Abstract
Objective:
Several studies suggest that alcohol and cannabis co-users are heavier drinkers and experience more alcohol-related consequences. However, day-level associations between co-use and drinking levels are mixed. One reason may be that individual characteristics moderate the daily impact of using alcohol alone or in conjunction with cannabis. Theory would suggest that highly impulsive individuals may drink more on co-use days, yet this assertion remains untested. Therefore, the current study tested whether impulsivity moderated the effect of co-use on same-day drinking quantity within veterans, a high-risk sample for substance use and impulsivity.
Method:
In a longitudinal observational study, co-using veterans (N=139) completed three semi-annual assessments reporting on their daily drinking quantity and cannabis use via Timeline Followback (Observations=19,245) and impulsivity via the UPPS-P. Mixed effect modeling was used to test hypotheses that co-use (compared to alcohol-only) days would be associated with heavier drinking for those high (but not low) in positive and negative urgency.
Results:
Significant interactions were found for positive urgency (PU) and lack of perseverance (LP), such that individuals at mean and low levels of PU and LP drank less on co-use (compared to alcohol-only) days. There were no significant interactions for other UPPS-P impulsivity facets.
Conclusion:
Findings are consistent with a substitution/compensatory effect for individuals at mean and low levels of both UPPS-P facets, and may be a byproduct of frequent cannabis use in veterans. In contrast, findings suggest that co-use and alcohol-only days may be characterized by similarly high levels of drinking for highly impulsive individuals.
Keywords: Co-Use, Alcohol, Cannabis, Impulsivity, Urgency
Introduction
Heavy drinking (4+ drinks for women, 5+ drinks for men) is a serious and growing public health concern. Heavy drinking is associated with negative consequences such as risky sex, intoxicated driving, alcohol-related injury, and Alcohol Use Disorder (AUD) (Perkins, 2002; Hingson & Zha, 2009; Wechsler et al., 1994). Despite decades of research delineating risk factors for heavy drinking, prevalence rates are still rising across all age groups (Grant et al., 2017). Thus, refining our understanding of both individual- and contextual-level antecedents of heavy drinking may better inform early intervention efforts aimed at reducing heavy drinking.
Alcohol Use, Cannabis Use, and Alcohol and Cannabis Co-Use
One person-level risk factor for heavy drinking is being a co-user of alcohol and cannabis. Alcohol and cannabis co-use, defined as either using both substances at the same time so that their effects overlap [simultaneous use] or being a dual user [concurrent use], is common and on the rise (e.g., Subbaraman & Kerr, 2020; Terry-McElrath & Patrick, 2018). Several cross-sectional and longitudinal studies, using predominately adolescent and young adult samples, suggest that alcohol and cannabis co-users are heavier drinkers (e.g., Haas et al., 2015; Patrick et al., 2017; Shillington & Clapp, 2006; Subbaraman & Kerr, 2015), experience more alcohol-related consequences (e.g., Green et al., 2019; Jackson et al., 2020; Linden-Carmichael et al., 2019; Patrick et al., 2017; Subbaraman & Kerr, 2015; Wardell et al., 2020; White et al., 2019), and are at higher risk for the development of AUD (Midanik et al., 2007) compared to alcohol-only users. Notably, in a cross-sectional study, Jackson et al. (2020) found that college co-users reported more cognitive problems, vomiting, drunk driving, and overall risk behavior, and Wardell et al. (2020) found that increases in cannabis use during college (when accounting for alcohol use) were associated with risky behavior, a lack of self-care, and alcohol dependence.
Although cross-sectional and longitudinal designs are informative, daily/event-level studies may provide additional detail about between-person versus within-person effects of cannabis use on drinking behavior. Emerging research on alcohol and cannabis co-use suggests two competing theories of use, where an individual co-uses to substitute the effects of one substance (i.e., an individual uses less of one substance in the presence of the other via replacement) or to complement the effects of the other substance (i.e., an individual uses one substance to enhance the effect of the other) (Risso et al., 2020; Subbaraman, 2016). Event-level assessments (i.e., daily diaries, momentary assessments, Timeline Followback interviewing) allow for a dynamic within-person investigation of these theories, testing whether co-use (versus single substance use) days are related to within-person fluctuations in drinking.
Studies using event-level assessment methodologies have demonstrated daily relations between cannabis use and initiation of any alcohol use in community sampled adults (Rouche et al., 2019), more drinks per drinking day in college students (Gunn et al., 2018) and veterans (Gunn et al., 2019), and higher likelihood of moderate and heavy drinking in veterans (Metrik et al., 2018a). In contrast, associations between daily co-use and other indices of alcohol use, including alcohol-related consequences and subjective intoxication, have been less consistent in young adult samples. Two studies found that co-use days (compared to alcohol-only days) were associated with more alcohol-related consequences (Mallet et al., 2017; Lipperman-Kreda et al., 2017). In addition, Linden-Carmichael et al. (2020) found that co-use days were associated with more consequences but were not associated with heightened subjective intoxication. In contrast, Sokolovsky et al. (2020) found that co-use days were associated with higher subjective intoxication, but not directly associated with more alcohol consequences. Lastly, Lee et al. (2020) found that, when accounting for levels of drinking, co-use was associated with positive (but not negative) consequences, and Mallet et al. (2019) found that heavy drinking days were associated with more consequences, regardless of whether cannabis was co-used with alcohol. Together, these day-level investigations suggest that while co-use may not consistently predict increased consequences or subjective intoxication, it may lead to increased number of drinks in college students, community adult samples, and veteran samples.
Person-Level Moderators
One potential reason for inconsistent results in prior event-level studies may be that the relation between co-use days and indices of alcohol use varies by person-level characteristics. For instance, three studies have found that associations between co-use and drinking outcomes differ based on alcohol-related problems. Gunn et al. (2018) found that co-use days were associated with more drinking and higher eBAC in college students with higher AUDIT problem drinking scores in high school, and Metrik et al. (2018a) found that co-use was associated with heavier drinking for those with an AUD diagnosis. Relatedly, Sokolovsky et al. (2020) found that the association between co-use days and alcohol consequences was weakened at higher levels of consumption (Sokolovsky et al., 2020). In addition, Gunn et al. (2019) found that, compared to medical cannabis users, recreational users reported heavier drinking on co-use days, and using cannabis for substitution reasons was associated with lighter drinking on co-use days.
Taken together, these findings suggest that person-level characteristics may play an important role in identifying co-users at higher risk for heavy drinking and consequences on days when both substances are used. One potentially important person-level moderator largely absent in co-use studies is impulsive personality traits, defined as the predilection toward rash and ill-advised action (Whiteside & Lynam, 2001). The UPPS-P model breaks impulsivity into distinct, yet correlated sub facets, namely positive and negative urgency (i.e., rash action in the presence of positive and negative mood, respectively), lack of perseverance (i.e., lack of focus), lack of premeditation (i.e., lack of planning), and sensation seeking (i.e., novelty seeking) (Whiteside & Lynam, 2001; Lynam et al., 2007). Meta-analytic results suggest that all impulsive personality traits are associated with heavier drinking and alcohol-related problems (Coskunpinar et al., 2013). Meta-analyses also suggest that all impulsive personality traits (except for perseverance) are associated with heavier cannabis use, and all traits (except negative urgency and perseverance) are associated with cannabis problems (VanderVeen et al., 2016). Lastly, Linden-Carmichael et al. 2019 found that sensation seeking is associated with being an alcohol and cannabis co-user.
Furthermore, the acquired preparedness model suggests that those who are highly impulsive learn differently about the acute experience of substance use by discounting negative effects and attuning to positive effects (Smith & Anderson, 2001). Consistent with this model, several studies suggest that highly impulsive individuals expect and feel stronger positive alcohol effects (e.g., Berey et al., 2019; Corbin et al., 2011; Settles et al., 2015) and stronger positive cannabis effects (e.g., Bolles et al., 2014; Day et al., 2013; Vangness et al., 2005). Thus, it is possible that highly impulsive individuals are particularly vulnerable to the disinhibiting effects of both cannabis (Metrik et al., 2012; Ramaekers et al., 2006) and alcohol (Corbin et al., 2020; McCarthy et al., 2012) on a given co-use day, resulting in impaired control over drinking. However, models of impulsivity suggest that the construct is multifaceted (Strickland & Johnson, 2020; Whiteside & Lynam, 2001), and there is reason to believe specific subscales of impulsive personality traits may lead an individual to drink more on co-use days.
In line with the complementary hypothesis of co-use, individuals high in positive urgency (i.e., rash action in the presence of a positive mood state) may drink more on co-use days for positive reinforcement, due to enhanced intoxication/pleasure when cannabis is co-used with alcohol (Lukas & Orozco, 2001; Lukas et al., 1992; Patrick et al., 2020). On the contrary, individuals high in negative urgency (i.e., rash action in the presence of a negative mood state) may drink more on co-use days for negative reinforcement, when both substances may be used to alleviate negative affective states. Thus, individual high in both urgency facets may come to expect heightened intoxication and affective change from co-use, leading to heavier drinking when co-using both substances. However, to our knowledge, no study to date has tested the moderating effects of UPPS-P impulsive personality traits on the association between co-use (versus alcohol-only) days and drinking quantity.
Co-Use Among Veterans vs. Adolescents and Young Adults
Considering prior studies have largely focused on adolescents or college students, it is important to understand the effects of co-use in other high-risk samples. Veteran samples may thus be ideal to examine for associations between impulsivity, daily co-use (versus alcohol-only), and daily drinking quantity. Veterans represent a high-risk population in terms of alcohol use, with roughly 35% of veterans reporting problem drinking (Meadows et al., 2015). Data also suggest that veterans report more heavy episodic drinking (Agaku et al., 2020; Bohnert et al., 2012) and have higher AUDIT scores (Albright et al., 2020) than non-veteran comparisons. Research also suggests that impulsivity within veterans is related to a host of negative outcomes, most importantly heavier drinking (e.g., Hawn et al., 2019; Gunn et al., 2020). Further, polysubstance use is common in veterans (Bhalla et al., 2019) and recent research suggests that veterans with higher symptom counts of ADHD (a disorder marked by impulsive action) use cannabis more often (Stevens et al., 2020). In concert, veterans may represent a higher-risk population in terms of impulsivity and both heavier alcohol and cannabis use. Yet, findings that alcohol and cannabis co-use days are associated with heavier drinking are consistent across both veteran (e.g., Gunn et al., 2019; Metrik et al., 2018a) and non-veteran samples (e.g., Gunn et al., 2018; Roche et al., 2019), suggesting that co-use phenomenon may generalize to both adolescent/young adult and veteran populations. Thus, using a sample of veterans allows for a theoretically appealing test of hypotheses within a higher-risk population, with findings that would be generalizable to general population samples.
Current Study
Therefore, the current study sought to test how UPPS-P impulsive personality traits moderate the effect of daily alcohol and cannabis co-use on drinking quantity in a sample of veterans. Analyses extend previous findings (Gunn et al., 2019; Metrik et al., 2018a) by testing whether facets of impulsivity moderate the association between co-use and daily drinking in a sample of veterans. We hypothesized that individuals with high levels of positive and negative urgency would drink more on co-use days relative to alcohol-only days, compared to those at mean and low levels of urgency. Interactions for lack of perseverance, lack of premeditation, and sensation seeking were considered exploratory hypotheses.
Methods
Sample and Procedure
The current sample was drawn from a larger prospective study on cannabis use and affective disorders in post 9/11 deployed OEF/OIF/OND veterans (Metrik et al., 2020). Veterans were recruited from a Veterans Health Administration (VHA) facility in the northeast U.S. between February 2013 and December 2015. Participants were recruited via advertisements and using the VHA OEF/OIF/OND roster of combat veterans returning from Iran and Afghanistan. Inclusion criteria were a) being at least 18 years old, b) being an OEF/OIF/OND veteran confirmed in the VHA Computerized Patient Record System (CPRS), and c) using cannabis at least once in their lifetime. Exclusion criteria were a) having past two-week suicidal risk, b) having past-month psychotic symptoms, c) having a score of less than or equal to 23 on the Mini-Mental Status Exam (Folstein et al., 1975), and d) being active duty at baseline. A total of 361 veterans enrolled in the study and attended a baseline session, where they completed informed consent, a clinical interview, and a battery of assessments. Follow-up visits were scheduled at 6-months (N = 312, 86.4%) and 12-months (N = 310, 85.9%) and consisted of parallel assessments. All study procedures were approved by the Brown University and local VHA Institutional Review Boards. For a full description of study procedures see Metrik et al. (2016).
The current sample (N = 139) comprised veterans who reported at least one co-use day on the Timeline Followback interview over the course of the three assessments. The sample was predominately men (92.4%) with a mean age of 30.78 (SD = 7.99), non-Hispanic/Latinx ethnicity (84%), and White race (78%). Veterans had an average of 13.2 (SD = 1.91) years of education and an average household income of between $30–39,999. Sixty-three percent of veterans had a lifetime diagnosis of Major Depressive Disorder (MDD), and 33.8% of veterans had a lifetime diagnosis of Post-Traumatic Stress Disorder (PTSD). Sixty-nine percent of veterans were in the army, 18% in the marines, 7.9% in the navy, and 5% in the air force. Included co-using participants were heavier drinkers (t = 3.91, p < .001), younger (t = 18.9, p < .001), and had higher levels of positive urgency (t = 5.94, p < .001), negative urgency (t = 3.42, p = .001), and lack of premeditation (t = 1.99, p = .047) compared to excluded (non-co-using) participants. Included (co-using) participants did not differ on the other UPPS-P subscales.
Measures
Demographics
Age and sex were assessed at the baseline interview and verified through the VHA medical record system.
Post-Traumatic Stress Disorder and Major Depressive Disorder
PTSD and MDD were assessed via structural clinical interviews (see Metrik et al., 2016 for details) and scored as 1 = lifetime diagnosis, 0 = no lifetime diagnosis.
Daily Substance Use
A Timeline Followback interview (TLFB; Sobell & Sobell, 1992) was administered at all three sessions. The TLFB is a calendar-based structured interview, where participants are asked to recall their substance use over a period of time. Participants were encouraged to reference memory aids to support in accurate recall. Participants were asked to report on the past 180 days (6 months prior) at each assessment, reporting the number of standard drinks consumed each day (defined as 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of 80 proof distilled spirits) and whether they used any cannabis, cigarettes, or other drugs. The TLFB has been validated for the retrospective recall of both alcohol and cannabis use (Sobell & Sobell, 1992; Dennis et al., 2004), gives highly valid estimates compared to biological measures of use (Hjorthøj et al., 2012), and has high test-retest reliability and stability across 180- and 360-day assessments (Carey, 1997; Sobell & Sobell, 1992). Rather than using the TLFB in solely aggregate form, both day (within-person) and aggregate (between-person) level variables were used in analyses. We created a drinking quantity variable (within- and between-person), a percent cannabis use days variable (between-person), and daily variables for any cannabis use, any cigarette use, and any other drug use (0 = no use, 1 = use). We also created a day of week variable, Monday through Thursday were coded as weekdays, and Friday, Saturday, and Sunday were coded as weekends (0 = weekday, 1 = weekend).
Impulsive Personality Traits
Impulsive personality traits were assessed using the Short UPPS-P Impulsivity Scale (Cyders et al., 2014). The Short UPPS-P is a 20-item self-report measure assessing positive urgency (i.e., rash action in a positive mood state; a = .83), negative urgency (i.e., rash action in a negative mood state, a = .73), lack of perseverance (i.e., lack of focus; a = 69), lack of premeditation (i.e., lack of planning, a = .83), and sensation seeking (thrill seeking, adventurousness; a = .48). All responses were measured on a scale of 1 (Agree Strongly) to 4 (Disagree Strongly) and were reverse-scored so that higher values indicated higher impulsivity.
Data Analytic Plan
All variables were examined for assumptions of normality, and outliers were winsorized by replacing values outside of 3 standard deviations from the mean with the next highest integer (Tabachnick & Fidell, 2007). Since hypotheses were for co-use (compared to alcohol-only) days, non-drinking days were removed prior to analysis (Lee et al., 2020).
A series of linear mixed effects models were built within the R package lmer4 with the lmertest extension to obtain exact p-values (Bates et al., 2014; Kuznetsova et al., 2015). All models were built such that drinking quantity (within-person) was regressed on whether cannabis was used that day (0 = alcohol-only, 1 = co-use), the UPPS-P impulsivity facet of interest, and their cross-level interaction (separate models for each impulsivity facet). Model covariates included age, sex, lifetime diagnoses of MDD and PTSD, percent cannabis use days from the TLFB, and average drinking quantity from the TLFB as fixed between-person level covariates. Any cigarette use (0 = no use, 1 = use), any other drug use (0 = no use, 1 = use), weekday versus weekend (0 = weekday, 1 = weekend), and day of the study (days 1–540) were modeled as fixed within-person covariates. Group-mean centering was used for within-level predictors and grand-mean centering for between-level predictors (Enders & Tofighi, 2007).
In the presence of a significant interaction, simple slopes were estimated at 1 SD above the mean, at the mean, and 1 SD below the mean of the UPPS-P impulsivity facet (Preacher et al., 2006). In addition, regions of significance testing was employed to reveal the exact value at which the impulsivity facet moderated co-use. Lastly, to ensure accuracy of the 180-day TLFB recall period, sensitivity analyses were tested with the most recent 90 days of data at each time-point. All sensitivity models were estimated identically to the 180-day models.
Results
Descriptive Statistics and Bivariate Correlations
Extreme daily drinking quantity values (>3 standard deviations above the mean) were winsorized to the next highest value within the distribution of values (.4% of cases winsorized). After censuring outliers, the daily drinking variable had adequate skewness (1.11) and kurtosis (1.09) for a linear model.
Demographic and descriptive statistics are displayed in Supplemental Table 1. Across all study days (540), participants reported using cannabis on 39.5% of days, using alcohol on 27.9% of days, and co-using on 8.1% of days. All remaining statistics and analyses considered drinking days only. Participants reported a total of 19,245 drinking days across the 18-month period (M per person = 138.5 drinking days), of which 5,590 (29%) were alcohol and cannabis co-use days. Mean number of drinks on co-use and alcohol-only days were 5.69 (SD = 3.52) and 5.48 (SD = 3.67), respectively. Participants used cigarettes on 40.9% of drinking days, used other drugs on 3.9% of drinking days, and just over half of drinking days (53%) occurred on weekends.
For a full list of bivariate correlations see Table 1. Daily drinking quantity was significantly correlated with all daily variables, such that cannabis, cigarette, and drug use were positively correlated with heavier drinking, later days in the study were positively correlated with heavier drinking, and older age was positively correlated with heavier drinking. Cannabis use days were also positively correlated with cigarette use, drug use, weekend days, and later days in the study. Heavier average drinking quantity across days was positively correlated with male sex and all impulsive personality characteristics except for sensation seeking.
Table 1:
Bivariate Correlations
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Drinking Quantity (Daily) | -- | .03** | .04** | .08** | .15** | .03** | .69** | .02** | .10** | .07** | .04** | .19** | −.01† |
| 2. Cannabis Use (Daily) | -- | .23** | .09** | .04** | .03** | .03** | .75** | −.03** | .05** | .03** | .04** | −.03** | |
| 3. Cigarette Use (Daily) | -- | .02** | −.05** | −.03** | .03** | .25** | .19** | .20** | .09** | .25** | −.15** | ||
| 4. Other Drug Use (Daily) | -- | .06** | −.03** | .06** | .04** | .01 | .04** | −.09** | −.01 | .15** | |||
| 5. Weekend vs. Weekday (Daily) | -- | −.02** | .01 | −.02* | .01 | −.03** | −.08** | −.09** | .06** | ||||
| 6. Day of Study (Daily) | -- | −.02** | −.01 | −.03** | −.01 | −.02** | .01 | .01 | |||||
| 7. Aggregate Drinking Quantity | -- | .01 | .20* | .19* | .06* | .24** | .03 | ||||||
| 8. Percent Cannabis Use Days | -- | −.07 | .06 | .01 | .03 | .02 | |||||||
| 9. Positive Urgency | -- | .62** | .07 | .42** | .18** | ||||||||
| 10. Negative Urgency | -- | .24** | .47** | .02 | |||||||||
| 11. Lack of Perseverance | -- | .36** | −.01* | ||||||||||
| 12. Lack of Premeditation | -- | .11 | |||||||||||
| 13. Sensation Seeking | -- |
Note. Correlations between two within-person variables or between a within- and between-person variable used the full N of 19,245 drinking days; Correlations between two between-person variables used the person-mean N of 139.
p < .01,
p < .05,
p < .10.
Positive and Negative Urgency Models
Model parameters for the positive and negative urgency models are shown in Table 2. Covariate effects for both positive and negative urgency models were largely in the expected direction. Any drug or cigarette use, later days in the study, weekend days, and heavier between-person drinking were associated with heavier daily drinking; however, older age was associated with heavier drinking. Covariate effects were identical for all models, and thus are not discussed in the subsequent models (See Tables 2 and 3).
Table 2:
Model Parameters for Positive and Negative Urgency Models Predicting Daily Drinking Quantity
| Positive Urgency | Negative Urgency | |||||||
|---|---|---|---|---|---|---|---|---|
| Est. | SE | 95% CI | p | Est. | SE | 95% CI | p | |
| Intercept | 3.81 | .16 | (3.54, 4.15) | < .001 | 3.81 | .17 | (3.53, 4.17) | < .001 |
| Age | .005 | .002 | (.001, .01) | .021 | .005 | .002 | (.001, .01) | .036 |
| Sex (Male) | .19 | .13 | (−.04, .43) | .15 | .19 | .13 | (−.05, .43) | .16 |
| Percent Cannabis Days | .11 | .09 | (−.05, .28) | .22 | .08 | .08 | (−.07, .25) | .35 |
| Drink Count (BP) | 1.00 | .009 | (.98, 1.01) | < .001 | .99 | .009 | (.98, 1.01) | < .001 |
| MDD Diagnosis | −.04 | .05 | (−.13, .04) | .43 | −.04 | .05 | (−.14, .05) | .40 |
| PTSD Diagnosis | −.03 | .06 | (−.14, .08) | .64 | −.03 | .06 | (−.14, .08) | .64 |
| Day of Study (1–540)* | .001 | .0001 | (.0009, .001) | < .001 | .001 | .0001 | (.0008, .001) | < .001 |
| Weekend* | 1.05 | .04 | (.96, 1.11) | < .001 | 1.05 | .04 | (.95, 1.11) | < .001 |
| Cigarette Use* | .26 | .05 | (.15, .34) | < .001 | .26 | .05 | (.14, .34) | < .001 |
| Other Drug Use* | .71 | .10 | (.47, .88) | < .001 | .73 | .10 | (.49, .90) | < .001 |
| Cannabis Use* | −.18 | .06 | (−.30, −.05) | .006 | −.14 | .06 | (−.27, −.02) | .023 |
| UPPS-P Urgency Facet | −.08 | .04 | (−.15, −.002) | .052 | −.02 | .04 | (−.10, .06) | .61 |
| Cannabis Use × Urgency | .22 | .07 | (.09, .34) | .002 | .04 | .07 | (−.09, .16) | .54 |
Note.
Within-Person, Time-Varying Covariate; MDD = Lifetime Major Depressive Disorder; PTSD = Lifetime Post-Traumatic Stress Disorder; Urgency = UPPS-P Positive Urgency and Negative Urgency, respectively.
Table 3:
Model Parameters for Lack of Perseverance, Lack of Premeditation, and Sensation Seeking Models Predicting Daily Drinking
| Lack of Perseverance | Lack of Premeditation | Sensation Seeking | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est. | SE | 95% CI | p | Est. | SE | 95% CI | p | Est. | SE | 95% CI | p | |
| Intercept | 3.82 | .16 | (3.53, 4.16) | < .001 | 3.83 | .16 | (3.60, 4.17) | < .001 | 3.88 | .17 | (3.59, 4.23) | < .001 |
| Age | .005 | .002 | (.001, .01) | .031 | .006 | .002 | (.001, .01) | .022 | .004 | .003 | (−.001, .01) | .15 |
| Sex | .18 | .13 | (−.07, .43) | .19 | .18 | .13 | (−.04, .42) | .16 | .17 | .13 | (−.07, .42) | .19 |
| Percent Cannabis Days | .09 | .09 | (−.07, .26) | .32 | .09 | .09 | (−.05, .26) | .28 | .09 | .09 | (−.10, .25) | .32 |
| Drink Count (BP) | 1.00 | .009 | (.98, 1.01) | < .001 | .99 | .009 | (.98, 1.01) | < .001 | 1.00 | .009 | (.98, 1.01) | < .001 |
| MDD Diagnosis | −.06 | .05 | (−.15, .03) | .25 | −.06 | .05 | (−.14, .02) | .24 | −.05 | .05 | (−.15, .03) | .29 |
| PTSD Diagnosis | −.03 | .06 | (−.14, .07) | .61 | −.04 | .06 | (−.15, .05) | .50 | −.02 | .06 | (−.13, .09) | .76 |
| Day of Study (1–540)* | .001 | .0001 | (.0009, .001) | < .001 | .001 | .0001 | (.0008, .001) | < .001 | .001 | .0001 | (.0009, .001) | < .001 |
| Weekend* | 1.06 | .04 | (.97, 1.01) | < .001 | 1.05 | .04 | (.96, 1.11) | < .001 | 1.05 | .04 | (.96, 1.11) | < .001 |
| Cigarette Use* | .26 | .05 | (.14, .34) | < .001 | .23 | .05 | (.14, .28) | < .001 | .25 | .05 | (.13, .33) | < .001 |
| Other Drug Use | .75 | .10 | (.51, .93) | < .001 | .73 | .10 | (.50, .87) | < .001 | .75 | .10 | (.50, .92) | < .001 |
| Cannabis Use | −.16 | .06 | (−.29, −.04) | .01 | −.13 | .06 | (−.26, −.02) | .028 | −.15 | .07 | (−.27, −.02) | .025 |
| UPPS-P Facet | .01 | .06 | (−.10, .11) | .89 | .08 | .04 | (−.01, .16) | .079 | −.06 | .05 | (−.15, .04) | .24 |
| Cannabis Use × UPPS-P | .24 | .09 | (.06, .40) | .006 | −.03 | .07 | (−.16, .10) | .71 | .02 | .08 | (−.14, .15) | .83 |
Note.
= Within-Person, Time-Varying Covariate; MDD = Lifetime Major Depressive Disorder; PTSD = Lifetime Post-Traumatic Stress Disorder; UPPS-P Facet = UPPS-P Impulsivity facet of interest in each model (i.e., lack of perseverance, lack of premeditation, sensation seeking, respectively).
The positive urgency model indicated a significant interaction between co-use and positive urgency (b = .22, SE = .07, p = .002). Tests of simple slopes suggested that co-use days were associated with lighter drinking for individuals with mean (b = −.18, SE = .06, p = .006) and low (b = −.34, SE = .09, p < .001) levels of positive urgency, whereas drinking quantity on co-use and alcohol-only days were comparable for individuals with high levels of positive urgency (b = −.02, SE = .07, p = .81). Regions of significance testing indicated that the slope of positive urgency became significant under a value of .24, slightly above the mean (Region of Significance = [.24, 2.18]). A value of 2.18 was outside the range of observable data. Although the slope of high positive urgency was not significantly different for alcohol-only versus co-use days, those with high levels of positive urgency reported the highest levels of drinking (compared to mean and lower positive urgency) on co-use days (see Figure 1). The negative urgency model did not indicate a significant interaction between co-use and negative urgency (b = .04, SE = .07, p = .54, Table 2).
Figure 1: Positive Urgency Interaction.
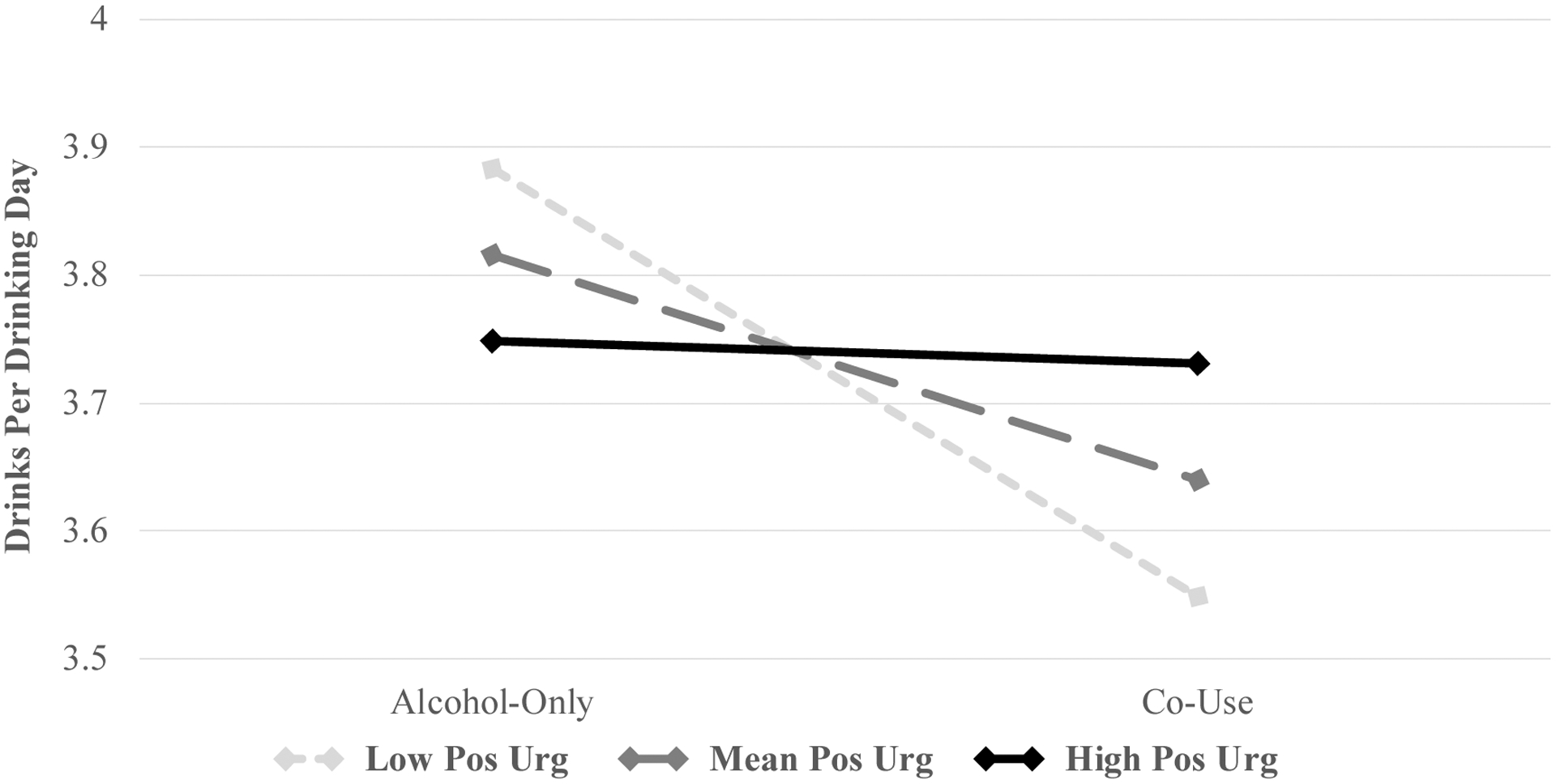
Alcohol-Only Days had N = 13,655 records and Co-Use Days had 5,590 records across 139 individuals. Individuals with average and low (−1 SD), but not high (+1 SD), levels of Positive Urgency drank less on co-use days relative to alcohol-only days.
Perseverance, Premeditation, and Sensation Seeking Models
Model parameters for all remaining impulsivity models are shown in Table 3. There was a significant interaction between co-use and lack of perseverance (b = .24, SE = .09, p = .006). Similar to positive urgency, tests of simple slopes suggested that co-use days were associated with lighter drinking for individuals with mean (b = −16, SE = .06, p = .01) and low (b = −.29, SE = 08, p < .001) levels of lack of perseverance, whereas drinking on co-use and alcohol-only days was comparable for individuals high in lack of perseverance (b = −.04, SE = .07, p = .59; see Figure 2). Regions of significance testing indicated that the slope for lack of perseverance became significant at values under .15, slightly above the mean (Region of Significance = [.15, 2.29]). A value of 2.29 was outside the range of observable data. There were no significant interactions for lack of premeditation or sensation seeking (See Table 3).
Figure 2: Lack of Perseverance Interaction.
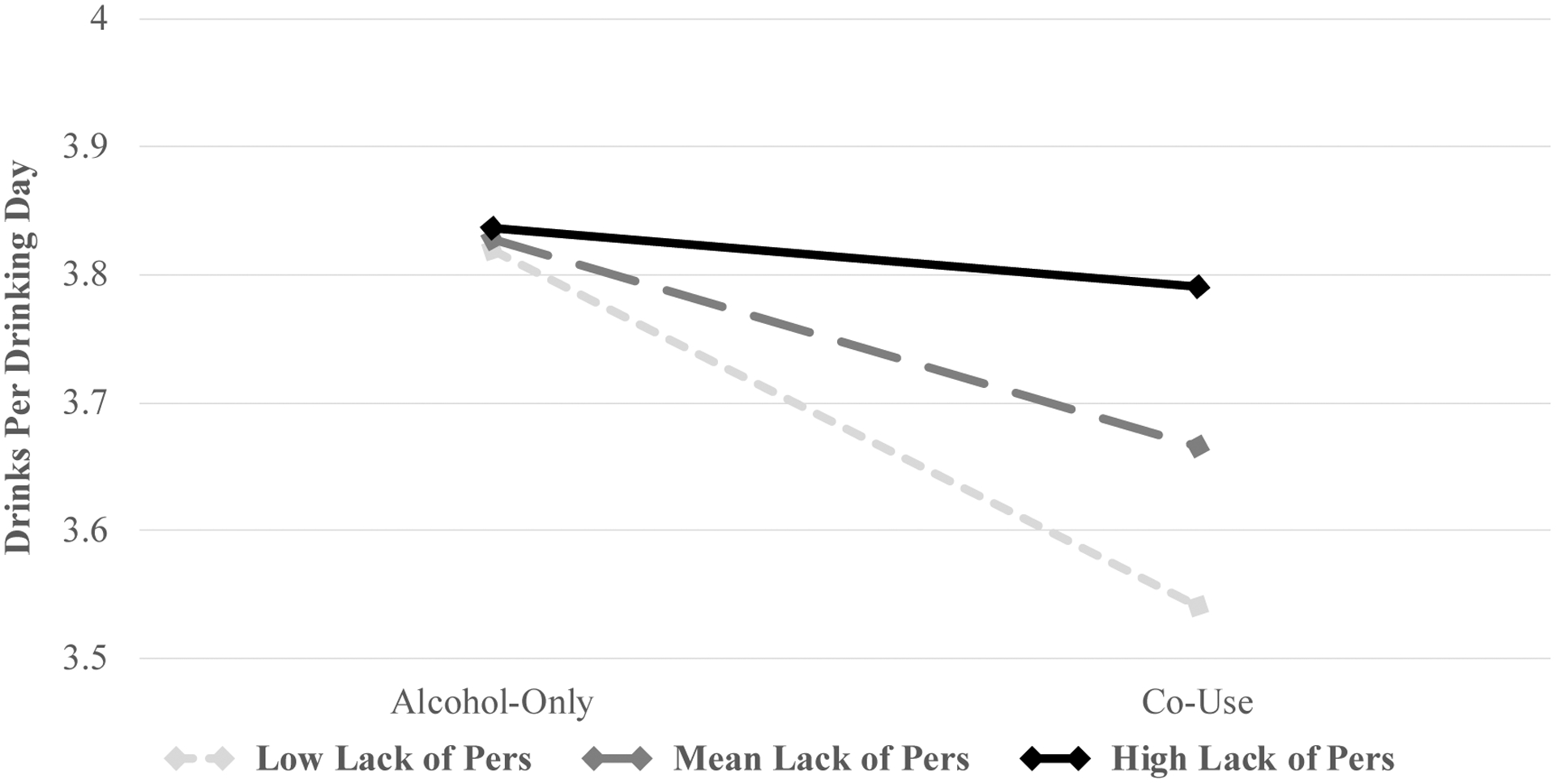
Alcohol-Only Days had N = 13,655 records and Co-Use Days had 5,590 records across 139 individuals. Individuals with average and low (−1 SD), but not high (+1 SD), levels of Lack of Perseverance drank less on co-use days relative to alcohol-only days.
Sensitivity Analyses
Sensitivity analyses replicated models with 90 days of the TLFB (total of 270 days across assessments) prior to each assessment, rather than 180 days (total of 540 days). Sensitivity analyses are shown in Supplementary Tables 2 and 3 and graphed in Supplementary Figures 1 and 2. As with the main analyses, positive urgency (b = .34, SE = .11, p = .002) and lack of perseverance (b = .39, SE = .14, p = .005) were the only impulsivity facets that significantly interacted with co-use to predict daily drinking quantity (see supplemental material). Simple slopes were largely similar, such that co-use days were associated with less drinking for individuals with low levels of positive urgency and lack of perseverance. However, it is worth noting that the simple slopes for those high in positive urgency (b = .24, SE = .11, p = .036) and lack of perseverance (b = .20, SE = .11, p = .062) suggest that co-use days were associated with heavier drinking for those high in each impulsive personality trait (see supplemental material).
Discussion
The current study was the first to test whether impulsive personality traits moderate the effect of daily alcohol and cannabis co-use on same-day drinking quantity. Several studies suggest that college student and community adult co-users may be at higher risk for heavy drinking and consequences due to higher levels of impulsivity (e.g., Linden-Carmichael et al., 2019; Yurasek et al., 2017), and thus the current study tested this theory by examining these associations at the daily level in an older, veteran sample. Using UPPS-P impulsivity facets and detailed TLFB interviews, results indicated significant interactions for positive urgency and lack of perseverance, such that those with mean and low levels of both traits drank less on co-use days; drinking quantity was similar on co-use and alcohol-only days among those at high levels of these impulsivity facets. Interactions involving negative urgency, lack of premeditation, and sensation seeking were all non-significant. Lastly, sensitivity analyses to account for potential bias in TLFB retrospective reporting revealed a similar pattern of results, with the exception of significant differences in drinks consumed between co-use days and alcohol-only days for those high in positive urgency and lack of perseverance. At high levels of positive urgency and lack of perseverance, co-use days were associated with heavier drinking relative to alcohol-only days.
One interpretation of study findings may be that individuals with lower levels of impulsivity, particularly positive urgency and lack of perseverance, may be less inclined to engage in heavier, problem-level drinking on co-use days (Linden-Carmichael et al., 2019). The dual process model suggests that there are two decision-making processes, an impulsive, bottom-up process and a less-impulsive, top-down process (e.g., Hoffman et al., 2009). Individuals who engage in a top-down, purposeful decision-making process may be motivated to avoid negative consequences of heavy drinking on co-use days, whereas those who use a bottom-up, impulsive decision-making process may attend more to the reinforcing effects of enhanced intoxication when combining heavy drinking and cannabis use. Alternatively stated, less impulsive individuals may be more risk averse and less willing to experience negative consequences that ensue from heavier drinking on co-use days, and thus those using a top-down decision-making process may compensate for co-use by drinking less. Linden-Carmichael et al. (2019) found that co-users were more willing to experience negative alcohol consequences, and Trager et al. (2019) found that higher levels of impulsivity predicted more negative alcohol consequences indirectly through higher willingness to experience consequences. Taken together, it is possible that less impulsive individuals, particularly in the facets of positive urgency and perseverance, may actively consider the consequences of heavy drinking on co-use days, and may decide to drink less on co-use days due to a lower willingness to experience negative consequences.
Particularly for positive and negative urgency, the hypothesis that higher levels of both would be associated with heavier drinking on co-using days was not supported; rather, individuals with low and mean levels of positive urgency drank less on co-use (compared to alcohol-only) days, and there was no difference for individuals with high levels of positive urgency. Furthermore, those who have lower levels of positive urgency may use cannabis specifically in order to drink less alcohol (i.e., for substitution reasons) rather than to enhance alcohol’s effects with cannabis (i.e., to complement). Metrik et al. (2018b) found that medical cannabis users reported lower frequency of alcohol use relative to recreational users, and Gunn et al. (2019) found that medical cannabis users who endorsed one of the reasons for using cannabis as a substitute for alcohol in fact drank less alcohol on cannabis use days relative to recreational users. Thus, it is possible that individuals with lower levels of positive urgency use cannabis in a more deliberate fashion, perhaps to specifically curb their alcohol use on a given day. Considering two daily studies found that co-use days are coupled with increased risk for negative consequences (Mallet et al., 2017; Lipperman-Kreda et al., 2017), it may be that these individuals are able to make more thoughtful decisions about their drinking quantity even in the presence of a positive mood state (e.g., when celebrating). In contrast, those with higher levels of positive urgency may lack the ability to inhibit rash action (i.e., continued drinking), and drink equally heavily on co-use and alcohol-only days. Given that daily drinking quantity is a strong and proximal predictor of daily consequences (e.g., Dvorak et al., 2014; Lee et al., 2019), having lower levels of positive urgency may buffer against negative consequences on co-use days.
Despite a significant interaction for positive urgency, the same effect was not observed for negative urgency. Although inconsistent with our hypotheses, there are several reasons why this effect may have been absent. Although alcohol and cannabis co-use is thought to enhance subjective intoxication, increased intoxication may not necessarily lead to a reduction in negative affect. Several studies show mixed findings in relation to self-medicating effects of alcohol (e.g., Carrigan & Randall, 2003), and one study in particular found that tension reduction alcohol expectancies were associated with higher negative, but not positive, mood ratings post-alcohol consumption (Merrill et al., 2009). In addition, acute cannabis administration has been linked to paranoia and anxiety (D’Souza et al., 2004), which may be associated with highly arousing negative cannabis effects (Morean et al., 2013; Waddell et al., in press). Considering hypotheses related to negative urgency were grounded in negative reinforcement on co-use days, it may then be the case that co-use, and heightened intoxication, do not relieve negative affect (and in some cases may increase negative affect), providing little reinforcement for those high in negative urgency. However, future research incorporating subjective response to co-use is needed.
Another main finding was that individuals at mean and low levels of lack of perseverance drank less on co-use (compared to alcohol-only) days. Thus, those who have greater ability to persist in spite of potential difficulties may also co-use for substitution reasons, similar to positive urgency. Considering that a lack of perseverance is the strongest predictor of alcohol use of the UPPS-P impulsivity facets (Coskunpinar et al., 2013), it may be that those who have high perseverance already drink less (than those who lack perseverance), and thus gain less reward from drinking. If individuals high in perseverance do not receive as much reward from one substance, it may be possible that they purposefully switch to the other substance to substitute the effects. However, an alternative possibility may be that those who lack perseverance switch back and forth between substances (lacking the ability to focus on just one), leading to equally heavy drinking on co-use and alcohol-only days. However, the current study was not able to test which substance was used first, if the effects overlapped, or how many episodes of each substance use occurred each day; thus, future research is needed to test these hypotheses.
In sensitivity analyses with only 90 days of prior TLFB assessments, results were largely the same, though the nature of the significant interactions differed slightly from the main analyses. Those high in positive urgency and lack of perseverance drank more on co-use days, those low in both drank less on co-use (compared to alcohol-only) days, and there were no differences at mean levels of either impulsivity facet. Thus, the effects of low levels of impulsivity were in line with the 180-day analyses, but sensitivity analyses indicate that high levels of impulsivity were, in fact, a risk factor for heavier drinking on co-use days. One reason this was evident for the restricted 90 days but not 180 days may be that longer retrospective estimates better account for between-subject, habitual drinking patterns (i.e., how much one typically uses on an alcohol-only versus co-use day) (e.g., Hoeppner et al., 2010). Thus, the 180-day analyses may prime individuals to think about their general drinking quantity on co-use and alcohol-only days, whereas 90-day analyses may have more intraindividual variability from single instances. Future prospective research using daily dairies or momentary assessments that are less likely to have recall bias are needed to replicate the effects identified in the current study.
Age and veteran status are important considerations in interpreting study findings. The current sample was older (mean age of 30.78) than other co-use samples of college students, community adults, and adolescents. Age was a significant between-person predictor of heavier drinking in some models, however we believe this is confounded by impulsivity and veteran status. Main effects of age were variant depending on which impulsivity facet was tested, and veterans are older and drank more than most samples of samples discussed.
Given that veterans are a high-risk group for impulsivity, alcohol use, and cannabis use, daily associations may have been stronger in the current study than other, non-Veteran studies. Mean-levels of impulsivity and drinking in the current sample were similar to those in non-Veteran samples (e.g., Cyders et al., 2014; O’Hara et al., 2014), however, the current study of veterans reported much higher rates of cannabis use than non-veteran, young adult/college samples (Gunn et al., 2018; O’Hara et al., 2014). Thus, the high rates of cannabis use in the current veteran sample may have driven a substitution, rather than complementary, effect. If veterans are already experiencing steady intoxication/impairment from cannabis, it would make sense that adding alcohol would lead to lower levels of drinking, particularly for those with low levels of impulsivity. In further support, veteran’s mean-levels of enhancement alcohol motives are substantially lower than young adults/college students in past studies (e.g., McDevitt-Murphy et al., 2017; Merrill et al., 2010), reaffirming the notion that veterans, particularly those with lower levels of impulsivity, may be less likely than college students/young adults to drink and co-use for enhancement/complementary reasons (Merrill et al., 2010; Patrick et al., 2020). The current veteran sample also had high levels of lifetime major depressive disorder and PTSD, and thus veterans may have been using substances for coping reasons instead of enhancement motivation (Metrik et al., 2016). Collectively, results of the current study, combined with findings from past studies with veteran samples, suggests that veterans a) have higher rates of cannabis use and b) may drink more to cope than enhance. Longitudinal research incorporating drinking motives in studies of veterans and non-veterans is needed to determine how current findings generalize to younger and non-Veteran populations. Such research may also identify unique needs of veterans to be targeted in substance use prevention/intervention efforts.
Despite novel contributions of the current study, findings must be interpreted in light of several limitations. First, although the current study was able to test daily effects of alcohol and cannabis co-use, the use of TLFB interviewing may provide less sensitive estimates of within-person fluctuations compared to daily diaries or ecological momentary assessments (e.g., Merrill et al., 2020). Prior research has found that recall biases may be present past 60 days (Hoeppner et al., 2010), however studies also suggest the reliability of the TLFB is consistent at intervals from 30, 60, and 366 days (Searles et al., 2002) and from 30 to 180 days (Carey, 1997). Second, new research suggests that the UPPS-P impulsivity facets may fluctuate within a day (e.g., Stevens et al., 2020). Thus, future research using daily and momentary assessment methods to examine the impact of acute changes in impulsivity on patterns of use is needed. Third, temporal ordering of cannabis and alcohol or simultaneous use of substances could not be established with these data, although Sokolovsky et al. (2020) suggests timing of co-use was not a predictor of use or problems. In addition, one’s context, a strong predictor of use and problems (e.g., Waddell et al., 2020) may rapidly change for highly impulsive individuals, demonstrating another reason future research using momentary assessments is needed. Fourth, the reliability of the sensation seeking subscale was low. Future research should confirm this finding, as other studies suggest higher levels of sensation seeking in co-users (Linden-Carmichael et al., 2019). Lastly, the current sample largely comprised male (92%) and White (78%) veterans. Future research should replicate findings in more heterogenous samples of woman and non-White individuals.
Notwithstanding these limitations, the current study advances the literature on daily alcohol and cannabis co-use, its effects on drinking quantity, and for whom co-use days may be most risky. Results indicated that those with lower levels of positive urgency and lack of perseverance drank less on co-use days, whereas those with higher levels of both drank similarly on co-use and alcohol-only days. These findings suggest a potential substitution and/or compensatory effect of cannabis on alcohol use for less-impulsive individuals. In addition, findings may help resolve conflicting results observed in prior studies, as co-use may only predict heavier drinking among those with higher levels of impulsivity. For highly impulsive individuals, co-use days were characterized by equivalent drinking quantity compared to alcohol-only days, though sensitivity analyses provided some support that highly impulsive individuals drinking more on co-use days. Future studies should test both person- (e.g., alcohol and cannabis expectancies) and contextual- (e.g., drinking context, time of day) level moderators of co-use and drinking quantity/negative consequences using ecological momentary assessment methods.
Supplementary Material
Public Health Significance Statement:
The current study found that, within a high-risk sample of veterans, individuals with low levels of impulsivity showed a substitution/compensatory effect when co-using alcohol and cannabis, such that they consumed less alcohol on days when cannabis was also used. These findings suggest that co-use of alcohol and cannabis on a given day may be associated with less drinking, but only among less impulsive individuals who are thus already at lower risk for alcohol misuse. Individuals with elevated levels of impulsivity may be drinking heavily even when co-using cannabis, resulting in unwanted consequences.
Acknowledgments
This study was supported by Grants R01 DA033425 from the National Institute on Drug Abuse (PI Metrik & Borsari) and K08 AA027551 from the National Institute on Alcohol Abuse and Alcoholism (PI Gunn). The authors report no conflicts of interest. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the Department of Veterans Affairs, or the United States Government.
References:
- Agaku I, Odani S, & Nelson JR (2020). US military veteran versus nonveteran use of licit and illicit substances. American Journal of Preventive Medicine, 59, 733–741. [DOI] [PubMed] [Google Scholar]
- Albright DL, Holmes L, Lawson M, McDaniel J, Laha-Walsh K, & McIntosh S (2020). Veteran-nonveteran differences in alcohol and drug misuse by tobacco use status in Alabama SBIRT. Journal of Social Work Practice in the Addictions, 20, 46–58. [Google Scholar]
- Bates D, Maechler M, Bolker B, & Walker S (2014). lme4: Linear mixed-effects models using Eigen and S4. R Package Version 1. 1–7. [Google Scholar]
- Berey BL, Leeman RF, Chavarria J, & King AC (2019). Relationships between generalized impulsivity and subjective stimulant and sedative responses following alcohol administration. Psychology of Addictive Behaviors, 33, 616–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhalla IP, Stefanovics EA, & Rosenheck RA (2019). Polysubstance use among veterans in intensive PTSD programs: association with symptoms and outcomes following treatment. Journal of Dual Diagnosis, 15, 36–45. [DOI] [PubMed] [Google Scholar]
- Bohnert AS, Ilgen MA, Bossarte RM, Britton PC, Chermack ST, & Blow FC (2012). Veteran status and alcohol use in U.S. men. Military Medicine, 177, 198–203. [DOI] [PubMed] [Google Scholar]
- Bolles JR, Earleywine M, & Gordis E (2014). Acquired preparedness model and impulsivity moderated expectancies: Examining predictors of marijuana use. Addiction Research & Theory, 22, 490–497. [Google Scholar]
- Carey KB (1997). Reliability and validity of the time-line follow-back interview among psychiatric outpatients: a preliminary report. Psychology of Addictive Behaviors, 11, 26–33. [Google Scholar]
- Carrigan MH, & Randall CL (2003). Self-medication in social phobia: a review of the alcohol literature. Addictive Behaviors, 28, 269–284. [DOI] [PubMed] [Google Scholar]
- Corbin WR, Berey BL, Waddell JT, & Leeman RF (2020). Relations between acute effects of alcohol on response inhibition, impaired control over alcohol use, and alcohol‐related problems. Alcoholism: Clinical and Experimental Research, 44, 1123–1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbin WR, Iwamoto DK, & Fromme K (2011). A comprehensive longitudinal test of the acquired preparedness model for alcohol use and related problems. Journal of Studies on Alcohol and Drugs, 72, 602–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coskunpinar A, Dir AL, & Cyders MA (2013). Multidimensionality in impulsivity and alcohol use: A meta‐analysis using the UPPS model of impulsivity. Alcoholism: Clinical and Experimental Research, 37, 1441–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell KG, Chung T, Clark DB, & Martin CS (2014). Solitary alcohol use in teens is associated with drinking in response to negative affect and predicts alcohol problems in young adulthood. Clinical Psychological Science, 2, 602–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Littlefield AK, Coffey S, & Karyadi KA (2014). Examination of a short english version of the UPPS-P impulsive behavior scale. Addictive Behaviors, 39, 1372–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Braley G, … & Krystal JH (2004). The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology, 29, 1558–1572. [DOI] [PubMed] [Google Scholar]
- Day AM, Metrik J, Spillane NS, & Kahler CW (2013). Working memory and impulsivity predict marijuana-related problems among frequent users. Drug and Alcohol Dependence, 131, 171–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Funk R, Harrington Godley S, Godley MD, & Waldron H (2004). Cross validation of the alcohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction, 99, 125–133. [DOI] [PubMed] [Google Scholar]
- Dick DM, Smith G, Olausson P, Mitchell SH, Leeman RF, O’Malley SS, & Sher K (2010). Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addiction Biology, 15, 217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, & Tofighi D (2007). Centering predictor variables in cross-sectional multilevel models: a new look at an old issue. Psychological Methods, 12, 121–138. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, & McHugh PR (1975). “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, … & Hasin DS (2017). Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). JAMA Psychiatry, 74, 911–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green KM, Reboussin BA, Pacek LR, Storr CL, Mojtabai R, Cullen BA, & Crum RM (2019). The effects of marijuana use on transitions through stages of alcohol involvement for men and women in the NESARC I and II. Substance Use & Misuse, 54, 2167–2176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn RL, Norris AL, Sokolovsky A, Micalizzi L, Merrill JE, & Barnett NP (2018). Marijuana use is associated with alcohol use and consequences across the first 2 years of college. Psychology of Addictive Behaviors, 32, 885–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn R, Jackson K, Borsari B, & Metrik J (2019). A longitudinal examination of daily patterns of cannabis and alcohol co-use among medicinal and recreational veteran cannabis users. Drug and Alcohol Dependence, 205, 107661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn RL, Stevens AK, Micalizzi L, Jackson KM, Borsari B, & Metrik J (2020). Longitudinal associations between negative urgency, symptoms of depression, cannabis and alcohol use in veterans. Experimental and Clinical Psychopharmacology, 28, 426–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas AL, Wickham R, Macia K, Shields M, Macher R, & Schulte T (2015). Identifying classes of conjoint alcohol and marijuana use in entering freshmen. Psychology of Addictive Behaviors, 29, 620–626. [DOI] [PubMed] [Google Scholar]
- Harrington M, Baird J, Lee C, Nirenberg T, Longabaugh R, Mello MJ, & Woolard R (2012). Identifying subtypes of dual alcohol and marijuana users: A methodological approach using cluster analysis. Addictive Behaviors, 37, 119–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawn SE, Chowdhury N, Kevorkian S, Sheth D, Brown RC, Berenz E, … & Amstadter AB (2019). Examination of the effects of impulsivity and risk-taking propensity on alcohol use in OEF/OIF/OND Veterans. Journal of Military, Veteran and Family Health, 5, 88–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, & Zha W (2009). Age of drinking onset, alcohol use disorders, frequent heavy drinking, and unintentionally injuring oneself and others after drinking. Pediatrics, 123, 1477–1484. [DOI] [PubMed] [Google Scholar]
- Hjorthøj CR, Hjorthøj AR, & Nordentoft M (2012). Validity of timeline follow-back for self-reported use of cannabis and other illicit substances — systematic review and meta-analysis. Addictive Behaviors, 37, 225–233. [DOI] [PubMed] [Google Scholar]
- Hoeppner BB, Stout RL, Jackson KM, & Barnett NP (2010). How good is fine-grained timeline follow-back data? Comparing 30-day TLFB and repeated 7-day TLFB alcohol consumption reports on the person and daily level. Addictive Behaviors, 35, 1138–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Sokolovsky AW, Gunn RL, & White HR (2020). Consequences of alcohol and marijuana use among college students: prevalence rates and attributions to substance-specific versus simultaneous use. Psychology of Addictive Behaviors, Advanced Online Publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuznetsova A, Brockhoff PB, & Christensen RHB (2015). Package ‘lmertest’. R Package Version 2. [Google Scholar]
- Lee CM, Patrick ME, Fleming CB, Cadigan JM, Abdallah DA, Fairlie AM, & Larimer ME (2020). A daily study comparing alcohol-related positive and negative consequences for days with only alcohol use versus days with simultaneous alcohol and marijuana use in a community sample of young adults. Alcoholism: Clinical and Experimental Research, 44, 689–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Stamates AL, Lau-Barraco C (2019). Simultaneous use of alcohol and marijuana: patterns and individual differences. Substance Use & Misuse, 54, 2156–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Van Doren N, Masters LD, & Lanza ST (2020). Simultaneous alcohol and marijuana use in daily life: implications for level of use, subjective intoxication, and positive and negative consequences. Psychology of Addictive Behaviors, Advanced Online Publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden‐Carmichael AN, Mallett KA, Sell N, & Turrisi R (2019). Are co‐users of alcohol and marijuana more willing to experience consequences from drinking? A longitudinal examination among first‐year college students. Alcoholism: Clinical and Experimental Research, 43, 1567–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipperman-Kreda S, Gruenewald PJ, Grube JW, & Bersamin M (2017). Adolescents, alcohol, and marijuana: context characteristics and problems associated with simultaneous use. Drug and Alcohol Dependence. 179, 55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipperman-Kreda S, Paschall MJ, Robert SF, & Morrison CN (2018). Places and social contexts associated with simultaneous use of alcohol, tobacco and marijuana among young adults. Drug and Alcohol Review, 37, 188–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynam D, Smith GT, Cyders MA, Fischer S, & Whiteside SA (2007). The UPPS-P: A multidimensional measure of risk for impulsive behavior. Unpublished technical report. [Google Scholar]
- Mallett KA, Turrisi R, Hultgren BA, Sell N, Reavy R, Cleveland M, Hultgren BA, Reavy R, & Cleveland M (2017). When alcohol is only part of the problem: An event-level analysis of negative consequences related to alcohol and other substance use. Psychology of Addictive Behaviors, 31, 307–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallett KA, Turrisi R, Trager BM, Sell N, & Linden-Carmichael AN (2019). An examination of consequences among college student drinkers on occasions involving alcohol-only, marijuana-only, or combined alcohol and marijuana use. Psychology of Addictive Behaviors, 33, 331–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy DM, Niculete ME, Treloar HR, Morris DH, & Bartholow BD (2012). Acute alcohol effects on impulsivity: associations with drinking and driving behavior. Addiction, 107, 2109–2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt‐Murphy ME, Williams JL, Bracken KL, Fields JA, Monahan CJ, & Murphy JG (2010). PTSD symptoms, hazardous drinking, and health functioning among US OEF and OIF veterans presenting to primary care. Journal of Traumatic Stress, 23, 108–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meadows SO, Engel CC, Collins RL, Beckman RL, Cefalu M, Hawes-Dawson J, & Williams KM (2018). 2015 health related behaviors survey: substance use among U.S. active-duty service members. Santa Monica, CA: RAND Corporation, 2018. [Google Scholar]
- Merrill JE, Fan P, Wray TB, & Miranda R Jr (2020). Assessment of alcohol use and consequences: comparison of data collected via timeline followback interview and daily reports. Journal of Studies on Alcohol and Drugs, 81, 212–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill JE, & Read JP (2010). Motivational pathways to unique types of alcohol consequences. Psychology of Addictive Behaviors, 24, 705–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill JE, Wardell JD, & Read JP (2009). Is expectancy reality? Associations between tension reduction beliefs and mood following alcohol consumption. Experimental and Clinical Psychopharmacology, 17, 434–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Gunn RL, Jackson KM, Sokolovsky AW, & Borsari B (2018a). Daily patterns of marijuana and alcohol co-use among individuals with alcohol and cannabis use disorders. Alcoholism: Clinical and Experimental Research, 42, 1096–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Bassett SS, Aston ER, Jackson KM, & Borsari B (2018b). Medicinal versus recreational cannabis use among returning veterans. Translational Issues in Psychological Science, 4, 6–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Jackson K, Bassett SS, Zvolensky MJ, Seal K, & Borsari B (2016). The mediating roles of coping, sleep, and anxiety motives in cannabis use and problems among returning veterans with PTSD and MDD. Psychology of Addictive Behaviors, 30, 743–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Stevens AK, Gunn RL, Borsari B, & Jackson KM (2020). Cannabis use and posttraumatic stress disorder: prospective evidence from a longitudinal study of veterans, Psychological Medicine, Advanced Online Publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midanik LT, Tam TW, Weisner C (2007). Concurrent and simultaneous drug and alcohol use: results of the 2000 National Alcohol Survey. Drug and Alcohol Dependence, 90, 72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morean ME, Corbin WR, & Treat TA (2013). The Subjective Effects of Alcohol Scale: Development and psychometric evaluation of a novel assessment tool for measuring subjective response to alcohol. Psychological Assessment, 25, 780–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Fleming CB, Fairlie AM, & Lee CM (2020). Cross-fading motives for simultaneous alcohol and marijuana use: associations with young adults’ use and consequences across days. Drug and Alcohol Dependence, 108077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Veliz PT, & Terry-McElrath YM (2017). High intensity and simultaneous alcohol and marijuana use among high school seniors in the United States. Substance Abuse, 38, 498–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins HW (2002). Surveying the damage: a review of research on consequences of alcohol misuse in college populations. Journal of Studies on Alcohol Supplement, 91–100. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, & Bauer DJ (2006). Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31, 437–448. [Google Scholar]
- Ramaekers JG, Berghaus G, van Laar M, & Drummer OH (2006). Dose related risk of motor vehicle crashes after cannabis use. Drug and Alcohol Dependence, 73, 109–119. [DOI] [PubMed] [Google Scholar]
- Risso C, Boniface S, Subbaraman MS, & Englund A (2020). Does cannabis complement or substitute alcohol consumption? A systematic review of human and animal studies. Journal of Psychopharmacology, 34, 938–954. [DOI] [PubMed] [Google Scholar]
- Roche DJO, Bujarski S, Green R, Hartwell EE, Leventhal AM, & Ray LA (2019). Alcohol, tobacco, and marijuana consumption is associated with increased odds of same-day substance co-and tri-use. Drug and Alcohol Dependence, 200, 40–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Searles JS, Helzer JE, Rose GL, & Badger GJ (2002). Concurrent and retrospective reports of alcohol consumption across 30, 90 and 366 days: interactive voice response compared with the timeline follow back. Journal of Studies on Alcohol, 63, 352–362. [DOI] [PubMed] [Google Scholar]
- Settles RF, Cyders M, & Smith GT (2010). Longitudinal validation of the acquired preparedness model of drinking risk. Psychology of Addictive Behaviors, 24, 198–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shillington AM, & Clapp JD (2006). Heavy alcohol use compared to alcohol and marijuana use: Do college students experience a difference in substance use problems? Journal of Drug Education, 36, 91–103. [DOI] [PubMed] [Google Scholar]
- Smith GT, & Anderson KG (2001). Adolescent risk for alcohol problems as acquired preparedness: A model and suggestions for intervention. Adolescents, alcohol, and substance abuse: Reaching teens through brief interventions, 109–144. [Google Scholar]
- Sobell L, & Sobell M (1992). Timeline Follow-Back: a technique for assessing self-reported alcohol consumption. Psychosocial and Biological Methods. Humana Press, Totowa, [Google Scholar]
- Sokolovsky AW, Gunn RL, Micalizzi L, White HR, & Jackson KM (2020). Alcohol and marijuana co-use: consequences, subjective intoxication, and the operationalization of simultaneous use. Drug and Alcohol Dependence, 107986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staddon JE, & Cerutti DT (2003). Operant conditioning. Annual Review of Psychology, 54, 115–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens AK, Blanchard BE, Talley AE, Brown JL, Halvorson MA, Janssen T, … & Littlefield AK (2020). State-level impulsivity, affect, and alcohol: A psychometric evaluation of the momentary impulsivity scale across two intensive longitudinal samples. Journal of Research in Personality, 85, 103914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens AK, Gunn RL, Jackson KM, Borsari B, & Metrik J (2020). Examining motivational pathways from adult attention-deficit/hyperactivity disorder symptoms to cannabis use: results from a prospective study of veterans. Psychology of Addictive Behaviors, Advanced Online Publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strickland JC, & Johnson MW (2020). Rejecting impulsivity as a psychological construct: a theoretical, empirical, and sociocultural argument. Psychological Review. Advanced Online Publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS (2016). Substitution and complementarity of alcohol and cannabis: A review of the literature. Substance Use & Misuse, 51, 1399–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, & Kerr WC (2015). Simultaneous versus concurrent use of alcohol and cannabis in the National Alcohol Survey. Alcoholism: Clinical and Experimental Research, 39, 872–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, & Kerr WC (2020). Subgroup trends in alcohol and cannabis co-use and related harms during the rollout of recreational cannabis legalization in Washington state. International Journal of Drug Policy, 75, 102508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (2007). Using multivariate statistics. Boston, MA: Pearson. [Google Scholar]
- Terry‐McElrath YM, & Patrick ME (2018). Simultaneous alcohol and marijuana use among young adult drinkers: age‐specific changes in prevalence from 1977 to 2016. Alcoholism: Clinical and Experimental Research, 42, 2224–2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trager BM, Mallett KA, Turrisi R, Sell NM, & Hultgren BA (2019). Willingness as a mediator of the effects of personality on alcohol-related consequences between the first and second years of college: A longitudinal prospective study. Addictive Behaviors, 89, 172–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Um M, Hershberger AR, & Cyders MA (2019). The relationship among depressive symptoms, urgency, and problematic alcohol and cannabis use in community adults. Addictive Behaviors, 88, 36–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderVeen JD, Hershberger AR, & Cyders MA (2016). UPPS-P model impulsivity and marijuana use behaviors in adolescents: A meta-analysis. Drug and Alcohol Dependence, 168, 181–190. [DOI] [PubMed] [Google Scholar]
- Vangsness L, Bry BH, & LaBouvie EW (2005). Impulsivity, expectancies, and marijuana use: A test of the acquired preparedness model. Addictive Behaviors, 30, 1071–1076. [DOI] [PubMed] [Google Scholar]
- Waddell JT, Corbin WR, & Marohnic SD (2020). Putting things in context: longitudinal relations between drinking contexts, drinking motives, and negative alcohol consequences. Psychology of Addictive Behaviors, Advanced Online Publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waddell JT, Corbin WR, Meier MH, Morean ME, & Metrik J (in press). The Anticipated Effects of Cannabis Scale (AECS): initial development and validation of an affect- and valence-based expectancy measure, Psychological Assessment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell JD, Egerton GA, & Read JP (2020). Does cannabis use predict more severe types of alcohol consequences? Longitudinal associations in a 3‐year study of college students. Alcoholism: Clinical and Experimental Research, 44, 1141–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weschler H, Davenport A, Dowdall G, Moeykens B, & Castillo S (1994). Health and behavioral consequences of binge drinking in college. Journal of the American Medical Association, 272, 1672–1677. [PubMed] [Google Scholar]
- White HR, Kilmer JR, Fossos‐Wong N, Hayes K, Sokolovsky AW, & Jackson KM (2019). Simultaneous alcohol and marijuana use among college students: patterns, correlates, norms, and consequences. Alcoholism: Clinical and Experimental Research, 43, 1545–1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside SP, & Lynam DR (2001). The five-factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30, 669–689. [Google Scholar]
- Yurasek AM, Aston ER, & Metrik J (2017). Co-use of alcohol and cannabis: a review. Current Addiction Reports, 4, 184–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


