Abstract
Purpose:
This study assessed “model of care” (MoC) knowledge among Riyadh First Health Cluster (C1) staff (health workers and admin) at Saudi Arabia's Ministry of Health (MOH).
Methods:
This study is cross-sectional, observational, and analytic. Raw data were collected from the data warehouse of the Vision Realization Office (VRO) at the MOH. It was then entered into SPSS, Version 24, and 3,696 individuals were analyzed. Descriptive statistics were presented as numbers and percentages, and a Chi-square test was used to test for associations. The study was approved by the hospital research committee and the Institutional Review Board (HlRI-15-Dec l9-01).
Results:
The staff who knew of the transformation occurring in the healthcare sector were 98.2% male and 93.6% female (P < .001). The staff having more than 20 years of experience represented the highest level of understanding (44.4%). In contrast, a team with 0–1 years of experience had the lowest level of understanding (13.6%) (P < .001). However, the staff with 0–1 years of experience was associated with the highest agreement percentages (93.4%, 92.2%) while the staff with more than 20 years of experience was associated with a lower agreement of percentages (88.2%, 79.1%) (P < .001). Finally, we found pharmacists and primary healthcare centers to generally have the highest knowledge percentages across the studied dimensions (P < .001).
Conclusion:
The C1 staff who participated in this study had good knowledge of Saudi Arabia's MoC. We recommend future elaborating research about the Saudi MoC to compare in detail with the staff in the other sectors and reach an international benchmark.
Keywords: Model of care (MoC), Riyadh First Health Cluster (C1), system of care (SoC), Vision Realization Office (VRO)
Introduction
A “model of care” (MoC) is defined as the way health services are delivered. It outlines the best practices for care and services for people and population groups. It also aims to ensure that people receive the right care at the right time from the right team and in the right place.[1]
The healthcare in Saudi Arabia is currently provided free of charge to all citizens and expatriates working in the public sector, primarily through the Ministry of Health (MOH).[2]
Another unique aspect of the healthcare in Saudi Arabia is that the country serves more than 5 million pilgrims and visitors to the Holy Mosque at Makkah annually and provides free healthcare services to the pilgrims through MOH facilities.[3,4,5]
Healthcare services in Saudi Arabia are provided through three main sectors: the MOH network of hospitals and primary care centers distributed throughout the country, the largest provider, other governmental sectors, and private institutions.[6]
The MOH focuses intensely on prevention and primary care, and it sponsors over 3,300 health centers across Saudi Arabia.[7]
The healthcare system in Saudi Arabia has improved rapidly over recent years, and this development may be attributed to the high prioritization of providing citizens with high-quality healthcare.[8] Currently, the Saudi healthcare system is undergoing a reform process.[9]
Saudi Arabia adopted the “Vision 2030” plan and will achieve its objectives through three main pillars: “A Vibrant Society,” “A Thriving Economy,” and “An Ambitious Nation.”[10] The National Transformation Program (NTP) is one of the executive programs implemented to achieve the Saudi “Vision 2030” plan.[11]
The first theme of the NTP is to “Transform Healthcare” in order to achieve a vibrant society by restructuring a comprehensive and useful health system.[12] This theme will promote public health by implementing a new care model that focuses on prevention and improving Saudi society's health awareness.[12]
The essential components of the Saudi health transformation are the institutionalization of a new health system and a redrafted approach to financing that is independent and flexible, depending on payments for services and not on the budget system. The institutional transformation process separates service providers from regulators.[13,14] The primary objective behind assigning healthcare services is to provide top-quality services to Saudi citizens while allowing the MOH to focus on its central role of supervising, monitoring, and designing health policies.[14]
A health cluster is an integrated and interconnected network of healthcare providers under a single administrative structure that aims to facilitate beneficiaries' access to health services and move them between several types of care.[15] The First Health Cluster in Riyadh (C1) includes five hospitals—King Saud Medical City (KSMC), King Salman Hospital, Al-Iman General Hospital, Imam Abdulrahman Al-Faisal Hospital, Al Naqaha Hospital—and several primary healthcare centers (PHCs), the city's “49 PHCs.”[16] The new MoC was initiated by Saudi MOH in 2018 and was designed based on the six care systems selected based on the demands a person will have of a healthcare system throughout their life, from before birth to supporting their bereaved family after their death.[16] These systems are called the six systems of care (SoC): “Keep Well,” “Planned Care,” “Safe Birth,” “Urgent Care,” “Chronic Care,” and “Last Phase.”[16,17]
The emergency care model team at the Makkah Health Affairs began the pilot stage of the first emergency care model at the Kedi and Al-Eskan health centers on the 1st of Rajab, 1439 AH (March 18, 2018), to relieve pressure on the emergency departments.[18]
A study published in November 2017 discussed implementing a model of emergency care at an Australian hospital.[19] The study aimed to implement a supportive system of emergency nursing care that improves nursing workloads and promotes individual responsibility and accountability for patient care since a fast-paced, quick turnover rate characterized emergency departments alongside a high-acuity workload.[19] Therefore, appropriate staffing was vital to securing positive patient outcomes, and MoCs provide frameworks in which safe and effective patient-to-nurse ratios can be ensured. Quantitative data were analyzed using descriptive statistics, and the qualitative data used a thematic analysis to identify recurrent themes. After implementing an emergency model, the post-data implementation of the emergency nursing care model indicated improved staff satisfaction about workloads and patient care.[19]
A systematic review concerning chronic diseases was published in May 2015.[20] This systematic literature review aimed to identify and synthesize international evidence on the effectiveness of elements included in a Chronic Care model to improve healthcare practices and health outcomes within primary healthcare settings. In this review, the authors focused on the efficacy of healthcare practice and health outcomes associated with implementing a Chronic Care model. Relevant case series and case studies were also included. Of the 77 reviewed papers that met the study's inclusion criteria, all but two reported improvements to healthcare practice or health outcomes for people living with chronic conditions. While the most commonly used elements of a Chronic Care model were self-management support and delivery system design, considerable variations were observed between studies regarding which combinations of elements were included and how Chronic Care model elements were implemented. These papers suggested several factors including supporting reflective healthcare practices and sending clear messages about the importance of chronic disease care. Also, ensuring that leaders support the implementation and sustainability of the interventions was found to possibly have been just as crucial as a Chronic Care model's elements in improving healthcare practice and health outcomes for patients living with chronic diseases.[20]
Accordingly, the current study aimed to assess knowledge through four dimensions (awareness, understanding, acceptance, and action) toward the MoC among C1 staff (health workers and admin) at the MOH.
Methods
Materials
We analyzed data collected from a validated and piloted questionnaire containing multiple questions. Knowledge was assessed along four dimensions: awareness, understanding, acceptance, and action. The first five questions reflected demographic data, and two items explored awareness levels regarding the kingdom's health sector transformation. The rest of the questions sought to measure each of the study's four dimensions of knowledge assessment.
The parameters used in this study were gender, job function, years of experience, and name of the facility. The questionnaire divided the job function into six categories (leadership, admin, nurse, physician, pharmacist, and allied health). Years of experience was categorized as 0–1, 2–5, 6–10, 11–20, and more than 20. Finally, the name of facility parameter indicated all C1 institutions, including King Saud Medical City (KSMC), King Salman Hospital, Al-Iman General Hospital, Imam Abdulrahman Al-Faisal Hospital, Al Naqaha Hospital, and PHCs. Others indicated unspecified facilities, such as any place belonging to the C1 that was not a hospital or a PHC, such as the headquarters of the C1, community health centers, and portable clinics in malls.
Setting
This research was conducted at C1 of the MOH, which includes five hospitals—KSMC, King Salman Hospital, Al-Iman General Hospital, Imam Abdulrahman Al-Faisal Hospital, Al Naqaha Hospital—and the “49 PHCs” within the city as well as C1 locations that were not hospitals or PHCs.
Design
This research is a cross-sectional, observational, and analytic study that seeks to assess MoC knowledge among staff (health workers and admin) working at hospitals and PHCs belonging to C1 of the MOH. The study was approved by the hospital research committee and the Institutional Review Board (IRB), with approval number HlRI-15-Dec l9-01 (Approved in 16 December, 2019).
Population
The studied population was the staff (health workers and admin) working in C1 hospitals and PHCs.
Data collection
Raw data were collected from the data warehouse of the Vision Realization Office (VRO) at the MOH in a table format. These data included gender, jobs, years of experience, and facilities. A PulseCheck survey was developed by VRO and used to help leaders steer the health system transformation by unveiling real-time insights and pinpointing focus areas to increase staff understanding and engagement. The VRO distributed two validated piloted questionnaires in Arabic and English, which contained the same information in order to ensure coverage of the highest number of C1 staff. The survey link was distributed to all the 16,700 C1 staff through the C1 Communications Team, who were free to distribute the survey as they saw fit via WhatsApp, email, text message, and QR codes. The survey was open to responses for 2 weeks, from July 15, 2019 to August 1, 2019, in order to ensure a high response rate. In total, 3,696 out of 16,700 employees responded to the questionnaire.
Statistical method
The study's table of collected data included 3,696 out of 16,700 C1 employees. These data were entered into the SPSS statistical package, Version 24. Descriptive statistics were presented through numbers and percentages, and a Chi-square test was used to test for associations. A P value of <.05 was taken as the level of significance between responses.
Results
In total, 3,696 C1 staff responded to the study's survey. Respondents were 57.7% males and 42.3% females. Based on the respondents' jobs, nurses represented about one-third of the respondents. The staff with 10 years of experience or less represented more than two-thirds of the respondents. Also, about three-quarters of the respondents worked at KSMC. Table 1 shows the respondents' demographic profile.
Table 1.
Demographic profile of the survey respondents
| Demographic Profile | n (%) |
|---|---|
| Gender | |
| Male | 2131 (57.7%) |
| Female | 1565 (42.3%) |
| Job Function | |
| Leadership role | 283 (7.6%) |
| Admin role | 614 (16.6%) |
| Nurse | 1254 (34%) |
| Physician | 808 (21.8%) |
| Pharmacist | 514 (14%) |
| Allied Healtha | 223 (6.0%) |
| Years of experience | |
| 0-1 year | 243 (6.5%) |
| 2-5 years | 1001 (27.1%) |
| 6-10 years | 1631 (44.1%) |
| 11-20 years | 625 (17.0%) |
| More than 20 years | 196 (5.3%) |
| Name of the facility | |
| King Saud Medical City | 2764 (74.8%) |
| King Salman Hospital | 217 (5.9%) |
| Imam Abdul Rahman Hospital | 165 (4.5%) |
| Al -Iman General Hospital | 120 (3.2%) |
| Al Naqaha Hospital | 95 (2.6%) |
| Primary Health Center (PHC) | 319 (8.6%) |
| Othersb | 16 (.4%) |
| Total | 3696 (100.0%) |
aAny professions that provide a range of diagnostic, technical, therapeutic, and support services in connection with healthcare. bUnspecified facilities, such as any place belonging to the C1 that was not a hospital or a PHC, such as the headquarters of the C1, community health centers, and portable clinics in malls
By job function [Table 2], we expected males to outnumber females in all job categories because the total number of male workers (2,131; 57.7%) exceeded the total number of female workers (1,565; 42.3%). But we found women were significantly more than men in the nursing role.
Table 2.
Job function according to the gender
| Male n (%) | Female n (%) | |
|---|---|---|
| Job Function | ||
| Leadership role | 225 (79.5%) | 58 (20.5%) |
| Admin role | 371 (60.4%) | 243 (39.6%) |
| Nurse | 407 (32.5%) | 847 (67.5%) |
| Physician | 607 (75.1%) | 201 (24.9%) |
| Pharmacist | 339 (66.0%) | 175 (34.0%) |
| Allied Health | 182 (81.6%) | 41 (18.4%) |
| Total | 2131 (57.7%) | 1565 (42.3%) |
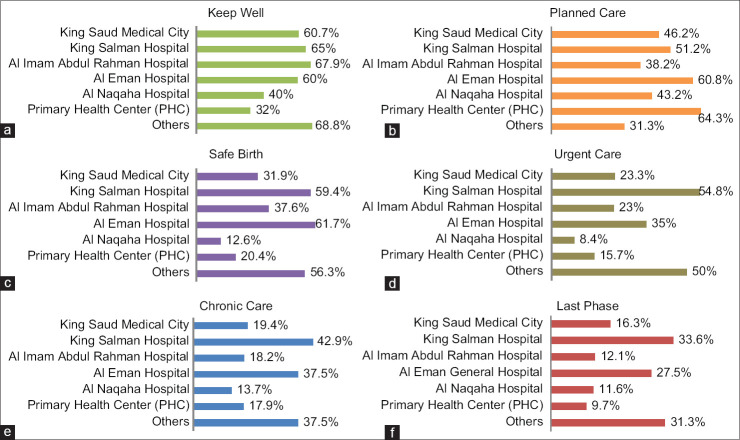
Our study began with the staff who had heard of the transformation occurring in the healthcare sector, including 3,557 respondents out of a total of 3,696 and representing 96.2% of the total staff. By gender, 98.2% of these respondents were male and 93.6% were female (P < .001), reflecting high awareness about the healthcare system transformation in Saudi Arabia [Figure 1].
Figure 1.
Staff who heard of transformation based on gender
Also, all respondents from all parameters had heard about the Saudi MoC—according to their answers, a question was intended to measure awareness.
The data in Table 3 reflect the respondents' answers to “which outcome is the MoC aiming to achieve?” and were intended to measure the C1 staff's understanding by comparing across genders, jobs, years of experience, and facility names. The MoC outcome response choices were “Preventing healthy people from getting sick,” “Detecting diseases early,” “Ensuring the patient has a clear path through the healthcare system,” “Two aims,” “All three aims,” and “I don't know.” The respondents answered this question as follows.
Table 3.
Staff who answer which outcomes is Model of Care aiming to achieve
| n (%) | Siga | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Preventing healthy people from getting sick | Detecting diseases early | Ensuring the patient has a clear path through the healthcare system | Tow aims | All three aims | I don’t know | ||
| Gender | <0.001 | ||||||
| Male | 649 (30.4%) | 509 (23.8%) | 256 (12.0%) | 270 (12.7%) | 415 (19.4%) | 32 (1.5%) | |
| Female | 383 (24.5%) | 303 (19.4%) | 258 (16.5%) | 213 (13.6%) | 376 (24%) | 32 (2.1%) | |
| Job Function | |||||||
| Leadership role | 56 (19.8%) | 31 (11.0%) | 56 (19.8%) | 46 (16.2%) | 88 (31.1%) | 6 (2.1%) | <0.001 |
| Admin role | 133 (21.7%) | 110 (18.0%) | 107 (17.4%) | 88 (14.3%) | 158 (23.4%) | 18 (3.0%) | |
| Nurse | 343 (27.4%) | 265 (21.2%) | 167 (13.3%) | 165 (13.1%) | 295 (23.6%) | 19 (1.5%) | |
| Physician | 262 (32.4%) | 191 (23.6%) | 109 (13.5%) | 92 (11.4%) | 145 (17.9%) | 9 (1.1%) | |
| Pharmacist | 185 (36.0%) | 173 (33.7%) | 44 (8.6%) | 63 (12.2%) | 48 (9.3%) | 1 (.2%) | |
| Allied Health | 53 (23.7%) | 43 (19.3%) | 31 (13.9%) | 28 (12.5%) | 57 (25.6%) | 11 (4.9%) | |
| Years of experience | |||||||
| 0-1 year | 104 (42.8%) | 50 (20.6%) | 29 (11.9%) | 22 (9.0%) | 33 (13.6%) | 5 (2.1%) | <0.001 |
| 2-5 years | 355 (35.5%) | 241 (24.1%) | 128 (12.8%) | 116 (11.5%) | 145 (14.5%) | 16 (1.6%) | |
| 6-10 years | 461 (28.3%) | 443 (27.2%) | 180 (11.0%) | 223 (13.6%) | 299 (18.4%) | 25 (1.5%) | |
| 11-20 years | 99 (15.8%) | 65 (10.6%) | 132 (21.2%) | 88 (14.0%) | 227 (36.3%) | 14 (2.2%) | |
| More than 20 years | 13 (6.6%) | 13 (6.6%) | 45 (23.0%) | 34 (17.3%) | 87 (44.4%) | 4 (2.0%) | |
| Name of Facility | |||||||
| King Saud Medical City | 789 (28.5%) | 632 (23.0%) | 394 (14.2%) | 356 (12.9%) | 548 (19.8%) | 45 (1.6%) | <0.001 |
| King Salman Hospital | 20 (9.3%) | 10 (4.6%) | 43 (19.8%) | 38 (17.5%) | 98 (45.2%) | 8 (3.7%) | |
| Imam Abdul Rahman Hospital | 48 (29.1%) | 21 (12.7%) | 24 (14.5%) | 28 (17.0%) | 41 (24.8%) | 3 (1.8%) | |
| Al-Iman General Hospital | 14 (11.7%) | 11 (9.2%) | 21 (17.5%) | 23 (19.1%) | 47 (39.2%) | 4 (3.3%) | |
| Al Naqaha Hospital | 29 (30.5%) | 27 (28.4%) | 8 (8.4%) | 10 (10.5%) | 19 (20.0%) | 2 (2.1%) | |
| Primary Health Center (PHC) | 131 (41.1%) | 110 (34.5%) | 21 (6.6%) | 24 (7.5%) | 31 (9.7%) | 2 (.6%) | |
| Others | 1 (6.3%) | 1 (6.3%) | 3 (18.8%) | 4 (25.0%) | 7 (43.8%) | 0 (.0%) | |
| Total | 1032 (28.0%) | 812 (22.0%) | 514 (13.9%) | 483 (13.0%) | 791 (21.4%) | 64 (1.7%) | 3696 (100%) |
aP was calculated based on Chi-square
“Preventing healthy people from getting sick”: 28%
”Detecting diseases early”: 22%
”Ensuring the patient has a clear path through the healthcare system”: 13.9%
”Two aims”: 13%
”All three aims”: 21.4%
”I don't' know”: 1.7%
The responses to this question showed that just a few of the 64 staff represented (1.7%) did not know the MoC aims, and these numbers reflected the right understanding in general.
We considered respondents who chose “All three aims” to be the most understanding of the MoC based on each parameter. The percentage of respondents based on gender was 24% females and 19.4% males (P < .001).
Based on job function, we found that the staff in leadership roles had the highest understanding (31.1%), which we expected due to their position and responsibility for change. The lowest understanding level corresponded to the Allied Health staff because they were the highest percentage who chose “I don't know” (4.9%; P < .001).
The result based on “Years of experience,” we found that the staff which had more experience also had more knowledge. Respondents who had “More than 20 years of experience” represented the highest understanding (44.4%), while the staff with 0–1 years of experience had the lowest level of understanding (13.6%) (P < .001).
Finally, our results based on facility names showed that the staff which worked at King Salman Hospital reflected the highest percentage for choosing “All three aims” (45.2%) and also had the highest rate of choosing “I don't know” (3.7%) (P < .001).
For all agreement scale questions in the result Tables 4-8, we interpreted the collected data by merging the “strongly agree” and “agree” choices together to ensure a good measure of the total agreement in general and based on each parameter.
Table 4.
Staff who can confidently explain what Model of Care is to a colleague or a friend
| n (%) | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Strongly agree | Agree | Neutral | Disagree | Strongly disagree | Missing | Sig | |
| Gender | |||||||
| Male | 1359 (63.8%) | 522 (24.5%) | 199 (9.3%) | 38 (1.8%) | 9 (.4%) | 4 (.2%) | <0.001 |
| Female | 792 (50.6%) | 506 (32.3%) | 236 (15.1%) | 25 (1.6%) | 5 (.3%) | 1 (.1%) | |
| Job Function | |||||||
| Leadership role | 123 (43.5%) | 97 (34.3%) | 46 (16.3%) | 13 (4.6%) | 3 (1.1%) | 1 (.4%) | |
| Admin role | 295 (48.0%) | 205 (33.4%) | 98 (16.0%) | 12 (2.0%) | 3 (.5%) | 1 (.2%) | <0.001 |
| Nurse | 687 (54.8%) | 397 (31.7%) | 155 (12.4%) | 11 (.9%) | 3 (.2%) | 1 (.1%) | |
| Physician | 522 (64.6%) | 186 (23.0%) | 80 (9.9%) | 16 (2.0%) | 3 (.4%) | 1 (.1%) | |
| Pharmacist | 420 (81.7%) | 79 (15.4%) | 15 (2.9%) | 0 (.0%) | 0 (.0%) | 0 (.0%) | |
| Allied Health | 104 (46.6%) | 64 (28.7%) | 41 (18.4%) | 11 (4.9%) | 2 (.9%) | 1 (.4%) | |
| Years of experience | |||||||
| 0-1 year | 183 (75.3%) | 34 (14.0%) | 23 (9.5%) | 2 (.8%) | 0 (.0%) | 1 (.4%) | |
| 2-5 years | 692 (69.1%) | 200 (20.0%) | 92 (9.2%) | 13 (1.3%) | 4 (.4%) | 0 (.0%) | <0.001 |
| 6-10 years | 998 (61.2%) | 457 (28.0%) | 143 (8.8%) | 27 (1.7%) | 4 (.2%) | 2 (.1%) | |
| 11-20 years | 234 (37.4%) | 237 (37.9%) | 132 (21.1%) | 14 (2.2%) | 6 (1.0%) | 2 (.3%) | |
| More than 20 years | 44 (22.4%) | 100 (51.0%) | 45 (23.0%) | 7 (3.6%) | 0 (.0%) | 0 (.0%) | |
| Name of the facility | |||||||
| King Saud Medical City | 1650 (59.7%) | 759 (27.5%) | 303 (11.0%) | 41 (1.5%) | 11 (.4%) | 0 (.0%) | |
| King Salman Hospital | 70 (32.3%) | 95 (43.8%) | 44 (20.3%) | 7 (3.2%) | 1 (.5%) | 0 (.0%) | <0.001 |
| Imam Abdul Rahman Hospital | 85 (51.5%) | 49 (29.7%) | 22 (13.3%) | 4 (2.4%) | 0 (.0%) | 5 (3.0%) | |
| Al-Iman General Hospital | 41 (34.2%) | 48 (40.0%) | 27 (22.5%) | 3 (2.5%) | 1 (.8%) | 0 (.0%) | |
| Al Naqaha Hospital | 58 (61.1%) | 22 (23.2%) | 9 (9.5%) | 6 (6.3%) | 0 (.0%) | 0 (.0%) | |
| Primary Health Center (PHC) | 243 (76.2%) | 46 (14.4%) | 28 (8.8%) | 2 (.6%) | 0 (.0%) | 0 (.0%) | |
| Others | 4 (25.0%) | 9 (56.3%) | 2 (12.5%) | 0 (.0%) | 1 (6.3%) | 0 (.0%) | |
| Total | 2151 (58.2%) | 1028 (27.8%) | 435 (11.8%) | 63 (1.7%) | 14 (.4%) | 5 (.1%) | 3696 (100%) |
Table 8.
Staff who are ready to convince my colleagues and friends of the benefits of Model of Care
| n (%) | Sig | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Strongly agree | Agree | Neutral | Disagree | Strongly disagree | Missing | ||
| Gender | |||||||
| Male | 1402 (65.8%) | 447 (21.0%) | 249 (11.7%) | 21 (1.0%) | 3 (.1%) | 9 (.4%) | |
| Female | 862 (55.1%) | 511 (32.7%) | 172 (11.0%) | 13 (.8%) | 3 (.2%) | 4 (.3%) | <0.001 |
| Job Function | |||||||
| Leadership role | 152 (53.7%) | 92 (32.5%) | 36 (12.7%) | 0 (.0%) | 1 (.4%) | 2 (.7%) | |
| Admin role | 322 (52.4%) | 133 (21.7%) | 143 (23.3%) | 12 (2.0%) | 3 (.5%) | 1 (.2%) | <0.001 |
| Nurse | 728 (58.1%) | 420 (33.5%) | 92 (7.3%) | 8 (.6%) | 1 (.1%) | 5 (.4%) | |
| Physician | 546 (67.6%) | 167 (20.7%) | 84 (10.4%) | 9 (1.1%) | 0 (.0%) | 2 (.2%) | |
| Pharmacist | 409 (79.6%) | 84 (16.3%) | 18 (3.5%) | 2 (.4%) | 0 (.0%) | 1 (.2%) | |
| Allied Health | 107 (48.0%) | 62 (27.8%) | 48 (21.5%) | 3 (1.3%) | 1 (.4%) | 2 (.9%) | |
| Years of experience | |||||||
| 0-1 year | 191 (78.6%) | 33 (13.6%) | 14 (5.8%) | 3 (1.2%) | 0 (.0%) | 2 (.8%) | |
| 2-5 years | 714 (71.3%) | 172 (17.2%) | 106 (10.6%) | 6 (.6%) | 1 (.1%) | 2 (.2%) | <0.001 |
| 6-10 years | 1034 (63.4%) | 422 (25.9%) | 145 (8.9%) | 20 (1.2%) | 4 (.2%) | 6 (.4%) | |
| 11-20 years | 260 (41.6%) | 241 (38.6%) | 115 (18.4%) | 5 (.8%) | 1 (.2%) | 3 (.5%) | |
| More than 20 years | 65 (33.2%) | 90 (45.9%) | 41 (20.9%) | 0 (.0%) | 0 (.0%) | 0 (.0%) | |
| Name of the facility | |||||||
| King Saud Medical City | 1705 (61.7%) | 727 (26.3%) | 294 (10.6%) | 28 (1.0%) | 4 (.1%) | 6 (.2%) | |
| King Salman Hospital | 93 (42.9%) | 69 (31.8%) | 52 (24.0%) | 3 (1.4%) | 0 (.0%) | 0 (.0%) | <0.001 |
| Imam Abdul Rahman Hospital | 97 (58.8%) | 42 (25.5%) | 18 (10.9%) | 1 (.6%) | 0 (.0%) | 7 (4.2%) | |
| Al-Iman General Hospital | 50 (41.7%) | 46 (38.3%) | 22 (18.3%) | 1 (.8%) | 1 (.8%) | 0 (.0%) | |
| Al Naqaha Hospital | 58 (61.1%) | 15 (15.8%) | 20 (21.1%) | 1 (1.1%) | 1 (1.1%) | 0 (.0%) | |
| Primary Health Center (PHC) | 255 (79.9%) | 50 (15.7%) | 14 (4.4%) | 0 (.0%) | 0 (.0%) | 0 (.0%) | |
| Others | 6 (37.5%) | 9 (56.3%) | 1 (6.3%) | 0 (.0) | 0 (.0%) | 0 (.0%) | |
| Total | 2264 (61.3%) | 958 (25.9%) | 421 (11.4%) | 34 (.9%) | 6 (.2%) | 13 (.4%) | 3696 (100%) |
As shown in Table 4, the question “I am confident that I can explain what the MoC is to a colleague or a friend” was subject to staff reactions and confidence levels with staff sharing their understandings. The respondents' total agreement was 86% for this question, which reflected a good response and high confidence levels among the C1 staff.
By gender, we found that the men's agreement was higher than the women's by percentage (88.3% vs. 82.9%; P < .001). Also, based on job function, we found that the Pharmacist's role had the highest agreement (97.1%) and Allied Health had the lowest agreement (75.3%), with a significant P value (<.001).
In the years of experience aspect, we found that the less-experienced staff had the strongest reaction and the most confidence in sharing their understandings and explaining what the MoC is. In contrast, the more experienced staff were less reactive and expressed low confidence. Indeed, respondents with 0–1 years of experience agreed at 89.3%, and the staff with more than 20 years' experience had the lowest agreement percentage at 73% (P < .001).
Finally, our results based on facility names found that the staff who worked at PHCs had the highest agreement (90.6%) and the staff who worked at Al-Iman General Hospital had the lowest agreement (74.2%), with statistical significance (P < .001).
Two questions measured the acceptance dimension. One of these questions stated, “The model of care will improve the quality of healthcare services that patients receive,” measuring acceptance among C1 staff toward the MoC [Table 5]. The respondents' total agreement was 93.1%, which reflected their high level of acceptance, through this question to the new MoC and its ongoing implementation.
Table 5.
Staff agreed that Model of Care will improve the quality of healthcare services the patient is receiving
| Strongly agree | Agree | Neutral | Disagree | Strongly disagree | Missing | Sig | |
|---|---|---|---|---|---|---|---|
| Gender | |||||||
| Male | 1367 (64.1%) | 604 (28.3%) | 141 (6.6%) | 11 (.5%) | 4 (.2%) | 4 (.2%) | |
| Female | 897 (57.3%) | 573 (36.6%) | 89 (5.7%) | 5 (.3%) | 0 (.0%) | 1 (.1%) | <0.001 |
| Job Function | |||||||
| Leadership role | 142 (50.2%) | 111 (39.2%) | 27 (9.5%) | 2 (.7%) | 0 (.0%) | 1 (.4%) | |
| Admin role | 331 (53.9%) | 210 (34.2%) | 69 (11.2%) | 3 (.5%) | 1 (.2%) | 0 (.0%) | <0.001 |
| Nurse | 746 (59.5%) | 450 (35.9%) | 54 (4.3%) | 3 (.2%) | 0 (.0%) | 1 (.1%) | |
| Physician | 534 (66.1%) | 216 (26.7%) | 49 (6.1%) | 6 (.7%) | 2 (.2%) | 1 (.1%) | |
| Pharmacist | 393 (76.5%) | 113 (22.0%) | 7 (1.4%) | 0 (.0%) | 0 (.0%) | 1 (.2%) | |
| Allied Health | 118 (52.9%) | 77 (34.5%) | 24 (10.8%) | 2 (.9%) | 1 (.4%) | 1 (.4%) | |
| Years of experience | |||||||
| 0-1 year | 180 (74.1%) | 54 (22.2%) | 7 (2.9%) | 1 (.4%) | 0 (.0%) | 1 (.4%) | |
| 2-5 years | 690 (68.9%) | 242 (24.2%) | 65 (6.5%) | 3 (.3%) | 0 (.0%) | 1 (.1%) | <0.001 |
| 6-10 years | 1037 (63.6%) | 510 (31.3%) | 73 (4.5%) | 6 (.4%) | 3 (.2%) | 2 (.1%) | |
| 11-20 years | 288 (46.1%) | 267 (42.7%) | 65 (10.4%) | 3 (.5%) | 1 (.2%) | 1 (.2%) | |
| More than 20 years | 69 (35.2%) | 104 (53.1%) | 20 (10.2%) | 3 (1.5%) | 0 (.0%) | 0 (.0%) | |
| Name of the facility | |||||||
| King Saud Medical City | 1697 (61.4%) | 893 (32.3%) | 163 (5.9%) | 10 (.4%) | 1 (.0%) | 0 (.0%) | |
| King Salman Hospital | 100 (46.1%) | 87 (40.1%) | 26 (12.0%) | 3 (1.4%) | 0 (.0%) | 1 (.5%) | <0.001 |
| Imam Abdul Rahman Hospital | 90 (54.5%) | 56 (33.9%) | 13 (7.9%) | 1 (.6%) | 1 (.6%) | 4 (2.4%) | |
| Al -Iman General Hospital | 53 (44.2%) | 50 (41.7%) | 15 (12.5%) | 0 (.0%) | 2 (1.7%) | 0 (.0%) | |
| Al Naqaha Hospital | 63 (66.3%) | 26 (27.4%) | 4 (4.2%) | 2 (2.1%) | 0 (.0%) | 0 (.0%) | |
| Primary Health Center (PHC) | 250 (78.4%) | 60 (18.8%) | 9 (2.8%) | 0 (.0%) | 0 (.0%) | 0 (.0%) | |
| Others | 11 (68.8%) | 5 (31.2%) | 0 (.0%) | 0 (.0%) | 0 (.0%) | 0 (.0%) | |
| Total | 2264 (61.3%) | 1177 (31.8%) | 230 (6.2%) | 16 (.4%) | 4 (.1%) | 5 (.1%) | 3696 (100%) |
Our results based on gender showed that women's agreement was higher than men's agreement, at 93.9 and 92.4%, respectively (P < .001). In assessing job function, we found that the Pharmacist's role had the highest agreement (98.5%) and Allied Health's had the lowest agreement (87.4%) with a significant P value (<.001). Also, for the years of experience aspect, we found the staff with 0–1 years of experience expressed the highest agreement (96.3%) while the staff with more than 20 years of experience reflected less agreement (88.3%) (P < .001).
Finally, the results for this question based on facility names showed that the staff who worked at any C1 location that was not a hospital or PHCs (”others”) had the highest agreement (100%), and the staff who worked at Al-Iman General Hospital had the lowest agreement (85.9%), with statistical significance (P < .001).
The result of the question stating, “The model of care will have a positive impact on my career,” complemented the acceptance dimension measures, as the second question intended to measure this dimension [Table 6]. This question's total agreement was 88.9%, which also reflected a high level of acceptance toward the new MoC among the C1 staff.
Table 6.
Staff Agreed that Model of Care will have a positive impact on their career
| n (%) | Sig | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Strongly agree | Agree | Neutral | Disagree | Strongly disagree | Missing | ||
| Gender | |||||||
| Male | 1396 (65.5%) | 476 (22.3%) | 233 (10.9%) | 15 (.7%) | 6 (.3%) | 5 (.2%) | |
| Female | 881 (56.3%) | 532 (34.0%) | 141 (9.0%) | 5 (.3%) | 1 (.1%) | 5 (.3%) | <0.001 |
| Job Function | |||||||
| Leadership role | 136 (48.1%) | 93 (32.9%) | 50 (17.7%) | 1 (.4%) | 2 (.7%) | 1 (.4%) | |
| Admin role | 311 (50.7%) | 179 (29.2%) | 112 (18.2%) | 6 (1.0%) | 3 (.5%) | 3 (.5%) | <0.001 |
| Nurse | 747 (59.6%) | 423 (33.7%) | 82 (6.5%) | 2 (.2%) | 0 (.0%) | 0 (.0%) | |
| Physician | 551 (68.2%) | 167 (20.7%) | 76 (9.4%) | 8 (1.0%) | 2 (.2%) | 4 (.5%) | |
| Pharmacist | 415 (80.7%) | 84 (16.3%) | 13 (2.5%) | 0 (.0%) | 0 (.0%) | 2 (.4%) | |
| Allied Health | 117 (52.5%) | 62 (27.8%) | 41 (18.4%) | 3 (1.3%) | 0 (.0%) | 0 (.0%) | |
| Years of experience | |||||||
| 0-1 year | 188 (77.4%) | 35 (14.4%) | 16 (6.6%) | 1 (.4%) | 0 (.0%) | 3 (1.2%) | |
| 2-5 years | 716 (71.5%) | 180 (18.0%) | 98 (9.8%) | 4 (.4%) | 2 (.2%) | 1 (.1%) | <0.001 |
| 6-10 years | 1050 (64.4%) | 445 (27.3%) | 119 (7.3%) | 8 (.5%) | 4 (.2%) | 5 (.3%) | |
| 11-20 years | 260 (41.6%) | 252 (40.3%) | 108 (17.3%) | 3 (.5%) | 1 (.2%) | 1 (.2%) | |
| More than 20 years | 63 (32.1%) | 96 (49.0%) | 33 (16.8%) | 4 (2.0%) | 0 (.0%) | 0 (.0%) | |
| Name of the facility | |||||||
| King Saud Medical City | 1721 (62.3%) | 751 (27.2%) | 267 (9.7%) | 14 (.5%) | 6 (.2%) | 5 (.2%) | |
| King Salman Hospital | 92 (42.4%) | 82 (37.8%) | 41 (18.9%) | 2 (.9%) | 0 (.0%) | 0 (.0%) | <0.001 |
| Imam Abdul Rahman Hospital | 92 (55.8%) | 44 (26.7%) | 22 (13.3%) | 3 (1.8%) | 0 (.0%) | 4 (2.4%) | |
| Al-Iman General Hospital | 53 (44.2%) | 45 (37.5%) | 21 (17.5%) | 0 (.0%) | 1 (.8%) | 0 (.0%) | |
| Al Naqaha Hospital | 62 (65.3%) | 20 (21.1%) | 11 (11.6%) | 1 (1.1%) | 0 (.0%) | 1 (1.1%) | |
| Primary Health Center (PHC) | 249 (78.1%) | 59 (18.5%) | 11 (3.4%) | 0 (.0%) | 0 (.0%) | 0 (.0%) | |
| Others | 8 (50.0%) | 7 (43.8%) | 1 (6.3%) | 0 (.0%) | 0 (.0%) | 0 (.0%) | |
| Total | 2277 (61.6%) | 1008 (27.3%) | 374 (10.1%) | 20 (.5%) | 7 (.2%) | 10 (.3%) | 3696 (100%) |
Based on gender, women's agreement in responding to this question was higher than men's agreement, at 90.3 and 87.8%, respectively (P < .001). Based on job function, our results for this question showed that the Pharmacist role had the highest agreement (97%), and the Admin role had the lowest agreement (79.9%), with a significant P value (<.001).
In assessing years of experience again, we found that the staff with 0–1 years of experience expressed the highest agreement (91.8%) while the staff with more than 20 years of experience expressed less agreement (81.8%) (P < .001).
Finally, our results based on facility names for this question showed that the staff who worked at PHCs expressed the highest agreement (96.6%), and the staff who worked at King Salman Hospital expressed the lowest agreement (80.2%), with statistical significance (P < .001).
The final knowledge assessment dimension of our data was action, which was measured through two questions. One of these questions was, “I am ready to participate in the implementation of the model of care,” measuring C1 staff's action in implementing the new MoC. This action reflected in their readiness to participate in implementing the MoC in our health system [Table 7]. The total agreement for this question was 90.9% across respondents.
Table 7.
Staff who ready to participate in the implementation of Model of Care
| n (%) | Sig | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Strongly agree | Agree | Neutral | Disagree | Strongly disagree | Missing | ||
| Gender | |||||||
| Male | 1400 (65.7%) | 540 (25.3%) | 170 (8.0%) | 11 (.5%) | 1 (.0%) | 9 (.4%) | |
| Female | 884 (56.5%) | 537 (34.3%) | 131 (8.4%) | 5 (.3%) | 2 (.1%) | 6 (.4%) | <0.001 |
| Job Function | |||||||
| Leadership role | 165 (58.3%) | 96 (33.9%) | 18 (6.4%) | 1 (.4%) | 0 (.0%) | 3 (1.1%) | |
| Admin role | 323 (52.6%) | 154 (25.1%) | 123 (20.0%) | 7 (1.1%) | 2 (.3%) | 5 (.8%) | <0.001 |
| Nurse | 734 (58.5%) | 437 (34.8%) | 75 (6.0%) | 5 (.4%) | 0 (.0%) | 3 (.2%) | |
| Physician | 545 (67.5%) | 209 (25.9%) | 49 (6.1%) | 2 (.2%) | 1 (.1%) | 2 (.2%) | |
| Pharmacist | 400 (77.8%) | 102 (19.8%) | 10 (1.9%) | 1 (.2%) | 0 (.0%) | 1 (.2%) | |
| Allied Health | 117 (52.5%) | 79 (35.4%) | 26 (11.7%) | 0 (.0%) | 0 (.0%) | 1 (.4%) | |
| Years of experience | |||||||
| 0-1 year | 181 (74.5%) | 46 (18.9%) | 12 (4.9%) | 1 (.4%) | 0 (.0%) | 3 (1.2%) | |
| 2-5 years | 684 (68.3%) | 230 (23.0%) | 80 (8.0%) | 3 (.3%) | 0 (.0%) | 4 (.4%) | <0.001 |
| 6-10 years | 1046 (64.1%) | 460 (28.2%) | 112 (6.9%) | 7 (.4%) | 2 (.1%) | 4 (.2%) | |
| 11-20 years | 300 (48.0%) | 241 (38.6%) | 76 (12.2%) | 4 (.6%) | 1 (.2%) | 3 (.5%) | |
| More than 20 years | 73 (37.2%) | 100 (51.0%) | 21 (10.7%) | 1 (.5%) | 0 (.0%) | 1 (.5%) | |
| Name of the facility | |||||||
| King Saud Medical City | 1703 (61.6%) | 816 (29.5%) | 227 (8.2%) | 11 (.4%) | 1 (.0%) | 6 (.2%) | |
| King Salman Hospital | 109 (50.2%) | 79 (36.4%) | 26 (12.0%) | 2 (.9%) | 0 (.0%) | 1 (.5%) | <0.001 |
| Imam Abdul Rahman Hospital | 93 (56.4%) | 50 (30.3%) | 11 (6.7%) | 2 (1.2%) | 1 (.6%) | 8 (4.8%) | |
| Al-Iman General Hospital | 54 (45.0%) | 48 (40.0%) | 17 (14.2%) | 0 (.0%) | 1 (.8%) | 0 (.0%) | |
| Al Naqaha Hospital | 62 (65.3%) | 21 (22.1%) | 12 (12.6%) | 0 (.0%) | 0 (.0%) | 0 (.0%) | |
| Primary Health Center (PHC) | 255 (79.9%) | 57 (17.9%) | 7 (2.2%) | 0 (.0%) | 0 (.0%) | 0 (.0%) | |
| Others | 8 (50.0%) | 6 (37.5%) | 1 (6.3%) | 1 (6.3%) | 0 (.0%) | 0 (.0%) | |
| Total | 2284 (61.8%) | 1077 (29.1%) | 301 (8.1%) | 16 (.4%) | 3 (.1%) | 15 (.4%) | 3696 (100%) |
Based on gender, the men's agreement was higher than the women's agreement, at 91 and 90.8%, respectively (P < .001). And by taking job function, we found the Pharmacist to have the highest agreement (97.6%) and the Admin role to have the lowest agreement (77.7%), with a significant P value (<.001).
By years of experience, we found the staff with 0–1 years of experience had the highest agreement (93.4%) while the staff with 11–20 years' experience expressed less agreement (86.6%) (P < .001).
Finally, our results for this question by facility names suggested that the staff who worked at PHCs had the highest agreement (97.8%) and the staff who worked at Al-Iman General Hospital had the lowest agreement (85%), with statistical significance (P < .001).
The question “I am ready to convince my colleagues and friends of the benefits of the model of care” complements the former action measuring the question. The second question intended to measure this dimension [Table 8]. This question's total agreement was 87.2%, which also gave us a good impression of the action level toward the new MoC among the C1 staff.
The female respondents' agreement to this question was higher than the male respondents' agreement, at 87.8 and 86.8%, respectively (P < .001). Our job function results showed that the Pharmacist role had the highest agreement (95.9%), and the Admin role had the lowest agreement (74.1%), with a significant P value (<.001).
The staff with 0-1 years of experience expressed the highest agreement (92.2%), while the staff with more than 20 years' experience expressed less agreement (79.1%) (P < .001).
Finally, the results for this question based on facility names showed that the staff who worked at PHCs had the highest agreement (95.6%) and the staff who worked at King Salman Hospital had the lowest agreement (74.7%), with statistical significance (P < .001).
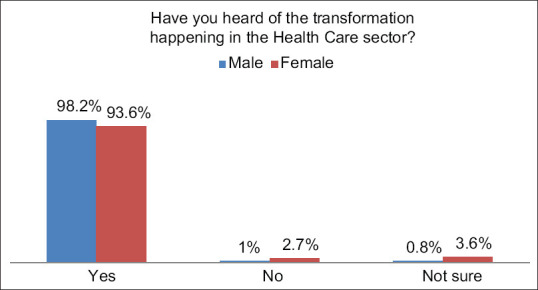
The data presented in Figure 2 (a–-f) show that each system of the Six Systems of Care (”Keep Well,” “Planned Care,” “Safe Birth,” “Urgent Care,” “Chronic Care,” and “Last Phase”) reflected awareness levels among the C1 staff-based facility names. The question that we intended to measure awareness of the SoC was, “Which of systems of care have you heard about?”
Figure 2.
Systems of care heard about based on the name of the facility. (a) Keep Well (b) Planned Care (c) Safe Birth (d) Urgent Care (e) Chronic Care (f) Last Phase
Starting with the “Keep Well” system and the percentage of staff who had heard about it, we found that C1 locations that were not a hospital or PHC (”others”) had the highest percentage of awareness (68.8%) while PHCs had the lowest rate (32%) (P < .001) [Figure 2a]. For the “Planned Care” system, PHCs had the highest percentage (64.3%), and the lowest rate was for “others” (31.3%), with a significant P value (<.001) [Figure 2b]. Moreover, the corresponding results for the “Safe Birth” system showed that the staff at Al-Iman General Hospital had the highest percentage of awareness (61.7%), while the lowest percentage was the staff at Al Naqaha Hospital (12.6%) (P < .001) [Figure 2c]. The “Urgent Care” system had a high percentage of awareness at King Salman Hospital (54.8%) and the lowest percentage at Al Naqaha Hospital (8.4%) (P < .001) [Figure 2d]. For the “Chronic Care” system, King Salman Hospital also had the highest percentage of awareness (42.9%), while the lowest rate was at Al Naqaha Hospital (13.7%) again (P < .001) [Figure 2e]. Finally, the “Last Phase” System saw the highest percentage of awareness at King Salman Hospital (33.6%) and the lowest at PHCs (9.7%) (P < .001) [Figure 2f].
In summary, these results showed that the overall knowledge recorded high percentages for each dimension among the study's total respondents.
Discussion
This study was assessing the knowledge of the MoC among staff (health workers and admin) at hospitals and PHCs in the C1. The studies mentioned in our literature review were recently conducted, and they perfectly discussed the impact of applying MoCs on the quality of patient services; however, each study discussed only one SoC. We did not find any study that included all SoCs and that was designed for Saudi Arabia. This gap in the literature was due to the MoC concept being into the health system in Saudi Arabia, having been adapted from several models around the world. Our study used the VRO expectations and information about how to measure C1 staff's knowledge because no previous studies offered beneficial questionnaires for the current research.
In this study, we found that each dimension's proportions reflected a good impression of C1 staff's MoC knowledge.
The most exciting aspect of all the tables depicting our results was that, based on years of experience, we noticed that the staff who had more experience also had more knowledge and a better understanding of the Saudi MoC. On the other hand, we found that the less-experienced staff had the highest reaction, motivation, readiness to change, and confidence in sharing their knowledge about the MoC. In contrast, the more experienced staff were less reactive and expressed low confidence. This outcome also reflected in the responses to the question, “Which outcomes are MoC aiming to achieve?,” which intended to test the understanding not only for measuring whether or not the respondents knew the MoC's aims but by asking about each goal separately to ensure whether they understood these aims. The highest percentage who chose “All three aims” in response was the staff with more than 20 years of experience. However, the other agreement scale questions were subjective and dependent on staff judgment, and we found that respondents with 0-1 years of experience recorded the highest percentages across dimensions. In general, we always found that new workers were more motivated than the other workers due to many psychological reasons.
Several times, we found that the pharmacists had the highest agreement in all the dimensions regarding all agreement scale questions, which gave us the impression that they are generally the most knowledgeable. This finding may be due to their early involvement in the health system development process (e.g. the electronic prescriptions system Wasfaty that was implemented at PHCs, which supported them in their field as a job in applying the MoC).
But for questions intended to gauge understanding, asking about the MoC's aims showed us that the Leadership role had the highest understanding. We expected this result due to the leaders' position and responsibility to change. They play a direct role in the MoC's application. Meanwhile, the lowest percentage for all dimensions—in both the MoC aims questions and agreement scale questions—varied between Allied Health and Admin roles. We also expected this result because of the nature of these positions' work within institutes, especially for the Admin role.
Most MoC is related to primary care and family physicians. PHCs are the basis for applying the MoC. However, many PHCs have not yet been fully implemented; they will be implemented gradually, and soon. Accordingly, we found that PHCs had the highest knowledge of the MoC in most dimensions. This outcome explains the PHC staff's high level of knowledge in general toward the MoC.
Similarly, for the second system, when we looked at “Planned Care,” PHCs were the most knowledgeable because PHCs are the starting point of this system—their staff expressed high corresponding knowledge.
The other six SoCs in terms of knowledge, based on C1 facilities' findings are logical and reflect the current situation in our health system. For example, in the first system, “Keep Well,” we found that “other locations” were the most knowledgeable because most are practicing public health and preventive medicine, and the message of this system is the basis of their specialties.
While the percentage for the fifth system “Chronic Care” was high at King Salman Hospital, this result may have been due to diabetes and endocrine center at this location.
Finally, our study involved several limitations. Not all C1 staff participated. Some participants did not complete the questionnaire correctly, and the demographic data did not all available. Moreover, not all specialties at the C1 facilities participated. For example, the sample lacked the dentists' participation. Additionally, using an online survey can lead to biased data. Without using identity verification tools, knowing whether one person submitted multiple responses and was considered as a different participant is impossible.
Conclusion
Having assessed the C1 staff's knowledge through awareness, understanding, acceptance, and action regarding the Saudi MoC, we find that the C1 staff has good knowledge about the MoC in Saudi Arabia. We recommend conducting elaborate research in the future about the MoC to compare the understanding in detail with the other sectors to reach an international benchmark.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to acknowledge the Vision Realization Office (VRO) for supporting us with raw data. We would like to thank Dr. Fahad Aljasser for his assistance with earlier drafts of this research.
References
- 1.Agency for Clinical Innovation. A practical guide on how to develop a model of care at the Agency for Clinical Innovation [Version 1.0, May 2013] [[Last accessed on 2018 Nov 17]]. Available from: https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0009/181935/HS13-034_Framework-DevelopMoC_D7.pdf .
- 2.Walston S, Al-Harbi Y, Al-Omar B. The changing face of healthcare in Saudi Arabia. Ann Saudi Med. 2008;28:243–50. doi: 10.5144/0256-4947.2008.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saudi Arabian Ministry of Health. The Kingdom successfully make another Haj season. 2006. [[Last accessed on 2018 Nov 16]]. Available from: http://www.moh.gov.sa/ar/modules/news/print.php?storyid=383 .
- 4.General Authority for Statistics. Kingdom of Saudi Arabia. Haj 2019–1440. [[Last accessed on 2020 May 17]]. Available from: https://www. stats. gov. sa/sites/default/files/haj_40_ar.pdf .
- 5.Ministry of Health. MOH's Efforts during 1440H-Hajj Season. [[Last accessed on 2020 Aug 29]]. Available from: https://www.moh.gov.sa/en/Ministry/MediaCenter/News/Pages/News-2019-08-25-016.aspx .
- 6.Saudi Arabian Ministry of Health. Health statistic book for the year of 2005. [[Last accessed on 2018 Nov 16]]. Available from: http://www.moh.gov.sa/statistics/1425/index.html .
- 7.Mufti MH. Healthcare Development Strategies in the Kingdom of Saudi Arabia. Springer Science and Business Media. 2000 [Google Scholar]
- 8.Baranowski J. Health systems of the world – Saudi Arabia profiling a consultant's view of the health care system of Saudi Arabia. Glob Health. 2009;2:1–8. [Google Scholar]
- 9.Al-Hanawi MK. The healthcare system in Saudi Arabia: How can we best move forward with funding to protect equitable and accessible care for all? International Journal of Healthcare. 2017;3:78. [Google Scholar]
- 10.Kingdom of Saudi Arabia. Saudi Vision 2030. [[Last accessed on 2019 Dec 03]]. Available from: https://vision2030.gov.sa/en .
- 11.Ministry of Health. HSTP guide. [[Last accessed on 2018 Nov 16]]. Available from: https://www.moh.gov.sa/en/Ministry/vro/Pages/manual.aspx .
- 12.Kingdom of Saudi Arabia. Saudi Vision 2030. [[Last accessed on 2019 Dec 03]]. Available from: https://vision2030.gov.sa/sites/default/files/attachments/NTP%20English%20Public%20Document_2810.pdf .
- 13.Ministry of Health. MOH initiatives 2030. [[Last accessed on 2020 Jun 21]]. Available from: https://www.moh.gov.sa/en/Ministry/nehs/Pages/vision2030.aspx .
- 14.Ministry of Health. Institutional transformation program. [[Last accessed on 2019 Jan 17]]. Available from: https://www.moh.gov.sa/en/Ministry/Structure/Programs/Institutional-Transformation-Program/Pages/default.aspx .
- 15.Ministry of Health. [[Last accessed on 2019 Jan 17]]. Available from: https://www.moh.gov.sa/Ministry/MediaCenter/News/Pages/news-2018-05-05-001.aspx .
- 16.Ministry of Health. The health sector transformation plan guide [Version 4.0, February 2019] (available only in Arabic) [translated] [[Last accessed on 2019 Jan 22]]. Available from: https://www.moh.gov.sa/Ministry/MediaCenter/Publications/Documents/2019-01-15.pdf .
- 17.Healthcare Transformation Strategy Manual [Version 3.0] [[Last accessed on 2019 Jan 18]]. Available from: https://www.moh.gov.sa/en/Ministry/vro/Documents/Healthcare-Transformation-Strategy.pdf .
- 18.Ministry of Health. First emergency care model adopted in Kedi and al-Eskan centers. [[Last accessed on 2018 Nov 18]]. Available from: ht t p s : / /www.moh.gov.sa/en/Mini s t r y/MediaCenter/News/Pages/news-2018-03-18-003.aspx .
- 19.Millichamp T, Bakon S, Christensen M, Stock K, Howarth S. Implementation of a model of emergency care in an Australian hospital. Emerg Nurse. 2017;25:35–42. doi: 10.7748/en.2017.e1741. [DOI] [PubMed] [Google Scholar]
- 20.Davy C, Bleasel J, Liu H, Tchan M, Ponniah S, Brown A. Effectiveness of chronic care models: Opportunities for improving healthcare practice and health outcomes: A systematic review. BMC Health Serv Res. 2015;15:194. doi: 10.1186/s12913-015-0854-8. [DOI] [PMC free article] [PubMed] [Google Scholar]