Abstract
Global spread of COVID-19 has seriously threatened human life and health. The aerosol transmission route of SARS-CoV-2 is observed often associated with infection clusters under poorly ventilated environment. In the context of COVID-19 pandemic, significant transformation and optimization of traditional ventilation systems are needed. This paper is aimed to offer better understanding and insights into effective ventilation design to maximize its ability in airborne risk control, for particularly the COVID-19. Comprehensive reviews of each phase of aerosol transmission of SARS-CoV-2 from source to receptor are conducted, so as to provide a theoretical basis for risk prediction and control. Infection risk models and their key parameters for risk assessment of SARS-CoV-2 are analyzed. Special focus is given on the efficacy of different ventilation strategies in mitigating airborne transmission. Ventilation interventions are found mainly impacting on the dispersion and inhalation phases of aerosol transmission. The airflow patterns become a key factor in controlling the aerosol diffusion and distribution. Novel and personalized ventilation design, effective integration with other environmental control techniques and resilient HVAC system design to adapt both common and epidemic conditions are still remaining challenging, which need to be solved with the aid of multidisciplinary research and intelligent technologies.
Keywords: Aerosol transmission, Ventilation, Aerodynamics, Infection risk model, SARS-CoV-2, HVAC
1. Introduction
The novel coronavirus disease COVID-19 pandemic, caused by SARS-CoV-2 virus, remains a global challenge and a severe threat to public health. As of 29 August 2021, there have been more than 216 million infected cases globally, including over 4.4 million deaths as reported by the World Health Organization COVID-19 dashboard (https://covid19.who.int/). These astonishing numbers have highlighted the importance of using effective measures to prevent and control the spread of this highly contagious disease.
The World Health Organization (WHO) issued an updated scientific brief on 31 April 2021, which summarized the current knowledge about the transmission routes of SARS-CoV-2 and indicated the possibility of aerosol transmission of the virus (WHO, 2021). The virus can be released by the infector through sneezing, coughing, talking or breathing in small particles ranging from larger droplets to smaller aerosols (5 μm as a cut-off size in this work). Current evidence suggests that the SARS-CoV-2 can be transmitted between people in short range (<1 m) by inhaling or contacting the aerosols or droplets containing the virus or it can be transmitted in long-range (>1 m) in poorly ventilated and/or crowed indoor settings over long exposure time. Touching contaminated surfaces with the virus when touching the eyes, nose or mouth with hands can also be a transmission way.
Among the reported transmission modes of SARS-CoV-2, including droplet, aerosol, contact and contamination (WHO, 2020), aerosol transmission is one of the most critical routes for infection prevention and control and it is usually associated with clusters of infection in public spaces, especially when poorly ventilated. An outbreak of COVID-19 in an air-conditioned restaurant in Guangzhou, China, causing 10 infections by one infector, showed no direct contact or fomite contact identified from the surveillance recordings and the airflow was modeled of consistent direction with aerosol transmission (Li et al., 2021; Lu et al., 2020). This implied probable airborne transmission of SARS-CoV-2 with insufficient ventilation of merely 1 L/s per person (Li et al., 2021). The superspreading event occurred in a 2.5-hour choir practice of the Skagit Valley Chorale where 61 persons attended with 52 COVID-19 infected cases, illustrated the airborne route as a major contributor despite adequate precautions being made to avoid either fomite or ballistic droplet transmission (Hamner et al., 2020). Miller et al. (2020) also investigated this event and estimated a ventilation air change rate of 0.3 to 1 h−1 during the choir practice, which might promote the spreading of aerosols and inhalation by the exposed members. Katelaris et al. (2021) investigated a SARS-CoV-2 outbreak in a church in Sydney, and reviewed the epidemiologic and environmental findings to assess the possibility of airborne transmission, suggesting the probable airborne transmission route of the virus and poor ventilation possibly being a contributor to this route (Katelaris et al., 2021). Other cluster reports also suggested involvement of airborne transmission (Hijnen et al., 2020; Hwang et al., 2021; Jang et al., 2020; Muller et al., 2020; Park et al., 2020;). Although the circumstances under which aerosol transmission of SARS-CoV-2 might occur are still uncertain, there is growing evidence that aerosol transmission of the virus is plausible under conditions conductive to disease transmission (Morawska et al., 2020; Tang et al., 2020), particularly in relatively confined space with dense occupancy, long duration and poor ventilation (Miller et al., 2020). Therefore, ventilation that is used as a primary engineering measure for aerosol transmission control should be considered as a non-negligible factor in SARS-CoV-2 prevention and control in indoor settings (Correia et al., 2020).
Heating, ventilation and air conditioning (HVAC) system is typically used to provide mechanical ventilation in buildings. Natural ventilation is also a good practice providing outdoor fresh air, which has been practiced in many healthcare facilities in regions with favorable climate conditions (e.g. hot or warm climate) (Aviv et al., 2021). Ventilation plays a critical role in removing contaminants including infectious aerosols indoor to maintain a good air quality. (Liu, Ning et al., 2020)detected air samples in two hospitals in Wuhan, China, and found positive SARS-CoV-2 RNA in the air in medical staff areas, isolation wards, ventilated patient wards and toilets. Air samples containing positive SARS-CoV-2 particles were also detected by other studies in hospitals (Chia et al., 2020; Kenarkoohi et al., 2020; Razzini et al., 2020; Santarpia et al., 2020). SARS-CoV-2 virus has been shown to remain viable in aerosols for over 3 hours with an estimated half-life of 1.1∼1.2 hours (van Doremalen et al., 2020). The evidence shows that aerosols released by infected patient can be potentially infectious pollutant source in the air which should be removed by ventilation to prevent further infection and spread to susceptible individuals.
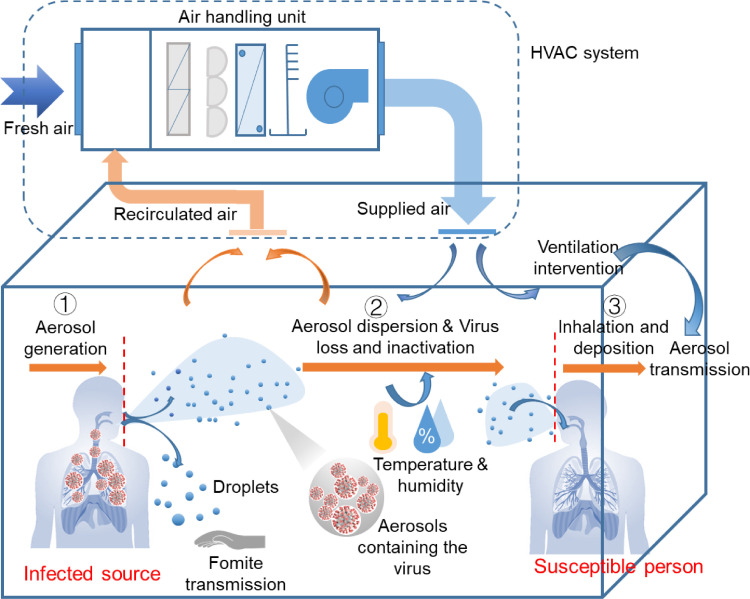
Fig. 1 depicts the aerosol transmission process of SARS-CoV-2 indoor with three different phases from the source to the receptor in a ventilated room. The basic concept of ventilation against aerosol transmission is to dilute the overall viral concentration to a safe level with adequate ventilation rates (Ding et al., 2020; Li et al., 2007). Filtration and sterilization means coupled with the HVAC systems are capable to remove the airborne pathogens before entering the room or after leaving the exhaust to avoid contamination (Morawska et al., 2020; Xu, Luo, Yu & Cao, 2020; Zheng et al., 2021). Moreover, appropriate air distribution patterns are also important to avoid the build-up of viral contamination in specific locations in ventilated context (Berlanga et al., 2018; Dietz et al., 2020; Kong et al., 2021). Buonanno et al. (2020) found that ventilation can change the distributed locations of SARS-CoV-2 and reasonable airflow pattern is helpful to reduce the accumulation of the virus. As a traditional engineering method, ventilation not only shows effectiveness in protecting occupants from long-range aerosol transmission, but may also affect the short-range dispersions of the exhaled virus-laden air from the source end. Chen et al. (2021) reported that an increase of ventilation flow rate will decrease short-range exposure of exhaled aerosols due to enhanced dilution effect of ventilation. Novel occupant-targeted ventilation strategies can also be a shift to improve the local viral contamination (Melikov, 2020). Overall, effective ventilation strategies should intervene the transmission process of virus-laden aerosols, after leaving the infected source and before entering the inhalation of another person.
Fig. 1.
Schematic of potential aerosol transmission route of SARS-CoV-2 and the intervention of HVAC system. Aerosol transmission can be divided into three phases: ① aerosol generation by the infector, ② aerosol dispersion and virus inactivation, and ③ inhalation and deposition on target tissues to cause infection.
Therefore, to better understand how building ventilation affects the mode of aerosol transmission of SARS-CoV-2 and to develop optimal intervention strategies, this paper: (1) reviews each process of the infection pathway from the source to the receptor to provide a theoretical basis for SARS-CoV-2 risk assessment and control; (2) investigate applicable infection risk models for SARS-CoV-2 in ventilated context based on the understating of the probable aerosol transmission route of the virus; and (3) analyze the merits of different ventilation strategies concerning airborne infection risk mitigation. The remaining challenges and developing trends of ventilation systems for airborne infection risk control are also discussed. This paper will provide meaningful insights into aerosol transmission mechanisms, associated risk assessment methods and potential engineering control strategies to prevent and control the spread of COVID-19 in indoor environment. Results of this study will be helpful to offer better understanding and insights into effective ventilation design to maximize its ability in reducing airborne infection risk in the context of COVID-19.
2. Aerosol transmission of SARS-CoV-2
Aerosol transmission of a certain disease is biologically plausible when: (1) infectious aerosols are generated from an infector; (2) the pathogens contained in the aerosols remain viable in the air for some time; and (3) the target tissues are accessible to the aerosols where the pathogens initiates infection (Jones & Brosseau, 2015). The transmission process of SARS-CoV-2 illustrated in Fig. 1 basically complies with the criteria proposed by Jones and Brosseau (2015), but it will be discussed more from aerodynamics perspectives to assist further implementation of engineering control measures, in particular, the ventilation strategies. Tracking of the three phases of SARS-CoV-2 transmission will simultaneously provide more evidence to support the aerosol transmission route.
2.1. Aerosol generation
Respiratory droplets are generated by atomization of secretions in respiratory tract during daily breathing activities (e.g. normal breathing, talking, singing, sneezing and coughing) (Roy & Milton, 2004). The droplets are normally polydispersed with many different sizes. The concept of aerosol in this work is adopted as droplet or droplet nucleus (Wells, 1934) with an aerodynamic diameter smaller than 5 μm, which can contribute to both short range and long range transmission of SARS-CoV-2. The SARS-CoV-2 virus has been frequently detected in nasopharyngeal exudates, sputum, blood and other body excreta like urine and feces of infected patients (Costa et al., 2021; Hou et al., 2020; Jacot et al., 2020; Jeong et al., 2020; Xie et al., 2020). Aerosols derived from sites bearing pathogens have the highest possibility to carry with them (Gralton et al., 2011). Aerosolization of the respiratory secretions of patients infected by SARS-CoV-2 is likely to produce virus-containing droplets or aerosols through the respiratory activities. The virus of SARS-CoV-2 has been detected in the condensate of patient's exhaled breath and millions of particles containing the virus may be released by the patient per hour due to merely tidal breathing (Ma et al., 2021).
2.1.1. Atomization mechanism
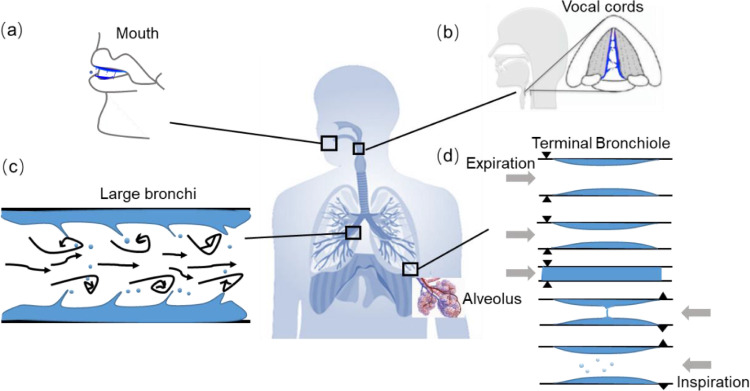
The atomization mechanisms of the respiratory secretions have been postulated with several modes occurring at different sites at the respiratory tract between the mouth and alveoli, as shown in Fig. 2 (Gralton et al., 2011; Johnson & Morawska, 2009; Johnson et al., 2011; Morawska et al., 2009; Patterson & Wood, 2019). Understanding the atomization mechanisms can be helpful to understand the origins of the infectious aerosols.
Fig. 2.
Illustration of the aerosolization mechanisms occurring in human respiratory tract (Johnson & Morawska, 2009; Patterson et al., 2019). (a) Film burst and filament in the mouth; (b) laryngeal generation due to vocal fold vibration and open/close action; (c) film burst by shear stress due to high velocity in large bronchi; and (d) bronchiole fluid film burst mechanism (BFFB) from re-opening of terminal bronchiole during breathing.
Early studies proposed the generation of aerosol during tidal breathing through high-speed atomization (Jennison, 1942; Slonim & Chapin, 1967). Later studies (Gebhar et al., 1998; Johnson & Morawska, 2009; Johnson et al., 2011) indicated the aerosols generated by the re-opening of terminal bronchioles during inhalation and consensus have been emerged on the bronchiole fluid film burst mechanism (BFFB) for aerosol generation during tidal breathing (Fig. 2(d)). Aerosols may also be produced by shear stress with high-speed flow, which drives the lining fluid in large bronchi to rupture (Leith et al., 1986) (Fig. 2(c)). This may occur in violent breathing activities like coughing or sneezing. Energetic vocal fold vibrations during speech or coughing may also generate aerosols (Fig. 2 (b)) (Johnson et al., 2011). In the process of speaking, the tongue moves in the mouth to produce fluid film and then breaks to produce droplets (Johnson et al., 2011). The closure and re-opening of the mouth tips may also cause filament and burst of droplets (Abkarian & Stone, 2020) (Fig. 2(a)). Large droplets produced by the oral mode (mouth, tongue and lips) are inferred to be originated from saliva (Guo et al., 2021).
Table 1 summarizes the probable mechanisms of droplet generation with different breathing activities and the produced droplet sizes along with these activities. Morawska et al. (2009) and Johnson et al. (2011) identified overlapping modes within different breathing activities, implying the possibility of a mixture of different origins of the expelled aerosols from the respiratory tract. This explains why there is wide range of droplet size distributions from coughing, sneezing or speaking, but a relatively concentrated droplet size distribution <5 μm from tidal breathing, predominantly being considered as aerosols. This is because the aerosols generated by tidal breathing is mainly governed by BFFB. Droplets from other respiratory activities (e.g. coughing, sneezing or speaking) may be driven by overlapping mechanisms with multimodal droplet size distributions. Table 1 also shows that there is large discrepancy of droplet size distribution among different studies, varying from sub-micrometer to 1000 μm range as a result of the complexities of physical formation mechanisms and measurement techniques. The droplet sizes strongly influence the fate of droplet transport in indoor environment. Accurate determination of the size distributions of infectious particles remains critical. The broadly distributed sizes indicate the expelled particles from the infected source may be transmitted to others avail of both droplets and aerosols. Precautions for airborne infection control should be made to include measures for both transmission routes.
Table 1.
Probable aerosolization mechanisms involved in different breathing activities and the measured initial droplet sizes and concentration.
| Respiratory activities | |||||
|---|---|---|---|---|---|
| Breathing | Speaking | Coughing | Sneezing | ||
| Aerosolization mechanism (Fig. 2) | (a) Film burst and filament in the mouth | − | + | + | + |
| (b) Laryngeal generation due to vocal fold vibration | − | + | + | + | |
| (c) Film burst by shear stress in large bronchi | − | − | + | + | |
| (d) BFFB in terminal bronchioles | + | + | + | + | |
| Initial droplet size and concentration distribution expelled at mouth/nose opening | Droplet size (μm) | • Mode: 0.8 (Morawska et al., 2009) | • Peak size: 0.8-0.9 (Morawska et al., 2009) | • Peak size: 0.8-0.9 (Morawska et al., 2009) | • Range: 1-1000 (Duguid, 1946) |
| • 0.3-0.4 (Almstrand et al., 2010) | • Geometric mean: 16 (Chao et al., 2009) | • Geometric mean: 13.5 (Chao et al., 2009) | • Range: 0.1-1000; 360.1 μm (geometric mean of | ||
| • 0.05-5 (Milton et al., 2013) | • 1.6, 2.5 and 145 μm (count median) were detected. (Johnson and Morawska, 2009) | • Range: 1-2000, 95% between 2 and 100 μm (Duguid, 1946) | unimodal distribution, SD = 1.5) and 74.4 μm (geometric mean of bimodal distribution, SD = 1.7) (Han et al., 2013) | ||
| Droplet concentration (cm−3) | • 0.05-0.092 (Morawska et al., 2009) | • 0.307 (Morawska et al., 2009) | • 0.67 (Morawska et al., 2009) | • An average number of a sneeze releases is 1 × 106, 200-fold more | |
| • 0.004-0.223 (Chao et al., 2009) | • 2.4-5.2 (Chao et al., 2009) | particles than a cough. Fluid volume for a sneeze is 1.2 × | |||
| • 5 × 103(average number emitted per cough) (Duguid, 1946) | 10−5 mL. (Duguid, 1946) | ||||
*”+” means possible and “−” means largely impossible to occur.
2.1.2. Viral load of SARS-CoV-2 in body fluid
The quantification of viral load expelled from the infected source is vital for subsequent risk assessment. For SARS-CoV-2, the viral load may be non-uniformly distributed in the fluid of different sites in respiratory tract. It may also differ between asymptomatic and symptomatic patients. Zou et al. (2020) detected higher viral loads in the nose than in the throat but no significant difference between asymptomatic and symptomatic patients. While Costa et al. (2021) detected significant higher viral load of SARS-CoV-2 in symptomatic than in asymptomatic subjects from patients’ nasopharyngeal exudates. SARS-CoV-2 was found in sputum at an average concentration of 7.00 × 106 copies per mL and a maximum load of 7.11 × 108 copies per throat swab (Wölfel et al., 2020), which suggested active virus replication in tissues of the upper respiratory tract. However, not all the aerosolized droplets will contain virus. The expelled viral load of SARS-CoV-2 would be more representative to indicate the viral transmissibility through aerosols than the viral load obtained by swabs from respiratory fluids.
The detected viral load in exhaled breath samples (mean: 2.47 × 103 copies per 20 times exhaled breath) was found significantly lower than that in oral-nasopharyngeal swabs (mean: 7.97 × 106 copies per swab) (Malik et al., 2021). Compared detecting SARS-CoV-2 RNA in oral-nasopharyngeal swabs, detecting the samples of exhaled breath may be more suitable for evaluating the infectivity of SARS-CoV-2 through droplets (Malik et al., 2021; Yun et al., 2020). Laser scattering observations show that loud speech can produce thousands of droplets per second and they can stay in the air for 8-14 minutes, presumably corresponding to the behavior of droplets of 12-21 μm before dehydration or droplet nulcei of ca. 4 μm (Anfinrud et al., 2020; Stadnytskyi et al., 2020). As the existence of SARS-CoV-2 in exhaled droplets or aerosols has been proved, infection is likely to occur if the virus-contained droplets being inhaled by susceptible persons. It also implies the control measures, like wearing face masks (Cravero and Marsano, 2021; Milton et al., 2013) or exhaust the exhaled particles from source timely, would be possible to block or exhaust viral particles to mitigate the transmission risk of the disease from the source end.
2.2. Dispersion and viability
2.2.1. Droplet evaporation and deposition
Exhaled droplets contain water and non-volatile solutes. After complete evaporation, the solid residuals in droplets are left. They were first named by Wells as droplet nuclei in 1934 (Wells, 1934). Saliva is a comprise of water (about 99.5% in volume) and a variety of inorganic or organic matters such as salt, proteins, enzymes, peptides and so on (Humphrey & Williamson, 2001; Rezaei & Netz, 2021). Solid component in droplets may also contain microorganisms e.g. bacteria or viruses. As SARS-CoV-2 RNA is reported in exhaled droplets with thousands of copies in exhaled breath for several times’ exhalation (Malik et al., 2021), the droplet nuclei (aerosols) containing active viruses may contribute to airborne transmission to susceptible persons.
The fate of droplets expelled from the source are found dependent on their initial sizes. Droplet sizes govern their deposition, evaporation and dispersion behaviors and determine the survival of microorganisms within the droplets (Biswas & Dhawan, 2020; Lieber et al., 2021; Morawska, 2006; Wells, 1934; Xie et al., 2007). Recent studies reported the SARS-CoV-2 virus remaining viable in the air or on surfaces for several hours or even more (Gidari et al., 2021; van Doremalen et al., 2020). It's therefore vital to answer these fundamental questions regarding how far the droplets can travel and how fast they fall to ground or evaporate to droplet nuclei. Discerning the deposition rate is important for understanding the lifetime of droplets, surface contamination and aerosol removal effect via ventilation. Fig. 3 illustrates the trajectory of droplets depending on their initial sizes. Particles in the air are mainly subject to the gravity force and the aerodynamic drag force (Ge et al., 2021; Silva, 2020; Zhang et al., 2020). The compete of the two forces varies among different droplets sizes. For droplets smaller than 10 μm, the time of complete evaporation to a solid residue is normally within 1 s (Morawska, 2006; Wei & Li, 2015) and the drag force is more important than the gravity, leading to droplet floating and moving with air streamlines. The trajectory of large droplets is approximately parabolic, settling to the ground fast due to the greater effect of gravity as well as longer evaporation time of about 10 s for droplets of 100 μm (Morawska, 2006; Wei & Li, 2015).
Fig. 3.
Trajectory of exhaled droplets from an infected source, depending on droplet size (Silva, 2020). Deposition and evaporation behavior of droplets are affected by environmental factors e.g. temperature, humidity and airflow from ventilation (Rezaei & Netz, 2021).
The classic Wells evaporation-falling curve model (Wells, 1934) was the first to reveal the quantified relationship between droplet sizes, evaporation time, and sedimentation rate. The predicted results with this model were partly confirmed by later studies (Biswas & Dhawan, 2020; Morawska, 2006; Nicas et al., 2005; Xie et al., 2007). These studies indicate droplets larger than 50-100 μm will quickly fall to ground, while droplets smaller than 50 μm will fully evaporate before settling and suspend in the air to travel for longer distance. Wang, Li et al. (2020a) revealed that the droplets smaller than 50 μm from a cough will evaporate in the puff region, and thus stay longer at the initial height expelled. This may result in easier inhalation for person of same height and probability of infection. The Wells model assumes the expelled droplets are all within fully mixed environment with homogenous ambient temperature, humidity and turbulent velocity (Wells, 1934). But more recent studies (Bourouiba, 2020; Bourouiba et al., 2014; Chong et al., 2021) indicate the vortex in exhaled puff will trap small clusters of respiratory droplets and slow down the evaporation rate due to local moist and warm atmosphere within the expelled gas cloud. This will cause extended life-time of droplets and decrease the possibility of the formation of droplet nuclei compared with the Wells model. Observations of the captured videos of real coughing and sneezing show that the larger droplets will fall to the ground quickly (<1-2 m), and aerosols containing small droplets and nuclei can travel a further distance even up to 8 m for a sneeze and stay suspended for up to 10 minutes depending on the environmental conditions (Bourouiba, 2020). The deposition and evaporation rate of droplets are also affected by a number of other factors such as initial velocity and viscosity of droplets, temperature, humidity, turbulence, air velocity and so on (Ram et al., 2021). These physical factors control the evaporation and deposition rate of droplets and also play important roles in determining the fate of infectious viruses contained in droplets.
2.2.2. Dispersed SARS-CoV-2 aerosols
Proofs of SARS-CoV-2 virus existing in room air with the infector can serve as important indirect evidence of aerosol transmission. Droplets expelled from the infector may contain virus. Aerosols (<5 μm) are dispersed into the room air and travel with air current to different locations after full evaporation. The deposited droplets or aerosols on surfaces may also cause resuspension. Recent studies (Chia et al., 2020; Guo et al., 2020; Liu, Ning et al., 2020; Ong et al., 2020; Santarpia et al., 2020) have confirmed the existence of SARS-CoV-2 virus in the air of rooms with COVID-19 patients. (Liu, Ning et al., 2020) detected relatively higher concentration of SARS-CoV-2 RNA in aerosols in toilet area used by patients (maximum of 19 copies/m3) and in some medical staff areas (16-42 copies/m−3 in the protective-apparel removal rooms). Relatively lower level of the viral RNA was detected in isolation wards and ventilated patient rooms. The SARS-CoV-2 aerosols were found to mainly include two size ranges: 0.25-1 μm and >0.25 μm. Aerosol deposition was also found in two deposited samples with an estimated deposition rate of 31 and 113 copies/(m2•h), respectively, which were placed 2 m and 3 m from the bed of a patient (Liu, Ning et al., 2020)(). This study implies both suspended and deposited aerosols in environment with patients not evenly distributed in space. A similar study (Guo et al., 2020) conducted in two Wuhan hospitals also found SARS-CoV-2 widely distributed in the air and surfaces in ICU and general hospital wards with patients. SARS-CoV-2 aerosols were found in the upstream area of a patient with a maximum detected transmission distance of 4 m (Guo et al., 2020), which implies SARS-CoV-2 aerosols being transported to a long distance via air. Chia et al. (2020) also found positive samples of SARS-CoV-2 RNA on surfaces and in the air of isolation rooms holding the patients, in which the SARS-CoV-2 aerosols were detected with sizes of > 4 μm and 1-4 μm, respectively in two rooms, despite with ventilation of an air change rate of 12 h−1. Ong et al. (2020) tested the air samples in an isolation room in Singapore with a SARS-CoV-2 symptomatic patient and an air change rate of 12 h−1, but indicated negative results despite the contamination of the environment. While swabs from the air exhaust were tested positive, suggesting SARS-CoV-2 aerosols being replaced by ventilation and deposited on the exhaust device when leaving the room (Ong et al., 2020). This study also implies ventilation can be a potential way to remove SARS-CoV-2 aerosols in indoor environment to reduce airborne infection risk.
However, these studies can only indicate the viral load of SARS-CoV-2 RNA relying on polymerase chain reaction (PCR) without knowing the virus activity. Inactivated virus even with high load will not cause infection. Hereby, a recent study carried out by Santarpia et al. (2020) made cell culture of the virus collected from the air and surfaces in a National Quarantine Unit in Nebraska, USA. Active SARS-CoV-2 virus is reported in the hallway air sample (Santarpia et al., 2020). This is an important evidence to support SARS-CoV-2 being kept alive in aerosols suspended in the air.
2.2.3. Viability of SARS-CoV-2
As it has been confirmed with the presence of active SARS-CoV-2 virus in aerosols persistent in the air (Santarpia et al., 2020), the next important question need to be answered is how long it can survive and how the viability of the virus decays. van Doremalen et al. (2020) compared the viability decay rate of aerosolized SARS-CoV-2 with SARS-CoV-1, indicating similar half-life time of median estimates of about 1.1-1.2 hours and 95% confidence intervals of 0.64-2.64 hours for SARS-CoV-2 and 0.78-2.43 hours for SARS-CoV-1. The viability of SARS-CoV-2 on surfaces are longer than in aerosols with stainless steel of 5.6 hours and plastic of 6.8 hours at a temperature of 21-23°C and 40% relative humidity (RH) (van Doremalen et al., 2020). However, the artificially aerosolized particles with virus from a nebulizer may be different from the natural aerosolization process in human respiratory tract (Fig. 2) as to different droplet compounds, droplet size distributions and viral load. Smither et al. (2020) reported a UK variant of SARS-CoV-2 in aerosols can stay viable for at least 1.5 hours with a medium and a high humidity under experimental conditions. The decay rates of the SARS-CoV-2 variant are reported ranging 0.4-2.27% per minute and the half-life of 0.5-2.95 hours (Smither et al., 2020). Fears et al. (2020) revealed the SARS-CoV-2 virus maintained infectious at a test time of 16 hours by aerosol suspension stability experiment under normal environmental conditions (23±2°C and 53±11% RH). The inactivation rate of the virus strongly depends on ambient temperature and humidity conditions. SARS-CoV-2 is estimated to survive longer at low temperature and relatively low humidity on surfaces, with half-life time of over 24 hours at 10°C and 40% RH and about 1.5 hours at 27°C and 65% RH (Morris et al., 2020). However, there is still lack of accurate information on the relationship between the environmental factors (e.g. temperature and humidity) on the stability, viability and decay rate of SARS-CoV-2 existing in aerosols, which should be clearly demonstrated in future studies.
2.3. Inhalation, deposition and infection
The inhaled droplets or aerosols of the exposed person may be directly drawn from the exhaled flow of the infected source when they are in close distance (usually smaller than 1 m). The inhalation can also be originated indirectly from the ambient environment as a result of mixing of the infectious aerosols from the infector with room air. The indirect pattern also occurs both in short distance and long distance between the two persons (Fu et al., 2021; Nielsen et al., 2014; Vuorinen et al., 2020). Fig. 4 depicts the origins of inhaled infectious aerosols for the exposed person. The majority of inhalation is from the air around and below the nose or mouth for a standing person, upward along the free convective boundary layer around human body (Murakami, 2004). The boundary layer (body plume) moves upward from the bottom of the room and entrains ambient air with development. The inhalation of a standing person in calm environment is then directly drawn from the upward convective boundary layer. The inhaled air quality is thereby predominately determined by the microenvironment around the lower part of the human body (Brohus & Nielsen, 1996; Licina et al., 2015). This is particularly important for displacement ventilation where the distribution of contaminant stratifies in vertical height with clean air in the lower part of the room (Brohus & Nielsen, 1996). Personalized ventilation is developed based on the concept to directly intervene the thermal boundary layer and bring clean air to inhalation, and is considered as a novel ventilation strategy to minimize airborne infection risk (Melikov, 2004; Xu & Liu, 2018).
Fig. 4.
Inhalation of susceptible individual directly and indirectly drawn from the exhaled droplets/aerosols from the infected source.
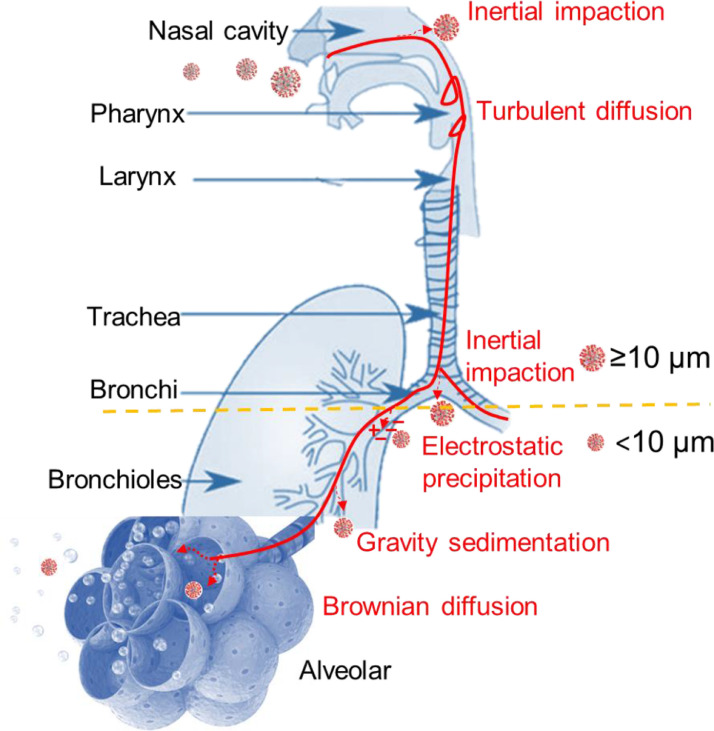
Once inhaled, particles containing virus may deposit on surfaces of respiratory tract and trigger infection. Aerosols with aerodynamic diameter smaller than 5 μm are reported to have the ability to readily penetrate deep into the alveolar region of the lungs of an exposed person (Buonanno et al., 2020). The deposition behaviors of infectious particles in human respiratory tract are also predominately governed by their sizes. Various effects act on the particles and cause deposition on different sites. The acting forces including inertial impaction, gravity sedimentation, electrostatic precipitation, Brownian diffusion and interception (Darquenne, 2012, 2020; Phuong et al., 2020; ;(Wang, Prather et al., 2021) Wei et al., 2021) (see Fig. 5 ). Several studies (Nicas et al., 2005; Stilianakis & Drossinos, 2010; Weber & Stilianakis, 2008) suggested an equilibrium size of 10 μm as the cut-off size by considering the likelihood of deposition in respiratory tract. It's generally considered that aerosols larger than 10 μm attend to deposit in the nasopharyngeal region mainly through inertial impaction (Fig. 5), while those larger than 6 μm generally will not reach the alveolar (Darquenne, 2012; Hinds, 1999; Sznitman, 2013). Aerosols smaller than 2 μm are primarily considered to deposit in the Bronchial and alveolar regions (Darquenne, 2012). Brownian diffusion is typically considered as the dominant mechanism for aerosols smaller than 0.5 μm and gravity sedimentation is mainly for aerosols in the size range 1-8 μm. Larger particles deposit mainly as a result of inertial impaction rather than sedimentation.
Fig. 5.
Deposition mechanism of infectious particles through inhalation (Darquenne, 2012 & 2020). The deposition rate is governed by particle sizes. 10 μm is suggested a cut-off size for particles to deposit and transmit disease (Weber & Stilianakis, 2008). Particles larger than 10 μm tend to impact on surfaces of upper airways due to inertia; particles smaller than 10 μm are more likely to penetrate to lower pulmonary region and sediment as a result of gravity and Brownian diffusion (Hinds, 1999; Nicas et al., 2005).
After deposition, the virus contained in particles may initiate infection. (Hou et al., 2020) reported possible higher nasal susceptibility to SARS-CoV-2 with likely subsequent aspirated virus seeding to the lung in SARS-CoV-2 pathogenesis. The mechanism of SARS-CoV-2 viral infection and its associations with the deposition sites are still not clearly addressed (Murphy et al., 2020)(Mortazavi et al., 2020). But all the existing evidence tracing from the source to the susceptible host (Sections 2.1-2.3) basically proves the probability of aerosol transmission of SARS-CoV-2.
3. Infection risk prediction of SARS-CoV-2
Infection risk assessment is useful for the quantification of infection probability of a certain disease and can serve as a meaningful tool in epidemic modeling to evaluate the effectiveness of corresponding control measures (Sze To & Chao, 2010). Section 2 reviews the aerodynamic and biological characteristics of SARS-CoV-2 transmitted from the source to the receptor, which provides a basis for predicting airborne infection risk of the virus. Models describe the process of transmission can be referred as infection risk models. Two broadly used models in epidemic modeling: Wells-Riley model and dose-response model, are discussed in this section to demonstrate their applications in infection risk prediction of SARS-CoV-2 through the airborne route in ventilated indoor settings. These two models mainly consider the aerosol generation and inhalation or intake dose phases (Fig. 1, ① & ③) and the intermediate transport process (Fig. 1, ②) is less considered.
3.1. Wells-Riley model
The correlation between airborne infection risk and ventilation rate can be assessed by the Wells-Riley model. It has been extensively used in predicting the infection risk of SARS-CoV-2 for epidemiological analysis (Li & Tang, 2021; Park et al., 2021; Peng & Jimenez, 2021; Sha et al., 2021). This model was established based on the concept of “quanta of infection”, which means the number of infectious aerosols required to infect a single person (Riley et al., 1978; Wells, 1955). The Wells-Riley model regards a fully mixing condition of infectious aerosols with ventilation, which can be expressed as:
| (1) |
where PI is the probability of infection, C is the number of infections, S is the total number of susceptible persons, I is the number of infectors, q is quanta emission rate from the infected source (quanta/h), p is the pulmonary ventilation rate of a susceptible person (inhaled) (m3/h), Q is room ventilation rate with clean air (m3/h) and t is the exposure time interval (h). The quanta emission rate, q, is a key parameter for quantifying the infection risk, which can be obtained by estimating the outbreak cases epidemiologically. Table 2 shows the quanta emission rates derived from some known COVID-19 outbreak cases indoor by retrospective calculations. These selected cases are indicated airborne transmission probable and should be accessible with information on I, p, t and Q for reverse calculation of q.
Table 2.
Retrospective calculation of the quanta emission rate (q) of SARS-CoV-2 based on some known airborne transmission cases.
| Case | Country | Number of infections, C | Total number of susceptible persons, S | Number of infector, I | Pulmonary ventilation rate, p (m3/h) | Exposure, t (h) | Ventilation rate, Q (m3/h) | Quanta emission rate, q (quanta/h) |
|---|---|---|---|---|---|---|---|---|
| Guangzhou restaurant (Lu et al., 2020) | China | 9 | 19 | 1 | 0.54 | 1.2 | 94 | 92 |
| Vietnam bar (Chau et al., 2020) | Vietnam | 12 | 200 | 1 | 0.54 | 4.5 | 6000 | 152 |
| Ningbo bus (Shen et al., 2020) | China | 20-23 | 60 | 1 | 0.54 | 1.67 | 234 | 90-107 |
| Dublin flight | Ireland | 13 | 49 | 1 | 0.5 | 7.5 | 7075 | 596 |
| Vietnam flight (Khanh et al., 2020) | Vietnam | 12 | 20 | 1 | 0.5 | 11 | 840 | 140 |
| Choir rehearsal (Hamner et al., 2020) | USA | 32 | 60 | 1 | 0.64 | 2.5 | 549 | 253 |
| Call center (11th floor) (Park et al., 2020) | Korea | 6-15 | 216 | 1 | 0.54 | 8 | 6480 | 42-107 |
Buonanno et al. (2020) estimated the quanta emission rate of SARS-CoV-2 from an infector based on the emitted viral load from the mouth, regarding respiratory activity types, activity levels, and the removal rates as a result of ventilation, droplet deposition and virus inactivation. The estimated q ranges from <1 quanta/h to >100 quanta/h for an asymptomatic infector with light activity (Buonanno et al., 2020). The estimated q derived from previous outbreak cases (Table 2) varies in wide range (42-596 quanta/h) with a median value of 140 quanta/h. This median value basically corresponds to the estimated q by Buonanno et al. (2020) of 142 quanta/h for speaking. However, the ventilation rate, Q, is often difficult to determine from the retrospective study of an outbreak case. Some of the ventilation rates given in Table 2 are extrapolated based on the minimal fresh air requirements for HVAC systems in specific occasions (ASHRAE, 2016). Different estimates of the ventilation rates will cause deviations of q from those in Table 2.
The Wells-Riley model implicitly considers the infectivity of the virus by using the concept of quanta, and only considers the removal effect by ventilation. Later studies improved the model by incorporating effects of deposition loss, viral inactivation, filtration with face masks or filters and social distancing (Cravero & Marsano, 2021; Kriegel et al., 2020; Sun & Zhai, 2020; Sze To & Chao, 2010). By combining with the spatial distribution characteristics of the virus, the spatially distributed infection risk can be predicted by improved Wells-Riley models (Guo et al., 2021; Zhai & Li, 2021; Zhang & Lin, 2021).
3.2. Dose-response model
Dose-response models have been extensively adopted in assessing the infection risk of diseases as well as the adverse health effect caused by other hazardous materials. A dose-response model developed by Sze To et al. (2008) incorporates the aerodynamic size dependent factors of infectious particles and forms a non-threshold stochastic model to predict infection risk:
| (2) |
where P 1(t 0) is the probability of infection with an exposure time interval of t 0; as the infectivity depends on sizes of pathogen-laden particles (Day & Berendt, 1972; Wells, 1955), the particles are divided into different size bins with a total number of m; rj indicates the infectivity and βj is the deposition fraction of particles containing pathogens of the jth size bin; c is pathogen concentration in exhaled droplets; p is pulmonary ventilation rate of the susceptible host; q is breathing frequency of the infector; v(t)j is the volume density of exhaled droplets in infector's exhalation of the jth size bin; and f(t) is the pathogen viability over time.
This model (Eq. 2) is suitable to evaluate the effect of ventilation on airborne infection risk. v(t)j can be reversely inferred from the concentration of particles in inhalation of the susceptible individual (Sze To et al., 2008), which is affected by ventilation. To evaluate the infection risk of SARS-CoV-2 in indoor environment with this model, the required key parameters related to this virus are summarized in Table 3 , which are mainly obtained from existing aerodynamic and biological studies discussed in Section 2.
Table 3.
Available information for prediction of infection risk of SARS-CoV-2.
| Parameter | Available data | References | Remarks |
|---|---|---|---|
| Virus concentration, c | c=1 × 105.25 TCID50a/mL | van Doremalen et al. (2020) | Obtained in the upper and lower respiratory tract in human subjects |
| Infectivity term, rj and deposition fraction, βj | ID50b = 1.8TCID50 (Infectious dose for aerosol ≤3 μm, [mean value range: 0.6-3.0]) r≤3μm = 0.385 β≤3μm = 0.6 | Alford et al. (1966) (rj for influenza A) | rj, infectious term of SARS-CoV-2, is not available at present. rj of influenza A is listed here instead. |
| ID50 = 223.5TCID50 (Infectious dose for aerosols ≥3 μm, for a larger aerosol mean value range: 127-320) r≥3μm = 0.0031 β≥3μm, determined by Hinds (1999) | Douglas (1975) (rj for influenza A) & Hinds (1999) | ||
| Viability of SARS-CoV-2, f(t) | f(t) = 0.01778 × (0.5)−t/1.15 | van Doremalen et al. (2020), | Extrapolated from Fig. 1 in van Doremalen et al. (2020). Half-live of SARS-CoV-2 of about 1.1 to 1.2 hours (21-23°C, 40% RH) |
| Volume density of exhaled droplets, v(t)j | Final nucleus size is assumed as 6% of its initial volume | Nicas et al. (2005) |
TCID50 is a unit to describe the quantity of the virus, referring to 50% tissue-culture infectious dose.
ID50 50% infectious dose, can be used to calculate the infectivity term r (r=-ln 0.5/ID50).
The dose-response model provides more explicit and realistic exposure estimates than the Wells-Riley model, but it's highly dependent on the biological data of the virus, which may be difficult to obtain especially at the initial stage of the outbreak. As shown in Table 3, the infectivity term (rj) of SARS-CoV-2 is still not clear at present stage. The sizes of infectious particles are strongly associated with the transmission modes, which also affect the infection sites of the virus in upper or lower respiratory tract. The quantitative determinations of the aerodynamic size dependent terms, including rj , βj and v(t)j of the infectious particles, are complex but important with respect to the accuracy of this model. Especially for the evaluation of aerosol transmission risk of SARS-CoV-2, the intake dose, deposition and infection mechanisms of the virus should be further clarified.
4. Ventilation control strategies
Ventilation systems can be classified according to the driven forces as natural ventilation or mechanical ventilation (positive pressure or negative pressure). Indoor ventilation mainly impacts the last two phases of aerosol transmission: dispersion phase and inhalation phase as shown in Fig. 1 (② & ③). To better understand the impact of ventilation on aerosol transmission of SARS-CoV-2, the prevailing ventilation strategies applied in buildings are compared and discussed in this section, mainly focusing on their abilities in mitigating airborne infection indoor.
4.1. Natural ventilation
Natural ventilation is driven by natural forces such as wind pressure or buoyancy caused by temperature differences between indoor and outdoor environment. Natural ventilation is inexpensive and can achieve high ventilation rate compared with mechanical ventilation, which is especially suitable for warm climate and has shown robust energy saving potentials (Aviv et al., 2021; Oropeza-Perez & Østergaard, 2014; Park et al., 2021; Rackes et al., 2016). By proper passive design of the building structures and their openings (e.g. windows, doors, solar chimneys or wind towers) or combining passive cooling or heating systems, fresh outdoor air can be directly induced to improve indoor air quality and thermal comfort (Abdullah & Alibaba, 2020; Deng & Tan, 2020; Deng et al., 2021; Fan et al., 2020; Jia et al., 2021; Lipinski et al., 2020; Wang et al., 2020a, Wang et al., 2020; Wen et al., 2020; Wu et al., 2021). WHO specified a fresh air volume of 160 L/s per patient for naturally ventilated in health-care facilities (WHO, 2020). This high flow volume of fresh air is normally difficult to realize by using mechanical ventilation which is restricted by the high energy consumption. Park et al. (2021) explored the potential of natural ventilation in preventing COVID-19 airborne transmission in a Korean school and found reduced infection risk of lower than 1% with cross-ventilation of over 15% windows opened (equivalent to an air change rate of 6.51 h−1) simultaneously assisted by wearing face masks.
However, there are still concerns about inter-building and inter-unit transmission of the virus. The airborne transmission route of SARS-CoV-1 between both neighboring buildings and the household units in a building was reported in 2004 (Yu et al., 2004). Wind-driven inter-unit transmission and indoor-outdoor transmission of airborne pathogens were also reported by previous studies (Dai et al., 2019; Liu & You, 2012). Therefore, careful plans and designs of airborne precaution areas and the placement of infected patients are strongly needed so as to apply natural ventilation to reduce the infection risk of people in the surrounding areas, e.g. in health care facilities (WHO, 2009). Fluctuation of ventilation rate driven by variable forces and varying flow directions add difficulties in natural ventilation design. To avoid inter-building or inter-unit airborne transmission, the airflow from infected source area should be directed to areas having sufficient dilution and preferably outdoor with adequate building spacing (Li & Chen, 2021; Liu & You, 2012; Liu et al., 2020; Wang, 2020; Wang, Yin et al., 2020).
Due to the dynamic outdoor conditions and the narrow favorable air temperature (20-26°C) (Axley & Emmerich, 2002), the thermal comfort of indoor space cannot always be guaranteed. Another strategy to utilize natural ventilation is to adapt it with HVAC systems (or hybrid ventilation). The mixed system adds complexity to the system but can extend the use of natural ventilation in other climate zones and can be under better control (Qi et al., 2020). Aviv et al. (2021) estimated the performance of the system coupled natural ventilation with radiant cooling to increase fresh air supply and prevent COVID-19 transmission. The combined system is reported to successfully balance the natural ventilation and energy saving, and an energy decrease of 10-45% can be achieved by using this system compared with traditional HVAC systems in global major cities (Aviv et al., 2021).
Natural ventilation is proved with the ability to act as a possible solution to mitigate airborne transmission risk of COVID-19 by increasing the fresh air volume during the epidemic (Lepore et al., 2021; Park et al., 2021; Zivelonghi & Lai, 2021). Resilient system design and appropriate combination with HVAC systems can maximize its ability in airborne infection control by simultaneously taking comfort and energy savings into account (Lomas & Ji, 2009).
4.2. Mechanical ventilation
4.2.1. Total volume air distribution
Mixing ventilation and displacement ventilation are two conventional total volume air distribution principles in indoor settings, both treating air in the whole room scale. Mixing ventilation is realized by inducing high speed air from diffusers located at the upper part of the room, which facilitates the mixing of supplied air with ambient air due to high momentum (Fig. 6 (a)). For displacement ventilation, cooled air is supplied from lower diffusers, driven by convective thermal flow around heat sources (e.g. persons, equipment or lamps), and discharged from the top of the room (Brohus & Nielsen, 1996) (Fig. 6 (b)).
Fig. 6.
Schematic of ventilation principles and interactions with dispersed exhalation flow from source to receptor with the three different ventilation strategies: (a) mixing ventilation, (b) displacement ventilation and (c) personalized ventilation (combined with mixing ventilation).
There have been some other ventilation strategies like downward ventilation, diffuse ceiling ventilation, underfloor ventilation, piston ventilation and stratum ventilation, which are designed between the two principles (Yang et al., 2019). Other developing ventilation strategies including wall-attached ventilation, impinging ventilation and confluent jet ventilation are all realized based on the displacement principle in later flow development stage (Bu et al., 2021). Different combinations of the supply or exhaust openings and their relative positions to the infector or the susceptible person will affect the efficacy of the ventilation principles in airborne risk control (Chen et al., 2020; Kong et al., 2021). Despite diverse air distribution principles indoor, three prevailing and basic ventilation strategies are discussed in detail, which are mixing ventilation, displacement ventilation and personalized ventilation (Fig. 6). Personalized ventilation is an old system form being used in vehicles for years but is a new system in other occasions and with novel designs. Their efficacy in mitigating airborne infection and the impact on different phases of airborne transmission are emphasized. The comparisons among the three prevailing ventilation strategies and three other emerging ventilation strategies that may potentially contribute to airborne risk control are summarized in Table 4 .
Table 4.
Comparisons of different ventilation strategies with respect to their efficacy in aerosol transmission control.
| Ventilation principle | Aerosol transmission intervention | Advantages | Limitations | Applicable Occasions | Use priority during epidemic (ASHRAE, 2020) |
|---|---|---|---|---|---|
Mixing ventilation (MV) 
|
Intervene dispersion phase and inhalation phase by influencing the total environment (Fig. 1); the effect of MV on dispersion of aerosols in microenvironment between persons is minimal (Nielsen et al., 2014) | Widely used; simple system form; uniform thermal environment and air quality | Facilitate dispersion of aerosols; low ventilation efficiency; high air volume for infection control and increased energy cost | Applicable in most occasions | High |
Displacement ventilation (DV) 
|
Intervene dispersion phase and inhalation phase (Fig. 1) by influencing both total environment and human microenvironment due to the effect of temperature gradient (Bjørn & Nielsen, 2002) | High ventilation efficiency at lower clean zone; reduced contaminant mixing with ambient air; low air supply velocity | Thermal stratification can increase penetration distance and decrease diffusion of exhaled flow (Bjørn & Nielsen, 2002; Qian et al., 2006; Xu et al., 2015); not applicable for heating mode | Applicable in high space (normally >3 m) with cooling needs | Low; not recommended in healthcare facilities (ASHRAE, 2008) |
Personalized ventilation (PV) 
|
Directly intervene early dispersion phase (with PV or PE) and inhalation phase (Fig. 1) | Direct supply of fresh air to inhalation (PV) or direct exhaust of exhaled aerosols from the source (PE); high localized efficiency; energy saving | Possibly facilitate aerosol diffusion from source (Xu, Wei et al., 2020); lack of mature design criteria and technical installation solutions; system form is complex and often needs to couple with total volume ventilation (Melikov, 2004) | People seated for a relatively long time, such as offices, schools, public transportations, theaters, clinics, etc.; PV can be used with total volume ventilation like MV or DV | High |
Downward ventilation (DWV) 
|
Intervene dispersion phase and inhalation phase by influencing the total environment or the microenvironment depending on the airflow pattern similar to MV or DV (Fig. 1) | DWV diffuser outside the occupied zone and local exhausts at high locations will create a flow pattern like DV and be able to remove exhaled aerosols, suitable for hospital wards (Nielsen et al., 2010) | Not able to produce laminar and unidirectional airflow pattern in the occupied zone as expected (Qian et al., 2005); low-velocity DWV from diffusers above persons is often unable to penetrate human microenvironment (Olmedo et al., 2013); flow pattern similar to MV with downward flow above occupants as thermal plume increases mixing | Recommended by CDC (2005) for isolation wards; locations of diffuser and exhaust should be optimized considering the positions of patient and healthcare workers (Nielsen et al., 2010). | Medium |
Protected zone ventilation (PZV) 
|
Intervene dispersion phase and inhalation phase (Fig. 1) by influencing both total environment and human microenvironment with air curtain partition | Separate the room into subzones by plane jet; higher protection efficiency against airborne transmission than MV (Cao et al., 2015; Aganovic & Cao, 2019) | Possible thermal discomfort; high flow volume and energy consumption; only for cooling purpose (Cao et al., 2013) | Applicable in clinics or hospital wards | Medium |
Stratum ventilation (SV) 
|
Intervene dispersion phase and inhalation phase in the occupied zone affected by SV | High air quality in the breathing zone of occupants by delivering clean air directly to this height; small temperature difference between head and feet (Tian et al., 2011) | Relative position between the airborne agent source and the SV diffuser affects its performance (Lin et al., 2012) | Applicable in schools, offices and other small or medium sized rooms | Medium |
Mixing ventilation (MV) is one of the most widely used ventilation principle in buildings to maintain good thermal comfort and inhaled air quality for occupants. Expelled aerosols from the infected person can be diluted and removed by supplying fresh air from MV. Jiang et al. (2009) indicated the infection risk of SARS-CoV-1 can be effectively reduced by increasing the equivalent dilution ratio of fresh air volume to infectious flow with over 10,000 times, which can only be realized by using natural ventilation in practice. WHO (2009) recommends that the fresh air volume in environment with patients should be no less than 150 m3/h per person. This number is derived based on the predicted results with the Wells-Riley model, assuming pathogens distributed uniformly under fully mixing conditions (WHO, 2009). ASHRAE (2008) requires a minimum air change rate of 12 h−1 and negative pressure for airborne infection isolation rooms in newly built buildings. However, there is still debate about “sufficient ventilation rate” for airborne infection prevention indoor (Li et al., 2007). As the ventilation efficiency of MV is low of merely around 1 (Yang et al., 2019), its protection effect of removal aerosol pathogens is hereby limited and should be enhanced by supplying large volume of fresh and conditioned air to the entire room, which may lead to high energy cost of the HVAC system. As the dilution process of pathogens with MV may bring the infectious pathogens to all parts of the room by means of mixing (Berlanga et al., 2018; Ren et al., 2021; Sandberg et al., 2020), this ventilation principle is not applicable to occasions operated at low fresh air volume and with the presence of infectors. Therefore, to overcome this two-sided role of MV in airborne transmission, the supplied fresh air should always be maintained at a relatively high level for the purpose of mitigating airborne infection risk.
Displacement ventilation (DV) is suitable for a relatively high space (>3 m) operating at cooling mode (Brohus & Nielsen, 1996). Clean and cool air is supplied from bottom diffusers in the room and heated up by internal heat sources to move upward, which creates a stratified clean zone at the lower part and a relatively polluted zone at the upper part of the room (Fig. 6 (b)). Ventilation efficiency of DV in the lower clean zone is significantly higher than MV (Bjørn & Nielsen, 2002), but it is normally not recommended for occasions containing infected patients. ASHRAE (2008) strictly restricts its application in these health care facilities. It is mainly due to the “lock-up” phenomenon, which restricts the diffusion of exhaled pathogens with the effect of reverse temperature gradient along vertical height (temperature grows with height) (Fig. 6(b)). This phenomenon has been reported by previous studies (Gao et al., 2008; Olmedo et al., 2012; Qian et al., 2006; Xu et al., 2015). It will cause increased penetration distance of the exhaled flow and a reduced mixing rate with ambient air, which may increase the exposure risk of infectious particles for the exposed person in close proximity. However, other studies (e.g. Berlanga et al., 2018; Li et al., 2013) indicated better performance of DV in reducing airborne infection than with MV. This may occur with no direct exposure to the exhaled flow from the infected source and with a relative distant distance apart from the source.
4.2.2. Personalized ventilation
Personalized ventilation (PV) is a novel concept to deliver clean air directly to the inhalation zone of a person, which is considered as a promising solution to reduce airborne cross-infection between occupants (Melikov, 2020; Xu & Liu, 2018; Xu, Wei et al., 2020). Different from the overall dilution effect of MV, PV is aimed to improve the local ventilation efficiency around human body (Fig. 6 (c)). Through proper design, it can minimize airflow mixing with ambient air, and can provide clean air with an efficiency of more than 90% (Bolashikov & Melikov, 2009; Melikov & Dzhartov, 2013). Air terminal devices of PV have various forms and can be flexibly controlled according to the user's need (Katramiz et al., 2020; Melikov, 2004). This system has distinct advantages in improving the thermal comfort, air quality and energy efficiency (Assaad, et al., 2021; Liu, Li et al., 2020; Melikov, 2004;). A number of studies (Gao & Niu, 2007; Li et al., 2013; Melikov & Dzhartov, 2013; Nielsen et al., 2007; Niu et al., 2007; Pantelic et al., 2009; Xu et al., 2020; (Xu, Wang et al., 2021)) have reported excellent performance in reducing the intake dose of infectious pathogens for the exposed occupant. For example, Nielsen et al. (2007) proposed bed-integrated PV devices including a pillow and a blanket made by textile and indicated a high protection efficiency of clean air delivery of 95% against airborne infection. Pantelic et al. (2009) evaluated the infection risk reduction ratio of influenza A and tuberculosis with a desk amounted PV device and reported a reduction of 27% and 65% for the two kinds of diseases, respectively.
However, it also should be noted that when PV is applied to the infector alone, the impacting airflow from PV will accelerate the mixing of infectious aerosols with room air, and hereby may increase the infection risk of the exposed occupant (Bolashikov & Melikov, 2009; Xu et al., 2021). Xu, Wei et al. (2020b) reported a nozzle-based PV jet entrains droplets from the infector's exhalation with a close face-to-face orientation. Direct exposure risk (Fig. 4) from infectious exhaled flow is therefore increased by using PV (Xu, Wei et al., 2020). The accelerated mixing effect of PV to the infected source is also observed by this study but it only increases indirect exposure by a small percentage (Xu, Wei et al., 2020). In this context, to avoid the promotion of PV on dispersion of exhaled droplets, a personalized exhaust (PE) can be used to control the source. The effectiveness of PE or combined PV-PE system in aerosol transmission control has been primarily proved in previous studies (Dygert & Dang, 2010; Yang et al., 2015).
PV can typically provide a flow ranging from 5 L/s to 20 L/s per person depending on the terminal device types and the positioning, which can be used to improve the thermal comfort and inhaled air quality in a localized environment (Liang et al., 2021; Melikov, 2004). In order to keep an acceptable background thermal environment, PV is normally coupled with MV or DV (Melikov, 2004). There are several remaining questions to be addressed for practical use of PV in mitigating airborne infection risk, such as the development of highly efficient PV terminal devices, effective combination of PV with the total ventilation or the PE system, and technical solutions for installation of PV in specific occasions like offices, theaters, or vehicles with high occupancy.
5. Challenges and research trends
In the context COVID-19 pandemic, the prevention and control of aerosol transmission of the virus SARS-CoV-2 in indoor environment is remaining challenging. It's necessary to carefully examine each process of the aerosol transmission route to cut off and prevent the transmission at any possible stage.
The discussions in previous sections have demonstrated close relationship between ventilation and aerosol transmission of SARS-CoV-2. Ventilation is found to mainly intervenes the dispersion and inhalation phases of aerosol transmission, which can be realized by natural ventilation, mechanical ventilation or hybrid ventilation. Improper air distribution design may increase the risk of aerosol transmission by facilitating aerosol dispersion to unfavorable areas or by locking accumulated aerosols to undesired levels (Correia et al., 2020). The ventilation system has even been reported as a transmission way of airborne diseases (e.g. SARS-CoV-1, measles, tuberculosis, influenza, chickenpox and smallpox) (Li et al., 2007). Inversely, with proper design and operation of the ventilation system, aerosol transmission can be minimized (Ding et al., 2020; Morawska et al., 2020).
To maximize the efficacy of ventilation systems in airborne infection control including SARS-CoV-2, there are several challenges remain to be solved: (1) novel ventilation strategies to intervene the aerosol transmission route from source to receptor to the greatest extent and as early as possible; (2) effective integration of other environmental control techniques to maximize the efficacy of ventilation in aerosol transmission mitigation; (3) resilient design of HVAC systems to adapt both normal and epidemic situations, and being operated with relatively low energy consumption.
In order to effectively address these challenges, future research is needed regarding following aspects:
-
•
To intervene the aerosol transmission process of significance, novel ventilation design should be established on a basis of full understanding of the transmission mechanisms of the infectious diseases and their influencing factors. Accurate prediction of the airborne infection risk of SARS-CoV-2 relies on adequate information of the viral load, viability, and pathogenicity of the virus combined with information of the aerodynamic characteristics of virus-laden droplets or aerosols. Multidisciplinary research needs to be established with joint efforts from multidisciplinary fields, such as virology, epidemiology, aerodynamics, public health, environmental engineering and so on, which will be helpful to predict the infection risk of the disease and develop control strategies accordingly.
-
•
Most of the present ventilation strategies mainly impact the dispersion process of exhaled aerosols and the inhalation process (phases ②&③ in Fig. 1) by influencing the total environment (e.g. mixing ventilation to dilute the overall concentration of infectious particles). As the dispersion and inhalation of aerosols mainly occur within human microenvironment, this indirect impact from overall ventilation may be inefficient (Nielsen et al., 2014; Zhao et al., 2020; Zhao et al., 2020). By respecting this special microenvironment between short-ranged occupants and developing appropriate ventilation strategies towards it, both short-range and long-range aerosol transmission can be minimized (Melikov, 2004; Xu & Liu, 2018; Xu, Wei et al., 2020). Future ventilation should be designed more personalized and occupant-oriented with a paradigm shift (Cao et al., 2020; Li et al., 2020; Melikov, 2020; (Wang, Wang et al., 2021)). Personalized ventilation that directly intervenes inhalation (PV) and the dispersion of exhaled droplets from early stage (by PV or PE) may serve as a solution to prevent aerosol transmission both from the source and to the receptor. But the efficiency of PV is affected by numbers of factors such as the air terminal device configurations, interaction of multi-airflows in human microenvironment, and so on (Melikov, 2004; Xu et al., 2018). Occupant-oriented ventilation is more targeted and energy efficient but is also highly dependent on intelligent monitoring and control algorithms (Cao, 2019; Nienaber et al., 2020; Ren & Cao, 2020; (Wang, Wang et al., 2021); Wang, Huang et al., 2021; Zhu et al., 2020). Future research is needed in fields of fluid mechanics and fluid dynamics to develop highly efficient air terminal devices. Airflow patterns favorable to control the aerosol transmission route and minimize airborne infection risk need further investigation. Intelligent monitoring and controlling are also needed to be properly integrated to the ventilation system to optimize the operation modes with multiple objectives. This will be helpful to develop personalized and smart ventilation systems, which can be expected in future buildings.
-
•
According to guidelines for HVAC system operation in normal time, current system design cannot provide adequate protection during the pandemic (Zheng et al., 2021). In addition to ventilation, other environmental control techniques are recommended to couple with the HVAC systems although they are not mandatory, which may include HEPA filtration, ultraviolet germicidal irradiation (UVGI), heat inactivation, air ionization, plasma purification, etc. (Berry et al., 2021; Feng et al., 2021; Feng et al., 2021; Feng et al., 2021; Sodiq et al., 2021). Studies on these assistive techniques to HVAC systems are normally based on normal conditions and the effectiveness should be further verified during pandemic. The adaptive abilities of these control measures to both normal and epidemic conditions also need to be evaluated. Novel disinfection devices with high efficiency of virus removal and relatively low energy consumption are urgently needed. The integration of these techniques with ventilation systems may promote their own efficacy in airborne risk control and should be further validated in future studies.
-
•
Current ventilation systems designed according to previous guidelines for normal conditions may not meet the requirements for risk control during the pandemic. They may fail to supply sufficient clean air to dilute the virus. To develop resilient ventilation systems adapting both normal and epidemic conditions, measures to adapt the shift should be investigated. For example, disabling the air circulation system may be realized by merely increasing heating or cooling load (Morawska et al., 2020); increase of ventilation rate or using HEPA can be made by increasing the capacity of fans (Zheng et al., 2021); or the performance of HVAC systems in disease control can be improved by installation of sterilization equipment (e.g. UVGI, plasma air purifier, heat inactivation facilities, etc.). The selection and determination of effective adaptation measures should be a research focus of future HVAC systems. Another important question is how to operate the HVAC system in low energy consumption. A series of measures like natural ventilation (Aviv et al., 2021), heat recovery system or phase change materials for energy storage may be integrated to the HVAC systems. More research efforts should be made to enrich and improve current HVAC guidelines and to promote the technical measures being practiced in future engineering projects.
6. Conclusion
This paper roughly divides the probable aerosol transmission route of SARS-CoV-2 into three phases: (1) aerosol generation from an infected source, (2) aerosol dispersion and loss, and (3) inhalation, deposition and infection to susceptible host. As the understanding of the transmission mechanisms is essential for risk assessment and control, this paper comprehensively reviews the aerosol transmission characteristics of SARS-CoV-2 in each stage. Two infection risk models which can be used to evaluate the associations between ventilation and the probability of SARS-CoV-2 infection are discussed. The key parameters required by the two models are analyzed based on available literatures, which can provide a basis for SARS-CoV-2 risk assessment in ventilated context.
Aerosol transmission of SARS-CoV-2 can only proceed before all the three phases are completed, and this provides possibility to reduce the transmission risk by intervening each transmission phase with environmental control measures, including ventilation. The ultimate goal of ventilation applied in epidemic control is to reduce the intake dose of the exposed person. To reveal the impact of ventilation on the transmission process between the source and the receptor, three prevailing ventilation strategies are analyzed, which are mixing ventilation, displacement ventilation and personalized ventilation. It can be concluded that different air distribution strategies may influence the aerosol transmission route differently. For example, mixing ventilation can indirectly affect both the dispersion phase and the inhalation phase by diluting the overall pathogen concentration in the entire room. While personalized ventilation may directly intervene both the early stage of dispersion from the source (with PV or PE) and the inhalation by delivering clean air to the breathing zone of the receptor, which is expected to be a promising way for airborne infection control. The airflow pattern with ventilation serves as a very important factor in affecting the dispersion and distribution of exhaled aerosols in indoor environment and also directly or indirectly influences the inhalation of exposed occupants. Novel airflow patterns should be designed by combining the clear objective of epidemic control of airborne diseases to effectively and efficiently response to possible new outbreaks.
To better utilize ventilation or HVAC systems in protecting people against the aerosol transmission of COVID-19, the remaining challenges including novel ventilation design to mitigate airborne infection, effective integration of ventilation with other environmental control strategies and resilient HVAC system development to adapt both common and epidemic conditions should be further resolved. With the aid of interdisciplinary research and the development of intelligent technologies, these challenges can be addressed to form innovated HVAC system adapting both normal and epidemic situations and energy efficient in epidemic control.
Declaration of Competing Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgements
This project was financially supported by the National Natural Science Foundation of China (51808555), the Natural Science Foundation of Shandong Province (ZR2019MEE060), the Opening Fund of State Key Laboratory of Green Building in Western China (LSKF202014), the Fundamental Research Funds for the Central Universities (XZY032020029) and the Danish Agency for Higher Education and Science International Network Programme (case no. 0192-00036B).
References
- Abdullah H.K., Alibaba H. Open-plan office design for improved natural ventilation and reduced mixed mode supplementary loads. Indoor and Built Environment. 2020 doi: 10.1177/1420326x20953458. (online published) [DOI] [Google Scholar]
- Abkarian M., Stone H. Stretching and break-up of saliva filaments during speech: A route for pathogen aerosolization and its potential mitigation. Physical Review Fluids. 2020;5(10) doi: 10.1103/PHYSREVFLUIDS.5.102301. [DOI] [Google Scholar]
- Aganovic A., Cao G. Evaluation of airborne contaminant exposure in a single-bed isolation ward equipped with a protected occupied zone ventilation system. Indoor and Built Environment. 2019;28:1092–1103. doi: 10.1177/1420326X18823048. [DOI] [Google Scholar]
- Alford R., Kasel J., Gerone P., Knight V. Human influenza resulting from aerosol inhalation. Proceedings of the Society for Experimental Biology and Medicine. 1966;122:800–804. doi: 10.3181/00379727-122-31255. [DOI] [PubMed] [Google Scholar]
- Almstrand A., Bake B., Ljungström E., Larsson P., Bredberg A., Mirgorodskaya E., Olin A. Effect of airway opening on production of exhaled particles. Journal of Applied Physiology. 2010;108(3):584–588. doi: 10.1152/japplphysiol.00873.2009. [DOI] [PubMed] [Google Scholar]
- Anfinrud P., Stadnytskyi V., Bax C.E., Bax A. Visualizing speech-generated oral fluid droplets with laser light scattering. New England Journal of Medicine. 2020;382(21):2061–2063. doi: 10.1056/NEJMc2007800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ASHRAE . American Society of Heating, Refrigerating, and Air-conditioning Engineers, Inc., 2008; 2008. Ventilation of health care facilities. Tech. Rep. BSR/ASHRAE/ASHE Standard 170-2008. [Google Scholar]
- ASHRAE . American Society of Heating, Refrigerating, and Air-conditioning Engineers, Inc., 2016; 2016. Ventilation for acceptable indoor air quality. ASHRAE Standard 62.1-2016. [Google Scholar]
- ASHRAE . 2020. ASHRAE position document on infectious aerosols.https://www.ashrae.org/file%20library/about/position%20documents/pd_infectiousaerosols_2020.pdf [Google Scholar]
- Assaad D.A., Ghali K., Ghaddar N., Katramiz E., Ghani S. Evaluation of different personalized ventilation air terminal devices: Inhalation vs. clothing-mediated exposures. Building and Environment. 2021;192 doi: 10.1016/j.buildenv.2021.107637. [DOI] [Google Scholar]
- Aviv D., Chen K., Teitelbaum E., Sheppard D., Pantelic J., Rysanek A., Meggers F. A fresh (air) look at ventilation for COVID-19: Estimating the global energy savings potential of coupling natural ventilation with novel radiant cooling strategies. Applied Energy. 2021;292 doi: 10.1016/j.apenergy.2021.116848. 116848-116848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axley J.W., Emmerich S.J. A method to assess the suitability of a climate for natural ventilation of commercial buildings. Proceedings: Indoor Air (2002); Monterey, CA; 2002. [Google Scholar]
- Berlanga F.A., Olmedo I., de Adana M.R., Villafruela J.M., San José J.F., Castro F. Experimental assessment of different mixing air ventilation systems on ventilation performance and exposure to exhaled contaminants in hospital rooms. Energy & Buildings. 2018;177:207–219. doi: 10.1016/j.enbuild.2018.07.053. [DOI] [Google Scholar]
- Berry G., Parsons A., Morgan M., Rickert J., Cho H. A review of methods to reduce the probability of the airborne spread of COVID-19 in ventilation systems and enclosed spaces. Environmental Research. 2021 doi: 10.1016/j.envres.2021.111765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biswas, P., & Dhawan, S. (2020). Evaporation of emitted droplets are an important factor affecting the lifetime of the airborne coronavirus. 10.20944/preprints202004.0523.v1.
- Bjørn E., Nielsen P. Dispersal of exhaled air and personal exposure in displacement ventilated rooms. Indoor Air. 2002;12(3):147–164. doi: 10.1034/j.1600-0668.2002.08126.X. [DOI] [PubMed] [Google Scholar]
- Bolashikov Z., Melikov A. Methods for air cleaning and protection of building occupants from airborne pathogens. Building and Environment. 2009;44:1378–1385. doi: 10.1016/j.buildenv.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourouiba L. Turbulent Gas Clouds and Respiratory Pathogen Emissions: Potential Implications for Reducing Transmission of COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.4756. [DOI] [PubMed] [Google Scholar]
- Bourouiba L., Dehandschoewercker É., Bush J.M. Violent expiratory events: On coughing and sneezing. Journal of Fluid Mechanics. 2014;745:537–563. doi: 10.1017/jfm.2014.88. [DOI] [Google Scholar]
- Brohus H., Nielsen P. Personal Exposure in Displacement Ventilated Rooms. Indoor Air. 1996;6:157–167. doi: 10.1111/J.1600-0668.1996.T01-1-00003.X. [DOI] [PubMed] [Google Scholar]
- Bu Y., Ooka R., Kikumoto H., Oh W. Recent research on expiratory particles in respiratory viral infection and control strategies: A review. Sustainable Cities and Society. 2021;103106 doi: 10.1016/j.scs.2021.103106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buonanno G., Stabile L., Morawska L. Estimation of airborne viral emission: Quanta emission rate of SARS-CoV-2 for infection risk assessment. Environment International. 2020;141 doi: 10.1016/j.envint.2020.105794. 105794-105794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao G., Nielsen P.V., Jensen R.L., Heiselberg P., Liu L., Heikkinen J. Protected zone ventilation and reduced personal exposure to airborne cross-infection. Indoor Air. 2015;25:307–319. doi: 10.1111/ina.12142. [DOI] [PubMed] [Google Scholar]
- Cao G., Sirén K., Kilpeläinen S. Modelling and experimental study of performance of the protected occupied zone ventilation. Energy and Buildings. 2013;68:515–531. doi: 10.1016/j.enbuild.2013.10.008. [DOI] [Google Scholar]
- Cao S. Challenges of using CFD simulation for the design and online control of ventilation systems. Indoor and Built Environment. 2019;28:3–6. doi: 10.1177/1420326X18810568. [DOI] [Google Scholar]
- Cao S., Yu C., Luo X. New and emerging building ventilation technologies. Indoor and Built Environment. 2020;29:483–484. doi: 10.1177/1420326X20909092. [DOI] [Google Scholar]
- CDC . U.S. Department of Health and Human Services Centers for Disease Control and Prevention (CDC); USA: 2005. Guidelines for preventing the transmission of mycobacterium tuberculosis in health-care settings. [Google Scholar]
- Chao C., Wan M., Morawska L., Johnson G., Ristovski Z., Hargreaves M., Mengersen K., Corbett S., Li Y., Xie X., Katoshevski D. Characterization of expiration air jets and droplet size distributions immediately at the mouth opening. Journal of Aerosol Science. 2009;40(2):122–133. doi: 10.1016/j.jaerosci.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chau N., Hong N., Ngoc N.M., Thanh T.T., Khanh P.N., Nguyet L.A., Nhu L., Ny N., Man D.N., Hang V., Phong N., Que N.T., Tuyen P.T., Tu T.N., Hien T., Minh N.N., Hung L., Truong N., Yen L.…Tan L.V. Superspreading Event of SARS-CoV-2 Infection at a Bar, Ho Chi Minh City, Vietnam. Emerging Infectious Diseases. 2020;27:310–314. doi: 10.3201/eid2701.203480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen T., Feng Z., Cao S. The effect of vent inlet aspect ratio and its location on ventilation efficiency. Indoor and Built Environment. 2020;29:180–195. doi: 10.1177/1420326X19865930. [DOI] [Google Scholar]
- Chen W., Qian H., Zhang N., Liu F., Liu L., Li Y. Extended short-range airborne transmission of respiratory infections. Journal of Hazardous Materials. 2021;422 doi: 10.1016/j.jhazmat.2021.126837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chia P.Y., Coleman K.K., Tan Y.K., Ong S., Gum M., Lau S.K., Lim X., Lim A., Sutjipto S., Lee P.H., Son T.T., Young B.E., Milton D.K., Gray G.C., Schuster S., Barkham T., De P.P., Vasoo S., Chan M.…Marimuthu K. Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients. Nature Communications. 2020;11:2800. doi: 10.1038/s41467-020-16670-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong K., Ng C.S., Hori N., Yang R., Verzicco R., Lohse D. Extended lifetime of respiratory droplets in a turbulent vapor puff and its implications on airborne disease transmission. Physical Review Letters. 2021;126(3) doi: 10.1103/PhysRevLett.126.034502. [DOI] [PubMed] [Google Scholar]
- Correia G., Rodrigues L., Silva M.G., Gonçalves T. Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission. Medical Hypotheses. 2020;141 doi: 10.1016/j.mehy.2020.109781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa R., Bueno F., Albert E., Torres I., Carbonell-Sahuquillo S., Barrés-Fernández A., Sánchez D., Padrón C., Colomina J., Carreño M.I., Bretón-Martínez J.R., Martínez-Costa C., Navarro D. Upper respiratory tract SARS-CoV-2 RNA loads in symptomatic and asymptomatic children and adults. Clinical Microbiology and Infection. 2021 doi: 10.1016/j.cmi.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cravero C., Marsano D. Simulation of COVID-19 indoor emissions from coughing and breathing with air conditioning and mask protection effects. Indoor and Built Environment. 2021 doi: 10.1177/1420326X211039546. (online published) [DOI] [Google Scholar]
- Dai Y.W., Mak C.M., Ai Z.T. Computational fluid dynamics simulation of wind-driven inter-unit dispersion around multi-storey buildings: Upstream building effect. Indoor and Built Environment. 2019;28:217–234. doi: 10.1177/1420326X17745943. [DOI] [Google Scholar]
- Darquenne C. Aerosol deposition in health and disease. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2012;25(3):140–147. doi: 10.1089/jamp.2011.0916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darquenne C. Deposition Mechanisms. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2020;33:181–185. doi: 10.1089/jamp.2020.29029.cd. [DOI] [PubMed] [Google Scholar]
- Day W., Berendt R.F. Experimental tularemia in macaca mulatta: Relationship of aerosol particle size to the infectivity of airborne pasteurella tularensis. Infection and Immunity. 1972;5:77–82. doi: 10.1016/j.culher.2019.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng T., Shen X., Cheng X., Liu J. Investigation of window-opening behaviour and indoor air quality in dwellings situated in the temperate zone in China. Indoor and Built Environment. 2021;30(7):938–956. doi: 10.1177/1420326X20924746. [DOI] [Google Scholar]
- Deng X., Tan Z. Numerical analysis of local thermal comfort in a plan office under natural ventilation. Indoor and Built Environment. 2020;29:972–986. doi: 10.1177/1420326X19866497. [DOI] [Google Scholar]
- Dietz L., Horve P., Coil D., Fretz M., Eisen J., Wymelenberg K.G. 2019 novel coronavirus (COVID-19) pandemic: Built environment considerations to reduce transmission. mSystems. 2020:1–13. doi: 10.1128/mSystems.00245-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding J., Yu C., Cao S. HVAC systems for environmental control to minimize the COVID-19 infection. Indoor and Built Environment. 2020;29:1195–1201. doi: 10.1177/1420326X20951968. [DOI] [Google Scholar]
- van Doremalen N.V., Bushmaker T., Morris D.H., Holbrook M., Gamble A., Williamson B.N., Tamin A., Harcourt J., Thornburg N., Gerber S., Lloyd-Smith J., Wit E.D., Munster V. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. The New England Journal of Medicine. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas R.G. In: The influenza viruses and influenza. Kilbourne E.D., editor. 1975. Influenza in man; pp. 375–447. New York, NY. [Google Scholar]
- Duguid J. The size and the duration of air-carriage of respiratory droplets and droplet-nuclei. The Journal of hygiene. 1946;44:471–479. doi: 10.1017/S0022172400019288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dygert R.K., Dang T.Q. Mitigation of cross-contamination in an aircraft cabin via localized exhaust. Building and Environment. 2010;45(9):2015–2026. doi: 10.1016/j.buildenv.2010.01.014. [DOI] [Google Scholar]
- Fan D., Wang Q., Zhao L., Liu M. Status, standards, technologies and existing problems of residential ventilation in China. Indoor and Built Environment. 2020;29:485–495. doi: 10.1177/1420326X19862604. [DOI] [Google Scholar]
- Fears A.C., Klimstra W., Duprex P., Hartman A., Weaver S., Plante K., Mirchandani D., Plante J., Aguilar P., Fernández D., Nalca A., Totura A., Dyer D., Kearney B., Lackemeyer M., Bohannon J., Johnson R.F., Garry R., Reed D., Roy C. Comparative dynamic aerosol efficiencies of three emergent coronaviruses and the unusual persistence of SARS-CoV-2 in aerosol suspensions. medRxiv: The preprint Server for Health Sciences. 2020 doi: 10.1101/2020.04.13.20063784. [DOI] [Google Scholar]
- Feng Z., Cao S.J., Haghighat F. Removal of SARS-CoV-2 using UV+ Filter in built environment: Simulation/evaluation by utilizing validated numerical method. Sustainable Cities and Society. 2021;103226 doi: 10.1016/j.scs.2021.103226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Z., Cao S., Wang J., Kumar P., Haghighat F. Indoor airborne disinfection with electrostatic disinfector (ESD): Numerical simulations of ESD performance and reduction of computing time. Building and Environment. 2021;200 doi: 10.1016/j.buildenv.2021.107956. 107956-107956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Z., Wei F., Li H., Yu C.W. Evaluation of indoor disinfection technologies for airborne disease control in hospital. Indoor and Built Environment. 2021;30(6):727–731. doi: 10.1177/1420326X211002948. [DOI] [Google Scholar]
- Fu L., Nielsen P.V., Wang Y., Liu L. Measuring interpersonal transmission of expiratory droplet nuclei in close proximity. Indoor and Built Environment. 2021 doi: 10.1177/1420326X211029689. (online published) [DOI] [Google Scholar]
- Gao N., Niu J. Personalized ventilation for commercial aircraft cabins. Journal of Aircraft. 2007;45:508–512. doi: 10.2514/1.30272. [DOI] [Google Scholar]
- Gao N., Niu J., Morawska L. Distribution of respiratory droplets in enclosed environments under different air distribution methods. Building Simulation. 2008;1:326–335. doi: 10.1007/S12273-008-8328-0. [DOI] [Google Scholar]
- Ge H., Chen L., Xu C., Cui X. Large-eddy simulation of droplet-laden cough jets with a realistic manikin model. Indoor and Built Environment. 2021 doi: 10.1177/1420326X211032247. (online published) [DOI] [Google Scholar]
- Gebhar J., Anselm A., Heyder J., Stalhofen W. The human lung as aerosol particle Generator. Journal of Aerosol Medicine. 1998;1 [Google Scholar]
- Gidari A., Sabbatini S., Bastianelli S., Pierucci S., Busti C., Bartolini D., Stabile A., Monari C., Galli F., Rende M., Cruciani G., Francisci D. SARS-CoV-2 survival on surfaces and the effect of UV-C light. Viruses. 2021;13(3):408. doi: 10.3390/v13030408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gralton J., Tovey E., McLaws M., Rawlinson W. The role of particle size in aerosolised pathogen transmission: A review. The Journal of Infection. 2011;62:1–13. doi: 10.1016/j.jinf.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y., Qian H., Sun Z., Cao J., Liu F., Luo X., Ling R., Weschler L., Mo J., Zhang Y. Assessing and controlling infection risk with Wells-Riley model and spatial flow impact factor (SFIF) Sustainable Cities and Society. 2021;67 doi: 10.1016/j.scs.2021.102719. 102719-102719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Z., Wang Z., Zhang S., Li X., Li L., Li C., Cui Y., Fu R., Dong Y., Chi X., Zhang M., Liu K., Cao C., Liu B., Zhang K., Gao Y., Lu B., Chen W. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerging Infectious Diseases. 2020;26:1586–1591. doi: 10.3201/eid2607.200885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamner L., Dubbel P., Capron I., Ross A., Jordan A., Lee J., Lynn J., Ball A., Narwal S., Russell S., Patrick D., Leibrand H. High SARS-CoV-2 attack rate following exposure at a choir practice - Skagit County, Washington, March 2020. MMWR. Morbidity and mortality weekly report. 2020;69:606–610. doi: 10.15585/mmwr.mm6919e6. [DOI] [PubMed] [Google Scholar]
- Han Z., Weng W., Huang Q.Y. Characterizations of particle size distribution of the droplets exhaled by sneeze. Journal of The Royal Society Interface. 2013;10 doi: 10.1098/rsif.2013.0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hijnen D., Marzano A., Eyerich K., Geurtsvankessel C., Gimenez-Arnau A., Joly P., Vestergaard C., Sticherling M., Schmidt E. SARS-CoV-2 transmission from presymptomatic meeting attendee, Germany. Emerging Infectious Diseases. 2020;26:1935–1937. doi: 10.3201/eid2608.201235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds W.C. John Wiley & Sons, Inc.; New York, NY: 1999. Aerosol technology. [Google Scholar]
- Hou Y., Okuda K., Edwards C.E., Martinez D.R., Asakura T., Dinnon K., Kato T., Lee R.E., Yount B., Mascenik T., Chen G., Olivier K., Ghio A., Tse L.V., Leist S., Gralinski L.E., Schäfer A., Dang H., Gilmore R.…Baric R. SARS-CoV-2 reverse genetics reveals a variable infection gradient in the respiratory tract. Cell. 2020;182:429–446. doi: 10.1016/j.cell.2020.05.042. e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphrey S., Williamson R. A review of saliva: Normal composition, flow, and function. The Journal of prosthetic dentistry. 2001;85(2):162–169. doi: 10.1067/mpr.2001.113778. [DOI] [PubMed] [Google Scholar]
- Hwang S., Chang J.H., Oh B., Heo J. Possible aerosol transmission of COVID-19 associated with an outbreak in an apartment in Seoul, South Korea, 2020. International Journal of Infectious Diseases. 2021;104:73–76. doi: 10.1016/j.ijid.2020.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacot D., Greub G., Jaton K., Opota O. Viral load of SARS-CoV-2 across patients and compared to other respiratory viruses. Microbes and Infection. 2020;22:617–621. doi: 10.1016/j.micinf.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang S., Han S., Rhee J. Cluster of coronavirus disease associated with fitness dance classes, South Korea. Emerging Infectious Diseases. 2020;26:1917–1920. doi: 10.3201/eid2608.200633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennison M.W. Atomizing of mouth and nose secretions into the air as revealed by high-speed photography. Aerobiology. 1942;17:106–128. [Google Scholar]
- Jeong H., Kim S., Kim H., Kim Y., Kim J.H., Cho J., Kim S., Kang H., Kim S., Park S., Kim E., Choi Y.K. Viable SARS-CoV-2 in various specimens from COVID-19 patients. Clinical Microbiology and Infection. 2020;26:1520–1524. doi: 10.1016/j.cmi.2020.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia Y., Zheng X., Guan J., Tan X., Chen S., Qi B., Zheng H. Investigation of indoor total volatile organic compound concentrations in densely occupied university buildings under natural ventilation: Temporal variation, correlation and source contribution. Indoor and Built Environment. 2021;30:838–850. doi: 10.1177/1420326X20914000. [DOI] [Google Scholar]
- Jiang Y., Zhao B., Li X., Yang X., Zhang Z., Zhang Y. Investigating a safe ventilation rate for the prevention of indoor SARS transmission: An attempt based on a simulation approach. Building Simulation. 2009;2:281–289. doi: 10.1016/10.1007/s12273-009-9325-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson G., Morawska L. The mechanism of breath aerosol formation. Journal of aerosol medicine and pulmonary drug delivery. 2009;22(3):229–237. doi: 10.1089/JAMP.2008.0720. [DOI] [PubMed] [Google Scholar]
- Johnson G., Morawska L., Ristovski Z., Hargreaves M., Mengersen K., Chao C., Wan M., Li Y., Xie X., Katoshevski D., Corbett S. Modality of human expired aerosol size distributions. Journal of Aerosol Science. 2011;42:839–851. doi: 10.1016/J.JAEROSCI.2011.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones R.M., Brosseau L. Aerosol transmission of infectious disease. Journal of Occupational and Environmental Medicine. 2015;57:501–508. doi: 10.1097/JOM.0000000000000448. [DOI] [PubMed] [Google Scholar]
- Katelaris A., Wells J., Clark P., Norton S., Rockett R., Arnott A., Sintchenko V., Corbett S., Bag S. Epidemiologic evidence for airborne transmission of SARS-CoV-2 during church singing, Australia, 2020. Emerging Infectious Diseases. 2021;27:1677–1680. doi: 10.3201/eid2706.210465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katramiz E., Assaad D.A., Ghaddar N., Ghali K. The effect of human breathing on the effectiveness of intermittent personalized ventilation coupled with mixing ventilation. Building and Environment. 2020;174 doi: 10.1016/j.buildenv.2020.106755. [DOI] [Google Scholar]
- Kenarkoohi A., Noorimotlagh Z., Falahi S., Amarloei A., Mirzaee S.A., Pakzad I., Bastani E. Hospital indoor air quality monitoring for the detection of SARS-CoV-2 (COVID-19) virus. The Science of the Total Environment. 2020;748:141323–141324. doi: 10.1016/j.scitotenv.2020.141324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanh N.C., Thai P.Q., Quach H., Thi N.H., Dinh P.C., Duong T., Mai L., Nghia N.D., Tú T.A., Quang L., Quang T.D., Nguyen T., Vogt F., Anh D.D. Transmission of SARS-CoV 2 during long-haul flight. Emerging Infectious Diseases. 2020;26:2617–2624. doi: 10.3201/eid2611.203299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong X., Guo C., Lin Z., Duan S., He J., Ren Y., Ren J. Experimental study on the control effect of different ventilation systems on fine particles in a simulated hospital ward. Sustainable Cities and Society. 2021;73 doi: 10.1016/j.scs.2021.103102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kriegel M., Buchholz U., Gastmeier P., Bischoff P., Abdelgawad I., Hartmann A. Predicted infection risk for aerosol transmission of SARS-CoV-2. medRxiv. 2020 doi: 10.1101/2020.10.08.20209106. [DOI] [Google Scholar]
- Leith D.E., Butler J.P., Sneddon S.L., Brain J.D. Handbook of physiology. The respiratory system, V. III. Mechanics of breathing, part I. 1986. Cough. [Google Scholar]
- Lepore E., Benito P.A., Ramírez C.P., Viccione G. Indoors ventilation in times of confinement by SARS-CoV-2 epidemic: A comparative approach between Spain and Italy. Sustainable Cities and Society. 2021;103051 doi: 10.1016/j.scs.2021.103051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C., Tang H. Study on ventilation rates and assessment of infection risks of COVID-19 in an outpatient building. Journal of Building Engineering. 2021;103090 doi: 10.1016/j.jobe.2021.103090. [DOI] [Google Scholar]
- Li X., Yan S., Yu C. How far is demand-oriented ventilation from us? Indoor and Built Environment. 2020;29:917–920. doi: 10.1177/1420326X20922204. [DOI] [Google Scholar]
- Li X., Niu J., Gao N. Co-occupant's exposure to exhaled pollutants with two types of personalized ventilation strategies under mixing and displacement ventilation systems. Indoor Air. 2013;23(2):162–171. doi: 10.1111/ina.12005. [DOI] [PubMed] [Google Scholar]
- Li Y., Chen L. The relationship between the internal condition and the ventilation environment in a modular building. Indoor and Built Environment. 2021;30:375–390. doi: 10.1177/1420326X19893044. [DOI] [Google Scholar]
- Li Y., Leung G., Tang J., Yang X., Chao C., Lin J., Lu J., Nielsen P., Niu J., Qian H., Sleigh A., Su H., Sundell J., Wong T., Yuen P. Role of ventilation in airborne transmission of infectious agents in the built environment-a multidisciplinary systematic review. Indoor air. 2007;17:2–18. doi: 10.1111/J.1600-0668.2006.00445.X. [DOI] [PubMed] [Google Scholar]
- Li Y., Qian H., Hang J., Chen X., Cheng P., Ling H., Wang S., Liang P., Li J., Xiao S., Wei J., Liu L., Cowling B., Kang M. Probable airborne transmission of SARS-CoV-2 in a poorly ventilated restaurant. Building and Environment. 2021;196 doi: 10.1016/j.buildenv.2021.107788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang C., Melikov A.K., Li X. The influence of heat source distribution on the space cooling load oriented to local thermal requirements. Indoor and Built Environment. 2021;30(2):264–277. doi: 10.1177/1420326X19891632. [DOI] [Google Scholar]
- Licina D., Melikov A., Sekhar C., Tham K. Human convective boundary layer and its interaction with room ventilation flow. Indoor air. 2015;25(1):21–35. doi: 10.1111/ina.12120. [DOI] [PubMed] [Google Scholar]
- Lieber C., Melekidis S., Koch R., Bauer H. Insights into the evaporation characteristics of saliva droplets and aerosols: Levitation experiments and numerical modeling. Journal of Aerosol Science. 2021;154 doi: 10.1016/j.jaerosci.2021.105760. 105760-105760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Z., Wang J., Yao T., Chow T.T. Investigation into anti-airborne infection performance of stratum ventilation. Building and Environment. 2012;54:29–38. doi: 10.1016/j.buildenv.2012.01.017. [DOI] [Google Scholar]
- Lipinski T., Ahmad D., Serey N., Jouhara H. Review of ventilation strategies to reduce the risk of disease transmission in high occupancy buildings. International Journal of Thermofluids. 2020 doi: 10.1016/j.ijft.2020.100045. [DOI] [Google Scholar]
- Liu J., Li Z., Kim M., Zhu S., Zhang L., Srebric J. A comparison of the thermal comfort performances of a radiation floor cooling system when combined with a range of ventilation systems. Indoor and Built Environment. 2020;29:527–542. doi: 10.1177/1420326X19869412. [DOI] [Google Scholar]
- Liu W., You X.Y. Transportation and risk analysis of influenza indoor and outdoor transportation and exposure risk analysis of influenza aerosol. Indoor and Built Environment. 2012;21:614–621. doi: 10.1177/1420326X11426164. [DOI] [Google Scholar]
- Liu W., Zhang C., Li Y. Outdoor transportation of influenza virus under natural wind field. Indoor and Built Environment. 2020 doi: 10.1177/1420326x20951615. (online published) [DOI] [Google Scholar]
- Liu Y., Ning Z., Chen Y., Guo M., Liu Y., Gali N.K., Sun L., Duan Y., Cai J., Westerdahl D., Liu X., Xu K., Ho K., Kan H., Fu Q., Lan K. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020;582:557–560. doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- Lomas K.J., Ji Y. Resilience of naturally ventilated buildings to climate change: Advanced natural ventilation and hospital wards. Energy & Buildings. 2009;41(6):629–653. doi: 10.1016/j.enbuild.2009.01.001. [DOI] [Google Scholar]
- Lu J., Gu J., Li K., Xu C., Su W., Lai Z., Zhou D., Yu C., Xu B., Yang Z. COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerging Infectious Diseases. 2020;26:1628–1631. doi: 10.3201/eid2607.200764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J., Qi X., Chen H., Li X., Zhang Z., Wang H., Sun L., Zhang L., Guo J., Morawska L., Grinshpun S.A.Biswas.P., Flagan R.C., Yao M. Coronavirus disease 2019 patients in earlier stages exhaled millions of severe acute respiratory syndrome coronavirus 2 per hour. Clinical Infectious Diseases. 2021;72(10):e652–e654. doi: 10.1093/CID/CIAA1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik M., Kunze A., Bahmer T., Herget-Rosenthal S., Kunze T. SARS-CoV-2: Viral loads of exhaled breath and oronasopharyngeal specimens in hospitalized patients with COVID-19. International Journal of Infectious Diseases. 2021;110:105–110. doi: 10.1016/j.ijid.2021.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melikov A.K. Personalized ventilation. Indoor Air. 2004;14:157–167. doi: 10.1111/j.1600-0668.2004.00284.x. [DOI] [PubMed] [Google Scholar]
- Melikov A., Dzhartov V. Advanced air distribution for minimizing airborne cross-infection in aircraft cabins. HVAC&R Research. 2013;19:926–933. doi: 10.1080/10789669.2013.818468. [DOI] [Google Scholar]
- Melikov A. COVID-19: Reduction of airborne transmission needs paradigm shift in ventilation. Building and Environment. 2020;186 doi: 10.1016/j.buildenv.2020.107336. 107336-107336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller S.L., Nazaroff W., Jimenez J., Boerstra A., Buonanno G., Dancer S., Kurnitski J., Marr L., Morawska L., Noakes C. Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event. Indoor Air. 2020;31:314–323. doi: 10.1111/ina.12751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milton D.K., Fabian M.P., Cowling B.J., Grantham M.L., McDevitt J.J. Influenza virus aerosols in human exhaled breath: Particle size, culturability, and effect of surgical masks. PLoS Pathogens. 2013;9(3) doi: 10.1371/journal.ppat.1003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L. Droplet fate in indoor environments, or can we prevent the spread of infection? Indoor Air. 2006;16(5):335–347. doi: 10.1111/j.1600-0668.2006.00432.x. [DOI] [PubMed] [Google Scholar]
- Morawska L., Johnson G., Ristovski Z., Hargreaves M., Mengersen K., Corbett S., Chao C., Li Y., Katoshevski D. Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. Journal of Aerosol Science. 2009;40:256–269. doi: 10.1016/J.JAEROSCI.2008.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Tang J., Bahnfleth W., Bluyssen P., Boerstra A., Buonanno G., Cao J., Dancer S., Floto A., Franchimon F., Haworth C., Hogeling J., Isaxon C., Jimenez J., Kurnitski J., Li Y., Loomans M., Marks G., Marr L.…Yao M. How can airborne transmission of COVID-19 indoors be minimised? Environment International. 2020;142 doi: 10.1016/j.envint.2020.105832. 105832-105832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris D.H., Yinda K.C., Gamble A., Rossine F.W., Huang Q., Bushmaker T., Fischer R.J., Matson M., Doremalen N.V., Vikesland P., Marr L., Munster V., Lloyd-Smith J. The effect of temperature and humidity on the stability of SARS-CoV-2 and other enveloped viruses. bioRxiv: The Preprint Server for Biology. 2020 doi: 10.1101/2020.10.16.341883. [DOI] [Google Scholar]
- Mortazavi H., beni H.M., Aghaei F., Sajadian S.H. SARS-CoV-2 droplet deposition path and its effects on the human upper airway in the oral inhalation. Computer Methods and Programs in Biomedicine. 2020;200 doi: 10.1016/j.cmpb.2020.105843. 105843-105843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller N., Kunze M., Steitz F., Saad N., Mühlemann B., Beheim-Schwarzbach J., Schneider J., Drosten C., Murajda L., Kochs S., Ruscher C., Walter J., Zeitlmann N., Corman V. Severe acute respiratory ayndrome coronavirus 2 outbreak related to a nightclub, Germany, 2020. Emerging Infectious Diseases. 2020;27:645–648. doi: 10.3201/eid2702.204443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murakami S. Analysis and design of micro-climate around the human body with respiration by CFD. Indoor air. 2004;14:144–156. doi: 10.1111/J.1600-0668.2004.00283.X. [DOI] [PubMed] [Google Scholar]
- Murphy N., Boland M., Bambury N., Fitzgerald M., Comerford L., Dever N., O'Sullivan M., Petty-Saphon N., Kiernan R., Jensen M., O'Connor L. A large national outbreak of COVID-19 linked to air travel, Ireland, summer 2020. Eurosurveillance. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.42.2001624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicas M., Nazaroff W., Hubbard A. Toward understanding the risk of secondary airborne infection: Emission of respirable pathogens. Journal of Occupational and Environmental Hygiene. 2005;2:143–154. doi: 10.1080/15459620590918466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen P.V., Jiang H., Polak M. Proceedings of Roomvent 2007: Helsinki 13-15 June 2007. 2007. Bed with integrated personalized ventilation for minimizing cross infection; pp. 218–228. FINVAC ry. [Google Scholar]
- Nielsen P.V., Li Y., Buus M., Winther F.V. Risk of cross-infection in a hospital ward with downward ventilation. Building & Environment. 2010;45(9):2008–2014. doi: 10.1016/j.buildenv.2010.02.017. [DOI] [Google Scholar]
- Nielsen P.V., Zajas J.J., Litewnicki M., Jensen R.L. Breathing and cross-infection risk in the microenvironment around people. Ashrae Transactions. 2014:120. [Google Scholar]
- Nienaber F., Wolf S., Wesseling M.T., Calì D., Müller D., Madsen H. Validation, optimisation and comparison of carbon dioxide-based occupancy estimation algorithms. Indoor and Built Environment. 2020;29:820–834. doi: 10.1177/1420326X19871332. [DOI] [Google Scholar]
- Niu J., Gao N., Phoebe M., Huigang Z. Experimental study on a chair-based personalized ventilation system. Building and Environment. 2007;42:913–925. doi: 10.1016/j.buildenv.2005.10.011. [DOI] [Google Scholar]
- Olmedo I., Nielsen P., Adana M.R., Jensen R.L., Grzelecki P. Distribution of exhaled contaminants and personal exposure in a room using three different air distribution strategies. Indoor air. 2012;22(1):64–76. doi: 10.1111/j.1600-0668.2011.00736.x. [DOI] [PubMed] [Google Scholar]
- Olmedo I., Nielsen P.V., Adana M., Jensen R.L. The risk of airborne cross-infection in a room with vertical low-velocity ventilation. Indoor Air. 2013;23(1):62–73. doi: 10.1111/j.1600-0668.2012.00794.x. [DOI] [PubMed] [Google Scholar]
- Ong S.W., Tan Y.K., Chia P., Lee T., Ng O., Wong M., Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020 doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oropeza-Perez I., Østergaard P.A. Energy saving potential of utilizing natural ventilation under warm conditions-A case study of Mexico. Applied Energy. 2014;130:20–32. doi: 10.1016/J.APENERGY.2014.05.035. [DOI] [Google Scholar]
- Pantelic J., Sze-To G.N., Tham K., Chao C., Khoo Y. Personalized ventilation as a control measure for airborne transmissible disease spread. Journal of The Royal Society Interface. 2009;6:S715–S726. doi: 10.1098/rsif.2009.0311.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S., Kim Y., Yi S., Lee S., Na B., Kim C.B., Kim J., Kim H.S., Kim Y.B., Park Y., Huh I.S., Kim H.K., Yoon H., Jang H., Kim K., Chang Y., Kim I., Lee H., Gwack J.…Jeong E. Coronavirus disease outbreak in call center, South Korea. Emerging Infectious Diseases. 2020;26:1666–1670. doi: 10.3201/eid2608.201274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S., Choi Y., Song D., Kim E.K. Natural ventilation strategy and related issues to prevent coronavirus disease 2019 (COVID-19) airborne transmission in a school building. The Science of the Total Environment. 2021;789 doi: 10.1016/j.scitotenv.2021.147764. 147764-147764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson B., Wood R. Is cough really necessary for TB transmission? Tuberculosis (Edinburgh, Scotland) 2019;117:31–35. doi: 10.1016/j.tube.2019.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng Z., Jimenez J.L. Exhaled CO2 as a COVID-19 infection risk proxy for different indoor environments and activities. Environmental Science & Technology Letters. 2021;8(5):392–397. doi: 10.1021/acs.estlett.1c00183. [DOI] [PubMed] [Google Scholar]
- Phuong N.L., Khoa N.D., Ito K. Comparative numerical simulation of inhaled particle dispersion in upper human airway to analyse intersubject differences. Indoor and Built Environment. 2020;29:793–809. doi: 10.1177/1420326X19894128. [DOI] [Google Scholar]
- Qi D., Cheng J., Katal A., Wang L., Athienitis A. Multizone modelling of a hybrid ventilated high-rise building based on full-scale measurements for predictive control. Indoor and Built Environment. 2020;29:496–507. doi: 10.1177/1420326X19856405. [DOI] [Google Scholar]
- Qian H., Li Y., Nielsen P., Hyldgaard C.E., Wong T., Chwang A. Dispersion of exhaled droplet nuclei in a two-bed hospital ward with three different ventilation systems. Indoor Air. 2006;16(2):111–128. doi: 10.1016/10.1111/J.1600-0668.2005.00407.X. [DOI] [PubMed] [Google Scholar]
- Qian H., Nielsen P., Li Y., Hyldgaard C. Dispersion of exhalation pollutants in a two-bed hospital ward with a downward ventilation system. Building and Environment. 2005;43(2008):344–354. doi: 10.1016/j.buildenv.2006.03.025. [DOI] [Google Scholar]
- Rackes A., Melo A.P., Lamberts R. Naturally comfortable and sustainable: Informed design guidance and performance labeling for passive commercial buildings in hot climates. Applied Energy. 2016;174:256–274. doi: 10.1016/j.apenergy.2016.04.081. [DOI] [Google Scholar]
- Ram K., Thakur R., Singh D.K., Kawamura K., Shimouchi A., Sekine Y., Nishimura H., Singh S.K., Pavuluri C., Singh R.S., Tripathi S.N. Why airborne transmission hasn't been conclusive in case of COVID-19? An atmospheric science perspective. The Science of the Total Environment. 2021;773 doi: 10.1016/j.scitotenv.2021.145525. 145525-145525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razzini K., Castrica M., Menchetti L., Maggi L., Negroni L., Orfeo N., Pizzoccheri A., Stocco M., Muttini S., Balzaretti C. SARS-CoV-2 RNA detection in the air and on surfaces in the COVID-19 ward of a hospital in Milan, Italy. The Science of the Total Environment. 2020;742 doi: 10.1016/j.scitotenv.2020.140540. 140540-140540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren C., Cao S. Implementation and visualization of artificial intelligent ventilation control system using fast prediction models and limited monitoring data. Sustainable Cities and Society. 2020;52 doi: 10.1016/j.scs.2019.101860. [DOI] [Google Scholar]
- Ren C., Xi C., Wang J., Feng Z., Nasiri F., Cao S.J., Haghighat F. Mitigating COVID-19 infection disease transmission in indoor environment using physical barriers. Sustainable cities and society. 2021;74 doi: 10.1016/j.scs.2021.103175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezaei M., Netz R. Airborne virus transmission via respiratory droplets: Effects of droplet evaporation and sedimentation. Current Opinion in Colloid & Interface Science. 2021;55 doi: 10.1016/j.cocis.2021.101471. 101471-101471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley E., Murphy G., Riley R. Airborne spread of measles in a suburban elementary school. American Journal of Epidemiology. 1978;107:421–432. doi: 10.1093/oxfordjournals.aje.a112560. [DOI] [PubMed] [Google Scholar]
- Roy C.J., Milton D. Airborne transmission of communicable infection–the elusive pathway. The New England Journal of Medicine. 2004;350(17):1710–1712. doi: 10.1056/NEJMP048051. [DOI] [PubMed] [Google Scholar]
- Sandberg M., Kabanshi A., Wigö H. Is building ventilation a process of diluting contaminants or delivering clean air? Indoor and Built Environment. 2020;29:768–774. doi: 10.1177/1420326X19837340. [DOI] [Google Scholar]
- Santarpia J., Rivera D.N., Herrera V., Morwitzer M.J., Creager H., Santarpia G.W., Crown K., Brett-Major D., Schnaubelt E., Broadhurst M.J., Lawler J., Reid S., Lowe J. Transmission potential of SARS-CoV-2 in viral shedding observed at the University of Nebraska Medical Center. medRxiv. 2020 doi: 10.1101/2020.03.23.20039446. [DOI] [Google Scholar]
- Sha H., Xin Z., Qi D. Optimal control of high-rise building mechanical ventilation system for achieving low risk of COVID-19 transmission and ventilative cooling. Sustainable Cities and Society. 2021 doi: 10.1016/j.scs.2021.103256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen Y., Li C., Dong H., Wang Z., Martinez L., Sun Z., Handel A., Chen Z., Chen E., Ebell M., Wang F., Yi B., Wang H., Wang X., Wang A., Chen B., Qi Y., Liang L., Li Y.…Xu G. Community outbreak investigation of SARS-CoV-2 transmission among bus riders in eastern China. JAMA Internal Medicine. 2020;180:1665–1671. doi: 10.1001/jamainternmed.2020.5225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva M. An analysis of the transmission modes of COVID-19 in light of the concepts of indoor air quality. ResearchGate. 2020 doi: 10.13140/RG.2.2.28663.78240. [DOI] [Google Scholar]
- Slonim N.B., Chapin J.L. Saint Louis: The C.V. Mosby Company; 1967. Respiratory physiology. [Google Scholar]
- Smither S., Eastaugh L., Findlay J.S., Lever M. Experimental aerosol survival of SARS-CoV-2 in artificial saliva and tissue culture media at medium and high humidity. Emerging Microbes & Infections. 2020;9:1415–1417. doi: 10.1080/22221751.2020.1777906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sodiq A., Khan M., Naas M., Amhamed A. Addressing COVID-19 contagion through the HVAC systems by reviewing indoor airborne nature of infectious microbes: Will an innovative air recirculation concept provide a practical solution? Environmental Research. 2021;199 doi: 10.1016/j.envres.2021.111329. 111329-111329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stadnytskyi V., Bax C., Bax A., Anfinrud P. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proceedings of the National Academy of Sciences of the United States of America. 2020;117:11875–11877. doi: 10.1073/pnas.2006874117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stilianakis N., Drossinos Y. Dynamics of infectious disease transmission by inhalable respiratory droplets. Journal of The Royal Society Interface. 2010;7:1355–1366. doi: 10.1098/rsif.2010.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun C., Zhai Z. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustainable Cities and Society. 2020;62 doi: 10.1016/j.scs.2020.102390. 102390-102390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sznitman J. Respiratory microflows in the pulmonary acinus. Journal of Biomechanics. 2013;46(2):284–298. doi: 10.1016/j.jbiomech.2012.10.028. [DOI] [PubMed] [Google Scholar]
- Sze To G.N., Wan M., Chao C., Wei F., Yu S.C., Kwan J. A methodology for estimating airborne virus exposures in indoor environments using the spatial distribution of expiratory aerosols and virus viability characteristics. Indoor Air. 2008;18:425–438. doi: 10.1111/j.1600-0668.2008.00544.x. [DOI] [PubMed] [Google Scholar]
- Sze To G.N., Chao C. Review and comparison between the Wells–Riley and dose-response approaches to risk assessment of infectious respiratory diseases. Indoor Air. 2010;20:2–16. doi: 10.1111/j.1600-0668.2009.00621.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang S., Mao Y., Jones R.M., Tan Q., Shi X. Aerosol transmission of SARS-CoV-2? evidence, prevention and control. Environment International. 2020 doi: 10.1016/j.envint.2020.106039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian L., Lin Z., Wang Q. Experimental investigation of thermal and ventilation performances of stratum ventilation. Building and Environment. 2011;46:1309–1320. doi: 10.1016/j.buildenv.2011.01.002. [DOI] [Google Scholar]
- Vuorinen V., Aarnio M., Alava M., Alopaeus V., Atanasova N.S., Auvinen M., Balasubramanian N., Bordbar H., Erästö P., Grande R., Hayward N., Hellsten A., Hostikka S., Hokkanen J., Kaario O., Karvinen A., Kivistö I., Korhonen M., Kosonen R.…Österberg M. Modelling aerosol transport and virus exposure with numerical simulations in relation to SARS-CoV-2 transmission by inhalation indoors. Safety Science. 2020;130 doi: 10.1016/j.ssci.2020.104866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C.C., Prather K., Sznitman J., Jimenez J.L., Lakdawala S., Tufekci Z., Marr L. Airborne transmission of respiratory viruses. Science. 2021;373 doi: 10.1126/science.abd9149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Li Z., Zhang X., Zhu L., Liu Y., Wang S. The motion of respiratory droplets produced by coughing. Physics of Fluids. 2020;32(12) doi: 10.1063/5.0033849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Wang G., Li X. Image-based occupancy positioning system using pose-estimation model for demand-oriented ventilation. Journal of Building Engineering. 2021;39 doi: 10.1016/J.JOBE.2021.102220. [DOI] [Google Scholar]
- Wang J. Vision of China's future urban construction reform: In the perspective of comprehensive prevention and control for multi disasters. Sustainable Cities and Society. 2020;64 doi: 10.1016/j.scs.2020.102511. 102511-102511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Cao S., Yu C. Development trend and challenges of sustainable urban design in the digital age. Indoor and Built Environment. 2020;30:3–6. doi: 10.1177/1420326X20976058. [DOI] [Google Scholar]
- Wang J., Huang J., Feng Z., Cao S., Haghighat F. Occupant-density-detection based energy efficient ventilation system: Prevention of infection transmission. Energy & Buildings. 2021;240 doi: 10.1016/j.enbuild.2021.110883. 110883-110883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang T., Yin W., Fu L., Zhang Z. Estimation model for natural ventilation by wind force considering wind direction and building orientation for low-rise building in China. Indoor and Built Environment. 2020 doi: 10.1177/1420326x20944983. (online published) [DOI] [Google Scholar]
- Weber T.P., Stilianakis N. Inactivation of influenza A viruses in the environment and modes of transmission: A critical review. The Journal of Infection. 2008;57:361–373. doi: 10.1016/j.jinf.2008.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei J., Li Y. Enhanced spread of expiratory droplets by turbulence in a cough jet. Building and Environment. 2015;93:86–96. doi: 10.1016/j.buildenv.2015.06.018. [DOI] [Google Scholar]
- Wei J., Guo Y., Lei H., Wang L., Jin T., Tang L. Numerical investigation on the origin of virus-laden droplets in the respiratory tract. Chinese Science Bulletin. 2021;66:486–492. doi: 10.1360/TB-2020-0811. [DOI] [Google Scholar]
- Wells W. On air-borne infection. Study II. Droplets and Droplet nuclei. American Journal of Epidemiology. 1934;20:611–618. doi: 10.1093/oxfordjournals.aje.a118097. [DOI] [Google Scholar]
- Wen Y., Leng J., Yu F., Yu C.W. Integrated design for underground space environment control of subway stations with atriums using piston ventilation. Indoor and Built Environment. 2020;29:1300–1315. doi: 10.1177/1420326X20941349. [DOI] [Google Scholar]
- Wells W. Cambridge University Press; Cambridge, MA: 1955. Airborne contagion and air hygiene; pp. 117–122. [DOI] [Google Scholar]
- Wu Y., Gao N., Niu J., Zang J., Cao Q. Numerical study on natural ventilation of the wind tower: Effects of combining with different window configurations in a low-rise house. Building and Environment. 2021;188 doi: 10.1016/j.buildenv.2020.107450. [DOI] [Google Scholar]
- WHO . In: WHO Publication/Guidelines. Atkinson J., Chartier Y., Pessoa-Silva C., Jensen P., Li Y., et al., editors. WHO Press; Geneva, Switzerland: 2009. Natural ventilation for infection control in health-care settings. [PubMed] [Google Scholar]
- WHO . 2020. Infection Prevention and Control during Health Care when COVID-19 Is Suspected: Interim Guidance, 19 March 2020. [Google Scholar]
- WHO . 2021. Coronavirus disease (COVID-19): How is it transmitted?https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-how-is-it-transmitted Assessed August 1, 2021. [Google Scholar]
- Wölfel R., Corman V., Guggemos W., Seilmaier M., Zange S., Müller M., Niemeyer D., Jones T., Vollmar P., Rothe C., Hoelscher M., Bleicker T., Brünink S., Schneider J., Ehmann R., Zwirglmaier K., Drosten C., Wendtner C. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- Xie C., Jiang L., Huang G., Pu H., Gong B., Lin H., Ma S., Chen X., Long B., Si G., Yu H., Jiang L., Yang X., Shi Y., Yang Z. Comparison of different samples for 2019 novel coronavirus detection by nucleic acid amplification tests. International Journal of Infectious Diseases. 2020;93:264–267. doi: 10.1016/j.ijid.2020.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X., Li Y., Chwang A.T., Ho P., Seto W. How far droplets can move in indoor environments–revisiting the Wells evaporation-falling curve. Indoor air. 2007;17(3):211–225. doi: 10.1111/j.1600-0668.2007.00469.x. [DOI] [PubMed] [Google Scholar]
- Xu C., Nielsen P., Gong G., Jensen R.L., Liu L. Influence of air stability and metabolic rate on exhaled flow. Indoor air. 2015;25(2):198–209. doi: 10.1111/ina.12135. [DOI] [PubMed] [Google Scholar]
- Xu C., Liu L. Personalized ventilation: One possible solution for airborne infection control in highly occupied space? Indoor and Built Environment. 2018;27:873–876. doi: 10.1177/1420326X18777383. [DOI] [Google Scholar]
- Xu C., Nielsen P., Liu L., Jensen R.L., Gong G. Impacts of airflow interactions with thermal boundary layer on performance of personalized ventilation. Building and Environment. 2018;135:31–41. doi: 10.1016/J.BUILDENV.2018.02.048. [DOI] [Google Scholar]
- Xu C., Luo X., Yu C., Cao S.J. The 2019-nCoV epidemic control strategies and future challenges of building healthy smart cities. Indoor and Built Environment. 2020;29:639–644. doi: 10.1177/1420326X20910408. [DOI] [Google Scholar]
- Xu C., Wei X., Liu L., Su L., Liu W., Wang Y., Nielsen P. Effects of personalized ventilation interventions on airborne infection risk and transmission between occupants. Building and Environment. 2020;180 doi: 10.1016/j.buildenv.2020.107008. 107008-107008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu C., Liu W., Liu L., Cao S., Ren Y. Non-uniform risk assessment methods for personalized ventilation on prevention and control of COVID-19. Kexue Tongbao/Chinese Science Bulletin. 2021;66(4-5) doi: 10.1360/TB-2020-0830. [DOI] [Google Scholar]
- Xu J., Wang C., Fu S., Chan K.C., Chao C. Short-range bioaerosol deposition and inhalation of cough droplets and performance of personalized ventilation. Aerosol Science and Technology. 2021;55:474–485. doi: 10.1080/02786826.2020.1870922. [DOI] [Google Scholar]
- Yang B., Melikov A.K., Kabanshi A., Zhang C., Bauman F.S., Cao G., Awbi H., Wigöd H., Niu J., Cheong K.W.D., Tham K.W., Sandberg M., Nielsen P.V., Kosonen R., Yao R., Kato S., Sekhar S.C., Schiavon S., Karimipanah T.…Lin Z. A review of advanced air distribution methods - theory, practice, limitations and solutions. Energy & Buildings. 2019 doi: 10.1016/j.enbuild.2019.109359. [DOI] [Google Scholar]
- Yang J., Sekhar S.C., Cheong K.W.D., Raphael B. Performance evaluation of a novel personalized ventilation-personalized exhaust system for airborne infection control. Indoor Air. 2015;25(2):176–187. doi: 10.1111/ina.12127. [DOI] [PubMed] [Google Scholar]
- Yu I.T., Li Y., Wong T.W., Tam W., Chan A.T., Lee J.H., Leung D.Y., Ho T. Evidence of airborne transmission of the severe acute respiratory syndrome virus. The New England Journal of Medicine. 2004;350(17):1731–1739. doi: 10.1056/NEJMoa032867. [DOI] [PubMed] [Google Scholar]
- Yun H., Yang J., Seo J., Sohn J. Methodology for sampling and detection of airborne coronavirus including SARS-CoV-2. Indoor and Built Environment. 2020 doi: 10.1177/1420326x20980160. (online published) [DOI] [Google Scholar]
- Zhai Z., Li H. Distributed probability of infection risk of airborne respiratory diseases. Indoor and Built Environment. 2021 doi: 10.1177/1420326X211030324. (online published) [DOI] [Google Scholar]
- Zhang B., Guo G., Zhu C., Ji Z., Lin C.H. Transport and trajectory of cough-induced bimodal aerosol in an air-conditioned space. Indoor and Built Environment. 2020 doi: 10.1177/1420326X20941166. 1420326X20941166. [DOI] [Google Scholar]
- Zhang S., Lin Z. Dilution-based evaluation of airborne infection risk-Thorough expansion of Wells-Riley model. Building and Environment. 2021;194 doi: 10.1016/j.buildenv.2021.107674. 107674-107674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao W., Kilpeläinen S., Kosonen R., Jokisalo J. Experimental comparison of local low velocity unit combined with radiant panel and diffuse ceiling ventilation systems. Indoor and Built Environment. 2020;29:895–914. doi: 10.1177/1420326X20918398. [DOI] [Google Scholar]
- Zhao W., Lestinen S., Kilpeläinen S., Kosonen R. An experimental study of the influence of a moving person on airflow characteristics and thermal conditions with diffuse ceiling ventilation. Indoor and Built Environment. 2020;29:860–880. doi: 10.1177/1420326X20917202. [DOI] [Google Scholar]
- Zheng W., Hu J., Wang Z., Li J., Fu Z., Li H., Jurasz J., Chou S., Yan J. COVID-19 Impact on Operation and Energy Consumption of Heating, Ventilation and Air-Conditioning (HVAC) Systems. Advances in Applied Energy. 2021;3 doi: 10.1016/j.adapen.2021.100040. 100040-100040. [DOI] [Google Scholar]
- Zhu H.C., Yu C.W., Cao S.J. Ventilation online monitoring and control system from the perspectives of technology application. Indoor and Built Environment. 2020;29(4):587–602. doi: 10.1177/1420326X19878586. [DOI] [Google Scholar]
- Zivelonghi A., Lai M. Mitigating aerosol infection risk in school buildings: The role of natural ventilation, volume, occupancy and CO2 monitoring. Building and Environment. 2021;204 doi: 10.1016/j.buildenv.2021.108139. [DOI] [Google Scholar]
- Zou L., Ruan F., Huang M., Liang L., Huang H., Hong Z., Yu J., Xia J., Guo Q., Yen H., Wu J. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. The New England Journal of Medicine. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]