Abstract
Adverse birth outcomes put children at increased risk of poor future health. They also put families under sudden socioeconomic and psychological strain, which has poorly understood consequences. We tested whether infants experiencing an adverse birth outcome—low birthweight or prematurity, as well as lengthy hospital stays—were more likely to be evicted in early childhood, through age 5 years. We analyzed 5,655 observations contributed by 2,115 participants in the Fragile Families and Child Wellbeing Study—a national, randomly sampled cohort of infants born in large US cities between 1998 and 2000—living in rental housing at baseline. We fitted proportional hazards models using piecewise logistic regression, controlling for an array of confounders and applying inverse probability of selection weights. Having been born low birthweight or preterm was associated with a 1.74-fold increase in children’s hazard of eviction (95% confidence interval: 1.02, 2.95), and lengthy neonatal hospital stays were independently associated with a relative hazard of 2.50 (95% confidence interval: 1.15, 5.44) compared with uncomplicated births. Given recent findings that unstable housing during pregnancy is associated with adverse birth outcomes, our results suggest eviction and health may be cyclical and co-constitutive. Children experiencing adverse birth outcomes are vulnerable to eviction and require additional supports.
Keywords: birth, children, cities, eviction, housing, low birthweight, prematurity, selection
Abbreviations
- CI
confidence interval
- FFCWS
Fragile Families and Child Wellbeing Study
- HR
hazard ratio
- LBW
low birthweight
Infants born with adverse birth outcomes are at heightened risk of poor health as they age. Research on the long-term health impacts of these outcomes, which has tended to focus on low birthweight (LBW) or prematurity (e.g., studies from the US Environmental Protection Agency (1), Sapkota et al (2), and Blumenshine et al (3)) has shown that infants born too light or too early are at higher risk of impaired growth, neurodevelopmental impairment, childhood hospitalization, cardiovascular disease, diabetes, nephropathy, and poor mental health in adulthood, among other conditions (4–7).
Less is known about the socioeconomic strain adverse birth outcomes place on families (8–11), which may itself impose consequences for health and well-being (12, 13). This strain includes direct out-of-pocket medical expenditures, lost wages from being out of work to care for sick children, and travel costs of hospital visitation (8, 10). Adverse birth outcome–related socioeconomic strain can be acute (related directly to the birth) or chronic, with families experiencing repeated financial shocks related to higher rates of childhood illness and disability (10). On the acute end, a 2005 study of US families found out-of-pocket health care costs for LBW or preterm infants in their first year of life totaled $1,987 on average, more than 3 times the average for infants with uncomplicated births ($654) (8). Infants born with other medical complications also had higher average out-of-pocket costs, at $953. Expenses increased when prescription and maternal care costs were included. Lost wages and benefits for mothers of LBW/preterm infants were also substantial, at an average of $1,513 (10); findings of a Finnish study suggest even higher wage losses during infants’ second year, indicating serious financial consequences for chronic health issues in early childhood (9). Such financial shocks may not be manageable for lower-income families in a country like the United States, where the median household in the poorest quintile of income earners has $0 in savings (14). Sudden and recurring costs may be especially difficult to navigate while burdened by the immense psychological toll of parenting a sick newborn (15).
We use data from the Fragile Families and Child Wellbeing Study (FFCWS)—a national, randomly selected, urban birth cohort—to examine whether adverse birth outcomes are associated with risk of eviction during early childhood. This study comes after reporting of recent findings, including from a study that used the same data, that unstable housing during pregnancy is associated with an increased risk of being born preterm or low birthweight (16–18). Here, we examined the reverse, assessing whether adverse birth outcomes (namely, LBW/prematurity or other intensive neonatal medical needs) put families at heightened risk of eviction.
At issue is whether the costs of adverse birth outcomes are enough to push families out of good standing on their rental payments and out of their homes. If so, evictions resulting from adverse birth would exacerbate affected children’s heightened medical and socioeconomic vulnerabilities and further jeopardize their well-being. Eviction is theorized to harm health both directly (e.g., the mental health repercussions of losing one’s home (19)) and indirectly, shunting families into lower-quality housing and underserved neighborhoods, negatively affecting their finances, and disrupting social networks (20–23).
Because of the long-term impact of poor health in childhood on adult outcomes and the greater sensitivity of children to environmental insults (24–28), eviction during childhood may be uniquely harmful, though direct evidence on this hypothesis is sparse. In only a handful of studies have researchers examined the fallout of eviction for youth, connecting eviction to increased risk of childhood lead poisoning (29), food insecurity (30), poor parent-rated health (31), and, with ecological data, rates of child abuse (32). Any impacts, even small ones, may have a sizeable effect on population health, because 1 in 7 babies born to low-income mothers has low birthweight and/or is preterm (33).
METHODS
Data collection
We analyzed data from the FFCWS, a birth cohort of a random sample of babies born between 1998 and 2000 in large US cities. A multistage sampling design was used for the FFCWS, whereby 20 large cities, 75 hospitals within those cities, and 4,898 infants within those hospitals were sampled in succession. Baseline and follow-up interviews were conducted with the children’s biological parents and primary caregivers, as well as (at appropriate ages) the children themselves; follow-up interviews occurred approximately at ages 1, 3, 5, 9, and 15 years. By design, infants born to unmarried mothers were oversampled; low-income families were well represented. Details about the FFCWS are available elsewhere (34).
For the present study, we tracked FFCWS participants’ eviction trajectories during early childhood, from birth through age 5 years. Four inclusion criteria applied (Figure 1). First, 109 children were sampled as part of a prestudy, not as part of the national random sample; these children were excluded. Second, most birth complication and prior medical history data available in the FFCWS were collected from medical records. We thus limited our analysis to the 77% of participants (n = 3,676) whose infant and maternal medical records were extracted. Medical records missingness was largely driven by hospital nonparticipation or trouble locating records (67% of the time), as opposed to mothers personally declining consent (33%). Third, to align with prior literature that was focused on rental eviction (as opposed to foreclosure), we limited our sample to those 2,395 children with medical records whose families were renting at baseline. Fourth, because some of these children were censored before we could observe their eviction outcomes, our outcome models were run only on 5,655 observations contributed by 2,115 children with at least 1 wave of complete eviction data.
Figure 1.
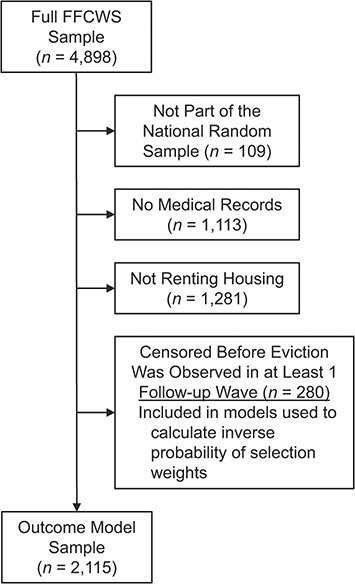
Flow diagram of sample inclusion criteria (n = 2,115), Fragile Families and Child Wellbeing Study (children born 1998–2000).
We defined 2 exposures. Our first exposure was a binary variable representing whether infants were born preterm (<37 weeks) and/or low birthweight (<2,500 g), or not. Our second exposure, which may also be a mediator between LBW/preterm and eviction, was defined as an infant hospital stay of 1 week or longer, which we used as a proxy for extreme or extended medical need. Because we had little information on the severity of newborns’ health problems other than whether infants experienced (binary: yes/no) each of a (somewhat arbitrary) set of complications during birth, and because infants’ health trajectories after many specific complications are extremely heterogeneous, a lengthy hospital stay allowed us to capture extreme or extended medical need despite limited available complications data. We used 1 week or longer because nearly all study infants (97%) who did not require neonatal intensive unit care left the hospital by this time, compared with only 53% of those who required neonatal intensive unit care. This standard contrasts with the legal standard for how long a hospital must allow a mother and child to stay in hospital after a birth (i.e., 2 days for a vaginal birth, 4 days for a cesarean (35)), which is sometimes used to define extended hospital stays (36). For our purposes, however, that standard was less helpful because it was not meant to identify infants with heightened medical needs, nor was it based on population-level research (37). The legal standard also had lower sensitivity than our 1-week standard when predicting which infants were born with an array of medical complications (see Web Table 1) (available at https://doi.org/10.1093/aje/kwab007).
Our outcome is eviction from rental housing during early childhood. In each follow-up wave, parents were asked whether they had been “evicted from their home or apartment for not paying the rent or mortgage” in the past 12 months. We coded children as evicted if the parent they lived with at least half of the time (defaulting to their mother) reported being evicted in any wave through age 5 years, with the earliest wave at which they reported being evicted serving as their event time in our survival analysis.
Statistical analysis
To estimate the discrete hazard of eviction (i.e., the probability of being evicted in any given wave conditional on having not been evicted in an earlier wave), we fitted a proportional hazards model, using inverse probability of selection weights to account for loss to follow-up. We fitted 3 models: (1) an unweighted model for eviction, predicted by LBW/prematurity only; (2) a weighted model for eviction, predicted by LBW/prematurity and potential confounders; and (3) a weighted model for eviction, predicted by LBW/prematurity, a lengthy hospital stay, an interaction between the 2, and potential confounders.
We fitted model 2 (including only LBW/preterm and excluding hospital stay) followed by model 3 (including both LBW/preterm and hospital stay), because we conceptualized a lengthy hospital stay as a potential mediator of the relationship between LBW/prematurity and eviction (Figure 2), where C1 and C2 are sets of baseline confounders. Fitting these 2 models and controlling for both sets of confounders allowed us to estimate both the ``overall effect'' of LBW/prematurity (model 2) as well as the ``controlled direct effect'' of LBW/prematurity (model 3), that is, the effect of LBW/prematurity not mediated through hospital length of stay (38).
Figure 2.
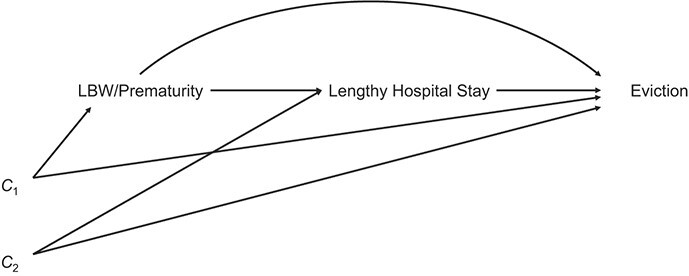
Hypothesized directed acyclic graph for adverse birth and eviction (n = 2,115), Fragile Families and Child Wellbeing Study (children born 1998–2000).
To fit these models, we analyzed person-times with piecewise logistic regression (39). Because eviction was rare, odds and odds ratios approximated discrete hazards and hazard ratios. To account for clustering induced by repeated observations (as well as our selection weights), we estimated robust standard errors, making P values and confidence intervals conservative.
To select covariates, we started with a pool of potential confounders chosen a priori on the basis of prior literature (19, 20, 22, 40, 41). We then used a disjunctive cause criterion and a form of backwards selection to remove covariates 1 by 1 that, conditional on the other covariates in the model, were unlikely to be confounders, following VanderWeele (42). In practice, we retained variables that were either clear predictors of 1 of our birth outcomes (P < 0.05, or approaching it, assessed via logistic regression), clear predictors of eviction in models excluding our exposures, or promising predictors of both (P < 0.20). Though this selection process helped us choose a parsimonious model that still guarded against confounding, selecting covariates in this way can bias inferences (43). In sensitivity analyses, results from models including all initially proposed covariates were nearly identical, suggesting minimal bias was induced via covariate selection.
Retained predictors included unstable housing during pregnancy (binary); poor housing conditions during pregnancy (binary); insurance type (public, private, or uninsured); number of prenatal care visits (continuous); number of prenatal hospitalizations (continuous; excluding the birth itself); history of maternal mental health problems (binary); maternal self-rated health (on a 1–5 Likert scale, treated as continuous); maternal disability (binary); a multiple-birth indicator (binary); ratio of household income to the federal poverty line (continuous); maternal education (less than high school, high school, some college, college); parental smoking intensity (nonsmoker, < 1 pack/day, 1–2 packs/day, ≥3 packs/day); maternal race/ethnicity (White, Black, Hispanic, other race/ethnicity; included to identify populations at risk of racism exposures, following Ford and Airhihenbuwa (40, 44–46)); maternal age (years; continuous); single motherhood (binary); relationship quality (an FFCWS-specific, 5-question scale about the quality of mothers’ relationships with their children’s biological father;  = 0.98); number of children in the household (continuous); and child sex (binary), as well as dummy variables for time. Rejected predictors included maternal alcohol or illegal drug use during pregnancy (binary), neighborhood poverty rate (continuous), and whether families were receiving public assistance for housing costs (binary). All covariates were measured at baseline, with medical and housing history variables derived from medical records and the remainder pulled from baseline parent surveys. For more information on covariate coding and sensitivity analyses using alternate covariate specifications, see the Web Appendix.
= 0.98); number of children in the household (continuous); and child sex (binary), as well as dummy variables for time. Rejected predictors included maternal alcohol or illegal drug use during pregnancy (binary), neighborhood poverty rate (continuous), and whether families were receiving public assistance for housing costs (binary). All covariates were measured at baseline, with medical and housing history variables derived from medical records and the remainder pulled from baseline parent surveys. For more information on covariate coding and sensitivity analyses using alternate covariate specifications, see the Web Appendix.
To calculate inverse probability of selection weights, participants who otherwise met our inclusion criteria (i.e., renters with medical records data) were considered censored for any wave in which they 1) had missing data on eviction or 2) did not participate in data collection, as well as all future waves. In general, censoring because of missing eviction data was rare, with 22, 8, and 3 children initially censored this way in years 1, 3, and 5, respectively, compared with 258, 186, and 157 participants, respectively, censored because of general nonparticipation. We built models for selection the same way we built models for treatment. Retained predictors of selection included both exposures; unstable housing; number of prenatal visits; single parenthood status; neighborhood poverty; receipt of publicly funded housing support; and maternal mental health, self-rated health, substance abuse, education, smoking intensity, race/ethnicity, and age.
Multiple imputation using chained equations enabled us to account for missing exposure and covariate data. Rates of missingness were generally low—below 3% for all variables other than number of prenatal hospitalizations (8.3%) and number of prenatal visits (21.6%). All analyses were conducted in Stata MP, version 15 (47).
In sensitivity analyses, we included fixed effects for cities. These accounted for clustering at the city level and potential confounding by time-invariant city characteristics. Cities with fewer resources, for example, may have had fewer protections against eviction and fewer resources to protect the health of pregnant women. We also tested the proportional hazards assumption that adverse birth outcomes had the same relation to infants’ hazard of eviction at all follow-up ages, interacting each treatment with dummy variables for time and assessing whether any time by treatment interaction was significant. Finally, because our treatment was much more common than our outcome, we re-ran these analyses using 1) inverse probability of treatment weights as our confounding control method (48, 49) and 2) doubly robust methods, using both treatment weights and direct covariate control to lower the risk of model misspecification (50).
RESULTS
Of the 2,395 infants in our study cohort, 18.5% (n = 443) experienced an adverse birth outcome. These included 3 groups: those born LBW/preterm with short hospital stays (n = 239; 10.0%), those born LBW/preterm with long hospital stays (n = 123; 5.1%), and those with long hospital stays who were not born LBW or preterm (n = 81; 3.4%). Eviction was much rarer: 136 children (6.4%) were evicted at some point in early childhood while under observation, with 78 (3.7% of those uncensored) evicted in the year 1 wave, 31 (1.67% of uncensored survivors) evicted in the year 3 wave, and 27 (1.61% of uncensored survivors) evicted in the year 5 wave.
Those who experienced an adverse birth outcome and those who did not differed in several ways (see Web Table 2). Infants with adverse birth outcomes were more likely to show signs of social and medical disadvantage, including fewer prenatal visits, lower income-to-poverty ratio, unhealthier smoking behavior (i.e., were more likely to smoke and more likely to smoke greater quantities of cigarettes), unstable housing during pregnancy, and single parenthood. Black mothers and multiple births were over-represented among adverse birth outcome cases. Table 1 lists characteristics of infants in the FFCWS.
Table 1.
Baseline Characteristics of Study Infants (n = 2,115), Fragile Families and Child Wellbeing Study (Children Born 1998–2000)
| Variable | Prevalence, % | Mean (SD) |
|---|---|---|
| Unstable housing during pregnancy | ||
| Poor housing quality during pregnancy | 0.96 | |
| No. of prenatal visits | 8.65 (4.16) | |
| No. of hospitalizations during pregnancy (excluding the birth) | 0.66 (0.96) | |
| Maternal self-rated health (5-point Likert scale) | 3.79 (0.97) | |
| Maternal disability | 1.71 | |
| History of maternal mental health problems | 13.74 | |
| Multiple birth | 1.54 | |
| Maternal age, years | 24.63 (5.66) | |
| Single parent | 43.47 | |
| Parental relationship quality (scale from 3–15) | 9.32 (6.41) | |
| No. of children in household | 1.64 (1.08) | |
| Male child sex (binary) | 52.28 | |
| Income as proportion of federal poverty line | 1.6 (1.63) | |
| Maternal education | ||
| <High school | 41.95 | |
| High school | 30.73 | |
| Some college | 22.33 | |
| College | 4.99 | |
| Parental smoking | ||
| Nonsmoker | 65.36 | |
| <1 pack/day | 27.28 | |
| 1–2 packs/day | 6.15 | |
| ≥3 packs/day | 1.22 | |
| Health insurance type | ||
| Publicly insured | 71.48 | |
| Privately insured | 21.81 | |
| Uninsured | 6.71 | |
| Maternal race/ethnicity | ||
| Black | 50.77 | |
| Hispanic | 31.67 | |
| Other race/ethnicity | 3.74 | |
| White | 13.82 |
Abbreviation: SD, standard deviation.
Selected results from our models for eviction are listed in Table 2 and presented graphically in Figure 3. Full results are available in Web Table 3. Risk of eviction was estimated to be highest in the first year of life, with a hazard of 2% among the reference group. That hazard declined by a factor of approximately 0.45 between years 1 and 3 and remained there between years 3 and 5. In model 1, which was not adjusted for confounding or selection bias, we estimated that infants who experienced LBW/prematurity had 1.71 times the hazard of eviction at any given time point (2-sided P = 0.012; 95% confidence interval (CI): 1.12, 2.59). Adding controls for confounding and applying weights for selection in model 2 attenuated this association, and it was no longer statistically significant (hazard ratio (HR) = 1.47, 95% CI: 0.91, 2.39; P = 0.114).
Table 2.
Estimated Hazard Ratios for Eviction (From Birth Through Age 5 Years) Associated With Adverse Birth Outcomes (n = 2,115), Fragile Families and Child Wellbeing Study (Children Born 1998–2000)a
| Variable | Model 1 (Unweighted) | Model 2 (LBW/Preterm Only) | Model 3 (LBW/Preterm and Lengthy Hospital Stay) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient (SE) | P Value | 95% CI | Coefficient (SE) | P Value | 95% CI | Coefficient (SE) | P Value | 95% CI | |
| LBW or preterm | 1.71 (0.36) | 0.012 | 1.12, 2.59 | 1.47 (0.36) | 0.114 | 0.91, 2.39 | 1.74 (0.47) | 0.041 | 1.02, 2.95 |
| ≥7 Days in hospital | 2.50 (0.99) | 0.021 | 1.15, 5.44 | ||||||
| LBW/Preterm × ≥7 days | 0.29 (0.17) | 0.03 | 0.09, 0.89 | ||||||
Abbreviations: CI, confidence interval; LBW, low birthweight; SE, standard error.
a Estimates relating adverse birth-outcome exposures to participants’ conditional odds of eviction were calculated with piecewise logistic regression with 5,655 observations contributed by 2,115 children in the Fragile Families and Child Wellbeing Study cohort. Eviction, the outcome, is rare; thus, odds ratios approximate hazard ratios. P values are from 2-sided tests.
Figure 3.
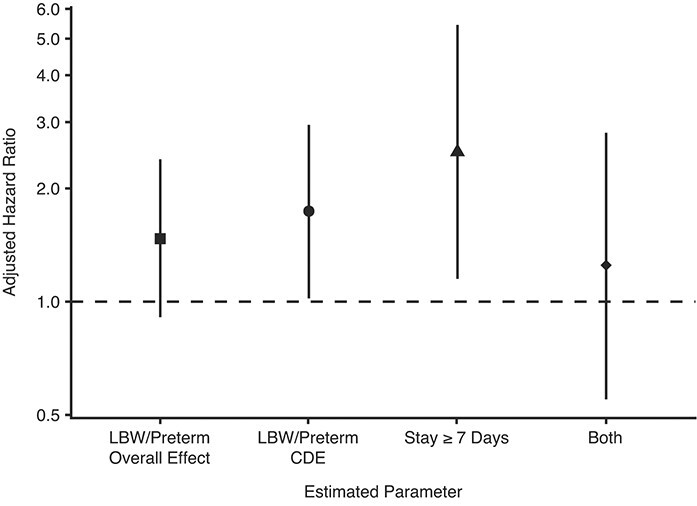
Forest plot visualizing estimates from the piecewise logistic regression model we used to analyze 5,655 observations contributed by 2,115 infants from the Fragile Families and Child Wellbeing Study, a cohort of infants born in large US cities between 1998 and 2000 that oversampled unmarried mothers by design. Eviction, the outcome, is rare, thus, odds ratios approximate hazard ratios. The vertical position of each shape relative to the y-axis represents the magnitude of the estimated association, with ratios relative to uncomplicated births. Vertical black lines represent 95% confidence intervals. “LBW/Preterm Overall Effect” represents our estimate on low birthweight (LBW)/preterm status from model 2 (i.e., not incorporating extended hospital stays). All other bars represent estimates from model 3: the controlled direct effect (CDE) of LBW/preterm birth on eviction, the direct path from an extended hospital stay to eviction (≥7 days in hospital), and the hazard ratio associated with being born LBW/preterm and having an extended hospital stay (reported as “Both”).
In model 3, however, we added a term for a lengthy hospital stay, thus estimating 3 associations: the “controlled direct effect” of LBW/preterm on eviction, the “direct effect” of an extended hospital stay, and the added risk associated with both being born LBW/preterm and experiencing a lengthy hospital stay. These 3 groups appear to experience quite different levels of eviction risk, and looking at them separately is informative. First, LBW/prematurity alone (for its controlled direct effect) predicted a significantly increased hazard of eviction of nearly 75% (HR = 1.74, 95% CI: 1.02, 2.95; P = 0.041). Those who had a lengthy hospital stay despite not being born LBW/preterm were also estimated to have a higher hazard of eviction (HR = 2.50, 95% CI: 1.15, 5.44; P = 0.021). Second, the interaction term between LBW/preterm and an extended hospital stay was statistically significant and well below 1 (HR = 0.29, 95% CI: 0.09, 0.89; P = 0.030). This finding suggests that infants experiencing both LBW/preterm and an extended hospital stay also faced a higher hazard of eviction than did healthy infants (HR = 1.74 × 2.5 × 0.29 = 1.25) but less so than those who were only LBW/preterm or only had an extended hospital stay. The linear combination of these terms was imprecisely estimated (95% CI: 0.55, 2.81).
Results remained consistent regardless of our modeling approach or whether we included city fixed effects. Repeating our analyses using inverse probability of treatment weights or using a doubly robust estimator (applying inverse probability of treatment weights while simultaneously directly adjusting for potential confounders) did not substantively alter our findings (see Web Table 4). Interactions between our exposures and time were statistically insignificant.
DISCUSSION
In this analysis of a lower income, urban birth cohort, children born preterm or with low birthweight had a substantially higher hazard of being evicted in their first 5 years of life compared with infants with uncomplicated births, with a hazard ratio of 1.74 in fully adjusted models, though confidence intervals were wide (95% CI: 1.02, 2.95; P = 0.041). Children with intensive medical needs in the absence of LBW/prematurity, as indicated by a hospital stay of at least 1 week, also experienced heightened risk of eviction, with a hazard ratio of 2.50 (95% CI: 1.15, 5.44; P = 0.021).
Those who experienced a lengthy hospital stay after being born LBW/preterm also appeared to face a higher hazard of eviction than those who had uncomplicated births (HR = 1.25, 95% 95% CI: 0.55, 2.81), but less so than infants facing either adverse birth outcome alone. This may reflect that a lengthy hospital stay for this group may serve as a proxy for something other than high medical needs. A lengthy hospital stay for term, normal-weight babies may signal serious medical complications, whereas a lengthy hospital stay after being born LBW/preterm may signal that those LBW/preterm infants are receiving high-quality, intensive preterm or low birthweight follow-up care (51). Such intensive follow-up care may improve those infants’ long-term health trajectories and thus prevent future, adverse, birth-related medical costs, which may provide some protection against eviction.
If our results are causal, they have troubling synergies with 1) recent results showing that infants who experienced unstable housing during gestation were more likely to be born LBW/preterm (17, 52, 53) and 2) the increasing amount of literature suggesting that eviction harms health (19, 31, 32, 54). If being sick makes people more likely to be evicted and being evicted makes people more likely to become sick, eviction and poor health may cyclically ratchet low-income families down the ladder of well-being and opportunity.
Much concern has been raised in research on the effects of housing and neighborhoods on health about the direction of the association (55–62); that is, do low-quality housing or disadvantaged neighborhoods cause poor health, or are people in poor health sorted into low-quality housing and disadvantaged neighborhoods? To be sure, our results agree that this is a critical challenge for the field in terms of determining the direction of causality between eviction and health. But our and others’ longitudinal results (17, 52, 53) suggest a bidirectional relationship is most likely, at least in terms of birth outcomes.
To our knowledge, we are the first to demonstrate that a poor health outcome may lead to rental eviction. Our results are in accord, however, with findings on foreclosure (63) and with those of 2 large, quasi-experimental studies in which researchers found state-level Medicaid expansion under the Affordable Care Act lowered eviction rates and eviction filings (64, 65). From a microeconomic perspective, these studies’ ecological findings might be explained either by Medicaid expansion preventing catastrophic medical debt from forcing low-income families out of their homes; by families being able to reallocate money spent on health insurance into housing payments; or by the provision of medical care preventing illness and thereby protecting workers’ earning time. Our findings suggest a direct role of illness, particularly in the early years of life and parenthood.
Furthermore, evidence that adverse birth outcomes can lead to eviction raises critical questions about health equity. Given socioeconomic and racial/ethnic disparities in both adverse birth outcomes (3, 66) and eviction (40), results highlight a potentially important mechanism by which racial and social inequality may be reproduced and become entrenched.
Limitations and strengths
There are several limitations to our study. First, we likely did not perfectly control for confounding or perfectly model selection, though consistent results when using doubly robust estimators lower concern about model misspecification. Second, controlling for many potential confounders runs the risk of inducing M-bias by stratifying on a collider (43). Third, by limiting our data to the approximately 75% of participants with extracted medical records, it is possible that we have limited generalizability. The magnitude of differences between mothers whose medical records were extracted and those whose records were not were small, but excluded mothers were slightly less poor, slightly better educated, and slightly less likely to be White and more likely to be Hispanic (see Web Table 5).
Mismeasurement may also hinder causal inference. On the exposure and covariate side, this is likely to be minimal, due to our use of medical records, though we cannot rule out recall bias for covariates from survey data. On the outcome side, misclassification is a known problem. Informal evictions (i.e., those not carried out via legal means) are largely missed by questions asking directly about eviction (23, 67). Furthermore, gaps between FFCWS waves are longer than 1 year, and eviction questions only solicit information about evictions in the last 12 months, meaning evictions in the 12-month periods immediately after the age 1 year and age 3 years interviews were missed entirely. If this misclassification was nondifferential by exposure status (which, in the case of systematically not asking about certain evictions, is likely the case), associations would be biased toward the null, making our results conservative, all else being equal.
Use of FFCWS data is a strength, having oversampled some of the most disadvantaged families at highest risk of both eviction and adverse birth outcomes. The more socioeconomically homogenous sample also helps dampen the threat of residual confounding. However, these results may not generalize to more advantaged or rural settings. The number of observed evictions is low, hampering power and precluding us from assessing whether the estimated association between adverse birth outcomes and eviction varies by individual characteristics, such as race/ethnicity or socioeconomic status. Finally, FFCWS also lacks the necessary data to shed light on what mediates potential paths between adverse birth outcomes and eviction, including differentiating the role of immediate birth costs versus higher health care costs throughout early childhood; we leave this to future work.
Implications for practice
Our results are important whether or not they are causal. Causal results would mean that preventing adverse birth outcomes would protect families from a high risk of eviction and its health-related sequelae. It also means eviction would be a mediator of the negative influence of LBW/prematurity on children’s life chances or later health. Associational results also demand attention: identifying children with adverse birth outcomes as at heightened risk of early childhood eviction net of many other risk factors. To the extent that eviction puts children on a trajectory of impaired opportunity, our results identify children born preterm, with low birthweights, or with other neonatal medical needs as in especial need of intervention to prevent eviction.
In the short term, our results suggest pediatricians and neonatal care providers should connect families experiencing adverse birth outcomes to supports that could help them secure and maintain tenancy in stable housing, such as medical-legal partnerships (68), tenant advocacy organizations (69–71), or social welfare programs for which young families are newly eligible (e.g., Temporary Assistance for Needy Families; Women, Infants, and Children program) (72, 73). Health care payers and public programs, such as Medicaid, could help parents of neonates spending large amounts of time in hospital cover nonmedical costs stemming from adverse birth outcomes. In the long term, policies that support families and low-income workers—such as paid family leave, higher wages, stronger and more readily enforceable protections for tenants, and more affordable housing—could make birth-related costs more manageable, protecting children from harm.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Social & Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, Massachusetts, United States (Gabriel L. Schwartz, Lisa F. Berkman, Jarvis T. Chen); Institute for Health Policy Studies, University of California San Francisco, San Francisco, California, United States (Gabriel L. Schwartz); Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, United States (Kathryn M. Leifheit); Department of Health Policy & Management, University of California, Los Angeles, Fielding School of Public Health, Los Angeles, California, United States (Kathryn M. Leifheit); and Department of Urban Studies and Planning, Massachusetts Institute of Technology, Cambridge, Massachusetts, United States (Mariana C. Arcaya).
GL.S. and K.M.L. attended the Fragile Families Summer Data Training Workshop, which was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD) at the National Institutes for Health (grants R01HD36916, R01HD39135, R01HD40421, and R25HD074544). K.M.L. was supported by an NICHD Pre-Doctoral Fellowship (award F31HD096767) and an Agency for Healthcare Research and Quality Post-Doctoral Fellowship (award 2T32HS000046).
We thank Dr. Ellice S. Lieberman and Dr. Gopika Krishna for their guidance on coding adverse birth outcomes. We are also grateful to the Fragile Families & Child Wellbeing Study team and to the study’s participants for their time, dedication, and willingness to share about their lives.
The content is solely the responsibility of the authors and does not necessarily represent the official views of these funding agencies.
Conflicts of interest: none declared.
REFERENCES
- 1.US Environmental Protection Agency . Adverse Birth Outcomes. In: America’s Children and the Environment. Washington, DC: National Service Center for Environmental Publications; 2019:264–288. https://www.epa.gov/sites/production/files/2015-06/documents/health-adverse-birth-outcomes.pdf. Accessed January 15, 2020. [Google Scholar]
- 2.Sapkota A, Chelikowsky AP, Nachman KE, et al. Exposure to particulate matter and adverse birth outcomes: a comprehensive review and meta-analysis. Air Qual Atmos Heal. 2012;5(4):369–381. [Google Scholar]
- 3.Blumenshine P, Egerter S, Barclay CJ, et al. Socioeconomic disparities in adverse birth outcomes: a systematic review. Am J Prev Med. 2010;39(3):263–272. [DOI] [PubMed] [Google Scholar]
- 4.Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371(9608):261–269. [DOI] [PubMed] [Google Scholar]
- 5.Hack M, Klein NK, Taylor HG. Long-term developmental outcomes of low birth weight infants. Future Child. 1995;5(1):176–196. [PubMed] [Google Scholar]
- 6.Reyes L, Mañalich R. Long-term consequences of low birth weight. In: Kidney Int Suppl. 2005:S107–S111. [DOI] [PubMed]
- 7.Van Lieshout RJ, Boyle MH, Saigal S, et al. Mental health of extremely low birth weight survivors in their 30s. Pediatrics. 2015;135(3):452–459. [DOI] [PubMed] [Google Scholar]
- 8.March of Dimes Foundation . The Cost of Prematurity and Complicated Deliveries to U.S. Employers. 2008. https://www.marchofdimes.org/Peristats/pdfdocs/cts/ThomsonAnalysis2008_SummaryDocument_final121208.pdf. Accessed January 16, 2020.
- 9.Tommiska V, Tuominen R, Fellman V. Economic costs of care in extremely low birthweight infants during the first 2 years of life. Pediatr Crit Care Med. 2003;4(2):157–163. [DOI] [PubMed] [Google Scholar]
- 10.US Institute of Medicine Committee on Understanding Premature Birth and Assuring Healthy Outcomes . Societal costs of preterm birth. In: Behrman RE, Butler AS, eds. Preterm Birth: Causes, Consequences, and Prevention. Washington, DC: National Academies Press; 2007:398–429. [PubMed] [Google Scholar]
- 11.Gennaro S. Leave and employment in families of preterm low birthweight infants. Image J Nurs Sch. 1996;28(3):193–198. [DOI] [PubMed] [Google Scholar]
- 12.Yoshikawa H, Aber JL, Beardslee WR. The effects of poverty on the mental, emotional, and behavioral health of children and youth. Am Psychol. 2012;67(4):272–284. [DOI] [PubMed] [Google Scholar]
- 13.Gitterman B, Flanagan P, Cotton W, et al. Poverty and child health in the United States. Pediatrics. 2016;137(4):e20160339. [DOI] [PubMed] [Google Scholar]
- 14.Elkins K. Here’s how much money Americans have in savings at every income level. CNBC. 2018; https://www.cnbc.com/2018/09/27/heres-how-much-money-americans-have-in-savings-at-every-income-level.html. Accessed February 1, 2020.
- 15.US Institute of Medicine Committee on Understanding Premature Birth and Assuring Healthy Outcomes; Behrman RE, Stith Butler A (eds) . Preterm Birth: Causes, Consequences, and Prevention. 2007. https://www.ncbi.nlm.nih.gov/books/NBK11362/. Accessed January 27, 2020.
- 16.Leifheit KM, Schwartz GL, Pollack CE, et al. Severe housing insecurity during pregnancy: association with adverse birth and infant outcomes. Int J Environ Res Public Health. 2020;17(22):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Himmelstein G, Desmond M. The infant and maternal health consequences of eviction. Presented at the Population Association of America Annual Meeting, held virtually, April 23-25, 2020.
- 18.Khadka A, Fink G, Gromis A, et al. In utero exposure to threat of evictions and preterm birth: evidence from the United States. Health Serv Res. 2020;55(suppl 2):823–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vásquez-Vera H, Palència L, Magna I, et al. The threat of home eviction and its effects on health through the equity lens: a systematic review. Soc Sci Med. 2017;175:199–208. [DOI] [PubMed] [Google Scholar]
- 20.Desmond M. Evicted: Poverty and Profit in the American City. New York, NY: Broadway Books; 2016. [Google Scholar]
- 21.Desmond M. Unaffordable America: poverty, housing, and eviction. 2015. https://www.irp.wisc.edu/publications/fastfocus/pdfs/FF22-2015.pdf. Accessed September 9, 2019.
- 22.Leifheit KM, Pollack CC, Black MM, et al. Eviction in the United States: affected populations, housing and neighborhood-level consequences, and implications for health. Presented at the Society for Epidemiologic Research Meeting. Baltimore, MD, June 19-22, 2018. [Google Scholar]
- 23.Collyer S, Bushman-Copp L. Forced Moves and Eviction in New York City. 2019. https://robinhoodorg-production.s3.amazonaws.com/uploads/2019/08/HOUSING-REPORT_8.5.pdf. Accessed January 18, 2020.
- 24.Gluckman PD, Hanson MA, Beedle AS. Early life events and their consequences for later disease: a life history and evolutionary perspective. Am J Hum Biol. 2007;19(1):1–19. [DOI] [PubMed] [Google Scholar]
- 25.Shonkoff JP. Capitalizing on advances in science to reduce the health consequences of early childhood adversity. JAMA Pediatr. 2016;170(10):1003–1007. [DOI] [PubMed] [Google Scholar]
- 26.Landrigan PJ, Goldman LR. Children’s vulnerability to toxic chemicals: a challenge and opportunity to strengthen health and environmental policy. Health Aff. 2011;30(5):842–850. [DOI] [PubMed] [Google Scholar]
- 27.Monnat SM, Chandler RF. Long-term physical health consequences of adverse childhood experiences. Sociol Q. 2015;56(4):723–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gilbert LK, Breiding MJ, Merrick MT, et al. Childhood adversity and adult chronic disease: an update from ten states and the District of Columbia, 2010. Am J Prev Med. 2015;48(3):345–349. [DOI] [PubMed] [Google Scholar]
- 29.García-Cobián Richter F, Urban AH, Coulton C, et al. The Cleveland Eviction Study: Downstream Paths of Evictions into Homelessness and Loss of Human Capital. 2019. https://case.edu/socialwork/povertycenter/sites/case.edu.povertycenter/files/2019-11/Costs%20of%20Eviction_11052019-accessible.pdf. Accessed October 15, 2020.
- 30.Leifheit KM, Schwartz GL, Pollack CE, et al. Eviction in early childhood and neighborhood poverty, food security, and obesity in later childhood and adolescence: evidence from a longitudinal birth cohort. SSM Popul Heal. 2020;11: 100575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Desmond M, Kimbro RT. Eviction’s fallout: housing, hardship, and health. Soc Forces. 2015;94(1):295–324. [Google Scholar]
- 32.Wood JN, Medina SP, Feudtner C, et al. Local macroeconomic trends and hospital admissions for child abuse, 2000-2009. Pediatrics. 2012;130(2):e358–e364. [DOI] [PubMed] [Google Scholar]
- 33.US National Center for Health Statistics . Natality public-use data 2016–2018. 2019. http://wonder.cdc.gov/natality-expanded-current.html. Accessed February 1, 2020.
- 34.Reichman NE, Teitler JO, Garfinkel I, et al. Fragile families: sample and design. Child Youth Serv Rev. 2001;23(4-5):303–326. [Google Scholar]
- 35.US Centers for Medicare & Medicaid Services . Newborns’ and Mothers’ Health Protection Act (NMHPA). 2013. https://www.cms.gov/CCIIO/Programs-and-Initiatives/Other-Insurance-Protections/nmhpa_factsheet. Accessed February 25, 2020.
- 36.Pantell MS, Baer RJ, Torres JM, et al. Unstable housing is linked to adverse obstetric outcomes. Am J Obstet Gynecol. 2019;220(1):S308. [DOI] [PubMed] [Google Scholar]
- 37.Kassebaum N. S. Rept. 104–326- Newborns’ and Mothers’ Health Protection Act of 1996. 1996. https://www.congress.gov/congressional-report/104th-congress/senate-report/326/1. Accessed February 10, 2020.
- 38.Vanderweele TJ. Marginal structural models for the estimation of direct and indirect effects. Epidemiology. 2009;20(1):18–26. [DOI] [PubMed] [Google Scholar]
- 39.Friedman M. Piecewise exponential models for survival data with covariates. Ann Stat. 1982;10(1):101–113. [Google Scholar]
- 40.Desmond M, Gershenson C. Who gets evicted? Assessing individual, neighborhood, and network factors. Soc Sci Res. 2017;62:362–377. [DOI] [PubMed] [Google Scholar]
- 41.US Institute of Medicine Committee on Understanding Premature Birth and Assuring Healthy Outcomes . Sociodemographic and community factors contributing to preterm birth. In: Behrman RE, Butler AS, eds. Preterm Birth: Causes, Consequences, and Prevention. Washington, DC: National Academies Press; 2007:124–147. [PubMed] [Google Scholar]
- 42.Vanderweele TJ. Principles of confounder selection. Eur J Epidemiol. 2019;34(3):211–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu W, Brookhart MA, Schneeweiss S, et al. Implications of M bias in epidemiologic studies: a simulation study. Am J Epidemiol. 2012;176(10):938–948. [DOI] [PubMed] [Google Scholar]
- 44.Ford CL, Airhihenbuwa CO. The public health critical race methodology: praxis for antiracism research. Soc Sci Med. 2010;71(8):1390–1398. [DOI] [PubMed] [Google Scholar]
- 45.Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health. 2019;40(1):105–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alhusen JL, Bower KM, Epstein E, et al. Racial discrimination and adverse birth outcomes: an integrative review. J Midwifery Womens Health. 2016;61(6):707–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.StataCorp . Stata Statistical Software: Release 15. College Station, TX: StataCorp; 2017.
- 48.Hernán MA, Brumback B, Robins JM. Marginal structural models to estimate the joint causal effect of nonrandomized treatments. J Am Stat Assoc. 2001;96(454):440–448. [Google Scholar]
- 49.Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–560. [DOI] [PubMed] [Google Scholar]
- 50.Funk MJ, Westreich D, Wiesen C, et al. Doubly robust estimation of causal effects. Am J Epidemiol. 2011;173(7):761–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Symington AJ, Pinelli J. Developmental care for promoting development and preventing morbidity in preterm infants. Cochrane Database Syst Rev. 2006;(2):CD001814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Khadka A, Fink G, Gromis A, et al. In-utero exposure to threatened evictions and preterm births: evidence from the United States. Presented at the Population Association of America Annual Meeting, held virtually, April 23-25, 2020.
- 53.Leifheit K, Schwartz G, Pollack C, et al. Severe housing insecurity in pregnancy: Association with adverse birth outcomes in a cohort of urban mothers and infants. Presented at the Population Association of America Annual Meeting,. Philadelphia, PA, November 2-6, 2019. https://apha.confex.com/apha/2019/meetingapp.cgi/Paper/444457. [Google Scholar]
- 54.Kennedy MC, Kerr T, McNeil R, et al. Residential eviction and risk of detectable plasma HIV-1 RNA viral load among HIV-positive people who use drugs. AIDS Behav. 2017;21(3):678–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Arcaya MC, Subramanian SV, Rhodes JE, et al. Role of health in predicting moves to poor neighborhoods among Hurricane Katrina survivors. Proc Natl Acad Sci U S A. 2014;111(46):16246–16253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.James P, Hart JE, Arcaya MC, et al. Neighborhood self-selection: the role of pre-move health factors on the built and socioeconomic environment. Int J Environ Res Public Health. 2015;12(10):12489–12504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jokela M. Are neighborhood health associations causal? A 10-year prospective cohort study with repeated measurements. Am J Epidemiol. 2014;180(8):776–784. [DOI] [PubMed] [Google Scholar]
- 58.Linton SL, Haley DF, Hunter-Jones J, et al. Social causation and neighborhood selection underlie associations of neighborhood factors with illicit drug-using social networks and illicit drug use among adults relocating from public housing. Soc Sci Med. 2017;185:81–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Glass TA, Bilal U. Are neighborhoods causal? Complications arising from the ‘stickiness’ of ZNA. Soc Sci Med. 2016;166:244–253. [DOI] [PubMed] [Google Scholar]
- 60.Smith KR, Hanson HA, Brown BB, et al. Movers and stayers: how residential selection contributes to the association between female body mass index and neighborhood characteristics. Int J Obes (Lond). 2016;40(9):1384–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zang P, Lu Y, Ma J, et al. Disentangling residential self-selection from impacts of built environment characteristics on travel behaviors for older adults. Soc Sci Med. 2019;238:112515. [DOI] [PubMed] [Google Scholar]
- 62.Arcaya MC, Graif C, Waters MC, et al. Health selection into neighborhoods among families in the moving to opportunity program. Am J Epidemiol. 2016;183(2):130–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Houle JN, Keene DE. Getting sick and falling behind: health and the risk of mortgage default and home foreclosure. J Epidemiol Community Health. 2015;69(4):382–387. [DOI] [PubMed] [Google Scholar]
- 64.Allen HL, Eliason E, Zewde N, et al. Can Medicaid expansion prevent housing evictions? Health Aff. 2019;38(9):1451–1457. [DOI] [PubMed] [Google Scholar]
- 65.Zewde N, Eliason E, Allen H, et al. The effects of the ACA Medicaid expansion on nationwide home evictions and eviction-court initiations: United States, 2000-2016. Am J Public Health. 2019;109(10):1379–1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dominguez TP. Race, racism, and racial disparities in adverse birth outcomes. Clin Obstet Gynecol. 2008;51(2):360–370. [DOI] [PubMed] [Google Scholar]
- 67.Flowers A. How we undercounted evictions by asking the wrong questions. FiveThirtyEight. 2016; https://fivethirtyeight.com/features/how-we-undercounted-evictions-by-asking-the-wrong-questions/. Accessed September 9, 2019.
- 68.Bittle J. NYC’s legal assistance program for tenants is saving thousands from eviction. Gothamist. 2018. https://gothamist.com/news/nycs-legal-assistance-program-for-tenants-is-saving-thousands-from-eviction. Accessed December 17, 2019.
- 69.Kromrei G. “We’re seeing more militant direct action:” tenant groups fight evictions with power drills and other tools. TheRealDeal. 2020. https://therealdeal.com/2020/08/05/were-seeing-more-militant-direct-action-tenant-groups-fight-evictions-with-power-drills-and-other-tools/. Accessed October 15, 2020.
- 70.Weisman R. As housing crunch tightens, older women fight eviction from Kenmore Square rooming house. Boston Globe. 2019. https://www.bostonglobe.com/metro/2019/03/29/housing-crunch-tightens-older-women-fight-eviction-from-kenmore-square-rooming-house/nsWY1SZJA4bzBWlqR8iFzL/story.html. Accessed October 15, 2020.
- 71.Desmond M. The tenants who evicted their landlord. New York Times. 2020. https://www.nytimes.com/2020/10/13/magazine/rental-housing-crisis-minneapolis.html. (Accessed October 15, 2020).
- 72.Sandel M, Cutts D, Meyers A, et al. Co-enrollment for child health: how receipt and loss of food and housing subsidies relate to housing security and statutes for streamlined, multi-subsidy application. J Appl Res Child Informing Policy Child Risk. 2014;5(2). [Google Scholar]
- 73.Office of Family Assistance . TANF-ACF-IM-2013-01 (Use of TANF funds to serve homeless families and families at risk of experiencing homelessness). Washington, DC: US Department of Health and Human Services; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


