Abstract
Objective:
This study evaluates the personal and professional experiences of physician mothers during the coronavirus disease 2019 (COVID-19) pandemic and the impact of the pandemic on the lives of physician mothers.
Methods:
Using social media to reach a broad range of physicians, a convenience sample of physician mothers completed an on-line survey posted between April 27 and May 11. Members were encouraged to repost on social media and share with personal contacts resulting in a passive snowball sampling effect.
Results:
A total of 2709 physician mothers from 48 states, Puerto Rico, and 19 countries representing more than 25 medical specialties completed the survey. Most were between 30 and 39 y of age, 67% self-identified as white, 17% as Asian, 4% as African American. Most had been working for 11-16 y. A total of 91% had a spouse/partner of the opposite sex. Over half were practicing in an area they identified as high COVID-19 density, while 50% had personally cared for a person with COVID-19. Physician mothers were most concerned about exposing their children to COVID-19 and about the morale and safety of their staff.
Conclusions:
This is one of the first studies to explore the personal and professional challenges facing physician mothers during a pandemic. Physician mothers were most concerned about exposing their families to COVID-19. Mothers continued to work and at times increased their work, despite having domestic, childcare, and schooling responsibilities.
Keywords: physician moms, COVID-19 pandemic, impact
The face of medicine is changing. Women comprise the majority of medical school applicants and matriculants.1 Of those women, 80% are expected to become mothers.2 These mothers may experience unique stressors and have been shown to be more dissatisfied with their work-life balance.3 They are at higher risk for work-family conflict than their male counterparts and men and women in other careers.3,4 Finding childcare for an average work-week of 51 h and sometimes up to 80 h,5 balancing home responsibilities with after-hours administrative work, and limited control over work schedules all contribute to maternal frustration.6 Physician mothers tackle the daily responsibilities of being both a physician and a mother while pregnant, nursing, and performing the majority of household and familial roles, including childcare.7 One study found that women physicians spent nearly 9 h/wk more on domestic duties than their male counterparts and were responsible for childcare duties when usual childcare arrangements were disrupted.8
During previous pandemics, research found that health-care workers (HCWs) had many personal and professional concerns. Devnani performed an integrative review featuring 32 articles on factors associated with the willingness of health-care workers to work during an influenza emergency and found many personal and professional concerns.9 During a pandemic, HCWs were willing to stay at work but concern for their families was a barrier to working.10-20 These studies did not focus on women HCWs. In a few studies, women HCW were found less likely to work during a pandemic and parents were also less likely to report to work than individuals without care responsibilities.16,21 Much of the previous research, however, focused on nonphysician health-care workers. There is little research focused on physician mothers.
In this study, we surveyed physician mothers to determine the personal and professional impact of the coronavirus disease 2019 (COVID-19) pandemic. By describing the experiences of physician mothers both at home and in the workplace, this study provides insights into the personal and professional experiences of physician mothers during the COVID-19 pandemic and the impact of the pandemic on the lives of physician mothers as this unprecedented event changes how physicians treat their patients while simultaneously caring for their families.
Methods
A primarily quantitative on-line survey was developed to determine the impact of the COVID-19 pandemic on women physicians who self-identify as physician mothers and/or are members of Physician Moms Group on Facebook. Social media platforms, such as Facebook, offer a rich source of global information with nearly 2.2 billion monthly active users, 43% of whom are women.22 Facebook surveys have previously been used to understand physician mothers’ professional and personal responsibilities.23 Survey development was informed by the literature, review of surveys related to HCW stresses and experiences during pandemics, and by the personal experience of practicing physician mothers from several specialties (emergency medicine [EM], internal medicine [IM], and infectious diseases [ID]). The survey evaluated numerous factors impacting the personal and professional lives of physicians during the pandemic including the role of specialty, status, and familial and professional responsibilities, as well as whether participants prepared personally and/or professionally for the pandemic. There were 44 primarily multiple-choice questions and 3 open-ended questions; quantitative data are reported here.
Face validity of the survey was examined by 7 experts from 2 academic medical centers: Wayne State University in Detroit, Michigan, and the Mayo Clinic in Scottsdale, Arizona. All experts were physicians with experience in research and survey methodology. A usability survey was then sent to 12 physicians from different specialties in different locations (Michigan, Alabama, Georgia, and Canada) to determine survey usability and quality with resultant minor changes to the survey instrument. The final survey instrument comprised 3 sections addressing the personal impact of COVID-19, the professional impact of COVID-19, and demographic information.
The study was a convenience sample with passive snowball sampling. To reach a broad community of physician mothers we used the Facebook group “Physicians Moms Group” (PMG), a highly active group with over 70,000 members, as well as social media (including Twitter and LinkedIn). A post was made on the PMG Facebook group which included a link to access the information sheet and the survey. The survey was initially posted to PMG on April 27, 2020. Study authors also recruited participants from their personal social media accounts and through personal and professional email contacts, including Twitter and LinkedIn. All recruited participants could also share the study with other potential participants. The survey remained open from April 27 through May 11, 2020. The survey was presented using the Qualtrics (Provo, UT) online platform. Repeat submissions to the survey by a single user were limited by Internet Protocol (IP) address. The Wayne State University Institutional Review Board reviewed the protocol and deemed it exempt. Primary endpoints were understanding how the pandemic affected physician mothers’ professional, personal, and family life. Inclusion criteria were self-selected physician mothers over the age of 18 and currently pregnant with a first child or parenting at least 1 child. In 2016, there were over 319,000 female physicians in the United States; it is estimated 2/3 were mothers.24 To obtain a representative sample, we aimed for a sample size of 1% or approximately 2000 responses for a more inclusive representation.
Statistical Analysis
Statistical analysis was conducted using IBM SPSS® Statistics, Version 26.0 (Armonk, NY: IBM Corp.). Bivariate analysis was performed to examine the differences in the effect of COVID-19 pandemic, particularly the differences in personal and professional concerns, across the different physician mom groups. Categorical variables were compared using χ2 and Fischer’s exact tests using 2 × 2 tables. For the sake of conducting 2 × 2 tables, the results from questions using the Likert scale—Strongly disagree, Disagree, Neither agree nor disagree, Agree, Strongly agree—were collapsed to result in 2 final categories: “Disagree/Neither agree nor disagree” and “Agree.” All significance tests were 2-sided and used a 5% level of significance.
Results
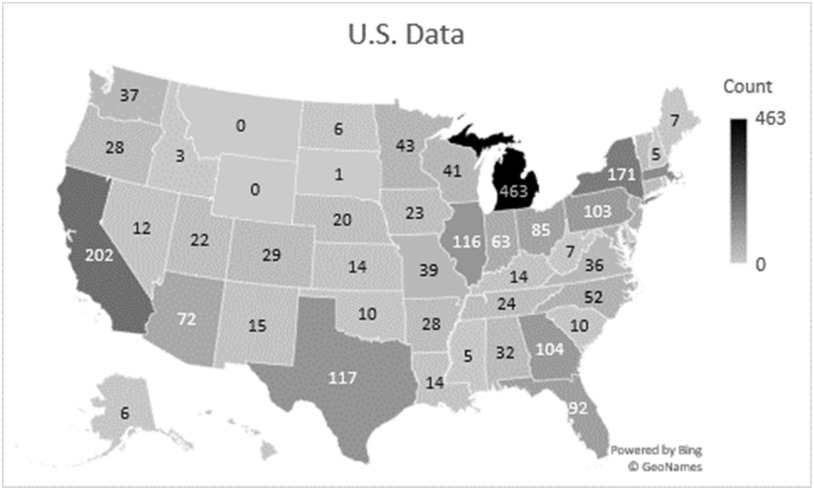
There were a total of 3522 unique responses. Partially completed surveys (n = 178) or surveys opened but not advanced beyond the first page (n = 635) were excluded. Responses were received from 20 countries with the United States contributing 93% of responses. Of those outside of the United States, the largest number of responses were from 3 countries, Finland (50), Japan (42), and Canada (40), making up approximately 70% of the non-US response total. All states were represented except Montana and Wyoming; US data are shown in Figure 1. Figures 2 and 3 represents international data. Demographic information is reported in Table 1. The majority of respondents were 30-39 y old (45%), 11-15 y post residency (30%), white (67%), married to a partner of the opposite sex (91%), and had elementary-school aged children (48%). Twenty-four percent had a spouse with a high-risk job (eg, firefighter, emergency medical technician, etc.), and 32% had a spouse who was also a physician.
Figure 1.
Distribution of responses by state
Figure 2.

Distribution of responses by continent
Figure 3.
Distribution of responses by geographic location
Table 1.
Characteristics of respondersa
| Demographics and characteristics | Total number N = 2709 | % |
|---|---|---|
| Age (range, y) | 2706 | |
| 24-29 | 31 | 1% |
| 30-39 | 1207 | 45% |
| 40-49 | 1117 | 41% |
| 50-59 | 283 | 10% |
| 60 and above | 67 | 2% |
| Time since graduation from medical school (range, y) | 2694 | |
| Less than 5 | 154 | 6% |
| 6-10 | 647 | 24% |
| 11-15 | 823 | 31% |
| 16-20 | 569 | 21% |
| More than 20 | 496 | 18% |
| Race /ethnicity | 2709 | |
| Asian | 471 | 17% |
| Black or African American | 104 | 4% |
| White | 1824 | 67% |
| Hispanic or Latina | 89 | 3% |
| Other | 205 | 8% |
| Current relationship status | 2705 | |
| Single | 56 | 2% |
| Married/partner – opposite sex | 2455 | 91% |
| Married/partner- same sex | 71 | 3% |
| Divorced/Separated | 106 | 4% |
| Widowed | 6 | 0% |
| Other | 10 | 0% |
| Physician moms with spouses/partners working in high risk jobs | 2542 | |
| Spouses/partners with high-risk jobs (eg, firefighter, EMT, police, etc.) | 663 | 26% |
| Spouses/partners who are physicians | 864 | 34% |
| Mothers with children at home | 4334 | |
| Infants and babies < than 2 y old | 648 | 15% |
| Children 2 y old through preschool | 1147 | 26% |
| Elementary-school-aged children | 1295 | 30% |
| Middle-school aged children | 508 | 12% |
| High-school-aged children | 369 | 9% |
| College-aged children | 194 | 4% |
| Children with special needs | 74 | 2% |
| Medical specialty | 2671 | |
| IM | 571 | 21% |
| Primary care | 263 | 10% |
| Hospitalist | 191 | 7% |
| ID | 76 | 3% |
| Pulmonary-critical care | 41 | 2% |
| Pediatrics | 357 | 13% |
| Primary care | 254 | 10% |
| OBGYN | 260 | 10% |
| Family medicine | 255 | 10% |
| EM | 194 | 7% |
Only specialties with > 7% of survey total are represented in this table.
Respondents were queried regarding how they personally prepared for the pandemic; results are reported in Table 2. For the physician mothers who did take steps to prepare, the most common ways they prepared were ensuring their families had adequate food (73%), cleaning supplies (57%), and medications (54%). A small percent (7%) reported that they did not personally prepare for the COVID-19 pandemic. As for the measures taken to prepare professionally, nearly all focused on self-education, including educating themselves about COVID-19, pandemics (64%), and critical care medicine (eg, ventilator management) (33%). Nearly a third (32%) ordered additional personal protective equipment (PPE) for their clinical site. Nearly all physician mothers (98%) continued to work. Of those, 18% increased their work hours, including 12% who voluntarily increased hours. Physician mothers modified their work, with 55% of respondents providing telehealth visits and 28% limited in-person patient contact. Of women with school-aged children, around half (46%) did not have to change their work schedule. Slightly more than a third did the same amount of work but shifted to working from home (38%); 9% worked entirely from home. Fewer women decreased the amount of work with only 15% cutting back on hours.
Table 2.
Ways physician mothers prepared
| How did you personally prepare | Count | % |
|---|---|---|
| Made sure we had adequate food | 1981 | 73% |
| Made sure we had cleaning supplies | 1548 | 57% |
| Made sure we had medications | 1469 | 54% |
| Made sure we had adequate toilet paper | 1394 | 51% |
| Developed a plan for child/family care | 1255 | 46% |
| Made sure we were financially prepared with emergency funds | 1119 | 41% |
| Obtained PPE for myself | 1028 | 38% |
| Obtained PPE for family | 869 | 32% |
| Made sure I had adequate feminine hygiene products | 631 | 23% |
| Made sure we had plenty of bottled water | 623 | 23% |
| Updated my/our will | 412 | 15% |
| I did not prepare | 308 | 11% |
| Made sure we had adequate baby formula | 201 | 7% |
| Other | 154 | 6% |
| How did you professionally prepare | ||
| Educated self about COVID | 2555 | 94% |
| Educated self about pandemics | 1734 | 64% |
| Reviewed critical care medicine (eg, ventilator management) | 892 | 33% |
| Ordered additional PPE for clinical site | 875 | 32% |
| Attended disaster training | 366 | 14% |
| Arranged disaster/preparedness training for employees | 362 | 13% |
| Other | 236 | 9% |
Comparing personal concerns among physician mothers who personally prepared for the pandemic with those who did not, the most commonly listed concern among both groups was exposing their children to COVID-19 with no statistical difference between these groups for this top concern (51% vs 50%; odds ratio [OR], 0.98; P = 0.78) (Table 3). Mothers who had personally prepared were significantly more likely to be concerned about disrupted family life (30% vs 23%; OR, 0.71; P < 0.001), schooling children from home (29% vs 23%; OR, 0.76; P = 0.002), and financial hardship (23% vs 18.5%; OR, 0.77; P = 0.007). Looking at professional concerns, mothers who had not personally prepared were more likely to be concerned about lack of PPE for self (44% vs 39%; OR, 0.83; P = 0.01) and health of the department (13% vs 10%; OR, 0.74; P = 0.02). On the other hand, those who had not personally prepared were less likely to be concerned about making appropriate policies (32% vs 36%; OR 1.2; P = 0.03). Among both personally prepared and unprepared mothers, the most commonly listed professional concern was staff morale.
Table 3.
Bivariate analysis comparing personal and professional concerns among physician moms who were personally and professionally not prepared versus physician moms who were (personally or professionally) prepared
| Personally non-prepared | Personally prepared | |||||
|---|---|---|---|---|---|---|
| Variables | N1 = 1645 | (%) | N2 = 1064 | % | OR | P-value |
| Biggest personal concerns during the COVID 19 pandemic | ||||||
| Exposing my children to COVID | 834 | 51% | 532 | 50% | 0.98 | 0.78 |
| Disrupted family life | 492 | 30% | 247 | 23% | 0.71 | <0.001 |
| Schooling children from home | 474 | 29% | 249 | 23% | 0.76 | 0.002 |
| Childcare | 410 | 25% | 189 | 18% | 0.65 | <0.001 |
| Financial hardship | 375 | 23% | 196 | 18% | 0.77 | 0.007 |
| Biggest professional concerns during the COVID 19 pandemic | ||||||
| Morale of staff | 729 | 44% | 445 | 42% | 0.9 | 0.2 |
| Not enough PPE for self | 717 | 44% | 415 | 39% | 0.83 | 0.01 |
| Financial challenges | 706 | 43% | 406 | 38% | 0.82 | 0.01 |
| Making appropriate policies | 523 | 32% | 381 | 36% | 1.2 | 0.03 |
| Health of department | 218 | 13% | 108 | 10% | 0.74 | 0.02 |
Comparing professional concerns among physician mothers who considered themselves professionally prepared for the pandemic versus mothers who were not professionally prepared, exposing one’s children to COVID-19 again emerged as the most frequent concern (52% vs 48%; OR, 0.85; P = 0.045), although exposing one’s children was significantly more of a concern to those women who considered themselves professionally prepared (Table 3). Additionally, mothers who had professionally prepared for the pandemic were less likely to be concerned about dying from COVID-19 (44% vs 37%; OR, 0.75; P = 0.001) or financial hardship (23% vs 18%; OR, 0.76; P = 0.006). The professionally unprepared were most concerned about lack of PPE for themselves, co-workers, and staff.
Looking at physician mothers practicing in a self-identified high-density COVID-19 area compared with those practicing in low density area revealed no differences in the most common concerns; both groups identified exposing children to COVID-19 and exposing parents as their top concerns. Similarly, there was no difference in professional concerns. Both groups were most concerned about morale of the staff along with concerns for PPE. Physician mothers who were personally caring for COVID-19 patients at the time of the survey had more concerns over exposing their children and spouse/partner to COVID-19, morale of the staff, and having enough physicians to care for patients than mothers who were not personally involved in the care of COVID-19 patients.
For all participants, when asked about their career choices, a small percentage of mothers (10%) wished they had not gone into medicine as a consequence of the pandemic, with 5% wishing they had not gone into their specialty. Front-line physicians including EM physicians, anesthesiologists, and internists were overrepresented in those wishing they had not gone into their specialty.
School cancelations impacted childcare. Most women used multiple means to secure care for their children. While 21% of women already had childcare in the home, 16% hired someone to provide care. Partners were already providing care in approximately 10% of families. At the time of the survey, 10% of mothers were still struggling to find childcare. Both mothers and partners adjusted schedules equally.
Over 90% of women were responsible in some way for helping their children with assigned homework. Approximately 40% were entirely or primarily responsible and 51% were partially responsible for helping with assigned homework. During the pandemic, 12% found their children’s behavior to be moderately to much better, while 29% found behavior to be moderately or much worse.
Before the pandemic, 41% of women unequally shared domestic obligations and were responsible for more than half of the domestic duties. Another 46% equally shared duties. Only 13% of women provided less than half of the domestic duties. During the pandemic, these numbers remained relatively unchanged, with 39% unequally sharing domestic duties, 44% equally sharing domestic duties, and 17% with others doing less than half of duties, a 4% absolute change from before the pandemic. When duties were unequally shared, women were greater than 3 times more likely to do more domestic duties than others. During the pandemic, women were twice as likely to do the majority of domestic duties.
More mothers were satisfied with the amount of time they spent with their family during the pandemic compared with before the pandemic and felt less guilt about not spending time with their family during the pandemic (Table 4). Approximately half of the time, women noted a worsening in the balance between professional and personal responsibilities. If the balance changed from baseline, it was more likely to worsen than improve. From a personal standpoint, the pandemic disrupted social activity for nearly everyone (94%), and sleep was disrupted in more than half of the respondents
Table 4.
Physician mother responses during COVID-19 pandemic
| Before the pandemic | Mean (SD) | During the pandemic | Mean (SD) | P-Value | |
|---|---|---|---|---|---|
| I am satisfied with the amount of time I spent with my family | 2.06 | 1.1 | 2.58 | 1.17 | <0.001 |
| Infants & pre-school-aged children | 2.04 | 1.11 | 2.65 | 1.16 | <0.001 |
| Elementary school-aged children | 2.04 | 1.09 | 2.57 | 1.17 | <0.001 |
| Middle school-aged children | 2.03 | 1.13 | 2.59 | 1.18 | 0.005 |
| High school-aged children | 2.03 | 1.15 | 2.79 | 1.02 | <0.001 |
| I feel guilty about not spending time with my family | 2.79 | 1.03 | 1.94 | 1.3 | <0.001 |
| Infants & pre-school-aged children | 2.97 | 0.88 | 1.88 | 1.25 | <0.001 |
| Elementary school-aged children | 2.82 | 1.02 | 1.99 | 1.31 | <0.001 |
| Middle school-aged children | 2.82 | 1.23 | 1.88 | 1.34 | <0.001 |
| High school-aged children | 2.69 | 1.82 | 1.21 | 1.37 | <0.001 |
Only a small portion (5%) of our study population was pregnant. Of these, 62% did not change their birth plans while 10% planned to deliver at a different hospital from where they originally planned to deliver. The majority of women in this study did not have plans to have more children. However, 17% responded that they were delaying plans to have another child during the pandemic. Of note, 30% of departments or employers allowed physicians to opt out of caring for COVID-19 positive patients. The primary determinates were immunocompromising conditions (26%) and pregnancy (22%).
Discussion
This study of 2709 physician mothers during the COVID-19 pandemic assessed personal and professional concerns and the impact of the pandemic on the physician mothers’ lives. Previous studies have examined the preparedness, concerns, and mental health of HCWs during pandemics; however, none have focused specifically on physician mothers.
Our results show that the biggest concerns for physician mothers during this pandemic were exposing their children, their spouse/partner, and their parents to COVID-19, or dying from COVID-19, and that this was more concerning than personally acquiring COVID-19. Previous studies also showed that health-care workers felt a duty to serve but also strong competing duties to themselves and their family, while financial hardships, childcare, separation from family, and disrupted family life were less of a concern.13
A previous study by Qureshi et al. found that 53% of HCWs had child-care responsibilities, 63% of HCWs had children under age 13, and 30% had a spouse who would also be expected to work during a disaster.19 In this study, we found that the majority of physician mothers had a spouse in a high-risk job or had a spouse/partner who was a physician. Obligations on behalf of both parents to serve in a pandemic may further strain the health-care system. Qureshi et al. also found that fear and concern for family (47%) and self (31%) were reasons HCWs were not willing to report to work.
The strain on the health-care system and HCWs’ willingness to work during previous pandemics have been noted14,15,25-28 Most providers have a sense of duty during these taxing times. Many mothers had concerns about availability of PPE for not only themselves but staff and co-workers. For future planning, tangible items such as food, water, PPE, and cleaning supplies in the home, and having enough staff and beds, are the primary concerns of physician mothers. However, financial preparedness and health and morale of co-workers are also important.
Ehrenstein et al. found that, during the 2006 influenza pandemic, 24% of physicians felt it was acceptable to abandon their workplaces to protect themselves and their families, and 25% felt they should be allowed to decide if they should report to work. Surprisingly, 37% and 29% of administrators, respectively, felt this to be acceptable.11 In contrast, nearly all women physicians in our study continued to work with many increasing their hours to provide care. Previous studies have found that, if there was a pregnancy in the family or the provider was pregnant, there was a higher degree of unwillingness to work.17 In our study, a third of departments or employers allowed physicians to opt out of caring for COVID-19 patients due to a variety of reasons, including pregnancy. The impact of loss of workforce due to pregnancy is unclear but should be considered in manpower planning. Finally, despite the possibility of accommodations, the pandemic impacted family planning with 1 in 6 women planning to delay pregnancy.
Wong et al. found that 84% of health-care professionals felt their clinic was prepared for an avian influenza outbreak, while only 74% felt individually prepared.12 Physician mothers in our study were less prepared both professionally and personally. This may be due to the fact that physicians are familiar with influenza and were comfortably prepared for an influenza outbreak, whereas there was uncertainty regarding COVID-19, a novel coronavirus. Additionally, lack of preparedness may have been related to the enormity of COVID-19 pandemic compared with the avian influenza pandemic. After the avian influenza pandemic, 15% of HCWs felt they might look for another job because of risk from the pandemic.12 We found that the minority of physician mothers wished they had not pursued medicine and a smaller percentage wished they had chosen a different specialty.
In this study, we found that physician mothers are primarily concerned with the health and safety of their families. This concern for family well-being should be prioritized in future disaster planning to ensure the workforce can continue to perform their jobs and workplaces need to be cognizant of the needs of women physicians with children in the home.
Limitations
The data presented are self-reported and, therefore, cannot be verified. Additionally, the study is a convenience sample and may, therefore, not be representative of all physician mothers. Posting on social media has the potential to have a survey such as this shared, reposted, and further disseminated but does make it impossible to establish a denominator, and thus impossible to establish a survey response rate. This initial study sought to describe the physician mothers’ experience. We do not know if the concerns identified reflect the concerns of all physician parents or are unique to physician mothers. Data collection for physician fathers is currently underway.
Conclusion and Next Steps
This is one of the first studies to investigate the personal and professional concerns and challenges that physician mothers experience during a pandemic. The insights provided could be used to inform efforts to develop and prioritize strategies for physician mothers as the health-care community addresses the continued COVID-19 pandemic and prepares for future pandemics.
References
- 1.AAMC. Women were majority of U.S. medical school applicants in 2018. 2018. https://www.aamc.org/news-insights/press-releases/women-were-majority-us-medical-school-applicants-2018. Accessed May 6, 2020.
- 2.Stentz NC, Griffith KA, Perkins E, et al. Fertility and childbearing among American female physicians. J Womens Health (Larchmt). 2016;25(10):1059–1065. [DOI] [PubMed] [Google Scholar]
- 3.Treister-Goltzman Y, Peleg R.Female physicians and the work-family conflict. Isr Med Assoc J. 2016;18(5):261–266. [PubMed] [Google Scholar]
- 4.Guille C, Frank E, Zhao Z, et al. Work-family conflict and the sex difference in depression among training physicians. JAMA Intern Med. 2017;177(12):1766-1772. [DOI] [PMC free article] [PubMed]
- 5.AMA Association. Introduction to the 2014 work/life profiles of today’s U.S. Physicians. AMA Insurance Agency Inc., a subsidery of the American Medical Association. https://www.researchgate.net/profile/Soeren-Mattke/publication/317086140_Factors_Affecting_Physician_Professional_Satisfaction_and_Their_Implications_for_Patient_Care_Health_Systems_and_Health_Policy/links/595cec14aca27230850cf251/Factors-Affecting-Physician-Professional-Satisfaction-and-Their-Implications-for-Patient-Care-Health-Systems-and-Health-Policy.pdf. Accessed April 26, 2021.
- 6.Halley MC, Rustagi AS, Torres JS, et al. Physician mothers’ experience of workplace discrimination: a qualitative analysis. BMJ. 2018;363:k4926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang J, Krivkovich A, Starikova I, et al. Women in the workplace 2019. McKinsey & Company. https://www.mckinsey.com/∼/media/McKinsey/Featured%20Insights/Gender%20Equality/Women%20in%20the%20Workplace%202019/Women-in-the-workplace-2019.pdf. Accessed March 14, 2021. [Google Scholar]
- 8.Jolly S, Griffith KA, DeCastro R, et al. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Intern Med. 2014;160(5):344–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Devnani M.Factors associated with the willingness of health care personnel to work during an influenza public health emergency: an integrative review. Prehosp Disaster Med. 2012;27(6):551–566. [DOI] [PubMed] [Google Scholar]
- 10.Wong EL, Wong SY, Lee N, et al. Healthcare workers’ duty concerns of working in the isolation ward during the novel H1N1 pandemic. J Clin Nurs. 2012;21(9-10):1466–1475. [DOI] [PubMed] [Google Scholar]
- 11.Ehrenstein BP, Hanses F, Salzberger B.Influenza pandemic and professional duty: family or patients first? A survey of hospital employees. BMC Public Health. 2006;6:311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wong TY, Koh G, Cheong SK, et al. Concerns, perceived impact and preparedness in an avian influenza pandemic--a comparative study between healthcare workers in primary and tertiary care. Ann Acad Med Singapore. 2008;37(2):96–102. [PubMed] [Google Scholar]
- 13.Damery S, Draper H, Wilson S, et al. Healthcare workers’ perceptions of the duty to work during an influenza pandemic. J Med Ethics. 2010;36(1):12–18. [DOI] [PubMed] [Google Scholar]
- 14.Seale H, Wang Q, Yang P, et al. Hospital health care workers’ understanding of and attitudes toward pandemic influenza in Beijing. Asia Pac J Public Health. 2012;24(1):39–47. [DOI] [PubMed] [Google Scholar]
- 15.Barnett DJ, Levine R, Thompson CB, et al. Gauging U.S. Emergency Medical Services workers’ willingness to respond to pandemic influenza using a threat- and efficacy-based assessment framework. PLoS One. 2010;5(3):e9856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Damery S, Wilson S, Draper H, et al. Will the NHS continue to function in an influenza pandemic? A survey of healthcare workers in the West Midlands, UK. BMC Public Health. 2009;9:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martinese F, Keijzers G, Grant S, et al. How would Australian hospital staff react to an avian influenza admission, or an influenza pandemic? Emerg Med Australas. 2009;21(1):12–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garrett AL, Park YS, Redlener I.Mitigating absenteeism in hospital workers during a pandemic. Disaster Med Public Health Prep. 2009;3(Suppl 2):S141–S147. [DOI] [PubMed] [Google Scholar]
- 19.Qureshi K, Gershon RR, Sherman MF, et al. Health care workers’ ability and willingness to report to duty during catastrophic disasters. J Urban Health. 2005;82(3):378–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bai Y, Lin CC, Lin CY, et al. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 2004;55(9):1055–1057. [DOI] [PubMed] [Google Scholar]
- 21.Butsashvili M, Triner W, Kamkamidze G, et al. Knowledge and anticipated behavior of health care workers in response to an outbreak of pandemic influenza in Georgia. J Infect Dev Ctries. 2007;1(3):329–332. [PubMed] [Google Scholar]
- 22.Corrigan JR, Alhabash S, Rousu M, et al. How much is social media worth? Estimating the value of Facebook by paying users to stop using it. PLoS One. 2018;13(12):e0207101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lyu HG, Davids JS, Scully RE, et al. Association of domestic responsibilities with career satisfaction for physician mothers in procedural vs nonprocedural fields. JAMA Surg. 2019;154(8):689–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Young A, Chaudhry HJ, Pei X, et al. A census of actively licensed physicians in the United States, 2013. J Med Regul. 2017;103(2):7–21. [Google Scholar]
- 25.Seale H, Leask J, Po K, et al. “Will they just pack up and leave?” - attitudes and intended behaviour of hospital health care workers during an influenza pandemic. BMC Health Serv Res. 2009;9:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Balicer RD, Barnett DJ, Thompson CB, et al. Characterizing hospital workers’ willingness to report to duty in an influenza pandemic through threat- and efficacy-based assessment. BMC Public Health. 2010;10:436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barnett DJ, Balicer RD, Thompson CB, et al. Assessment of local public health workers’ willingness to respond to pandemic influenza through application of the extended parallel process model. PLoS One. 2009;4(7):e6365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Basta NE, Edwards SE, Schulte J.Assessing public health department employees’ willingness to report to work during an influenza pandemic. J Public Health Manag Pract. 2009;15(5):375–383. [DOI] [PubMed] [Google Scholar]