Abstract
Background
We evaluated long‐term outcome of isolation of pulmonary veins, left atrial posterior wall, and superior vena cava, including time to recurrence and prevalent triggering foci at repeat ablation in patients with paroxysmal atrial fibrillation with or without cardiovascular comorbidities.
Methods and Results
A total of 1633 consecutive patients with paroxysmal atrial fibrillation that were arrhythmia‐free for 2 years following the index ablation were classified into: group 1 (without comorbidities); n=692 and group 2 (with comorbidities); n=941. We excluded patients with documented ablation of areas other than pulmonary veins, the left atrial posterior wall, and the superior vena cava at the index procedure. At 10 years after an average of 1.2 procedures, 215 (31%) and 480 (51%) patients had recurrence with median time to recurrence being 7.4 (interquartile interval [IQI] 4.3–8.5) and 5.6 (IQI 3.8–8.3) years in group 1 and 2, respectively. A total of 201 (93.5%) and 456 (95%) patients from group 1 and 2 underwent redo ablation; 147/201 and 414/456 received left atrial appendage and coronary sinus isolation and 54/201 and 42/456 had left atrial lines and flutter ablation. At 2 years after the redo, 134 (91.1%) and 391 (94.4%) patients from group 1 and 2 receiving left atrial appendage/coronary sinus isolation remained arrhythmia‐free whereas sinus rhythm was maintained in 4 (7.4%) and 3 (7.1%) patients in respective groups undergoing empirical lines and flutter ablation (P<0.001).
Conclusions
Very late recurrence of atrial fibrillation after successful isolation of pulmonary veins, regardless of the comorbidity profile, was majorly driven by non‐pulmonary vein triggers and ablation of these foci resulted in high success rate. However, presence of comorbidities was associated with significantly earlier recurrence.
Keywords: catheter ablation, late recurrence, left atrial appendage, paroxysmal atrial fibrillation, pulmonary vein isolation
Subject Categories: Atrial Fibrillation
Nonstandard Abbreviations and Acronyms
- IQI
interquartile intervals
- PAF
paroxysmal atrial fibrillation
Clinical Perspective
What Is New?
Despite permanent pulmonary vein isolation, patients with paroxysmal atrial fibrillation experienced very late recurrences that were mainly driven by non‐pulmonary vein triggers, especially from the left atrial appendage and coronary sinus.
The median time to recurrence was significantly shorter in patients with cardiovascular comorbidities.
What Are the Clinical Implications?
These findings will plausibly impact the risk‐stratification and decision‐making for ablation strategies in patients with paroxysmal atrial fibrillation experiencing very late arrhythmia recurrence.
Based on the findings by Haïssaguerre et al and others, pulmonary veins (PVs) have been recognized as the major source of arrhythmogenic activity involved in the initiation of atrial fibrillation (AF).1, 2 Consequently, isolation of the PVs (PVI) by radio‐frequency catheter ablation has been considered an effective therapeutic strategy, especially in drug‐refractory paroxysmal AF patients with benefits consistently demonstrated in multiple randomized trials.3 However, some patients experience late relapse of AF even in the presence of permanent electrical isolation of PVs4 and very late recurrence after successful PVI represent an understudied PAF population. Complex interplay between the triggering structures and a continuously evolving cardiac substrate has been speculated as the underlying mechanism of late AF recurrences.5 Yet, it is unclear what drives the arrhythmia‐recurrence in patients with persistent PV isolation.
Moreover, with the decrease in the incidence of PV reconnections in recent years, because of the advancement in the technique and technology of catheter ablation, electrophysiologists have started encountering increasing number of patients with late recurrences after initial long‐term success.5 Therefore, there is a pressing need to characterize the disease process that would enable the physicians to counsel their patients properly. In order to outline the course of the arrhythmia in the PAF patients, we followed them over a period of ≈15 years to evaluate the long‐term outcome after successful PVI+isolation of left atrial posterior wall and superior vena cava (SVC) including the time to recurrence, the prevalent triggering foci detected at redo and the procedure‐outcome of repeat ablations.
Methods
In this prospective observational study, consecutive PAF patients who received their first or first and second ablation procedure between 2004 and 2008 were screened for enrollment. The first ablation or the latest of the two procedures (for patients having 2 ablations) is described as the “index” procedure in the manuscript.
Inclusion Criteria
Patients were included in the study if (1) their index ablation consisted only of pulmonary vein isolation (PVI) plus isolation of the left atrial posterior wall and SVC,6, 7 and (2) they remained in sinus rhythm off‐antiarrhythmic drugs for at least 2 years following the index procedure. During these 2 years, standard institutional protocol was used for arrhythmia‐monitoring; event recorders for first 5 months followed by quarterly ECG and Holter‐monitoring for 1 year. In the second year, patients were followed up biannually.
Patients were included in group 1 if they had either no cardiovascular comorbidities or only hypertension that was well‐controlled by a single anti‐hypertensive agent.
All group 2 patients had ≥1 of the following comorbidities: (1) moderate to severe sleep apnea (apnea‐hypopnea index >15/h), (2) diabetes mellitus, (3) body mass index ≥30 kg/m2, (4) hypertension treated with multiple anti‐hypertensive agents, and (5) low left ventricular ejection fraction (<45%).
Exclusion Criteria
Patients were excluded (1) if they experienced recurrence off‐drugs within 2 years following the index procedure, and (2) if they received ablation of non‐PV sites other than the left atrial posterior wall and SVC, especially left atrial appendage (LAA) and coronary sinus (CS) during the first or the second procedure.
The current analysis reports the long‐term success rate of the index procedure, time to first recurrence after the index procedure, triggers detected and targeted at the redo and outcome of the redo procedures at 2 years follow‐up.
All patients provided written informed consent for the ablation procedure. The patient data was prospectively collected in the database approved by the Institutional Review Board or ethics committee. The de‐identified data supporting the findings of this study will be available from the corresponding author upon reasonable request.
Ablation Procedure
Our standard ablation procedure included PVI plus isolation of the left atrial posterior wall and SVC.4, 6, 7 All patients received the standard ablation at their index procedure. Posterior wall isolation was performed using multiple ablation points covering the whole posterior wall. SVC was mapped and isolated circumferentially in all patients. Briefly, the circular mapping catheter, guided by intracardiac echocardiography, was positioned at the SVC–right atrial junction, which is marked by the lower border of the pulmonary artery. Isolation of the SVC was then performed at that level.4
All anti‐arrhythmic drugs were discontinued 4 to 5 half‐lives before ablation whereas amiodarone was stopped at least 4 months before the procedure. Early in the practice, warfarin was discontinued before the procedure and patients were bridged with low molecular weight heparin. This anticoagulation strategy continued until 2005 when uninterrupted warfarin approach was adapted. Pulmonary vein antrum isolation was performed guided by circular mapping catheter and intracardiac echocardiography using 8‐mm non‐irrigated or 4‐mm cooled‐tip catheter and open irrigation was used for procedures after 2006. The electrical isolation of PV was extended to the posterior wall contained between the pulmonary veins. Complete abolition of all PV potentials rather than decrease in the amplitudes was the end point and confirmed by entrance and/or exit block.
With the 8‐mm‐tip catheter, radio frequency energy was set at 30 W and 55°C, and power was titrated upward every 5 seconds from 30 to 70 W while monitoring for microbubble formation. Each lesion typically lasted 30 to 50 seconds. A temperature probe was routinely placed in the esophagus. Radiofrequency applications were limited to 20 seconds at a single location over esophagus and immediately halted if the temperature reached 39°C or rapidly rose.
With the 4‐mm cooled‐tip catheter, radio frequency energy was delivered using an average power of 35±7 W to maintain a target temperature of 35 to 40°C; power was titrated down whenever microbubbles formed. Energy was delivered for 40 to 60 seconds at each site and no more than 20 seconds at LA sites close to the esophagus and was terminated automatically if there was a rise in impedance.
With the open‐irrigation catheter, initially a temperature of 45°C and maximum power of 50 W was used. However, after observation of high incidence of “steam pops” and pericardial effusion at higher power in a randomized trial, the maximum temperature and power were changed to 42°C and 45 W respectively.4
Repeat Procedure
The ablation strategy of the repeat procedure was heterogeneous, according to the performing operators' preference. In case of PV, PW, and SVC reconnection, these structures were re‐isolated. Additional ablation was performed following two main strategies:
Further ablation of non‐PV triggers, including ablation of significant triggers seen during the procedure along with empirical LAA and CS isolation if neither PV, PW, and SVC reconnection or additional non‐PV triggers were detected.6, 8 High‐dose isoproterenol challenge (up to 30 µg/min) was used to disclose non‐PV triggers which were targeted using additional radio frequency energy.
Targeted ablation of any presenting atrial tachycardia, OR empirical left‐sided ablation lines (roof, mitral isthmus) if the patient was in sinus rhythm.
Significant non‐PV triggers were defined as: focal atrial tachycardia (AT; sustained or non‐sustained), frequent premature atrial contractions (premature atrial contractions, ≥10/min), or premature atrial contractions triggering AF/atrial flutter. The procedural endpoint was their elimination, which included targeted ablation of non‐CS/LAA triggers, and CS or LAA isolations if triggers originated from these structures. The endpoint for CS and LAA isolation was electrical silence, as confirmed by entrance block.
Figure 1 shows the representative lesion sets during the index and repeat procedures.
Figure 1. Representative images showing lesion sets during the index and repeat procedures.
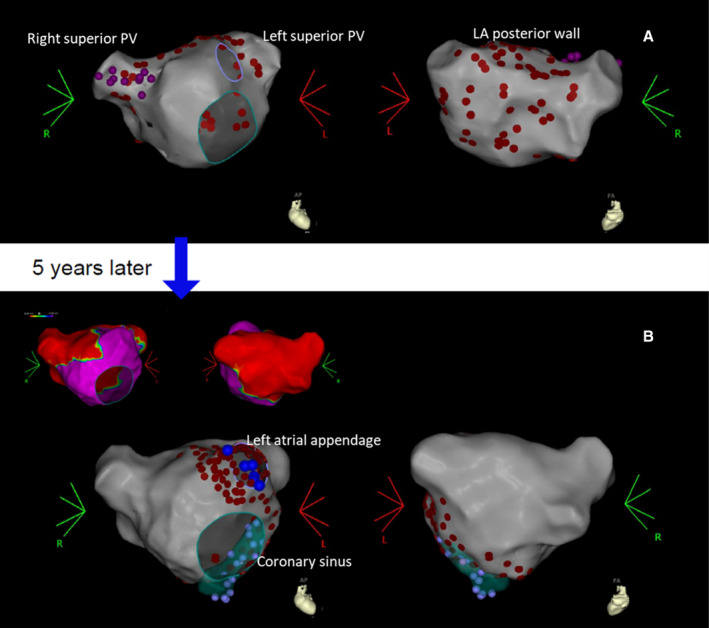
A, Index procedure included isolation of pulmonary veins (PVs), left atrial posterior wall (LAPW), and superior vena cava. B, The same patient underwent repeat procedure after 5 years, during which ablation was extended anteriorly and inferiorly to left atrial appendage and coronary sinus. The red areas in the voltage map shows electrically isolated PVs and LAPW from the index ablation.
The endpoint for atrial tachycardia ablation was its termination with documented bidirectional block in case of lines performed for a macro‐reentrant tachycardia.
Patients were discharged after an overnight stay on their previously ineffective antiarrhythmic drugs, with the exception of amiodarone, which was never restarted following the procedure.
Follow‐Up
Follow‐up was performed at 1, 3, 6, and 12 months with office visits, cardiology evaluation, 12‐lead electrocardiogram (ECG) and 7‐day Holter monitoring at 1, 6, and 12 months. Additionally, patients were provided with event‐recorders for the first 5 months following the procedure and were asked to transmit their rhythm every time they had symptoms compatible with arrhythmias and at least 3 to 4 times a week even if asymptomatic. After 1 year, patients were followed up annually with a 7‐day Holter and were asked to check their pulse regularly to monitor rate. Ablation success was defined as absence of arrhythmia off‐antiarrhythmic drugs.
Oral anticoagulant therapy was continued up to 6 months following the procedure, after which it was discontinued in all patients that remained arrhythmia‐free. If the patients underwent LAA isolation (at the repeat procedure), either they were kept on life‐long anticoagulation or LAA occlusion was performed irrespective of the CHA2DS2‐VASc score. TEE was performed at 6 months and 1 year in these patients to rule out thrombus formation in the appendage.
Statistical Analysis
This prospective observational study included consecutive patients who underwent the first or the first and the second ablation at our centers. Baseline clinical and demographic characteristics are presented using descriptive analysis methods. Continuous data are described as mean±standard deviation (median and interquartile intervals [IQI] for non‐normal data) and as counts and percent if categorical. Continuous data were compared using the independent sample t test and categorical data were compared using the Chi‐Square test.
The endpoints for the study included (1) time to recurrence after index procedure, (2) triggers identified at recurrence, (3) freedom from recurrence after the index procedure, and (4) freedom from recurrence after re‐ablation during the follow‐up. Freedom from arrhythmia at the long‐term follow‐up was assessed by Kaplan‐Meier curves. Success after repeat ablation was compared between the ablation strategies using log‐rank method. Event‐free duration was defined as time from the index procedure to arrhythmia recurrence and from re‐ablation to recurrence for repeat procedure. Patients remaining arrhythmia‐free at the end of 10 years of follow‐up were censored. Patients were censored on date of death or last contact, if they died or lost to follow‐up without documented recurrence. All tests were 2‐sided, and a P<0.05 was considered statistically significant. To identify the predictors of recurrence, univariable and multivariable analyses were performed using Cox proportional hazard model. In the multivariable analysis, all the variables with significant association with recurrence in univariable analysis were included; in addition, variables having clinical relevance (age, hypertension, dyslipidemia and coronary artery disease) with recurrence were also included. Statistical analyses were performed using IBM SPSS Statistics 22.0 (IBM SPSS Inc., Chicago, IL).
Results
A total of 1877 paroxysmal AF patients receiving their first or first and second ablations during the study period were screened and 1633 (87%) consecutive patients with paroxysmal AF meeting the eligibility criteria were included in the study.
These 1633 patients were arrhythmia‐free for 2 years after their first or second catheter ablation (index procedure) at our centers (Figure 2). Based on the presence or absence of comorbidities, they were classified into: group 1 (without comorbidities), 692 and group 2 (with comorbidities), 941. Baseline characteristics and procedural parameters (of the index ablation procedure) of the study population are presented in Table 1.
Figure 2. Study flow‐diagram showing ablation strategies and long‐term outcome.
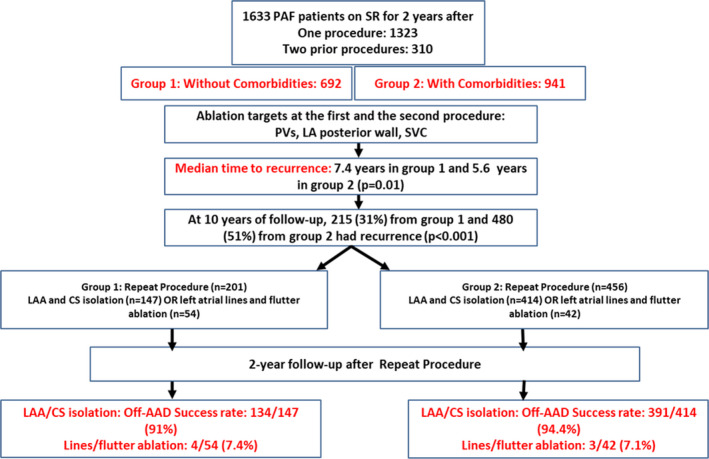
AAD indicates anti‐arrhythmic drug; CS, coronary sinus; LA, left atrial; LAA, left atrial appendage; PAF, paroxysmal atrial fibrillation; PV, pulmonary vein; SR, sinus rhythm; and SVC, superior vena cava.
Table 1.
Baseline Clinical Characteristics and Procedural Parameters of the Overall Study Population
| Variables |
Paroxysmal AF Patients Without Comorbidity (N=692) |
Paroxysmal AF Patients With Comorbidity (N=941) |
P Value |
|---|---|---|---|
| Demographics and clinical characteristics | |||
| Age | 57.4±9.9 | 63.3±9.8 | <0.001 |
| Male | 480 (69.4) | 617 (65.6) | 0.11 |
| Body mass index | 22.9±1.5 | 33.5±6.0 | <0.001 |
| Duration of AF, mo | 54.3±33.1 | 43.7±64.4 | <0.001 |
| Left atrial size, cm | 3.88±0.41 | 4.34±0.67 | <0.001 |
| Left ventricular ejection fraction, % | 61.2±7.0 | 57.3±10.8 | <0.001 |
| Dyslipidemia | 293 (42.3) | 473 (50.3) | 0.002 |
| Diabetes mellitus | 0 (0.0) | 344 (36.6) | <0.001 |
| Hypertension | 262 (37.9) | 831 (88.3) | <0.001 |
| Heart failure | 0 (0.0) | 183 (19.4) | <0.001 |
| History of transient ischemic attack or stroke | 9 (1.3) | 37 (3.9) | 0.001 |
| Coronary artery disease | 0 (0.0) | 184 (19.6) | <0.001 |
| Sleep apnea | 27 (3.9) | 185 (19.7) | <0.001 |
| Procedural parameters | |||
| Flouroscopy time | 30.1±21.1 | 39.21±19.43 | <0.001 |
| Radiofrequency time | 43.4±23.8 | 43.89±20.26 | 0.66 |
| Procedure time | 117.4±36.8 | 124.44±38.65 | <0.001 |
| Electrical cardioversion | 83 (12.0) | 118 (12.5) | 0.74 |
| Peri‐procedural medications | |||
| ACE inhibitors/angiotensin II receptor blockers | 131 (18.9) | 496 (52.7) | <0.001 |
| β‐blockers | 268 (38.7) | 640 (68.0) | <0.001 |
| Lipid lowering drugs | 291 (42.1) | 512 (54.4) | <0.001 |
| Aspirin | 81 (11.7) | 169 (18.0) | <0.001 |
ACE indicates angiotensin‐converting enzyme; AF, atrial fibrillation.
Of the 1633 patients, it was the first ablation for 1323 (81.1%) and second ablation for 310 (18.9%). For group 1, it was the first ablation for 578 (83.5%) patients and the second for 114 (16.5%) patients. For group 2, it was the first and second ablation for 745 (79.2%) and 196 (20.8%) patients, respectively.
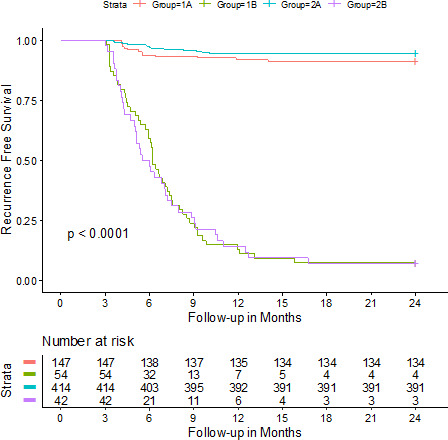
During the follow‐up after the index procedure, 215 of 692 (31.1%) patients from group 1 and 480 of 941 (51%) from group 2 experienced recurrence (P<0.001) (Figure 3).
Figure 3. Kaplan‐Meier curve showing recurrence‐free survival after the index procedure.
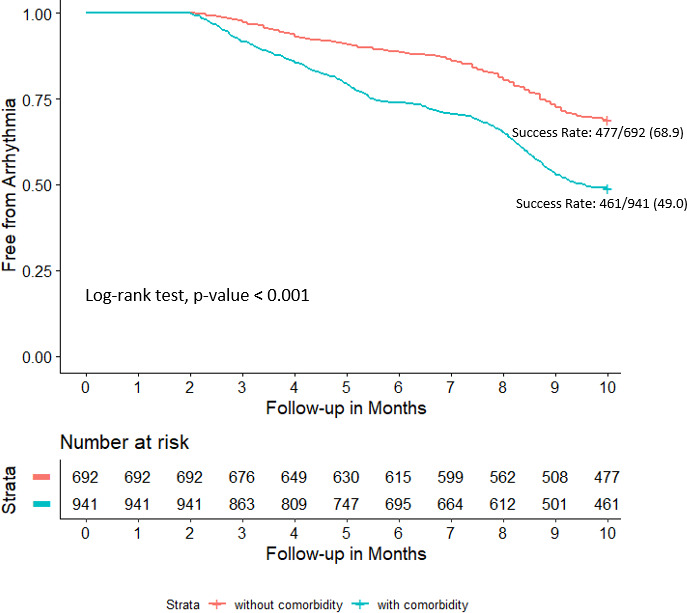
During the follow‐up after the index procedure, 215 of 692 (31.1%) patients from group 1 and 480 of 941 (51%) from group 2 experienced recurrence (P<0.001). Median time to recurrence was 7.4 (IQI 4.3–8.5) and 5.6 (IQI 3.8–8.3) years in group 1 and 2, respectively (P=0.01).
Among the patients who failed the index procedure, median time to recurrence was 7.4 (IQI 4.3–8.5) and 5.6 (IQI 3.8–8.3) years in group 1 and 2 respectively (P=0.01). In group 2, 205/480 (42.7%) recurrent patients had obesity plus OSA.
In the overall population, recurrence was reported in 450 of 1323 (34%) patients who received their first procedure, and 59 of the 310 (19%) patients with two earlier procedures (P=0.001).
During follow‐up, 164 patients in group 1 with no comorbidities at baseline developed new‐onset hypertension that was well‐controlled by a single anti‐hypertensive agent. Based on our inclusion criteria, they were still stratified as group 1. The recurrence rate in these 164 patients was similar to that of the remaining patients in group 1 (54/164 [33%] vs 161/528 [30.5%], P=0.75).
In group 2 (with ≥1 comorbidities at baseline), 7 patients reported new onset diabetes mellitus and 12 were diagnosed with moderate to severe sleep apnea. The recurrence rate in these 19 patients was comparable (9 of 19, 47.3%) with the rest of the group 2 population (471/922, 51%).
Univariable and multivariable analysis for predictors of recurrence are presented in Table 2. In the multivariable analysis age (HR 1.03, 95% CI 1.01–1.04, P<0.001) and female sex (HR 1.49, 95% CI 1.11–2.01, P=0.008) were predictors of recurrence in group 1 and age (HR 1.03, 95% CI 1.02–1.05, P<0.001) and obesity+ OSA (HR 1.32, 95% CI 1.10–1.58, P=0.003) were predictors of recurrence in group 2.
Table 2.
Univariable and Multivariable Analysis Showing Independent Predictors of Recurrence in Group 1 and 2 After Index Procedure
| Variable | Univariable Analysis | Multivariable Analysis | ||||
|---|---|---|---|---|---|---|
| Hazard Ratio | 95% CI | P Value | Hazard Ratio | 95% CI | P Value | |
| Group 1 | ||||||
| Age | 1.04 | 1.02–1.05 | <0.001 | 1.03 | 1.01–1.04 | <0.001 |
| Female | 1.88 | 1.44–2.47 | <0.001 | 1.49 | 1.11–2.01 | 0.008 |
| Hypertension | 0.99 | 0.75–1.31 | 0.96 | 0.98 | 0.75–1.30 | 0.91 |
| Dyslipidemia | 1.17 | 0.90–1.54 | 0.24 | 1.09 | 0.83–1.43 | 0.53 |
| Group 2 | ||||||
| Age | 1.03 | 1.02–1.04 | <0.001 | 1.03 | 1.02–1.04 | <0.001 |
| Female | 1.21 | 1.01–1.45 | 0.045 | 1.14 | 0.95–1.38 | 0.17 |
| BMI+OSA | 1.33 | 1.11–1.59 | 0.002 | 1.32 | 1.10–1.58 | 0.003 |
| Hypertension | 1.16 | 0.87–1.55 | 0.31 | 1.16 | 0.87–1.56 | 0.31 |
| Dyslipidemia | 0.96 | 0.80–1.15 | 0.65 | 0.94 | 0.78–1.13 | 0.49 |
| Coronary artery disease | 1.13 | 0.91–1.41 | 0.27 | 1.05 | 0.83–1.31 | 0.7 |
BMI indicates body mass index; OSA, obstructive sleep apnea.
Repeat Procedure
Repeat procedure was performed in 201/215 (93.5%) and 456/480 (95%) patients from group 1 and 2, respectively: LAA and CS isolation with detectable triggers in 106/201 (52.7%) and 378/456 (82.9%), empirical isolation of LAA/CS in 41/201 (20.4%) and 36/456 (7.9%), lines and flutter ablation in 54/201 (27%) and 42/456 (9.2%), and re‐isolation of PVs in 4/201 (2%) and 5/456 (1.3%) patients (Figures 4 and 5). PV reconnection was not noted in any of the patients with two prior procedures. SVC was found to be permanently isolated in 642 (97.7%) and no reconnection of posterior wall in 611 (93%) cases.
Figure 4. Bar diagram showing ablation targets at the repeat procedure.
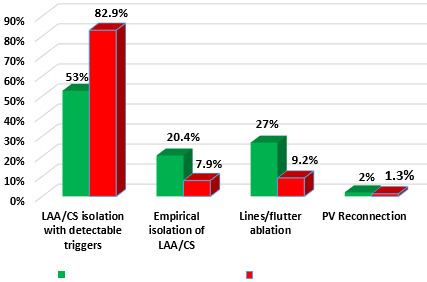
Repeat procedure was performed in 201/215 (93.5%) and 456/480 (95%) patients in group 1 and 2, respectively: LAA and CS isolation with detectable triggers in 106/201 (52.7%) and 378/456 (82.9%), empirical isolation of LAA/CS in 41/201 (20.4%) and 36/456 (7.9%), lines and flutter ablation in 54/201 (27%) and 42/456 (9.2%) and re‐isolation of PVs in 4/201 (2%) and 5/456 (1.3%) patients. CS indicates coronary sinus; LAA, left atrial appendage; and PV, pulmonary vein.
Figure 5. Kaplan‐Meier curve showing recurrence‐free survival after the repeat procedure.
At 2‐year follow‐up, in the LAA/CS isolation population, 134/147 (91.1%) patients from group 1 and 391/414 (94.4%) from group 2 remained arrhythmia‐free (log‐rank test, P‐value 0.19). Success rate in patients receiving lines and flutter ablation was 4/54 (7.4%) in group 1 and 3/42 (7.1%) in group 2 (0.86). Subgroup 1A and 2A received LAA/CS isolation. Subgroup 1B and 2B received lines and flutter ablation. CS indicates coronary sinus; and LAA, left atrial appendage.
In the 484 patients (group 1 [n=106] and 2 [n=378]) receiving non‐PV trigger ablation with detectable triggers, the following were the most common foci: interatrial septum: 87, 18%, LAA: 353, 73% and CS: 315, 65.1%. Foci from the interatrial septum were targeted for ablation in all 87 patients. LAA and CS were empirically isolated in 77 patients from both groups in whom PVs were permanently isolated and no extra‐PV triggers were detected on isoproterenol‐challenge.
At 2‐year follow‐up, in the LAA/CS isolation population, 134/147 (91.1%) patients from group 1 and 391/414 (94.4%) from group 2 remained arrhythmia‐free (log‐rank test, P‐value 0.19). Success rate in patients receiving lines and flutter ablation was 4/54 (7.4%) in group 1 and 3/42 (7.1%) in group 2 (0.86). Procedural complications:
No major procedural complications were observed after the repeat procedures. In total, there were 19 groin hematomas and 6 minor pericardial effusions that were managed conservatively.
At the end of the follow‐up, 6 (0.36%) thromboembolic events, 12 (0.7%) cases of cancer, and 15 (0.9%) deaths were reported. Causes of death were documented to be cancer and heart failure with asystole in 3 patients and “natural cause” in the remaining 12 patients.
No patients were lost to follow‐up. Some of the recurrences happened in patients that died later.
Discussion
The current study was designed to evaluate the disease course of the arrhythmia over a decade after successful index ablation procedure in paroxysmal AF patients with or without comorbidities such as diabetes mellitus, heart failure, obesity, and moderate to severe sleep apnea, which are known risk factors for abnormal cardiac substrate. The main objective of this study was to understand why arrhythmia relapses years after successful PV isolation in PAF patients and whether the presence or absence of comorbidities modulate the underlying mechanism of very late recurrences.
Our main findings were the following: (1) median time to recurrence after the index procedure was significantly shorter in patients with comorbidities, (2) PV reconnection was detected in a very small number of cases (≤2%) at redo, (3) LAA and CS triggers were highly prevalent in patients with late recurrences in both groups, and (4) more than 90% of patients remained arrhythmia‐free after electrical isolation of the LAA and CS.
Although PVs have been recognized as the primary source of triggers for the initiation of AF, emerging evidences question the role of PV triggers in late recurrences after initial long‐term success.9 Studies have not only shown similar PV reconnection rate in patients with and without recurrent arrhythmia but also maintenance of sinus rhythm in the presence of PV reconnection (detected at follow‐up electrophysiology study).9, 10, 11, 12 Moreover, in a recently published article, PV firing or presence of fibrillation within the PVs were reported to be not associated with ablation‐outcome.13
All of our patients underwent PVI plus isolation of PW and SVC before being included in the current study. At the repeat procedure during the 10‐year follow‐up period, PV reconnection was observed in a very small number of cases and none in patients with two procedures at baseline. Thus, regained electrical conduction in the PVs was not the underlying mechanism of recurrence in the majority of our study population.
In our experience and others', ablation strategies including isolation of left atrial posterior wall result in higher success rate compared to PV isolation alone.14, 15 Similarly, SVC has been demonstrated as a source of non‐PV triggers.16 The atrial myocardial sleeves extend into the SVC for up to 2 to 5 cm; thus harboring ectopic pacing cells that provide the substrate for atrial arrhythmia.17 Earlier trials in paroxysmal AF have demonstrated superior success rate following empirical SVC isolation during the first procedure.16, 18
In the current study, AF was recurrent despite permanent electrical isolation of PVs, PW, and SVC and ectopic beats driving the arrhythmia were detected to be originating from the extra‐PV sites such as the interatrial septum, LAA, and CS.
These results clearly indicate that at a later period in the course of this disease, beats originating from the non‐PV foci became the primary source of the arrhythmia‐initiating ectopic triggers. In fact, in an earlier study published by our group, similar findings were observed in the PAF patients having very late recurrence in the absence of PV and PW reconnection.4 However, there is a major difference between that study and the current analysis; here we examined the progression of cardiac arrhythmia in patients with versus without cardiovascular risk factors.
Relapse of AF being exclusively attributable to non‐PV triggers is of utmost importance as it proposes that the evolution of the disease does not halt during the years of arrhythmia‐free interval. Emerging evidences suggest that risk factors such as age, sex, genetic predisposition, left atrial size and comorbidities such as hypertension, obesity, sleep apnea, structural heart disease, and left ventricular dysfunction possibly contribute to progression of the rhythm disorder even after establishment of sinus rhythm by earlier procedures.4, 28 The impact of comorbidities would explain the prevalence of non‐PV triggers and the plausible underlying mechanism for significantly earlier recurrence in our group 2 patients. Earlier reports have shown the development and progression of atrial substrate to be independent of AF, either due to a primary fibrotic cardiomyopathy or modulators such as obesity and inflammation, or a combination of both.29 In agreement with this explanation, obesity+ OSA was observed to be an independent predictor of recurrence in our group 2 population.
However, high prevalence of non‐PV triggers was also observed in group 1 patients with no or minimal comorbidities, which indicates that regardless of the comorbidity status and subsequent substrate remodeling, triggers from non‐PV sites originate over years, causing very late relapse of the arrhythmia. It could be an ageing‐related phenomenon that happens plausibly in genetically predisposed individuals.
Ablation strategy was observed to be a very strong predictor of recurrence in our study population. A significantly low success rate was observed in our patients that received lines and flutter ablation at the repeat procedure compared to the cohort undergoing LAA and CS isolation. In two randomized trials, adjunctive linear ablation was shown to have no added advantage over PVI alone in terms of arrhythmia‐free survival in paroxysmal AF patients.30, 31 The most likely underlying mechanism of the recurrent tachyarrhythmia was reported to be reentry across linear lesion sets.32 Furthermore, in the randomized APPROVAL (Impact of Ablation Approaches on Outcome in Atrial Fibrillation and Flutter) trial, the success rate at 2‐year follow‐up after CTI‐only was very low (19%) in patients with coexistent AF and flutter.33 Even, in patients with isolated atrial flutter and no history of AF, CTI ablation alone had significantly lower success rate compared to CTI+PVI, proposing potential unmasking of underlying AF after elimination of atrial flutter.34
Contrary to the population with linear ablation, ablation‐outcome was significantly better when non‐PV triggers were ablated in the repeat procedure. This finding reinforces the crucial role of these triggers in the relapse of AF after a long arrhythmia‐free period in patients with permanently isolated PVs and demonstrates the importance of effective ablation of these ectopic foci to attain durable freedom from arrhythmia.
In this context, it is important to mention the high risk of stroke in patients with poor compliance to anticoagulant therapy or discontinuation of the same after effective LAA isolation, as shown by our group in a recent series of post‐LAAEI cases.35 LAA occlusion seems to be a reasonable choice for patients that are poor candidates for long‐term OAC therapy.
Limitations
In the current study, the follow‐up arrhythmia‐monitoring was discontinuous, which implies possible underestimation of recurrent events. However, all symptomatic episodes were captured and the probability of having asymptomatic arrhythmia in this population is very low as patients were highly symptomatic and were aware of their symptoms. Furthermore, we did not evaluate the ageing‐associated atrial substrate remodeling using voltage mapping or cardiac imaging that could have explained its potential role in the mechanism of late recurrence.
Conclusions
In our study population of paroxysmal AF patients, regardless of the comorbidity status, very late relapse of arrhythmia was observed in a sizeable number of cases despite persistent PV isolation, although median time to recurrence was significantly shorter in patients with comorbidities than those without. Furthermore, recurrent arrhythmia was almost entirely driven by non‐PV triggers as evidenced by substantial improvement in the success rate following ablation of those triggers.
Sources of Funding
None.
Disclosures
Dr Natale is a consultant for Boston Scientific, Biosense Webster, St. Jude/Abbott Medical, Biotronik, Baylis, and Medtronic. Dr Di Biase is a consultant for Biosense Webster, Boston Scientific, Stereotaxis, and St. Jude Medical. Dr Di Biase received speaker honoraria/travel support from Medtronic, Bristol Meyers Squibb, Pfizer, and Biotronik. Dr Burkhardt is a consultant for Biosense‐Webster and Stereotaxis. The remaining authors have no disclosures to report.
(J Am Heart Assoc. 2021;10:e020563. DOI: 10.1161/JAHA.120.020563.)
For Sources of Funding and Disclosures, see page 10.
References
- 1.Haïssaguerre M, Jaïs P, Shah DC, Takahashi A, Hocini M, Quiniou G, Garrigue S, Le Mouroux A, Le Métayer P, Clémenty J. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998;339:659–666. DOI: 10.1056/NEJM199809033391003. [DOI] [PubMed] [Google Scholar]
- 2.Ball J, Carrington MJ, McMurray JJ, Stewart S. Atrial fibrillation: profile and burden of an evolving epidemic in the 21st century. Int J Cardiol. 2013;167:1807–1824. DOI: 10.1016/j.ijcard.2012.12.093. [DOI] [PubMed] [Google Scholar]
- 3.Santangeli P, Marchlinski FE. Techniques for the provocation, localization, and ablation of non–pulmonary vein triggers for atrial fibrillation. Heart Rhythm. 2017;14:1087–1096. DOI: 10.1016/j.hrthm.2017.02.030. [DOI] [PubMed] [Google Scholar]
- 4.Gökoğlan Y, Mohanty S, Güneş MF, Trivedi C, Santangeli P, Gianni C, Asfour IK, Bai R, Burkhardt JD, Horton R, et al. Pulmonary vein antrum isolation in patients with paroxysmal atrial fibrillation: more than a decade of follow‐up. Circ Arrhythm Electrophysiol. 2016;9:e003660. DOI: 10.1161/CIRCEP.115.003660. [DOI] [PubMed] [Google Scholar]
- 5.Yamaguchi T, Marrouche NF. Recurrence post‐atrial fibrillation ablation: think outside the pulmonary veins. Circ Arrhythm Electrophysiol. 2018;11:e006379. DOI: 10.1161/CIRCEP.118.006379. [DOI] [PubMed] [Google Scholar]
- 6.Mohanty S, Trivedi C, Gianni C, Della Rocca DG, Morris EH, Burkhardt JD, Sanchez JE, Horton R, Gallinghouse GJ, Hongo R, et al. Procedural findings and ablation outcome in patients with atrial fibrillation referred after two or more failed catheter ablations. J Cardiovasc Electrophysiol. 2017;28:1379–1386. DOI: 10.1111/jce.13329. [DOI] [PubMed] [Google Scholar]
- 7.January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, et al.; ACC/AHA Task Force Members . 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130:2071–2104. DOI: 10.1161/CIR.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 8.Di Biase L, Burkhardt JD, Mohanty P, Mohanty S, Sanchez JE, Trivedi C, Güneş M, Gökoğlan Y, Gianni C, Horton RP, et al. Left atrial appendage isolation in patients with longstanding persistent AF undergoing catheter ablation: BELIEF trial. J Am Coll Cardiol. 2016;68:1929–1940. [DOI] [PubMed] [Google Scholar]
- 9.Usui E, Miyazaki S, Taniguchi H, Ichihara N, Kanaji Y, Takagi T, Iwasawa J, Kuroi A, Nakamura H, Hachiya H, et al. Recurrence after "long‐term success" in catheter ablation of paroxysmal atrial fibrillation. Heart Rhythm. 2015;12:893–898. DOI: 10.1016/j.hrthm.2015.01.043. [DOI] [PubMed] [Google Scholar]
- 10.Jiang R‐H, Po SS, Tung R, Liu Q, Sheng X, Zhang Z‐W, Sun Y‐X, Yu LU, Zhang P, Fu G‐S, et al. Incidence of pulmonary vein conduction recovery in patients without clinical recurrence after ablation of paroxysmal atrial fibrillation: mechanistic implications. Heart Rhythm. 2014;11:969–976. DOI: 10.1016/j.hrthm.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 11.Farrell M, Yoneda Z, Montgomery J, Crawford D, Wray LL, Xu M, Kolek MJ, Richardson T, Lugo R, Metawee M, et al. Non‐pulmonary vein mediated atrial fibrillation: a novel sub‐phenotype. PLoS One. 2017;12:e0184354. DOI: 10.1371/journal.pone.0184354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nery PB, Belliveau D, Nair GM, Bernick J, Redpath CJ, Szczotka A, Sadek MM, Green MS, Wells G, Birnie DH. Relationship between pulmonary vein reconnection and atrial fibrillation recurrence: a systematic review and meta‐analysis. JACC Clin Electrophysiol. 2016;2:474–483. DOI: 10.1016/j.jacep.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 13.Prabhu S, Kalla M, Peck KY, Voskoboinik A, McLellan AJA, Pathik B, Nalliah CJ, Wong GR, Sugumar H, Azzopardi SM, et al. Pulmonary vein activity does not predict the outcome of catheter ablation for persistent atrial fibrillation: a long‐term multicenter prospective study. Heart Rhythm. 2018;15:980–986. DOI: 10.1016/j.hrthm.2018.02.029. [DOI] [PubMed] [Google Scholar]
- 14.Bai R, Di Biase L, Mohanty P, Trivedi C, Dello Russo A, Themistoclakis S, Casella M, Santarelli P, Fassini G, Santangeli P, et al. Proven isolation of the pulmonary vein antrum with or without left atrial posterior wall isolation in patients with persistent atrial fibrillation. Heart Rhythm. 2016;13:132–140. DOI: 10.1016/j.hrthm.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 15.Ouyang F, Bänsch D, Ernst S, Schaumann A, Hachiya H, Chen M, Chun J, Falk P, Khanedani A, Antz M, et al. Complete isolation of left atrium surrounding the pulmonary veins: new insights from the double‐Lasso technique in paroxysmal atrial fibrillation. Circulation. 2004;110:2090–2096. DOI: 10.1161/01.CIR.0000144459.37455.EE. [DOI] [PubMed] [Google Scholar]
- 16.Ejima K, Kato K, Iwanami Y, Henmi R, Yagishita D, Manaka T, Fukushima K, Arai K, Ashihara K, Shoda M, et al. Impact of an empiric isolation of the superior vena cava in addition to circumferential pulmonary vein isolation on the outcome of paroxysmal atrial fibrillation ablation. Am J Cardiol. 2015;116:1711–1716. DOI: 10.1016/j.amjcard.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 17.Jalife J, Kaur K. Atrial remodeling, fibrosis, and atrial fibrillation. Trends Cardiovasc Med. 2015;25:475–484. DOI: 10.1016/j.tcm.2014.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsai CF, Tai CT, Hsieh MH, Lin WS, Yu WC, Ueng KC, Ding YA, Chang MS, Chen SA. Initiation of atrial fibrillation by ectopic beats originating from the superior vena cava: electrophysiological characteristics and results of radiofrequency ablation. Circulation. 2000;102:67–74. DOI: 10.1161/01.CIR.102.1.67. [DOI] [PubMed] [Google Scholar]
- 19.Sotomi Y, Inoue K, Tanaka K, Toyoshima Y, Oka T, Tanaka N, Nozato Y, Orihara Y, Koyama Y, Iwakura K, et al. Persistent left atrial remodeling after catheter ablation for non‐paroxysmal atrial fibrillation is associated with very late recurrence. J Cardiol. 2015;66:370–376. DOI: 10.1016/j.jjcc.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 20.Parwani AS, Morris DA, Blaschke F, Huemer M, Pieske B, Haverkamp W, Boldt LH. Left atrial strain predicts recurrence of atrial arrhythmias after catheter ablation of persistent atrial fibrillation. Open Heart. 2017;4:e000572. DOI: 10.1136/openhrt-2016-000572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De Maat GE, Mulder BA, Berretty WL, Al‐Jazairi MIH, Tan ES, Wiesfeld ACP, Mariani MA, Van Gelder IC, Rienstra M, Blaauw Y. Obesity is associated with impaired long‐term success of pulmonary vein isolation: a plea for risk factor management before ablation. Open Heart. 2018;5:e000771. DOI: 10.1136/openhrt-2017-000771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pathak RK, Middeldorp ME, Lau DH, Mehta AB, Mahajan R, Twomey D, Alasady M, Hanley L, Antic NA, McEvoy RD, et al. Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation: the ARREST‐AF cohort study. J Am Coll Cardiol. 2014;64:2222–2231. DOI: 10.1016/j.jacc.2014.09.028. [DOI] [PubMed] [Google Scholar]
- 23.Anter E, Di Biase L, Contreras‐Valdes FM, Gianni C, Mohanty S, Tschabrunn CM, Viles‐Gonzalez JF, Leshem E, Buxton AE, Kulbak G, et al. Atrial substrate and triggers of paroxysmal atrial fibrillation in patients with obstructive sleep apnea. Circ Arrhythm Electrophysiol. 2017;10:e005407. DOI: 10.1161/CIRCEP.117.005407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoyer FF, Lickfett LM, Mittmann‐Braun E, Ruland C, Kreuz J, Pabst S, Schrickel J, Juergens U, Tasci S, Nickenig G, et al. High prevalence of obstructive sleep apnea in patients with resistant paroxysmal atrial fibrillation after pulmonary vein isolation. J Interv Card Electrophysiol. 2010;29:37–41. DOI: 10.1007/s10840-010-9502-8. [DOI] [PubMed] [Google Scholar]
- 25.Santoro F, Di Biase L, Trivedi C, Burkhardt JD, Paoletti Perini A, Sanchez J, Horton R, Mohanty P, Mohanty S, Bai R, et al. Impact of uncontrolled hypertension on atrial fibrillation ablation outcome. JACC Clin Electrophysiol. 2015;1:164–173. DOI: 10.1016/j.jacep.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 26.Santangeli P, Di Biase L, Themistoclakis S, Raviele A, Schweikert RA, Lakkireddy D, Mohanty P, Bai R, Mohanty S, Pump A, et al. Catheter ablation of atrial fibrillation in hypertrophic cardiomyopathy: long‐term outcomes and mechanisms of arrhythmia recurrence. Circ Arrhythm Electrophysiol. 2013;6:1089–1094. DOI: 10.1161/CIRCEP.113.000339. [DOI] [PubMed] [Google Scholar]
- 27.Lu Z‐H, Liu N, Bai R, Yao Y, Li S‐N, Yu R‐H, Sang C‐H, Tang R‐B, Long D‐Y, Du X, et al. HbA1c levels as predictors of ablation outcome in type 2 diabetes mellitus and paroxysmal atrial fibrillation. Herz. 2015;40(suppl 2):130–136. DOI: 10.1007/s00059-014-4154-6. [DOI] [PubMed] [Google Scholar]
- 28.Onishi N, Kaitani K, Amano M, Imamura S, Sakamoto J, Tamaki Y, Enomoto S, Miyake M, Tamura T, Kondo H, et al. Relationship between left ventricular diastolic dysfunction and very late recurrences after multiple procedures for atrial fibrillation ablation. Heart Vessels. 2018;33:41–48. DOI: 10.1007/s00380-017-1027-y. [DOI] [PubMed] [Google Scholar]
- 29.Guichard JB, Nattel S. Atrial cardiomyopathy: a useful notion in cardiac disease management or a passing fad? J Am Coll Cardiol. 2017;70:756–765. DOI: 10.1016/j.jacc.2017.06.033. [DOI] [PubMed] [Google Scholar]
- 30.Yu HT, Shim J, Park J, Kim IS, Kim TH, Uhm JS, Joung B, Lee MH, Kim YH, Pak HN. Pulmonary vein isolation alone versus additional linear ablation in patients with persistent atrial fibrillation converted to paroxysmal type with antiarrhythmic drug therapy: a multicenter, prospective, randomized study. Circ Arrhythm Electrophysiol. 2017;10:e004915. DOI: 10.1161/CIRCEP.116.004915. [DOI] [PubMed] [Google Scholar]
- 31.Arbelo E, Guiu E, Ramos P, Bisbal F, Borras R, Andreu D, Tolosana JM, Berruezo A, Brugada J, Mont L. Benefit of left atrial roof linear ablation in paroxysmal atrial fibrillation: a prospective, randomized study. J Am Heart Assoc. 2014;3:e000877. DOI: 10.1161/JAHA.114.000877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dixit S, Liang JJ, Pathak RK. Modifying arrhythmia behavior preablation with drug therapy may improve single procedure efficacy of a limited ablation strategy in patients with persistent atrial fibrillation. Circ Arrhythm Electrophysiol. 2017;10:e005379. DOI: 10.1161/CIRCEP.117.005379. [DOI] [PubMed] [Google Scholar]
- 33.Mohanty S, Mohanty P, Di Biase L, Bai R, Santangeli P, Casella M, Russo AD, Tondo C, Themistoclakis S, Raviele A, et al. Results from a single‐blind, randomized study comparing the impact of different ablation approaches on long‐term procedure outcome in coexistent atrial fibrillation and flutter (APPROVAL). Circulation. 2013;127:1853–1860. DOI: 10.1161/CIRCULATIONAHA.113.001855. [DOI] [PubMed] [Google Scholar]
- 34.Mohanty S, Natale A, Mohanty P, Di Biase L, Trivedi C, Santangeli P, Bai R, Burkhardt JD, Gallinghouse GJ, Horton R, et al. Pulmonary vein isolation to reduce future risk of atrial fibrillation in patients undergoing typical flutter ablation: results from a randomized pilot study (REDUCE AF). J Cardiovasc Electrophysiol. 2015;26:819–825. DOI: 10.1111/jce.12688. [DOI] [PubMed] [Google Scholar]
- 35.Di Biase L, Mohanty S, Trivedi C, Romero J, Natale V, Briceno D, Gadiyaram V, Couts L, Gianni C, Al‐Ahmad A, et al. Stroke risk in patients with atrial fibrillation undergoing electrical isolation of the left atrial appendage. J Am Coll Cardiol. 2019;74:1019–1028. DOI: 10.1016/j.jacc.2019.06.045. [DOI] [PubMed] [Google Scholar]


