Abstract
Background
Global dissemination of SARS-CoV-2 Variants of Concern (VOCs) remains a concern. The aim of this study is to describe how mass testing and phylogenetic analysis successfully prevented local transmission of SARS-CoV-2 VOC in a densely populated city with low herd immunity for COVID-19.
Methods
In this descriptive study, we conducted contact tracing, quarantine, and mass testing of the potentially exposed contacts with the index case. Epidemiological investigation and phylogeographic analysis were performed.
Findings
Among 11,818 laboratory confirmed cases of COVID-19 diagnosed till 13th May 2021 in Hong Kong, SARS-CoV-2 VOCs were found in 271 (2.3%) cases. Except for 10 locally acquired secondary cases, all SARS-CoV-2 VOCs were imported or acquired in quarantine hotels. The index case of this SARS-CoV-2 VOC B.1.351 epidemic, an inbound traveler with asymptomatic infection, was diagnosed 9 days after completing 21 days of quarantine. Contact tracing of 163 contacts in household, hotel, and residential building only revealed 1 (0.6%) secondary case. A symptomatic foreign domestic helper (FDH) without apparent epidemiological link but infected by virus with identical genome sequence was subsequently confirmed. Mass testing of 0.34 million FDHs identified two more cases which were phylogenetically linked. A total of 10 secondary cases were identified that were related to two household gatherings. The clinical attack rate of household close contact was significantly higher than non-household exposure during quarantine (7/25, 28% vs 0/2051, 0%; p<0.001).
Interpretation
The rising epidemic of SARS-CoV-2 VOC transmission could be successfully controlled by contact tracing, quarantine, and rapid genome sequencing complemented by mass testing.
Funding
Health and Medical Research Fund Commissioned Research on Control of Infectious Disease (see acknowledgments for full list).
Keywords: SARS-CoV-2, Variants of Concern, Contact tracing, Mass testing, Phylogenetic analysis
1. Introduction
The pandemic of Coronavirus Disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has disseminated globally since the outbreak of community acquired pneumonia in Wuhan, Hubei Province was officially announced by National Health Commission of the People's Republic of China on 31st December 2019 (day 1).1 There have been 157 million infections with >3.2 million deaths globally as of 16th May 2021.2 The emergence of SARS-CoV-2 Variants of Concern (VOCs) with increased transmissibility and potential reduction in COVID-19 vaccine efficacy poses further threat to the outbreak control. The first SARS-CoV-2 VOC originated from South Africa (B.1.351) in May 2020. Subsequently, SARS-CoV-2 VOCs were identified in the United Kingdom (B.1.1.7) in September 2020, India (B.1.167) in October 2020, and Brazil (B.1.1.28.1, alias P.1) in November 2020.2 Restriction on international travel, border control, and quarantine measures are crucial in preventing the importation of SARS-CoV-2 VOCs which may cause subsequent community outbreak.3
In Hong Kong, all inbound travelers arriving at Hong Kong International Airport need to receive on-site COVID-19 testing since March 2020,4 followed by compulsory quarantine either at home or at self-arranged premises including hotels for 14 days. Lapse in these control measures was suspected to have resulted in imported cases leaking into the community which started the fourth wave of COVID-19 in November 2020.5 Because of the high transmissibility of SARS-CoV-2 VOCs and low seroprevalence in Hong Kong, the duration of mandatory quarantine of persons requiring from all countries except China in designated hotels has been extended to 21 days starting from 25th December 2020.6 This is to minimize the risk of importation and subsequent community spread of SARS-CoV-2 VOCs.
However, all these measures were not sufficient to prevent COVID-19 spreading from an imported case with beta COVID-19 variant (SARS-CoV-2 VOC B.1.351) in April 2021. In response to this first incidence of community transmission of SARS-CoV-2 VOC in Hong Kong, we conducted contact tracing complemented by mass testing of 0.81 million people, along with phylogeographic analysis, to control the community outbreak. The objective of this study is to describe how mass testing and phylogenetic analysis successfully prevented local transmission of SARS-CoV-2 VOC in a densely populated city with low herd immunity for COVID-19, which may be useful to other areas, especially the Western Pacific region, with similar geo-epidemiological background. In addition, we further emphasize the importance of contact tracing in outbreak control, especially in regard to household close contacts.
2. Methods
2.1. Epidemiology of COVID-19 in Hong Kong
The epidemiological information on COVID-19 was prospectively retrieved from the website of the Centre for Health Protection, Department of Health, the Government of Hong Kong Special Administrative Region, China.7 The public health measures in the community and infection control and prevention measures in hospitals were escalated when the outbreak of community acquired pneumonia in Wuhan, Hubei Province, was officially announced on 31st December 2019.1 Since we adopted a hospital-based approach for COVID-19 control, i.e. admitting all COVID-19 patients to the isolation facilities in public hospitals or the community isolation and treatment facilities,8 both under the governance of the Hospital Authority, we have progressively intensified the infection control training and measures to minimize the risk of nosocomial transmission of COVID-19.[9], [10], [11], [12] From the public health perspective, universal masking in the community was practiced since the early phase of the pandemic.13 A stepwise implementation of COVID-19 testing was introduced at the border as well as in the community for high-risk occupations and those who perceived themselves as at increased risk of acquiring COVID-19 (Table 1). Lock down measures were not implemented in Hong Kong during the COVID-19 pandemic.
Table 1.
Tiers of community testing for COVID-19 in Hong Konga
| Tier | Criteria |
|---|---|
| 1. | Enhanced surveillance for asymptomatic inbound travelers |
| Testing upon arrival (since 19th March 2020) | |
| Testing between 3rd day and 12th day of arrival (since 20th April 2020) | |
| Testing on 19th day of arrival (since 18th December 2020) | |
| 2. | Enhanced surveillance for persons with higher risk of exposure |
| Staff at Hong Kong International Airport (since 15th May 2020) | |
| Staff at residential care home for the elderly and disability (since 20th May 2020) | |
| Frontline workers of bus companies (since 12th June 2020) | |
| Essential staff of critical infrastructure and services (14th July 2020) | |
| Any persons who perceives themselves to have higher risk of exposure and experience mild discomfort (since 27th July 2020). | |
| 3. | Community testing center |
| Self-paid services (since 15th November 2020) | |
| Free for persons under compulsory testing notice (since 22nd November 2020) b |
Respiratory specimens such as nasopharyngeal swab, nasal swab, throat swab, and deep throat saliva were used as screening specimen.
The Government exercised the power under the Prevention and Control of Disease (Compulsory Testing for Certain Persons) Regulation (Cap. 599J) and published in the Gazette a compulsory testing notice.
Contact tracing was conducted whenever a newly confirmed COVID-19 case was identified. Household members, attendees at household gatherings, and workplace contacts in the same office would be defined as close contacts, regardless of surgical mask usage, and quarantined for 14 days or 21 days for index patients carrying non-SARS-CoV-2 VOC or SARS-CoV-2 VOCs respectively. When the first few cases of locally acquired SARS-CoV-2 VOC of unknown epidemiological source were identified, all residents staying in the same building were sent to quarantine centers for 21 days and tested for SARS-CoV-2 on first day and on days 3, 7, 12 and 19. Currently, the period of contact tracing for local cases without epidemiological link to a known case was counted from 14 days before onset of symptoms for symptomatic COVID-19 patients or 14 days before the laboratory confirmation of SARS-CoV-2 for asymptomatic COVID-19 patients. The period of contact tracing would be extended to 21 days if the index case is carrying SARS-CoV-2 VOC. If the close contact had respiratory symptoms, he or she would be admitted to the airborne infection isolation room in public hospitals for further management. The household contacts of close contacts, as the second layer of close contacts, would be subjected to compulsory testing. They would be sent to quarantine center for 2 days if the first layer close contact was symptomatic while waiting for the test results of the first layer close contact.
Compulsory testing for COVID-19 is enacted by law, The Prevention and Control of Disease Ordinance under Cap. 599 in Hong Kong (Table 2). It requires the persons who may be infected with SARS-CoV-2 to undergo mandatory testing, in order to facilitate the early diagnosis and isolation of infected cases. Compulsory testing not only applied to the inbound travelers (Cap. 599C & Cap.599E), but also to any persons who had attended the premises including buildings, schools, shopping malls, restaurants and other public and private facilities in the community, where a confirmed COVID-19 patient had lived or worked, or where SARS-CoV-2 VOC cases had visited during the incubation period (Cap. 599J).14 Compulsory testing operations in the specified restricted areas were also implemented for the control of COVID-19 by the use of a restriction-testing declaration.15 Regular testing for SARS-CoV-2 in specifically defined high-risk occupations in the public service provision was also mandated. Those who had compulsory testing notice issued by the government could receive free testing at community testing centers, which also provided self-paid services to those who may require a laboratory report for crossing border or visiting hospitals or elderly homes.
Table 2.
The Prevention and Control of Disease Ordinance under Cap. 599 in Hong Kong
| Cap. | Title |
|---|---|
| 599 | The Prevention and Control of Disease Ordinance (14th July 2008): An Ordinance to provide for the control and prevention of disease among human beings; to prevent the introduction into, the spread in and the transmission from, Hong Kong of any disease, source of disease or contamination; to apply relevant measures of the International Health Regulations promulgated by the World Health Organization; and to provide for connected purposes. |
| 599C | Compulsory Quarantine of Certain Persons Arriving at Hong Kong Regulation (8th February 2020) |
| 599D | Prevention and Control of Disease (Disclosure of Information) Regulation (8th February 2020) |
| 599E | Compulsory Quarantine of Persons Arriving at Hong Kong from Foreign Places Regulation (19th March 2020) |
| 599F | Prevention and Control of Disease (Requirements and Directions) (Business and Premises) Regulation (28th March 2020) |
| 599G | Prevention and Control of Disease (Prohibition on Group Gathering) Regulation (29th March 2020) |
| 599H | Prevention and Control of Disease (Regulation of Cross-boundary Conveyances and Travellers) Regulation (15th July 2020) |
| 599I | Prevention and Control of Disease (Wearing of Mask) Regulation (15th July 2020) |
| 599J | Prevention and Control of Disease (Compulsory Testing for Certain Persons) Regulation (15th November 2020) |
| 599K | Prevention and Control of Disease (Use of Vaccines) Regulation (24th December 2020) |
2.2. Study design and participants
For all persons under compulsory testing or requiring regular testing for COVID-19, combined nasal and throat swabs were collected by staff with medical and healthcare training in the community testing centers. SARS-CoV-2 RNA was detected by reverse transcription polymerase chain reaction (RT-PCR). Those who were tested positive for SARS-CoV-2 were admitted to public hospitals or the newly built temporary hospital adjacent to the community treatment facility at AsiaWorld-Expo in Hong Kong. Respiratory specimens such as nasopharyngeal swabs, throat swabs, and sputum were collected for serial monitoring of viral load by RT-PCR. Deep throat saliva was accepted as an alternative specimen.16 Whole genome sequencing was performed on respiratory specimens or deep throat saliva from laboratory confirmed COVID-19 cases. This study was approved by the Institutional Review Boards of The Hong Kong Polytechnic University (approval no. RSA20021) and the public hospitals involved (HKECREC-20200-014; KWC-2020-0040; HKWC UW 20-292).
2.3. Whole genome sequencing
Whole genome sequencing of SARS-CoV-2 was performed using Nanopore sequencing technology (Oxford Nanopore Technologies, Oxford, UK) as we previously described.5,17 Briefly, the total nucleic acid was extracted from respiratory specimens by NucliSENS® easyMAG® (bioMérieux, The Netherlands) following the manufacturers’ standard protocols. Host DNA was then removed using ezDNase™ Enzyme (ThermoFisher Scientific, USA). Dnase-treated RNA was reverse-transcribed to cDNA by LunaScript® RT SuperMix Kit (New England Biolabs, UK). Viral cDNA was amplified using the ARTIC nCov-2019 V3 Panel and Q5® Hot Start High-Fidelity 2X Master Mix (IDT, USA). PCR products clean-up was done by Agencourt AMPure XP for PCR Purification (Beckman Coulter, California, USA). End-prep, barcode ligation and sequencing adaptor ligation were performed according to the PCR tiling of SARS-CoV-2 virus with Native Barcoding Expansion 96 protocol (Version: PTCN_9103_v109_revJ_13Jul2020). The library was loaded and sequenced on MinION or GridION (ONT, UK) with R9.4.1 flow cells for 48 h. Nanopore sequencing data were analyzed using Artic Network nCoV-2019 novel coronavirus bioinformatics protocol.18
2.4. Phylogeographic analysis
Maximum-likelihood phylogenetic tree was constructed by first performing multiple sequence alignment (MSA) using MAFFT with fasta as the output format.19 The MSA file was converted to phylip format by TrimAL. Smart Model Selection (SMS) in PhyML was used to select the best-fitting nucleotide substitution model based on Akaike information criterion (AIC). PhyML was used to construct the maximum likelihood phylogenetic tree with Felsenstein bootstrap replicates having 1000x and be rooted on the SARS-CoV-2 reference genome (accession no.: MN908947.3).20 Cases with bootstrap of 70% and Bayesian probability of 0.95 were defined as part of a phylogenetic cluster.
The coordinates of the residences and the premises that were visited by the confirmed cases during the incubation period were retrieved from publicly accessible websites.21,22 The geographic distributions of the cases were displayed on Hong Kong map using ArcGIS Pro v.2.7.1 (Ersi, CA, US).
2.5. Statistical Analysis
Differences in the clinical attack rate of SARS-CoV-2 acquisition were evaluated between the household close contact and non-household contact during quarantine period using Fisher exact test for categorical variables. All statistical analyses were performed using IBM SPSS Statistics (version 26). A two-sided p-value of < 0.05 was considered statistically significant.
2.6. Role of the funding source
The funding sources had no role in the study design, data collection, analysis, interpretation, or writing of the report. The corresponding author had full access to all data in the study and had the final responsibility for the decision to submit for publication.
3. Results
3.1. Epidemiology of COVID-19 in Hong Kong
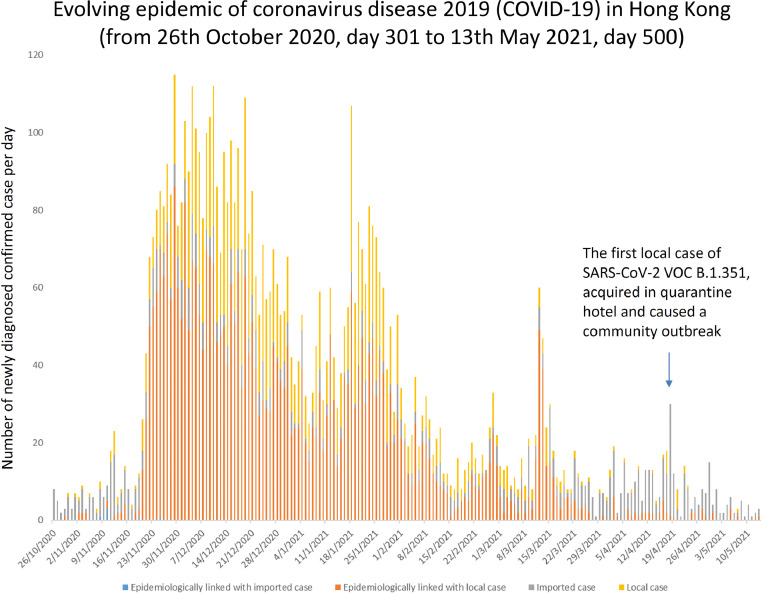
From day 1 to day 500 (13th May 2021) since the declaration of community acquired pneumonia in Wuhan, there were 11,818 laboratory confirmed case of COVID-19 in Hong Kong, of which 6,157 (52.1%) were female. The median age was 44 years (range, 1 month to 100 years). The overall case-fatality rate was 1.8% (210/11,818). Ninety-six percent (11,396/11,818) were Hong Kong residents, while the remaining were travelers. The imported cases and their secondary transmission comprised 20.9% of all cases (2,465), while the remaining were locally acquired. There were three waves of COVID-19 in the first 300 days of the pandemic. However, it was the fourth wave, which started after day 301 (26th October 2020), that contributed the largest number of cases. Fifty-five percent (6,522/11,818) of confirmed cases were diagnosed from day 301 to 500, of which 4,731 (72.5%) were locally acquired (Figure 1). Among 11,818 COVID-19 cases, SARS-CoV-2 VOCs were found in 271 (2.3%). Except for the 10 cases (case 2 to 11, Table 3) acquired in the local community, all SARS-CoV-2 VOCs were imported or epidemiologically related to cases detected at Hong Kong International Airport or the designated quarantine hotels.
Figure 1.
Evolving epidemic of coronavirus disease 2019 (COVID-19) in Hong Kong (from 26th October 2020, day 301 to 13th May 2021, day 500)
Note. The fourth wave of COVID-19 occurred between November 2020 and March 2021.
Table 3.
Epidemiological analysis of a cluster of 11 patients with SARS-CoV-2 VOC B.1.351 in Hong Kong
| Case | Sex/Age | Clinical symptomsa (date) | Epidemiological background | Source of acquisition | Date of diagnosisb | Reason for testing | Diagnosis after first exposurec (day) | Total number of contact to be quarantined for 21 days among household members or household gathering, (workplace), and [residential building]; remark |
|---|---|---|---|---|---|---|---|---|
| Case 1 [11643] |
M/29 | Nil | Travelling from Dubai | Quarantine hoteld | 17th Apr 2021 | Attend CTC for COVID-19 test for departure from HK | 24 | 163: 1, (42) [120]e |
| Case 2 [11672] |
F/31 | Nil | Friend of case 1; working as clinic nurse in HK | Household | 18th Apr 2021 | Close contact to case 1 | 11 | 106: 6, (100); Contact of residential building: same as case 1 |
| Case 3 [11773] |
F/39 | Cough (23 Apr 2021) |
FDH working in Lantau island, HK | Social gatheringf | 30th Apr 2021 | Respiratory symptoms | 8 | 1057: 3, [1054]; CTN to all 0.37 million FDHs working in HKg |
| Case 4 [11774] |
F/10 months | Diarrhea (29 Apr 2021) | Cared by case 3 | Household | 30th Apr 2021 | Close contact to case 3 | 9 | Contact of residential building: same as case 3 |
| Case 5 [11792] |
F/36 | Nil | Mother of case 4 and household member of case 3 | Household | 5th May 2021 | Close contact to case 3 | 15 | Contact of residential building: same as case 3 |
| Case 6 [11793] |
F/46 | Nil | FDH working in Eastern district, HK | Social gatheringf | 5th May 2021 | CTN to all FDHs in HK | 18 | 516: 7, [509] |
| Case 7 [11797] |
F/38 | Nil | FDH working in Southern district, HK | Social gatheringf | 5th May 2021 | CTN to all FDHs in HK | 18 | 123: 4, [119] |
| Case 8 [11800] |
F/67 | Nil | Mother of case 2 | Social gatheringh | 7th May 2021 | Retrospective contact tracingi | 25 | 1: 1 |
| Case 9 [11815] |
M/42 | Nil | Brother of case 2 | Social gatheringf,h | 12th May 2021 | Retrospective contact tracingi | 30 | 110: 3, [107] |
| Case 10 [11816] |
F/40 | Nil | Girlfriend of case 9 | Social gatheringf,h | 13th May 2021 | Retrospective contact tracingi | 31 | Nil |
| Case 11 [11825] |
M/4 months | Nil | Son of case 10 | Social gatheringf,h | 16th May 2021 | Retrospective contact tracingi | 35 | Nil |
Note. CTC, community testing center; CTN, compulsory testing notice; FDH, foreign domestic helper; HK, Hong Kong.
Clinical symptoms suggestive of COVID-19 were reported and non-specific clinical manifestation was not included.
The date of official report by Centre for Health Protection, Hong Kong (https://www.chp.gov.hk/files/xls/previous_cases_covid19_en.xlsx).
Either attending an event of social gathering with exposure to COVID-19 case or being household member with exposure to COVID-19 case.
An imported case (M/28) from Philippine stayed in the adjacent room with case 1 in the quarantine hotel for 13 days (from 25th March 2021 to 6th April 2021). Whole genome sequencing showed that this imported case was the ancestor of the community outbreak of SARS-CoV-2 VOC B.1.351 in Hong Kong.
Since all 120 persons staying in the residential building of the first 2 cases of SARS-CoV-2 VOC B.1.351 (case 1 and 2) were not infected during quarantine period, the non-household resident would be subjected to compulsory testing on the 3rd, 7th, 12th, and 19th day after isolation of the confirmed case of SARS-CoV-2 VOC B.1.351 without an epidemiological source. Quarantine of the all residents in the residential building for 21 days would be enforced if there were more than one case of SARS-CoV-2 VOC B.1.351 without epidemiological link.
Social gathering of cases 3, 6, 7, 9, 10 and 11 in the apartment of case 9 (No. 37 Fuk Wing Street) with alcohol consumption on 18th April 2021.
Compulsory testing for COVID-19 could be exempted for FDHs who had received two doses of COVID-19 vaccine for 14 days.
Social gathering of cases 1, 2, 8, 9, 10 and 11 in the apartment of case 8 (Fung Hing House, Hing Wah II Estate) without alcohol consumption on 13th April 2021 but case 1 & 2 did not disclose this information until 5th May 2021. Therefore, contact tracing could not be performed timely for identification of case 8, 9, 10, and 11.
The case was retrospectively identified when case 1 and 2 disclosed the events of social gathering.
The first case of SARS-CoV-2 VOC B.1.351 (index, case 1) detected in the community was an asymptomatic 29-year old male traveler from Dubai, who was tested positive in the community treatment center on day 473 (16th April 2021), 9 days after completion of 21 days of quarantine in one of the designated hotels in Hong Kong. The source of acquisition was postulated to be due to airborne transmission inside the quarantine hotel.23 Contact tracing was conducted per protocol. A female friend of the index case who did not have travel history but shared accommodation with the index case after his completion of quarantine was defined as close contact and diagnosed to have asymptomatic SARS-CoV-2 VOC B.1.351 infection one day later (case 2). 120 residents and workers in the residential building were sent to a quarantine center for 21 days. None of the residents under quarantine and persons subjected to compulsorily testing based on contact tracing had positive results. General population exposed to the other premises that the cases attended, including restaurants, shopping malls, and workplaces were subjected to compulsory testing in the community testing centers.
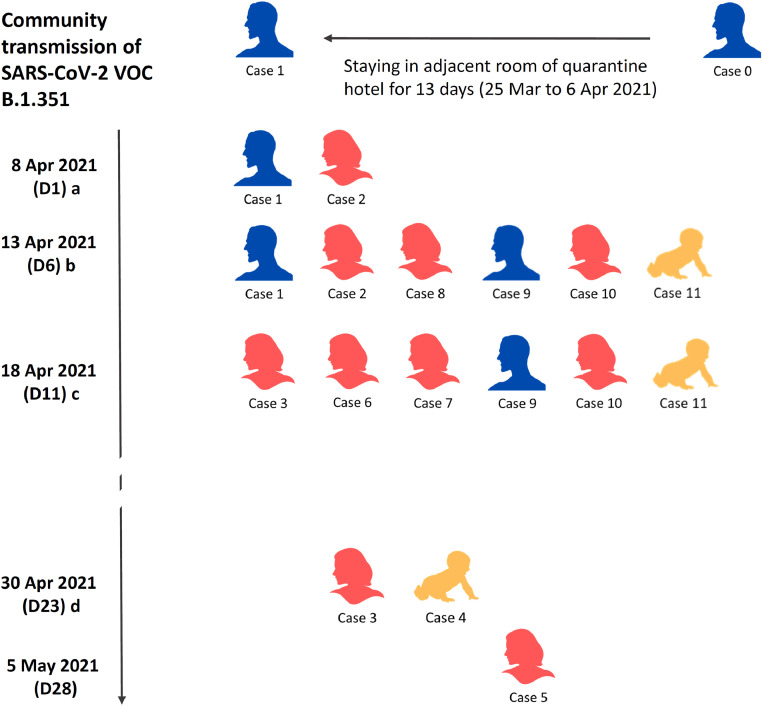
Another symptomatic SARS-CoV-2 VOC B.1.351 case in the community was identified on day 487 (30th April 2021), 13 days after the diagnosis of case 1 (Table 3). This case, designated case 3, was a 39-year old foreign domestic helper (FDH), who had no apparent epidemiological link with either case 1 or case 2. The geographic distance between the residences of case 1 and case 3 were 32 km. Since FDHs always gather during the weekends, compulsory testing notice was issued to all 0.34 million FDHs, who were tested for SARS-CoV-2 by RT-PCR between 1st May and 9th May 2021. Exemption was given to 0.03 million of FDHs who had completed two doses of COVID-19 vaccine at least 14 days beforehand. Two more FDHs were diagnosed by mass testing on day 492 (5th May 2021). All these cases were phylogenetically linked to case 1 and 2. On further questioning, they later admitted that they attended social gatherings on 13th April 2021, leading to further contact tracing per protocol which revealed a total of 10 secondary cases of SARS-CoV-2 VOC B.1.351 in this cluster (Figure 2). As for the possible source of this outbreak, a person (potential case 0) staying in the adjacent room of case 1 in the quarantine hotel was diagnosed to have SARS-CoV-2 VOC B.1.351. Case 1 and 2 were charged with infringement of Cap. 599D for failure of disclosure of information (Table 2).
Figure 2.
Community transmission of SARS-CoV-2 VOC B.1.351 in Hong Kong
Note. D, represent day of commencement of community transmission of SARS-CoV-2 VOC B.1.351. a) Case 1 and 2 were staying together as household contact & visiting many places in Hong Kong since 8 Apr 2021; diagnosis of COVID-19 on 17th April & 18th April 2021 respectively. b) Retrospectively recognized social gathering at home of case 8. c) Retrospectively recognized social gathering at home of case 9. d) Diagnosis of symptomatic case 3 and 4 activated contact tracing and mass testing to recognize case 5, 6, & 7 prospectively, and case 8, 9, 10, & 11 retrospectively.
During the contact tracing, a total of 2076 persons who were household contacts, workplace contacts, attendees at household gatherings or who had stayed in the same residential buildings were quarantined, and 7 (0.34%) of them were confirmed to be infected with SARS-CoV-2 B.1.351 during the quarantine period. The clinical attack rate among household contacts was significantly higher than that with non-household exposure (7/25, 28% vs 0/2051, 0%; p<0.001).
Based on the contact tracing and mass testing of 0.47 million of general population and 0.34 FDHs, a total of 10 secondary cases were identified in this first cluster of community outbreak of COVID-19 VOC in Hong Kong. Of these 11 cases (one index case and 10 secondary cases), the median time from exposure to diagnosis was 18 days (range: 8 – 35 days). The outbreak was successfully controlled without further dissemination 21 days after the last confirmed case.
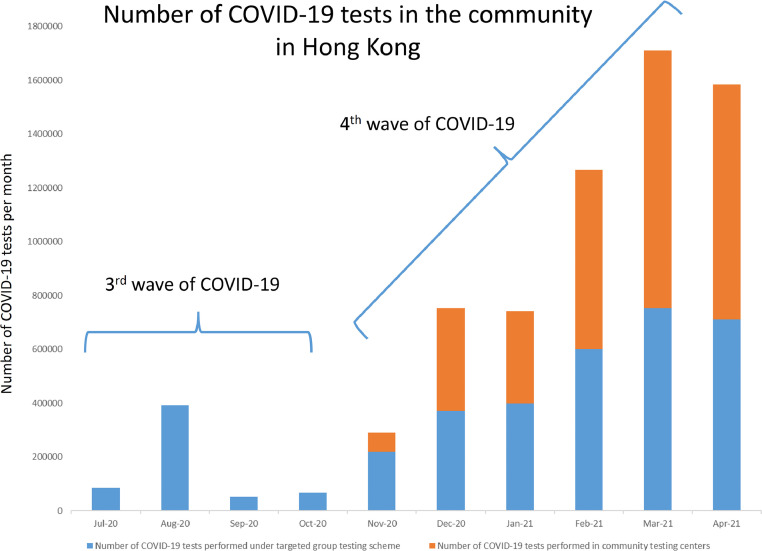
Alongside the large number of COVID-19 testing under the scheme specified by the government,12 the number of self-paid voluntary testing in the community also had a sharp rise since the 4th wave. Figure 3 shows the number of COVID-19 tests performed in the community per month in Hong Kong.
Figure 3.
Number of COVID-19 tests in the community in Hong Kong
3.2. Whole genome phylogenetic analysis
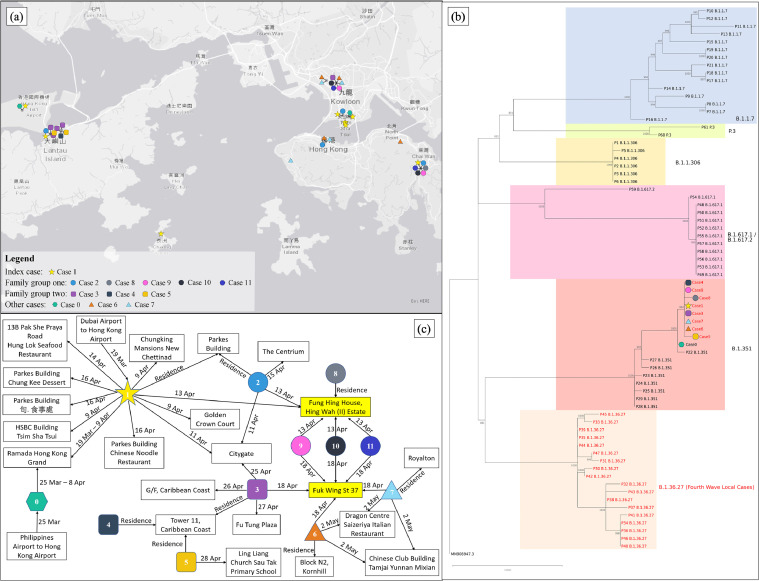
Whole genome sequencing was conducted for all the 11 cases as soon as the diagnosis of COVID-19 was confirmed. Unfortunately, the viral genome of three cases (i.e. cases 2, 10 and 11) could be not obtained because of low viral load in their respiratory specimens (CT value >38.0). Comparative genomic analysis revealed that the remaining eight cases shared six unique single nucleotide polymorphisms (SNPs), namely 2305 g>t (Orf1a K680N), 5941 t>g (Orf1a I1892M), 13011 c>t (Orf1a T4249I), 17127 c>t, 24932 g>t (S G1124C), and 25333 t>c. These mutations were rarely found in other sequences publicly available at GISAID as of 13th May 2021. Phylogenetic analysis also showed that these eight cases formed a cluster and were segregated from the other 62 cases collected over the same period (i.e. April – May 2021) (Figure 4a), supporting that these cases were infected by the same SARS-CoV-2 strain and likely belonged to the same transmission chain.
Figure 4.
Phylogeographic analysis of the genomic and spatial relationship among the patients with SARS-CoV-2 VOC B.1.351 in Hong Kong. (a) A geographic map of Hong Kong illustrated the locations of the premises visited by the patients. Cases were linked up with black lines if they visited the same premise on the same day. (b) A phylogenetic tree involved 70 COVID-19 cases identified in April 2021. The tree was rooted on the earliest published genome (accession no.: MN_908947.3). The cases written in red indicated locally-acquired cases, whereas the cases written in black were imported cases. The letters on the right were the PANGO lineages of the cases in the respective colored boxes. The cases of concerns in this study were donated by the same symbols used in (a). Please note that the genomes of cases 2, 10 and 11 were not available as viral loads in their specimens were too low (Ct value >38) to be sequenced. (c) A linkage chart displayed spatial relationships among the patients with SARS-CoV-2 VOC B.1.351. The date on solid line indicated when the patient visited the respective premises. The boxes highlighted in yellow indicated the premises where some of the patients had gathering and direct transmission was believed to occur.
3.3. Geo-temporal analysis
Initially, there was no apparent epidemiological linkage between cases 1 and 2 and the FDHs (i.e. cases 3, 6 and 7). However, with the support of phylogenetic evidence, the cases were re-questioned about the premises that they had visited during the incubation period. A total of 41 premises were eventually identified. The location of these premises and their associated cases are shown in Figure 4b. A linkage chart was used to illustrate the spatial and temporal relationships between the premises and the cases (Figure 4c). Case 1 has the highest degree of centrality (n=12) among all the cases. Based on the combined phylogenetic, epidemiological and geo-temporal analysis, we assumed that case 1 was the index case of this transmission cluster. Among the premises, Fung Hing House, Hing Wah II Estate and No. 37 Fuk Wing Street have the highest degree of centrality (n=6). This is supported by the fact that 8 cases attended social gatherings including mask-off activities at two of the premises (Fung Hing House and No. 37 Fuk Wing Street). On 13th April 2021, case 1 had gathering with case 2 and her family members (i.e. cases 8-11) at Fung Hing House. Later, the three confirmed family members of case 2 had a party gathering with the FDHs, cases 3, 6 and 7, at No. 37 Fuk Wing Street on 18th April 2021. Case 3 then further infected her employer and her 10-month-old baby (i.e. cases 4 and 5) at their residence. Based on the combined epidemiological and geo-temporal analysis, we believed that viral transmission occurred in these premises.
Discussion
Transmission of SARS-CoV-2 remains uncontrolled in many countries despite the implementation of border control, public health measures in the community, and infection control measures in the healthcare settings. With the emergence of SARS-CoV-2 VOCs, the control of COVID-19 becomes even more challenging. The presence of N501Y mutation on the spike protein, which is shared by the beta variant (B.1.351), alpha variant (B.1.1.7), and gamma variant (P.1), likely increases the transmissibility by increasing the binding of SARS-CoV-2 virion to the cell receptor ACE2. The B.1.351 and P.1 variants also possess the E484K mutation, which decreases the affinity of the neutralizing antibodies, and may result in immune escape and reinfection.24 The recent emergence of the delta variant (B.1.167) caused an unprecedented outbreak in India with over 0.4 million new case per day, resulting in a humanitarian catastrophe.25 In Hong Kong, we have faced four waves of attack with over 11,000 confirmed cases in the past 500 days. Each wave was caused by unrecognized imported cases, initially from mainland China, and subsequently from overseas, leading to community transmission and local outbreaks by a predominating strain.17,26 Non-pharmaceutical inventions, including universal masking, social distancing, and closure of school and certain business with high risk of transmission such as bars and eateries, played an important role in the control of each wave, in addition to isolation of cases and quarantine of contacts.27 Since SARS-CoV-2 VOCs were not previously reported in the local case in Hong Kong, it is of utmost importance to prevent the importation of SARS-CoV-2 VOCs, which may potentially cause the 5th wave of COVID-19.
Therefore, when the first SARS-CoV-2 VOC B.1.351 (index case) was recognized in the community, contact tracing and mass testing was implemented in the community. While contact tracing is commonly applied during infectious disease outbreaks,28 mass testing is an underexplored strategy for COVID-19 control.29 The strategy of mass testing by RT-PCR was adopted in the endemic communities,30 as well as during institutional outbreaks in hospitals,31 long term care facilities or care home for the elderly,32,33 and prisons,34 with a testing capacity ranging from 300-6000 in institutional settings. In this SARS-CoV-2 VOC B.1.351 epidemic in Hong Kong, we implemented an aggressive approach of mass testing in the community soon after local transmission was identified. All persons attending any premises such as residential buildings, schools, shopping malls, restaurants, and other public and private facilities in the community where the confirmed cases had visited, were subjected to compulsory testing. In addition, under the restriction-testing declaration, personal movement in the concerned premises was restricted until all persons were tested for SARS-CoV-2 in the on-site mobile testing center arranged by the government. All FDHs were subjected to compulsory testing, unless they have completed two doses of COVID-19 vaccine, because of the finding of SARS-CoV-2 VOC with unknown epidemiological link in an FDH. A total of 0.34 million FDHs were tested in the community testing centers within 9 days, which was an unprecedented measure in the literature. With this mass screening, another two FDHs with no obvious epidemiological link carrying SARS-CoV-2 VOC B.1.351 were identified.
Using whole genome sequencing, the SARS-CoV-2 sequences of the index case and all three FDHs were shown to be identical. The index case could no longer deny the attendance of social gatherings during the incubation period. This further piece of history helped to identify the other secondary cases in this cluster (Figure 2). Failure of disclosure of epidemiological exposure jeopardizes the contact tracing and outbreak control. In a modelling study, optimizing testing and tracing coverage, and minimizing tracing delays could enhance contact tracing effectiveness with the potential of preventing up to 80% of all transmissions.35 Timely use of whole genome sequencing can greatly facilitate outbreak investigation, not only to understand the cryptic chain of transmission,36 but also to explore the possible mode of transmission.37 The source of SARS-CoV-2 VOC B.1.351 acquisition for the index case remains to be resolved. When he was under quarantine in the designated hotel, a person staying in the adjacent room was diagnosed to have SARS-CoV-2 VOC B.1.351 (potential case 0). Airborne transmission of COVID-19 inside the quarantine hotel was postulated.23
In this instance, the community transmission of SARS-CoV-2 VOC B.1.351 was successfully brought under control, partly due to the timely mobilization of mass testing and rapid application of whole genome sequencing, on top of the previously implemented public health measures. Despite a long lag period from exposure to diagnosis (median 18 days) and the well-known presence of pre-symptomatic transmission for SARS-CoV-2, only household close contacts but not workplace contacts were infected in this cluster, likely due to a higher degree of exposure in home settings and good compliance with masking at workplace. The predominance of household transmission is evident since the number of secondary cases due to household contact was significantly higher than that due to non-household contact.38 Mask-off settings during household and social gatherings also increased risk of COVID-19 transmission and should not be overlooked.39,40 Despite the potential increased transmissibility of SARS-CoV-2 VOC B.1.351, the current policy of contact tracing complemented by mass testing, along with the prevailing public health measures were able to contain this community outbreak in a timely fashion.
There are several limitations in this study. Firstly, we did not perform case-control analysis to identify the risk factors for community acquisition of SARS-CoV-2 VOC B.1.351 in this outbreak. As the primary goal of contact tracing and mass testing was to control the community outbreak, the detailed epidemiological data of the persons who were tested negative were not obtained. Secondly, we did not address the cost effectiveness of contact tracing and mass testing. However, the cost saving in terms of reduction in hospital admissions, minimization of salary lost for those who undergo compulsory quarantine, and prevention of economic lost if the outbreak was not controlled in a timely fashion likely outweighs the expenditure of contact tracing and mass testing.
Research in context
Evidence before this study
Public health measures, including universal masking, social distancing, contact tracing, and quarantine of close contacts, have played an important role in the control of community transmission of SARS-CoV-2. Mass testing has been conducted in certain areas, but its role as an effective measure for COVID-19 control is less established. We searched PubMed without language restrictions on 10th May 2021 for articles using the term “mass testing” and the terms “COVID-19” or “SARS-CoV-2”. Most of the studies were conducted in the areas with endemic COVID-19 transmission in the community, or for outbreak control in hospitals, long term care facilities, care homes for the elderly, and prisons. The number of persons recruited in mass testing in the outbreak cases were in the range of 300 to 6000. None of these studies addressed the control of the emerging SARS-CoV-2 VOCs in low incidence areas of COVID-19.
Added value of this study
In Hong Kong, we have intensified the control measures for inbound travelers in response to the global spread of SARS-CoV-2 VOCs. They are subjected to mandatory nucleic acid testing for SARS-CoV-2 at Hong Kong International Airport and compulsory quarantine for 21 days in the designated hotels to minimize the risk of importation and subsequent community spread of SARS-CoV-2 VOCs. When we recognized the first incidence of community transmission of SARS-CoV-2 VOC B.1.351, mass testing of 0.47 million of the general population and 0.34 million foreign domestic helpers was conducted within 1 month, in addition to contact tracing, quarantine of close contacts, and timely use of whole genome sequencing. With these measures in place, the epidemic of SARS-CoV-2 VOC B.1.351 was successfully contained in Hong Kong.
Implications of all available evidence
In view of the increased transmissibility of SARS-CoV-2 VOCs, explosive outbreak of COVID-19 can easily occur in low incidence areas when there is an undetected imported case. Mass testing can be a useful strategy, especially if it is targeted to the specific group of people with common exposure to premises where the confirmed COVID-19 case has visited or resided in.
Author's contribution
VC-CC, GK-HS, S-CW, and K-YY had roles in study design, data analysis, literature search, and writing up of the manuscript. VC-CC, S-CW, AK-WA, CS-FN, CH, S-KC, and K-YY had roles in outbreak investigation. GK-HS, DCL, HT, and KK-WT had roles in whole genome sequencing and phylogenetic analysis. L-KL, JS-LL, KKL, HW-HL, and EY-KW had roles in laboratory work. L-KL had role in spatial geographic analysis. LX, SL, BH-SL, W-KT, RAL, and MY-WK had roles in collection of patient specimens. All authors reviewed and approved the final version of the manuscript.
Funding
This study was partially supported by the Health and Medical Research Fund (HMRF) Commissioned Research on Control of Infectious Disease (Phase IV), CID-HKU1-2 and CID-HKU1-16, and HMRF Commissioned Research on COVID-19, COVID190204, Food and Health Bureau, Hong Kong SAR Government.
Data sharing
Data are available upon reasonable request.
Declaration of Competing Interest
All authors declare no conflict of interest
Acknowledgement
We thank our frontline staff and management team of Centre for Health Protection, Department of Health and Hospital Authority to facilitate this study.
References
- 1.The Centre for Health Protection closely monitors cluster of pneumonia cases on Mainland. Press release of the Department of Health. Hong Kong Special Administrative Region. Available at. 2019 https://www.info.gov.hk/gia/general/201912/31/P2019123100667.htm Accessed on 25th May 2021. [Google Scholar]
- 2.World Health Organization. COVID-19 Weekly Epidemiological Update. 16 May 2021. Available at file:///C:/Users/Vincent%20CHENG/Downloads/20210518_Weekly_Epi_Update_40.pdf. Accessed on 25th May 2021.
- 3.Burns J, Movsisyan A, Stratil JM, Biallas RL, Coenen M, Emmert-Fees KM. International travel-related control measures to contain the COVID-19 pandemic: a rapid review. Cochrane Database Syst Rev. 2021;3 doi: 10.1002/14651858.CD013717.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong SC, Leung M, Lee LL, Chung KL, Cheng VC. Infection control challenge in setting up a temporary test centre at Hong Kong International Airport for rapid diagnosis of COVID-19 due to SARS-CoV-2. J Hosp Infect. 2020;105:571–573. doi: 10.1016/j.jhin.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siu GK, Lee LK, Leung KS, Leung JS, Ng TT, Chan CT. Will a new clade of SARS-CoV-2 imported into the community spark a fourth wave of the COVID-19 outbreak in Hong Kong? Emerg Microbes Infect. 2020;9:2497–2500. doi: 10.1080/22221751.2020.1851146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hong Kong, China, extends quarantine period for most inbound travelers effective Dec. 25. Available at https://www.garda.com/crisis24/news-alerts/421761/china-officials-extend-quarantine-period-for-most-inbound-travelers-effective-dec-25-entry-banned-for-travelers-from-south-africa-update-45. Accessed on 25th May 2021.
- 7.COVID-19 Thematic Website. Centre for Health Protection. Department of Health. The Government of the Hong Kong Special Administrative Region. Available at https://www.coronavirus.gov.hk/eng/index.html. Accessed on 25th May 2021.
- 8.Wong SC, Leung M, Tong DW, Lee LL, Leung WL, Chan FW. Infection control challenges in setting up community isolation and treatment facilities for patients with coronavirus disease 2019 (COVID-19): Implementation of directly observed environmental disinfection. Infect Control Hosp Epidemiol. 2020:1–9. doi: 10.1017/ice.2020.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheng VCC, Wong SC, To KKW, Ho PL, Yuen KY. Preparedness and proactive infection control measures against the emerging novel coronavirus in China. J Hosp Infect. 2020;104:254–255. doi: 10.1016/j.jhin.2020.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheng VCC, Wong SC, Chen JHK, Yip CCY, Chuang VWM, Tsang OTY. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020;41:493–498. doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng VCC, Wong SC, Chuang VWM, So SYC, Chen JHK, Sridhar S. Absence of nosocomial transmission of coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in the prepandemic phase in Hong Kong. Am J Infect Control. 2020;48:890–896. doi: 10.1016/j.ajic.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheng VC, Wong SC, Tong DW, Chuang VW, Chen JH, Lee LL. Multipronged infection control strategy to achieve zero nosocomial coronavirus disease 2019 (COVID-19) cases among Hong Kong healthcare workers in the first 300 days of the pandemic. Infect Control Hosp Epidemiol. 2021:1–10. doi: 10.1017/ice.2021.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheng VC, Wong SC, Chuang VW, So SY, Chen JH, Sridhar S. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J Infect. 2020;81:107–114. doi: 10.1016/j.jinf.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Compulsory testing notice. Centre for Health Protection. Department of Health. The Government of the Hong Kong Special Administrative Region. Available at https://www.coronavirus.gov.hk/eng/compulsory-testing.html#compulsory-testing. Accessed 30th May 2021.
- 15.Restriction-testing declaration. Centre for Health Protection. Department of Health. The Government of the Hong Kong Special Administrative Region. Available at https://www.coronavirus.gov.hk/eng/compulsory-testing.html#Restriction-testing-declaration. Accessed 30th May 2021.
- 16.To KK, Tsang OT, Leung WS, Tam AR, Wu TC, Lung DC. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20:565–574. doi: 10.1016/S1473-3099(20)30196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan WM, Ip JD, Chu AW, Tse H, Tam AR, Li X. Phylogenomic analysis of COVID-19 summer and winter outbreaks in Hong Kong: An observational study. Lancet Reg Health West Pac. 2021;10 doi: 10.1016/j.lanwpc.2021.100130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Loman N, Rambaut A. nCoV-2019 novel coronavirus bioinformatics protocol. 2020. Available at https://artic.network/ncov-2019/ncov2019-bioinformatics-sop.html. Accessed 10th May 2021.
- 19.Katoh K, Standley DM. MAFFT multiple sequence alignment software version 7: improvements in performance and usability. Mol Biol Evol. 2013;30:772–780. doi: 10.1093/molbev/mst010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guindon S, Lethiec F, Duroux P, Gascuel O. PHYML Online–a web server for fast maximum likelihood-based phylogenetic inference. Nucleic Acids Res. 2005;33:W557–W559. doi: 10.1093/nar/gki352. Web Server issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Government of the Hong Kong Special Administrative Region. Data in Coronavirus Disease (COVID-19). Available at https://chp-dashboard.geodata.gov.hk/covid-19/en.html. Accessed 20th May 2021.
- 22.Leung YF, Wong HB, Shing Y, Wong HW, Wong WK. wars.vote4.hk - Coronavirus in HK. 2020. Available at https://wars.vote4.hk/en/. Accessed 20th May 2021.
- 23.Wong SC, Chen H, Lung DC, Ho PL, Yuen KY, Cheng VC. To prevent SARS-CoV-2 transmission in designated quarantine hotel for travelers: Is ventilation system a concern? Indoor Air. 2021;31:1295–1297. doi: 10.1111/ina.12870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boehm E, Kronig I, Neher RA, Eckerle I, Vetter P, Kaiser L. Geneva Center for Emerging Viral Diseases. Novel SARS-CoV-2 variants: the pandemics within the pandemic. Clin Microbiol Infect. 2021 doi: 10.1016/j.cmi.2021.05.022. S1198-743X(21)00262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rahman N. International aid and covid-19 in India: a humanitarian catastrophe at risk of a familiar response. BMJ. 2021;373:n1362. doi: 10.1136/bmj.n1362. [DOI] [PubMed] [Google Scholar]
- 26.To KK, Chan WM, Ip JD, Chu AW, Tam AR, Liu R. Unique SARS-CoV-2 clusters causing a large COVID-19 outbreak in Hong Kong. Clin Infect Dis. 2020;73:137–142. doi: 10.1093/cid/ciaa1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cowling BJ, Ali ST, Ng TWY, Tsang TK, Li JCM, Fong MW. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5:e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Megnin-Viggars O, Carter P, Melendez-Torres GJ, Weston D, Rubin GJ. Facilitators and barriers to engagement with contact tracing during infectious disease outbreaks: A rapid review of the evidence. PLoS One. 2020;15 doi: 10.1371/journal.pone.0241473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shen M, Xiao Y, Zhuang G, Li Y, Zhang L. Mass testing-An underexplored strategy for COVID-19 control. Innovation (N Y) 2021;2 doi: 10.1016/j.xinn.2021.100114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shi Q, Hu Y, Peng B, Tang XJ, Wang W, Su K. Effective control of SARS-CoV-2 transmission in Wanzhou, China. Nat Med. 2021;27:86–93. doi: 10.1038/s41591-020-01178-5. [DOI] [PubMed] [Google Scholar]
- 31.Porru S, Carta A, Monaco MGL, Verlato G, Battaggia A, Parpaiola M. Health Surveillance and Response to SARS-CoV-2 Mass Testing in Health Workers of a Large Italian Hospital in Verona, Veneto. Int J Environ Res Public Health. 2020;17:5104. doi: 10.3390/ijerph17145104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Louie JK, Scott HM, DuBois A, Sturtz N, Lu W, Stoltey J. San Francisco Department of Public Health COVID-19 Skilled Nursing Facility Outbreak Response Team. Lessons from Mass-Testing for COVID-19 in Long Term Care Facilities for the Elderly in San Francisco. Clin Infect Dis. 2020;72:2018–2020. [Google Scholar]
- 33.Tang S, Sanchez Perez M, Saavedra-Campos M, Paranthaman K, Myers R. Mass testing after a single suspected or confirmed case of COVID-19 in London care homes, April-May 2020: implications for policy and practice. Age Ageing. 2021;50:649–656. doi: 10.1093/ageing/afab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hagan LM, Williams SP, Spaulding AC, Toblin RL, Figlenski J, Ocampo J. Mass Testing for SARS-CoV-2 in 16 Prisons and Jails - Six Jurisdictions, United States, April-May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1139–1143. doi: 10.15585/mmwr.mm6933a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kretzschmar ME, Rozhnova G, Bootsma MCJ, van Boven M, van de Wijgert JHHM, Bonten MJM. Impact of delays on effectiveness of contact tracing strategies for COVID-19: a modelling study. Lancet Public Health. 2020;5:e452–e459. doi: 10.1016/S2468-2667(20)30157-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Borges V, Isidro J, Macedo F, Neves J, Silva L, Paiva M. Nosocomial Outbreak of SARS-CoV-2 in a "Non-COVID-19" Hospital Ward: Virus Genome Sequencing as a Key Tool to Understand Cryptic Transmission. Viruses. 2021;13:604. doi: 10.3390/v13040604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cheng VC, Fung KS, Siu GK, Wong SC, Cheng LS, Wong MS. Nosocomial outbreak of COVID-19 by possible airborne transmission leading to a superspreading event. Clin Infect Dis. 2021:ciab313. doi: 10.1093/cid/ciab313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Luo L, Liu D, Liao X, Wu X, Jing Q, Zheng J. Contact Settings and Risk for Transmission in 3410 Close Contacts of Patients With COVID-19 in Guangzhou, China: A Prospective Cohort Study. Ann Intern Med. 2020;173:879–887. doi: 10.7326/M20-2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lam HY, Lam TS, Wong CH, Lam WH, Mei ELC, Kuen YLC. A superspreading event involving a cluster of 14 coronavirus disease 2019 (COVID-19) infections from a family gathering in Hong Kong Special Administrative Region SAR (China) Western Pac Surveill Response J. 2020;11:36–40. doi: 10.5365/wpsar.2020.11.1.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Martín-Sánchez M, Lim WW, Yeung A, Adam DC, ST Ali, Lau EHY. COVID-19 transmission in Hong Kong despite universal masking. J Infect. 2021;83:92–95. doi: 10.1016/j.jinf.2021.04.019. S0163-4453(21)00205-X. [DOI] [PMC free article] [PubMed] [Google Scholar]