Abstract
Over the past decade, chimeric antigen receptor (CAR) T cells have emerged as the prototype gene therapy for B cell leukemias. These so-called living drugs are derived from a patient’s own cells, reprogrammed to recognize and destroy cancer cells, and then reintroduced into the body. The huge success of this therapy for cancer is rooted in pioneering clinical and preclinical studies, established more than three decades ago, focused on persistent HIV-1 infection. In this issue of the JCI, Bingfeng Liu et al. revisit HIV-specific CAR T cells in an important clinical study that supports broader application of this groundbreaking therapy. Although curative endpoints were not achieved, these findings lay the foundation for augmented approaches applying combinatorial technologies including antigen supplementation.
CAR T cells from HIV to cancer and back
CAR T cell therapies were first described in the early 1990s as a treatment for antiretroviral therapy–suppressed (ART-suppressed) people living with HIV (PLWH). Despite promising initial data in preclinical experiments (1–3), three clinical trials between 1998 and 2005 found minimal impact on virus persistence in PLWH (4, 5). Long-term follow-up in these clinical cohorts established the safety of CAR-modified cell products and suggested that CAR T cells maintain the capacity to expand in response to exogenous activation stimuli (6). In parallel, advents in CAR engineering took this approach to new heights as a potent therapy for patients with hematological malignancies, namely CD19+ B cell leukemias and lymphomas. Among many approaches to potentiate CAR T cell function against malignant targets, various groups have validated more advanced lentiviral vector designs, methods to control ratios of T cell subsets within a CAR product, culture conditions geared toward memory T cell phenotypes, and perhaps most importantly, the addition of costimulatory domains within the CAR molecule, designed to enhance target-dependent killing (7–10).
In this issue of the JCI, Bingfeng Liu et al. took the impressive clinical efficacy of these next-generation CAR products for cancer into account, and built on the safety of first-generation HIV-specific CAR T cells that were established over 20 years ago. Liu and colleagues reported on the results of a clinical trial involving 15 HIV-infected, ART-suppressed participants who received next-generation HIV-specific CAR T cells. The authors’ goal was to assess the safety and impact of CD8+ CAR T cells on virological parameters before and, in the case of six participants, after ART treatment interruption (ATI) (11).
HIV CAR T cell effects on reactivated viral reservoirs
Liu et al. enrolled 15 participants with ART-suppressed HIV-1 infection and successfully manufactured a virus-specific CAR T cell product for 14 out of 15 individuals. The CAR featured a single chain variable fragment (scFv) derived from the HIV-1 broadly neutralizing antibody, VRC01, and contained both CD28 and 4-1BB costimulatory domains. Further, the lentiviral vector used to modify CD8+ T cells from each participant coexpressed short hairpin RNA molecules designed to knock down the expression of immune exhaustion proteins PD1, TIM3, and LAG3. In the six participants who underwent ATI, time to viral rebound was substantially longer than in a historical control cohort (12). Correlative measurements further suggested that CAR+ cells expanded coincident with increases in cell-associated viral RNA after ART interruption. Intact provirus detection assays, a current gold standard for virus persistence (13, 14), showed a marked decrease in intact proviruses in this cohort over time. Sequencing experiments suggested that viral diversity decreased following CAR treatments and selection for CAR-resistant variants occurred, although these data were limited in scope. Comparisons to untreated controls (participants who underwent ATI without CAR T cell therapy) were notably limited to historical reports. This limitation is understandable when considering ethical challenges for noninterventional ATI studies (15, 16). The key findings from Liu et al., namely a delay of up to 10 weeks in viral rebound following ATI, offer a tantalizing glimpse of the potential for HIV-specific CAR T cell therapies in ongoing and future studies. One intriguing question is whether posttreatment immune control would have been seen in the six ATI participants if their ART interruption period had been extended beyond a single documented virus-positive time point.
Next steps for HIV CAR T cell therapies
Much remains to be learned regarding the requirements for an effective CAR T cell strategy for persistent HIV infection. Many will continue to highlight similarities and opportunities for synergy with CAR T cells for cancer. It is increasingly clear that the local immune environment, the frequency of antigen-expressing target cells, and/or the density of antigen on the surface of each target (Figure 1) are important considerations that must be addressed. Due to the well-characterized persistence of HIV-infected cells in secondary tissue sites, including lymph nodes, gut, spleen, and the central nervous system, a successful HIV cure approach will almost certainly need to maintain function at these sites as well as in peripheral blood. However, decreased numbers and function of immune effectors like CAR T cells in tissues is a common limitation for solid tumors as well as HIV. Lessons from the cancer field highlight a key barrier to this goal—the immunosuppressive nature of the solid tumor microenvironment, which downregulates function and decreases persistence of CAR T cells (17–19) and other immunotherapies. Unsurprisingly, early studies similarly show only limited trafficking of virus-specific CAR T cells to sites of HIV-1 persistence, such as B cell follicles in lymph nodes, and a failure to recognize and clear infected cells at these sites (20–22).
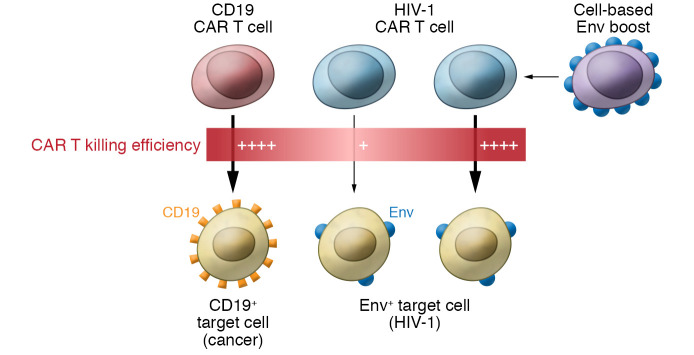
Figure 1. CAR T cell function above and below threshold levels of cognate antigen.
Malignant cells, for example CD19+ leukemias, express high levels of CD19 antigen at the cell surface and are efficiently killed by CD19 CAR T cells (left). HIV-1–positive cells with latent infection express much lower levels of cell surface antigens (namely, Env), resulting in substantially lower killing efficiencies (middle). An approach to boost HIV-1 CAR T cells with cell-associated Env would provide exogenous antigen in vivo and increase CAR T killing efficiency (right).
The sparsity of cell-associated envelope (Env) antigen during ART-suppressed HIV-1 infection is also a critical barrier, juxtaposed with FDA-approved CAR T cell therapies for leukemia (Figure 1). CD19+ leukemias frequently contain kilogram quantities of malignant cells in peripheral blood and bone marrow and express high levels of surface CD19 that facilitate rapid and efficient recognition and killing by CD19 CAR T cells. In contrast, CAR T cell therapy for HIV is confounded by the extremely low expression of HIV-1 Env protein at the surface of latently infected cells, namely primary CD4+ T cells (23, 24) and by the low number of latently infected cells (no more than 1 per million CD4+ T cells) in a typical PLWH (13, 25). Several groups including ours have and continue to address these barriers in small and large animal models of HIV persistence (26, 27).
The clinical data from Liu et al. represent a welcome return of HIV-specific CAR T cells to the clinic. Iteratively developing gene therapy and gene editing approaches that augment CAR T cell safety, function, and persistence will be essential to further augment these therapies, with the ultimate goal of enabling lifelong HIV remission without the need for daily ART. Beyond optimizing the best CAR molecules and cell manufacturing approaches in preclinical models, aligning these studies with rationally designed clinical trials will, likewise, be critical. Our previous nonhuman primate study was designed to inform an ongoing clinical trial (Clinicaltrials.gov identifier NCT03617198), in particular focused on the timing between CAR T cell infusion and ATI. Liu et al. interrupted ART 3 to 6 weeks following infusion of CAR-modified cells, and it remains unclear whether a shorter period may be required to ensure remission (i.e., so that recrudescent viral antigen coincides with the peak window of CAR T cell immune surveillance in vivo). Other aspects, including exogenous antigen boosting, enhancement of cell-intrinsic CAR properties, and/or modifications to the local viral reservoir environment, may require further studies in preclinical models. The study by Liu et al. reminds us that CAR T cells were born as a treatment for infectious disease and, following lessons learned in cancer immunotherapy, have come full circle as an HIV-specific clinical therapy. Much work remains to develop this approach into a form that will consistently lead to HIV cure endpoints. A call to action to invest the necessary resources in this extremely promising immunotherapy, not just for HIV, but numerous other diseases, may provide profound clinical benefit.
Acknowledgments
The author thanks Helen Crawford for assistance in preparing this manuscript and Hans-Peter Kiem and James Riley for helpful comments and feedback. Funding support was provided by the National Institutes of Health, the National Heart, Lung, and Blood Institute (U19 HL156247), and the National Institute of Allergy and Infectious Diseases (U19 AI149676, U19 AI149680, U19 AI149504).
Version 1. 10/01/2021
Electronic publication
Footnotes
Conflict of interest: The author has declared that no conflict of interest exists.
Copyright: © 2021, American Society for Clinical Investigation.
Reference information: J Clin Invest. 2021;131(19):e153204. https://doi.org/10.1172/JCI153204.
See the related article at Broadly neutralizing antibody-derived CAR T cells reduce viral reservoir in individuals infected with HIV-1.
References
- 1.Roberts MR, et al. Targeting of human immunodeficiency virus-infected cells by CD8+ T lymphocytes armed with universal T-cell receptors. Blood. 1994;84(9):2878–2889. [PubMed] [Google Scholar]
- 2.Romeo C, Seed B. Cellular immunity to HIV activated by CD4 fused to T cell or Fc receptor polypeptides. Cell. 1991;64(5):1037–1046. doi: 10.1016/0092-8674(91)90327-U. [DOI] [PubMed] [Google Scholar]
- 3.Yang OO, et al. Lysis of HIV-1-infected cells and inhibition of viral replication by universal receptor T cells. Proc Natl Acad Sci U S A. 1997;94(21):11478–11483. doi: 10.1073/pnas.94.21.11478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deeks SG, et al. A phase II randomized study of HIV-specific T-cell gene therapy in subjects with undetectable plasma viremia on combination antiretroviral therapy. Mol Ther. 2002;5(6):788–797. doi: 10.1006/mthe.2002.0611. [DOI] [PubMed] [Google Scholar]
- 5.Mitsuyasu RT, et al. Prolonged survival and tissue trafficking following adoptive transfer of CD4zeta gene-modified autologous CD4(+) and CD8(+) T cells in human immunodeficiency virus-infected subjects. Blood. 2000;96(3):785–793. [PubMed] [Google Scholar]
- 6.Scholler J, et al. Decade-long safety and function of retroviral-modified chimeric antigen receptor T cells. Sci Transl Med. 2012;4(132):132ra53. doi: 10.1126/scitranslmed.3003761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fraietta JA, et al. Determinants of response and resistance to CD19 chimeric antigen receptor (CAR) T cell therapy of chronic lymphocytic leukemia. Nat Med. 2018;24(5):563–571. doi: 10.1038/s41591-018-0010-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turtle CJ, et al. Immunotherapy of non-Hodgkin’s lymphoma with a defined ratio of CD8+ and CD4+ CD19-specific chimeric antigen receptor-modified T cells. Sci Transl Med. 2016;8(355):355ra116. doi: 10.1126/scitranslmed.aaf8621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feucht J, et al. Calibration of CAR activation potential directs alternative T cell fates and therapeutic potency. Nat Med. 2019;25(1):82–88. doi: 10.1038/s41591-018-0290-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schuster SJ, et al. Chimeric antigen receptor T cells in refractory B-cell lymphomas. N Engl J Med. 2017;377(26):2545–2554. doi: 10.1056/NEJMoa1708566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu B, et al. Broadly neutralizing antibody-derived CAR T cells reduce viral reservoir in individuals infected with HIV-1. J Clin Invest. 2021;131(19):e150211. doi: 10.1172/JCI150211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li JZ, et al. The size of the expressed HIV reservoir predicts timing of viral rebound after treatment interruption. AIDS. 2016;30(3):343–353. doi: 10.1097/QAD.0000000000000953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bruner KM, et al. A quantitative approach for measuring the reservoir of latent HIV-1 proviruses. Nature. 2019;566(7742):120–125. doi: 10.1038/s41586-019-0898-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levy CN, et al. A highly multiplexed droplet digital PCR assay to measure the intact HIV-1 proviral reservoir. Cell Rep Med. 2021;2(4):100243. doi: 10.1016/j.xcrm.2021.100243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dube K, et al. Ethics of HIV cure research: an unfinished agenda. BMC Med Ethics. 2021;22(1):83. doi: 10.1186/s12910-021-00651-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Julg B, et al. Recommendations for analytical antiretroviral treatment interruptions in HIV research trials-report of a consensus meeting. Lancet HIV. 2019;6(4):e259–e268. doi: 10.1016/S2352-3018(19)30052-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mardiana S, et al. Supercharging adoptive T cell therapy to overcome solid tumor-induced immunosuppression. Sci Transl Med. 2019;11(495):eaaw2293. doi: 10.1126/scitranslmed.aaw2293. [DOI] [PubMed] [Google Scholar]
- 18.Schurich A, et al. Metabolic regulation of CAR T cell function by the hypoxic microenvironment in solid tumors. Immunotherapy. 2019;11(4):335–345. doi: 10.2217/imt-2018-0141. [DOI] [PubMed] [Google Scholar]
- 19.Pituch KC, et al. Adoptive transfer of IL13Rα2-Specific chimeric antigen receptor T cells creates a pro-inflammatory environment in glioblastoma. Mol Ther. 2018;26(4):986–995. doi: 10.1016/j.ymthe.2018.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ollerton MT, et al. HIV-1-specific chimeric antigen receptor T cells fail to recognize and eliminate the follicular dendritic cell HIV reservoir in vitro. J Virol. 2020;94(10):e00190-20. doi: 10.1128/JVI.00190-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haran KP, et al. Simian immunodeficiency virus (SIV)-specific chimeric antigen receptor-T cells engineered to target B cell follicles and suppress SIV replication. Front Immunol. 2018;9:492. doi: 10.3389/fimmu.2018.00492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ayala VI, et al. CXCR5-dependent entry of CD8 T cells into rhesus macaque B-cell follicles achieved through T-cell engineering. J Virol. 2017;91(11):e02507-16. doi: 10.1128/JVI.02507-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stano A, et al. Dense array of spikes on HIV-1 virion particles. J Virol. 2017;91(14):e00415-17. doi: 10.1128/JVI.00415-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bruel T, et al. Elimination of HIV-1-infected cells by broadly neutralizing antibodies. Nat Commun. 2016;7:10844. doi: 10.1038/ncomms10844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chun TW, et al. Relationship between the size of the human immunodeficiency virus type 1 (HIV-1) reservoir in peripheral blood CD4+ T cells and CD4+:CD8+ T cell ratios in aviremic HIV-1-infected individuals receiving long-term highly active antiretroviral therapy. J Infect Dis. 2002;185(11):1672–1676. doi: 10.1086/340521. [DOI] [PubMed] [Google Scholar]
- 26.Maldini CR, et al. Dual CD4-based CAR T cells with distinct costimulatory domains mitigate HIV pathogenesis in vivo. Nat Med. 2020;26(11):1776–1787. doi: 10.1038/s41591-020-1039-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rust BJ, et al. Robust expansion of HIV CAR T cells following antigen boosting in ART-suppressed nonhuman primates. Blood. 2020;136(15):1722–1734. doi: 10.1182/blood.2020006372. [DOI] [PMC free article] [PubMed] [Google Scholar]