Abstract
Background: Nonpharmaceutical interventions (NPIs) are public health measures that aim to suppress the transmission of infectious diseases, including border restrictions, quarantine and isolation, community management, social distancing, face mask usage, and personal hygiene. This research aimed to assess the co-benefits of NPIs against COVID-19 on notifiable infectious diseases (NIDs) in Guangdong Province, China.
Methods: Based on NID data from the Notifiable Infectious Diseases Surveillance System in Guangdong, we first compared the incidence of NIDs during the emergency response period (weeks 4–53 of 2020) with those in the same period of 2015–2019 and then compared that with the expected incidence during the synchronous period of 2020 for each city by using a Bayesian structural time series model.
Findings: A total of 514,341 cases of 39 types of NIDs were reported in Guangdong during the emergency response period in 2020, which decreased by 50·7% compared with the synchronous period during 2015–2019. It was estimated that the number of 39 NIDs during the emergency response in 2020 was 65·6% (95% credible interval [CI]: 64·0% – 68·2%) lower than expected, which means that 982,356 (95% CI: 913,443 – 1,105,170) cases were averted. The largest reduction (82·1%) was found for children aged 0–14 years. For different categories of NIDs, natural focal diseases and insect-borne infectious diseases had the greatest reduction (89·4%), followed by respiratory infectious diseases (87·4%), intestinal infectious diseases (59·4%), and blood-borne and sexually transmitted infections (18·2%). Dengue, influenza, and hand-foot-and-mouth disease were reduced by 99·3%, 95·1%, and 76·2%, respectively. Larger reductions were found in the regions with developed economies and a higher number of COVID-19 cases.
Interpretation: NPIs against COVID-19 may have a large co-benefit on the prevention of other infectious diseases in Guangdong, China, and the effects have heterogeneity in populations, diseases, time and space.
Funding: Key-Area Research and Development Program of Guangdong Province
Keywords: COVID-19, Notifiable infectious diseases, Nonpharmaceutical interventions
Research in context.
Evidence before this study
The COVID-19 pandemic has had a significant disruptive impact on the economy, society, environment, and human health throughout the world. As of 15 July 2021, several studies have described that a few infectious diseases were collaterally reduced during the COVID-19 pandemic. To our knowledge, no study has comprehensively assessed the spatial and temporal co-benefits of nonpharmaceutical interventions (NPIs) against COVID-19 on notifiable infectious diseases (NIDs) in a large population where strict NPIs have been implemented.
Added value of this study
Stricter NPIs against COVID-19 may have greater co-benefits on NIDs in Guangdong Province but with spatiotemporal or disease-specific heterogeneity. The largest reduction in NIDs was found for NIDs in children, natural focal diseases and insect-borne infectious diseases (i.e., dengue), respiratory infectious diseases (i.e., influenza), intestinal infectious diseases (i.e., hand-foot-and-mouth disease), and the reduction may be associated with NPIs implemented against the COVID-19 pandemic.
Implications of all the available evidence
The findings in Guangdong indicate that NPIs are crucial for NID prevention and control. Our study also suggests that some NPIs, such as border restrictions, quarantine and isolation, community management, social distancing, face mask usage, and personal hygiene encouragement, would be very effective measures for the prevention and control of infectious diseases in the future, especially for respiratory infectious diseases (e.g., influenza), vector-borne infectious diseases (e.g., dengue), and intestinal infectious diseases (e.g., hand-foot-month disease).
Alt-text: Unlabelled box
1. Introduction
Coronavirus disease 2019 (COVID-19) was declared a pandemic by the World Health Organization (WHO) on 11 March 2020, and it is affecting more than 200 countries and areas, with more than 216 million cases by 29 August 2021 [1]. The COVID-19 pandemic has had significantly disruptive impacts on the economy [2], society [3], environment [4], and human health [5] throughout the world.
However, studies have shown that several infectious diseases, such as influenza and tuberculosis, were collaterally reduced during the COVID-19 pandemic. For instance, the overall number of twelve notifiable infectious diseases and five non-infectious respiratory diseases in Pakistan declined by 52·3% in 2020 [6]. A similar reduction was found for seasonal influenza in Japan [7] and tuberculosis in Jiangsu, China [8]. In the Taiwan region, the cases of notifiable infectious diseases (NIDs) decreased dramatically [9], except for sexually transmitted diseases [10]. In contrast, Buckley et al. found that social distancing led to a marked decrease in sexually transmitted diseases and foodborne infections in Spain [11]. However, to our knowledge, no study has comprehensively described the demographical characteristics of the effects of NPIs against COVID-19 at spatial and temporal scales on NIDs in a large population where strict NPIs have been implemented. Such evidence is invaluable to inform public health policy on the prevention and control of infectious diseases in the future.
Guangdong Province offers an opportunity to study the effects of NPIs on NIDs, and the findings could be referenced to other locations around the world. Guangdong Province is located in southern China and had a 126 million population in 2020. It has a hot and humid subtropical climate and is adjacent to the Hong Kong and Macao Special Administrative Regions. Guangdong is always at the front line of any outbreak of emerging infectious diseases, and it experienced the outbreak of severe acute respiratory syndrome (SARS) in 2003 and a dengue epidemic in 2014 [12,13]. During 2020, Guangdong also faced the crucial challenge of containing COVID-19 [14], and a set of NPIs was implemented to suppress COVID-19 transmission, including but not limited to intensive surveillance, border restrictions, quarantine and isolation, contact tracing, school closure, large gatherings cancelled, social distancing, mask wearing and personal hand hygiene [14,15]. Finally, the COVID-19 epidemic was successfully controlled in Guangdong in 2020 [15].
In this study, we used NID data from the Notifiable Infectious Diseases Surveillance System (NIDSS) to examine the effect of NPIs against COVID-19 on overall and specific NIDs in Guangdong, China. This study will assess the co-benefits of NPIs against COVID-19 on NIDs and deepen the understanding of NID prevention and control based on NPIs.
2. Methods
2.1. Study setting
This study selected Guangdong Province as the study site. Guangdong had the largest number of confirmed cases of COVID-19 outside of Hubei Province as of 22 January 2020 and was threatened by local epidemics and imported COVID-19, which pushed Guangdong to implement aggressive and strict NPIs to curb the epidemic of COVID-19 during 2020.
2.2. Data collection
2.2.1. NIDs
Data on NIDs from 1 January 2015 to 31 December 2020 in Guangdong were retrieved from the NIDSS in China. The NIDSS is an internet-based timely reporting system that was developed by the Chinese Center for Disease Control and Prevention and officially launched in 2004 [16]. NID data have been widely utilized by government sectors as well as domestic and overseas organizations to implement and evaluate public health programs. The NIDSS covers all public and private medical institutions in Guangdong, collecting case data with unified reporting cards [16]. All NIDs diagnosed by a doctor are required to be reported to the system. Information for each case includes gender, age, address, nationality, diagnosis, date of illness onset, imported or local case, and various potential risk factors. The NIDs were classified into three groups: Class A, Class B and Class C based on the disease characteristics and management requirements [17]. Generally, the NIDs of Class A often have higher transmissibility and pathogenicity and should be reported within 2 hours; the NIDs of Class B and Class C should be reported within 24 hours. During 2009–2019, the types of NID was 39, including 2 for Class A, 26 for Class B, and 11 for Class C. In January 2020, COVID-19 was added as a statutory NID and classified as Class B, but it was managed as a Class A NID. Table S1 provides detailed information for the 40 NIDs in China.
Population data were collected from the Guangdong Statistics Yearbook (http://stats.gd.gov.cn/). The flow of flight was collected from the Variflight company (http://www.variflight.com). The NID data in mainland China during 2015–2020 were annual data, which were collected from the annual statistical statement published on the official website of the National Health Commission of the People's Republic of China (http://www.nhc.gov.cn/jkj/).
2.2.2. NPIs against COVID-19
According to the emergency plan for public emergencies of China [18], the emergency response is divided into four levels (from level 1 to level 4). The level 1 emergency response is the highest level of response, which would initiate the strictest public health intervention measures, such as region lockdown, travel restrictions, crowd prohibition, and compulsory health quarantine. The intervention level is downgraded stepwise from level 1 to level 4. In 2020, based on the COVID-19 epidemic, the Guangdong provincial government implemented three different levels (level 1, level 2 and level 3) of public health emergency responses against COVID-19. On 23 January 2020, Guangdong initiated a level 1 emergency response, which lasted until 23 February 2020 (weeks 4–8). From 24 February to 8 May 2020 (weeks 9–19), Guangdong implemented a level 2 response. From 9 May to 31 December 2020 (weeks 20–53), Guangdong implemented a level 3 response. During the three periods, Guangdong implemented a series of NPIs to contain COVID-19. Information on NPIs during the emergency response was collected from Guangdong Provincial Center for Disease Control and Prevention and official reports (http://wsjkw.gd.gov.cn/).
2.3. Data analysis
This study focused on the impact of NPIs against COVID-19 on 39 other NIDs in 2020 in Guangdong Province. The 39 NIDs are classified into five categories according to the NIDSS categories: intestinal infectious diseases, respiratory infectious diseases, natural focal diseases and insect-borne infectious diseases, blood-borne and sexually transmitted infections, and other infectious diseases (Table S1). The incidence rates of NIDs in 2020 were calculated by the number of NID cases divided by the population in 2020, and the average incidence rates of NIDs in 2015–2019 were calculated by the total number of NID cases during 2015–2019 divided by the sum of the annual population during 2015–2019.
To investigate the impact of NPIs on NIDs, we first compared the incidence of NIDs during weeks 4–53 of 2020 with the average NID incidence during the same period of 2015–2019 and then with the expected NID incidence in weeks 4–53 of 2020. The expected numbers of NIDs in weeks 4–53 of 2020 were estimated by the Bayesian structural time series (BSTS) model, which has been widely used in previous studies [19,20].
The BSTS model consists of three main components: the Kalman filter, spike-and-slab method, and Bayesian model averaging [20], and it is well suited to discover causations with its counterfactual prediction and the observed data [20], [21], [22]. Based on the observed weekly number of NID cases during 2015–2019, we used the BSTS model to estimate the weekly counts of cases in weeks 4–53 of 2020 by accounting for seasonality and long-term trends, and the lower and upper 95% credible intervals (95% CI) were estimated. The BSTS model was specified as follows:
| (1) |
| (2) |
Equation (1) is the observation equation, and Equation (2) is the transition equation that defines how the latent state evolves [22], where yt is the number of NID cases in week t linked to a vector of latent state variables αt. Zt, Tt, and Rt are model matrices that contain a mix of known values (0 and 1). εt and ηt are the randomly and independently distributed Gaussian error terms with zero mean and variance Ht and Qt. In the model, μt is used to control the long-term trend; τt is used to control the seasonality with a variable of week (53 per year); and the model is implemented with the Markov chain Monte Carlo (MCMC) algorithm using 1000 iterations. In the initial study, the fitted curves and the values of R square showed good fitting for the model (Figure S1).
We further estimated the expected cases in 2020 by the three emergency response periods, five categories of NIDs, specific NIDs, sex, age group (children: 0–14 years; adults: 15–64 years; the elderly: ≥65 years), and city (21 prefectures in Guangdong Province). To estimate the benefits of NPIs against COVID-19 on NIDs, we used the relative reduction in NID incidence during weeks 4–53 of 2020 as the indicator [19], and the calculation formula of relative reduction was:
Relative reduction (%) = 100% × (number of expected cases – number of observed cases)/number of expected cases.
We plotted the epidemic curve of COVID-19 in Guangdong in 2020 and integrated synchronous NPIs into the plot. The NPIs were grouped into three categories according to Leung et al.’s report [23]: case-based measures (e.g., epidemiological investigation, health quarantine, nucleic acid screening), community measures (e.g., social distancing, using face masks, closing schools), and travel-related measures (e.g., limiting international airline, management and quarantine for residents from overseas countries or risk regions).
To explore the link between the reduction of NIDs and the COVID-19 cases reported in Guangdong, Spearman's correlation analysis was used to investigate the relationship between the reduction rate of NIDs and the number of COVID-19 cases in 21 cities of Guangdong Province.
We implemented the BSTS model analysis using the “bsts” and “CausalImpact” packages in R software (version 3.6.0).
2.4. Role of the funding source
The study funders had no role in the study design, data analysis, data interpretation or writing of the report. The corresponding author had full access to the data in the study and had final responsibility for the decision to submit for publication.
3. Results
3.1. Comparison between the number of NID cases in 2020 and the average annual number of NID cases during 2015–2019
As Table 1 shows, 514,341 cases of 39 NIDs were reported in Guangdong during weeks 4–53 in 2020, which decreased by 50·7% (50·2% for females vs. 51·6% for males) compared with the average annual cases during weeks 4–53 in 2015–2019. The reduction decreased with increasing age, with 73·0%, 17·5%, and 8·4% reductions for the 0–14-, 15–64-, and ≥65-year-old groups, respectively. The reduction rates varied by year, which were observed from 39·2% (2020 vs. 2015) to 65·3% (2020 vs. 2019) (Table S2). In China overall, the number of the 39 NIDs decreased by 25·5% in 2020 (5,719,657 in 2020 vs. 7,679,761 in 2019) (Table S3).
Table 1.
Comparison between the number of NID cases during weeks 4–53 in 2020 and the average annual number of NID cases during weeks 4–53 in 2015–2019 in Guangdong Province
| Notifiable infectious diseases | Weeks 4–53 |
Weeks 4–8 |
Weeks 9–19 |
Weeks 20–53 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2020 | 2015–2019 | Relative reduction (%) | 2020 | 2015–2019 | Relative reduction (%) | 2020 | 2015–2019 | Relative reduction (%) | 2020 | 2015–2019 | Relative reduction (%) | |
| Overall | 514,341 | 1,043,939 | 50·7 | 43,755 | 70,778 | 38·2 | 86,434 | 210,943 | 59·0 | 384,152 | 762,216 | 49·6 |
| Gender | ||||||||||||
| Male | 319,852 | 642,514 | 50·2 | 25,901 | 43,545 | 40·5 | 54,915 | 129,989 | 57·8 | 239,036 | 468,988 | 49·0 |
| Female | 194,489 | 401,425 | 51·6 | 17,854 | 27,233 | 34·4 | 31,519 | 80,964 | 61·1 | 145,116 | 293,228 | 50·5 |
| Age group | ||||||||||||
| Children (0–14 years) | 171,263 | 634,427 | 73·0 | 20,723 | 35,773 | 42·1 | 17,874 | 113,034 | 84·2 | 132,667 | 485,619 | 72·7 |
| Adults (15–64 years) | 291,707 | 353,454 | 17·5 | 19,768 | 30,154 | 34·4 | 57,857 | 84,695 | 31·7 | 214,082 | 238,604 | 10·3 |
| The elderly (65- years) | 51,371 | 56,058 | 8·4 | 3,264 | 4,851 | 32·7 | 10,703 | 13,214 | 19·0 | 37,403 | 37,993 | 1·6 |
| Intestinal infectious disease | 178,580 | 509,409 | 64·9 | 10,341 | 26,761 | 61·4 | 18,645 | 77,916 | 76·1 | 149,594 | 404,731 | 63·0 |
| Hand-foot-and-mouth disease | 59,448 | 368,116 | 83·9 | 445 | 3,455 | 87·1 | 1,162 | 47,714 | 97·6 | 57,841 | 316,947 | 81·8 |
| Infectious diarrhea* | 115,201 | 133,826 | 13·9 | 9,612 | 22,812 | 57·9 | 16,793 | 28,648 | 41·4 | 88,796 | 82,366 | -7·8 |
| Acute hemorrhagic conjunctivitis | 2,085 | 3,743 | 44·3 | 152 | 228 | 33·3 | 365 | 808 | 54·8 | 1,568 | 2,707 | 42·1 |
| Others | 1,846 | 3,724 | 50·4 | 132 | 266 | 50·4 | 325 | 746 | 56·4 | 1,389 | 2,711 | 48·8 |
| Respiratory infectious disease | 102,684 | 282,875 | 63·7 | 21,268 | 23,845 | 10·8 | 19,887 | 74,840 | 73·4 | 61,529 | 184,190 | 66·6 |
| Influenza | 35,590 | 184,545 | 80·7 | 16,030 | 15,891 | -0·9 | 5,034 | 50,214 | 90·0 | 14,526 | 118,441 | 87·7 |
| Pulmonary tuberculosis | 53,964 | 70,458 | 23·4 | 4,196 | 6,279 | 33·2 | 12,895 | 18,204 | 29·2 | 36,873 | 45,975 | 19·8 |
| Mumps | 11,453 | 20,265 | 43·5 | 769 | 1,144 | 32·8 | 1,567 | 4,150 | 62·2 | 9,117 | 14,971 | 39·1 |
| Scarlet Fever | 763 | 3,838 | 80·1 | 62 | 301 | 79·4 | 109 | 1,236 | 91·2 | 592 | 2,302 | 74·3 |
| Pertussis | 686 | 1,908 | 64·0 | 187 | 123 | -52·0 | 245 | 415 | 41·0 | 254 | 1,369 | 81·4 |
| Others | 228 | 1,861 | 87·7 | 24 | 107 | 77·6 | 37 | 621 | 94·0 | 167 | 1,132 | 85·2 |
| Natural focal diseases and insect-borne infectious diseases | 851 | 3,751 | 77·3 | 58 | 115 | 49·6 | 189 | 359 | 47·4 | 604 | 3,276 | 81·6 |
| Dengue fever | 50 | 2,643 | 98·1 | 5 | 14 | 64·3 | 4 | 34 | 88·2 | 41 | 2,595 | 98·4 |
| HFRS | 165 | 369 | 55·3 | 12 | 49 | 75·5 | 47 | 119 | 60·5 | 106 | 201 | 47·3 |
| Human brucellosis | 335 | 404 | 17·1 | 25 | 29 | 13·8 | 106 | 151 | 29·8 | 204 | 223 | 8·5 |
| Others | 301 | 335 | 10·1 | 16 | 23 | 30·4 | 32 | 55 | 41·8 | 253 | 257 | 1·6 |
| Blood-borne and sexually transmitted infections | 78,146 | 80,818 | 3·3 | 3543 | 5650 | 37·3 | 15,347 | 17,972 | 14·6 | 59,256 | 57,195 | -3·6 |
| Syphilis | 50,140 | 52,594 | 4·7 | 2529 | 3728 | 32·2 | 11,097 | 12,068 | 8·0 | 36,514 | 36,798 | 0·8 |
| Gonorrhea | 24,221 | 24,096 | -0·5 | 888 | 1666 | 46·7 | 3,531 | 4,999 | 29·4 | 19,802 | 17,430 | -13·6 |
| AIDS | 3,785 | 4,127 | 8·3 | 126 | 255 | 50·6 | 719 | 905 | 20·6 | 2,940 | 2,967 | 0·9 |
| Other infectious diseases | 154,080 | 167,087 | 7·8 | 8545 | 14407 | 40·7 | 32,366 | 39,856 | 18·8 | 113,169 | 112,824 | -0·3 |
| Hepatitis B | 127,567 | 139,217 | 8·4 | 7020 | 11999 | 41·5 | 26,684 | 33,078 | 19·3 | 93,863 | 94,140 | 0·3 |
| Other hepatitis# and neonatal tetanus | 26,513 | 27,870 | 4·9 | 1525 | 2408 | 36·7 | 5,682 | 6,778 | 16·2 | 19,306 | 18,684 | -3·3 |
Infectious diarrhea here does not include cholera, dysentery, typhoid and paratyphoid fever.
Other hepatitis includes hepatitis A, hepatitis C, hepatitis D, hepatitis E, and unidentified hepatitis. Relative reduction (%) = 100% × (average annual number of cases during 2015–2019 – number of cases in 2020)/average annual number of cases during 2015–2019. HFRS: Hemorrhagic fever with renal syndrome. AIDS: Acquired immune deficiency syndrome.
For different NID categories in Guangdong, natural focal diseases and insect-borne infectious diseases were reduced most dramatically (77·3%), followed by intestinal infectious diseases (64·9%), respiratory infectious diseases (63·7%), and blood-borne and sexually transmitted infections (3·3%). In China, the most significant reductions were intestinal infectious diseases (44·5%), natural focal diseases and insect-borne infectious diseases (22·4%), respiratory infectious diseases (11·6%) and blood-borne and sexually transmitted infections (3·7%).
For specific NIDs, the top five reductions were observed in dengue fever (98·1%), hand-foot-and-mouth disease (83·9%), influenza (80·7%), scarlet fever (80·1%), and pertussis (64·0%) in Guangdong, while the top five reductions of NIDs in China were dengue fever (90·1%), scarlet fever (77·2%), pertussis (70·1%), hand-foot-and-mouth disease (64·2%) and mumps (44·8%). Detailed information on each NID is shown in Table S4.
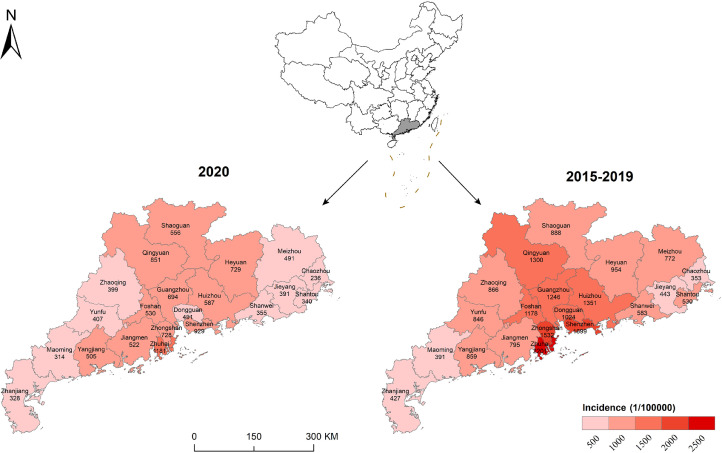
Figure 1 shows the spatial distribution of NID incidence in 2020 and 2015–2019 in Guangdong. The overall incidence of NIDs in 2020 in Guangdong Province was 520 per 100,000. We found that all 21 cities had much lower NID incidences in 2020 than in 2015–2019, and cities in the Pearl River Delta, such as Shenzhen, Zhuhai, Zhongshan, and Guangzhou, had larger reductions than the other cities in Guangdong.
Figure 1.
The spatial distribution of the incidence of 39 notifiable infectious diseases in 2020 and during 2015–2019 in Guangdong Province of China
3.2. Comparison between the observed NIDs and the expected NIDs in 2020
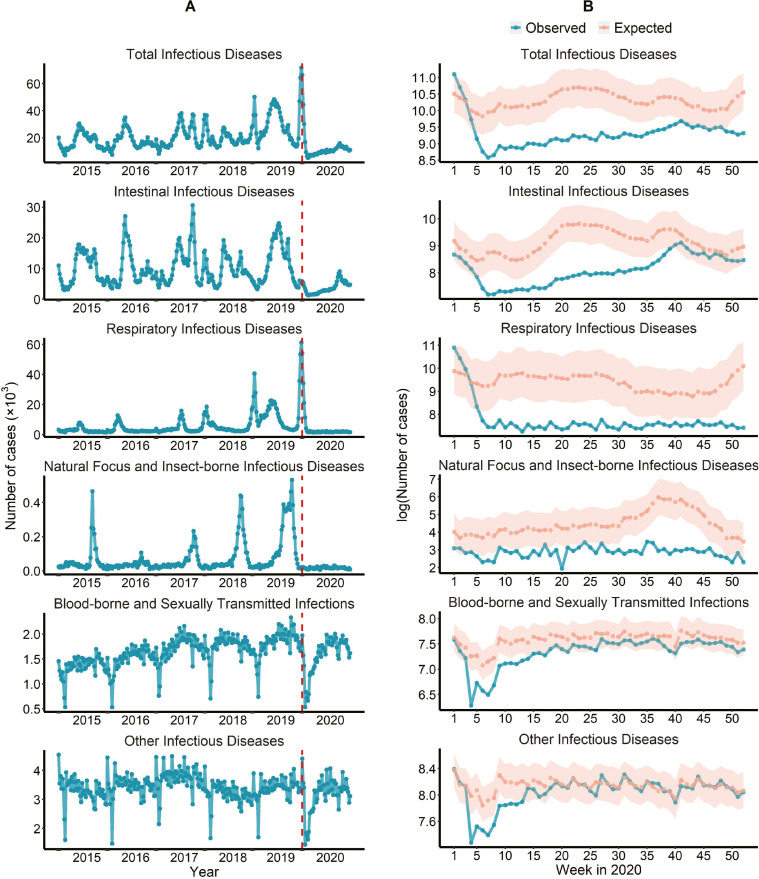
Figure 2 describes the temporal trend of observed and expected weekly counts of NIDs in Guangdong. During 2015–2019, the numbers of observed NIDs showed a slight increase with seasonal fluctuations, dropped dramatically in the first 7 weeks of 2020, and then rose gradually (Figure 2A). However, the observed numbers were much less than expected during the majority of the weeks of 2020, especially for intestinal infectious diseases, natural focus and insect-borne infectious diseases, and respiratory diseases (Figure 2B). The results for each specific NID and age- and sex-specific group are presented in Figure S2 and Figure S3.
Figure 2.
The weekly counts of observed NIDs during 2015–2020 (A) and the comparison of observed NIDs with expected NIDs (B) in 2020 in Guangdong Province, China
Table 2 shows the relative reduction of NIDs after level 1 response implementation on 23 January 2020 in Guangdong. Overall, the observed number in 2020 was 65·6% (95%CI: 64·0%–68·2%) lower than expected, which means 982,356 (95%CI: 913,443–1,105,170) cases were averted (Table S5). We found similar decreases for females (68·0%, 95% CI: 65·6%–71·6%) and males (64·0%, 95% CI: 61·6%–67·5%) and a much larger reduction for children (82·1%, 95% CI: 80·4%–84·9%) than for adults (38·2%, 95% CI: 35·3%–42·0%) and the elderly (26·2%, 95% CI: 23·1%–30·2%). For different categories of NIDs, natural focal diseases and insect-borne infectious diseases had the greatest reduction (89·4%, 95% CI: 87·2%–94·1%), followed by respiratory infectious diseases (87·4%, 95% CI: 85·6%–93·1%), intestinal infectious disease (59·4%, 95% CI: 56·3%–66·4%), and blood-borne and sexually transmitted infections (18·2%, 95% CI: 16·0%–21·0%). For specific NIDs, the five NIDS with the largest reduction were dengue fever (99·3%, 95% CI: 99·1%–99·6%), influenza (95·1%, 95% CI: 94·3%–97·4%), pertussis (90·3%, 95% CI: 89·5%–91·9%), scarlet fever (86·0%, 95% CI: 84·6%–88·7%) and hand-foot-and-mouth disease (76·2%, 95% CI: 73·0%–82·4%).
Table 2.
The relative reduction (%) of observed number of NIDs during weeks 4–53 compared with the expected in Guangdong Province of China in 2020
| Notifiable infectious diseases | Weeks 4–53 (95% CI) | Weeks 4–8 (95% CI) | Weeks 9–19 (95% CI) | Weeks 20–53 (95% CI) |
|---|---|---|---|---|
| Overall | 65·6 (64·0– 68·2) | 57·9 (50·9– 66·1) | 71·8 (68·7 – 75·8) | 64·6 (62·6 – 67·9) |
| Gender | ||||
| Male | 64·0 (61·6 – 67·5) | 58·1 (48·2 – 68·1) | 69·8 (65·3 – 75·3) | 62·9 (60·0 – 67·2) |
| Female | 68·0 (65·6 – 71·6) | 57·6 (46·5 – 69·1) | 74·6 (70·4 – 79·9) | 67·1 (64·2 – 71·5) |
| Age group | ||||
| Children (0–14 years) | 82·1 (80·4 – 84·9) | 62·4 (50·0 – 76·0) | 89·5 (87·3 – 92·4) | 81·8 (79·8 – 85·1) |
| Adults (15–64 years) | 38·2 (35·3 – 42·0) | 51·5 (43·7 – 59·6) | 49·2 (43·7 – 55·4) | 32·6 (28·6 – 37·6) |
| The elderly (65- years) | 26·2 (23·1 – 30·2) | 46·0 (38·1 – 54·4) | 35·3 (29·2 – 42·3) | 20·5 (16·4 – 25·6) |
| Intestinal infectious disease | 59·4 (56·3 – 66·4) | 68·4 (60·5 – 77·2) | 75·2 (70·8 – 82·0) | 55·0 (50·7 – 64·2) |
| Hand-foot-and-mouth disease | 76·2 (73·0 – 82·4) | 75·7 (65·5 – 87·0) | 96·5 (95·1 – 98·0) | 73·1 (69·0 – 80·6) |
| Infectious diarrhea* | 37·5 (32·8 – 44·8) | 68·4 (59·9 – 77·6) | 58·5 (51·3 – 67·9) | 21·7 (14·5 – 32·0) |
| Acute hemorrhagic conjunctivitis | 47·4 (44·2 – 52·1) | 35·6 (21·6 – 51·1) | 57·9 (52·2 – 64·7) | 45·2 (41·1 – 51·0) |
| Others | 21·5 (17·3 – 27·4) | 23·3 (9·0 – 38·0) | 31·4 (23·3 – 41·3) | 18·6 (13·1 – 25·9) |
| Respiratory infectious disease | 87·4 (85·6 – 93·1) | 71·4 (56·4 – 91·6) | 92·7 (90·5 – 97·2) | 86·8 (84·5 – 93·6) |
| Influenza | 95·1 (94·3 – 97·4) | 76·1 (61·3 – 93·5) | 98·0 (97·3 – 99·3) | 96·4 (95·6 – 98·4) |
| Pulmonary tuberculosis | 6·4 (3·2 – 10·1) | 18·7 (10·0 – 27·8) | 13·5 (7·3 – 20·3) | 1·8 (-2·2 – 6·5) |
| Mumps | 51·8 (49·7 – 54·5) | 43·2 (35·3 – 51·7) | 67·8 (64·8 – 71·2) | 48·0 (45·2 – 51·5) |
| Scarlet Fever | 86·0 (84·6 – 88·7) | 84·7 (79·6 – 89·8) | 93·7 (92·4 – 95·4) | 82·2 (79·7 – 86·6) |
| Pertussis | 90·3 (89·5 – 91·9) | 55·8 (41·2 – 71·2) | 85·5 (82·6 – 89·5) | 94·9 (94·3 – 95·9) |
| Others | 85·2 (83·3 – 88·9) | 75·8 (66·7 – 85·3) | 92·6 (90·8 – 95·3) | 82·2 (79·3 – 87·8) |
| Natural focal diseases and insect-borne infectious diseases | 89·4 (87·2 – 94·1) | 59·7 (50·0 – 77·5) | 55·6 (49·5 – 68·9) | 91·9 (90·1 – 95·7) |
| Dengue fever | 99·3 (99·1 – 99·6) | 91·7 (86·5 – 97·0) | 97·2 (96·2 – 98·7) | 99·4 (99·3 – 99·7) |
| HFRS | 36·0 (28·6 – 48·6) | 65·7 (50·0 – 80·0) | 45·3 (31·9 – 62·7) | 23·2 (11·7 – 40·8) |
| Human brucellosis | 18·9 (9·7 – 34·7) | 21·9 (-13·6 – 54·5) | 30·3 (13·8 – 52·0) | 11·3 (-1·5 – 31·8) |
| Others | -9·9 (-22·4 – 10·9) | 5·9 (-33·3– 48·4) | 28·9 (8·6 – 52·9) | -19·9 (-36·0 – 6·3) |
| Blood-borne and sexually transmitted infections | 18·2 (16·0 – 21·0) | 45·4 (40·6 – 50·8) | 27·9 (23·6 – 32·8) | 12·5 (9·7 – 16·2) |
| Syphilis | 14·6 (7·4 – 26·9) | 47·3 (30·0 – 65·6) | 26·3 (12·3 – 45·4) | 8·6 (-0·8 – 24) |
| Gonorrhea | 15·4 (12·0 – 19·5) | 53·8 (47·9 – 59·8) | 40·4 (35·5 – 45·9) | 4·7 (0 – 10·3) |
| AIDS | 19·7 (16·7 – 23·4) | 41·5 (34·3 – 49·1) | 22·9 (16·5 – 29·7) | 16·5 (12·8 – 21·2) |
| Other infectious diseases | 8·5 (5·8 – 11·9) | 40·1 (34·1 – 46·4) | 19·7 (14·5 – 25·7) | 0·6 (-3·1– 5·0) |
| Hepatitis B | 7·8 (4·5 – 11·8) | 40·1 (32·8 – 47·4) | 19·1 (12·7 – 26·3) | -0·2 (-4·6 – 5·1) |
| Other hepatitis# and neonatal tetanus | 11·7 (8·5 – 15·5) | 40·3 (33·2 – 47·4) | 22·4 (16·3 – 29·1) | 4·2 (0 – 9·1) |
Infectious diarrhea here does not include cholera, dysentery, typhoid and paratyphoid fever.
Other hepatitis includes hepatitis A, hepatitis C, hepatitis D, hepatitis E, and unidentified hepatitis. HFRS Hemorrhagic fever with renal syndrome. AIDS: Acquired immune deficiency syndrome Relative reduction (%) = 100% × (number of expected cases – number of observed cases)/number of expected cases.
During different levels of response, the reductions varied. Overall, the reduction was greater in response level 2 (71·8%, 95% CI: 68·7%–75·8%) than in response level 3 (64·6%, 95% CI: 62·6%–67·9%) and response level 1 (57·9%, 95% CI: 50·9%–66·1%), with a similar pattern for males and females. Among the different age groups, children had the same pattern as the total population, while adults and the elderly had a slowed reduction rate from a level 1 response to a level 3 response. For different NIDs categories, intestinal infectious diseases and respiratory diseases followed the reduction pattern of overall NIDs, while natural focal diseases and insect-borne infectious diseases had a much larger reduction in level 3 response (91·9%, 95% CI: 90·1%–95·7%) than that in level 1 response (59·7%, 95% CI: 50·0%–77·5%) and level 2 response (55·6%, 95% CI: 49·5%–68·9%), and blood-borne and sexually transmitted infections had a stepwise reduction from level 1 response (45·4%, 95% CI: 40·6%–50·8%), level 2 response (27·9%, 95% CI: 23·6%–32·8%) to a level 3 response (12·5%, 95% CI: 9·7%–16·2%).
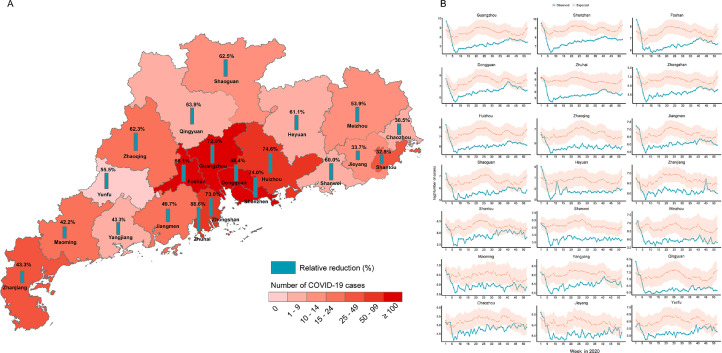
We found that a larger reduction in NIDs occurred in the regions that had higher economic development or had a higher number of COVID-19 cases (Figure 3). The developed cities in the Pearl River Delta (i.e., Guangzhou, Shenzhen, Foshan, Dongguan, Zhongshan, Zhuhai) had larger reductions than developing cities such as Qingyuan, Heyuan, Yangjiang and Chaozhou (Figure 3A and Figure 3B). Spearman's correlation analyses show that the reduction in 21 cities was positively correlated with the number of COVID-19 cases reported in the city (r = 0·53, P value < 0·05).
Figure 3.
Relative reduction (%) of 39 notifiable infectious diseases and the counts of COVID-19 cases during weeks 4–53 of 2020 in Guangdong Province (A) and the observed and expected trends of notifiable infectious diseases stratified by city in Guangdong Province in 2020 (B)
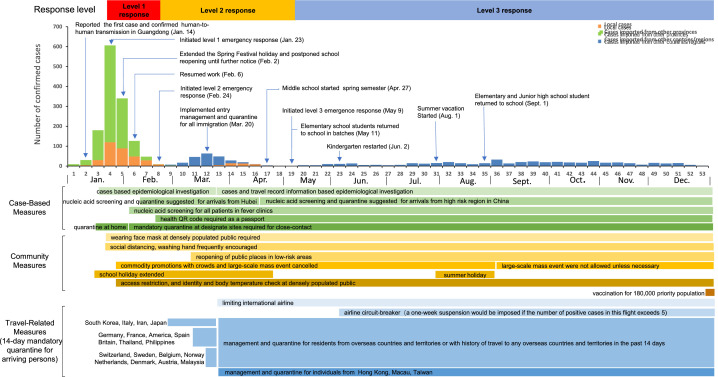
3.3. NPIs against COVID-19
In 2020, a total of 2,046 confirmed cases of COVID-19 were reported in Guangdong, including 375 local cases, 1,021 cases imported from other provinces, and 650 cases imported from other countries or regions. Figure 4 presents the epidemic curve of COVID-19 in Guangdong in 2020.
Figure 4.
The epidemic process of COVID-19 and synchronous nonpharmaceutical interventions in 2020 in Guangdong Province, China
Guangdong reported the first COVID-19 case on 14 January 2020, and the province initiated a level 1 emergency response on 23 January 2020. A series of NPIs had been implemented, including provincial border quarantine to prevent cases from Hubei Province, mandatory quarantine at designated sites for close contact, social distancing, and face mask-wearing in public (Figure 4). In addition, the start date of the spring semester for middle school, primary school, and kindergarten was postponed to 27 April, 11 May, and 2 June in 2020, respectively.
Due to the effective control of COVID-19, Guangdong resumed work on 6 February and downgraded the emergency response to level 2 on 24 February 2020. During this period, residents from or with a history of travel to overseas countries and territories needed to be quarantined for 14 days and receive health management. International flights were subsequently cut down, and travel was restricted to a specific airline.
Since 8 May 2020, as the local epidemic had been contained, the emergency response was downgraded to level 3, which is called the regular prevention and control phase. During this period, schools returned to a normal routine, but travel-related and case-based NPIs continued to be implemented. However, some NPIs had been alleviated. The implementation of the main NPIs is illustrated in Figure 4.
4. Discussion
A series of aggressive and timely NPIs were implemented by the Chinese government after the COVID-19 outbreak, which was proven to be associated with successful control of the epidemic in China [24], [25], [26]. As an unprecedented pandemic in the last century, the COVID-19 pandemic has exerted an extensive and profound negative influence on human society [4,27,28]. In the present study, using NIDSS data in Guangdong, we found that during the COVID-19 epidemic in 2020, non-COVID-19 NIDs declined significantly.
The observed NIDs in 2020 decreased dramatically compared to both the mean NID cases per year during 2015–2019 and the expected NIDs in 2020. This finding was consistent with a study in the Taiwan region [10]. Some hospital-based studies also reported similar results [8,29]. A possible reason could be the aggressive NPIs against COVID-19 implemented in Guangdong since early 2020. Most of those NPIs, such as social distancing, school closure, mask-wearing, and travel restriction, blocked the transmission of other infectious diseases, bringing the co-benefits of NIDs. However, the magnitude of reduction in Guangdong was much higher than that in the Taiwan region (10·5% reduction) [10] or mainland China (25·5% reduction). This may be attributed to stricter and more aggressive NPIs implemented by Guangdong because Guangdong reported the largest number of confirmed cases of COVID-19 in the early epidemic (1,490 cases as of 31 March 2020) outside Hubei in mainland China and faced continuous importation risk of COVID-19 across 2020. In addition, we observed a greater reduction in NIDs in the Pearl River Delta than in other cities in Guangdong because the Pearl River Delta was heavily attacked by COVID-19, and local governments implemented stricter NPIs than other regions in Guangdong.
We further found the largest reduction in NIDs in children (0–14 years). It is well known that children contribute to a major proportion of several NIDs, such as hand-foot-and-mouth disease, influenza, mumps, and scarlet fever, and these NIDs are transmitted mostly by personal contact or by air [30]. During the emergency response, schools and kindergarten were closed until May 2020 in Guangdong (Figure 4), and children paid more attention to personal hygiene, which may decrease the cases of NIDs related to children. This result was in line with the findings of previous studies [31,32], which highlights the importance of school closure for infectious disease prevention and control among children.
We also observed a significant decrease in natural focal diseases and insect-borne infectious disease, followed by intestinal infectious disease and respiratory infectious disease, and only a slight decrease was observed for blood-borne and sexually transmitted infections. The various reductions for different NID categories may depend on the extent of transmission routes impacted by NPIs. For example, dengue fever in natural focal diseases and insect-borne infectious diseases was reduced the most, and the main reason for this may be strict border restrictions and quarantine, which decrease cross-border international movement. We observed that the flow of international flights arriving in Guangdong in 2020 was reduced by 83·1% in 2020 (Figure S4), the average annual number of imported dengue cases dropped from 387 during 2015–2019 to 45 in 2020, and most of the imported cases were managed at the quarantine sites. Generally, dengue in Guangdong remains a seasonal disease occasionally triggered by imported dengue viruses in travellers [33]. Due to the large reduction in imported cases in 2020, the risk of local transmission of dengue in Guangdong decreased. This finding suggests that border quarantine may be helpful to prevent dengue outbreaks in Guangdong.
For intestinal infectious diseases, the incidence of hand-foot-and-mouth disease was reduced most significantly. Children are vulnerable to hand-foot-and-mouth disease [34]. Because of school closure extension during level 2 response in Guangdong, children spent less time in public and person-to-person contact with other children was also substantially reduced; in addition, children paid more attention to their personal hygiene, such as washing hands more frequently, which may decrease the risk of being infected with hand-foot-and-mouth disease. We also found a large reduction in respiratory infectious disease, especially of influenza, which is in line with previous studies [7,35]. Influenza infects people by droplet or contact [36], which is similar to COVID-19, and the implementation of some NPIs, such as wearing masks, washing hands, school closure and social distancing, may lead to a decrease in airborne diseases such as influenza. We found that the blood-borne and sexually transmitted infections had a reduction of 18·2%, which varied from previous findings [10,37]. For instance, Lai et al. observed that the incidence of sexually transmitted diseases was 6·7% higher in 2020 than in 2019 [10]. Our findings suggest that NIPs against COVID-19 may also have a positive impact on sexually transmitted diseases.
In 2020, the public's behaviours changed greatly to comply with NPIs. During the level 1 and 2 emergency responses, people avoided going to crowded places, stayed at home as much as possible, used face masks more often, and paid more attention to hand washing, according to two surveys [38,39]. For instance, the rates of using face masks in the period of the emergency response were high, ranging from 83·7% to 97·0% [39,40]. These findings suggest that the population in Guangdong has high protection awareness and action against COVID-19, which results in a lower risk of being infected by other NIDs.
In the level 3 emergency response, due to the effective control of COVID-19, Guangdong restarted various social and economic activities [41], and people engaged in more travel and social activity, which increased interpersonal contacts and transmission risk of other NIDs, which may explain why the reduction of some NIDs during the level 3 response decreased relative to the level 1 or 2 response. In our study, we observed the largest reduction in incidence for the 39 NIDs during the level 2 response but not during the level 1 response, possibly because NPIs have a delayed effect on controlling infectious diseases.
Based on a population of more than 126 million, the present study comprehensively investigated the spatial and temporal effects of NPIs against COVID-19 on other NIDs, which indicates the demographic and disease-specific characteristics of the effect. However, several limitations should be mentioned. First, during the COVID-19 epidemic, some people with NID infection may have hesitated to visit hospitals owing to the fear of COVID-19 infection, or some medical institutions may not have been operating regularly, and these changes may lead to underreporting for some NIDs. Second, the seasonality of several NIDs varied by year, which may lead to challenges for modelling the expected incidence. Third, the impact of NPIs on NIDs in this study is indirect due to its ecological study design, and further study based on a rigid research design is needed to determine causal inference in the future. Finally, the NPIs in Guangdong were strict, especially during the level 1 response period, which may limit the extrapolation of our findings to other countries or regions where strict NPIs were not carried out. However, based on our findings during the level 3 response, even less strict NPIs may also have great benefits for infectious disease prevention and control.
In conclusion, our study suggests that NPIs (including border restrictions, quarantine and isolation, community management, social distancing, face mask usage, and personal hygiene) against COVID-19 may have a large co-benefit on the prevention of other NIDs in Guangdong, China, and the effects have heterogeneity in populations, diseases, time and space. This finding highlights the importance of NPIs against NIDs, and some NPIs should be priorities for controlling respiratory infectious diseases (e.g., influenza), vector-borne infectious diseases (e.g., dengue), and intestinal infectious diseases (e.g., hand-foot-month disease) in the future.
Supplementary materials
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanwpc.2021.100282.
Appendix. Supplementary materials
Contributors
WM and HZ designed the study, JX, JD, JH (Jianxiong Hu),TL, XL and WM drafted the manuscript and interpreting the results. JD, KM, YZ (Yingtao Zhang) and HZ performed surveillance and collected the data. JX, JH (Jianxiong Hu), DG, YZ (Yan Zhou), YL (Yihan Li), YQ, GH, RZ and ZZ standardized the data and performed the statistical analysis. TL, MK, HZ, QH, QD, JH (Jianhua Huang), YL (Yan Li), TS and WH provided substantial scientific insight into the interpretation of the results of the manuscript. The corresponding authors attest that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Ethical approval
The study was approved by the ethics committee of Guangdong Provincial Center for Disease Control and Prevention (No. W96-027E-202104).
Data sharing
The annual number of cases of NIDs from 2015 to 2020 in Guangdong can be accessed from the official website of the Health Commission of Guangdong Province (http://wsjkw.gd.gov.cn/). The detailed surveillance data are not available owing to data management requirements. The lead authors (HZ and WM) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported.
Declaration of Competing Interest
The authors declare they have no actual or potential competing financial interests.
Acknowledgments
We thank all the health workers who fight against the COVID-19. We thank the members of the health department and CDC in Guangdong Province for their contribution to data collection. This study was supported by Key-Area Research and Development Program of Guangdong Province (2019B111103001, 2020B111107001); Chinese Postdoctoral Science Foundation (2020T130020ZX); the Science and Technology Program of Guangdong Province (2018A030313729); Foshan Key Technology Project for COVID-19 (2020001000376).
Contributor Information
Haojie Zhong, Email: gdhaojie@163.com.
Wenjun Ma, Email: mawj@gdiph.org.cn.
References
- 1.WHO. Coronavirus disease (COVID-19) pandemic. [cited 2021 29 August]; Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- 2.Verschuur J, Koks EE, Hall JW. Observed impacts of the COVID-19 pandemic on global trade. Nature Human Behaviour. 2021;5(3):305–307. doi: 10.1038/s41562-021-01060-5. [DOI] [PubMed] [Google Scholar]
- 3.Van Bavel JJ, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M. Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour. 2020;4(5):460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- 4.Wang Q, Su M. A preliminary assessment of the impact of COVID-19 on environment–A case study of China. Science of the Total Environment. 2020;728 doi: 10.1016/j.scitotenv.2020.138915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu J, Zhang L, Yan Y, Zhou Y, Yin P, Qi J. Excess mortality in Wuhan city and other parts of China during the three months of the covid-19 outbreak: findings from nationwide mortality registries. BMJ. 2021:372. doi: 10.1136/bmj.n415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rana MS, Usman M, Alam MM, Ikram A, Salman M, Zaidi SSZ. Impact of COVID-19 preventive measures on other infectious and non-infectious respiratory diseases in Pakistan. The Journal of infection. 2021;82(5):e31–e32. doi: 10.1016/j.jinf.2021.01.018. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sakamoto H, Ishikane M, Ueda P. Seasonal influenza activity during the SARS-CoV-2 outbreak in Japan. JAMA. 2020;323(19):1969–1971. doi: 10.1001/jama.2020.6173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Q, Lu P, Shen Y, Li C, Wang J, Zhu L. Collateral impact of the Covid-19 pandemic on tuberculosis control in Jiangsu Province. China. Clinical infectious diseases. 2021;273(3):542–544. doi: 10.1093/cid/ciaa1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galvin CJ, Li YJ, Malwade S, Syed-Abdul S. COVID-19 preventive measures showing an unintended decline in infectious diseases in Taiwan. International journal of infectious diseases. 2020;98:18–20. doi: 10.1016/j.ijid.2020.06.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lai C-C, Chen S-Y, Yen M-Y, Lee P-I, Ko W-C, Hsueh P-R. 2021. The impact of the coronavirus disease 2019 epidemic on notifiable infectious diseases in Taiwan: a database analysis. Travel medicine and infectious disease. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Miguel, Buckley R, Trigo E, de la Calle-Prieto F, Arsuaga M, Díaz-Menéndez M. Social distancing to combat COVID-19 led to a marked decrease in food-borne infections and sexually transmitted diseases in Spain. Journal of Travel Medicine. 2020;27(8) doi: 10.1093/jtm/taaa134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chinese SARS Molecular Epidemiology Consortium Molecular evolution of the SARS coronavirus during the course of the SARS epidemic in China. Science. 2004;303(5664):1666–1669. doi: 10.1126/science.1092002. [DOI] [PubMed] [Google Scholar]
- 13.Xiao JP, He JF, Deng AP, Lin HL, Song T, Peng ZQ. Characterizing a large outbreak of dengue fever in Guangdong Province, China. Infectious diseases of poverty. 2016;5:44. doi: 10.1186/s40249-016-0131-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu J, du Plessis L, Liu Z, Hill V, Kang M, Lin H. Genomic Epidemiology of SARS-CoV-2 in Guangdong Province. China. Cell. 2020;181(5):997–1003. doi: 10.1016/j.cell.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xiao J, Hu J, He G, Liu T, Kang M, Rong Z. The time-varying transmission dynamics of COVID-19 and synchronous public health interventions in China. International journal of infectious diseases. 2021;103:617–623. doi: 10.1016/j.ijid.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang L, Ren X, Cowling BJ, Zeng L, Geng M, Wu P. Systematic review: national notifiable infectious disease surveillance system in China. Online Journal of Public Health Informatics. 2019;11(1):e414. [Google Scholar]
- 17.Wang L, Wang Y, Jin S, Wu Z, Chin DP, Koplan JP. Emergence and control of infectious diseases in China. Lancet. 2008;372(9649):1598–1605. doi: 10.1016/S0140-6736(08)61365-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The Government of the People's Republic of China, Emergency plan for public emergencies. 2006. [cited 2021 22 May]; Available from: http://www.gov.cn:8080/jrzg/2006-01/08/content_150878.htm.
- 19.Vizzotti C, Juarez MV, Bergel E, Romanin V, Califano G, Sagradini S. Impact of a maternal immunization program against pertussis in a developing country. Vaccine. 2016;34(50):6223–6228. doi: 10.1016/j.vaccine.2016.10.081. [DOI] [PubMed] [Google Scholar]
- 20.Brodersen KH, Gallusser F, Koehler J, Remy N, Scott SL. Inferring causal impact using Bayesian structural time-series models. The Annals of Applied Statistics. 2015;9(1):247–274. [Google Scholar]
- 21.Feroze N. Assessing the future progression of COVID-19 in Iran and its neighbors using Bayesian models. Infectious Disease Modelling. 2021;6:343–350. doi: 10.1016/j.idm.2021.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scott SL, Varian HR. Predicting the present with Bayesian structural time series. International Journal of Mathematical Modelling and Numerical Optimisation. 2014;5(1-2):4–23. [Google Scholar]
- 23.Leung GM, Cowling BJ, Wu JT. From a Sprint to a Marathon in Hong Kong. New England Journal of Medicine. 2020;382(18):e45. doi: 10.1056/NEJMc2009790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cowling BJ, Ali ST, Ng TW, Tsang TK, Li JC, Fong MW. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. The Lancet Public Health. 2020;5(5):e279–ee88. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan. China. JAMA. 2020;323(19):1915–1923. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang B, Wang J, Cai J, Yao S, Chan PKS, Tam TH. Integrated vaccination and physical distancing interventions to prevent future COVID-19 waves in Chinese cities. Nature Human Behaviour. 2021 doi: 10.1038/s41562-021-01063-2. [DOI] [PubMed] [Google Scholar]
- 27.Maliszewska M, Mattoo A, Van Der Mensbrugghe D. 2020. The potential impact of COVID-19 on GDP and trade: A preliminary assessment. World Bank Policy Research Working Paper(9211) [Google Scholar]
- 28.Škare M, Soriano DR, Porada-Rochoń M. Impact of COVID-19 on the travel and tourism industry. Technological Forecasting and Social Change. 2021;163 doi: 10.1016/j.techfore.2020.120469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Luo Z, Li S, Li N, Li Y, Zhang Y, Cao Z. Assessment of Pediatric Outpatient Visits for Notifiable Infectious Diseases in a University Hospital in Beijing During COVID-19. JAMA network open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.19224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xing W, Liao Q, Viboud C, Zhang J, Sun J, Wu JT. Hand, foot, and mouth disease in China, 2008-12: an epidemiological study. The Lancet Infectious diseases. 2014;14(4):308–318. doi: 10.1016/S1473-3099(13)70342-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Earn DJ, He D, Loeb MB, Fonseca K, Lee BE, Dushoff J. Effects of school closure on incidence of pandemic influenza in Alberta. Canada. Annals of Internal Medicine. 2012;156(3):173–181. doi: 10.7326/0003-4819-156-3-201202070-00005. [DOI] [PubMed] [Google Scholar]
- 32.Luca G, Kerckhove KV, Coletti P, Poletto C, Bossuyt N, Hens N. The impact of regular school closure on seasonal influenza epidemics: a data-driven spatial transmission model for Belgium. BMC infectious diseases. 2018;18(1):29. doi: 10.1186/s12879-017-2934-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lai S, Johansson MA, Yin W, Wardrop NA, van Panhuis WG, Wesolowski A. Seasonal and interannual risks of dengue introduction from South-East Asia into China, 2005-2015. PLoS neglected tropical diseases. 2018;12(11) doi: 10.1371/journal.pntd.0006743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tan YW, Chu JJH. Protecting the most vulnerable from hand, foot, and mouth disease. The Lancet Infectious diseases. 2021;21(3):308–309. doi: 10.1016/S1473-3099(20)30452-7. [DOI] [PubMed] [Google Scholar]
- 35.Young G, Peng X, Rebeza A, Bermejo S, De C, Sharma L. Rapid decline of seasonal influenza during the outbreak of COVID-19. ERJ open research. 2020;6(3):0296–2020. doi: 10.1183/23120541.00296-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kutter JS, Spronken MI, Fraaij PL, Fouchier RA, Herfst S. Transmission routes of respiratory viruses among humans. Current Opinion in Virology. 2018;28:142–151. doi: 10.1016/j.coviro.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Balestri R, Magnano M, Rizzoli L, Infusino S, Urbani F, Rech G. STIs and the COVID-19 pandemic: the lockdown does not stop sexual infections. Journal of the European Academy of Dermatology and Venereology. 2020;34(12):e766–e7e8. doi: 10.1111/jdv.16808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Qin Z, Shi L, Xue Y, Lin H, Zhang J, Liang P. Prevalence and Risk Factors Associated With Self-reported Psychological Distress Among Children and Adolescents During the COVID-19 Pandemic in China. JAMA network open. 2021;4(1) doi: 10.1001/jamanetworkopen.2020.35487. e2035487-e20354e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu X, Luo W-T, Li Y, Li C-N, Hong Z-S, Chen H-L. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infectious diseases of poverty. 2020;9:1–11. doi: 10.1186/s40249-020-00678-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meng H, Zhong R, Huang Q, He G, Liu T, Xiao J. Analysis on the use of face masks and basic protection awareness of the public during the COVID-19 epidemic. South China Journal of Prevention Medicine (Chinese journal) 2021;47(2):188–192. [Google Scholar]
- 41.2021. People's Government of Guangdong Province. The operation of the macroeconomy in Guangdong in 2020.http://www.gd.gov.cn/zwgk/sjfb/sjkx/content/post_3184233.html [cited 2021 22 May]Available from. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.