work-up for PVD.[49,50,51] The evaluation comprises the intelligence quotient (IQ) test for both performance and verbal IQ, and tests for attention and memory. A verbal IQ better than the performance IQ, is considered an indicator of cognitive visual impairment. This is followed by various tests for cognitive visual functions like the Developmental Test of Visual Perception (DTVP), the Poppelreuter–Ghent Test, Beery's Visual-Motor Integration Test, and the L94 visual perceptual battery. One practical issue about Neuropsychological evaluation in a developing country like India is the lack of availability of a trained neuro-psychologist to perform and interpret these tests, while the clinical psychologists, who are available in certain cities, are not available in ophthalmologists’ offices. As a practical solution, we have found that an ophthalmologist or an optometrist himself or herself can administer one of these tests in the clinic with some training such as DTVP-3 (third edition)[52] or the Motor-Free Visual Perception Test- Fourth Edition (MVPT-4).[53] Each one of these takes about 20–25 min to administer and is fairly simple to use. One should keep in mind that these tests seek aberrance from normality and its degree. They do not seek out specific visual agnosias and have limited value when it comes to actual formulation of habilitation strategies for the child. Tsrika A et al. from the UK have found statistically significant correlations between CVI Inventory and corresponding domains of the neuropsychological tests like Wechsler Intelligence Scale for Children- Fourth Edition, the Beery-Buktenica Test of Visual-Motor Integration, and the Benton Facial Recognition Test (sample size 51 children, correlation coefficient ranging between –0.47 to –0.55 and P value <0.01) suggesting that, the CVI Inventory is an effective tool to assess PVDs.[40] This is particularly relevant for places where resources for neuro-psychological evaluation are not available.
Home visits and school visits
It is ideal to watch the child functioning in familiar environments like home and school, but logistic constraints, currently tend to preclude this in a typical Indian scenario. However, with the availability of smartphones, we have found video recordings taken by parents as per our instructions can be very useful to watch the child's visual functioning at home and school.
Use of optical coherence tomography (OCT)
Lena Jacobson's group in Sweden has shown that structural abnormalities in the optic radiations lead to a commensurate reduction in the peripapillary retinal nerve fiber layer (RNFL) thickness and ganglion cell layer (GCL) thickness at the macula, due to retrograde trans-synaptic degeneration. Thus the focal loss of peripapillary RNFL and macular GCL tends to correlate with the visual field defects in such patients and also the PVD.[54,55,56] OCT also helps to act as a surrogate marker for potential visual field defects, which are difficult to assess because of difficulties in using automated perimetry at a young age and the visual issues related to dorsal stream dysfunction. One should remember that there are many other causes for thinning of the RNFL and GCL in addition to optic radiation injury, and that visual field defects and PVD can be present even in those with a normal peripapilary RNFL and normal macular GCL thicknesses.
Differential Diagnoses
A child with PVD may manifest both adaptive and reactive behavioral responses due to their visual condition. These can overlap with behaviors typical of common neurodevelopmental disorders. These include autism spectrum disorder (ASD), attention deficit hyperactivity disorder (ADHD), specific learning disability (sLD) and intellectual disability.[45,57,58]
a. ASD refers to a group of disorders with features of impaired social interaction and communication, and inflexible stereotyped behaviors. A child with PVD may also manifest similar features. Red flags towards ASD include lack of progression of social communication disproportionate to visual abilities, as well as echolalia and repetitive behaviors (flapping, rocking, spinning) disproportionate to the visual difficulties.[57]
b. Children with ADHD have issues of inattention, hyperactivity, and impulsivity. An ophthalmologist or optometrist should strongly consider the possibility of ADHD in the context of the following behaviors: getting up and moving around when the child is expected to be sitting (for example, in the classroom), running or climbing excessively in situations in which it is inappropriate, difficulty quietly playing or engaging in leisure activities, talking excessively, interrupting or intruding on others (for example: when they are talking).[58]
c. Mild intellectual impairment can be confusing. But difficulty understanding instructions or remembering recently learned information, could be a strong indicator of mild intellectual impairment.[45]
d. It is difficult to distinguish between sLD and CVI, since there is significant overlap in their manifestations. Hence all children with suspected sLD should have a thorough ophthalmic evaluation including assessment of cognitive visual function before psychiatric evaluation.[45]
Conclusion
The diagnosis of PVD should be suspected in any child in whom the visual behaviors are not explained by the ophthalmic examination. The presence of a known neurological issue, such as an eventful perinatal history, lesions found on neuroimaging, the presence of optic disc pallor or cupping, a visual acuity crowding ratio >2, raises the index of suspicion for the diagnosis of PVD. One should then use an inventory to take a systematic history about each of the domains of visual functioning in the child's day-to-day life. The two purposes of the inventory are to elicit features consistent with the diagnosis of CVI and to profile the child's visual difficulties in order to plan management. To further substantiate the diagnosis, additional clinical tests for higher visual dysfunctions should be administered, remembering that although specific, they have low sensitivity, so cannot be used to ‘rule out’ the diagnosis of PVD. Videos recorded by parents are often useful to understand how their child functions in familiar environments. OCT of the retina provides a quick diagnostic tool in a busy clinic, again recognizing that only positive tests are informative. Neuropsychological evaluation is ideal, but often not available. There are testing tools like the DTVP-3 and MVPT-4 that an eye care professional can use after training. It is important to be aware of the close differential diagnoses like ASD, sLD, ADHD and mild intellectual impairment and to make appropriate referral if needed, yet recognizing that PVD can coexist. A key component in helping children with PVD is to educate parents, carers and teachers about the visual basis of symptoms and explaining simple, doable strategies appropriate for the family's socio-economic profile. In our experience such simple strategies often revolutionize the affected child's world and expedite learning and development.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos Available on: www.ijo.in
Acknowledgements
We are thankful the Hyderabad Eye Research Foundation for assistance in conducting this study.
Appendix 1: Inventory for Structured History Taking
For each of the items listed, please could you tick the box which best fits with your child's present behaviour?: Never/Rarely/Sometimes/Often/Always/Not applicable (NA)
| Questions about lower visual field | Never | Rarely | Sometimes | Often | Always | NA |
|---|---|---|---|---|---|---|
| Does your child… | ||||||
| 1. trip over toys and obstacles on the floor? | ||||||
| 2. have difficulty walking down stairs? | ||||||
| 5. appear to ‘get stuck’ at the top of a slide/hill? | ||||||
| 6. look down when crossing floor boundaries e.g. where tiles meet the soil? | ||||||
| 7. When walking, does your child hold onto your clothes, tugging down? | ||||||
| 8. Does your child find uneven ground difficult to walk over? | ||||||
| 9. Does your child bump into low furniture such as a teapoy? | ||||||
| 10. Does your child get angry if furniture is moved? | ||||||
| Questions about visual field on the sides | ||||||
| Does your child… | ||||||
| 11. have difficulty finding the beginning of a line when reading? | ||||||
| 12. have difficulty finding the next word when reading? | ||||||
| 13. walk out in front of traffic? | ||||||
| If so, which side? | right/ | left/ | both | |||
| 14. bump into doorframes or partly open doors? | ||||||
| If so, which side? | right/ | left/ | both | |||
| 15. miss pictures or words on one side of a page? | ||||||
| If so, which side? | right/ | left/ | both | |||
|
| ||||||
| Questions about motion perception | Never | Rarely | Sometimes | Often | Always | NA |
|
| ||||||
| Does your child… | ||||||
| 16. have difficulty seeing scenery from a moving vehicle? | ||||||
| 17. have difficulty seeing things which are moving quickly, such as small animals? | ||||||
| 18. avoid watching fast moving TV? | ||||||
| 19. choose to watch slow moving TV? | ||||||
| 20. have difficulty catching a ball? | ||||||
|
| ||||||
| Questions about difficulty in seeing when there is too much to see | Never | Rarely | Sometimes | Often | Always | NA |
|
| ||||||
| Does your child… | ||||||
| 21. have difficulty seeing something which is pointed out in the distance? | ||||||
| 22. have difficulty finding a close friend or relative who is standing in a group? | ||||||
| 23. have difficulty finding an item in a supermarket e.g., finding the breakfast cereal they want? | ||||||
| 24. get lost in places where there is a lot to see, e.g., a crowded shop? | ||||||
| 25. get lost in places which are well known to them? | ||||||
| 26. have difficulty locating an item of clothing in a pile of clothes? | ||||||
| 27. have difficulty selecting a chosen toy in a toy box? | ||||||
| 28. want to sit closer to the television than about 30 cm? | ||||||
| 29. find copying words or drawings time- consuming and difficult? | ||||||
| 30. Do quiet places/open countryside cause difficult behaviour? | ||||||
| 31. Is behaviour in a busy supermarket or shopping centre difficult? | ||||||
|
| ||||||
| Seeing when competing sensory stimuli present | Never | Rarely | Sometimes | Often | Always | NA |
|
| ||||||
| 32. After being distracted does your child find it difficult to get back to what they were doing? | ||||||
| 33. Does your child bump into things when walking and having a conversation? | ||||||
| 34. Does your child miss objects which are obvious to you because they are different from their background and seem to ‘pop out’ e.g., a bright ball in the grass? | ||||||
|
| ||||||
| Activities with sustained near vision task | Never | Rarely | Sometimes | Often | Always | NA |
|
| ||||||
| 35. Does your child react angrily when other restless children cause distraction? | ||||||
| 36. Does your child find it difficult to concentrate on a sustained near vision task for more than 5 min? | ||||||
|
| ||||||
| Difficulties in recognition and visual memory | Never | Rarely | Sometimes | Often | Always | NA |
|
| ||||||
| Does your child… | ||||||
| 37. have difficulty recognising close relatives in real life? | ||||||
| 38. have difficulty recognising close relatives from photographs? | ||||||
| 39. mistakenly identify strangers as people known to them? | ||||||
| 40. have difficulty understanding the meaning of facial expressions? | ||||||
| 41. have difficulty naming common colours? | ||||||
| 42. have difficulty naming basic shapes such as squares, triangles and circles? | ||||||
| 43. have difficulty recognising familiar objects such as the family car? | ||||||
Appendix 2: Strategies for Various Vision Related Difficulties
Intervention strategies for children with cognitive visual dysfunction
When a child has been found to have cognitive visual dysfunction, following strategies can be used to help the child work around those specific issues.
(Adopted from McKillop E, Dutton GN. Impairment of vision in children due to damage to the brain: a practical approach. British and Irish Orthoptic Journal. 2008; 5: 8-14.)
| Problem | Approaches |
|---|---|
| Reduced clarity of vision. | Enlarge text |
| Double space text | |
| Present text in small sections. | |
| Reduce distractions | |
| Limit tiredness | |
| Colour vision and contrast sensitivity impairment | Bright and clear educational material and toys. |
| Distinct color boundaries | |
| Good contrast | |
| Lack of vision on one side | Tracing of text with a finger or ruler |
| Turning text vertically or obliquely | |
| Appropriate seat position in classroom | |
| Turning of head to check the hemianopic side | |
| Careful guidance around new environments | |
| Training in crossing roads | |
| Turn plate to eat food | |
| Lack of vision down below | As with hemianopia |
| Regularly looking down to check the ground ahead | |
| Tactile guide to ground height | |
| Impaired ability to move the eyes | Movement of the head |
| Enlarging text | |
| Double spacing text | |
| Tracing of text with a finger or ruler | |
| Impaired ability to see movement | Television programs with limited movement |
| Educational material with limited movement | |
| Careful training or guidance in crossing roads. | |
| Difficulty finding a toy in a toy box or an item of clothing in a pile or wardrobe | Separate storage of favorite items |
| Organized storage systems | |
| Always store in same location | |
| Avoid clutter | |
| Colour coding and labels | |
| Difficulty finding an object on a patterned background. | Use plain carpets, bedspreads and decoration. |
| Difficulty finding food on a plate | Avoid patterned plates |
| Avoid sauces/gravy | |
| Separate food portions | |
| Problems seeing a distant object | Use zoom on video/digital camera to view |
| Problems reading | Enlarge text |
| Double space text | |
| Masking surrounding text | |
| Computer programs to present information | |
| Difficulty finding someone in a group. | Wear obvious identifier |
| Always stand in same location | |
| Waving | |
| Speak | |
| Tendency to get lost | Training in seeking and identifying landmarks Visit new locations at quiet times |
| Problems with floor boundaries, steps, kerbs and uneven surfaces | Avoid patterned floor surfaces Bannister |
| Mark edge of stairs | |
| Good lighting | |
| Tactile guides to gage the height of the ground | |
| Approach obstacles with | |
| “Look- Slow- Check- Go” | |
| Activities to improve coordination | |
| Inaccurate visually guided reach | Reaching beyond an object to gather it |
| Activities to improve coordination | |
| Occupational therapy | |
| Difficulty ‘seeing’ when talking at the same time | Limit conversation when walking |
| Identify obstacles by tactile stimulation | |
| Frustration at being distracted | Limit distraction |
| Minimize background clutter | |
| Minimize background activity | |
| Quiet table at school | |
| Difficulty recognizing people and photographs | Introductions |
| Training in identifying voices | |
| Consistent identifiers worn | |
| Training to recognize identifiers | |
| Difficulty recognizing shapes and objects | Training to identify and recognize identifiers |
| Training in tactile recognition | |
| Difficulty reading facial expression | Training in recognizing facial expressions |
| Expression of mood by tone of voice | |
| Explanation of mood in words | |
| Getting lost in known places | Training in orientation. |
| Encouraging leading | |
| Incorporating landmarks in Mnemonics/Poems | |
| Difficulty in new environments | Training in orientation. |
| Encourage exploration | |
| -Visit at quiet times | |
| - Hide and Seek | |
| - Treasure Hunts | |
| Visual fatigue | Minimize clutter |
| Prolonged visual processing | Reduce distractions |
| Reduce detail and complexity | |
| Well-earned breaks | |
| Social problems | Good understanding and support at school |
| Identify problems and solutions | |
| Encourage child to overcome them | |
| Well known informed peer group | |
| Find activities child enjoys and can excel in |
References
- 1.Saidkasimova S, Bennett DM, Butler S, Dutton GN. Cognitive visual impairment with good visual acuity in children with posterior periventricular white matter injury: A series of 7 cases. J AAPOS. 2007;11:426–30. doi: 10.1016/j.jaapos.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 2.Mitry D, Williams C, Northstone K, Akter A, Jewel J, Khan N, et al. Perceptual visual dysfunction, physical impairment and quality of life in Bangladeshi children with cerebral palsy. Br J Ophthalmol. 2016;100:1245–50. doi: 10.1136/bjophthalmol-2015-307296. [DOI] [PubMed] [Google Scholar]
- 3.Macintyre-Béon C, Young D, Dutton GN, Mitchell K, Simpson J, Loffler G, et al. Cerebral visual dysfunction in prematurely born children attending mainstream school. Doc Ophthalmol. 2013;127:89–102. doi: 10.1007/s10633-013-9405-y. [DOI] [PubMed] [Google Scholar]
- 4.Gorrie F, Goodall K, Rush R, Ravenscroft J. Towards population screening for cerebral visual impairment: Validity of the five questions and the CVI questionnaire. PLoS One. 2019;14:e0214290. doi: 10.1371/journal.pone.0214290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pehere N, Chougule P, Dutton GN. Cerebral visual impairment in children: Causes and associated ophthalmological problems. Indian J Ophthalmol. 2018;66:812–5. doi: 10.4103/ijo.IJO_1274_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. [Last accessed last on 2020 Sep 20]. Available from: https://nhm.gov.in/index1.php?lang=1&level=4&sublinkid=1190&lid=583 .
- 7.Leuck AH, Dutton GN, editors. Vision and Brain. 1st ed. AFB Press; pp. 8 and 30–36. [Google Scholar]
- 8.Newcombe F, Russel WR. Dissociated visual perceptual and spatial deficits in focal lesions of the right hemisphere. J Neurol Neurosurg Psychiat. 1969;32:73–81. [Google Scholar]
- 9.Mishkin M, Ungerleider LG. Contribution of striate inputs to the visuospatial functions of parieto-preoccipital cortex in monkeys. Behav Brain Res. 1982;6:57–77. doi: 10.1016/0166-4328(82)90081-x. [DOI] [PubMed] [Google Scholar]
- 10.Goodale MA, Milner AD, Jakobson LS, Carey DP. A Neurological dissociation between perceiving objects and grasping them. Nature. 1991;349:154–6. doi: 10.1038/349154a0. [DOI] [PubMed] [Google Scholar]
- 11.Milner D, Goodale M. The Visual Brain in Action. 2nd ed. Oxford: Oxford University Press; 2006. [Google Scholar]
- 12.Milner AD. How do the two visual streams interact with each other? Exp Brain Res. 2017;235:1297–308. doi: 10.1007/s00221-017-4917-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saur D, Kreher BW, Schnell S, Kümmerer D, Kellmeyer P, Vry MS, et al. Ventral and dorsal pathways for language. Proc Natl Acad Sci U S A. 2008;105:18035–40. doi: 10.1073/pnas.0805234105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goodale M, Milner D. Sight Unseen- An Exploration of Conscious and Unconscious Vision. Oxford: Oxford University Press; 2005. pp. 65–6. [Google Scholar]
- 15.Rizzo M, Vecera SP. Psychoanatomical substrates of Bálint's syn- drome. J Neurol Neurosurg Psychiatry. 2002;72:162–78. doi: 10.1136/jnnp.72.2.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gillen JA, Dutton GN. Balint's syndrome in a 10-year-old male. Dev Med Child Neurol. 2003;45:349–52. doi: 10.1017/s0012162203000641. [DOI] [PubMed] [Google Scholar]
- 17.Drummond SR, Dutton GN. Simultanagnosia following perinatal hypoxia: A possible pediatric variant of Balint syndrome. J AAPOS. 2007;11:497–8. doi: 10.1016/j.jaapos.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 18.Jacobson L, Flodmark O, Martin L. Visual field defects in prematurely born patients with white matter damage of immaturity: A multiple-case study. Acta Ophthalmol Scand. 2006;84:357–62. doi: 10.1111/j.1600-0420.2006.00636.x. [DOI] [PubMed] [Google Scholar]
- 19.Galli J, Ambrosi C, Micheletti S, Merabet LB, Pinardi C, Gasparotti R, et al. White matter changes associated with cognitive visual dysfunctions in children with cerebral palsy: A diffusion tensor imaging study. J Neurosci Res. 2018;96:1766–74. doi: 10.1002/jnr.24307. [DOI] [PubMed] [Google Scholar]
- 20.McCarthy RA, Evans JJ, Hodges JR. Topographic amnesia: Spatial memory disorder, perceptual dysfunction, or category specific semantic memory impairment? J Neurol Neurosurg Psychiatry. 1996;60:318–25. doi: 10.1136/jnnp.60.3.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barton JJ, Cherkasova M, O’Connor M. Covert recognition in acquired and developmental prosopagnosia. Neurology. 2001;57:1161–8. doi: 10.1212/wnl.57.7.1161. [DOI] [PubMed] [Google Scholar]
- 22.Shen L, Hu X, Yacoub E, Ugurbil K. Neural correlates of visual form and visual spatial processing. Hum Brain Mapp. 1999;8:60–71. doi: 10.1002/(SICI)1097-0193(1999)8:1<60::AID-HBM5>3.0.CO;2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tarkiainen A, Helenius P, Hansen PC, Cornelissen PL, Salmelin R. Dynamics of letter string perception in the human occipitotemporal cortex. Brain. 1999;122:119–32. doi: 10.1093/brain/122.11.2119. [DOI] [PubMed] [Google Scholar]
- 24.Weinstein JM, Gilmore RO, Shaikh SM, Kunselman AR, Trescher WV, Tashima LM, et al. Defective motion processing in children with cerebral visual impairment due to periventricular white matter damage. Dev Med Child Neurol. 2012;54:e1–8. doi: 10.1111/j.1469-8749.2010.03874.x. [DOI] [PubMed] [Google Scholar]
- 25.Boot FH, Pel JJ, van der Steen J, Evenhuis HM. Cerebral visual Impairment: Which perceptive visual dysfunctions can be expected in children with brain damage? A systematic review. Res Dev Disabil. 2010;31:1149–59. doi: 10.1016/j.ridd.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 26.Roza M, Bakker K, Bals I. My Child has CVI, Handbook for Parents of a Young Child with CVI. Bartiméus. 2017:13–7. [Google Scholar]
- 27.Jacobson L, Hellström A, Flodmark O. Large cups in normal-sized optic discs. A variant of optic nerve hypoplasia in children with periventricular leukomalacia. Arch Ophthalmol. 1997;15:1263–9. doi: 10.1001/archopht.1997.01100160433007. [DOI] [PubMed] [Google Scholar]
- 28.Salavati M, Waninge A, Rameckers EA, van der Steen J, Krijnen WP, van der Schans CP, et al. Development and face validity of a cerebral visual impairment motor questionnaire for children with cerebral palsy. Child Care Health Dev. 2017;43:37–47. doi: 10.1111/cch.12377. [DOI] [PubMed] [Google Scholar]
- 29.van Genderen M, Dekker M, Pilon F, Bals I. Diagnosing cerebral visual impairment in children with good visual acuity. Strabismus. 2012;20:78–83. doi: 10.3109/09273972.2012.680232. [DOI] [PubMed] [Google Scholar]
- 30.Dutton GN, Calvert J, Ibrahim H, Macdonald E, McCulloch DL, Macintyre-Beon C, et al. Structured clinical history taking for cognitive and perceptual visual dysfunction and for profound visual dis- abilities due to damage to the brain in children. Visual Impairment in Children due to Damage to the Brain. London: Mac Keith Press; 2010. pp. 117–28. [Google Scholar]
- 31.Ortibus E, Laenen A, Verhoeven J, De Cock P, Casteels I, Schoolmeesters B, et al. Screening for cerebral visual impairment: Value of a CVI questionnaire. Neuropediatrics. 2011;42:138–47. doi: 10.1055/s-0031-1285908. [DOI] [PubMed] [Google Scholar]
- 32.Williams C, Northstone K, Sabates R, Feinstein L, Emond A, Dutton GN. Visual perceptual difficulties and under-achievement at school in a large community-based sample of children. PLoS One. 2011;6:e14772. doi: 10.1371/journal.pone.0014772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Neumann G, Schaadt AK, Reinhart S, Kerkhoff G. Clinical and psychometric evaluations of the cerebral vision screening questionnaire in 461 nonaphasic individuals poststroke. Neurorehabil Neural Repair. 2016;30:187–98. doi: 10.1177/1545968315585355. [DOI] [PubMed] [Google Scholar]
- 34.Ferziger NB, Nemet P, Brezner A, Feldman R, Galili G, Zivotofsky AZ. Visual assessment in children with cerebral palsy: Implementation of a functional questionnaire. Dev Med Child Neurol. 2011;53:422–8. doi: 10.1111/j.1469-8749.2010.03905.x. [DOI] [PubMed] [Google Scholar]
- 35.Hyvärinen L, Walthes R, Freitag C, Petz V. Profile of visual functioning as a bridge between education and medicine in the assessment of impaired vision. Strabismus. 2012;20:63–8. doi: 10.3109/09273972.2012.680235. [DOI] [PubMed] [Google Scholar]
- 36.Ben Itzhak N, Vancleef K, Franki I, Laenen A, Wagemans J, Ortibus E. Visuoperceptual profiles of children using the Flemish cerebral visual impairment questionnaire. Dev Med Child Neurol. 2019;62:969–76. doi: 10.1111/dmcn.14448. [DOI] [PubMed] [Google Scholar]
- 37.Macintyre-Beon C, Young D, Calvert J, Ibrahim H, Dutton GN, Bowman R. Reliability of a question inventory for structured history taking in children with cerebral visual impairment. Eye. 2012;26:1393. doi: 10.1038/eye.2012.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McKillop E, Dutton GN. Impairment of vision in children due to damage to the brain: A practical approach. Br Ir Orthopt J. 2008;5:8–14. [Google Scholar]
- 39.Philip SS, Tsherlinga S, Thomas MM, Dutton GN, Bowman R. A validation of an examination protocol for cerebral visual impairment among children in a clinical population in India. J Clin Diagn Res. 2016;10:NC01–4. doi: 10.7860/JCDR/2016/22222.8943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tsirka A, Liasis A, Kuczynski A, Vargha-Khadem F, Kukadia R, Dutton G, et al. Clinical use of the Insight Inventory in cerebral visual impairment and the effectiveness of tailored habilitational strategies. Dev Med Child Neurol. 2020 doi: 10.1111/dmcn.14650. doi: 10.1111/dmcn. 14650. Online ahead of print. PMID: 32770793. [DOI] [PubMed] [Google Scholar]
- 41.van der Zee YJ, Stiers P, Evenhuis HM. Should we add visual acuity ratios to referral criteria for potential cerebral visual impairment? J Optom. 2017;10:95–103. doi: 10.1016/j.optom.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Available from: http://www.leatest.fi/index.html?start=en/vistests/instruct/lea3dpuz/lea3dpuz.html .
- 43. Available from: http://www.leatest.fi/index.html?start=en/vistests/instruct/pvmailbo/pvmailbo.html .
- 44.Williams C, Gilchrist ID, Fraser S, McCarthy HM, Parker J, Warnes P, et al. Normative data for three tests of visuocognitive function in primary school children: Cross-sectional study. Br J Ophthalmol. 2015;99:752–6. doi: 10.1136/bjophthalmol-2014-305868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dutton GN, Lueck AH, Dutton GN. Disorders of the brain and how they can affect vision. In: Dutton GN, Lueck AH, editors. Vision and the brain: Understanding visual impairment in children. Chapter 3. New York: American Foundation for the Blind; 2015. pp. 47–8. [Google Scholar]
- 46.Hyvarinen L, Jacob N. WHAT and HOW Does this Child See? Helsinki, Finland: VISITEST Ltd; 2011. [Google Scholar]
- 47.Brazis PW, Graff-Radford NR, Newman NJ, Lee AG. Ishihara color plates as a test for simultanagnosia. Am J Ophthalmol. 1998;126:850–1. doi: 10.1016/s0002-9394(98)00187-1. [DOI] [PubMed] [Google Scholar]
- 48. [Last accessed on 2020 Sep 20]. Available from: https://cviscotland.org/
- 49.Fazzi E, Bova SM, Uggetti C, Signorini SG, Bianchi PE, Maraucci I, et al. Visual-perceptual impairment in children with periventricular leukomalacia. Brain Dev. 2004;26:506–12. doi: 10.1016/j.braindev.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 50.van den Hout BM, de Vries LS, Meiners LC, Stiers P, van der Schouw YT, Jennekens-Schinkel A, et al. Visual perceptual impairment in children at 5 years of age with perinatal haemorrhagic or ischaemic brain damage in relation to cerebral magnetic resonance imaging. Brain Dev. 2004;26:251–61. doi: 10.1016/S0387-7604(03)00163-3. [DOI] [PubMed] [Google Scholar]
- 51.Fazzi E, Bova S, Giovenzana A, Signorini S, Uggetti C, Bianchi P. Cognitive visual dysfunctions in preterm children with periventricular leukomalacia. Dev Med Child Neurol. 2009;51:974–81. doi: 10.1111/j.1469-8749.2009.03272.x. [DOI] [PubMed] [Google Scholar]
- 52. [Last accessed on 2020 May 18]. Available from: https://www.pearsonassessments.com/store/usassessments/en/Store/Professional-Assessments/Motor-Sensory/Developmental-Test-of-Visual-Perception-%7C-Third-Edition/p/100000779.html .
- 53. [Last accessed on 2020 May 18]. https://www.wpspublish.com/mvpt-4-motor-free-visual-perception-test-4.
- 54.Lennartsson F, Nilsson M, Flodmark O, Jacobson L. Damage to the immature optic radiation causes severe reduction of the retinal nerve fiber layer, resulting in predictable visual field defects. Invest Ophthalmol Vis Sci. 2014;55:8278–88. doi: 10.1167/iovs.14-14913. [DOI] [PubMed] [Google Scholar]
- 55.Jacobson L, Lennartsson F, Nilsson M. Retinal ganglion cell topography predicts visual field function in spastic cerebral palsy? Dev Med Child Neurol. 2020 doi: 10.1111/dmcn.14545. doi: 10.1111/dmcn. 14545. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 56.Lennartsson F, Nilsson M, Flodmark O, Jacobson L, Larsson J. Injuries to the immature optic radiation show correlated thinning of the macular ganglion cell layer. Front Neurol. 2018;9:321. doi: 10.3389/fneur.2018.00321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Practice parameter for assessment and treatment of children and adolescents with autism, American academy of child and adolescent psychiatry. Available from: https://www.jaacap.org/article/S0890-8567(13)00819-8/pdf .
- 58.Clinical practice guidelines for diagnosis, evaluation and treatment of ADHD. American Academy of Pediatrics. Available from: https://pediatrics.aappublications.org/content/144/4 .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.