Abstract
Background
The prevalence of smoking in Central Queensland (CQ), Australia was higher than the state and national averages. A regional smoking cessation initiative (“10,000 Lives”) was launched to promote available interventions (e.g., Quitline). We investigated the impact of “10,000 Lives” on referral to and use of Quitline services.
Methods
We conducted an interrupted time series analysis using a segmented Poisson regression model to measure the impact of “10,000 Lives” on monthly referrals to, and use of Quitline services (counselling sessions and nicotine replacement therapy (NRT) dispatched by Quitline), in CQ compared to other areas in the state (control population). The control population included all regional areas in Queensland with a comparable smoking prevalence to CQ and similar access to Quitline's Intensive Quit Support Program. We calculated the changes in level and trend of outcomes in CQ relative to the change in the control area during the post-launch period of “10,000 Lives”. The models were checked for autocorrelation and seasonality and adjusted accordingly.
Findings
After the introduction of “10,000 Lives”, the mean monthly rate per 1,000 smoking population increased in the intervention area for each outcome; e.g., from 3.3 to 10.8 for referrals to Quitline, from 1.6 to 4.4 for initial counselling session completed. These results were validated by the controlled interrupted time series analysis which showed relative increases for each of these outcomes (238•5% for monthly rate of referral to Quitline per 1,000 smoking population and 248•6% for monthly rate of initial counselling sessions completed per 1,000 smoking population).
Interpretation
Our study demonstrates a locally coordinated health promotion initiative can promote and boost the referral to, and use of Quitline smoking cessation services.
Funding
The research is funded by a collaborative research grant between School of Public Health at University of Queensland and Central Queensland Public Health Unit which is awarded by the Central Queensland Hospital and Health Service (CQHHS93907). The lead author (AK) is supported by a University of Queensland Research Training Scholarship and a Research Higher Degree Top-up Scholarship.
Keywords: Smoking cessation, Regional initiative, Impact evaluation, Quitline, NRT, Interrupted time series
Research in context.
Evidence before this study
A recent Cochrane systematic review (Matkin, 2019) found that Quitline increase the success rate of smoking cessation attempts, but these services are under-used. Promotion and marketing of Quitline services could increase their uptake and use. We performed a search (latest at 27 April 2021) in PubMed with the following search terms related to strategies for enhancing referrals and use of Quitline: ((promot*[Title/Abstract] OR strategies *[Title/Abstract]) OR referral*[Title/Abstract]) AND (quitline[Title/Abstract]) AND (referral*[Title/Abstract] OR registration*[Title/Abstract] OR uptake*[Title/Abstract] OR call*[Title/Abstract] OR participation[Title/Abstract] OR call[Title/Abstract]))”. We reviewed 200 abstracts with title and excluded 150 articles that were not a systematic review, not an impact evaluation study, not published in English, or that were not relevant to interventions to increase the use of Quitline. We identified two relevant systematic reviews including a Cochrane review, six randomised control trials and 44 other impact evaluation studies. Research, primarily from North America and Canada shows that health promotion activities, including mass-media or social media campaigns, incentive payments to clinicians or pharmacy-led referrals, primary care practice or dental practice or nurse-led motivational referrals or electronic referrals (e.g., fax, email and web-based) can increase use of smoking Quitline services. A comprehensive strategy integrating multiple approaches including academic detailing, media campaign and access to free treatment was found to be even more effective for promotion of Quitline. Research from the Western Pacific region included in the review (three studies: two from Australia and one from Hong Kong) only examined the impact of mass media campaigns or peer-led referrals on use of Quitline services.
Added value of this study
Our study provides evidence that a low cost program focused on increasing stakeholder (e.g., clinicians, allied health professionals, community service staff) engagement substantially increased the use of Quitline services in a regional area of Australia that had high smoking prevalence. We found that immediately after the official launch of the initiative, the referrals to, initial counselling session and total counselling sessions with Quitline, and receipt of nicotine replacement therapy from the Quitline service substantially increased. This increase in use of Quitline services is expected to improve the potential impact of the service on smoking prevalence in the region.
Implication of the evidence
Health promotion programs that engage with key stakeholders can be cost-effective interventions to increase the use of Quitline services.
Alt-text: Unlabelled box
1. Introduction
Tobacco smoking remains a leading risk factor for premature mortality and morbidity in Australia. According to the Australian Burden of Disease Study, 9•3% of the total burden of disease in 2015 (13•3% of all deaths and 443,235 disability adjusted life years) were attributed to tobacco use.[1], [2] In 2016, 12•2% of the Australian adult population smoked daily, [3] compared to 14.5% in the state of Queensland. [4] Smoking prevalence is higher in regional areas, such as Central Queensland (CQ), where 16.7% of adults smoked daily in 2016.[5]
Smoking cessation support is available across Australia, including free Quitline services[6] and subsidised smoking cessation medicines when prescribed by a medical practitioner. Unsubsidised NRT is also available over the counter from pharmacies and general retailers.
In addition to the standard telephone counselling service that has been available to all people in Queensland since 2005,[7] the Queensland Quitline also offers an Intensive Quit Support Program (IQSP) for priority populations. The IQSP provides counselling and a free 12-week course of combination NRT.[8], [9] The populations eligible for the IQSP are determined according to having a higher smoking prevalence than the overall Queensland population, or being at higher risk of adverse outcomes (e.g. pregnant women). As a region with higher smoking prevalence than the state average, all people living in CQ have been eligible for the IQSP since February 2017.[7] Hence, people living in CQ have access to an evidence-based free smoking cessation intervention that provides combined pharmacological and behavioural support.[10], [11], [12], [13] However, under-use of the Quitline service limits the impact of this program. For example, fewer than 2% of Australians who smoke used a Quitline service in 2019.[14]
Previous research shows that health promotion programs, such as mass media campaigns, targeted mailings, incentive payments to clinicians, and pharmacy-led referrals can increase use of Quitline services.[15], [16], [17], [18], [19] However, the research on interventions to increase Quitline use in the Western Pacific region is limited to evaluations of Australian mass media campaigns. These studies found that mass media anti-smoking campaigns significantly increased the volume of calls to the Quitline.[19], [20] However, we did not find any published research from the region on the impact of other community based interventions to increase Quitline use.
Central Queensland Hospital and Health Service (CQHHS) set a goal of reducing the daily smoking rate in CQ from 16•7% in 2015-2016 to 9•5% by 2030.[21] Achieving this target is equal to reducing the number of people who smoke by 20,000, resulting in saving 10,000 lives from premature smoking-related mortality, based on the estimate that half of all people who smoke without quitting will die prematurely.[22] Central Queensland Public Health Unit (CQPHU), with support from CQHHS, translated this goal into an actionable health promotion initiative named “10,000 Lives,” which was officially launched in November 2017.
The “10,000 Lives” initiative promotes existing smoking cessation support services, particularly the Quitline IQSP, to clinical populations and the wider community in CQ using multiple strategies. The “10,000 Lives” program is described in detail elsewhere.[23] Briefly, “10,000 Lives” is coordinated by a Senior Project Officer (SPO) and guided by the Director and Public Health Physician of the CQPHU. The SPO identifies potential champions from CQHHS who are encouraged to implement smoking cessation activities. Clinicians are encouraged to identify patients who smoke and to refer them to Quitline either through an evidence-based tool called the ‘Smoking Cessation Clinical Pathway’ (SCCP),[24] the Quitline on-line referral form, or encouraging the patient to contact Quitline themselves via telephone or the website (https://quithq.initiatives.qld.gov.au/). The SPO also recruits and collaborates with champions from the general community, community service organisations, and the local media to promote smoking cessation interventions including Quitline.
In this study, we investigated the impact of the “10,000 Lives” initiative on referrals to and use of Quitline, in addition to the impact of making the IQSP available to the CQ population.
2. Methods
2.1. Study area and population
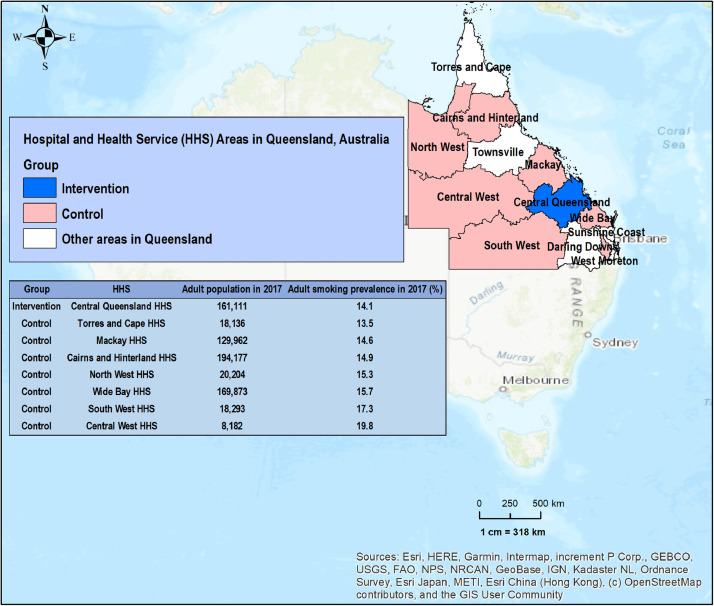
The intervention area (Figure 1) is the CQHHS catchment area (a regional area of Queensland, Australia), which has a population of ~218,283 (adult population ~161,111).[25] In 2016, 16.7% of the region's population smoked daily, which is about 40% higher than the state average (11.9%).[5], [26]
Figure 1.
Study area map showing the intervention and control areas in Queensland, Australia with their population size and smoking prevalence in 2017-2018.
The control area consists of the catchment areas of the Hospital and Health Services of Mackay, Cairns and Hinterland, Cape York and Torres, North West, South West, Central West, and Wide Bay (Figure 1). These areas were selected because of their similarity to CQ in terms of being regional areas with a smoking prevalence higher than the state average and access to the IQSP, but without a regional health promotion campaign to increase its use.
2.2. Study design
This quasi-experimental study evaluated the impact of “10,000 Lives” on referrals to and use of Quitline services in CQ using an interrupted time series analysis of data obtained from Quitline preceding and following the introduction of the initiative.
2.3. Study intervention
The study intervention was the “10,000 Lives” smoking cessation campaign in CQ (see Khan et al.[23] for a detailed description). The preliminary campaign activities commenced in September 2017 ahead of the official launch on 1 November 2017.[27] The campaign activities promote existing smoking cessation support services (e.g., Quitline) through diverse communication pathways including in-person/telephone/email communication with clinicians and community workers to encourage them to refer their clients who smoke to Quitline, sharing information about the Quitline service through local radio, digital display board, signage, local newspapers, staff newsletters and a weekly CQHHS bulletin, and local general practitioners, and their Facebook pages (Supplementary Table S1).[23] The IQSP is a free (Queensland Government‐funded) smoking cessation program offering 12 weeks of NRT combined with telephone counselling sessions, which has been available to all people living in CQ who smoke since February 2017.[28] We hypothesised that the addition of the IQSP to the Quitline services offered to CQ residents would increase their use of the Quitline, and the addition of the “10,000 Lives” initiative would further increase Quitline service use in CQ.
2.4. Data source
We obtained monthly summary data of Quitline service use from the Health Contact Centre of Queensland Health (HCC) for the intervention and control areas for 72 months (1 January 2014 to 31 December 2019). We also extracted the estimated numbers of adults who smoked in the intervention and control areas for each year between 2014 to 2019 from the Preventive Health Surveys conducted by Queensland Health.[25]
2.5. Participant involvement
We used anonymised routinely collected data sources and summary data for this impact evaluation. Individual participants were not recruited for this study.
2.6. Ethical approval
The study was approved by the CQHHS Human Research Ethics Committee (HREC) (HREC/2019/QCQ/50602), and was ratified by the HREC of the University of Queensland (Clearance Number: 2019001760).
2.7. Definitions of outcome variables
We measured six outcome variables as follows:
-
1
Referral: the number of client referrals to the Quitline service received by the HCC. This could be either by client self-referral or third party referral from another person or organisation.
-
2
Initial counselling session/Participation: the number of clients who completed at least the first Quitline call.
-
3
Total counselling sessions/Interaction: the number of individual Quitline telephone counselling sessions completed in the study area comprising of initial and subsequent calls.
-
4
NRT gum dispatch: the number of nicotine gum (4 mg) pieces dispatched to IQSP clients.
-
5
NRT lozenge dispatch: the number of nicotine lozenges (4 mg) dispatched to IQSP clients.
-
6
NRT patch dispatch: the number of nicotine patches (21 mg) dispatched to IQSP clients.
The daily recommended dose for NRT gum (4 mg) is 4 to 10 pieces, for NRT lozenge (4 mg) it is 9 to 15 lozenges, and NRT patch (21 mg) is once daily application to skin.[29] Multiple forms of NRT are often prescribed for use in combination, depending on heaviness of smoking, and recommended treatment duration is 8 to 12 months.[29] Quitline Queensland dispatch the NRT (gum, lozenge, patch, or a combination of these) based on the individual requirements of each client and is therefore variable between clients. However, the definition of all outcome variables is consistent across the intervention and control areas.
2.8. Defined study period
We considered the following three defined periods in our study:
-
•
Period 1 (1 January 2014 to 31 January 2017) is the pre-launch period of IQSP;
-
•
Period 2 (1 February 2017 to 31 August 2017) is the period between launching of IQSP by Quitline until the “10,000 Lives” was launched; and
-
•
Period 3 (1 November 2017 to 31 December 2019) is the post-launch period of “10,000 Lives”.
Since the “10,000 Lives” initiative started activities from 1 September 2017 and officially launched on 1 November 2017, we defined a buffer period (informal activities) of two months (1 September 2017 to 31 October 2017) and excluded this period during data modelling.
2.9. Statistical analysis
The data were imported from a Microsoft Excel spreadsheet into R studio[30] for cleaning, manipulation and analysis. Firstly, we conducted a descriptive analysis and produced summary statistics including monthly rates of referrals to Quitline, initial counselling session completion, total counselling sessions, and NRT (individual pieces of gum, lozenges and patches) dispatched from Quitline per 1,000 population who smoke for the intervention and control areas in the three defined time periods (defined above). We reported the differences in outcomes (measured by two-sample independent t-tests) between intervention and control areas for each period.
Subsequently, we conducted an interrupted time series (ITS) analysis[25], [31] using a segmented Poisson regression to measure the impact of “10,000 Lives” on the six outcomes. Our proposed impact model hypothesized a significant level change in the monthly rate of the outcomes in the post-“10,000 Lives” period (Period 3) and that the higher level in each outcome would be maintained. We considered the effect of the IQSP, which was launched prior to the main intervention of interest (“10,000 Lives”) in February 2017, for the first three outcomes: referrals to Quitline, initial counselling session completed, and total counselling sessions. In the final model (controlled ITS), we measured the impact of “10,000 Lives”, accounting for comparative changes in the monthly rate (per 1,000 population who smoke) in the intervention area relative to the control area. We conducted a similar statistical analysis to examine the outcome of NRT (gum, lozenges and patches) dispatched by Quitline only for the period between 1 February 2017 to 31 December 2019 (35 months) because the IQSP was not accessible to the whole population in the intervention and control areas until 1 February 2017.
We adapted[32] the following equation to measure impact by regressing an output series (Y) at time t and group g (g = 1 for intervention area and g = 0 for control area):
Where β0 denotes the pre-existing level at t = 0, β1 is the outcome that indicates the time unit (monthly) increase (i.e., underlying trend during the pre-intervention period), β2 is the level change following introduction of the first intervention (IQSP); β3 indicates the trend change following IQSP commencement, β4 is the level change of outcome after introduction of the main intervention of interest (10,000 Lives) and β5 indicates the trend changes following the introduction of “10,000 Lives”. We included the time variable (T), which is incremented since the beginning of the study, and two dummy variables: Pt (IQSP) and Qt (“10,000 Lives”) coded as 0 for pre-intervention and 1 for post-intervention. Finally, et indicates the correlation in the error terms.
We used a generalized linear model (GLM) with Poisson regression since our outcome variables were monthly counts. All models were adjusted for autocorrelation and seasonality. Autocorrelation was checked by plotting autocorrelation function (ACF) and partial autocorrelation function (PACF) demonstrating the Autoregressive (AR) and Moving Average (MA) process.[33] We checked for seasonality by fitting Fourier terms (pairs of sine and cosine functions) into our model.[33] Adjusted seasonal trend and AR and MA lags are considered in the final model where applicable.
2.10. Role of the funding source
The funders of the project had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
3. Results
3.1. Summary statistics of Quitline data
During the entire study period of 1 January 2014 and 31 December 2019, 11,791 Quitline referrals were made from the intervention area, resulting in 5,173 initial calls (initial counselling session in Quitline), 20,106 total counselling sessions with Quitline, and dispatch of 797,124 pieces of short acting NRT (402,004 pieces of 4 mg gum and 395,120 pieces of 4 mg lozenge) and 194,299 pieces of long acting NRT (21 mg patch) to IQSP clients from 1 February 2017.
During the 72 months, the intervention area had a higher overall monthly rate per 1,000 smoking population (mean ± standard deviation) for each outcome than the control area: 6•35 ± 3•72 vs 4•42 ± 1•19 for referrals to Quitline, 2•77 ± 1•51 vs 1•77 ± 0•34 for initial counselling sessions completed, and 10•88 ± 7•15 vs 6•76 ± 2•13 for total counselling sessions. The overall monthly rate per 1,000 smoking population (mean ± standard deviation) of dispatching each form of NRT to the intervention area clients was also substantially higher than the control area from February 2017 to December 2019 (35 months): 470•95 ± 212•51 vs 153•10 ± 54•71 for gum, 463•68 ± 233•91 vs 140•53 ± 59•73 for lozenges, and 227•51 ± 85 vs 69•03 ± 17•08 for patches. The summary statistics of the monthly rates of referral to Quitline, initial counselling sessions completed, and total counselling sessions for the intervention and control areas during the three different periods are presented in Table 1, including the monthly rate of dispatch of NRT gum, lozenge and patch to IQSP clients in those areas in periods 2 and 3.
Table 1.
Comparative summary statistics between intervention area and control area of the monthly rate of referral to, initial counselling session, and total counselling sessions with Quitline and different form of NRT (gum, lozenge and patch) dispatch from Quitline in three different periods.
|
Period 1 (N=37 months) |
Period 2 (N=07 months) |
Period 3 (N=26 months) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Indicators | Intervention area | Control area | Mean difference | Intervention area | Control area | Mean difference | Intervention area | Control area | Mean difference |
| (95% CI) | (95% CI) | (95% CI) | |||||||
| Referrals/1,000 smokers/month | |||||||||
| mean (sd) | 3•32 ± 0•85 | 3•75 ± 0•70 | -0•43* | 4•86 ± 0•49 | 3•72 ± 0•56 | 1•14 * | 10•76 ± 1•62 | 5•60 ± 0•98 | 5•16*** |
| (-0•07 to -0•79) | (0•52 to 1•75) | (4•41 to 5•91) | |||||||
| median (Q1, Q3) | 3•20 (2•86, 3•92) | 3•93 (3•19, 4•19) | 5•04 (4•56, 5•16) | 3•84 (3•69, 3•97) | 10•76 (9•91, 11•34) | 5•49 (5•01, 6•23) | |||
| min | 1•77 | 2•07 | 4•04 | 2•55 | 7•44 | 3.98 | |||
| max | 5•24 | 5•12 | 5•48 | 4•33 | 14•00 | 8•18 | |||
| Participation (Initial counselling sessions)/1,000 smokers/month | |||||||||
| mean (sd) | 1•59 ± 0•47 | 1•66 ± 0•33 | -0•08 | 2•27 ± 0•27 | 1•57 ± 0•24 | 0•70* | 4•36 ± 0•87 | 1•99 ± 0•30 | 2•37*** |
| (-0•25 to 0•12) | (0•40 to 1•00) | (2•00 to 2•74) | |||||||
| median (Q1, Q3) | 1•50 (1•32, 1•82) | 1•72 (1•46, 1•90) | 2•32 (2•10, 2•44) | 1•54 (1•50, 1•73) | 4•41 (3•75, 4•93) | 1•95 (1•78, 2•16) | |||
| min | 0•79 | 0•80 | 1•84 | 1•15 | 2•56 | 1•22 | |||
| max | 3•11 | 2•21 | 2•64 | 1•84 | 6•34 | 2•58 | |||
| Interaction (Total counselling sessions)/1,000 smokers/month | |||||||||
| mean (sd) | 4•99 ± 0•94 | 5•12 ± 0•65 | -0•13 | 7•80 ± 0•99 | 5•95 ± 0•87 | 1•85* | 19•62 ± 2•72 | 9•30 ± 1•10 | 10•32*** |
| (-0•50 to 0•25) | (0•75 to 2•94) | (9•14 to 11•50) | |||||||
| median (Q1, Q3) | 4•79 (4•47, 5•25) | 5•13 (4•84, 5•56) | 8•16 (7•22, 8•46) | 6•19 (5•24, 6•58) | 19•37 (18•38, 21•27) | 9•17 (8•53, 10•01) | |||
| min | 3•51 | 3•39 | 6•12 | 4•82 | 13•92 | 7•24 | |||
| max | 7•77 | 6•21 | 8.96 | 7•01 | 25•87 | 11•16 | |||
| NRT gums dispatch/1,000 smokers/month | |||||||||
| mean (sd) | 147•29 ± 39•68 | 72•35 ± 19•70 | 74•9** | 563•28 ± 148•42 | 179•44 ± 33•78 | 383•84*** | |||
| (36•92 to 112•95) | (322•64 to 445•02) | ||||||||
| median (Q1, Q3) | 139•68 (135•36, 172•80) | 64•35 (61•11, 90•67) | 605•08 (429•58, 671•04) | 180•84 (156•77, 199•16) | |||||
| min | 79•68 | 43•76 | 315•08 | 99.97 | |||||
| max | 195•36 | 94•77 | 807•48 | 234•90 | |||||
| NRT lozenges dispatch/1,000 smokers/month | |||||||||
| mean (sd) | 97•37 ± 43•99 | 51•60 ± 20•32 | 53.4* | 568.07 ± 156.81 | 168.92 ± 37.41 | 411.26*** | |||
| (3.92 to 87.62) | (334.37 to 463.92) | ||||||||
| median (Q1, Q3) | 92.80 (64.00, 126.40) | 55.90 (38.34, 68.08) | 574.65 (500.80, 677.39) | 169.99 (145.97, 195.15) | |||||
| min | 44.80 | 22.21 | 233.60 | 88.19 | |||||
| max | 163.20 | 70.23 | 831.30 | 228.36 | |||||
| NRT patches dispatch/1,000 smokers/month | |||||||||
| mean (sd) | 87.88 ± 31.08 | 44.40 ± 19.67 | 43.5* | 261.07 ± 53.20 | 76•10 ± 8•87 | 184•97*** | |||
| (12•57 to 74•40) | (163•24 to 506•70) | ||||||||
| median (Q1, Q3) | 95•76 (74•34, 110•60) | 51•29 (27•28, 59•79) | 266•33 (224•34, 293•16) | 77•24 (70•93, 83•76) | |||||
| min | 30•24 | 18•12 | 159•38 | 52•84 | |||||
| max | 119•28 | 67•22 | 352•43 | 88•05 | |||||
Notes:
Asterisk denotes significant p-value; * for <0•05, ** for <0•01 and *** for <0•001.
Referral:the number of client referrals to the Quitline service received by the Health Contact Centre of Queensland Health (HCC). This could be either by client self-referral or third party referral from another person or organisation.
Participation(Initial counselling session): the number of clients who completed at least the first Quitline call.
Interaction(Total counselling sessions): the number of individual Quitline telephone counselling sessions completed in the study area comprising of initial and subsequent calls.
NRT gum dispatch: the number of nicotine gum (4 mg) pieces dispatched to Intensive Quit Support Program (IQSP) clients.
NRT lozenge dispatch: the number of nicotine lozenges (4 mg) dispatched to IQSP clients.
NRT patch dispatch: the number of nicotine patches (21 mg) dispatched to IQSP clients.
Period 1 = Pre-launch period of any intervention (January 2014 to January 2017).
Period 2 = Time between launching of IQSP by Quitline until the “10,000 Lives” started to work (February 2017 to August 2017).
Period 3 = Post-launch period of “10,000 Lives” (November 2017 to December 2019).
We found a significantly (p<0.05) lower monthly rate (per 1,000 population smoking) of referrals from the intervention area than the control area in the pre-IQSP period (Period 1), with a mean difference of -0•43 [95% CI: -0•07, -0•79]. However, in the period between the introduction of the IQSP and the “10,000 Lives” phase-in (Period 2), the monthly rates of the outcomes for the intervention area were significantly (p<0.05) higher than the control area with a mean difference of 1•14 [95% CI: 0•43, 4•17] for referrals to Quitline, 0•70 [95% CI: 0•25, 2•53] for initial counselling sessions completed, and 1•85 [95% CI: 0.45, 6.92] for total counselling sessions. In this period, the monthly rates of dispatch of NRT to the intervention area were also significantly (p<0.05) higher than the control area with a mean difference of 74•9 [95% CI: 36•92, 112•95] for gum, 53•4 [95% CI: 3•92, 87•62] for lozenges, and 43•5 [95% CI: 12•57, 74•40] for patches. Subsequently, we observed even higher monthly rates (p<0.001) of use of Quitline services for the intervention area than the control area with the mean differences of 5•16 [95% CI: 4•41, 5•91] for referrals to Quitline, 2•37 [95% CI: 2•00, 2•74] for initial counselling sessions completed and 10•32 [95% CI: 9•14, 11•50] for total counselling sessions. Similarly, even higher monthly rates (p<0.001) of NRT dispatch to clients in the intervention area were observed compared to control areas with mean differences of 383•84 [95% CI: 322•64, 445•02] for gum, 411•26 [95% CI: 334•37, 463•92] for lozenges, and 184•97 [95% CI: 163•24, 506•70] for patches, during period 3 (post-“10,000 Lives”).
3.2. Result from Single ITS analysis
The single interrupted time series models found an increasing trend of all outcomes from baseline (Table 2 and Supplementary Figure S2) in CQ. Our single ITS models found that the level of all outcomes significantly increased (p<0.001 for all outcomes) in the intervention area, representing increases of 277•2% [95% CI: 199•4% to 375•4%] for referrals to Quitline, 154•9% [95% CI: 128•2%, 432•5%] for initial counselling session completed, 242•7% [95% CI: 187•2%, 308•9%] for total counselling sessions, 573•9% [95% CI: 553•6%, 594•9%] for dispatch of gum, 1170•6% [95% CI: 1121•8%, 1221•5%] for lozenges, and 740•9% [95% CI: 705•7%, 777.7%] for patches after the commencement of “10,000 Lives” (Period 3). Additionally, we found a slight increase in each of the pre-existing changes (after introduction of IQSP) on the levels of the first three outcomes (12•8% [95% CI: 2•2%, 24•6%] for referrals to Quitline, 62•1 [95% CI: 39•7%, 88•2%] for initial counselling sessions completed and 58•3% [95% CI: 45•9%, 71•8%] for total counselling sessions).
Table 2.
Result from single interrupted time-series analysis of monthly referrals to, initial counselling session and total counselling sessions with Quitline in Central Queensland, Australia in three different periods between January 2014, to December 2019 (70 months, excluding 2 months buffer period between September 2017 to October 2017).
| Outcomes => |
Referral |
Initial counselling session |
Total counselling sessions |
NRT gums@ | NRT lozenges@ | NRT patches@ | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Incidence Rate Ratio (IRR) | IRR[95% CI] | Seasonality adjusted IRR[95% CI] | IRR[95% CI] | Seasonality adjusted IRR[95% CI] | IRR[95% CI] | Seasonality adjusted IRR[95% CI] | IRR[95% CI] | IRR[95% CI] | IRR[95% CI] | |
| Predictors | Level at Period 1 (Intercept) | 0•003 ***[0•002, 0•003] | 0•003 ***[0•002, 0•003] | 0•002 ***[0•002, 0•002] | 0•002 ***[0•002, 0•002] | 0•005 ***[0•005, 0•005] | 0•005 ***[0•005, 0•005] | NA | NA | NA |
| Baseline# trend (slope) | 1•012 ***[1•009, 1•015] | 1•013 ***[1•010, 1•017] | 0•994 **[0•990, 0.999] | 0•994 *[0•990, 0•999] | 0•999[0•997, 1•002] | 0•999[0•996, 1•001] | 1•081 ***[1•074, 1•087] | 1•150 ***[1•141, 1•159] | 1•165 ***[1•155, 1•174] | |
| Level in Period 2 | 1•128 *[1•022, 1•246] | 1•040[0•939, 1•151] | 1•621 ***[1•397, 1•882] | 1•555 ***[1•332, 1•815] | 1•583 ***[1•459, 1•718] | 1•561 ***[1•435, 1•698] | 0•107 ***[0•104, 0•110] | 0•054 ***[0•052, 0•056] | 0•046 ***[0•044, 0•047] | |
| Level in Period 3 | 3•772 ***[2•994, 4•754] | 4•307 ***[3•396, 5•462] | 2•549 ***[1•795, 3•621] | 3•113 ***[2•169, 4•466] | 3•427 ***[2•872, 4•089] | 3•993 ***[3•332, 4•784] | 6•739 ***[6•536, 6•949] | 12•706 ***[12•218, 13•215] | 8•409 ***[8•057, 8•777] | |
| Slope in Period 3 | 0.987 ***[0.983, 0.992] | 0.986 ***[0.981, 0•990] | 0•997[0•990, 1•003] | 0•994[0•987, 1•001] | 0•995 **[0•991, 0•998] | 0•993 ***[0•989, 0•996] | 0•914 ***[0•908, 0•920] | 0•862 ***[0•855, 0•868] | 0•842 ***[0•835, 0•849] | |
| Model fit | AIC | 813•355 | 757•007 | 666•541 | 635•415 | 935•356 | 838•317 | 23238•056 | 28821•883 | 4068•585 |
| BIC | 824•598 | 777•244 | 677•784 | 655•652 | 946•599 | 858•553 | 23244•042 | 28827•869 | 4074•571 | |
| R[2] | 0•884 | 0•909 | 0•765 | 0•804 | 0•928 | 0•945 | 0•636 | 0•648 | 0•824 | |
Notes:*** p < 0•001; ** p < 0•01; * p < 0•05.
Referral:the number of client referrals to the Quitline service received by the Health Contact Centre of Queensland Health (HCC). This could be either by client self-referral or third party referral from another person or organisation.
Participation/ Initial counselling session: the number of clients who completed at least the first Quitline call.
Interaction/ Total counselling sessions: the number of individual Quitline telephone counselling sessions completed in the study area comprising of initial and subsequent calls.
NRT gum dispatch: the number of nicotine gum (4 mg) pieces dispatched to Intensive Quit Support Program (IQSP) clients.
NRT lozenge dispatch: the number of nicotine lozenges (4 mg) dispatched to IQSP clients.
NRT patch dispatch: the number of nicotine patches (21 mg) dispatched to IQSP clients.
Period 1= Pre-launch period of any intervention (Jan-2014 to Jan-2017), N=44 months;Period 2= Time between launching of IQSP by Quitline until the “10,000 Lives” started to work (February 2017 to August 2017), N=07 months;Period 3 = Post-launch period of “10,000 Lives”(November 2017 to December 2019), N=26 months; @ Data of this outcome during pre-intervention is only for 7 periods which may cause error in estimation and adjustment of seasonality is not viable. # Baseline period for the outcomes: Referral, initial counselling session and total counselling sessions is Period 1 and for NRT gum, lozenge and patch is Period 2.
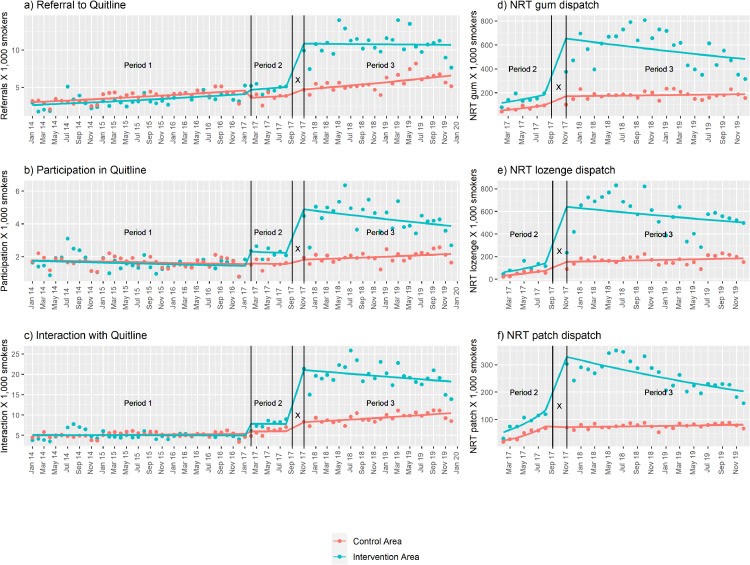
3.3. Result from controlled ITS analysis
The model results from the controlled ITS analysis are shown in Table 3 and model plots are shown in Figure 2. In these models, we found that “10,000 Lives” (Period 3) accounted for an increase of 238•5% [95% CI: 157•5%, 344•8%] for referrals to Quitline, 248•6% [95% CI: 128•2%, 432•5%] for initial counselling sessions completed, and 251•6% [95% CI: 184•9%,334•0%] for total counselling sessions (p< 0.001 for all outcomes) in the level of the monthly rates of these outcomes in the intervention area relative to the change in the control area. The level change in the rate of monthly dispatch of NRT to IQSP clients in the intervention area represented an increase (p<0.001 for all outcomes) of 93•6% [95% CI: 86•5%, 101•0%] for gum, 141•4% [95% CI: 130•2%, 153•1%] for lozenges and 121•6% [95% CI: 110•2%, 133•6%] for patches in the intervention area relative to the change in the control area. Through these models, we found a significant, but smaller increase in the level of the monthly rate of use of Quitline services in the intervention area relative to the change in the control area in Period 2 (45•7% [95% CI:30•5%, 62•8%] for referrals to Quitline, 58•0% [95% CI: 33•5%, 86•9%] for initial counselling sessions completed and 43•0% [95% CI: 30•5%, 56•7%] for total counselling sessions).
Table 3.
Result from of controlled interrupted time series analysis of monthly rate of referral to, initial counselling session, and total counselling sessions with Quitline, and NRT (gum, lozenge and patch) dispatched from Quitline.
| Outcomes => |
Referral | Initial counselling session | Total counselling sessions | NRT gum | NRT lozenge | NRT patch | |
|---|---|---|---|---|---|---|---|
| Incidence Rate Ratio (IRR) | IRR[95% CI] | IRR[95% CI] | IRR[95% CI] | IRR[95% CI] | IRR[95% CI] | IRR[95% CI] | |
| Predictors | Baseline (Intercept)# | 0.003 ***[0.003, 0.003] | 0.002 ***[0.002, 0.002] | 0.005 ***[0.005, 0.005] | 0.047 ***[0.046, 0.048] | 0.028 ***[0.027, 0.028] | 0.018 ***[0.018, 0.019] |
| Ration of level (Intervention/control) in Baseline# | 0.877 ***[0.813, 0.947] | 1.000[0.904, 1.107] | 1.034[0.975, 1.097] | 2.286 ***[2.206, 2.368] | 1.942 ***[1.856, 2.033] | 2.504 ***[2.383, 2.631] | |
| Trend (Slope) in Control Area in baseline period # | 1.012 ***[1.010, 1.013] | 0.996 ***[0.994, 0.998] | 1.002 ***[1.001, 1.004] | 1.110 ***[1.105, 1.114] | 1.157 ***[1.151, 1.163] | 1.225 ***[1.218, 1.231] | |
| Trend (Slope) in intervention Area in comparison to control in baseline period# | 1.001[0.997, 1.004] | 0.998[0.993, 1.003] | 0.997 *[0.994, 1.000] | 0.974 ***[0.967, 0.981] | 0.994[0.985, 1.003] | 0.951 ***[0.942, 0.961] | |
| Level in Control Area in Period 2 | 0.774 ***[0.737, 0.814] | 1.026[0.950, 1.109] | 1.107 ***[1.062, 1.153] | NA | NA | NA | |
| Level in intervention Area in comparison to control area in Period 2 | 1.457 ***[1.305, 1.628] | 1.580 ***[1.335, 1.869] | 1.430 ***[1.305, 1.567] | NA | NA | NA | |
| Level in Control Area in Period 3 | 1.115[0.964, 1.289] | 0.731 **[0.577, 0.927] | 0.975[0.869, 1.093] | 3.481 ***[3.406, 3.558] | 5.264 ***[5.127, 5.405] | 3.795 ***[3.678, 3.915] | |
| Level in intervention Area in comparison to control area in Period 3 | 3.385 ***[2.575, 4.448] | 3.486 ***[2.282, 5.325] | 3.516 ***[2.849, 4.340] | 1.936 ***[1.865, 2.010] | 2.414 ***[2.302, 2.531] | 2.216 ***[2.102, 2.336] | |
| Trend (Slope) in Control Area in Period 3 | 1.002[0.999, 1.004] | 1.011 ***[1.006, 1.015] | 1.008 ***[1.005, 1.010] | 0.905 ***[0.902, 0.909] | 0.871 ***[0.866, 0.875] | 0.820 ***[0.816, 0.825] | |
| Trend (Slope) in intervention Area in comparison to control in Period 3 | 0.986 ***[0.981, 0.991] | 0.986 ***[0.979, 0.994] | 0.987 ***[0.983, 0.991] | 1.009 *[1.002, 1.017] | 0.990 *[0.981, 0.999] | 1.026 ***[1.016, 1.036] | |
| Model Fit | AIC | 2039.824 | 1573.191 | 2164.507 | 40516.473 | 51705.044 | 7761.862 |
| BIC | 2069.241 | 1602.607 | 2193.924 | 40533.990 | 51722.561 | 7779.379 | |
| R[2] | 0.918 | 0.866 | 0.946 | 0.693 | 0.692 | 0.819 | |
Notes:
*** p < 0.001; ** p < 0.01; * p < 0.05;
Referral:the number of client referrals to the Quitline service received by the Health Contact Centre of Queensland Health (HCC). This could be either by client self-referral or third party referral from another person or organisation.
Participation/ Initial counselling session:the number of clients who completed at least the first Quitline call.
Interaction/ Total counselling sessions: the number of individual Quitline telephone counselling sessions completed in the study area comprising of initial and subsequent calls.
NRT gum dispatch: the number of nicotine gum (4 mg) pieces dispatched to Intensive Quit Support Program (IQSP) clients.
NRT lozenge dispatch: the number of nicotine lozenges (4 mg) dispatched to IQSP clients.
NRT patch dispatch: the number of nicotine patches (21 mg) dispatched to IQSP clients.
Period 1= Pre-launch period of any intervention (Jan-2014 to Jan-2017), N=44 months;Period 2= Time between launching of IQSP by Quitline until the “10,000 Lives” started to work (February 2017 to August 2017), N=07 months;Period 3 = Post-launch period of “10,000 Lives”(November 2017 to December 2019), N=26 months; @Data of this outcome during pre-intervention is only for 7 periods which may cause error in estimation and adjustment of seasonality is not viable. # Baseline period for the outcomes: Referral, initial counselling session and total counselling sessions isPeriod 1and for NRT (gum, lozenge and patch) isPeriod 2.
Figure 2.
The model plots from controlled interrupted time series analysis showing the monthly rate (per 1,000 smokers) of a) Referral to b) Participation (Initial counselling session) c) Interaction (Total counselling sessions) with Quitline and d) NRT gum, e) NRT lozenge and f) NRT patch dispatched from Quitline in intervention and control area during study period
Notes:
Referral: the number of client referrals to the Quitline service received by the Health Contact Centre of Queensland Health (HCC). This could be either by client self-referral or third party referral from another person or organisation.
Participation/ Initial counselling session: the number of clients who completed at least the first Quitline call.
Interaction/ Total counselling sessions: the number of individual Quitline telephone counselling sessions completed in the study area comprising of initial and subsequent calls.
NRT gum dispatch: the number of nicotine gum (4 mg) pieces dispatched to Intensive Quit Support Program (IQSP) clients.
NRT lozenge dispatch: the number of nicotine lozenges (4 mg) dispatched to IQSP clients.
NRT patch dispatch: the number of nicotine patches (21 mg) dispatched to IQSP clients
Period 1 = Pre-launch period of any intervention (1 January 2014 to 31 January 2017); Period 2 = Time between launching of IQSP by Quitline until the “10,000 Lives” started to work (1 February 2017 to 31 August 2017); Period 3 = Post-launch period of “10,000 Lives” (1 November 2017 to 31 December 2019); X= Buffer period (1 September 2017 to 31 October 2017) which is excluded from analysis.
3.4. Model check and sensitivity exploration
Plotting residuals and autocorrelation and partial autocorrelation functions confirmed no auto-correlation in the time series. However, seasonality was present and corrected for by reporting both seasonally adjusted and unadjusted effect sizes in the result (Table 2). Overall, we found a minimum of 0•636 R2 (Table 2 and Table 3) for the models, indicating a good fit that accounts for a large proportion of the variation in monthly rates.
Additional analyses we conducted included alternative regression models (e.g., Ordinary least squares (OLS) and generalized least squares (GLS)) after converting the count outcomes into rates. We explored and checked the model sensitivity by deducting 12 months of the pre- and post-“10,000 Lives” period data. We did not find any considerable change in the effect size in any of these models. While there were no substantial outliers detected in the data, we checked the impact of removing the months with the lowest (December) and highest (July) values consistently in the pre- and post-“10,000 Lives” periods in the model, finding no considerable change in the impact. The plots generated from the model checks are shown in Supplementary Figures S3 and S4.
4. Discussion
Our comprehensive analysis (pre-post monthly mean comparison, single ITS and controlled ITS) found that the mean monthly rates of referral to, initial counselling session, and total counselling sessions with Quitline were lower in CQ than the control areas in the first period (1 January 2014 to 31 January 2017). After introduction of the IQSP, the monthly rates of all outcomes were slightly higher in CQ than in the control area. For every outcome, we found that the introduction of “10,000 Lives” accounted for a further substantial increase in use of Quitline services within CQ. The increase in all outcomes observed after introduction of “10,000 Lives” in CQ was not observed in the control area, further validating that the increase was due to the “10,000 Lives” program.
According to our models, the “10,000 Lives” program accounted for 2,736 additional referrals, 1,396 clients who completed at least the initial Quitline counselling session, 6,597 total counselling sessions with Quitline. An additional 127,376 pieces NRT gum, 324,056 NRT lozenges and 33,245 NRT patches were dispatched from Quitline within the first 26 months of the “10,000 Lives” launched. Our models found that “10,000 Lives” further boosted the impact of the introduction of the IQSP (12 weeks free access to NRT). If “10,000 Lives” was not introduced in CQ, we estimate the IQSP alone would account for only 1,825 referrals, 450 new clients and 3,168 calls to Quitline in those 26 months.
Quitline services and other smoking cessation assistance (e.g., prescribed smoking cessation medicines) are under-used in Australia,[14] despite a strong evidence base that shows pharmacological and behavioural support can increase the success of quit attempts. Current evidence shows NRT increases the chance of successful quitting by 55% [95% CI: 49%, 61%].[13] A combination of NRT and behavioural support (e.g., Quitline telephone counselling) further enhances the chance of successful smoking cessation by 15 % [95% CI: 8%, 22%].[11], [34] Hence, the “10,000 Lives” program, which increases use of these interventions, in addition to increasing unaided quit attempts, is expected to contribute to reducing smoking prevalence in CQ. However, achieving the goal of the “10,000” Lives program will require ongoing investment in funding for the SPO position to maintain the program's momentum and ensure its sustainability.
Previous Australian studies have demonstrated the positive impact of mass media advertising campaigns on Quitline use. Also, another study found that the introduction of mandatory plain packaging for tobacco products increased calls to Quitline.[35] Our study is unique in demonstrating the substantial impact that can be achieved through a relatively inexpensive community-based program, which used multiple approaches (Supplementary Table S1) to promote the use of existing smoking cessation support. These included forming partnerships with existing programs and identifying local champions, regular communications to maintain motivation, delivery of brief intervention training in smoking cessation, and promotion of Quitline through posters, digital display boards, social media, and free mainstream media (e.g., joint activities with local radio stations). Our study demonstrated the difference that these activities made to the use of Quitline services, which maximised the impact of the introduction of the IQSP in CQ.
Our study has several limitations. The study used secondary data from Quitline, which limited the outcome variables we could evaluate due to the restricted format of the available data. For example, we were only able to calculate the monthly rate of dispatch of each individual NRT type per 1,000 smoking population because we could only obtain the number of pieces (patch, gum, and lozenges) sent to postcodes within the study and control areas rather than by client. Similarly, we were only able to access the number of initial and total counselling sessions by intervention and control area, rather than by client in each of the areas. In this study we demonstrated the impact of “10,000 Lives” on the monthly numbers or the rate of referrals to, and use of Quitline services (e.g., telephone counselling and access to NRT). These are not an absolute reflection of how many individuals have participated in the program and benefitted from this initiative for several reasons. Because the NRT dispatch started in February 2017, we had data only for 7 months of the post-IQSP period. The small number of periods limited our capacity to properly estimate the trend change during post-intervention of the outcomes related to NRT dispatch. We were also unable to fully control for other factors that might influence the Quitline data, such as other health promotion campaigns. We reviewed other concurrent health promotion campaigns that promoted Quitline services in CQ. These included a Quality Improvement Payment program which has encouraged mental health, oral health, maternal health and Indigenous health clinicians to increase smoking cessation activities since the 2014-15 financial year.[36] Some programs that focus on Indigenous peoples (e.g. Deadly Choices[37] and B.strong[38], a targeted brief intervention training program for Indigenous people funded by Queensland Health) were also active. However, all these programs were also available in the control areas and encouraging greater use of these pre-existing programs was part of the “10,000 Lives” activities. We also do not know how many people may have quit smoking in response to the “10,000 Lives” activities without using the Quitline services. We also do not know how many of the extra counselling sessions with Quitline resulted in successful quit attempts.
Nevertheless, we used a strong quasi-experimental design (ITS),[39] and incorporated both pre- and post-intervention time periods, and a comparable control group to control for random effects and to increase the validity of the study. We considered the co-intervention effect on the outcome to examine the extra impact of “10,000 Lives” in addition to the IQSP impact. The analysis evaluated the overall change in the whole population rather than the change at the individual level, which bypasses the sampling error of an experimental study.
We have not performed a cost-effectiveness analysis of the “10,000 Lives” campaign, but have previously reported[23] the total cost of the program in the first two years of its operation as A$280,748 including the amount of A$64,164 for the research and evaluation component. A cost-effectiveness analysis of the program is planned to inform the potential to implement “10,000 Lives” on a larger scale.
5. Conclusion
The “10,000 Lives” regional smoking cessation initiative increased the use of the Quitline in its first 26 months of operation. This provides a good case for leveraging existing smoking cessation interventions through a locally coordinated health promotion initiative to address a leading risk factor for premature mortality and morbidity. In light of our findings, the model of “10,000 Lives” could be an exemplar for other regional areas of Australia and internationally to address the under-use of existing smoking cessation support.
Authors contribution
AK, GK, SL and CG conceived and designed the study. AK communicated, collected and extracted the data from different sources. AK performed the primary analysis and interpretation of the data. AK, KG, GK, SL and CG critically reviewed the data analysis and interpretation. AK drafted the manuscript and all authors contributed with critical revisions to the content of the manuscript. The final version of the manuscript was approved by all authors.
Declaration of competing interests
None declared.
Acknowledgment
We acknowledge the unrestricted support from Central Queensland Public Health Unit, Central Queensland Hospital and Health Service Release of Information Unit, Quitline Queensland, Preventive Health Branch of Queensland Health for conducting this study. We are thankful to Health Contact Centre of Queensland Health for sharing the cleaned and summarised data. We are also thankful to Dr Nicolas Smoll, Public Health Registrar at Central Queensland Public Health Unit and Dr Gary Chan, NHMRC Emerging Leadership Fellow at the University of Queensland for their statistical advice and kind review of the analysis.
Data sharing statement
The primary summarised dataset that trigger the results reported in this publication will be available, with researchers who offer a methodologically comprehensive proposal, beginning 9 months and the ending 36 months following article publication. Please contact the corresponding author at gulam.khandaker@health.qld.gov.au
Patient Consent for Publication
Not applicable.
Editor note: The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of Competing Interest
The authors declare no conflict of interest.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanwpc.2021.100210.
Appendix. Supplementary materials
References
- 1.Australian Institute of Health and Welfare. Australian Burden of Disease Study 2015: Interactive data on risk factor burden 2019 [Available from: https://www.aihw.gov.au/reports/burden-of-disease/interactive-data-risk-factor-burden/contents/tobacco-use. [Access date: 17/06/2019].
- 2.Australian Institute of Health and Welfare. Data tables: ABDS 2015 Risk factors estimates 2019 [Available from: https://www.aihw.gov.au/getmedia/28658401-d7f2-4e93-bb6f-9cbd2d5fa64c/ABDS-2015-Risk-factor-data.xlsx.aspx. [Access date: 17/06/2020].
- 3.Australian Bureau of Statistics (ABS). National Health Survey: First Results, 2017-18, cat. no. 4364.0.55.001. Released at 11:30 AM (CANBERRA TIME) 07/02/2019 2018 [Available from: https://iepcp.org.au/wp-content/uploads/2019/01/4364.0.55.001-national-health-survey-first-results-2017-18.pdf. [Access date: 30/8/2019].
- 4.Australian Institute of Health and Welfare. Alcohol, tobacco & other drugs in Australia: Australian Institute of Health & Welfare; 2018 [Available from: https://www.aihw.gov.au/reports/alcohol/alcohol-tobacco-other-drugs-australia/contents/interactive-data/tobacco. [Access date: 10/8/2019].
- 5.Queensland Health. Detailed Queensland and regional preventive health survey results: Queensland Government; 2020 [updated 04/11/2020. Available from: https://www.health.qld.gov.au/research-reports/population-health/preventive-health-surveys/detailed-data. [Access date: 17/02/2021].
- 6.Greenhalgh E, Stillman S., Ford C. Cancer Council Victoria; Melbourne: 2016. 7.14 Cessation assistance: Telephone- and Internet-based interventions.https://www.tobaccoinaustralia.org.au/chapter-7-cessation/7-14-methods-services-and-products-for-quitting-te [Available from: [Access date: 05/09/2019] [Google Scholar]
- 7.Queensland Health. Smoking Prevention Strategy 2017 to 2020 2017 [Available from: https://www.health.qld.gov.au/__data/assets/pdf_file/0022/651802/health-wellbeing-strategic-framework-smoking.pdf. [Access date: 04/06/2020].
- 8.Queensland Health. Where Quitters Click: Queensland Government; 2019 [Available from: https://www.health.qld.gov.au/news-alerts/campaigns/tobacco/where-quitters-click-campaign. [Access date: 08/08/2019].
- 9.Wikepedia contributors. Quitline: Wikipedia, The Free Encyclopedia.; 2019 [Available from: https://en.wikipedia.org/w/index.php?title=Quitline&oldid=908421417. [Access date: 10/08/2019].
- 10.Patnode CD, Henderson JT, Coppola EL, Melnikow J, Durbin S, Thomas RG. Interventions for Tobacco Cessation in Adults, Including Pregnant Persons: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2021;325(3):280–298. doi: 10.1001/jama.2020.23541. [DOI] [PubMed] [Google Scholar]
- 11.Matkin W, Ordóñez-Mena JM, Hartmann-Boyce J. Telephone counselling for smoking cessation. Cochrane Database of Systematic Reviews. 2019;(5) doi: 10.1002/14651858.CD002850.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stead LF, Koilpillai P, Fanshawe TR, Lancaster T. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2016;(3) doi: 10.1002/14651858.CD008286.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hartmann-Boyce J, Chepkin SC, Ye W, Bullen C, Lancaster T. Nicotine replacement therapy versus control for smoking cessation. Cochrane Database of Systematic Reviews. 2018;(5) doi: 10.1002/14651858.CD000146.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Australian Institute of Health and Welfare. National Drug Strategy Household Survey 2019; Tobacco smoking chapter: Supplementary data tables 2020 [Available from: https://www.aihw.gov.au/reports-data/behaviours-risk-factors/smoking/data. [Access date: 29/04/2021].
- 15.Farrelly MC, Hussin A, Bauer UE. Effectiveness and cost effectiveness of television, radio and print advertisements in promoting the New York smokers' quitline. Tob Control. 2007;16(Suppl 1):i21–i23. doi: 10.1136/tc.2007.019984. Suppl 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hudmon KS, Corelli RL, de Moor C, Zillich AJ, Fenlon C, Miles L. Outcomes of a randomized trial evaluating two approaches for promoting pharmacy-based referrals to the tobacco quitline. Journal of the American Pharmacists Association : JAPhA. 2018;58(4):387–394. doi: 10.1016/j.japh.2018.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirst M, Schwartz R. Promoting a smokers' quitline in Ontario, Canada: an evaluation of an academic detailing approach. Health promotion international. 2015;30(2):310–317. doi: 10.1093/heapro/dat040. [DOI] [PubMed] [Google Scholar]
- 18.Nghiem N, Cleghorn CL, Leung W, Nair N, Deen FSV, Blakely T. A national quitline service and its promotion in the mass media: modelling the health gain, health equity and cost-utility. Tob Control. 2018;27(4):434–441. doi: 10.1136/tobaccocontrol-2017-053660. [DOI] [PubMed] [Google Scholar]
- 19.Miller CL, Wakefield M, Roberts L. Uptake and effectiveness of the Australian telephone Quitline service in the context of a mass media campaign. Tobacco Control. 2003;12(suppl 2):ii53. doi: 10.1136/tc.12.suppl_2.ii53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carroll T, Rock B. Generating Quitline calls during Australia's National Tobacco Campaign: effects of television advertisement execution and programme placement. Tob Control. 2003;12(Suppl 2) doi: 10.1136/tc.12.suppl_2.ii40. ii40-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Central Queensland Hospital and Health Services. Destination 2030 2017 [Available from: https://www.health.qld.gov.au/__data/assets/pdf_file/0037/669772/destination-2030-full.pdf. [Access date: 08/08/2019].
- 22.World Health Organization (WHO). Tobacco: WHO; 2019 [Available from: https://www.who.int/news-room/fact-sheets/detail/tobacco. [Access date: 05/08/2019].
- 23.Khan A, Green K, Khandaker G, Lawler S, Gartner C. How can a coordinated regional smoking cessation initiative be developed and implemented? A programme logic model to evaluate the ‘10,000 Lives’ health promotion initiative in Central Queensland. Australia. BMJ Open. 2021;11(3) doi: 10.1136/bmjopen-2020-044649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De Guzman KR, Snoswell CL, Puljevic C, Gupta D. Evaluating the utility of a Smoking Cessation Clinical Pathway tool to promote nicotine prescribing and use among inpatients of a tertiary hospital in Brisbane, Australia. Journal of Smoking Cessation. 2020:1–5. [Google Scholar]
- 25.Queensland Health. Data discovery tools: Queensland Governement; 2019 [Available from: https://www.health.qld.gov.au/research-reports/population-health/data-discovery. [Access date: 05/05/2020].
- 26.Queensland Health. The Health of Queenslanders 2018 Brisbane 2018 [Available from: https://www.health.qld.gov.au/__data/assets/pdf_file/0036/732789/cho-report-hhs-profiles.pdf. [Access date: 10/01/2020].
- 27.Queensland Health. 10000 Lives: Queensland Government; 2018 [Available from: https://www.health.qld.gov.au/cq/10000-lives. [Access date: 12/12/2018].
- 28.Cancer Council Queensland. Tackling Tobacco Queensland 2020 [Available from: https://cancerqld.org.au/cancer-prevention/programs-resources/tackling-tobacco-queensland/ [Access date: 23/04/2020].
- 29.Mendelsohn C. Optimising nicotine replacement therapy in clinical practice. Australian Family Physician. 2013;42:305–309. [PubMed] [Google Scholar]
- 30.Team. R. R Foundation for Statistical Computing; Vienna, Austria: 2020. R: A language and environment for statistical computing. [Google Scholar]
- 31.Linden A. Conducting Interrupted Time-series Analysis for Single- and Multiple-group Comparisons. The Stata Journal. 2015;15(2):480–500. [Google Scholar]
- 32.Beard E, Marsden J, Brown J, Tombor I, Stapleton J, Michie S. Understanding and using time series analyses in addiction research. 2019;114(10):1866–1884. doi: 10.1111/add.14643. [DOI] [PubMed] [Google Scholar]
- 33.Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B. Time series regression studies in environmental epidemiology. International journal of epidemiology. 2013;42(4):1187–1195. doi: 10.1093/ije/dyt092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hartmann-Boyce J, Hong B, Livingstone-Banks J, Wheat H, Fanshawe TR. Additional behavioural support as an adjunct to pharmacotherapy for smoking cessation. Cochrane Database of Systematic Reviews. 2019;(6) doi: 10.1002/14651858.CD009670.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Young JM, Stacey I, Dobbins TA, Dunlop S, Dessaix AL, Currow DC. Association between tobacco plain packaging and Quitline calls: a population-based, interrupted time-series analysis. The Medical journal of Australia. 2014;200(1):29–32. doi: 10.5694/mja13.11070. [DOI] [PubMed] [Google Scholar]
- 36.Queensland Health. Central Queensland Hospital and Health Service; Service Agreement 2016/17 - 2018/19 April 2019 Revision: State of Queensland (Queensland Health); 2019 [Available from: https://www.publications.qld.gov.au/dataset/central-queensland-hhs-service-agreements. [Access date: 01/10/2020].
- 37.Deadly Choices. Deadly Choices 2020 [Available from: https://deadlychoices.com.au/. [Access date: 05/05/2020].
- 38.Menzies School of Health Researc. B.strong; Quit, Eat & Move for Health 2020 [Available from: https://www.bstrong.org.au/. [Access date: 01/08/2020].
- 39.Palmgreen P. Interrupted time-series designs for evaluating health communication campaigns. Communication Methods. 2009;3(1-2):29–46. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.