INTRODUCTION
Over the last few decades, structural and regulatory changes have influenced US health care and caused a marked increase in the need for innovation. For example, the growing rate of chronically ill Americans has caused hospitals to consider new ways of utilizing limited resources, and the increasingly active role of patients in their own care has placed demands on designing novel delivery models. The push toward healthcare innovation has resulted in billions of dollars spent on R&D efforts by the private and public sectors. Yet, despite these efforts toward innovation, US healthcare costs have escalated to levels over twice the average of other developed countries (Anderson et al., 2019) and medical errors are now the third leading cause of death among Americans (Makary and Daniel, 2016). Consequently, in recent years, calls to expand the capacity for innovation in healthcare organizations through teams of interdisciplinary professionals have increased (Bindman et al., 2018). Prior research has affirmed the importance of interdisciplinary teams in implementing innovations that improve organizational performance by addressing complex system issues especially inherent to healthcare organizations (Grooms et al., 2017; Reiter-Palmon et al., 2018; Shea et al., 2018).
Notwithstanding their potential for benefit, the diversity in perspectives and expertise of interdisciplinary teams, especially when they tackle multi-level system challenges, make such teams more prone to experience barriers to progress (Milliken and Martins, 1996). Interdisciplinary teams involved in healthcare innovation or improvement projects, as compared to interdisciplinary teams engaged in care delivery, are likely to experience more barriers from within the organization as they develop novel, divergent ideas and attempt to integrate systemic changes into existing operations (e.g., Barry et al., 1999). Teams may employ boundary spanning roles and influence tactics to manage challenges arising from the organizational context in which teams operate. However, little is known about organizational obstacles such teams encounter and the skills required to design, implement, scale, and sustain innovations, despite challenges (Van de Ven, 2017). The aim of our research is to examine how interdisciplinary teams developing healthcare innovations manage challenges that may arise from within their organizational context.
New Contribution
Healthcare organizations can impose challenges on the effectiveness of interdisciplinary innovation teams operating within them. More research is needed to understand how innovation teams embedded in healthcare organizations experience and respond to challenges arising from their context as they attempt to make progress (Langley et al., 2019). Our study contributes to this lacuna of research by illustrating: (1) how conditions in the organizational context, or constraints, can impede team progress at various stages of innovation, and (2) the collective efforts, or tactics, teams use to manage or work around these constraints to further progress on their innovations. Through observations over three years, we demonstrate the range of constraints and tactics that can emerge during different stages of innovation. We focus on interdisciplinary teams organized to develop innovations such as quality improvement projects, rather than interdisciplinary clinical teams delivering health care, since our understanding of how such teams experience and manage organizational constraints is more limited (Schot et al., 2019). Our findings provide practical insights for innovation teams operating in health systems in their efforts to deal with organizational change, potential external conflicts, and implementation of innovations across organizational levels. Through this research, we highlight the need for interdisciplinary teams to be attuned to constraints early and often as they attempt to innovate, and to be ready with an arsenal of tactics, including preemptive measures, to address such challenges as they arise.
THEORETICAL FRAMEWORK
As healthcare organizations face more task complexity, constant change, and a flattening of organizational structure, innovation teams must increasingly coordinate boundaries and engage in relationships outside the team (Marrone, 2010). An external focus for healthcare innovation teams is key, since such teams are highly interdependent with their organizational context (Choi, 2002). Specifically, team progress depends on teams’ awareness of the pressures and difficulties the organization imposes on its efforts (Schippers et al., 2015). For example, as teamwork unfolds within a time-bounded project, teams will experience some interdependence with their organizational context; specifically, teams may depend on the organization for resources to achieve their objectives and organizations may depend on teams for innovative efficiency improvements. Organizational leaders and peer groups, through both action and inaction, can impact the innovation efforts of teams. This can require revision of interdepartmental relations and coordination activities to manage interdependencies (Adler, 1995). Consequently, what teams do to manage interdependencies is not constant; rather, emergent interdependencies require repeated adjustment. Compared to other types of organizations, the interdependencies are often more pronounced in healthcare organizations, like hospital systems, where social structures induce occupational boundaries that can challenge how information, resources, and knowledge are shared (Currie and White, 2012). Further, occupational subcultures in healthcare organizations can create silos across individuals and units, calling for strategies that bridge gaps (Burt, 2000). Interdisciplinary teams in healthcare organizations must address these aspects of the organizational context in order to succeed in their innovation efforts.
To address the organizational context in team activities, team members communicate with outside stakeholders through a practice called boundary spanning (Edmondson and Harvey, 2018; Johnson and Chang, 2000). Team boundary spanning includes a plethora activities through which teams actively engage and manage their organizational context to make progress in their work (Marrone et al., 2007). Team engagement of expertise and knowledge dispersed across the organization can be critical for propelling the innovation process forward (Orlikowski, 2002). Traditionally in the context of innovation, boundary spanning activities involve transferring technical information between the intra- and extra-team settings (Aldrich and Herker, 1977; Allen, 1984). Boundary spanning involves connecting to individuals external to the team, across organizational levels and types of expertise, often to secure needed resources and support for team progress (Ancona, 1990; Ancona and Caldwell, 1992). Teams engage in boundary spanning activities primarily through three modes: coordination of task performance, general information search, and activities used to persuade others and influence behavior (Marrone, 2010).
Boundary spanners attempt to employ influence tactics, which are methods of social persuasion to influence key leaders and stakeholders who may be resistant to certain ideas or innovations (Dutton and Ashford, 1993). For example, a person can use his or her position in the organization to communicate facts and statistics that can persuade others to move past political challenges (Anderson et al., 2008). Influence tactics can include practices such as rational appeals and exchanging resources, and their use depends on a given situation or context (Yukl and Falbe, 1990). Unlike using one’s power to persuade others, influence tactics are more subtle and less reliable (Fernandez and Vecchio, 1997). Influence tactics can be directed upward (e.g., leadership of higher rank), downward (e.g., frontline staff of lower rank), or laterally (e.g., across units and peer groups of similar rank, during an innovation’s initial implementation and scaling) (Yukl and Falbe, 1990). In recent decades, as healthcare organizations have moved toward “flatter” structures, it is critical to expand our understanding of how influence tactics are directed upward and laterally (Cohen and Bradford, 2005; Steizel and Rimbau-Gilabert, 2013).
While a substantial literature describes antecedents of boundary spanning practices, less is known about how and for what purposes teams engage in boundary spanning activities during their innovation journeys (Dey, 2017). In particular, research is limited in two prominent areas: the contextual conditions that impact the relationship between organizations and the way teams make progress on their innovations; and the tools that are instrumental to facilitating boundary spanning activities in the face of constraints arising from the team’s organizational context (Langley et al., 2019). Our research examines mechanisms by which the organizational context could constrain interdisciplinary teams’ innovation efforts and how the teams can overcome such constraints to achieve team objectives.
METHODS
Data Collection
We conducted fieldwork from October 2015 through October 2018, engaging as participant-observers in four interdisciplinary teams, each comprised of health system staff (e.g., physicians, nurses, pharmacists, case managers), engineers, and patient partners. Teams included five to 10 members and were formed as part of a program to redesign, implement, scale, and sustain healthcare delivery processes within their respective systems. This program aimed to improve quality at critical junctures between primary and specialty care, by directing teams through innovation cycles that utilized systems engineering principles to generate novel solutions or improve existing processes and then to implement, scale, and sustain them. The program provided cross-team learning sessions tri-annually that taught a common approach to innovation drawing on system engineering principles; between sessions, teams met weekly or more frequently to advance project aims. During our observation period, the teams experienced various demands from organizational decision-makers and units in their health system; the saliency of these demands made our context especially useful in observing team practices to manage organizational-level challenges.
All four study sites (Sites A, B, C, and D) were large, metropolitan health systems. Each site’s team selected its own focus for its innovation project. Site A’s team focus was improvement of the process for initiation and follow-up for specialty referrals. Site B’s team focused on improving processes related to perioperative care in the case of spinal fusion for children with medical complexity. Site C’s team focus was improvement of safe prescribing processes for patients with chronic pain who use opioids. Lastly, Site D’s team focus was improving the transition process from hospital to homecare for patients with medical complexity. As observers, we participated variably, e.g., by sharing lists of decisions taken at team meetings, providing feedback on teams’ data collection instruments, or offering process recommendations (Schein, 1995).
We used a mixed-qualitative methods approach to develop an empirically-derived model of teams’ experience managing constraints. Our data consisted of (1) participant observation; (2) semi-structured interviews; (3) focus groups; and (4) archival documents. First, we conducted approximately 190 hours of participant observation. We primarily observed team interactions at 60-minute, weekly or biweekly meetings. At these meetings, we collected detailed field notes aiming to produce thick descriptions; after observations, we produced running notes and memos to guide iterative data analysis. We also attended project-related meetings of team members and outside stakeholders (e.g., weekly meetings between anesthesiologists and team clinicians at Site B, half-day all team learning sessions every four months). For all sites, observation focused on understanding the organizational context in which teams operated, influence of organizational context on teams’ progress and learning, and practices teams used to address constraints arising from the organizational context.
Additionally, we conducted 18 interviews with members of the four interdisciplinary teams after 18-months of participant observation (5 physicians, 5 health system staff members, 4 engineers, 3 patient partners, and 1 managerial staff member). At this point in their projects, team members had experienced various challenges to team progress and worked to overcome them, allowing them to reflect meaningfully on these experiences. Interviews lasted 30-60 minutes and followed a semi-structured guide, based on emergent themes from our first round of coding. Subsequent to the interviews, we facilitated separate, hour-long semi-structured focus groups with each team to gain further insight as teams collectively discussed their challenges. Last, we used archival documents produced by each team in our data collection. Specifically, we used reports that teams completed throughout the study, which were designed to document progress of the overall program every four months. These reports encouraged teams to take stock of their progress-to-date, reflect on performance, and plan next steps. These reflection reports served as our primary source of information on team milestones (Shah and Corley, 2006).
Analytical Approach
We conducted data collection and analysis through an inductive and iterative process to refine theoretical findings (Glaser and Strauss 1967). In particular, we examined field notes and interview and focus group transcripts through multiple rounds of coding, accompanied by continual review of the literature. Analysis was performed through NVivo 11 software in three rounds of coding approximately 500 pages of participant observation notes, 18 interview transcripts, and four focus group transcripts. In the third round of coding, no new themes emerged and we had compiled copious examples of emergent themes, suggesting we approached theoretical saturation (Bowen, 2008).
We used field notes compiled in the first 18 months of each team’s innovation cycle as the basis of ongoing, informal running notes and more formalized memos. Both types of documents noted the external constraints experienced by the four teams and tactics teams used in response. We conducted the first round of coding midway through data collection using NVivo software. The first author and a research assistant separately used an open coding approach to code the same 13 field notes (Strauss and Corbin, 1994) to generate initial first-order empirical themes. Codes captured concepts related to both the organizational context in which teams operated and instances of team tactics. We compared the coding done by the research team to ascertain inter-rater reliability and found it to be acceptable (average Kappa coefficient of 0.70) (Cohen, 1960).
Following several iterations of extracting first-order themes, collecting more observational and interview data, and memo-writing, we aggregated first-order themes related to team tactics into higher-level, second-order conceptual categories, which distinguish tactics according to their purpose, i.e., whether primarily used to manage hierarchical or heterarchical constraints. For example, the second order theme tactics to manage heterarchical constraints, which include two first order codes, including empathic listening and information gathering. Open codes captured examples supporting each tactic. For instance, one example of the empathic listening tactic is sensemaking via personal anecdotes, such as when team members shared stories to describe organizational silos and develop shared understanding. Empathic listening and information gathering tactics enabled scaling by increasing the innovation’s relevance to others in the organization who would ultimately adopt the innovation. Throughout our analysis, both authors reviewed codes for fidelity to teams’ experience and conceptual clarity.
Finally, we used information gathered from focus groups for each team to help refine the major themes and our emergent framework, we revisited all available data and conducted selective coding, allowing us to reevaluate and challenge prior assumptions about the primary constraints faced by the teams and more closely examine team tactics (Strauss and Corbin, 1990). We compiled all relevant codes representing constraints and tactics and then compared the constraints teams experienced and team activities used to address them. This allowed us to recognize patterns in which tactics teams more often deployed to address different constraints and how the constraint impacted progress at various stages of the innovation process.
Analysis of Team Progress Milestones
Since each of the four teams had a different aim for its innovation project, we focused on collecting information about the number of milestones we could log and quantify over the course of the teams’ efforts. Examining milestones that each of the teams accomplished during our study provided a basis for understanding whether teams were able to maintain progress despite the constraints they experienced. We derived milestones from the reports regularly prepared by the teams to record their progress, and identified five types of milestones: (1) patient engagement; (2) leadership engagement; (3) health system engagement (i.e., health system staff outside of the immediate project team); (4) tangible output from activities; and (5) process redesign tools and implementation. We used the milestones to gauge the progress of activities undertaken by the teams and were not intended to be absolute markers of performance, which were unavailable during our study period. Instances of a specified milestone counted toward the total number of milestones for each team.
Patient engagement.
An explicit program goal, we defined patient engagement as instances in which team activities included patients, members of the population of interest for the team (Domecq et al., 2014). For example, establishing an ongoing partnership with a patient stakeholder (e.g., continued involvement of a patient at team meetings) counted as a milestone.
Leadership engagement.
We defined leadership engagement as instances in which a team established an ongoing partnership with health system executive leaders (e.g., Site D regularly attended manager-led work group meetings to establish manager buy-in for the team’s project).
Health system engagement.
We defined health system engagement as instances in which teams established ongoing partnerships with other health system staff, outside the core team (e.g., Site B established monthly meetings with other departments to collaborate on teamwork).
Tangible output from activities.
Tangible output emerged from team efforts and included instances of artifacts associated with use of systems engineering tools (e.g., Site A developed a swim lane diagram to show the current process of “close the loop” referrals), as well as scientific dissemination of team efforts (e.g., journal publications).
Redesign tool development and implementation.
We defined process redesign tool as any instrument produced as part of redesign activities or any instance of successful process redesign implementation (e.g., Site D developed a shared care plan to facilitate discharge from hospital to homecare for high risk patients).
FINDINGS
Table 1 shows milestones accomplished by each team and the duration of the teams’ involvement at our study’s conclusion. The milestones documented, though variable across teams, show that each team moved through their innovation cycles and maintained activity throughout our study, with the exception of Site A. Team progress was facilitated by what we describe as a constraint management process (CMP), displayed in Figure 1, which shows how two types of organizational constraints, heterarchical and hierarchical, repeatedly surfaced across the four teams to varying degrees and throughout the innovation cycle that primarily involved the following stages: (1) designing and implementing, (2) scaling, and (3) sustaining.
TABLE 1.
Team characterization of constraints, common tactics, and milestones of progress.
| Site | Hierarchical constraint |
Heterarchical constraint |
Team milestones (count) | Observation period |
|---|---|---|---|---|
| A | +++ | + |
Total: 12 Patient engagement: 1 Leadership engagement: 0 Health system engagement: 1 Tangible output from activities: 8 Process redesign tools and implementation: 2 |
October 2015 – September 2017 |
| B | + | ++ |
Total: 30 Patient engagement: 2 Leadership engagement: 0 Health system engagement: 4 Tangible output from activities: 15 Process redesign tools and implementation: 9 |
October 2015 – October 2018 |
| C | ++ | ++ |
Total: 23 Patient engagement:2 Leadership engagement: 0 Health system engagement:2 Tangible output from activities: 9 Process redesign tools and implementation: 10 |
October 2015 – October 2018 |
| D | ++ | + |
Total: 16 Patient engagement: 2 Leadership engagement: 1 Health system engagement: 1 Tangible output from activities: 8 Process redesign tools and implementation: 4 |
October 2016 – October 2018 |
+++ insurmountable, ++ intense and long-lasting, + intense but short-lived
FIGURE 1. Constraint management process model.
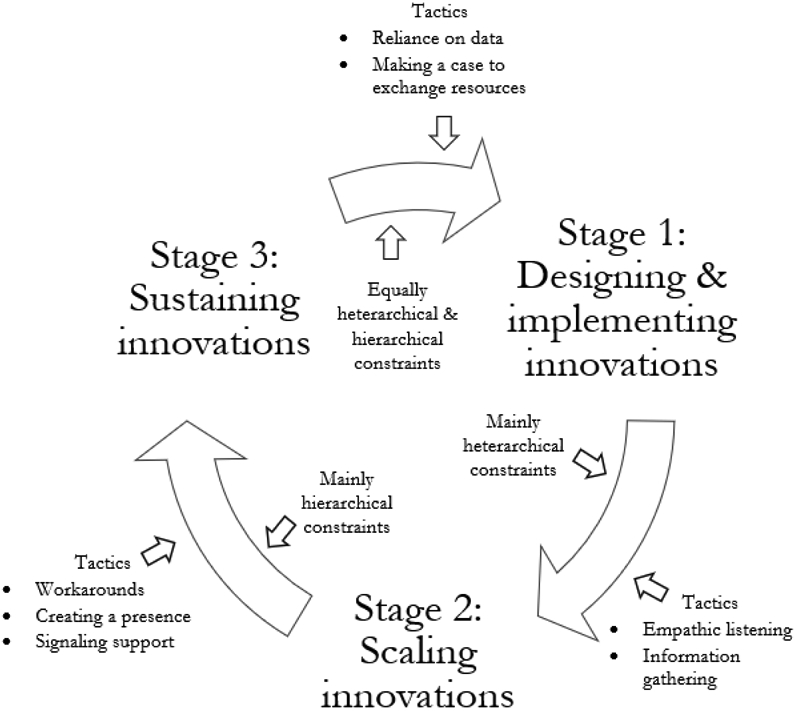
Care management processes, at each stage of the innovation cycle, propelled each of the tejims we studied forward in developing their health system innovations.
Hierarchical constraints often surfaced as directives from upper-level managers that impacted team activities, while heterarchical constraints surfaced as organizational professional groups resisted team efforts due to conflicting priorities. Table 1 captures our characterization of the relative strength and frequency (i.e., +++ insurmountable, ++ intense and long-lasting, + intense but short-lived) of the hierarchical and heterarchical constraints each team faced. The four teams enacted varying levels of constraint management based on their ability to identify tactics and apply them as they experienced constraints while iterating through the innovation cycle.
When teams first began working together, they focused on designing an innovation that would address the defined problem, and subsequently implement their solution. During this design and implementation stage, teams experienced both hierarchical and heterarchical constraints in relatively equal frequency and intensity. Once teams implemented their innovation, they began making strides to scale beyond the immediate implementation setting to other relevant contexts. In the scaling stage, heterarchical constraints were more pronounced. Last, teams realized and made efforts to sustain the innovation they had worked to scale. During the sustaining stage, teams more commonly experienced hierarchical constraints. The teams could engage in these stages repeatedly as they continued to adapt and refine their innovations.
As teams moved through their innovation cycle, the CMP involved recognizing constraints when they arose and responding appropriately by applying tactics to manage them. We sought to further examine linkages between the type of constraints and respective tactics used. We reviewed our findings for patterns and performed an analysis of code counts for each tactic applied to hierarchical and heterarchical constraints, as shown in Table 2. Of the 236 instances of hierarchical constraints, the most common tactic employed in response was workarounds (n=52). Of the 169 instances of heterarchical constraints, empathic listening (n=53) was the tactic most frequently deployed. For both hierarchical and heterarchical constraints, making a case to exchange resources (n=47 each) was the second-most frequent tactic.
TABLE 2.
Linkages between instances of constraints and tactics across all teams.
| Tactics | Hierarchical Constraints |
Heterarchical Constraints |
|---|---|---|
| Workarounds | 52 | 18 |
| Reliance on data | 17 | 17 |
| Empathic listening | 34 | 53 |
| Information gathering | 16 | 22 |
| Creating a presence | 38 | 3 |
| Making a case to exchange resources | 47 | 47 |
| Signaling support | 32 | 9 |
| TOTAL | 236 | 169 |
As we continued to analyze these frequencies and coded examples, we observed that teams employed two tactics frequently to address both hierarchical and heterarchical constraints: reliance on data and making a case to exchange resources. We described these as tactics to manage hierarchical and heterarchical constraints, since they were commonly used across both constraint types to enable progress. We also noted that teams tended to deploy these tactics especially in designing and implementing the innovation. Further, teams employed two tactics more frequently to address heterarchical than hierarchical constraints: empathic listening and information gathering. We consider these tactics to manage heterarchical constraints, since the tactics were used to garner broader peer support, and we noted that teams applied these tactics mainly to enable the team to scale these changes beyond their supporters in the immediate implementation settings. Last, teams employed three tactics more frequently to address hierarchical than heterarchical constraints: workarounds, creating a presence, and signaling support. Accordingly, these activities represented tactics to manage hierarchical constraints. Teams used these tactics mostly during the sustaining stage, since the tactics sought to achieve leader support so that teams could garner resources and establish greater visibility in the organization for long-term viability of the innovation.
Below, we first discuss the teams’ experiences of hierarchical and heterarchical constraints during stages of their innovation cycle. Then, we describe the tactics they used to manage them to design and implement, scale, and sustain their innovations, respectively. We examine the efficacy of these management tactics by tracking teams’ ability to make progress through the identification of various milestones.
Stage 1: Designing and Implementing Innovations
In the design and implementation stage, teams were involved in activities such as problem analysis to define the scope of team objectives and create shared understanding among members regarding team goals for innovation, simulation development to establish the requirements of new tools and process change, experimentation and pilot-testing aspects of the innovation, and implementing the design in a select context to further demonstrate efficacy and evaluate the innovation’s performance. In this stage, both hierarchical and heterarchical constraints were equally common. With regard to hierarchical constraints, upper-level stakeholders, or those with authoritative control over team activities, showed a lack of support in prioritizing the teams’ efforts which caused the teams to experience confusion around their activities and altered timelines as teams tried to conform to top-down changes. With regard to heterarchical constraints, lateral stakeholders, or those in other professional groups and units in the organization, influenced the team’s direction through resistance. For example, lateral stakeholders provided insufficient input in assisting with the design of the innovation and caused distractions from the goal as they communicated alternative priorities that derailed teams’ primary objectives.
In dealing with both hierarchical and heterarchical constraints, teams frequently relied on data and made a case to exchange resources. These tactics enabled the teams to design and implement their efforts, as they attempted to address upper-level and lateral stakeholders’ priorities and encourage buy-in. The teams used data to provide evidence and perform small tests of their innovations, which could serve as means to demonstrate efficacy in meeting needs in the organization and enhancing processes in useful ways. Further, the teams made a case to exchange resources, offering skills and expertise to stakeholders’ in exchange for information and access necessary in designing and implementing innovations.
Hierarchical Constraints
Confusion around team activities.
Hierarchal constraints often resulted in inconsistent actions, as teams reacted to the demands and organizational changes imposed by management. This reactivity typically impeded team progress, often derailing teams’ original plans in designing the innovation and causing course changes as teams were forced to put managerial priorities ahead of their own, as one health system staff team member described:
Around the same time [the project] started, management decided that they were going towards a completely different model where we were going to centralize all the referral staff into one place […] While the engineering team was trying to figure out how our processes work, we were in the middle of changing our processes in a completely radical way. So, it really made it hard to have any kind of consistency for the engineering team to see how we were working things because we were changing them every day. (Interview, Site A, 10/26/2017)
Altered timelines.
Hierarchical constraints slowed team activities as team members attempted to understand how their efforts fit into a dynamically changing organization. For example, system-level policy changes— one form of hierarchical constraint— influenced how teams developed redesign processes to ensure compliance with new organizational standards, slowing team activities, as described by a physician:
But now … a lot more of this is being done on a systems level, which both is a good thing because I think it helps with some of the IT challenges that we’ve had in the beginning, but I also think it slows things down. It doesn’t make sense to recreate the wheel here when it’s going to be done centrally. But when things are done centrally it takes forever and then you learn things that maybe you didn’t want to know. Like a licensed practice nurse can’t act on pended orders that aren’t signed. Which is a good thing – we need to follow hospital policy, but at the same time, it brings in barriers. (Focus Group, Site C, 4/26/2018)
Aligning the timing of team activities with organizational changes instituted by managers often meant slowing progress. Even in cases where managers supported team objectives, pacing was often based on managers’ top priorities, as one clinician explained:
[…] the other people on the [management-led] group, especially [the VP]; we’re kind of at their mercy. So, there’s work being done, but the frequency of those meetings and the agenda aren’t our decision. (Focus Group, Site D, 5/30/2018)
The high-risk working group at Site D had several key managerial staff as members, and meetings were steered by these individuals. Although members of the Site D team were invited to attend these meetings, their weighing-in on priorities was limited and as a result, innovation activities slowed, especially given the many other priorities management introduced at these meetings.
Heterarchical Constraints
Insufficient input.
Competing priorities of lateral stakeholders resulted in obstacles to providing needed information, resources, and other forms of supportive input that would enable teams to progress in designing and implementing their innovation. As this example describes, complete and accurate information from lateral stakeholders formed the basis for successful problem analysis for the team, yet the team at Site A struggled to get needed information:
We’ve done the FMEA [failure mode and effects analysis], but we haven’t completed it, because we needed [the lateral stakeholders] to provide input on this. And I personally asked and requested [of the lateral stakeholders], on more than one occasion, during the weekly meetings and through e-mails, to give us their feedback, but we got zero response on that. … so it’s difficult to gather all these individuals on more than one session and conduct this exercise and complete it. (Interview, Site A, 9/20/2017)
Team members, while able to sympathize with competing priorities that limited stakeholders’ involvement, nonetheless noted that this situation posed a challenge to completing their problem analysis, and thus, to deploying systems engineering tools necessary for designing their innovation. Engineers and project managers experienced hesitation in moving ahead with efforts because they lacked necessary lateral stakeholder input that would help the team conduct a more comprehensive analysis.
Distractions from the goal.
Health system redesign, as with redesign of other complex organizational processes, involves decision-making among individuals at all levels of an organization. Teams understood the importance of regular interaction with lateral stakeholders to ensure that redesigned processes aligned with the priorities and responsibilities of individuals throughout the organization, especially as they prepared for innovation implementation. However, repeated engagement introduced distractions that diffused team focus, as interactions often revealed new, and sometimes differing, stakeholder goals:
I think it just speaks to the nature of what we’re doing. It’s very interdisciplinary. It’s very collaborative. The [patients] themselves are very complicated with lots of issues. And these are hard, emotional decisions to be made. And all of those factors keep leading us in new directions. So I think that there’s clearly progress towards the general goal. … But the number of questions that are unearthed continues to multiply. (Interview, Site B, 9/14/2017)
When groups in the organization represented different preferences and priorities, team attention diffused as members sought to better understand the nature of the problem, potential solutions, and how best to satisfy the requests of lateral stakeholders. In another example, teams were distracted from regular activities as they spent time going on “fact finding missions,” to be able to procure needed information for innovation progress. These activities led to a richer understanding of the current care processes, but also revealed the team was required to both “give and take” as they transitioned from analysis to implementation in order to satisfy lateral stakeholders’ needs.
I accompanied [clinician] on a couple of his fact-finding missions. I was there when he talked to the urologist, the anesthesiologist, orthopedic surgeon. […] I think that has been successful in uncovering a lot of the things that make the processes, or lack of processes, higher risk and the patient experience much more negative. I think we’ve done a really good job at fact-finding. And we’ve trialed some improvements and now we need to have an honest conversation: can we pull these off and what will make them nicer for the doctor who is actually doing these? Because I can tell you, they don’t like it, and I think that’s important. (Interview, Site B, 9/14/2017)
Tactics Used to Manage Constraints When Designing and Implementing Innovations
Reliance on data.
In response to hierarchical constraints, teams used data analysis to generate shared understanding among members working on different sub-projects. This mitigated divergence in team perspectives as managers’ directives limited efforts. For example, teams attempted to predict how managers would influence team activities and relied on data analysis to show organizational leaders how the team’s innovation work aimed to improve performance overall:
So about future management decisions that might slow our team’s progress […] we’ve put in place a new process, and we’ve started to collect data to see how this new process is generating outcomes and how different those outcomes are. So if we continue doing this work and this analysis, it’s part of our business case. It would be very important to come up with a rigorous case study to present to management and tell them, “It seems that we have suggestive evidence that we’re making outcomes better. Patients are safer. Costs are lower.” And this might incentivize management to do some restructuring here and there to allow for this new standardization or philosophy to get embedded into the work. (Focus Group, Site B, 4/6/2018)
Similarly, teams worked to manage heterarchical constraints by using data analysis to identify the current scope of the problem. This strategy allowed them to generate evidence that could prove useful when engaging with lateral stakeholders. While one clinician at Site B noted that “data is good for measuring what we’re looking at, not planning or facilitating care coordination,” team understanding of the present state of a process allowed them to more confidently interact with lateral stakeholders in later interactions. In this way, data analysis was used as currency to translate ideas among interdisciplinary members of the team, and repeatedly served as an important tool to create shared understanding in managing constraints.
Making a case to exchange resources.
While experiencing hierarchical constraints, team members attempted to entice participation of upper-level stakeholders by providing skills or information those stakeholders would find useful. Teams approached upper-level stakeholder interactions transactionally, trying to understand what they could provide to address the concerns of others in the organization. Teams used knowledge obtained from activities specifically designed to gain understanding of their health system’s internal operations to identify ways in which they could appeal to upper-level stakeholders in hopes of building support once implementation was to take place. Teams then offered up this information or skills in hopes of obtaining lateral stakeholder support. One engineer described this tactic in response to losing multiple team members, due to managerial decisions:
So [the Vice President] joined a few meetings in the beginning of the project and in the failure modes effects analysis [activity], but was really not interested in the slow and steady. And she said, “Come back to me when you’re ready to start testing or you have something that you want to implement.” So we waited […] until we were ready to start testing, which was one strategy for [the Vice President] specifically, and then also for the Director of Operations, he’s really interested in the financials. So, we’re trying now to show some cost savings that this project will hopefully bring to [health system]. [The Vice President] cares more about patient safety, and the Chief Operations Officer cares more about the money. So, we’re tailoring to each. (Interview, Site D, 10/20/2017)
The team extended their activities to provide custom solutions addressing upper-level stakeholders’ needs, with hopes of gaining support. Previous experience with upper-level stakeholders, like the vice president, drove the team’s understanding of what to leverage to receive managerial resources. Knowledge of managerial needs also affected team planning in response to possible, future constraints. Team members assessed what they could give managers in order to receive needed resources in support of their innovation.
Similar to managing hierarchal constraints, teams that managed heterarchical constraints imposed by competing lateral stakeholder priorities encouraged participation by providing services or information:
I think, [the clinicians] are really good at highlighting what people are doing well in their practice and not making this a threatening type of approach. Playing off people's strengths and saying, “This is what you're doing already well. Hey, if we introduce this process, it should only help you.” […] It's almost like consumerism. Definitely, finding something that's going to pay off for [management]. (Interview, Site B, 10/6/2017)
Teams acknowledged the potential burden a new process could pose to lateral stakeholders who already had their own systems for providing care. In order to win these stakeholders over, the team worked to highlight the benefits of the new processes, framing the changes as a way of improving staff experience by integrating existing strengths. Teams also directly offered assistance with work; at Site B, the team offered to help another department with chart reviews to establish a partnership. In exchange, the team hoped to pilot newly designed processes within the department. The team recognized that without reciprocity in providing stakeholders with valuable help the team’s innovation efforts could be greatly delayed, or entirely unfeasible.
Stage 2: Scaling Innovations
When teams were in the scaling stage, they engaged in the following activities: attaining adopters from others outside of the immediate implementation setting to broaden use of the innovation in other relevant contexts, refining the innovation to address possible differences between the implementation and scale contexts, and performing further evaluations of the scale context to make a case for those wavering to adopt the innovation. Heterarchical constraints limited team progress as lateral stakeholders’ competing priorities influenced the direction of activities and the teams’ ability to scale the process redesign. In the scaling stage, lateral stakeholders were mostly outside of the immediate implementation context, and therefore their priorities diverged more notably than those of the lateral stakeholders in the implementation context. These more distant lateral stakeholders were highly reluctant to share responsibility in executing the team’s innovation efforts. In managing heterarchical constraints that arose while scaling their innovations, teams engaged in empathic listening and information gathering that demonstrated the innovation tended to lateral stakeholders’ needs and priorities. This in turn encouraged lateral stakeholders to share responsibility for using the innovation and to provide necessary information so teams could apply the innovation broadly and subsequently scale the team’s efforts.
Heterarchical Constraints
Reluctance to share responsibility.
Often teams contended with reluctance from organizational members outside the team to share responsibility for the innovation as the team worked to scale it, which produced stress, altered course, and shifts in team identity. As this example shows, teams had to address how their innovation could work at the system-level while accounting for different objectives of lateral stakeholders, causing the team to divert from its initial purpose:
We developed a general operating principle that these [patients] needed an approach in which all the elements of care before they could be cleared for surgery should be done before they go to the pre-op clinic. One of the outcome measures then would be [surgery performed as scheduled]. We’re going to reduce the times cardiology has to run over to clear a [patient] who otherwise would be cancelled. And I think […] it’s a nice goal for the hospital, but it’s not necessarily a nice goal for [the clinical service]. What does the clinical service get out of it? And that’s because the hospital is a siloed place and we are trying to break down some silos, but in the end you can end up holding the bag too much. (Interview, Site B, 9/14/2017)
Questions about responsibility for redesigned process steps surfaced many times and created worries that lateral stakeholders’ differing priorities could result in the team ultimately “holding the bag,” or being forced to take on work for which other individuals did not want responsibility. The concern resulted in a shift in the team’s purpose as they pushed to spread their redesigned processes and assumed responsibilities outside of the initial scope of the team’s work.
More generally, resistance from lateral stakeholders in implementing the team’s operational redesign produced concerns that the efforts would not scale:
[…] in general, the practice just said, “Do your own thing. You’re great doctors. Your patients love you and that’s the most important thing.” And so, then, when you try to do workflows that you really think are important for patient safety, those kind of ideas butt heads […] So you really have to bring the providers onboard or say, “I surrender.” (Focus Group, Site C, 4/26/2018)
This team acknowledged that physicians across the health system brought their own opinions to care provision and highlighted the importance of early engagement of lateral stakeholders in the team’s work. Without this, scaling the innovation would pose a greater challenge.
Tactics to Manage Heterarchical Constraints When Scaling Innovations
Empathic listening.
Teams sought to understand how lateral stakeholders were personally affected or could benefit from the work of the team in order to better understand and address different groups’ constraints. This tactic was foundational, as it provided the team with information about ways to tailor processes to appeal to those groups that initially resisted.
Well, when we had our first meeting with the chief of anesthesiology, we learned both about how rapid the process can be sometimes and how much they are concerned about the fact that they have to cancel surgeries…. I think that’s also one of the reasons we thought, “Well, let’s develop a tighter process… They come in, they are evaluated, the surgery’s planned, then that’s the signal for our team to go get the records, then set up an appointment for the pediatrician to review everything.” (Interview, Site B, 9/14/2018)
Teams recognized the importance of understanding what aspects of a process redesign effort were most beneficial to key lateral stakeholders, especially those for whom the innovation benefits were harder to define or align with priorities. As the teams planned for scale and sustainability of their innovations, they focused on provider or staff satisfaction. Anecdotal evidence grounded innovation efforts in day-to-day realities and offered more divergent opinions that enabled teams to understand differences in stakeholder perspectives.
But what I got the most use out of was doing usability testing with the providers that were outside the team. And I think, it’s also nice to have access to [a specific doctor] because he often represents an opinion that isn’t voiced in our meetings. Every time I talk to him, I just think about things a little bit differently and more from [a contrary perspective]. (Interview, Site C, 2/26/2018)
By focusing on lateral stakeholders’ personal experiences, both those that were congruent and divergent from team objectives, teams were able to directly address potential resistance on the part of individuals critical to team success. Furthermore, this tactic allowed teams to plan for future scaling, which teams recognized could also face resistance from lateral stakeholder groups.
Information gathering.
Teams addressed heterarchical constraints by calling upon stakeholders to fill information gaps regarding roles or organizational processes. Where stakeholders’ competing priorities meant they were unable to directly take part in team activities, team members worked to find other opportunities to engage with these groups, allowing them to identify new sources of data. These interactions also led team members to learn more about the heterarchical constraints they faced.
[…] every time we ask [stakeholders] for advice about a process, they’re always helpful in either confirming what we already knew, or guiding us in new directions that we didn’t think about, or debunking something that we thought was true and then wasn’t. Especially working with anesthesia; they’ve just helped us to understand how important the anesthesia piece is in the preoperative clearance process, and how siloed the process has been in the past, and how that could be beneficial to change for all the parties involved. (Interview, Site B, 5/31/2017)
The team made sense of the ways that the existing process siloed provider knowledge and communication. Taking stock of the political climate within the health system provided a realistic lens through which the teams viewed opportunities to scale their innovation. This tactic anticipated potential challenges arising from competing interests and combatted teams’ wariness to proceed with certain activities because it clarified roles or organizational processes through engagement with knowledgeable members of the health system and would in the long-term support scaling of the innovation across units.
Stage 3: Sustaining Innovations
As teams entered the sustaining innovations stage, they engaged in activities such as identifying and developing a strategy to procure needed resources for the innovation to continue in the long-term and developing measures that demonstrate long-term impact and viability. During this stage, hierarchal constraints impacted teams to different degrees, depending on the extent to which managerial priorities promoted or hindered the teams’ innovation efforts. As teams reflected on the hierarchical constraints they faced and reassessed how their activities fit within the larger health system, we noted progress halted or slowed, both in terms of team productivity and morale. In particular, at this stage, upper-level stakeholders caused teams to experience feelings of powerlessness in procuring needed resources and support to give their innovations long-term sustainability. The teams used tactics to deal with hierarchical constraints, which enabled them to position the organization to sustain efforts in the longer term. Sustaining efforts refers to the team’s ability to procure needed resources and garner necessary support from individuals in authoritative positions who would ultimately create the urgency and sense of necessity in the organization to adopt the team’s innovation.
Hierarchical Constraints
Powerlessness.
A lack of support from managers stemming from a disregard for the team’s efforts contributed to members feeling insecure about their abilities to execute on project goals. In this example, a sense of helplessness pervaded team interactions, creating a negative perception among team members of their ability to conceive that the innovation would be successful in the long-term:
Clinician 1: We had [a nurse] saying for a year that [a VP] did not like her and felt she was going to dump her…then did. [The nurse’s] argument that [the VP] didn’t like her [was based on the belief] that [the VP] did not choose her and that [the nurse] represented the “old guard.”
Clinician 2: As this project goes on, we become more and more peripheral to the process now that we’ve introduced homecare. We are not the people who have the power to change this, and we know who has the power to change it. (Team Meeting, Site D, 12/6/2017)
Perceived powerlessness often was demoralizing for teams, as they grew dissatisfied with team activities when noticing their organization’s leaders “pushing agendas” to use the redesign team to address organizational issues considered tangential to the group’s efforts. Hierarchical constraints ensued as decisions made by managers created divisions among team members.
Clinician 1: Yeah, so I think for the CCS [critical care service] visit, we can have the reminder saying “here’s the guide to try and use”
Clinician 2: I do think about how to set-up post-op CCS visits. If we set up actual visit times within EPIC. The thing that feels overwhelming is to add something on top of everything else. Having this listed as a visit for an afternoon, could mean provider could do one less clinic patient in the morning. This could help with sustainability [Clinician 2 looking for how to make things “stick”]
Clinician 1: I’m not sure that would have a chance… Will that get into billing issues? [Executive’s name] might be on us.
Clinician 2: Well, maybe in the inpatient world. We would have to try and track this down. (Team Meeting, Site B, 1/18/2018)
The two clinicians discussed possible options for streamlining their process changes so that the innovation could succeed long-term. However, one clinician believed these options wouldn’t succeed given upper-level stakeholders’ priorities, as they related to billing and hospital revenues. The diverging priorities of upper-level stakeholders conveyed a sense that the teams would not be able to procure necessary resources for long-term success.
Tactics to Manage Hierarchical Constraints When Sustaining Innovations
Workarounds.
When teams encountered hierarchical constraints, they often redirected efforts to project goals and objectives that relied less on leader support or input. By finding alternate, more feasible subprojects, teams sought to maintain momentum, which helped to avoid feelings of powerlessness due to the constraint. Often, this involved restating or tweaking goals to be able to maintain progress. For example, Site C team members lost a critical source of data used to show outcomes of their initiative to redesign clinical processes around urine toxicity testing of patients prescribed opioid medications. Loss of this data source resulted from an organizational-level decision to contract with a particular electronic medical record platform. One team member described the team’s response to divert attention toward other goals related more specifically to patient experience, yet still in line with the broader objectives of the team:
We completely switched gears and shifted [towards patient experience work] […] Which I think was a good move, and it made it really easy not to get hung up on the fact that we lost the provider data. I think it was just saying, “Let's not think about [the data registry] for now. Let's figure out something we can work on, and we'll come back to those things.” (Interview, Site C, 2/26/2018)
When experiencing constraints imposed by organizational leaders, team members frequently met outside regularly scheduled team meetings to address constraints and make progress through workarounds. Such meetings provided opportunities to focus on impediments as a smaller group with expertise applicable to the encountered hierarchical constraint, in this example:
I think, not related to the clinic, but related to our team, was the loss of the registry. And I think [name] has been helpful as an engineer working with the [pharmacist team member] without me and figuring out how they can use what data were in that registry, to create this proactive refill process. (Interview, Site C, 11/20/2017)
Work outside the full team meeting allowed system engineers and clinicians to develop novel solutions to problems resulting from health system changes that directly affected team goals. Ultimately, teams employed workarounds to maintain momentum and access needed resources through indirect means. Through this tactic, teams could sidestep potential power differentials with organizational leaders who did not prioritize the team’s innovation. Workarounds provided mechanisms for progress on innovations that would sustain the team’s work in the long run by being resilient to leaders’ lack of support.
Creating a presence.
To combat the influence of hierarchal constraints, teams increased stakeholder meetings with those relevant for the team’s work. These meetings served as opportunities to establish and maintain stakeholders’ focus on team innovation objectives, in order to better align leadership and team priorities. For example, the Site D team increased visibility through attendance at manager-led meetings, specifically by presenting their innovative work in a way that increased leaders’ interest in getting involved and offering team support for leaders’ initiatives. Rather than communicating indirectly, the team worked to connect their goals with leaders’ goals at larger meetings, even though these meetings were not directly relevant to the specific objectives of the team. In turn, team members gained understanding of how external stakeholders could be of help.
When team’s experienced feelings of powerlessness due to the pacing that upper-level stakeholders imposed, they assessed the organizational receptivity as they planned current and future activities and engaged in subprojects and timelines aligned with leader decisions in order to maintain progress.
I don’t know if it’s not as true in the engineering world, but I feel like there’s pressure that we need to be moving forward sometimes at a rate faster than we are, when I think we’re actually moving as quickly as we can. And sometimes that actually just means stopping [team activities] for a little so the clinic can catch up. (Interview, Site C, 11/20/2017)
This team addressed the impact that leaders’ decisions had on daily activities of the team. Operating within the context of the health system, which had its own goals and objectives, necessitated that teams account for these goals when timing their own work. As the clinician at Site C noted during an interview, it didn’t seem productive to “reinvent the wheel” when the team anticipated that eventually the work of the full clinic would come into alignment with the work of the team. This strategy anticipated the needs and demands of hospital leaders who could ultimately force a course change if teams moved forward without considering leaders’ timing. As the teams performed activities that enabled them to create a presence in the organization in managing hierarchical constraints, they used skills that would allow them to sustain effort through growing visibility.
Signaling support.
Teams invoked a strategy in which they highlighted previously-received upper-level stakeholders’ support to gain buy-in from new upper-level stakeholders. When teams lacked the power to directly engage with certain upper-level stakeholders, they attempted to work with leadership to indirectly influence other stakeholders to participate in the team’s work. Following the loss of several team members, due to hospital restructuring, one team sought to bring new team members on board by pointing to potential managerial support for team initiatives:
Clinician: But the head of Home Care is also the [Vice President] of transitional care. I don’t exactly understand the reporting lines, but she has some power in [getting new team members to join the team]. And then the head of Quality and Safety […] I believe she is just newly interested in our project. […] we had the buy-in of the people around because [the former case manager] was confident enough that she said, “Yep, I’ll do this,” and she just was able to make her own decision about whether she would be involved in this project. […] I’ve heard that [the new case manager] is not as confident. I think she needs the support and encouragement of the people around her to say, “Yes, the hospital wants you to do this.” (Interview, Site D, 11/13/2017)
This team recognized that they lacked the necessary resources and influence to directly convince the new case manager to join the team. The team drew on support from leaders who were interested in the project to garner new team membership from other upper-level stakeholders. When signaling support from respected and instrumental leaders in the organization, the teams performed activities that sustained their innovation efforts by enabling better alignment of priorities and timelines with key decision-makers.
DISCUSSION
Our research set out to examine how interdisciplinary teams experience and collectively respond to organizational constraints as they develop health system innovations. Through this study, as shown in Figure 1, we develop the CMP model, which illustrates that over time, teams experienced hierarchical and heterarchical constraints that obstructed team progress. While both constraints could appear at any time during the innovation process, we observed that hierarchical constraints posed challenges especially in the design/implementation and sustaining stages of innovation, while heterarchical constraints posed challenges more often in the design/implementation and scaling stages of innovation. In response, teams invoked various tactics to continue making progress on their innovations. To assess the teams’ effectiveness in making progress on their innovations, we tracked milestones over time and their status at the conclusion of our data collection period.
Previous studies have investigated aspects of collaborative teams that enable knowledge acquisition and team success, most commonly the inclusion of experts to teach teams improvement techniques, employ rapid cycle change methods (e.g., Deming’s PDSA cycles), and access to a repository of evidence-based practices and implementation strategies (Nembhard et al., 2009). Our research extends this work and shows how organizational challenges directly affect innovation teams’ progress and trigger responses through a variety of tactics, illustrating the linkage between organizational context and the inner workings of a team. Thus, our research demonstrates how teams are interdependent with the organization within which they operate, and how the organizational context impacts team effectiveness.
The interdependency between organizations and interdisciplinary teams operating within them is increasingly apparent in healthcare organizations, in which complexity, uncertainty, and specialization of staff and resources continue to increase. Today, teams rarely work in isolation, and team boundaries are more fluid and less clearly defined than ever— requiring greater emphasis on boundary spanning activities (Marrone, 2010). In accordance with these trends, our CMP model builds on the boundary spanning literature, explaining how tactics can be used by teams, not solely individuals, to span boundaries and address constraints by managing interactions with upper-level and lateral stakeholders. By showing the application of these tactics, our research highlights two broad takeaways for innovation teams: (1) identify, understand, and engage with the organization’s stakeholders early in the team’s efforts; and (2) use tactics to manage constraints, but also to keep team morale high by enabling members to work together productively and maintain momentum.
Drawing on these central findings, our research also has implications for boundary spanner roles in particular. Traditionally, boundary spanners have been referred to in the literature as organizational actors who gather and make sense of information from others with different expertise (Allen and Cohen, 1969). We show the communal and team-based aspects of boundary spanner activities. Specifically, team members in our study had boundary spanning roles, and as the team employed various tactics to manage and adapt to the challenges arising from organizational constraints, boundary spanners were able to collect, share, and incorporate useful knowledge to progress in their innovation projects. Our research suggests that boundary spanners are not primarily dependent on objects (i.e., embodiments of ideas or concepts such as work tools and explanatory instruments), as the traditional view of boundary spanning holds (Van de Ven and Zahra, 2016), but rather that they are also dependent on the combined efforts of their team to deal with the organizational context.
Most of the teams learned to develop and apply tactics effectively, with one team ultimately dismantling. One of the most prominent differences between the teams that continued to progress in their innovation cycles and the team that did not continue, was that successful teams had members across disciplines that tenaciously resolved to make progress, whether it was by working around or overcoming the constraint they experienced. For the team at Site A, differences among members’ disciplines became much more pronounced as the team experienced pressing hierarchical constraints; such differences were not addressed, and there was not a coherent or cohesive approach to applying tactics to address the hierarchical constraints, which ultimately undermined the design and implementation of the team’s innovation. Site A demonstrated what happens when talented, well-intentioned team members are strongly impacted by organizational leaders’ mandates that induce heavy loads of personal stress, leading to a shift in priorities and a breakdown in team cohesiveness. Further examination of such cases in which teams were unsuccessful in surmounting constraints at various stages of innovation through the use of the tactics we describe would further refine the findings of this research.
Our focus on interdisciplinary teams reflects the demands of complex health systems and the need to innovate. Though interdisciplinary teams enhance innovation in health care, such teams make constraints more salient by virtue of their diversity in expertise and perspectives when looking at the broader organization. However, the diversity of interdisciplinary teams also can provide a broader toolbox in dealing with organizational constraints. Though our findings can apply to many types of teams, we chose to focus on interdisciplinary teams because they are of growing importance in healthcare organizations desiring to innovate, and they enable a more comprehensive study of our phenomenon of interest by making constraints and tactics deployed more salient. We encourage scholars to continue to investigate how team composition relates to constraints and tactics.
While our research points to novel insights about the relationship between teams and organizational structure, we recognize the limitations of our work. Firstly, further research should be conducted on the relationship between these constraints, tactics, and measures of team progress. While all teams, except Site A, continued work on their innovation, our assessment of team progress was not rigorously quantified and reflects some subjective measures. Owing to the experimental nature of the innovation work, teams were not expected or required to present concrete products in a way that allowed us to measure whether teams completed pre-specified deliverables. Thus, we measured team progress by virtue of whether a team continued work throughout the study and documented this progress by assessing five categories of milestones at each site.
Since each of our teams were solving different types of problems, objectively characterizing innovations, relative application of the CMP, and subsequent progress, would be difficult. However, we note that innovation type can play a role in how teams apply the CMP and make progress on their innovations. For example, characteristics of an innovation can influence its adoption by different organizational members and therefore serve to mitigate constraints. In particular, innovations that diverge from routine practice are more likely to be adopted in organizations with siloed networks of actors, as innovation teams can leverage such gaps across units and individuals in the organization (Battilana and Casciaro, 2013). Our research provides a foundation for further evaluation of how innovation characteristics relate to the CMP and team progress, engendering a better understanding of the relationship between constraints, tactics, and team effectiveness.
Last, internal team dynamics were assumed to be functional across groups, though we did observe variations along interpersonal dimensions. These included attitude toward innovation and personality types among team members and over time. Our analysis did not focus on how such intra-team variations could affect the tactics teams employed or teams’ overall approach to managing constraints. Future research should consider studying the impact of interpersonal dynamics on teams’ approach to organizational constraints including the ways they learn to develop and deploy tactics.
Acknowledgements:
We are grateful to have had the support of our research assistant, Sophie Higgins. We would also like to thank several individuals for their feedback in developing this research along the way: members of the 4 project teams we studied, Jim Benneyan, Russell Phillips, Gordon Schiff, Lindsay Hunt, and attendees of the Academy of Management Annual Meeting (2019).
Funding Disclosure:
AHRQ P30HS024453
REFERENCES
- Adler PS, 1995. Interdepartmental interdependence and coordination: The case of the design/manufacturing interface. Organ. Sci 6, 147–167. [Google Scholar]
- Aldrich H, Herker D, 1977. Boundary spanning roles and organization structure. Acad. Manage. Rev 2, 217–230. [Google Scholar]
- Allen TJ, 1984. Managing the flow of technology: Technology transfer and the dissemination of technological information within the R&D organization. MIT Press Books; 1. [Google Scholar]
- Allen TJ, Cohen SI, 1969. Information flow in research and development laboratories. Adm. Sci. Q. 12–19. [Google Scholar]
- Ancona, 1990. Outward bound: strategic for team survival in an organization. Acad. Manage. J 33, 334–365. [Google Scholar]
- Ancona Caldwell, F. D, 1992. Bridging the boundary: External activity and performance in organizational teams. Adm. Sci. Q 634–665. [Google Scholar]
- Anderson C, Spataro SE, Flynn FJ, 2008. Personality and organizational culture as determinants of influence. J. Appl. Psychol 93, 702. [DOI] [PubMed] [Google Scholar]
- Anderson GF, Hussey P, Petrosyan V, 2019. It’s still the prices, stupid: Why the US spends so much on health care, and a tribute to Uwe Reinhardt. Health Aff. (Millwood) 38, 87–95. [DOI] [PubMed] [Google Scholar]
- Barry CA, Britten N, Barber N, Bradley C, Stevenson F, 1999. Using reflexivity to optimize teamwork in qualitative research. Qual. Health Res 9, 26–44. [DOI] [PubMed] [Google Scholar]
- Battilana J, Casciaro T, 2013. Overcoming resistance to organizational change: Strong ties and affective cooptation. Manag. Sci 59, 819–836. [Google Scholar]
- Bindman AB, Pronovost PJ, Asch DA, 2018. Funding innovation in a learning health care system. Jama 319, 119–120. [DOI] [PubMed] [Google Scholar]
- Bowen GA, 2008. Naturalistic inquiry and the saturation concept: a research note. Qual. Res 8, 137–152. [Google Scholar]
- Burt RS, 2000. The network structure of social capital. Res. Organ. Behav 22, 345–423. [Google Scholar]
- Charmaz K, 2006. Constructing grounded theory: A practical guide through qualitative analysis. Sage. [Google Scholar]
- Choi JN, 2002. External activities and team effectiveness: Review and theoretical development. Small Group Res. 33, 181–208. [Google Scholar]
- Cohen AR, Bradford DL, 2005. The influence model: Using reciprocity and exchange to get what you need. J. Organ. Excell 25, 57–80. [Google Scholar]
- Cohen J, 1960. A coefficient of agreement for nominal scales. Educ. Psychol. Meas 20, 37–46. [Google Scholar]
- Currie G, White L, 2012. Inter-professional barriers and knowledge brokering in an organizational context: the case of healthcare. Organ. Stud. 33, 1333–1361. [Google Scholar]
- Dey C, 2017. Team boundary activity: a review and directions for future research. Team Perform. Manag. Int. J 23, 273–292. [Google Scholar]
- Domecq JP, Prutsky G, Elraiyah T, Wang Z, Nabhan M, Shippee N, Brito JP, Boehmer K, Hasan R, Firwana B, 2014. Patient engagement in research: a systematic review. BMC Health Serv. Res 14, 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutton JE, Ashford SJ, 1993. Selling issues to top management. Acad. Manage. Rev 18, 397–428. [Google Scholar]
- Edmondson AC, Harvey J-F, 2018. Cross-boundary teaming for innovation: Integrating research on teams and knowledge in organizations. Hum. Resour. Manag. Rev 28, 347–360. [Google Scholar]
- Fernandez CF, Vecchio RP, 1997. Situational leadership theory revisited: A test of an across-jobs perspective. Leadersh. Q 8, 67–84. [Google Scholar]
- Glaser BG, Strauss AL, 1967. The discovery of grounded theory: strategies for qualitative theory. N. B. Aldine Trans. [Google Scholar]
- Grooms HR, Froehle CM, Provost LP, Handyside J, Kaplan HC, 2017. Improving the context supporting quality improvement in a neonatal intensive care unit quality collaborative: an exploratory field study. Am. J. Med. Qual 32, 313–321. [DOI] [PubMed] [Google Scholar]
- Johnson JD, Chang H-J, 2000. Internal and external communication, boundary spanning, and innovation adoption: An over-time comparison of three explanations of internal and external innovation communication in a new organizational form. J. Bus. Commun 197337, 238–263. [Google Scholar]
- Langley A, Lindberg K, Mørk BE, Nicolini D, Raviola E, Walter L, 2019. Boundary Work among Groups, Occupations, and Organizations: From Cartography to Process. Acad. Manag. Ann 13, 704–736. [Google Scholar]
- Makary MA, Daniel M, 2016. Medical error—the third leading cause of death in the US. Bmj 353, i2139. [DOI] [PubMed] [Google Scholar]
- Marrone JA, 2010. Team boundary spanning: A multilevel review of past research and proposals for the future. J. Manag 36, 911–940. [Google Scholar]
- Marrone JA, Tesluk PE, Carson JB, 2007. A multilevel investigation of antecedents and consequences of team member boundary-spanning behavior. Acad. Manage. J 50, 1423–1439. [Google Scholar]
- Milliken FJ, Martins LL, 1996. Searching for common threads: Understanding the multiple effects of diversity in organizational groups. Acad. Manage. Rev 21, 402–433. [Google Scholar]
- Nembhard IM, Alexander JA, Hoff TJ, Ramanujam R, 2009. Why does the quality of health care continue to lag? Insights from management research. Acad. Manag. Perspect 24–42. [Google Scholar]
- Orlikowski WJ, 2002. Knowing in practice: Enacting a collective capability in distributed organizing. Organ. Sci 13, 249–273. [Google Scholar]
- Reiter-Palmon R, Kennel V, Allen J, Jones KJ, 2018. Good Catch! Using Interdisciplinary Teams and Team Reflexivity to Improve Patient Safety. Group Organ. Manag 43, 414–439. [Google Scholar]
- Schein EH, 1995. Process consultation, action research and clinical inquiry: are they the same? J. Manag. Psychol 10, 14–19. [Google Scholar]
- Schippers MC, West MA, Dawson JF, 2015. Team reflexivity and innovation: The moderating role of team context. J. Manag 41, 769–788. [Google Scholar]
- Schot E, Tummers L, Noordegraaf M, 2019. Working on working together. A systematic review on how healthcare professionals contribute to interprofessional collaboration. J. Interprof. Care 1–11. [DOI] [PubMed] [Google Scholar]
- Shah SK, Corley KG, 2006. Building better theory by bridging the quantitative–qualitative divide. J. Manag. Stud 43, 1821–1835. [Google Scholar]
- Shea CM, Turner K, Albritton J, Reiter KL, 2018. Contextual factors that influence quality improvement implementation in primary care: The role of organizations, teams, and individuals. Health Care Manage. Rev 43, 261–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steizel S, Rimbau-Gilabert E, 2013. Upward influence tactics through technology-mediated communication tools. Comput. Hum. Behav 29, 462–472. [Google Scholar]
- Strauss A, Corbin J, 1994. Grounded theory methodology. Handb. Qual. Res 17, 273–85. [Google Scholar]
- Strauss A, Corbin JM, 1990. Basics of qualitative research: Grounded theory procedures and techniques. Sage Publications, Inc. [Google Scholar]
- Tortoriello M, Krackhardt D, 2010. Activating cross-boundary knowledge: The role of Simmelian ties in the generation of innovations. Acad. Manage. J 53, 167–181. [Google Scholar]
- Van de Ven A, Zahra SA, 2016. Boundary spanning, boundary objects, and innovation. Manag. Knowl. Integr. Boundaries 241–254. [Google Scholar]
- Van de Ven AH, 2017. The innovation journey: you can’t control it, but you can learn to maneuver it. Innovation 19, 39–42. [Google Scholar]
- Yukl G, Falbe CM, 1990. Influence tactics and objectives in upward, downward, and lateral influence attempts. J. Appl. Psychol 75, 132. [Google Scholar]


