Abstract
Background
The majority of medical students in China have experienced home confinement and a reliance on online resources to study medicine since the outbreak of COVID-19. More time spent studying online during the COVID-19 pandemic may be a potential risk factor for problematic smartphone use, since smartphones have become the most commonly used device for accessing the internet. The objective of the present study was to explore the association between anxiety, smartphone problematic use and sleep disturbance among medical students during the enforced COVID-19 home confinement.
Methods
Altogether, 666 medical students validly answered a self-administered questionnaire, which included the Chinese version of the Generalized Anxiety Disorder scale, Smartphone addiction scale - short version, and the PROMIS Sleep Disturbance scale (short form). Hierarchical multiple regression analyses were employed to explore the associated factors of anxiety. Structural equation modeling was conducted to test hypothesized associations.
Results
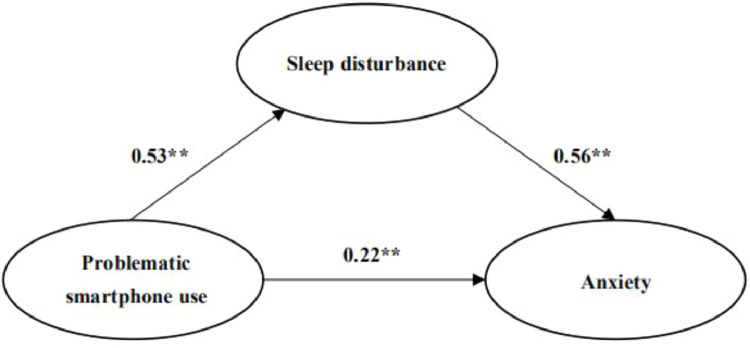
Anxiety was significantly associated with problematic smartphone use and sleep disturbance among medical students during the COVID-19 pandemic. Problematic smartphone use not only directly affected anxiety, but also exerted a significant indirect effect on anxiety via sleep disturbance. A significant decrease of the path coefficient of problematic smartphone use on anxiety (from β=0.53 to β=0.22, P<0.01) was observed with sleep disturbance being modeled as a mediator.
Limitations
Limitations include its cross-sectional design and samples recruited from only one medical school.
Conclusions
The detrimental impact of problematic smartphone use and the importance of sleep health on mitigating anxiety should be highlighted and incorporated into medical education.
Keywords: Anxiety, Sleep disturbance, Problematic smartphone use, Medical students, COVID-19, Structural equation modeling
Introduction
The majority of medical students around the world have experienced home confinement relying on online resources to study medicine remotely since the outbreak of the novel coronavirus disease 2019 (COVID-19) (Gill et al., 2020). As medical education was founded and developed on the basis of a highly-valued tradition of partnership, passing down knowledge and practical experience, the COVID-19 pandemic has induced substantial changes in medical education including the loss of routines, educational opportunities, and social connections (Gallagher and Schleyer, 2020). Feelings of anxiety and vulnerability, competing internally with a commitment to care for patients, are taking a serious toll on the psyche of medical students and trainees (Gallagher and Schleyer, 2020). A recent study conducted among undergraduates in a Chinese medical college reported that 24.9% of the participants experienced anxiety due to the pandemic of COVID-19 (Cao et al., 2020). In another cross-sectional survey conducted in Iran, 99% of the participating medical students reported suffering from extremely severe anxiety (Vahedian-Azimi et al., 2020).
During the 2020 spring semester, universities in China transformed the way that courses are traditionally taught and delivered live-streaming courses via various online platforms including Rain Classroom, Tencent Classroom, and Tencent Meeting in accordance with the China's Ministry of Education guidelines (Ministry of Education of China, 2020). These timely and effective policies played a significant role in preventing suspension in educational progress and ensuring the health and safety of all students and faculty during COVID-19 outbreak. However, an important unintended consequence of this policy is that the time spent studying online during the COVID pandemic may be a potential risk factor for problematic smartphone use, which could further result in negative psychological or behavioral disorders (Duan et al., 2020).
Problematic smartphone use among medical students has been found to be an emerging and widespread public health issue, leading to elevated risks of anxiety and sleep problems (Chen et al., 2017). Problematic smartphone use is conceptualized as an excessive and uncontrolled pattern of smartphone use, linked to functional impairment (Billieux et al., 2015). There has been accumulated evidence documenting that the use of blue light-emitting devices (e.g. smartphone) before sleep results in the disruption of the circadian clock causing cognitive stimulation and sleep disturbance (Jniene et al., 2019).
Sleep disturbance has been linked to anxiety, depression and suicidality. One of the methods to treat sleep disturbances is the alleviation of symptoms of psychiatric disorders (Sher, 2020). A recent longitudinal study conducted among undergraduate medical students in India revealed poor sleep increased levels of anxiety and stress symptoms during the COVID-19 pandemic (Saraswathi et al., 2020).
Despite the mounting evidence showing the association of sleep disturbance with anxiety and problematic smartphone use independently, research probing into the relationship that might exist between sleep disturbance, problematic smartphone use, and anxiety is scarce. A previous study among Chinese university students revealed that smartphone addiction could play an indirect effect on poor sleep quality via poor self-regulation (Zhang and Wu, 2020), while another recent study found that smartphone addiction mediated the relation between negative affect and sleep quality (Li et al., 2020). Although there has been empirical evidence indicating sleep disturbance as a mediator between smartphone use before sleep and psychological distress (Lemola et al., 2015) and on the association between adverse childhood experiences and psychological health outcomes and deficit in functions (Conway et al, 2020), no existing literature has examined sleep disturbance as a mediator in the relationship between problematic smartphone use and anxiety. Since the outbreak of the COVID-19 pandemic, evidence has accumulated showing a high rate of poor sleep quality, sleep loss, and insomnia among both the front-line medical staff (Lai et al., 2020, Zhang et al., 2020) and the general public (Cellini et al., 2020). There has not yet been research published on sleep disturbance among medical students during the COVID-19 pandemic. Medical students have been found to suffer increasing levels of anxiety due to the detrimental impact of the COVID-19 pandemic on their physical, emotional, and mental well-being (Chandratre, 2020). It is therefore imperative that educational authorities and frontline faculty provide effective and appropriate guidance for medical students to regulate their emotions and minimize educational losses during the COVID-19 pandemic. The objective of the present study was to explore the association between anxiety, problematic smartphone use and sleep disturbance among medical students who were studying online during the enforced COVID-19 home confinement, and to examine the mediating effect of sleep disturbance between problematic smartphone use and anxiety. This study hypothesized that (1) problematic smartphone use and sleep disturbance are positively associated with anxiety and (2) sleep disturbance plays a mediating role between problematic smartphone use and anxiety among medical students in China.
Methods
2.1. Study design and sample
This survey based on a cross-sectional design was carried out at a medical university in Shenyang, the largest city in the northeast of China, from the end of March to April 2020. This was the beginning of the spring semester during the COVID-19 pandemic when universities in China transformed the traditional classroom teaching according to China's Ministry of Education guidelines and delivered live-streaming courses via various online platforms. Ethical guidelines were strictly followed and the study protocol was scrutinized and approved by the institutional and national Committee on Human Experimentation. A self-administered questionnaire was distributed via Questionnaire Star (named “Wenjuanxing” in Chinese), a professional online survey tool widely used in China (Zhu et al., 2020). The questionnaire was completely anonymous and confidential, which took approximately 15 to 20 minutes to finish. First-year, second-year and third-year medical students were randomly selected from 24 classes (with 8 classes from each grade) of China Medical University, who were home-quarantined during the 2020 spring semester when courses of all universities in China were delivered online due to COVID-19. All the participants received a link to the questionnaire on their smartphones, which was sent by their teachers through WeChat and Tencent QQ, the most widely-used smartphone applications for communication in China. Participants started to fill in the questionnaire by clicking the link and submitted it by clicking the submit button upon completion. Before we started the investigation, we had preset the questionnaire so that it could not be submitted without being fully completed, which helps avoid the problem of missing values and does not allow for the possibility of incomplete, inconsistent and duplicate data. Before data analysis, we conducted a logic and data consistency test. The data consistency test was carried out after the elimination of the questionnaires with illogical answers, the result of which met the prerequisites of statistical analysis. All participants took part in the present study on a voluntary basis and had provided informed consent before they filled out the questionnaire. Fifty-four invalid questionnaires of the total responses (n=720) were eliminated. Our final sample, therefore, consisted of totally 666 medical students with a valid response rate of 92.5%.
2.2. Demographic characteristics of participants
Information on demographic data was gathered including age, gender, the year in which the medical student was in their training (freshman, sophomore or above), major (clinical medicine or other), level of education of both parents (secondary and below or junior college and above), total family income per month (≤5000 yuan or >5000 yuan). Questions with respect to online learning during the COVID-19 pandemic such as time spent learning online and adaptation to online classes were also included.
2.3. Measurement of Anxiety
Anxiety among medical students was evaluated by the Generalized Anxiety Disorder 7-item Scale (GAD-7), which provided a reliable and valid measure for general anxiety symptoms over the past two weeks (He et al., 2010). It consisted of 7 Likert-type items being scored from “not at all” to “nearly every day” that are scored from 0 to 3. A higher total score was indicative of a greater severity of anxiety. The Cronbach's alpha of GAD-7 was 0.941, which demonstrated good reliability.
2.4. Measurement of Problematic smartphone use
Problematic smartphone use was measured using the Chinese version of Smartphone addiction scale-short version (SAS-SV) (Chen et al., 2017). It assesses the presence of problematic smartphone use and smartphone-related functional impairment with 10 Likert-type items from “strongly disagree” to “strongly agree” that are scored from 1 to 6. The Chinese SAS-SV was a valid and reliable tool to measure problematic smartphone use, with good internal consistency and satisfactory test-retest reliability (Luk et al., 2018). The cut-off values of the Chinese SAS-SV were 31 for males and 33 for females in our study as proposed by the scale developers. The scale is used as a screening tool for identifying the risk of smartphone addiction and distinguish the high-risk population (Kwon et al., 2013). The higher the total scores, the higher degree of problematic smartphone use is represented. The internal consistency of this scale was 0.916.
2.5. Measurement of Sleep disturbance
Sleep disturbance was assessed with the PROMIS Sleep Disturbance scale (Short Form), which included 8 items scored on a 5-point scale evaluating the presence of sleep disturbance during the past week (Yu et al, 2011). A standardized T-score was obtained by converting the original total score of the 8 items, with higher scores representing more severe sleep disturbance (Hanish et al., 2017). The Cronbach's alpha of this scale was 0.884.
2.6. Statistical analysis
SPSS 17.0 was used for the statistical analyses and the statistical significance was determined with a two-tailed probability value of <0.05. Significant differences in anxiety among the categorical variables were tested using t-tests and one-way ANOVA. Descriptive statistics were calculated to summarize the distribution of demographic characteristics, problematic smartphone use, sleep disturbance, and anxiety. Correlations between problematic smartphone use, sleep disturbance, and anxiety were assessed using Spearman's correlation. The effects of demographic characteristics, problematic smartphone use and sleep disturbance on anxiety were measured using hierarchical regression analyses (HMR). Anxiety was the dependent variable and the independent variables were grouped into three blocks and put in the regression model successively: Step 1: demographic characteristics of medical students; Step 2: problematic smartphone use; Step 3: sleep disturbance. The contributions that the blocks of variables made to the HMR model were tested by entering them at later stages (Hong and Zhang, 2017). All variables involved in this study were standardized before being analyzed to explain scale differences.
The Amos 17.0 software was used for structural equation model (SEM) analyses to test whether sleep disturbance played a mediating role between problematic smartphone use and anxiety. Anxiety, sleep disturbance, and problematic smartphone use were modeled as the dependent variable, mediator variable, and independent variable, respectively. All indices involved in the SEM model exhibited good fitness with the SEM criteria (χ2/df < 5, RMSEA < 0.08, GFI > 0.90, CFI > 0.90, and TLI > 0.90). Evidence of the mediating effect was indicated by a decline in the direct path coefficient of problematic smartphone use on anxiety with sleep disturbance being added. The bootstrapping method was employed based on 5,000 samples. A bias-corrected and accelerated 95% confidence interval (BCa 95% CI) was estimated for a*b estimates and a two-tailed probability value of <0.05 was considered statistically significant.
Results
3.1. Description of the participants
Participants’ demographic characteristics and anxiety distribution in categorical variables are displayed in Table 1 . The majority of the 666 medical undergraduates were females 404 (60.7%) and 262 (39.3%) were males. The age distribution was even, as 315 (47.3%) were less than 20 years old, while 351 (52.7%) were 20 years old and above. Male students reported a significantly higher level of anxiety (P<0.01) compared with their female counterparts. Students who reported they had not adapted to online classes experienced significantly more severe anxiety (P<0.01) compared with those who have adapted.
Table 1.
Demographic characteristics and differences in anxiety among medical students (N=666).
| Variables | N(%) | AnxietyMean (SD) |
|---|---|---|
| Grade | ||
| Freshman | 278(41.7) | 2.74 (3.68) |
| Sophomore and above | 388(58.3) | 2.22 (3.29) |
| Gender | ||
| Male | 262(39.3) | 2.99 (4.02)** |
| Female | 404(60.7) | 2.08 (3.00) |
| Age | ||
| <20 | 315(47.3) | 2.37 (3.37) |
| ≥20 | 351(52.7) | 2.50 (3.55) |
| Fathers' education | ||
| Secondary and below | 369(55.4) | 2.46 (3.42) |
| Junior college and above | 297(44.6) | 2.41 (3.52) |
| Mothers’ Education | ||
| Secondary and below | 399(59.9) | 2.42 (3.35) |
| Junior college and above | 267(40.1) | 2.47 (3.64) |
| Monthly income | ||
| ≤5000 | 338(50.8) | 2.25 (2.99) |
| >5000 | 328(49.2) | 2.64 (3.89) |
| Profession | ||
| Clinical medicine | 460(69.1) | 2.38 (3.39) |
| Other | 206(30.9) | 2.57 (3.64) |
| Adapting to Online Classes | ||
| Yes | 592(88.9) | 2.07 (3.02) |
| No | 74(11.1) | 5.41 (5.03)** |
| Online learning time (hrs) | ||
| <6 | 411(61.7) | 2.60 (3.53) |
| ≥6 | 255(38.3) | 2.18 (3.34) |
*Significant at the 0.05 level (two-tailed)
⁎⁎ Significant at the 0.01 level (two-tailed)
3.2. Correlations between anxiety, problematic smartphone use and sleep disturbance
Table 2 demonstrates the means, standard deviations of continuous variables and results of the Spearman correlation analyses. As is shown in this table, both problematic smartphone use and sleep disturbance were significantly and positively correlated with anxiety (P<0.01).
Table 2.
Correlation analysis of anxiety and continuous variables.
| Mean (SD) | 1 | 2 | 3 | |
|---|---|---|---|---|
| 1. Anxiety | 2.44 (3.47) | 1 | ||
| 2. Problematic smartphone use | 38.72 (11.13) | 0.459** | 1 | |
| 3. Sleep disturbance | 14.94 (6.13) | 0.579** | 0.404** | 1 |
*Significant at the 0.05 level (two-tailed).
** Significant at the 0.01 level (two-tailed).
3.3. Hierarchical linear regression analysis of anxiety
Table 3 reveals results of the hierarchical multiple regression analyses for anxiety. Problematic smartphone use was significantly and positively associated with anxiety, contributing to 17.8% of the variance. Sleep disturbance was also significantly and positively associated with anxiety, accounting for an additional 14.6% of the variance. This study revealed that sleep disturbance might partially mediate the effect of problematic smartphone use on anxiety among Chinese medical undergraduates during the COVID-19 pandemic. The regression coefficient (β) for the association between problematic smartphone use and anxiety was reduced from 0.433 to 0.268 when sleep disturbance was added to the model.
Table 3.
The hierarchical linear regression analysis of anxiety.
| Anxiety |
|||
|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |
| Block 1 Demographic Characteristics |
|||
| Grade (Freshman vs. Sophomore and above) | -0.103* | -0.116** | -0.109** |
| Gender (male vs. female) | -0.081* | -0.107** | -0.061* |
| Age (<20 vs.≥20) | 0.051 | 0.082* | 0.083* |
| Fathers’ education (Secondary and below vs. Junior college and above) | -0.036 | -0.008 | -0.010 |
| Mothers’ Education (Secondary and below vs. Junior college and above) | 0.005 | 0.023 | 0.034 |
| Monthly income (≤5000 vs. >5000) | 0.065 | 0.054 | 0.038 |
| Major (Clinical medicine vs. Others) | 0.001 | -0.025 | -0.026 |
| Adapting to Online Classes(Yes vs. No) | 0.292** | 0.216** | 0.161** |
| Online learning time (<6 vs. ≥6) | -0.088* | -0.072* | -0.035 |
| Block 2 Problematic smartphone use | 0.433** | 0.268** | |
| Block 3 Sleep disturbance | 0.428** | ||
| R² | 0.117 | 0.295 | 0.441 |
| ΔR² | 0.117 | 0.178 | 0.146 |
*Significant at the 0.05 level (two-tailed); ** Significant at the 0.01 level (two-tailed)
3.4. Structural equation modeling of the mediating role of sleep disturbance between problematic smartphone use and anxiety
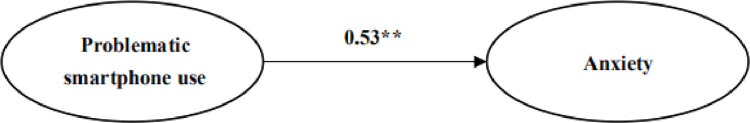
The results of SEM analysis are presented in Table 4 . The Sobel test was employed to confirm whether the mediating effect was statistically significant. A good fit of the proposed model to the observed data was obtained, which revealed that problematic smartphone use not only directly influenced anxiety, but also had a significant indirect effect on anxiety via sleep disturbance. Fig. 1 illustrates the direct pathway from problematic smartphone use to anxiety. As hypothesized, problematic smartphone use exerted a significantly positive influence on anxiety (β=0.53, P<0.01), which yielded a good fit to the data (χ2/df < 5, RMSEA = 0.047, CFI = 0.989, GFI = 0.957, AGFI = 0.974, and TLI = 0.985). Fig. 2 demonstrates the indirect pathway from problematic smartphone use to anxiety as mediated by sleep disturbance (c = 0.53, P<0.01), which exhibited goodness of fit (χ2/df < 5, P<0.05, GFI = 0.940, AGFI = 0.919, CFI = 0.973, TLI = 0.967, and RMSEA = 0.053). As is shown, sleep disturbance was significantly associated with both problematic smartphone use (β=0.53, P<0.01) and anxiety (β=0.56, P<0.01). A decrease of the path coefficient of problematic smartphone use on anxiety was observed (β=0.22, P<0.01) with sleep disturbance being modeled as a mediator. The bias-corrected and accelerated bootstrap method employed in this study demonstrated that sleep disturbance played a mediating role between problematic smartphone use and anxiety (a * b =0.31, BCa 95%, CI: 0.233∼0.363). The percentile 95% CI in this study was (0.233∼0.363), which is consistent with a bias-corrected 95% CI. For the indirect effect, the results confirmed the significant mediating effect of sleep disturbance (z=0.1899, P<0.001)
Table 4.
The path coefficients of the mediation model.
| B | β | S.E. | C.R. | P | |||
|---|---|---|---|---|---|---|---|
| Sleep disturbance | ← | Problematic smartphone use | 0.20 | 0.53 | 0.016 | 12.895 | <0.001 |
| Anxiety | ← | Sleep disturbance | 0.32 | 0.56 | 0.023 | 13.800 | <0.001 |
| Anxiety | ← | Problematic smartphone use | 0.05 | 0.22 | 0.009 | 5.701 | <0.001 |
Abbreviation: B: the unstandardized path coefficient. β: the standardized path coefficient. S.E.: the standard error. C.R.: the critical ratio.
Fig. 1.
Structural equation modeling of problematic smartphone use and anxiety.
Fig. 2.
Structural equation modeling of the mediating role of sleep disturbance between problematic smartphone use and anxiety.
Discussion
The objective of the present study was to explore the association between anxiety, problematic smartphone use and sleep disturbance among medical students who were studying online during the enforced COVID-19 home confinement, and to examine the mediating effect of sleep disturbance between problematic smartphone use and anxiety. This study fills a gap in existing literature. First, it probed into the association between anxiety, problematic smartphone use, and sleep disturbance among medical students who were studying online during the enforced COVID-19 home confinement. Second, it explored the mediating effect of sleep disturbance between problematic smartphone use and anxiety. Results from this study indicate that 17.9% of medical students in China experienced anxiety during COVID-19 home confinement, which was comparatively lower than that shown among medical students during the COVID-19 outbreak in Wuhan (24.9%) (Cao et al., 2020) and in Shanxi (22.1%) (Liu et al., 2020). One possible explanation might be that the present study was conducted in April 2020, which is later than the above-mentioned two studies and a time when China had brought the COVID-19 outbreak more under control with nationwide concerted efforts. This was consistent with findings from recent research showing that anxiety symptoms were less prevalent compared with that during the peak of the COVID-19 pandemic (Ran et al., 2020). Nonetheless, the prevalence rate of anxiety estimated in this study was much higher (7.7%) than was reported among university students (including both non-medical and medical students) in a cross-sectional study conducted across four universities in China from January to February 2020 (Wang et al., 2020). Undergraduate medical students in India also were reported in a prospective longitudinal study to have a high prevalence of anxiety during the COVID-19 home quarantine (Saraswathi et al., 2020). High prevalence rates of anxiety among medical students during the COVID-19 pandemic might partly result from their deeper understanding of the pandemic (Liu et al., 2020), their being a more exposed population to SARS-CoV-2, their having generally higher rates of depression and suicidal ideation, and their being less likely to seek psychological support (Schwenk et al, 2010). In addition, although systematic training and technical support for online teaching was provided by administrative departments at all levels during COVID-19 home confinement, there were still considerable challenges to achieving effective teaching outcomes. These challenges included limited online teaching experience among teaching staff, lack of effective monitoring of students’ participation in online learning environments, instability of network connectivity, and comparatively difficult internet accessibility in remote areas (Duan et al, 2020). The numerous challenges may have impaired the fulfillment of learning outcomes and given rise to anxiety among medical students under home confinement during the COVID-19 pandemic.
Results from this study indicated that problematic smartphone use exhibited a robust positive association with anxiety in the medical student population during COVID-19 home confinement. Smartphones have been increasingly used as an indispensable tool, not only for communicating, but also for educational purposes due to its convenient internet connectivity and user-friendly features providing easier access to study materials for students (Karki et al., 2020). The association between problematic smartphone use and anxiety could be bidirectional (Elhai et al., 2020). There is high probability that those suffering from affective psychopathological symptoms, e.g. anxiety, resort to using smartphones excessively to manage their anxiety, which, however, could lead to elevated anxiety and cause a vicious circle (Elhai et al., 2020; Rozgonjuk et al., 2018; Elhai et al., 2017). Prolonged and excessive use of smartphones may give rise to addiction and there has been mounting evidence documenting problematic smartphone use among children, adolescents, and university students. Problematic smartphone use has been linked with anxiety and sleep disturbance and may hinder academic growth (Karki et al., 2020; Richardson et al., 2018; Lee et al., 2018; Aker et al., 2017). The rate of smartphone addiction was recently reported to be 36.8% among medical students in Nepal (Karki et al., 2020), which was slightly higher than that reported (29.8%) among medical students in China (Chen et al., 2017). The obviously higher prevalence rates recorded in these studies compared to those of other studies conducted worldwide might be attributed to the differences between screening tools and assessment methods, which were nevertheless indicative of the potential of problematic smartphone use as a public health concern among medical students (Chen et al., 2017). During home confinement in the early stage of the COVID-19 pandemic, problematic smartphone use may have been partly triggered by the prolonged use of smartphones as an easily accessible device for online learning and partly by smartphones being excessively used as a (maladaptive) emotional process to cope with negative affect. One recent longitudinal study conducted among college students in the US revealed the association between COVID-19 news reporting, increased levels of anxiety, and increased smartphone use (Huckins et al., 2020). People tend to use smartphones to obtain information about COVID-19 and to manage anxiety amidst the unprecedented pandemic. More exposure to news about COVID-19, with a flood of COVID-19 disinformation and false reports bombarding social media, might lead to increased anxiety and smartphone use (Elhai et al, 2020; Gao et al., 2020). Meanwhile, social distancing resulting from enforced home confinement during the early COVID-19 period might fuel students’ fear of missing out on interaction with others, which might contribute to constantly checking social media via smartphones and subsequently resulting in higher levels of anxiety (Li, 2020).
Nevertheless, the positive role that smartphone use played in bridging social distancing between individuals during COVID-19 should not be ignored. COVID-19 pandemic is a worldwide public health crisis, in which strict social distancing has been recognized as the best way to avoid exposure to COVID-19 and ensure physical well-being (David & Roberts, 2021). However, social distancing could exert an undermining effect on one's feeling of social connectedness, which could in turn negatively influence one's psychological well-being with exhibition of signs of mental health problems, e.g. anxiety (David & Roberts, 2021; Van Orden et al., 2020). What is worth noting is that the negative impact of social distancing on social connectedness could be moderated by smartphone use which could provide sense of belonging and avenues for social support, thus ultimately enhancing the psychological well-being. Smartphone use, despite not being as effective as face-to-face interaction with regards to connecting with others, could be considered as an appropriate alternative during the COVID-19 crisis which challenges individuals’ coping mechanisms (David & Roberts, 2021). The frequent or increased use of smartphone could not necessarily be regarded as a maladaptive behavior; however, hallmark symptoms of addictive disorders and consequent functional impairment, are vital for determining if the smartphone use is beneficial or prejudicial (Billieux et al., 2015).
This study tested the mediating effect of sleep disturbance between problematic smartphone use and anxiety. Findings from this study show that problematic smartphone use could exert not only a direct path on anxiety but also an indirect path on anxiety through sleep disturbance. This study speculates that addiction to smartphone use could increase the likelihood of experiencing sleep disturbance, which might in turn lead to elevated levels of anxiety. Sleep has been established as having a fundamental effect on both physical and mental health (Morin et al., 2020) and playing an influential role in restoring emotional reactivity (Goldstein and Walker, 2014). Healthy sleep could play a critical role in coping with negative affect during major crises, such as the outbreak of COVID-19, which has been considered an unprecedented global health crisis (Morin et al., 2020). Conversely, deteriorated sleep might contribute to elevating negative affect, leading to increased vulnerability to anxiety (Becker and Gregory, 2020).
The present study was also consistent with prior research showing a positive association between problematic smartphone use and sleep disturbance. A recent one-year prospective study conducted among Chinese college students demonstrated that those with a higher degree of smartphone addiction were more prone to having a later chronotype and shorter sleep duration on weekdays (Kang, 2020). Under the enforced home confinement during the early COVID-19 period, online learning and social distancing might have contributed to students spending more time using smartphones. Prolonged exposure to the blue light emitted by smartphones may cause suppression of melatonin production. That, combined with the changes in daily routines and reduced outdoor exposure to sunlight, which are essential to the synchronization of biological clock, may result in sleep disruption (Morin et al., 2020; Becker and Gregory, 2020), thus elevating anxiety.
One major limitation of the present study is its cross-sectional design, which may generate biased estimates of longitudinal mediation parameters and does not allow conclusions on the direction of causality to be drawn. While it is plausible that problematic smartphone use influenced anxiety both directly and indirectly through the mediating effect of sleep disturbance, there is also likelihood that anxiety exerted effects on problematic smartphone use mediated by sleep disturbance. Hence, our preliminary cross-sectional study may serve as a prelude to further longitudinal designs to confirm causal relationships between anxiety, sleep disturbance, and problematic smartphone use. Second, data collected through self-report questionnaires were subject to potential response bias and difference in temporality between the three variables examined in this study. Third, the medical students recruited in this study were from one medical university in Northeast China. Thus, the generalizability of study findings to broader settings are yet to be confirmed.
Conclusion
Findings of this study demonstrate the positive association that anxiety exhibits with both problematic smartphone use and sleep disturbance and also problematic smartphone use exerts both a direct impact and an indirect impact on anxiety through the mediating path of sleep disturbance. Therefore, it is advisable that interventions should be provided to alleviate anxiety for medical students during the pandemic. Also, medical students should be informed of the detrimental impact of problematic smartphone use and the importance of healthy sleep habits on mitigating anxiety. This might be achieved by incorporating education on overcoming problematic smartphone use and improving healthy sleep habits into the preclinical curriculum of medical education. Reducing problematic smartphone use and improving the sleep of medical students might have a positive result on reducing anxiety in the short term and the continuation of the habits might have a positive long-term effect throughout their careers. The study was conducted during the 2020 spring semester when courses of all universities in China were delivered online, which might provide possible reference for other countries undertaking similar practices in the fight against the COVID-19 pandemic.
Ethics statement
The study was conducted in accordance with the ethical guidelines and approved by the Committee on Human Experimentation of China Medical University (CMU1210400061).
Author contributions
YS reviewed literature and wrote and revised the manuscript. KS provided assistance and reviewed and revised the manuscript. CC contributed to the acquisition and analysis of data and the revision of the manuscript. YY contributed to the acquisition and interpretation of data. YL provided assistance and contributed to the revision of the manuscript.
XY was responsible for the conception and design of the study and contributed to the revision of the manuscript.
Declaration of Competing Interest
The authors declare no potential conflicts of interest related to the research, authorship, and publication of this article.
Acknowledgments
Acknowledgements
The authors would like to express their sincere gratitude to all the medical students who participated in this survey. The authors are also very grateful to the editors and the reviewers for their valuable comments and constructive suggestions that would greatly improve the quality of this paper.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Aker S., Sahin M.K., Sezgin S., Oguz G. Psychosocial factors affecting smartphone addiction in university students. J. Addict. Nurs. 2017;28(4):215–219. doi: 10.1097/JAN.0000000000000197. [DOI] [PubMed] [Google Scholar]
- Becker S.P., Gregory A.M. Editorial Perspective: Perils and Promise for Child and Adolescent Sleep and Associated Psychopathology during the COVID-19 Pandemic. J. Child. Psychol. Psyc. 2020;61(7):757–759. doi: 10.1111/jcpp.13278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billieux J., Maurage P., Lopez-Fernandez O., Kuss D.J., Griffiths M.D. Can disordered mobile phone use be considered a behavioral addiction? An update on current evidence and a comprehensive model for future research. Curr. Addict. Rep. 2015;2(2):156–162. [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiat. Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time, and digital media use during COVID-19 lockdown in Italy. J. Sleep. Res. 2020;29(4):e13074. doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandratre S. Medical Students and COVID-19: Challenges and Supportive Strategies. J. Med. Educ. Curric. Dev. 2020;7 doi: 10.1177/2382120520935059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen B., Liu F., Ding S., Ying X., Wang L., Wen Y. Gender differences in factors associated with smartphone addiction: a cross-sectional study among medical college students. BMC. Psychiatry. 2017;17(1):341. doi: 10.1186/s12888-017-1503-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway M.A., Cabrera O.A., Clarke-Walper K., Dretsch M.N., Holzinger J.B., Riviere L.A., Quartana P.J. Sleep disturbance mediates the association of adverse childhood experiences with mental health symptoms and functional impairment in US soldiers. J. Sleep. Res. 2020;29(4):e13026. doi: 10.1111/jsr.13026. [DOI] [PubMed] [Google Scholar]
- David M.E., Roberts J.A. Smartphone use during the covid-19 pandemic: social versus physical distancing. Int. J. Environ. Res. Public Health. 2021;18(3):1034. doi: 10.3390/ijerph18031034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L., Shao X., Wang Y., Huang Y., Zhu G. An investigation of mental health status of children and adolescents in china during the outbreak of covid-19. J. Affect. Disord. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai J.D., Levine J.C., Dvorak R.D., Hall B.J. Problematic smartphone use: a conceptual overview and systematic review of relations with anxiety and depression psychopathology. J. Affect. Disord. 2017;207:251–259. doi: 10.1016/j.jad.2016.08.030. [DOI] [PubMed] [Google Scholar]
- Elhai J.D., Yang H., Mckay D., Asmundsone G.J.G. COVID-19 anxiety symptoms associated with problematic smartphone use severity in Chinese adults. J. Affect. Disord. 2020;274:576–582. doi: 10.1016/j.jad.2020.05.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher T.H., Schleyer A.M. We Signed Up for This!” — student and trainee responses to the COVID-19 pandemic. N. Engl. J. Med. 2020;382:e96. doi: 10.1056/NEJMp2005234. [DOI] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Wang Y., Fu H., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS. One. 2020;15 doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill D., Whitehead C., Wondimagegn D. Challenges to medical education at a time of physical distancing. Lancet. 2020;396(10244):77–79. doi: 10.1016/S0140-6736(20)31368-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein A.N., Walker M.P. The role of sleep in emotional brain function. Annu. Rev. Clin. Psychol. 2014;10:679–708. doi: 10.1146/annurev-clinpsy-032813-153716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanish A.E., Lin-Dyken D.C., Han J.C. PROMIS Sleep Disturbance and Sleep-Related Impairment in Adolescents: Examining Psychometrics Using Self-Report and Actigraphy. Nurs. Res. 2017;66(3):246–251. doi: 10.1097/NNR.0000000000000217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He X.Y., Li C.B., Qian J., Cui H.S., Wu W.Y. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatient. Shanghai. Arch. Psychiatry. 2010;22:200–203. [Google Scholar]
- Hong F., Zhang R.R. The Relationship between Job Requirements and Employees’ Occupational Well-being: Multiple Mediating Role of Recovery Experience. Manage. Admin. 2017;(7):33–36. [Google Scholar]
- Huckins J.F., daSilva A.W., Wang W.C., Hedlund E., Rogers C., Nepal S.K., Wu J.L., Obuchi M., Murphy E.I., Meyer M.L., Wagner D.D., Holtzheimer P.E., Campbell A.T. Mental Health and Behavior of College Students During the Early Phases of the COVID-19 Pandemic: Longitudinal Smartphone and Ecological Momentary Assessment Study. J. Med. Internet. Res. 2020;22(6):e20185. doi: 10.2196/20185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jniene A., Errguig L., El Hangouche A.J., Rkain H., Aboudrar S., El Ftouh M., Dakka T. Perception of Sleep Disturbances due to Bedtime Use of Blue Light-Emitting Devices and Its Impact on Habits and Sleep Quality among Young Medical Students. Biomed. Res. Int. 2019 doi: 10.1155/2019/7012350. 7012350-7012350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang Y., Liu S., Yang L., Xu B., Lin L., Xie L., Zhang W., Zhang J., Zhang B. Testing the Bidirectional Associations of Mobile Phone Addiction Behaviors With Mental Distress, Sleep Disturbances, and Sleep Patterns: A One-Year Prospective Study Among Chinese College Students. Front. Psychiatry. 2020;11:634. doi: 10.3389/fpsyt.2020.00634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karki S., Singh J.P., Paudel G., Khatiwada S., Timilsina S. How addicted are newly admitted undergraduate medical students to smartphones?: a cross-sectional study from Chitwan medical college. Nepal. BMC. Psychiatry. 2020;20:95. doi: 10.1186/s12888-020-02507-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon M., Kim D-J., Cho H., Yang S. The Smartphone Addiction Scale: Development and Validation of a Short Version for Adolescents. PLoS. ONE. 2013;8(12):e83558. doi: 10.1371/journal.pone.0083558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA. Netw. Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Sung M.J., Song S.H., Lee Y.M., Lee J.J., Cho S.M., Park M.K., Shin Y.M. Psychological factors associated with smartphone addiction in south Korean adolescents. J. Early. Adolescence. 2018;38(3):288–302. [Google Scholar]
- Lemola S., Perkinson-Gloor N., Brand S., Dewald-Kaufmann J.F., Grob A. Adolescents’ Electronic Media Use at Night, Sleep Disturbance, and Depressive Symptoms in the Smartphone Age. J. Youth. Adolesc. 2015;44(2):405–418. doi: 10.1007/s10964-014-0176-x. [DOI] [PubMed] [Google Scholar]
- Li L., Griffiths M.D., Mei S.L., Niu Z.M. Fear of Missing Out and Smartphone Addiction Mediates the Relationship Between Positive and Negative Affect and Sleep Quality Among Chinese University Students. Front. Psychiatry. 2020;11:877. doi: 10.3389/fpsyt.2020.00877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhu Q., Fan W.L., Makamure J., Zheng C.S., Wang J. Online Mental Health Survey in a Medical College in China During the COVID-19 Outbreak. Front. Psychiatry. 2020;11:459. doi: 10.3389/fpsyt.2020.00459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luk T.T., Wang M.P., Shen C., Wan A., Chau P.H., Oliffe J., Viswanath K., Chan S.S., Lam T.H. Short version of the Smartphone Addiction Scale in Chinese adults: Psychometric properties, sociodemographic, and health behavioral correlates. J. Behav. Addict. 2018;7(4):1157–1165. doi: 10.1556/2006.7.2018.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Education of China., 2020. The Notice of the Leading Party members’ Group of the Ministry of Education of the Communist Party of China on the Prevention and Control of Coronavirus Pneumonia and the Reform and Development of Education. Beijing: Ministry of Education of China. http://www.moe.gov.cn/srcsite/A17/s7059/202002/t20200228_425499.html. (in Chinese).
- Morin C.M., Carrier J., Bastien C., Godbout R. Sleep and circadian rhythm in response to the COVID-19 pandemic. Can. J. Public. Health. 2020;111(5) doi: 10.17269/s41997-020-00382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ran L., Wang W., Ai M., Kong Y., Chen J., Kuang L. Psychological resilience, depression, anxiety, and somatization symptoms in response to covid-19: a study of the general population in china at the peak of its epidemic. Soc. Sci. Med. 2020;262 doi: 10.1016/j.socscimed.2020.113261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson M., Hussain Z., Griffiths M.D. Problematic smartphone use, nature connectedness, and anxiety. J. Behav. Addict. 2018;7(1):109–116. doi: 10.1556/2006.7.2018.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozgonjuk D., Levine J.C., Hall B.J., Elhai J.D. The association between problematic smartphone use, depression and anxiety symptom severity, and objectively measured smartphone use over one week. Comput. Hum. Behav. 2018;87:10–17. [Google Scholar]
- Saraswathi I., Saikarthik J., Kumar K.S., Srinivasan K.M., Ardhanaari M., Gunapriya R., Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. PEERJ. 2020;8:e10164. doi: 10.7717/peerj.10164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwenk T.L., Davis L., Wimsatt L.A. Depression, stigma, and suicidal ideation in medical students. JAMA. 2010;304:1181–1190. doi: 10.1001/jama.2010.1300. [DOI] [PubMed] [Google Scholar]
- Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep. Med. 2020;70:124. doi: 10.1016/j.sleep.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahedian-Azimi A., Moayed M.S., Rahimibashar F., Shojaei S., Ashtari S., Pourhoseingholi M.A. Comparison of the severity of psychological distress among four groups of an Iranian population regarding COVID-19 pandemic. BMC. psychiatry. 2020;20(1):402. doi: 10.1186/s12888-020-02804-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden K., Bower E., Lutz J., Silva C., Gallegos A.M., Podgorski C.A., Santos E.J., Conwell Y. Strategies to promote social connections among older adults during “social distancing” restrictions. Am. J. Geriatr. Psychiatry. 2020 doi: 10.1016/j.jagp.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z.H., Yang H.L., Yang Y.Q., Liu D., Li Z.H., Zhang X.R., Zhang Y.J., Shen D., Chen P.L., Song W.Q., Wang X.M., Wu X.B., Yang X.F., Mao C. Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: a large cross-sectional study. J. Affect. Disord. 2020;275:188–193. doi: 10.1016/j.jad.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L., Buyssem D.J., Germain A., Moul D.E., Stover A., Dodds N.E., Johnston K.L., Pilkonis P.A. Development of Short Forms from the PROMIS Sleep Disturbance and Sleep-Related Impairment Item Banks. Behav. Sleep. Med. 2011;10(1):6–24. doi: 10.1080/15402002.2012.636266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang M.X., Wu A.M.S. Effects of smartphone addiction on sleep quality among Chinese university students: The mediating role of self-regulation and bedtime procrastination. Addict. Behav. 2020;111 doi: 10.1016/j.addbeh.2020.106552. [DOI] [PubMed] [Google Scholar]
- Zhang C., Yang L., Liu S., Ma S., Wang Y., Cai Z., Du H., Li R., Kang L., Su M., Zhang J., Liu Z., Zhang B. Survey of insomnia and related social psychological factors among medical staffs involved with the 2019 novel coronavirus disease outbreak. Front. Psychiatry. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J., Su L., Zhou Y., Qiao J., Hu W. The effect of nationwide quarantine on anxiety levels during the COVID outbreak in China. Brain. Behav. 2020 doi: 10.1002/brb3.1938. [DOI] [PMC free article] [PubMed] [Google Scholar]