Introduction
Pyoderma gangrenosum (PG) is a rare, inflammatory neutrophilic dermatosis that can have extracutaneous manifestations.1 Here, we present a patient with psoriasis on ixekizumab who first presented with a vaginal cuff abscess, with subsequent development of skin lesions on the hands, feet, and face. She was diagnosed with PG, initially treated with cyclosporine, and transitioned to adalimumab, with resolution of the cutaneous lesions and associated pain.
Case report
We present a 61-year-old woman with a past medical history of psoriasis and a surgical history of a vaginal hysterectomy 20 years prior and sacrospinous ligament suspension for pelvic organ prolapse 15 years earlier. She was admitted for a 9-month history of sanguinopurulent vaginal discharge, dyspareunia, and cutaneous ulcers, which were associated with persistent low-grade fevers, chills, fatigue, poor appetite, weight loss, and weakness. The patient initially presented to an outside urogynecology clinic 1 month after symptom onset (8 months prior to this admission), where an “infected stitch” was removed using sacrospinous ligament suspension. Over the next 7 months, the patient completed courses of ciprofloxacin, sulfamethoxazole-trimethoprim, and nitrofurantoin, without improvement. She was evaluated by a second gynecologist more than 8 months after symptom onset. Vaginal cultures grew Bacteroides (species unknown), and abdominal and pelvic magnetic resonance imaging revealed right-sided hydronephrosis secondary to an abnormal vaginal process, including marked thickening, enhancement, and areas of ill-defined fluid. Because of these results, she was started on levofloxacin and metronidazole. During this antibiotic course, painful pustular lesions on the patient's face, hands, and feet, and she was admitted for possible infectious endocarditis. Of note, the patient had a 2-year history of scalp psoriasis refractory to topical corticosteroids and was being treated with ixekizumab for approximately 1 year. Approximately 2 months prior to admission, the medication was discontinued by the patient. Upon admission, the patient was started on vancomycin; subsequently, antibacterial coverage was broadened with the addition of metronidazole and ceftriaxone. Transesophageal and thoracic echocardiograms showed no valvular vegetations.
With continued purulent drainage, the patient underwent vaginal washout and an examination, which revealed no necrotizing infection. Three stitches from the previous procedures were removed, a pocket of pus was drained during the procedure, and a ureteral stent was placed for the treatment of hydronephrosis. At this time, the cutaneous lesions were incised and drained. Blood cultures (×3), cutaneous wound cultures (×2), and vaginal tissue culture (×1) showed no growth. The results of tests for cryptococcal and histoplasma antigens and anti-Blastomyces antibody were negative.
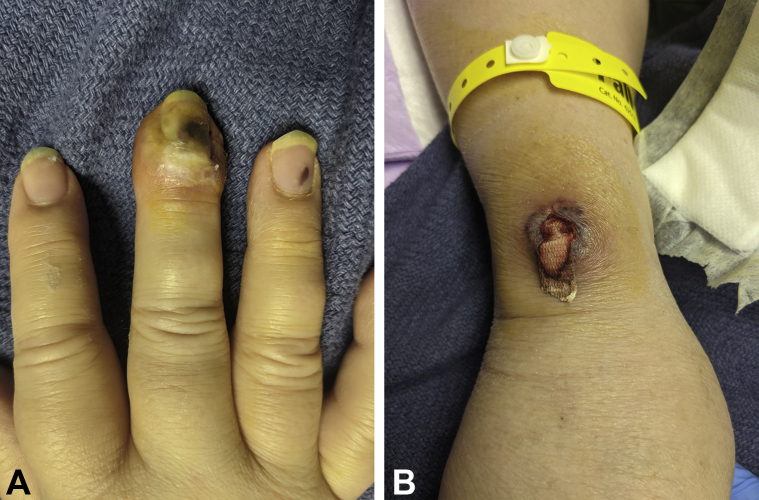
Upon examination, the patient was found to have numerous scattered violaceous-to-red papulonodules, some of which were pustular, on the face (Fig 1), dorsal and ventral aspects of the fingers, medial aspect of the palm, and plantar aspect of the feet (Fig 2). Punch biopsies of the lesion on the right wrist were performed: 1 for a histopathologic review and another for tissue culture. The tissue cultures grew no organisms. Hematoxylin-eosin staining revealed a predominantly neutrophilic infiltrate. The results of staining for microorganisms were negative.
Fig 1.
Pyoderma gangrenosum. On the left cheek, there is an ulcer with violaceous, undermined borders with a central clot.
Fig 2.
A, Pyoderma gangrenosum. On the right third finger, there is a periungual, violaceous, and pustular papulonodule. There is proximal onycholysis with a lake of pus. B, An ulcerated plaque with violaceous undermined borders on the dorsal aspect of the right wrist.
The morphology of the cutaneous lesions, the vaginal cuff findings, and the lack of evidence of an infectious etiology were believed to be most consistent with a diagnosis of PG. We considered the possibility that these lesions were extracutaneous manifestations of inflammatory bowel disease (IBD). However, the patient did not report any gastrointestinal symptoms consistent with those of IBD. The calprotectin levels were within normal limits, and she had no anti-Saccharomyces antibodies. With a presumptive diagnosis of PG, the patient was started on 2-3 mg/kg of cyclosporine; she experienced rapid improvement of the cutaneous lesions and pain as well as improvement of her vaginal discharge. After 2 months of cyclosporine administration, adalimumab was added at psoriasis dosing, and remission was maintained when cyclosporine was stopped after 3 months of treatment.
Discussion
Vaginal PG has been rarely reported in the literature and is often initially mistaken for an infection,2 resulting in ineffective treatment, including antibiotic therapy and/or surgical intervention. Vaginal PG can present after a hysterectomy2 or cone biopsy.3
Importantly, the patient presented in this case report had been treated with ixekizumab for psoriasis, raising the possibility of drug-induced PG. PG in the setting of interleukin (IL) 17 inhibition has been reported in a patient with psoriasis treated with secukinumab.4 Ixekizumab, like secukinumab, is a humanized monocloncal antibody (immunoglobulin G) that selectively binds IL-17A and is a Food and Drug Administration-approved medication for the treatment of moderate-to-severe plaque psoriasis. The common adverse effects of ixekizumab include neutropenia and hypersensitivity reactions. To the best of our knowledge, this is the first published case of ixekizumab-associated PG.
Mechanistically, it has been postulated that IL-17A inhibition leads to paradoxical IL-23 upregulation due to disruption of the IL-23/IL-17A axis. This upregulation may be critical for the subsequent development of PG in these patients because PG lesions have been shown to contain high levels of IL-23.5 Additionally, treatment with ustekinumab, an IL-12/IL-23 antibody, has been shown to markedly improve these lesions.5 Further laboratory and clinical research is needed to elucidate the mechanism by which IL-17 inhibition leads to the subsequent development of PG in patients with psoriasis.
Interestingly, IL-17 inhibition has been known to be broadly associated with the onset of paradoxical inflammatory disease, although cumulative risk data are yet to be compiled. Clinical trial data have revealed reports of newly diagnosed IBD or IBD exacerbation in patients with psoriasis, rheumatoid arthritis, and ankylosing spondylitis receiving anti-IL-17 therapies.6 Specifically, brodalumab, ixekizumab, and secukinumab have been studied and found to be associated with cases of new-onset IBD, even in patients with no family history or previous gastrointestinal symptoms. Although IL-17 inhibition is associated with a low incidence of IBD in patients with rheumatologic or dermatologic autoimmune disease,6 it is worth exploring possible parallels in the pathomechanism underlying the development of PG in this patient population. Moreover, it is well established that PG can present as a severe extraintestinal manifestation of IBD, further suggesting commonalities in the underlying pathophysiology. Although IL-17 inhibition may have had a role in the development of PG in this patient, pathergy due to an old suture or an infection might have also led to the development of the initial vaginal cuff PG. The diagnosis of PG remains a challenge, especially in patients presenting with extracutaneous involvement.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Borda L.J., Wong L.L., Marzano A.V., Ortega-Loayza A.G. Extracutaneous involvement of pyoderma gangrenosum. Arch Dermatol Res. 2019;311(6):425–434. doi: 10.1007/s00403-019-01912-1. [DOI] [PubMed] [Google Scholar]
- 2.Güth U., Wagner S., Huang D.J., Hess T.H. Pyoderma gangrenosum of the vaginal vault after vaginal hysterectomy: only the correct diagnosis of a rare entity can prevent long-term morbidity. Arch Gynecol Obstet. 2013;288(1):79–82. doi: 10.1007/s00404-012-2692-9. [DOI] [PubMed] [Google Scholar]
- 3.Lilford R.J., Tindall V.R., Batchelor A.G. Post-surgical pyoderma gangrenosum of the vaginal vault associated with ulcerative colitis and Behcet's disease; a case report. Eur J Obstet Gynecol Reprod Biol. 1989;31(1):93–94. doi: 10.1016/0028-2243(89)90030-0. [DOI] [PubMed] [Google Scholar]
- 4.Petty A.J., Whitley M.J., Balaban A., Ellington K., Marano A.L. Pyoderma gangrenosum induced by secukinumab in a patient with psoriasis successfully treated with ustekinumab. JAAD Case Rep. 2020;6(8):731–733. doi: 10.1016/j.jdcr.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guenova E., Teske A., Fehrenbacher B. Interleukin 23 expression in pyoderma gangrenosum and targeted therapy with ustekinumab. Arch Dermatol. 2011;147(10):1203–1205. doi: 10.1001/archdermatol.2011.168. [DOI] [PubMed] [Google Scholar]
- 6.Yamada A., Wang J., Komaki Y., Komaki F., Micic D., Sakuraba A. Systematic review with meta-analysis: risk of new onset IBD with the use of anti-interleukin-17 agents. Aliment Pharmacol Ther. 2019;50(4):373–385. doi: 10.1111/apt.15397. [DOI] [PubMed] [Google Scholar]