Abstract
Objective
This review looks at novel combinations of topical agents (i.e., zinc gluconate, zinc oxide, dexpanthenol, and taurine) that target a combination of mechanisms in diaper dermatitis.
Methods
A literature search of published studies was conducted using the search terms “diaper dermatitis”, “treatment of diaper dermatitis in infants”, “treatment of diaper dermatitis in adults”, “nonsteroidal”, “nonantibiotic”, “antiinflammatory”, “moisturizer”, and “treatment for irritation”. A total of 207 related articles were screened, and those categorized as clinical trials and reviews were studied and compared. Articles with common themes were categorized, summarized, and presented herein.
Results
Diaper dermatitis, also referred to as diaper rash, napkin dermatitis, and nappy rash, is the most common skin eruption in infants and toddlers. In the last several years, there have been several technologic advances in diaper design to lessen the severity of diaper dermatitis symptoms. However, due to the unique environment of the diaper area, children and adults continue to have recurring symptoms of diaper dermatitis. Both commercially available products and certain home remedies are considered effective for managing sensitive and delicate skin in the diaper area. These topical agents create a protective barrier over the skin and reduce the impact of external irritants, which cause the reddening and burning sensation often associated with diaper dermatitis.
Conclusion
A range of therapeutic strategies for preventing and controlling diaper dermatitis are summarized in this manuscript.
Keywords: Zinc gluconate, Zinc oxide, Dexpanthenol, Taurine, Diaper dermatitis, Novel treatment
Introduction
Various etiologic factors have been identified and considered important in irritant diaper dermatitis (IDD), namely maceration, friction, and the presence of both urine and feces (Blume-Peytavi and Kanti, 2018). Because newborn skin exhibits cutaneous immaturity, there exists an increased susceptibility to skin barrier disruption or percutaneous absorption of irritants. Furthermore, the skin in the diaper area is predisposed to prolonged contact with urine and feces, as well as diaper occlusion, which leads to overhydration and alterations in skin pH. This milieu promotes damage to the structure of the stratum corneum, which directly contributes to the impaired barrier function. Prolonged exposure to urine and feces leads to a more alkaline pH in diapered skin, which results in changes in microbial colonization, activation of fecal protease and lipase enzymes, and stratum corneum impairment. Friction from wet diapers can lead to a breakdown of the skin barrier and increased cutaneous permeability to potential irritants or inflammatory triggers. These factors, which summarily may be referred to as the pathophysiologic quaternity of diaper dermatitis, are believed to contribute to the disease process in varying degrees (Fig. 1; Blume-Peytavi and Kanti, 2018).
Fig. 1.

Pathophysiologic quaternity of diaper dermatitis.
Concurrently, due to an aging population, a growing number of adult patients have incontinence associated dermatitis (IAD), which has much in common with the infant variant. Like IDD, moist occlusion leads to increased susceptibility for skin friction and increased skin hydration, as well as alkalization of skin pH, which strongly impair the barrier function of the stratum corneum. Eventually, fecal enzymes attack the skin, further adding to the damage. In addition to these changes, age-associated skin changes lead to a prolonged recovery of the epidermal barrier, the skin becomes prone to xerosis, and the surface pH shifts away from the protective acidic state. Additionally, overt malnutrition or micronutrient deficiencies, which are common in the aged population, may further restrict reparative responses to harmful stimuli (Beguin et al., 2010).
The aim of appropriate skin care practices to prevent IDD and IAD is to support skin barrier function, maintain appropriate dryness, reduce friction, and limit exposure to irritants. Therefore, to prevent IDD and IAD, the most recommended modalities are disposable, superabsorbent, and breathable diapers, frequent diaper changing, gentle cleansing, and the application of protective emollients and agents that promote the restoration of the natural and physical skin barriers (Beguin et al., 2010, Blume-Peytavi and Kanti, 2018).
Modern topical agents (e.g., corticosteroids and antimicrobials) are known to have potent and quick effects on symptoms of diaper dermatitis. However, the excessive, persistent, and irrational use of these agents have documented adverse effects (e.g., skin atrophy, pigmentary alterations, suppression of the hypothalamic–pituitary–adrenal axis, and bacterial resistance), which may preclude the positive effects of treatment (Sharifi-Heris et al., 2018a) Hence, novel approaches and combinations have been explored as a replacement for the usual options for this condition.
In this review, nonsteroidal, nonantibiotic topical agents with known therapeutic effects on diaper dermatitis are discussed. The pathophysiologic quaternity of diaper dermatitis is also proposed as an alternative approach to identify targets for treatment in this skin condition. In addition, the cosmetic properties of skin care products for diaper dermatitis prevention and management are reviewed and summarized.
Materials and methods
A literature search of published studies was conducted in MedLine and Google Scholar using the search terms “diaper dermatitis”, “treatment of diaper dermatitis in infants”, “treatment of diaper dermatitis in adults”, “nonsteroidal”, “nonantibiotic”, “antiinflammatory”, “barrier cream”, “repair cream”, “moisturizer”, “home remedy”, and “treatment for irritation”. A total of 207 related articles were screened, and those categorized as clinical trials and reviews were studied and compared as deemed appropriate.
Results and discussion
Facing unmet needs in diaper dermatitis care
The management of IDD and IAD is based on two major objectives: acceleration of healing of damaged skin and prevention of recurring diaper dermatitis. Preventive management of IDD and IAD relies on knowledge of its etiology and elimination of causative factors (Blume-Peytavi and Kanti. 2018). Unfortunately, although most commonly available treatments have individually been shown to provide some relief, they have yet to demonstrate full restoration of normal barrier function. Overcoming limitations in choosing the safest, most effective, and cost-efficient type of treatment remains challenging (Sharifi-Heris et al., 2018a).
Common limitations of clinical evaluation studies in IDD and IAD therapy include inconsistent description of clinical characteristics and a lack of correlation between these characteristics and the condition of diapered skin. Also, many studies have focused solely on the efficacy of interventions with no understanding of the link between symptom severity and contributing risk factors (Esser and Johnson, 2020). Variable quality among the different clinical studies that evaluate the efficacy of these interventions is known to exist (Burdall et al., 2019). Hence, more prospective studies evaluating the mechanism and clinical effects of therapeutic options for diaper dermatitis are needed. Herein, we review the most used components of topical skincare products for IDD and IAD.
Clinical evaluation of novel creams and solutions for diaper dermatitis
The studies reviewed identified agents frequently identified as topical agents used as repair and/or barrier creams, some with anti-inflammatory components. Among these products are zinc salts (i.e., zinc gluconate and zinc oxide), dexpanthenol, taurine, botanicals/traditional medicines, and petrolatum hydrogel barrier/repair creams or ointments. Studies evaluating the clinical benefits of these agents are highlighted.
Zinc salts
The oxide salt of zinc has nearly zero solubility in water and has a mild anti-inflammatory, anti-irritant, regenerative, and moisturizing effect (Sharifi-Heris et al., 2018a). Topical zinc oxide has been found to have strong antioxidant and antibacterial properties (Gupta et al., 2014). There have been 17 studies on the antimicrobial properties of zinc oxide, which has shown effective antibacterial properties against Streptococcus mutans (Almoudi et al., 2018). Additionally, zinc oxide-based ointments act as a physical barrier to water absorption and reduces bacterial infections in mild dermatitis by inhibiting the adhesion and penetration of microorganisms. More importantly, no serious side effects have been reported in many decades of use.
Zinc oxide ointment 5% can be used to reduce the symptoms of diarrhea-induced diaper dermatitis. This barrier agent has antiperspirant properties in the diaper area, in combination with potassium, and is used as a topical treatment for dermatitis in children in combination with glycerin. The effects are most appreciated if zinc oxide is applied after each diaper change.
Reports of low doses of systemic zinc gluconate have been previously evaluated for treatment of inflammatory acne (Dreno et al., 1989), with clinical response attributed to the antimicrobial and anti-inflammatory effects of zinc.
Topical D-panthenol (dexpanthenol)
Topical dexpanthenol, the D enantiomer of panthenol, has moisturizer-like properties that are attributed to its hygroscopic nature. This ingredient acts as a humectant, but the full mechanism of action has not been well elucidated. Studies have evaluated dexpanthenol formulas in two different lipophilic vehicles on the epidermal barrier function in vivo. When used for 7 days, these topicals improved stratum corneum hydration and reduced transepidermal water loss (Ebner et al., 2002).
Taurine
Taurine in topical products has also been shown to provide additional protection against oxidative stress associated with various inflammatory diseases. Topical taurine significantly stimulates the synthesis of all three classes of barrier lipids (ceramides, cholesterol, and fatty acids) in reconstructed epidermis. This suggests that taurine helps prevent surfactant-induced dry and scaly skin by modulating the proinflammatory response and stimulating epidermal lipid synthesis (Anderheggen et al., 2006).
In vitro studies have shown how taurine accumulation in cultured keratinocytes protected these cells from both osmotically induced and ultraviolet-induced apoptosis. This protective action is probably due to taurine’s epidermal osmolyte properties that maintain keratinocyte hydration in a dry environment (Janeke et al., 2003). Other studies have highlighted its potential antioxidant and anti-inflammatory properties in vivo (i.e., gingival epithelium studies; Gültekin et al., 2012) and in clinical studies (i.e., rheumatoid arthritis; Marcinkiewicz and Kontny, 2014).
Plant-derived remedies
Medicinal plants have been used in folk medicine since prehistoric times. These botanicals have been found to possess antimicrobial and anti-inflammatory properties (Panahi et al., 2012). Home remedies derived from plants that have been evaluated in clinical trials to treat diaper rash include aloe vera, Calendula officinalis (marigold), and Olea europaea (source of olive oil), and their effectiveness is most likely attributed to their soothing properties on the skin or the barrier effects of the natural oils (Mahmoudi et al., 2015, Panahi et al., 2012, Sharifi-Heris et al., 2018b). Other traditional remedies include extracts from Malus domestica (apple cider vinegar from apples), Lawsonia inermis (henna), and citrus fruits (citric acid), which may have antimicrobial or antifungal effects due to tannins or organic acids (Keshavarz et al., 2016, Lavender et al., 2012, Mota et al., 2015). An evaluation of C. officinalis versus topical aloe vera showed that, although both botanicals reduced the severity of diaper dermatitis, C. officinalis was superior to aloe in terms of reducing the rash sites (Panahi et al., 2012). Infants and children treated with henna had a greater rate of improvement compared with hydrocortisone, which is likely due to the anti-inflammatory and antimicrobial properties of henna (Keshavarz et al., 2016).
Petrolatum-based barriers/creams
The preventive barrier effects of petrolatum jelly and petrolatum-based formulations delivered by a disposable diaper have been evaluated in clinical studies. Continuous dosimetric topical application from the diaper was shown to significantly improve skin roughness and to reduce erythema and diaper dermatitis severity (Odio et al., 2000a, Odio et al., 2000b). By itself, petrolatum jelly lowered the incidence of diaper rash, but not significantly compared with the control group (Alonso et al., 2013).
Combination agents
The clinical benefit of combination barrier creams (zinc oxide), repair creams (dexpanthenol) enriched with anti-inflammatory properties (from taurine), and antimicrobial properties (from zinc gluconate) as effective treatments in diaper dermatitis has come to light in recent years. A formulation combining these agents has been evaluated and shown to have good dermoprotective efficacy (Eurofins, 2017c), erythema-reducing properties (Cavalli and Cimaz, 2013), and good cosmetic acceptability (Eurofins, 2017c).
Limited clinical studies by an independent dermatologic laboratory in Europe evaluated a range of skincare products from RELIFE S.R.L. Relizema baby care cream, composed of zinc gluconate, taurine, dexpanthenol, zinc oxide, and almond oil, as well as Relizema spray and go, composed of zinc gluconate, taurine, dexpanthenol, and zinc oxide, were applied to treat diaper dermatitis in 20 infants and toddlers in separate trials (Eurofins, 2017a, Eurofins, 2017b). Test subjects were Italian infants and children age 3 to 36 months, with skin Fitzpatrick skin type I, II, III, or IV with slight skin irritation on the diaper area as determined by a board-certified dermatologist and pediatrician. These studies confirmed the efficacy of both devices in reducing skin erythema in the diaper area after 2 and 4 weeks of use (Fig. 2; Eurofins, 2017a, Eurofins, 2017b). In addition, the users (i.e., parents or guardians of the subjects) shared subjective ratings on the ease of application (100%), pleasant smell (95%), and other cosmetic parameters (Table 1). Overall, the products were rated high for their cosmetic qualities and efficacy (Eurofins, 2017a, Eurofins, 2017b). This study was limited by its quasi-experimental design (i.e., nonrandomized, no control) because the study was performed on a topical nonpharmaceutical device for the purpose of market approval. Robust studies are recommended to understand the clinical effects of Relizema baby cream and spray and go in infants and children with confirmed diagnosis of diaper dermatitis.
Fig. 2.
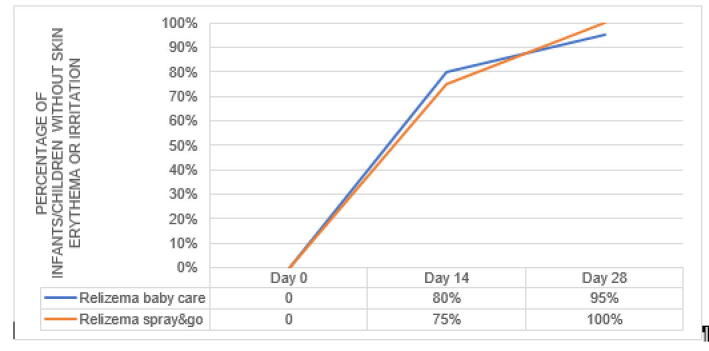
Efficacy of Relizema baby care and Relizema spray and go in the reduction of skin erythema in infants and toddlers with diaper dermatitis after 2 weeks of treatment. The studies confirmed the products’ efficacy with very good skin acceptability after application of both products at every diaper change for 28 consecutive days ± 2 days in infants and toddlers age 3 to 36 months with slight skin irritation of the nappy area. The pediatrician examined the treated zone (at the beginning of the study and after 2 and 4 weeks).
Table 1.
Ratings on parameters of cosmetic acceptability, rate 2 and 3 on 0–3 scale (3 being the highest level of agreement) after 28 days of product use.
| Items rated | Subjects satisfied with baby care cream, % | Subjects satisfied with spray and go, % |
|---|---|---|
| Moisturizing efficacy | 100 | 100 |
| Softening effects on skin | 100 | 100 |
| Ease of application | 100 | 100 |
| Pleasant smell | 95 | 95 |
| Would you recommend this product to friends or family? | 100 | 100 |
Conclusions and recommendations
The tested topical skin barrier and repair skincare products with the combination of zinc gluconate, taurine, panthenol, and zinc oxide are clinically proven to have good acceptability and efficacy in reducing skin erythema and irritation of the nappy area. In combination with other effective options for care, such as super-absorbent diapers and the potentially beneficial diaper-free time, the use of these agents may provide an effective treatment for nappy rash or diaper dermatitis (Burdall et al., 2019). Commercially available products have been shown to relieve and prevent irritation in the diaper area by forming a protective film against external irritants and providing additional humectant and antioxidant protection for both children and adults with diaper dermatitis. More prospective, controlled studies in synergy with objective diagnostic tools evaluating the signs and symptoms of diaper dermatitis could provide invaluable insights in the effective management of diaper dermatitis in the near future.
Conflicts of interest
Dr. Hebert has served as a consultant and speaker for RELIFE. She has received honoraria for those activities.
Funding
RELIFE S.r.l. provided an unrestricted educational grant in support of this manuscript.
Study approval
The author(s) confirm that any aspect of the work covered in this manuscript that has involved human patients has been conducted with the ethical approval of all relevant bodies.
References
- Almoudi M.M., Hussein A.S., Abu Hassan M.I., Mohamad Zain N. A systematic review on antibacterial activity of zinc against Streptococcus mutans. Saudi Dent J. 2018;30(4):283–291. doi: 10.1016/j.sdentj.2018.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alonso C., Larburu I., Bon E., González M.M., Iglesias M.T., Urreta I., Emparanza J.I. Efficacy of petrolatum jelly for the prevention of diaper rash: A randomized clinical trial. J Spec Pediatr Nurs. 2013;18(2):123–132. doi: 10.1111/jspn.12022. [DOI] [PubMed] [Google Scholar]
- Anderheggen B., Jassoy C., Waldmann-Laue M., Förster T., Wadle A., Doering T. Taurine improves epidermal barrier properties stressed by surfactants - A role for osmolytes in barrier homeostasis. J Cosmet Sci. 2006;57(1):1–10. [PubMed] [Google Scholar]
- Beguin A.M., Malaquin-Pavan E., Guihaire C., Hallet-Lezy A.M., Souchon S., Homann V. Improving diaper design to address incontinence associated dermatitis. BMC Geriatr. 2010;10(1):86. doi: 10.1186/1471-2318-10-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blume-Peytavi U., Kanti V. Prevention and treatment of diaper dermatitis. Pediatr Dermatol. 2018;35:s19–s23. doi: 10.1111/pde.13495. [DOI] [PubMed] [Google Scholar]
- Burdall O., Willgress L., Goad N. Neonatal skin care: developments in care to maintain neonatal barrier function and prevention of diaper dermatitis. Pediatr Dermatol. 2019;36(1):31–35. doi: 10.1111/pde.13714. [DOI] [PubMed] [Google Scholar]
- Cavalli G, Cimaz R. Relizema baby cream open label to evaluate tolerability and acceptability in diaper rash. 12th World Congress of Paediatric Dermatology, Madrid, Spain; October 2013.
- Dreno B., Amblard P., Agache P., Sirot S., Litoux P. Low doses of zinc gluconate for inflammatory acne. Acta Derm Venereol. 1989;69(6):541–543. [PubMed] [Google Scholar]
- Ebner F., Heller A., Rippke F., Tausch I. Topical use of dexpanthenol in skin disorders. Am J Clin Dermatol. 2002;3(6):427–433. doi: 10.2165/00128071-200203060-00005. [DOI] [PubMed] [Google Scholar]
- Esser M.S., Johnson T.S. An integrative review of clinical characteristics of infants with diaper dermatitis. Adv Neonatal Care. 2020;20(4):276–285. doi: 10.1097/ANC.0000000000000682. [DOI] [PubMed] [Google Scholar]
- Eurofins. Human in use test under paediatric control - Study report, version number 1 of 14/07/2017 - Study reference 17-070; 2017.
- Eurofins. Human in use test under paediatric control - Study report, version number 1 of 23/10/2017 - Study reference 17-015A; 2017.
- Eurofins. Instrumental assessment of the dermo-protective efficacy- Study report, version number 1 of 13/03/2017 - Study Reference 17-015B; 2017.
- Gültekin S.E., Sengüven B., Sofuoğlu A., Taner L., Koch M. Effect of the topical use of the antioxidant taurine on the two basement membrane proteins of regenerating oral gingival epithelium. J Periodontol. 2012;83(1):127–134. doi: 10.1902/jop.2011.100568. [DOI] [PubMed] [Google Scholar]
- Gupta M., Mahajan V.K., Mehta K.S., Chauhan P.S. Zinc therapy in dermatology: A review. Dermatol Res Pract. 2014;2014 doi: 10.1155/2014/709152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janeke G., Siefken W., Carstensen S., Springmann G., Bleck O., Steinhart H. Role of taurine accumulation in keratinocyte hydration. J Invest Dermatol. 2003;121(2):354–361. doi: 10.1046/j.1523-1747.2003.12366.x. [DOI] [PubMed] [Google Scholar]
- Keshavarz A., Zeinaloo A.A., Mahram M., Mohammadi N., Sadeghpour O., Maleki M.R. Efficacy of traditional medicine product henna and hydrocortisone on diaper dermatitis in infants. Iran Red Crescent Med J. 2016;18(5) doi: 10.5812/ircmj.24809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavender T., Furber C., Campbell M., Victor S., Roberts I., Bedwell C. Effect on skin hydration of using baby wipes to clean the napkin area of newborn babies: Assessor-blinded randomised controlled equivalence trial. BMC Pediatr. 2012;12:59. doi: 10.1186/1471-2431-12-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmoudi M., Adib-Hajbaghery M., Mashaiekhi M. Comparing the effects of Bentonite & Calendula on the improvement of infantile diaper dermatitis: A randomized controlled trial. Indian J Med Res. 2015;142(6):742–746. doi: 10.4103/0971-5916.174567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcinkiewicz J., Kontny E. Taurine and inflammatory diseases. Amino Acids. 2014;46(1):7–20. doi: 10.1007/s00726-012-1361-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mota A.C.L.G., de Castro R.D., de Araújo Oliveira J., de Oliveira Lima E. Antifungal activity of apple cider vinegar on candida species involved in denture stomatitis. J Prosthodont. 2015;24(4):296–302. doi: 10.1111/jopr.12207. [DOI] [PubMed] [Google Scholar]
- Odio M.R., O’Connor R.J., Sarbaugh F., Baldwin S. Continuous topical administration of a petrolatum formulation by a novel disposable diaper. 1. Effect on skin surface microtopography. Dermatology. 2000;200(3):232–237. doi: 10.1159/000018365. [DOI] [PubMed] [Google Scholar]
- Odio M.R., O’Connor R.J., Sarbaugh F., Baldwin S. Continuous topical administration of a petrolatum formulation by a novel disposable diaper. 2. Effect on skin condition. Dermatology. 2000;200(3):238–243. doi: 10.1159/000018366. [DOI] [PubMed] [Google Scholar]
- Panahi Y., Sharif M.R., Sharif A., Beiraghdar F., Zahiri Z., Amirchoopani G. A randomized comparative trial on the therapeutic efficacy of topical aloe vera and Calendula officinalis on diaper dermatitis in children. ScientificWorldJournal. 2012;2012 doi: 10.1100/2012/810234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharifi-Heris Z., Amiri Farahani L., Hasanpoor-Azghadi S.B. A review study of diaper rash dermatitis treatments. J Client-centered Nurs Care. 2018;4(1):1–12. [Google Scholar]
- Sharifi-Heris Z., Farahani L.A., Haghani H., Abdoli-Oskouee S., Hasanpoor-Azghady S.B. Comparison the effects of topical application of olive and calendula ointments on children’s diaper dermatitis: A triple-blind randomized clinical trial. Dermatol Ther. 2018;31(6):e12731. doi: 10.1111/dth.12731. [DOI] [PubMed] [Google Scholar]


