Abstract
Background:
Anterior cruciate ligament (ACL) reconstruction is usually performed with autologous bone–patellar tendon–bone (PT) or hamstring tendon (HT) graft. There has been only 1 randomized clinical trial examining ACL reconstruction with these grafts specifically in soccer players, and more studies comparing these graft types within a homogenous cohort such as soccer athletes may better highlight differences in outcomes.
Purpose:
To compare the results of ACL reconstruction with PT versus HT autograft in soccer players and to evaluate objective and subjective outcomes.
Study Design:
Randomized controlled trial; Level of evidence, 1.
Methods:
A total of 62 professional or semiprofessional soccer players (mean age, 25.1 years) with ACL injury were randomized to undergo reconstruction with PT or HT autograft by a single orthopaedic surgeon (n = 31 in each group). Outcome measures were recorded preoperatively and at 2 years postoperatively. The primary outcome was the modified Cincinnati Knee Rating System, and secondary outcomes were the objective and subjective International Knee Documentation Committee scores, Lachman test, pivot-shift test, anterior drawer test, and Lysholm score. The following variables were also evaluated postoperatively: return to soccer, level at return, graft rerupture, postoperative complications, anterior knee pain, patellar tendinitis, difficulty sprinting, and loss of kicking power.
Results:
The PT and HT groups were homogenous in terms of age, sex distribution, injured side, and time from injury to surgery, and there was no difference between them on any preoperative outcome score. At 2 years postoperatively, there were no differences between the groups on any outcome score; however, there were significantly fewer patients with anterior knee pain in the HT group compared with the PT group (7 [22.6%] vs 15 [48.4%], respectively; P = .03). Two patients from each group (2/31; 6.5%) sustained rerupture.
Conclusion:
There were no differences between soccer players who underwent different types of ACL reconstruction with the exception of anterior knee pain, which was more frequent in players who underwent reconstruction with PT graft.
Registration: NCT02642692 (ClinicalTrials.gov).
Keywords: ACL, graft, sports, reconstruction
Anterior cruciate ligament (ACL) reconstruction has been recommended to improve knee stability, and a number of techniques have been proposed and tested, including synthetic ligament, autograft tendon, allograft tendon, repair with biologic augmentation, and extra-articular reconstruction.6,16 Most surgeons prefer bone–patellar tendon–bone (PT) autografts or hamstring tendon (HT) autograft because of the favorable results, experience with graft use, and conventionality.16,20,28
The functional outcome and rerupture rates after ACL reconstruction with the PT or HT continue to be widely debated. Superiority of one graft over another has not been definitively borne out in the literature,4,6,7,9,10,12,16,21,28 as interpretation of outcomes has been clouded by differences in autograft preparation and fixation techniques, concomitant knee malalignment, concurrent intra-articular lesions, and heterogeneity in return-to-play protocols.
The risk of experiencing an injury to the ACL is quite low in the general population11,22,25 but is considerably higher among players of many popular team sports, including soccer.29 Soccer is the most popular sport worldwide; it has >260 million active players, of whom 10% are women, according to the Big Count survey in 2006.32 There has only been 1 randomized clinical trial comparing PT autografts and HT autografts specifically in soccer players,23 and more studies comparing these graft types within a homogenous cohort such as soccer athletes may better highlight differences in outcomes.
The objective of this study was to specifically evaluate the outcomes of PT autograft versus HT autograft ACL reconstruction in soccer players. The hypothesis of this study was that HT autograft ACL reconstruction would provide no statistically significant differences in patient-reported outcome scores, postoperative level of sports function, and harvest-site morbidity compared with PT autograft ACL reconstruction in a matched group of athletes from a specific sport (soccer).
Methods
Patient Selection and Randomization
Between January 2016 and August 2018, professional or semiprofessional soccer players with an ACL injury were evaluated by the knee group and the orthopaedic sports trauma group at a single public orthopaedic referral hospital in the state of São Paulo, Brazil. The inclusion criteria for admission to the study were as follows: confirmed unilateral ACL lesion, symptomatic patients (report of instability), skeletally mature patients with closed physis, age between 14 and 40 years, no previous surgery on the affected knee (except for arthroscopic meniscectomy), <1 year postinjury, and soccer players who hoped to resume playing soccer after surgery. The exclusion criteria were degenerative changes (Kellgren-Lawrence grades 2-4), associated ligament injuries (except for medial collateral ligament grades 1 and 2), and intraoperative identification of ≥1 chondral lesions >1 cm2. We did not consider soccer players who played <4 times a week. The protocol for this study received ethics committee approval, and all included patients signed an informed consent form.
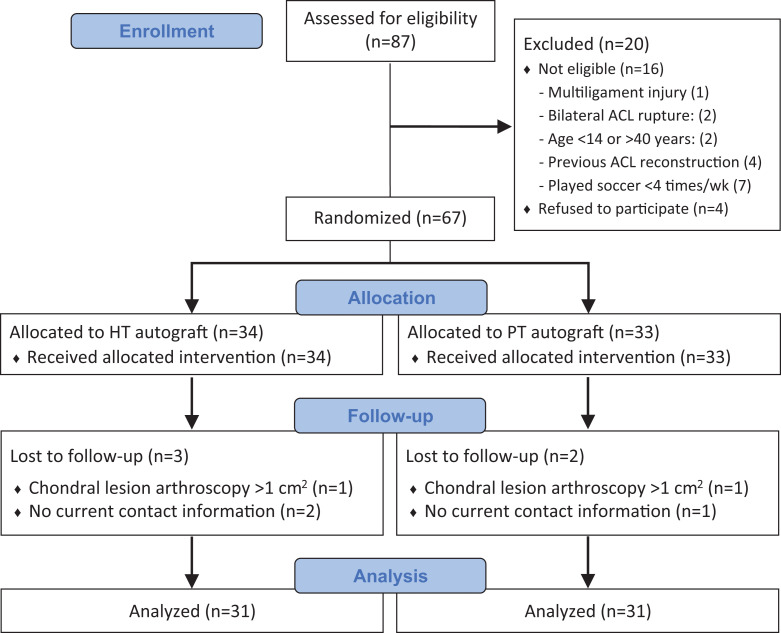
During the study recruitment period, 87 patients were screened, and 67 were eligible and randomized into the HT group or the PT group, depending on the graft used. Randomization was performed using SPSS 13.0 for Windows (SPSS Inc) by a member of the institution’s statistical group before the beginning of the study. Three patients were lost to follow-up, and 2 were excluded because of intraoperative chondral lesions >1 cm2. The final sample included 62 patients (95% follow-up): 31 in the PT group and 31 in the HT group (Figure 1).
Figure 1.
CONSORT flow diagram. ACL, anterior cruciate ligament; HT, hamstring tendon; PT, patellar tendon.
Surgical Technique and Postoperative Rehabilitation
All patients were operatively treated by the same surgeon (L.G.B.G.) or under his supervision. For both groups, the techniques were the same: the surgical technique involved arthroscopy, treatment of meniscal and chondral injuries, and ACL reconstruction with fixation of the flexor tendon graft (semitendinosus and gracilis) or the PT graft on the tibia and femur using metal interference screws. The tibial tunnel was drilled with the knee in flexion using a conventional guide. The femoral tunnel was drilled using the outside-in technique. No patient was treated with selective reconstruction of only 1 of the ACL bundles. The grafts were harvested by an assistant, using No. 1.0 Vicryl (Ethicon) for the flexor tendon graft in a 4-strand fashion and No. 5.0 Ethibond (Ethicon) for the PT graft. Both grafts were fixed first in the femur, tensioned manually, and then fixed in the tibia.
Both groups of patients underwent the same institutional timeline-based physical therapy protocol. In the immediate postoperative period, gain of passive range of motion began with measures to control effusion. Gait training using 2 crutches started in the first week; 1 crutch, in 2 weeks; and full weightbearing, in 3 weeks. Full passive extension was obtained in 1 week, and full flexion was obtained in 4 weeks. Open kinetic chain exercises began at 3 months. All patients fulfilled the following return-to-sports criteria: difference of muscle strength, hop test, and Y-balance test between sides <10% and plyometric exercises without pain for 1 month.
Evaluation
The patients were preoperatively and postoperatively evaluated using the modified Cincinnati Knee Rating System26 (CKRS) as the primary outcome measure and the objective International Knee Documentation Committee3 (IKDC), subjective IKDC, Lachman test, pivot-shift test, anterior drawer test, and Lysholm score19 as secondary outcome measures. In addition to these scores, other outcomes were evaluated postoperatively: return to soccer, level at return, graft rerupture, postoperative complications, anterior knee pain, patellar tendinitis, difficulty sprinting, and loss of kicking power. The final clinical evaluation was performed 2 years after surgery. This evaluation was made by a surgeon who was part of the knee group of our institution but was not an author. Because of the different types of scars, blinding was not possible.
Statistical Analysis
The data collected were statistically analyzed using SPSS 13.0 for Windows (SPSS Inc). For the descriptive analysis, the qualitative variables were described using frequencies (numbers and percentages) and graphs. The quantitative variables were described using summary measures (means, medians, standard deviations, minima and maxima). For qualitative versus qualitative inferences, the chi-square test or Fisher exact test was used. For qualitative versus quantitative inferences, the Student t test (parametric) or the Mann-Whitney test (nonparametric) was used. Both inferences used a 5% significance level. The modified CKRS was chosen as the primary outcome. A power analysis using a 2-tailed test with a power of 80% and an α of .05 showed that a sample size of 27 patients in each group was needed for a 10-point difference in modified CKRS score, assuming a mean ± standard deviation of 90 ± 13 for the control group.33 Expecting a 20% sample size attrition, 67 patients were randomized.
Results
Patient Characteristics
Of the 62 study patients, 42 were men, and 20 were women. Surgery was performed on 35 right knees and 27 left knees. The mean age of the patients was 25.1 years (range, 15-38 years). The average time between injury and surgery was 4 months. All the patients were evaluated within 24 months after surgery. Age, sex, injury side, subjective IKDC score, Lysholm score, CKRS score, and time between injury and surgery were not significantly different between the groups, indicating that the groups were homogenous during the preoperative period (Table 1).
Table 1.
Preoperative Characteristics of the Study Groupsa
| HT Group (n = 31) | PT Group (n = 31) | P Value | |
|---|---|---|---|
| Age, y | 24.64 ± 5.33 | 25.2 ± 5.48 | .82 |
| Sex, male/female | 19/12 | 23/8 | .76 |
| Side affected, right/left | 18/13 | 17/14 | .98 |
| Time between injury and surgery, mo | 4.02 ± 4.72 | 4.42 ± 4.91 | .87 |
aData are reported as mean ± SD or n. HT, hamstring tendon; PT, patellar tendon.
Postoperative Outcome Scores
Regarding the objective outcomes evaluated, there were no significant differences between the study groups in the Lachman, pivot-shift, and anterior drawer tests or the objective IKDC score (Table 2).
Table 2.
Postoperative Objective Outcomesa
| HT Group (n = 31) | PT Group (n = 31) | P Value | |
|---|---|---|---|
| Lachman grade | .94 | ||
| 0 | 22 (71) | 22 (71) | |
| 1 | 6 (19.4) | 7 (22.6) | |
| 2 | 2 (6.5) | 1 (3.2) | |
| 3 | 1 (3.2) | 1 (3.2) | |
| Anterior drawer test | .71 | ||
| 0 | 22 (71) | 21 (67.7) | |
| 1 | 5 (16.1) | 8 (25.8) | |
| 2 | 2 (6.5) | 1 (3.2) | |
| 3 | 2 (6.5) | 1 (3.2) | |
| Pivot-shift test | .34 | ||
| 0 | 20 (64.5) | 24 (77.4) | |
| 1 | 8 (25.8) | 5 (16.1) | |
| 2 | 2 (6.5) | — | |
| 3 | 1 (3.2) | 2 (6.5) | |
| IKDC objective score | .70 | ||
| 1 | 15 (48.4) | 18 (58.1) | |
| 2 | 13 (41.9) | 11 (35.5) | |
| 3 | 1 (3.2) | — | |
| 4 | 2 (6.5) | 2 (6.5) |
aData are reported as n (%). Dashes indicate no patients. HT, hamstring tendon; IKDC, International Knee Documentation Committee; PT, patellar tendon.
Concerning the subjective scores evaluated (Table 3), the mean postoperative CKRS score of the PT group was 89.61 (range, 48-100), and that of the HT group was 90.97 (range, 48-100). There was no significant difference (P = .40) between the groups according to the Mann-Whitney test. The mean IKDC subjective score of the PT group was 88.75 (range, 65-100), and that of the HT group was 91 (range, 58-100); the scores did not differ significantly (P = .54, Mann-Whitney test). The mean Lysholm score of the PT group was 89.87 (range, 65-100), and that of the HT group was 91.26 (range, 60-100) (P = .50, Mann-Whitney test).
Table 3.
Postoperative Subjective Outcomesa
| HT Group (n = 31) | PT Group (n = 31) | P Value | |
|---|---|---|---|
| CKRS score | .40 | ||
| Mean ± SD | 90.97 ± 13.87 | 89.61 ± 13.37 | |
| Median (range) | 96.0 (48-100) | 95.0 (48-100) | |
| IKDC subjective score | .54 | ||
| Mean ± SD | 91.0 ± 9.07 | 88.75 ± 9.27 | |
| Median (range) | 92.0 (58-100) | 92.0 (65-100) | |
| Lysholm score | .50 | ||
| Mean ± SD | 91.26 ± 9.36 | 89.87 ± 9.17 | |
| Median (range) | 94.0 (60-100) | 92.0 (65-100) |
aCKRS, Cincinnati Knee Rating System; HT, hamstring tendon; IKDC, International Knee Documentation Committee; PT, patellar tendon.
Other Outcomes
In the matter of the return to soccer, only 1 patient did not return; this patient was from the HT group, and the decision was not because of knee disability but a personal decision. Regarding the level of participation at return, 33 (53.2%) patients returned at the same technical level; 25 (40.3%), at a slightly lower level; and 3 (4.8%), at a much lower level; 1 (1.6%) did not return. In the PT group, 16 (51.6%) returned at the same level, 13 (41.9%) returned at a slightly lower level, and 2 (6.4%) returned at a much lower level. In the HT group, 17 (54.8%) returned at the same level; 12 (38.7%), at a slightly lower level; and 2 (6.4%), at a much lower level. The difference between the groups was not significant (P = .71, χ2 test).
Graft rerupture was considered when patients sustained a new sprain, patients experienced a feeling of instability after the sprain, and the clinical and magnetic resonance imaging examination showed rerupture. All the reruptures happened after full return to sports activity. In the PT group, 2 (6.5%) patients had a rerupture compared with 2 (6.5%) patients in the HT group; there was no significant difference (P ≥ .99, Fisher exact test). In the PT group, 1 patient experienced rerupture 9 months after surgery; the other, after 18 months. In the HT group, 1 patient had rerupture after 12 months; the other, 14 months after surgery.
Rerupture was also evaluated according to sex. Among the male patients, there were 3 (7.1%) reruptures, and among the female patients, there was 1 (5%) rerupture; there was no significance difference (P = .10, χ2 test).
Regarding postoperative complications, there was no infection (superficial or deep) or arthrofibrosis. Only 3 patients developed cyclops syndrome; 1 of these patients (HT group) had complete loss of extension and underwent surgery 3 months after the initial surgery, regaining full range of motion. The other 2 patients with cyclops syndrome (1 in the HT group and 1 in the PT group) did not lose range of motion but required arthroscopic resection of the cyclops lesion because of discomfort and progressed without symptoms after the resection.
The evaluations of the grafts in terms of anterior knee pain, patellar tendinopathy, hamstring tendinopathy, feeling of loss of kicking power, and feeling of loss of power to sprint are shown in Table 4. Patellar tendinitis and hamstring tendinitis were diagnosed clinically and sometimes using magnetic resonance imaging. Two years after surgery, 7 (22.6%) patients in the HT group reported anterior knee pain after returning to soccer; in the PT group, 15 (48.4%) patients reported it, and the difference was significant (P = .03, χ2 test). Before the surgery, none of the patients had significant anterior knee pain. Regarding postoperative patellar tendinitis, 3 (9.7%) patients in the HT group and 8 (25.8%) patients in the PT group were affected, with no significant difference between the groups (P = .10, χ2 test). Regarding postoperative hamstring tendinitis or injury, 7 (22.6%) patients in the HT group and 1 (3.2%) patient in the PT group reported its occurrence, with no significant difference between the groups (P = .05, Fisher exact test) but a trend toward more cases in the HT group. Regarding the feeling of loss of kicking power, 8 (25.8%) patients in the HT group and 9 (29%) patients in the PT group reported this sensation, with no significant difference between the groups (P = .77, χ2 test). Lastly, 6 (19.4%) patients in the HT group and 4 (12.9%) patients in the PT group reported loss of sprinting power, with no significant difference between the groups (P = .49, χ2 test).
Table 4.
Other Postoperative Outcomesa
| HT Group (n = 31) | PT Group (n = 31) | P Value | |
|---|---|---|---|
| Patellar tendinitis | .10 | ||
| Yes | 3 (9.7) | 8 (25.8) | |
| No | 28 (90.3) | 23 (74.2) | |
| Anterior knee pain | .03 | ||
| Yes | 7 (22.6) | 15 (48.4) | |
| No | 24 (77.4) | 16 (51.6) | |
| Hamstring tendinitis | .05 | ||
| Yes | 7 (22.6) | 1 (3.2) | |
| No | 24 (77.4) | 30 (96.8) | |
| Loss of kicking power | .77 | ||
| Yes | 8 (25.8) | 9 (29.0) | |
| No | 23 (74.2) | 22 (71.0) | |
| Loss of sprint start | .49 | ||
| Yes | 6 (19.4) | 4 (12.9) | |
| No | 25 (80.6) | 27 (87.1) |
aData are reported as n (%). Bolded P value indicates a statistically significant difference between groups (P < .05). HT, hamstring tendon; PT, patellar tendon.
Discussion
This is the second prospective and randomized series comparing ACL reconstruction with HT autograft versus PT autograft in soccer players,23 but the present study included a sample of >42 patients (62 patients). It included not only professional players but also individuals who play soccer ≥4 times a week, who are high-performance athletes at risk for surgery-related symptoms, new associated injuries, and graft rerupture. There is a debate regarding the best graft for each sports modality,8 but the answer is unclear because of the lack of prospective controlled series according to sports modality. The present study seeks to contribute to this discussion specifically with regard to soccer, the most practiced sport worldwide.32 Care was taken with methodological details (randomization method, inclusion and exclusion criteria, and surgery performed by the same team experienced with both techniques), but it was not possible to blind patients because the scars left from harvesting of the grafts were very clearly different.
In Brazil, soccer is played predominantly by men (96.3% of the participants),18 but in the present study, a considerable number of women underwent surgery (32.3%). This is because during the sample recruitment period, the hospital in question had a partnership with women’s soccer teams, such as the Brazilian women’s soccer team, and served as the referral surgical hospital for athletes from the professional team and lower divisions. It is known that women are more likely to sustain a rerupture,1,2 but this difference was not identified in the present study since there were 3 (7.1%) reruptures in the men and 1 (5%) in the women. Recalling that the final assessment was performed 2 years after surgery and that there were 42 male and 20 female patients, which is a small number, it is possible that a greater number of patients and a longer follow-up would yield results consistent with the trend of more reruptures among women. Regarding reruptures in the total sample (men and women), 2 patients in the PT group and 2 in the HT group sustained reruptures; thus, there was no difference between groups. In the literature, some studies have reported less rerupture and failure with PT autografts,8,10,13,17,24,27,31,34 but there is no consensus because other studies have shown no differences between these grafts.5,12,14,15,21 However, no studies that showed more reruptures in patients with PT grafts compared with HT grafts were found.
When evaluating the subjective parameters (CKRS score, Lysholm score, and IKDC subjective score), very similar results were observed between the groups; there was no significance difference and no trend toward better results in one group relative to the other in terms of the absolute values and percentages for these scores, thus reducing the possibility of a type 2 statistical error. We cannot fully rule out this possibility, but at first examination, the data do not lead us to believe it is likely. There are several studies, including systematic reviews and meta-analyses, that have compared PT with HT grafts8,13–15,17,27,31 and generally analyzed the outcomes of physical examinations and KT1000, IKDC, Lysholm, and CKRS scores,5,16,24,34 and most of these studies did not indicate differences between groups in these outcomes.
However, subjective evaluations, such as anterior knee pain, patellar tendinopathy, hamstring tendinopathy, feeling of loss of kicking power, and feeling of loss of power to sprint, are less frequently reported in the literature. In 2015, Heijne et al14 compared PT and HT groups and did not find differences regarding anterior knee pain or eccentric or concentric quadriceps torque. They found a difference in pes anserinus strength at 2 years after surgery, but the difference had disappeared 5 years after surgery. In the present study, anterior knee pain was more frequent in the PT group. The strength of the quadriceps and knee flexors was not evaluated; however, the feeling of loss of kicking power and of sprint start was evaluated, and no significant differences were observed. Additionally, in 2013, Mohammadi et al23 compared soccer players who had undergone ACL reconstruction with PT and HT grafts and obtained better results in the HT group for quadriceps torque and on proprioceptive tests (triple hop, crossover hop, and jump landing). In 2015, Kautzner et al15 compared PT versus HT grafts in women and did not find significant differences in relation to functional scores, stability, or rerupture. They found only a greater frequency of anterior knee pain in the PT group in the first 6 months after surgery. In 2016, Webster et al33 evaluated stability, functional scores, anterior knee pain, pain on kneeling, and extension deficit. No difference was found 15 years after surgery, but there was a difference in extension deficit at 3 years after surgery for the PT group. Another interesting recent study, published in 2020 by Smith et al,30 showed that athletes who undergo reconstruction with PT require longer rehabilitation before returning to sports than do patients who receive autologous or soft tissue allograft HT grafts. Although it is not possible to compare those data with the results of our study because we did not evaluate this variable, it is worth mentioning this finding because it suggests a possible advantage of the HT graft that should be reevaluated in future studies.
The limitations of the present study include the sample size. Despite the sample size calculation performed, only the CKRS score was used as an outcome, and more patients are probably necessary for the evaluation of the other outcomes. Additionally, the study was not blinded, the follow-up time was only 2 years, and the 2 sexes were mixed in the total sample. Furthermore, some outcomes were not assessed: time for return to sporting activity, patient satisfaction, hamstring muscle strength, quadriceps muscle strength, and hip or knee range of motion. Also, our evaluation was only at 2 years.
Conclusion
The evaluated outcomes did not show differences between soccer players who underwent ACL reconstruction with PT versus HT grafts, according to the hypothesis that there would be no difference, except in the case of anterior knee pain, which was more frequent in the PT group. Additional series with a similar method are needed for further conclusions.
Acknowledgment
The authors thank the Orthopedics Department of Santa Casa de Misericórdia de São Paulo for the opportunity to develop this study.
Footnotes
Final revision submitted February 27, 2021; accepted March 4, 2021.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Irmandade da Santa Casa de Misericórdia de São Paulo.
References
- 1.Allen MM, Pareek A, Krych AJ, et al. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med. 2016;44(10):2492–2498. [DOI] [PubMed] [Google Scholar]
- 2.Andernord D, Desai N, Bjornsson H, Ylander M, Karlsson J, Samuelsson K. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med. 2015;43(1):121–127. [DOI] [PubMed] [Google Scholar]
- 3.Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The International Knee Documentation Committee subjective knee evaluation form: normative data. Am J Sports Med. 2006;34(1):128–135. [DOI] [PubMed] [Google Scholar]
- 4.Carter TR, Edinger S. Isokinetic evaluation of anterior cruciate ligament reconstruction: hamstring versus patellar tendon. Arthroscopy. 1999;15(2):169–172. [DOI] [PubMed] [Google Scholar]
- 5.Chee MY, Chen Y, Pearce CJ, et al. Outcome of patellar tendon versus 4-strand hamstring tendon autografts for anterior cruciate ligament reconstruction: a systematic review and meta-analysis of prospective randomized trials. Arthroscopy. 2017;33(2):450–463. [DOI] [PubMed] [Google Scholar]
- 6.Corry IS, Webb JM, Clingeleffer AJ, Pinczewski LA. Arthroscopic reconstruction of the anterior cruciate ligament: a comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med. 1999;27(4):444–454. [DOI] [PubMed] [Google Scholar]
- 7.Doral MN, Leblebicioglu G, Atay OA, Baydar ML, Tetik O, Atik S. Arthroscopy-assisted anterior cruciate ligament reconstruction with patellar tendon or hamstring autografts. Bull Hosp Jt Dis. 2000;59(2):81–87. [PubMed] [Google Scholar]
- 8.Ekeland A, Engebretsen L, Fenstad AM, Heir S. Similar risk of ACL graft revision for alpine skiers, football and handball players: the graft revision rate is influenced by age and graft choice. Br J Sports Med. 2020;54(1):33. [DOI] [PubMed] [Google Scholar]
- 9.FIFA. FIFA Big Count 2006: 270 million people active in football. Accessed September 1, 2021. https://digitalhub.fifa.com/m/55621f9fdc8ea7b4/original/mzid0qmguixkcmruvema-pdf.pdf
- 10.Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR, Jr. Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31(1):2–11. doi:10.1177/03635465030310011501 [DOI] [PubMed] [Google Scholar]
- 11.Frobell RB, Lohmander LS, Roos HP. Acute rotational trauma to the knee: poor agreement between clinical assessment and magnetic resonance imaging findings. Scand J Med Sci Sports. 2007;17(2):109–114. [DOI] [PubMed] [Google Scholar]
- 12.Gabler CM, Jacobs CA, Howard JS, Mattacola CG, Johnson DL. Comparison of graft failure rate between autografts placed via an anatomic anterior cruciate ligament reconstruction technique: a systematic review, meta-analysis, and meta-regression. Am J Sports Med. 2016;44(4):1069–1079. doi:10.1177/0363546515584043 [DOI] [PubMed] [Google Scholar]
- 13.Gifstad T, Foss OA, Engebretsen L, et al. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014;42(10):2319–2328. [DOI] [PubMed] [Google Scholar]
- 14.Heijne A, Hagstromer M, Werner S. A two- and five-year follow-up of clinical outcome after ACL reconstruction using BPTB or hamstring tendon grafts: a prospective intervention outcome study. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):799–807. [DOI] [PubMed] [Google Scholar]
- 15.Kautzner J, Kos P, Hanus M, Trc T, Havlas V. A comparison of ACL reconstruction using patellar tendon versus hamstring autograft in female patients: a prospective randomised study. Int Orthop. 2015;39(1):125–130. [DOI] [PubMed] [Google Scholar]
- 16.Kurz A, Evaniew N, Yeung M, Samuelsson K, Peterson D, Ayeni OR. Credibility and quality of meta-analyses addressing graft choice in anterior cruciate ligament reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):538–551. [DOI] [PubMed] [Google Scholar]
- 17.Laboute E, James-Belin E, Puig PL, Trouve P, Verhaeghe E. Graft failure is more frequent after hamstring than patellar tendon autograft. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3537–3546. [DOI] [PubMed] [Google Scholar]
- 18.Lima DF, Piovani VGS, Lima LA. Prática de futebol recreativo entre adultos residentes nas capitais brasileiras, 2011-2015. Epidemiol Serv Saúde. 2018;27(2):e2017284. [DOI] [PubMed] [Google Scholar]
- 19.Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–154. [DOI] [PubMed] [Google Scholar]
- 20.Martin-Alguacil JL, Arroyo-Morales M, Martin-Gomez JL, et al. Strength recovery after anterior cruciate ligament reconstruction with quadriceps tendon versus hamstring tendon autografts in soccer players: a randomized controlled trial. Knee. 2018;25(4):704–714. [DOI] [PubMed] [Google Scholar]
- 21.Mascarenhas R, Tranovich MJ, Kropf EJ, Fu FH, Harner CD. Bone-patellar tendon-bone autograft versus hamstring autograft anterior cruciate ligament reconstruction in the young athlete: a retrospective matched analysis with 2-10 year follow-up. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1520–1527. [DOI] [PubMed] [Google Scholar]
- 22.Miyasaka KC, Daniel DM, Stone ML, Hirshman P. The incidence of knee ligament injuries in the general population. Am J Knee Surg. 1991;4:3–8. [Google Scholar]
- 23.Mohammadi F, Salavati M, Akhbari B, Mazaheri M, Mohsen Mir S, Etemadi Y. Comparison of functional outcome measures after ACL reconstruction in competitive soccer players: a randomized trial. J Bone Joint Surg Am. 2013;95(14):1271–1277. [DOI] [PubMed] [Google Scholar]
- 24.Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011;7(9):CD005960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nielsen AB, Yde J. Epidemiology of acute knee injuries: a prospective hospital investigation. J Trauma. 1991;31(12):1644–1648. [DOI] [PubMed] [Google Scholar]
- 26.Noyes FR, Barber SD, Mooar LA. A rationale for assessing sports activity levels and limitations in knee disorders. Clin Orthop Relat Res. 1989;246:238–249. [PubMed] [Google Scholar]
- 27.Persson A, Fjeldsgaard K, Gjertsen JE, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014;42(2):285–291. [DOI] [PubMed] [Google Scholar]
- 28.Samuelsen BT, Webster KE, Johnson NR, Hewett TE, Krych AJ. Hamstring autograft versus patellar tendon autograft for ACL reconstruction: is there a difference in graft failure rate? A meta-analysis of 47,613 patients. Clin Orthop Relat Res. 2017;475(10):2459–2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sandon A, Werner S, Forssblad M. Factors associated with returning to football after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23(9):2514–2521. [DOI] [PubMed] [Google Scholar]
- 30.Smith AH, Capin JJ, Zarzycki R, Snyder-Mackler L. Athletes with bone-patellar tendon-bone autograft for anterior cruciate ligament reconstruction were slower to meet rehabilitation milestones and return-to-sport criteria than athletes with hamstring tendon autograft or soft tissue allograft: secondary analysis from the ACL-SPORTS trial. J Orthop Sports Phys Ther. 2020;50(5):259–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spindler KP, Huston LJ, Zajichek A, et al. Anterior cruciate ligament reconstruction in high school and college-aged athletes: does autograft choice influence anterior cruciate ligament revision rates? Am J Sports Med. 2020;48(2):298–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Walden M, Hagglund M, Werner J, Ekstrand J. The epidemiology of anterior cruciate ligament injury in football (soccer): a review of the literature from a gender-related perspective. Knee Surg Sports Traumatol Arthrosc. 2011;19(1):3–10. [DOI] [PubMed] [Google Scholar]
- 33.Webster KE, Feller JA, Hartnett N, Leigh WB, Richmond AK. Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: a 15-year follow-up of a randomized controlled trial. Am J Sports Med. 2016;44(1):83–90. [DOI] [PubMed] [Google Scholar]
- 34.Xie X, Liu X, Chen Z, Yu Y, Peng S, Li Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015;22(2):100–110. [DOI] [PubMed] [Google Scholar]