Abstract
Background
Indonesia is undergoing a nutrition transition (NT) comprised of rising rates of overweight/obesity and consumption of high fat food/snacks but is still struck by undernutrition, causing a double burden of malnutrition. Little research pertains to the double burden of malnutrition and its associations with diet in rural Indonesia using primary village level data.
Methods
We conducted a 24-hour food recall and food frequency questionnaire and assessed anthropometric status of rural villagers from four villages in Central Java, Indonesia. Exploratory principal component analysis was used to identify dietary patterns and multi-level modeling was performed to identify variables associated with dietary pattern indicative of the NT.
Findings
1,521 participants were included in analysis. Double burden of malnutrition was prevalent whereby 32.3% of children were stunted, 68.8% of women 35–49 years-old were overweight, and 39% of homes were classified as double burden. The NT was evident in a dietary pattern associated with soft drink, snacks, and animal products. There was small but significant correlation between undernutrition and stunting status among children (r = −0.139, p < 0.01). The NT was associated with young age (B = 1.696, 95% CI = 1.508–1.885) but not with overweight (B = −0.099, 95% CI = −0.184–−0.013).
Interpretation
Our findings suggest that whilst the typical pattern of the double burden of malnutrition (stunted child/overweight adult) exists in rural Central Java, dietary patterns indicative of the NT are predominant among children, not adults. Overweight among adults may not be necessarily due to a diet indicative of the NT, and nutrition interventions in rural Central Java should focus on educating parents of young children about the health-risks of a diet associated with a NT.
Funding
Funding was obtained from the UBS-Optimus Foundation and the National Health and Medical Research Council.
Research in context.
Evidence before this study: We searched PubMed and Google Scholar databases for literature pertaining to the double burden of malnutrition using (but not limited to) the keywords: “double burden of malnutrition”, “NT”, “double burden of malnutrition Indonesia”, “NT Indonesia”, “dietary patterns Indonesia”, “stunting”, “stunting Indonesia”, “double burden households Indonesia”. The evidence we considered included studies using primary data in specific locations/regions, as well as studies using data from the Indonesian Family Life Survey – a national population survey. We also considered publications from organisations including the World Bank and the World Health Organisation.
Added value of this study: This is one of the first studies in Indonesia that assesses the double burden of malnutrition in conjunction with dietary patterns using primary data. We were able to ascertain that the double burden of malnutrition is prevalent in highly rural areas, not just urban cities. We were able to demonstrate that multiple dietary patterns exist, and demonstrate that the dietary pattern indicative of the NT is targeting young children the most.
Implications of all the available evidence: Nutrition policy and interventions in Indonesia need to be aware that stunted children are most likely to reside in a house with an overweight person, and need to be sensitive to the nutritional status of all household members. Tackling the rise in overweight and obesity in Indonesia will require nutrition interventions to target the youngest children as NT dietary patterns were prevalent among young children. Nutrition programs aimed at stunting recovery should identify strategies that would overcome low energy and protein intake among stunted children.
Alt-text: Unlabelled box
1. Introduction
The world is suffering from a double burden of malnutrition – the existence of undernutrition and overweight/obesity within populations, communities, households, and individuals [1]. This double burden occurs in populations which suffered historical underweight burdens, but are now undergoing a nutrition transition (NT) whereby lower physical activity is accompanied with higher consumption of calories from fat and snacks/sweetened beverages which contribute to overweight/obesity [2].
The current situation of the double burden of malnutrition and dietary patterns in Indonesia and Asia generally differ between rural and urban areas. It is well established that in lower- and middle-income countries the burden of underweight is higher in rural areas and the burden of overweight/obesity is higher in urban areas [3]. Studies have noted that children in rural areas consume less fat/protein and greater contribution of carbohydrates to energy intake than their urban counterparts [4]. This is due to the inherent lower socio-economic status of people in rural areas meaning that consumption of meat/eggs/dairy products is limited. Recently it has been noted however that the urban-rural gap in overweight is closing whereby the rise in overweight in rural areas outpaces urban areas [5].
Indonesia is no exception to this double burden, where rates of household level double burden of malnutrition (at least one member suffering from overweight/obesity and one suffering from undernutrition) as high as 30.6% have been reported [6]. Indonesia has the highest rate of child stunting in south-east Asia, but has also seen the highest percentage increase in adults overweight between 1980 to 2016 in the region [7]. Historically, undernutrition has been a focal point for assessing malnutrition in Indonesia [8] and is a disease of the poor [9], whilst overweight/obesity has not been seen as unhealthy [8] and is considered a disease of the rich [9]. This phenomenon has allowed the burden of overweight to steadily increase whilst undernutrition remains a problem, thus causing a double burden. A consequence is double burden households, where an individual suffering overweight and an individual suffering undernutrition (underweight/stunting) reside together [10]. Double burden households may be defined in multiple ways, such as the combination of overweight adult and stunted child, or overweight adult and underweight child [25]. Estimating the prevalence of double burden households is important because they are particularly sensitive towards nutrition interventions. An intervention to target underweight for example may be detrimental in a household with an underweight and an overweight member as increasing food availability to combat undernutrition may increase the severity of overweight in such persons [10].
There is mixed evidence concerning the scale of the NT in Indonesia. Panel data has suggested that despite urbanization and economic development, dietary patterns have not followed the expected NT that has been observed to occur in parallel with these changes in other settings; traditional staple diets still dominate [11]. The authors of this study did note however that moving to the capital city Jakarta was associated with increased expenditure of ‘western’ foods [11]. There is some evidence however that a NT is contributing to rising rates in overweight. Using the same national lifestyle survey dataset as Colozza et al. (2019), Roemling and Qaim (2012) observed that increasing expenditures on meat and dairy products were associated with overweight [12]. The finding that the percentage of energy from fat in West Sumatra, Indonesia increased from 11% to 23% between 1983 and 1999 supports the NT theory in Indonesia [13]. These surveys use expenditure on particular food groups as a proxy for food consumption which may not be the most reliable measurement as they do not take into account food quality, waste, or intra-household consumption differences [12]. This has led to the need for detailed studies of diet and malnutrition in Indonesia using primary data.
Little literature however has used primary localized data to investigate the double burden of malnutrition in conjunction with dietary patterns and the NT in rural Indonesia despite their clear connection [2]. Furthermore, most recent studies assessing the NT in Indonesia rely on datasets collected close to or over a decade ago, such as the Indonesian Family Life Survey [11], [14], [15] Studies tend to use either a 24-hour food recall or a food frequency questionnaire, but rarely both. This limits the reliability and precision of the data [16]. Changes in the NT have been explored between urban and rural areas [11] across time [13], [17], but little has looked at other demographic differences. As such, our study addresses these limitations as we aim to explore the double burden of malnutrition in conjunction with dietary patterns including those indicative of the NT using two types of dietary questionnaires at the village level in Central Java, Indonesia.
2. Methods
2.1. Study design, location, and population
This cross-sectional study consisted of a 24-hour food recall, food frequency questionnaire, and anthropometric measurements. Participants were male and female rural villagers aged between 3 and 94 years, and residing in Wonosobo, a primarily rural District of Central Java, Indonesia. This study was conducted in four villages (Bahasa Indonesia: Dusun) (namely Topengan, Moyosari, Rajon, and Losari) from the district of Wonosobo which are part of an overarching sanitation improvement intervention. This overarching study was a community based cluster-randomised intervention trial where 8 villages were selected on the basis of low levels of household latrine ownership, and stratified by topography (4 mountain Dusun and 4 hillside Dusun). The villages were further stratified into control and intervention groups. The four villages selected for this nutrition study comprised the control villages for the intervention, and data collection was carried out in November–December 2018. From each village 110 households were randomly selected and all members of those households aged 3 years and over were invited to join the study. 110 households per village was the sample size required to answer the research questions from the overarching study. This age group was pre-determined from the overarching sanitation improvement intervention conducted in these villages. Although pre-determined, we have retrospectively performed power calculations and they indicated sufficient sample size for our present nutrition related research questions.
2.2. Data collection
The 24-hour food recall was used to capture recent dietary intake [18]. A semi-structured questionnaire was administered by trained data collectors to ask participants to recall all foods and beverages consumed in the previous day, including the amount (measured in cups or pieces), preparation method (externally purchased vs. home-cooked), ingredients used, and time of day. When it was deemed a child too young to provide a recall, their parents/guardian reported for them. Participants were prompted to recall finer details such as side dishes, snacks, tea/coffee to encourage a complete snapshot of their consumption. Because 24-hour food recalls are prone to random error as day-to-day variation in eating habits are not accounted for, a food frequency questionnaire was also conducted. This consisted of asking participants to report the consumption of a variety of food groups (52 groups specific to the Indonesian context) as a frequency (every day, 1–2 times per week, 1–2 times per month, 1–2 times per year, never). Foods attributed to the NT such as deep-fried snacks, soft-drinks, ice-cream, chocolate, western fast-food were included in the questionnaire.
Anthropometric indicators comprising height (cm) and weight (kg) were also measured by trained project staff. Height was measured using a portable stadiometer with a measuring range of 150-2,100mm and a graduation of 1mm. Weight was measured with an Omron digital weight scale with a 0.1kg increment. Participants age, sex, education and employment were also collected.
2.3. Measurement of exposure/outcome variables
Body-mass-index (BMI) was calculated as weight in kg divided by height in m2. For adults aged 19+ years old, BMI cut-offs for asian populations were employed to categorise individuals as normal (18.5–23), underweight (<18.5), and overweight or obese (>23) [19]. For children 5–19 years old, BMI-for-age z-scores were calculated, and overweight was defined as >1 SD and underweight as <−2 SD [17]. Height-for-age z-scores were calculated for children 5–19 years old and a z-score below −2 was classified as stunted. For children younger than 5 years old, stunting was defined as height-for-age z-score <−2 SD, underweight as weight-for-age z-score <−2 SD, and overweight as BMI-for-age z-score as >2 SD [6]. Outliers for BMI among children were calculated as a BMI-for-age z-score <−5 or >5, and as BMI <14 for adults.
Energy and macronutrient intake were calculated only using the 24-hour food recall. Food and beverage intakes were tabulated as amount in cups or pieces and this was converted to grams or mililitres. A nutritional survey computer software package [20] with the Indonesian nutrient database installed was used to estimate the macronutrient (protein, carbohydrate, and fat) and energy (kcal) intake from each food and beverage, and this was used to estimate each participants daily macronutrient and energy intake. For foods where the database lacked nutrition information, an additional online Indonesian nutrition database was used [21].
Energy ratio as an exposure variable was defined as energy intake (kcal) divided by energy guideline value (kcal) given age and sex as set by the Indonesian Ministry of Health [22]. Protein ratio was calculated in the same manner. A higher energy or protein ratio implies that a participant is consuming amounts of energy/macronutrient in excess of the recommended amount.
The number of externally purchased foods consumed per day was calculated using the 24-hour food recall.
Data pertaining to food frequency was converted to a single frequency expressed as per day. For example, foods consumed every day were given a score of 1, and 1–2 times per week was calculated as 1.5 times per 7 days which corresponds to approximately 0.21 times per day. This method of standardisation to frequency per day has been performed elsewhere [23].
The double burden of malnutrition at the household level is typically defined as the presence of an overweight mother and a stunted child [24], however various definitions exist not stringent on the mother child relationship [25]. For this study we defined the double burden of malnutrition at the household level as having at least one individual suffering from a form of undernutrition measured in this study (underweight or stunting) as well as at least one individual suffering from overweight.
2.4. Statistical analysis
Statistical calculations were performed in IBM SPSS Statistics for Windows, Version 24. Participants with missing data were removed from analysis.
The prevalence of underweight, normal weight, overweight, and stunting was calculated across age and and sex categories. Following this, the distribution of the nutritional status of homes was calculated. A chi-square test of proportions was performed to measure the statistical significance of difference in stunting prevalence between age-groups.
Outliers for energy intake were identified using the following procedure. For each participant, the estimated energy requirement (EER) was calculated using age, sex, height, and weight as an input in the Institute of Medicine equation [26]. A physical activity level of 1.55 was assumed given very active agricultural activities. Then the participants estimated energy intake was divided by the EER to create a energy intake to requirement ratio and then converted to the logarithmic scale to reduce skewness and better approximate the normal distribution. Outliers were defined as those three standard deviations above or below the mean ratio. A similar method to identify outliers has been performed in other diet analysis literature [27]. A total of eight outliers for energy intake were excluded from analysis where energy intake was an exposure or outcome variable.
Factor analysis using the principal component extraction method was performed to identify dietary patterns using the standardised food frequency questionnaire data. An exploratory framework was employed whereby dietary patterns were investigated with no existing hypothesis as opposed to confirming externally recognized patterns. Varimax rotation was used to increase interpretability. Only variables with absolute rotated component loadings greater than 0.4 were considered in order to increase interpretability of the components. Variables that did not load onto any component with an absolute loading coefficient of at least 0.4 were removed sequentially in a four-step process until every variable has a loading of at least 0.4. Component scores were calculated using the regression method whereby component loadings are treated as coefficients in a multiple regression model for each participant. The Kaiser-Meyer-Olkin (KMO) test and Bartlett's test of sphericity to determine the suitability of principal component analysis for the included variables.
Correlations between nutrition-related variables (e.g macronutrient intake, externally purchased foods) and the three principal component scores were calculated using Pearson correlation.
Multi-level linear regression was performed to identify predictors of principal component scores. A multi-level model was chosen due to the hierarchial nature of the study design whereby individuals nested in homes which nested in villages. Given that dietary patterns are expected to depend on those of other household members and other households in a village a multi-level model is appropriate to account for this potential covariance. Age, sex and nutritional status that take a small number of discrete values are regarded as predictors, hence entered the model as fixed effects. To account for the hierarchial nature of the data, household and village were entered into the model as random effects. Age was categorised into six groups due to the observation that it did not have a linear association with the NT component factor score.
Point-biserial correlations between diet related variables and stunting status were calculated in order to identify significant correlates with stunting status. This correlation method is appropriate for use with dichotomous (stunting) and continuous (diet-related) variables [28].
2.5. Ethical considerations
All participants provided informed, written consent to take part in the food recall, food frequency questionnaire, and anthropometric measurements. This study was approved by Griffith University Human Research Ethics Committee (Protocol number 2014/541) and the Australian National University Human Research Ethics Committee (Protocol number 2017/038).
2.6. Role of funding source
Funding provided from the UBS-Optimus Foundation and the National Health and Medical Research Council was used to fund the data collection. The funders had no role in the study design, data analysis or interpretation, or the description of the results.
3. Results
The response rate was 81.1% leading to a total sample of 1,521 participants from four villages.
The socio-demographic characteristics of the study population are presented in Table 1. Participants were evenly spread out over age categories, villages, and sex (49.6% males). 55.7% of participants had reached elementary education and 3.9% had attained college education. Among adults, the most common occupation was farming (35.2%), followed by self-employed (18.5%). 10.5% of adults were unemployed and only 2.6% worked in a formal company.
Table 1.
Socio-demographics of the study population.
| Socio-demographic factor | N (%) | |
|---|---|---|
| Age (years) | 3–10 | 191 (12.6) |
| 10–19 | 264 (17.4) | |
| 19–34 | 333 (21.9) | |
| 34–49 | 313 (20.6) | |
| 49–64 | 314 (20.6) | |
| 64+ | 106 (7.0) | |
| Sex | Male | 754 (49.6) |
| Female | 767 (50.4) | |
| Village | Topengan | 380 (25.0) |
| Moyosari | 393 (25.8) | |
| Rajon | 340 (22.4) | |
| Losari | 408 (26.8) | |
| Education | None | 205 (13.5) |
| Elementary | 847 (55.7) | |
| Junior Secondary | 264 (17.4) | |
| Senior Secondary | 141 (9.3) | |
| College | 59 (3.9) | |
| Employment* | Company | 28 (2.6) |
| Self employed | 196 (18.5) | |
| Farmer | 374 (35.2) | |
| Home duties | 150 (14.1) | |
| Unemployed | 111 (10.5) | |
| Government employee | 25 (2.4) | |
| Other | 178 (16.7) | |
Distribution of employment type not calculated for children younger than 19.
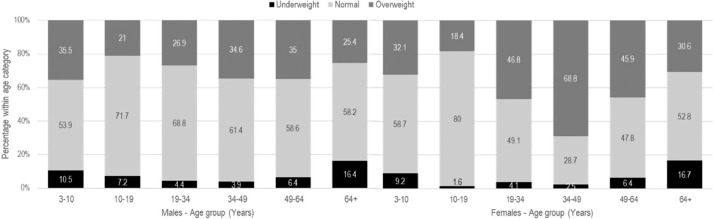
The distribution of nutritional status is shown in Figure 1. Nine outliers were removed from analysis. Among both males and females, underweight was most prevalent among the young children (10.5% and 9.2% among males and females respectively) and elderly (16.4% and 16.7% among males and females respectively). Overweight status had the lowest prevalence among 10–19 year-olds in both males and females, and peaked in middle-ages whereby the prevalence reached 68.8% in 34–49 year-old women.
Figure 1.
Distribution of normal, under- and over-weight by age and sex.
The prevalence of stunting status by age group among males and females is shown in Table 2. Prevalence was similar between 3-10 year-old and 10-19 year-old males (37.2% vs. 34.1%, p=0.376) but significantly higher among 10-19 year-old females compared to 3-10 year-old females (38.1% vs. 20.4%, p=0.002).
Table 2.
Prevalence of stunting status among children stratified by sex.
| Stunting* | p† | |
|---|---|---|
| Males – 3–10 years | 29 (37.2) | |
| 10–19 years | 47 (34.1) | 0.376 |
| Females – 3–10 years | 23 (20.4) | |
| 10–19 years | 48 (38.1) | 0.002 |
| All children 3–19 years | 147 (32.3) |
Stunting defined as Height-For-Age Z-score < -2 standard deviations [17]. Data reported as N (%) within age/sex group.
p-value obtained from chi-square test of proportion of stunting prevalence between age groups.
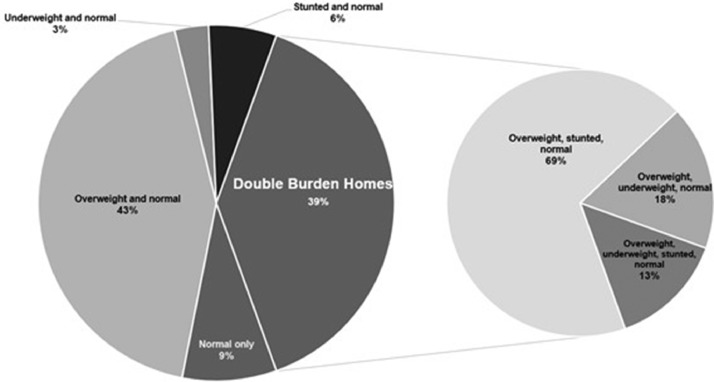
The distribution of households by nutritional status is presented in Figure 2. 43% of homes comprised overweight and normal weight individuals, while only 3% contained underweight and normal weight participants. 39% of homes were classified as double burden; comprised of overweight and stunted (69%), overweight and underweight (18%), and overweight, underweight, and stunted (13%) individuals. From this it can be calculated that of all the homes with an overweight person, 47.6% were double burden, of all the homes with an underweight person, 57.1% were double burden and of all homes with a stunted child, 84.2% were double burden.
Figure 2.
Distribution of homes in study by nutritional status. Smaller pie chart contains the breakdown of double burden homes by type (Overweight/stunted, overweight/underweight, overweight/underweight/stunted).
Initially, all 52 food groups with the exception of rice (all but one participant reported consuming rice every day) were entered into principal component analysis as variables. Initially, 15 components had eigenvalues above one indicating they explained more variation than one variable, however this was reduced to the three components with the largest eigenvalues in order to only identify dietary patterns that explained the most variance.
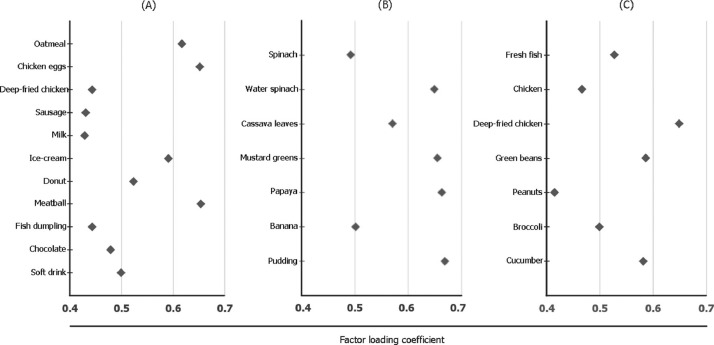
The rotated factor loading coefficients from principal component analysis are presented in Figure 3. Three components were identified: (a) “NT” (NT), (b) “Plant-based”, (c) “Staple”. The NT component was characterised by foods typically associated with the NT due to their high fat content, animal products and processing [2]. The strongest loadings were for oatmeal, chicken eggs, ice-cream, donuts, and meatballs. The “Plant-based” component was characterized by leafy greens and fruit. The last component “Staple” was a mixture of cheap meats (fresh fish, chicken) and vegetables (Green beans, Broccoli, and Cucumber). The KMO value was 0.80 indicating good fit and Bartlett's Test of Sphericity was significant at p<0.0001.
Figure 3.
Rotated factor loading coefficients of principle components identified in factor analysis of dietary patterns. (a): “Nutrition Transition” component, (b): “Plant-based diet, (c): “Staple” diet.
KMO value = 0.80. p<0.0001 for Bartlett's Test of Sphericity.
Eigenvalues for components (a), (b), and (c) respectively were 4.348, 2.561, and 1.747.
The Pearson correlations between nutrition related variables and the three dietary patterns identified are presented in Table 3. The NT component was significantly correlated with fat (r = 0.130, p < 0.01), protein (r = 0.088, p < 0.01), energy ratio (r = 0.172, p < 0.01) and externally purchased foods (r = 0.365, p < 0.01), whilst the “Plant-based” diet was negatively correlated with these variables, but positively correlated with the contribution of rice to daily energy intake. Few variables had significant correlations with the “Staple” diet. All correlations were relatively weak, with the greatest strength observed in the correlation between externally purchased foods and the NT component (r = 0.364, p < 0.01).
Table 3.
Pearson correlations of nutrients and eating habits with diet patterns identified in principle component analysis.
| Nutrition Transition | Plant-based diet | Staple diet | |
|---|---|---|---|
| Energy (kcal) | 0.036 | −0.083⁎⁎ | −0.037 |
| Fat (g) | 0.130⁎⁎ | −0.150⁎⁎ | −0.076⁎⁎ |
| Carbohydrate (g) | −0.090* | −0.024 | 0.025 |
| Protein (g) | 0.088⁎⁎ | −0.051* | −0.058* |
| Energy ratio (kcal/kcal) | 0.172⁎⁎ | −0.080⁎⁎ | −0.059* |
| Externally bought foods (#no./day) | 0.365⁎⁎ | −0.041 | −0.010 |
| Contribution of rice to energy (% kcal) | −0.157⁎⁎ | 0.193⁎⁎ | 0.046 |
p < 0.05.
p < 0.01.
Nutritional correlates with stunting status are presented in Table 4. Small but significant negative correlations were observed with energy (r = −0.139, p = 0.003) and protein ratios (r = −0.116, p = 0.014), and the Plant-based diet component identified in principal component analysis had a small but positive correlation with stunting status as positive outcome (r = 0.149, p = 0.001).
Table 4.
Point-biserial correlation of nutritional variables with stunting status.
| Factor | r | p |
|---|---|---|
| Energy ratio | −0.139 | 0.003 |
| Protein ratio | −0.116 | 0.014 |
| NT diet score | −0.026 | 0.59 |
| Plant-based diet score | 0.149 | 0.001 |
| Staple diet score | 0.022 | 0.641 |
Given the identification of a principal component suggestive of a NT, a multi-level linear regression was calculated to identify predictors of this component (Table 5). Increasing age was asasociated with lower NT component score and these associations were statistically significant (p < 0.0001, aged 65+ years as the reference group). Being overweight was associated with lower NT component scores compared to normal weight individuals (B = −0.099, 95% CI = −0.184–−0.013, p = 0.024). There was no significant difference between males and females (p = 0.386). Most variance was explained at the participant level (0.485) and less explained at the household level (0.184). These estimates were significantly different from 0 (p < 0.0001) whilst the village level estimate was not (p = 0.705).
Table 5.
Multi-level linear regression for nutrition transition factor score.
| Factor | B (95% CI) | p | |
|---|---|---|---|
| Sex | Male (Reference) | ||
| Female | 0.033 (−0.042, 0.109) | 0.386 | |
| Nutritional status | Normal (Reference) | ||
| Overweight | −0.099 (−0.184, -0.013) | 0.024 | |
| Underweight | −0.197 (−0.265, 0.071) | 0.257 | |
| Age (years) | 3–10 | 1.696 (1.508, 1.885) | <0.0001 |
| 10-19 | 1.186 (1.006, 1.366) | <0.0001 | |
| 19-34 | 0.451 (0.276, 0.626) | <0.0001 | |
| 34-49 | 0.248 (0.070, 0.425) | <0.0001 | |
| 49-64 | 0.136 (−0.041, 0.313) | 0.133 | |
| 64+ (reference) | |||
| Random effects variance (95% CI) | |||
| Village | 0.001 (0.000, 0.238, p=0.705) | ||
| Household | 0.184 (0.145, 0.234, p<0.0001) | ||
| Participant | 0.485 (0.445, 0.529, p<0.0001) | ||
First level consisted of individual level fixed effects, second level consisted of participants nested within homes, third level consisted of homes nested within villages.
Mean of nutrition transition component scores = 0, standard deviation = 1.
4. Discussion
This study assessed the prevalence of double burden of malnutrition and dietary patterns in rural Central Java, Indonesia. As hypothesized, the prevalence of the double burden was large and diets related to the NT were identified.
Overweight burdened males and females of all age groups but with the highest prevalence observed among middle-aged females and lowest prevalence among children (Figure 1). The finding that overweight prevalence was higher among women than men is consistent with other studies in Indonesia [6]. It is thought that various factors contribute to higher rates of overweight/obesity among adult women, such as physiological causes due to pregnancy and menopause, as well as the notion that the link between childhood malnutrition and subsequent overweight in adulthood is stronger in women than men [29]. This may be due to the observation of a lag in overweight trends in children compared to adults whereby overweight begins to emerge in adulthood [30]. There was a drastic drop in overweight rates in young children (32.1% prevalence in 3–10-year-old girls dropped to 18.4% in 10–19-year-old girls, Figure 1) which is reflective of general patterns of overweight prevalence in the Indonesian population [8]. It is also possible that the added physical exertion of children in this age group who would be more active participating in school and chores, as well as a more restricted diet, could explain the drop in overweight prevalence.
Almost 40% of homes in our study were double burden (Figure 2). This is comparatively larger than a national study from 2007 (16%) [31], while another study in rural parts of Indonesia found 11% of households had mother-child double burden of malnutrition [32]. Interpretation of these differences is difficult due to the plethora of double burden household definitions used. More than 84% of homes with a stunted child were double burden households (Figure 2). This is reflective of the fact that stunted child and overweight mother pairs are the epitome or paradox of the double burden of malnutrition [33]. What is also concerning was that 57.1% of homes with an underweight person were double burden (see text above Figure 2). This is because in such households where an overweight person also resides (hence double burden), interventions targeting underweight by increasing food availability for example may be detrimental by increasing the severity of overweight in such persons [10].
The three diet patterns identified in principal component analysis (Figure 3) were relatively consistent with our hypothesis: a staple diet is predicted based on the locally available and grown foods, a diet indicative of the NT is emerging, and a plant-based diet would be expected among the poorest villagers in this region. Follow-up analysis revealed that mean component scores for the Plant-based diet pattern were negatively associated with education level among adults (data not shown). The NT diet pattern correlated with animal-based food, confectionary, and snack consumption (Figure 3) and fat, protein, and externally purchased foods (Table 3) which are typical of NT diets [34].
Multi-level modelling revealed that there is an overwhelmingly negative association between age and NT component scores. These associations were significant despite adjusting for sex and BMI and household/village clustering (Table 5). The results suggest that in these villages the NT dietary pattern is driven by age, whereby the youngest have the highest consumption of these snacks, sweets, and externally purchased foods. No literature has explored this association in the same manner however the notion that parents in Java will permit their children to consume snack and junk foods has been observed in qualitative interviews [35]. There is no doubt however that such foods are more expensive, and parents in this rural region may only afford enough of these foods for their children [30]. The ramifications of this observation are important. First, given that a wealth of literature agrees that the NT is associated with the rise in overweight in developing countries [2], [12], [15], [33], [34], our data suggests that it will probably be the young children at the time of our study that are at greatest risk of overweight in adulthood from a NT related diet. Secondly, this rise in overweight may be slowed by childhood undernutrition. Interestingly, even after stratifying analysis into children and adults, the association between overweight and the diet indicative of the NT remained negative. It is possible that this association was not positive because the link between a NT diet and overweight has not had enough time to surface among children in our study. Further study to explore this notion and account for the negative association would be useful. Thirdly, it is concerning that if children are raised with a diet associated with the NT, then this diet pattern may continue into adulthood [36], thus increasing the risk of obesity and non-communicable disease even in the absence of overweight.
The rates of stunting in our study (32.3%, Table 2) were on par with the 36% national estimate in 2010 [1]. We observed an interesting positive correlation between energy/protein ratio and stunting status and negative correlation with the Plant-based diet component score (Table 4). Similar results were observed among Iranian children whereby a high carbohydrate-protein diet was negatively associated with stunting [37]. Because stunting was assessed among 3–19-year-olds in our study, these are not predictors of stunting as it is widely agreed that stunting is determined by height at two-years-old [38]. This is still concerning however, as children who are stunted require balanced meals and appropriate nutritional education to reverse the effects of stunting on growth [39] which would not be provided in a low energy, protein and/or Plant-based diet. It is also possible that stunted children in our study were malnourished as young children due to poverty that has not disappeared as they have aged thus showing association with the cheaper Plant-based diets in our study. This is concerning as whilst recently stunting prevention programs in Indonesia have received attention such as Scaling Up Nutrition (SUN), little research pertains to the treatment and recovery of stunted children, despite the need for nutritional interventions to stunted children into their adolescence [40]. Further research to address this question would be highly informative to stunting prevention and recovery interventions in Indonesia.
Our finding that stunting prevalence is high is consistent with other studies in rural areas [41], [42]. Whilst it has long been accepted that urban areas have higher prevalence of overweight than rural [42], the notion that this urban-rural gap is ‘closing’ [5] was supported by the observation that almost half of adults aged 20-64 years in our study were overweight (Figure 1). The diet patterns identified may reflect the fact that plant-based diets are predominant in rural areas of developing countries where food is self-grown [43], but the observation of the dietary pattern indicative of a nutrition transition is indicative of the fact that now not only urban, but rural areas are becoming exposed to these snacks/high fat content foods [35]. Whilst our results cannot ascertain this change in dietary patterns over time, they are indicative of these trends. In our study, the socio-economic status of participants was generally low, where there was great reliance on self-grown crops. Our findings should not be generalized to the rest of Indonesia due to the differences in socio-economic status and dietary patterns. It can be expected however, that similar observations would be found in other rural parts of Java.
The drawback of using a single 24-hour food recall is that it is an imperfect estimation of individual dietary patterns as well as energy/macronutrient intake as intra-individual variance is not accounted for. However, this does not pose a major issue to the analysis in this study as we were interested in looking at patterns across groups rather than at an individual level. By using a food-frequency questionnaire in conjunction with a single 24-hour food recall, we ensured that dietary data is drawn from both a broader time-dependent framework as well as a detailed recent recall. These techniques do not rely on expenditure as a proxy of food consumption which increases the internal reliability of our results. One drawback of the cross-sectional study design is that the temporal factor is not accounted for in analysis. This limits the ability to assess direction of causality in any of the associations we demonstrated. However, this paper aims to present a descriptive analysis of the ‘current state’ of malnutrition as opposed to test causal hypothesis. The observed prevalence of the household double burden of malnutrition in our study may be an underestimate due to the non-inclusion of children <3 years old, where stunting prevalence in this age group may be higher than in older children. Despite this, our sample size was sufficient to achieve statistical significance.
This study identified that the prevalence of the double burden of malnutrition remains high in rural Central Java. Overweight was most prevalent among women, whilst stunting affected young children. Household level double burden is common, with many households exhibiting a stunted child/overweight adult phenomenon. There is low but statistically significant correlation between a plant-based diet and stunting among children. Diets indicative of the NT are prevalent, but targeting young children. Nutrition policy and interventions should take into account the evidence that the shift to a western diet pattern may be impacting both underweight and overweight children. On top of this, nutrition interventions need to educate parents of young children about the risks associated with a NT diet pattern as these patterns once established may persist into adulthood.
5. Contributions
MK, DS, and DG conceptualized the study. JK developed and managed the database, and provided support for data collection tool development and activities. CL analysed the data and wrote the manuscript draft. HS and AR provided inputs into the analysis. MK, HS, AR, DG and CL edited the manuscript to produce the final copy. BL and SA provided administrative support in data collection. CL and MK verified the underlying data. All authors edited and reviewed the final manuscript.
Declaration of Competing Interest
All authors have no competing interests to declare.
Acknowledgments
Acknowledgements
The authors would like to thank all the Wonosobo residents who assisted us with this research, and particularly the village heads who dedicated their time and attention to this project amongst all their other responsibilities. We also thank the dedicated team of data collectors in Wonosobo. We acknowledge funding from the UBS-Optimus Foundation and the National Health and Medical Research Council
Data sharing
Data collected as part of this study are not publically available but can be shared upon reasonable request by emailing the corresponding author.
References
- 1.Shrimpton R, Rokx C. The Double Burden of Malnutrition: A Review of Global Evidence. 2012 https://documents.worldbank.org/en/publication/documents-reports/documentdetail/905651468339879888/the-double-burden-of-malnutrition-a-review-of-global-evidence Accessed 18 February 2020. [Google Scholar]
- 2.Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020;395(10217):65–74. doi: 10.1016/S0140-6736(19)32497-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neuman M, Kawachi I, Gortmaker S, Subramanian SV. Urban-rural differences in BMI in low- and middle-income countries: the role of socioeconomic status. Am J Clin Nutr. 2013;97(2):428–436. doi: 10.3945/ajcn.112.045997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kosaka S, Suda K, Gunawan B, Raksanagara A, Watanabe C, Umezaki M. Urban-rural difference in the determinants of dietary and energy intake patterns: A case study in West Java, Indonesia. PLoS One. 2018;13(5) doi: 10.1371/journal.pone.0197626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collaboration NCDRF. Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature. 2019;569(7755):260–264. doi: 10.1038/s41586-019-1171-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rachmi CN, Agho KE, Li M, Stunting Baur LA. Underweight and Overweight in Children Aged 2.0-4.9 Years in Indonesia: Prevalence Trends and Associated Risk Factors. PLoS One. 2016;11(5) doi: 10.1371/journal.pone.0154756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nkosinathi Vusizihlobo M, Sutayut O, Clarissa D. World Bank; Bangkok: 2019. Addressing the Double Burden of Malnutrition in ASEAN. https://openknowledge.worldbank.org/handle/10986/33142 Accessed 25 March 2021. [Google Scholar]
- 8.World Bank The Double Burden of Malnutrition in Indonesia. 2013 https://openknowledge.worldbank.org/handle/10986/17007 Accessed 15 March 2020. [Google Scholar]
- 9.Hanandita W, Tampubolon G. The double burden of malnutrition in Indonesia: Social determinants and geographical variations. SSM Popul Health. 2015;1:16–25. doi: 10.1016/j.ssmph.2015.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Doak CM, Adair LS, Bentley M, Monteiro C, Popkin BM. The dual burden household and the nutrition transition paradox. Int J Obes (Lond) 2005;29(1):129–136. doi: 10.1038/sj.ijo.0802824. [DOI] [PubMed] [Google Scholar]
- 11.Colozza D, Avendano M. Urbanisation, dietary change and traditional food practices in Indonesia: A longitudinal analysis. Soc Sci Med. 2019;233:103–112. doi: 10.1016/j.socscimed.2019.06.007. [DOI] [PubMed] [Google Scholar]
- 12.Roemling C, Qaim M. Obesity trends and determinants in Indonesia. Appetite. 2012;58(3):1005–1013. doi: 10.1016/j.appet.2012.02.053. [DOI] [PubMed] [Google Scholar]
- 13.Lipoeto NI, Wattanapenpaiboon N, Malik A, Wahlqvist ML. Nutrition transition in west Sumatra, Indonesia. Asia Pac J Clin Nutr. 2004;13(3):312–316. [PubMed] [Google Scholar]
- 14.Lienando AY, Lee S. Interrelationships of Multiple Forms of Transitions in Indonesia. Journal of Nutrition Education and Behavior. 2018;50(7):24–25. [Google Scholar]
- 15.Oddo VM, Maehara M, Rah JH. Overweight in Indonesia: an observational study of trends and risk factors among adults and children. BMJ Open. 2019;9(9) doi: 10.1136/bmjopen-2019-031198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freedman LS, Midthune D, Arab L, Prentice RL, Subar AF, Willett W. Combining a Food Frequency Questionnaire With 24-Hour Recalls to Increase the Precision of Estimation of Usual Dietary Intakes-Evidence From the Validation Studies Pooling Project. Am J Epidemiol. 2018;187(10):2227–2232. doi: 10.1093/aje/kwy126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lipoeto NI, Geok Lin K, Angeles-Agdeppa I. Food consumption patterns and nutrition transition in South-East Asia. Public Health Nutr. 2013;16(9):1637–1643. doi: 10.1017/S1368980012004569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shim JS, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health. 2014;36 doi: 10.4178/epih/e2014009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Consultation WHO . Vol. 363. 2004. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies; pp. 157–163. (Lancet). [DOI] [PubMed] [Google Scholar]
- 20.Nutrisurvey. [Computer software]. 2007. http://www.nutrisurvey.de/. Accessed 30 March 2020.
- 21.fatsecret 2020. https://www.fatsecret.co.id. Accessed 28 March 2020.
- 22.ANGKA KECUKUPAN GIZI YANG DIANJURKAN UNTUK MASYARAKAT INDONESIA Jakarta: MENTERI KESEHATAN REPUBLIK INDONESIA; 2019. http://hukor.kemkes.go.id/uploads/produk_hukum/PMK_No__28_Th_2019_ttg_Angka_Kecukupan_Gizi_Yang_Dianjurkan_Untuk_Masyarakat_Indonesia.pdf. Accessed 12 April 2020.
- 23.Tollosa DN, Van Camp J, Huybrechts I, Huybregts L, Van Loco J, De Smet S. Validity and Reproducibility of a Food Frequency Questionnaire for Dietary Factors Related to Colorectal Cancer. Nutrients. 2017;9(11) doi: 10.3390/nu9111257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.WHO . World Health Organization; Policy brief. Geneva: 2017. The double burden of malnutrition. http://apps.who.int/iris/bitstream/handle/10665/255413/WHO-NMH-NHD-17.3-eng.pdf?ua=1 Accessed 11 April 2021. [Google Scholar]
- 25.Fongar A, Godecke T, Qaim M. Various forms of double burden of malnutrition problems exist in rural Kenya. BMC Public Health. 2019;19(1):1543. doi: 10.1186/s12889-019-7882-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gerrior S, Juan W, Basiotis P. An easy approach to calculating estimated energy requirements. Prev Chronic Dis. 2006;3(4):A129. [PMC free article] [PubMed] [Google Scholar]
- 27.Angeles-Agdeppa I, Custodio MRS. Food Sources and Nutrient Intakes of Filipino Working Adults. Nutrients. 2020;12(4) doi: 10.3390/nu12041009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kornbrot D. Point Biserial Correlation. Wiley StatsRef: Statistics Reference Online.
- 29.Pujilestari CU, Nystrom L, Norberg M, Weinehall L, Hakimi M, Ng N. Socioeconomic inequality in abdominal obesity among older people in Purworejo District, Central Java, Indonesia - a decomposition analysis approach. Int J Equity Health. 2017;16(1):214. doi: 10.1186/s12939-017-0708-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Popkin BM, Conde W, Hou N, Monteiro C. Is There a Lag Globally in Overweight Trends for Children Compared with Adults? Obesity. 2006;14(10):1846–1853. doi: 10.1038/oby.2006.213. [DOI] [PubMed] [Google Scholar]
- 31.Roemling C, Qaim M. Dual burden households and intra-household nutritional inequality in Indonesia. Econ Hum Biol. 2013;11(4):563–573. doi: 10.1016/j.ehb.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 32.Oddo VM, Rah JH, Semba RD, Sun K, Akhter N, Sari M. Predictors of maternal and child double burden of malnutrition in rural Indonesia and Bangladesh. Am J Clin Nutr. 2012;95(4):951–958. doi: 10.3945/ajcn.111.026070. [DOI] [PubMed] [Google Scholar]
- 33.Jehn M, Brewis A. Paradoxical malnutrition in mother-child pairs: untangling the phenomenon of over- and under-nutrition in underdeveloped economies. Econ Hum Biol. 2009;7(1):28–35. doi: 10.1016/j.ehb.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 34.Popkin B, Adair L, Ng SW. NOW AND THEN: The Global Nutrition Transition: The Pandemic of Obesity in Developing Countries. Nutr Rev. 2012;70(1):3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vaezghasemi M. Umea University; Umea, Sweden: 2017. Nutrition transition and the double burden of malnutrition in Indonesia: a mixed method approach exploring social and contextual determinants of malnutrition.http://www.diva-portal.org/smash/get/diva2:1067919/FULLTEXT01.pdf [PhD Thesis]. Accessed 20 December 2020. [Google Scholar]
- 36.Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas. 2011;70(3):266–284. doi: 10.1016/j.maturitas.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 37.Esfarjani F, Roustaee R, Mohammadi-Nasrabadi F, Esmaillzadeh A. Major dietary patterns in relation to stunting among children in Tehran, Iran. J Health Popul Nutr. 2013;31(2):202–210. doi: 10.3329/jhpn.v31i2.16384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prendergast AJ, Humphrey JH. The stunting syndrome in developing countries. Paediatr Int Child Health. 2014;34(4):250–265. doi: 10.1179/2046905514Y.0000000158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bueno NB, Lisboa CB, Clemente AG, Antunes RT, Sawaya AL, Florencio TT. Effectiveness of a stunting recovery program for children treated in a specialized center. Pediatr Res. 2018;83(4):851–857. doi: 10.1038/pr.2017.321. [DOI] [PubMed] [Google Scholar]
- 40.Leroy JL, Frongillo EA. Perspective: What Does Stunting Really Mean? A Critical Review of the Evidence. Adv Nutr. 2019;10(2):196–204. doi: 10.1093/advances/nmy101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beal T, Tumilowicz A, Sutrisna A, Izwardy D, Neufeld LM. A review of child stunting determinants in Indonesia. Matern Child Nutr. 2018;14(4):e12617. doi: 10.1111/mcn.12617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Julia M, van Weissenbruch MM, de Waal HA, Surjono A. Influence of socioeconomic status on the prevalence of stunted growth and obesity in prepubertal Indonesian children. Food Nutr Bull. 2004;25(4):354–360. doi: 10.1177/156482650402500405. [DOI] [PubMed] [Google Scholar]
- 43.Solomons NW. Plant-based diets are traditional in developing countries: 21st century challenges for better nutrition and health. Asia Pac J Clin Nutr. 2000;9 Suppl 1:S41–S54. doi: 10.1046/j.1440-6047.2000.00165.x. [DOI] [PubMed] [Google Scholar]