Abstract
COVID-19 has disproportionally affected underrepresented minorities (URM) and low-income immigrants in the United States. The aim of the study is to examine the underlying vulnerabilities of Mexican immigrants in New York City (NYC) and Los Angeles (LA), its correspondence with area-level COVID-19 morbidity and mortality, and to document the role of trusted and culturally sensitive services offered during the pandemic through the Ventanillas de Salud (i.e. VDS, Health Windows) program. The study uses a mixed-methods approach including a cross-sectional survey of Mexican immigrants in LA and NYC collected in the Mexican Consulates at the onset of the pandemic, complemented with a georeferencing analysis and key informant interviews. Data suggested an increased vulnerability to COVID-19 given participants reported health status, health care profile and place of residence, which coincided with the georeferencing analysis. The key informant interviews confirmed the vulnerability of this population and the supporting role of VDS in helping immigrants navigate health systems and disseminate health information. Mexican immigrants had an increased vulnerability to COVID-19 at the individual, geographic and systemic levels. Trusted and culturally sensitive services are needed to overcome some of the barriers and risk factors that increase the vulnerability of URM and immigrant populations to COVID-19.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10903-021-01283-8.
Keywords: Hispanic, Immigrant health, COVID-19, Inequities, Health outreach
Introduction
The COVID-19 pandemic has disproportionally affected underrepresented minorities (URM) and low-income immigrants in the United States (U.S.) [1]. Studies based on geographic analyses document that COVID-19 case rates are higher in counties with a higher concentration of low-income and undocumented immigrant populations [2]. COVID-19 infection and mortality rates are also greater in counties and states with high Hispanic/Latino populations [3] and monolingual Spanish speakers [3–5]. Social determinants of health in Hispanic communities may be contributing to the disproportionate rate of infections and deaths [6]. In 2020, life expectancy declined one year in the U.S., however, 2 years for Hispanics [7].
The available evidence indicates that Hispanic immigrants in the US are a vulnerable population disproportionately affected by the COVID-19 pandemic due to individual (i.e. type of employment [4, 8], burden of chronic diseases [1, 5]), system related (i.e. limited access to health care due to low English proficiency or health insurance coverage [9, 10], citizenship status and public program eligibility [11–14], stigma and fear of deportation), and area-level factors (e.g. overcrowded housing [8], limited access to healthy foods [15]). The combination of pre-pandemic vulnerabilities at the individual, system and area-level likely contributed to increasing the risk of COVID-19 morbidity and mortality [16, 17].
Hispanic immigrants disproportionately participate as essential, front-line, low-wage, and uninsured workers in activities critical for operational functions and support of crucial supply chains [18], such as meatpacking, agricultural and service-based industries, which do not allow for remote work, and increase the risk of infection [4]. Therefore, shelter-in-place policies were unlikely to protect them [8]. Their limited access to health care, lack of familiarity and fear of interacting with the health system as a consequence of immigration enforcement and recent changes to public charge rules [15, 19, 20], may have discouraged testing and timely treatment for COVID-19.
The pandemic will not be controlled unless all individuals have equal access to health care [13]. Policies need to be put in place to expand coverage to the remaining uninsured, including undocumented immigrants [14]. This highlights the need to address the racial/ethnic disparities of the COVID-19 pandemic, including culturally appropriate and community competent interventions that consider the nuances of immigrant communities, families and individuals [8].
The aim of the study is to examine the underlying vulnerabilities of Mexican immigrants in NYC and LA to improve future preparedness for public health emergencies. Our approach uses mixed methods with three different sources of data that intend to inform individual, system and area level determinations. The main objectives are: (1) to describe pre-pandemic migrants’ health and psychosocial characteristics and vulnerabilities through a survey collected at the Mexican Consulates of NYC and LA; (2) to examine with a spatial analysis the correspondence between the survey respondents’ place of residence and area-level COVID-19 morbidity and mortality to confirm if Mexicans with identified underlying risk factors lived in affected areas; and (3) to interview key informants from Mexican Consulates in both cities to contextualize how Mexican immigrants faced the pandemic, and to document the role of trusted and culturally sensitive services offered during the pandemic through the Consulates’ Ventanillas de Salud (i.e. VDS, Health Windows) program. We triangulate the findings of the three sources to gauge a more granular understanding of individual, system, and area level factors shaping the vulnerabilities and experiences of Mexican immigrants during the pandemic, and the potential buffering role of trusted and culturally sensitive services, as those offered through the VDS. To our knowledge, there are no prior studies triangulating such types of data.
We selected NYC and LA because both cities have been greatly affected by the pandemic, and they have a large community of Mexican immigrants. It has also been documented that in NYC individuals living in high poverty areas and with high shares of URMs experienced the highest COVID-19 case and death rates [17]. Likewise, in January 2021, the average death rate among residents of Los Angeles County’s (LA) poorest neighborhoods was three times as high as that in the wealthiest areas [17]. Importantly, both cities have a well-established VDS program. The VDS is a promising example of a trusted and culturally sensitive outreach program that started in 2003 as a joint initiative between the Mexican Ministries of Health and Foreign Affairs. The goal of the VDS is to enable Mexican immigrants access to health care and local community resources [21]. Even though the Mexican government funds the VDS in 49 US cities, they partner with different public and private organizations to provide culturally and linguistically sensitive basic health services in a safe and trustful environment. A recent scoping review found that VDS mostly offer three free types of services: healthy lifestyles information and counseling; immunizations and early disease detection; and referral to local community clinics [22]. The VDS serves nearly 1.5 million individuals a year [21], mostly undocumented immigrants, and it was a key support for Mexican immigrants during the COVID-19 pandemic in NYC and LA.
Methods
Data Sources
The study used a survey with a cross-sectional design, complemented with a georeferencing analysis and with key informant interviews. The survey was conducted before the onset of the COVID-19 pandemic among Mexican immigrants between 18 and 64 years who resided in the NYC and LA Metropolitan areas and who identified themselves as living in the U.S. Data were collected at the main offices of the Consulate General of Mexico in both cities. Consulates provide services to both documented and undocumented Mexican immigrants, including renewal of Mexican passports, issuance of a consular ID (matrícula consular), legal counselling, health information and referral to local health care providers (provided through the VDS), among others. The advantages of conducting data collection at the Consulates have been highlighted in prior research [23, 24]. Mexicans visit the consulates regardless of their migratory status and most services are scheduled through a telephone appointment system that allocates time slots randomly. This appointment mechanism reduces unobserved biases compared to alternative sampling sites such as churches, community centers, clinics, or other settings where visitors are self-selected. In addition, Mexican immigrants are more open to participate within the premises of the Consulates, as they know this is a safe space, which reduces potential fears linked to their migratory condition and distress of ethnic stigmatization.
A convenience sampling approach was used in the general waiting areas of the Consulates and in the VDS located in the Consulates. Immigrants doing their paperwork at the Consulates’ offices were approached individually by four previously trained, bilingual and bicultural research assistants. They informed potential participants about the study details and invited eligible subjects to participate in a face-to-face survey that took approximately 20 min. Those who agreed to participate and met the eligibility criteria signed a consent form. Research assistants administered the survey in the waiting areas and electronically collected responses in tablets. The survey had previously been piloted in the NYC Mexican Consulate with the population it serves to assess it was culturally sensitive and was available both in English and Spanish. In NYC data was collected between May and June 2019; in LA data collection started the first week of March 2020 and needed to be abruptly discontinued due to the physical distancing COVID-19 measures. The sample size in NYC was n = 193 and n = 77 in LA. The original design of the study aimed for a minimum sample of 100 interviews per city, which was estimated based on demographic information provided by the Consulates.
Participants were subsequently matched through their zip codes of residence with COVID-19 morbidity and mortality data from LA and NYC to examine the burden of disease using a geospatial description. To build the NYC maps, we first matched the reported zip codes, neighborhoods and counties to the list of modified zip codes (ZCTA) of NYC counties and to a shapefile [25]. Then we matched the COVID-19 county-level data in NYC generated by the NYC Department of Health and Mental Hygiene1 [26]. We followed a similar process to build the LA maps. We matched the reported zip codes from the survey to a California list of zip codes [27] and then to the County of Los Angeles’ zip code2 and city/community classification [28]. Then we matched zip codes to COVID-19 cases and deaths in each city/community reported by the Los Angeles County Department of Public Health [29]. We used age-adjusted rates per 100,000 population to account for differences in the distribution of age in the underlying population. For both cities we used two cut-off dates, August 10, 2020 and January 17, 2021.
To link our analysis of vulnerabilities among Mexican immigrants to their experiences during the COVID19 pandemic, we conducted semi-structured key informant interviews (KII) (n = 4). We selected the personnel directly responsible of the COVID-19 response from the VDS in the Consulates in both cities during October 2020. The purpose of the interviews was to gain a closer understanding of the VDS role during the pandemic and to document the type of culturally appropriate services offered and how operations were adapted during the pandemic. These KII were also useful to document the systemic factor barriers faced by low-income Mexican immigrants during the pandemic (i.e. access to health care, distrust in health systems, fear of “public charge”) and to validate the sample and some of the key findings from the geospatial analysis. The interview guide is available in Spanish in the supplementary material.
Measures
Measures of Health Status
Consistent with prior studies [30], we collected self-reported health status and coded it as a three-level categorical variable (excellent and very good, good health, and fair or bad health). As previously published research suggests, poor self-rated health can be a predictor of mortality [31] and of pathological changes prior to disease diagnosis [32]. In addition, we collected data on 7 self-reported health problems; diabetes, hypertension, heart disease, asthma or bronchitis, cancer, depression, and arthritis, which have been established as some of the main morbidity causes among the study population [33]. Survey respondents were asked if a physician or another medical professional diagnosed any of the listed conditions. Dichotomous variables were generated for each condition, and favorable responses were added into a variable with values ranging from 0 to 7.
Measures of Healthcare Access and Utilization
A large body of empirical research highlights the effect of health insurance on access to and use of health care [12–14]. Hence, participants were asked if they had health insurance coverage in the U.S.. Participants were also asked how frequently they had received non-urgent health care during the last 6 months. Responses were coded in a Likert-scale (i.e. never, sometimes, usually, always, not required). These are common proxy measures that are generally used when studying vulnerable populations [34].
Social Capital
We used four items as proxies of social capital, each scored with Likert-type responses: “I can trust most people in my community”, “I can get help from my neighbors whenever I need it”, and “I feel safe when I walk alone at night in my community” (strongly agree [4] to strongly disagree [1]), and a rating of neighborhood perceived safety (very secure [4] to very insecure [1]). These measures have been used in prior studies [35, 36] as they have been found to be associated with adverse health outcomes and health care underuse among vulnerable populations [37–39]. We added the responses to each of these measures to generate an overall score of individual subjective perception of trust and safety ranging between 4 and 16; the higher the score, the greater the individual´s social capital.
Employment
Employment status was elicited from participants (i.e., not working, working, looking for a job), and among those working we inquired about their type of job. Through a qualitative coding we then assessed if it matched the classification of an essential worker during the pandemic, as defined by the U.S. Department of Homeland Security [18], which in May 19, 2020, issued an advisory memorandum with a list of workers who are essential to continue with critical infrastructure viability, working construction, operational functions, and support of crucial supply chains. Per this document, essential workers included health sector workers (including the ones providing eldercare); workers in laundromats, laundry services, and dry cleaners; workers from the construction sector (including technicians in maintenance of buildings, hospitals and residences); food and agriculture workers, restaurant and quick serve food operations (including dark kitchen and food prep-centers, carryout, and delivery food workers [18]. This list is non-exhaustive nor exclusive.
Sociodemographic Characteristics
Sociodemographic characteristics collected during the survey included age, gender, educational attainment, years of U.S. residence, and food insecurity collected through the Latin American and Caribbean Food Security Scale (ELCSA) to classify households by food security status (food secure, mild, moderate or severe food insecurity) [40].
Place of Residence
To ascertain migrants’ area of residence, respondents provided their zip code.
Analysis
Data from our survey was used for a comparison of means analysis between NYC and LA including: health-related variables, health care access, social capital, employment and sociodemographic characteristics. We used Fisher exact test for categorial variables and Mann–Whitney test for non-normally distributed data. All statistical analyses were performed with Stata 15 [41].
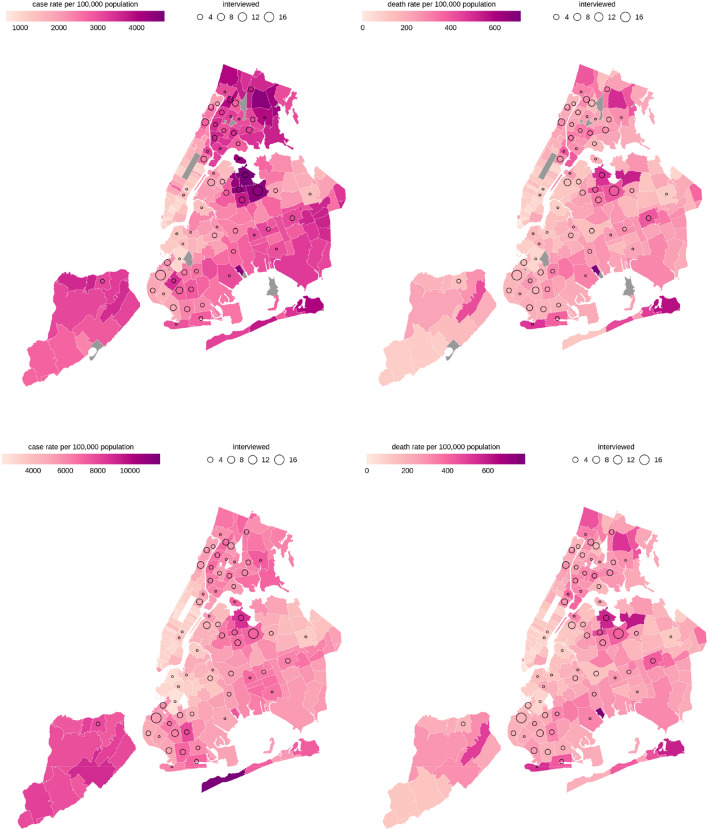
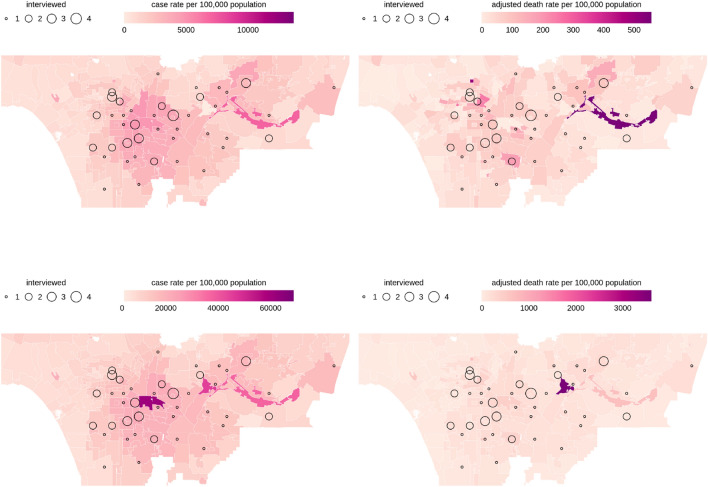
For the geospatial analysis, we mapped the participant’s area of residence based on their reported zip code and merged this information with age-adjusted COVID-19 morbidity and mortality. The spatial analysis consisted of joining two map layers: first, from the adjusted COVID-19 morbidity and mortality –where darker shades of pink denote higher cases by 100,000 inhabitants–, with self-reported place of residence. Larger bubbles indicate more survey participants live in the zip code. The geographic analysis was conducted with the “sf” package in R software [42, 43].
The qualitative semi-structure KII were analyzed using content analysis. An initial codebook followed the objectives of the interviews. Two separate researchers coded the qualitative material and contrasted the nodes and its content. We collapsed similar nodes and edited some remarks to facilitate the communication of the results. We kept the responses by city to highlight the similarities in all nodes. This study was reviewed and approved by the Research Ethics Committee at Universidad Iberoamericana, and was reviewed and given exempt status by the IRB at UCLA.
Results
Table 1 summarizes the characteristics of Mexican migrants who participated in the NYC and LA surveys. They were on average 40 years old and those interviewed in NYC had lived in the US for approximately 17 years, while individuals in LA reported an average of 23 years. In both cities most participants were employed at the time of the interview (75% in NYC and 79% in LA), however, a larger share of NYC respondents was classified into “essential work” activities compared to respondents in LA (47% to 31%, respectively). On average, migrants had low educational attainment, with about one third of respondents not completing middle school. Despite being a young sample overall, close to half of the respondents in NYC and about one third in LA reported a fair or bad health status. However, they reported less than one diagnosed comorbidity on average (0.59 in NYC and 0.57 in LA). The prevalence of previously diagnosed T2D was high in both cities, 11.4% in NYC and 11.7% in LA, slightly higher compared to the prevalence of diagnosed T2D reported by the CDC in 2020 among Hispanics, 10.3% [44].
Table 1.
Descriptive characteristics of a sample of Hispanic immigrants and stratified by city
| Variables | Total n = 270 | NYC (n = 193) | LA (n = 77) | p-value |
|---|---|---|---|---|
| Demographic variables | ||||
| Mean age (years) (s.d) | 40.51% (11.3) | 39.19(10.75) | 43.79(12.03) | 0.0034 |
| Mean length of residence in the U.S., (years) (s.d) | 18.95 (9.37) | 17.44 (8.22) | 22.82 (10.95) | 0.000 |
| Sex, % (n) | 0.588 | |||
| Male | 42.75% (115) | 56.47% (144) | 45.45% (35) | |
| Female | 57.25% (154) | 43.53% (111) | 54.55% (42) | |
| Employment status, % (n) | 0.847 | |||
| Not working | 18.15% (49) | 18.65% (36) | 16.88% (13) | |
| Working | 76.67% (207) | 75.65% (146) | 79.22% (61) | |
| Looking for a job | 5.19% (14) | 5.7% (11) | 3.90% (3) | |
| Type of worker, % (n) | 0.044 | |||
| Non-essential worker | 57.5% (115) | 52.86% (74) | 68.33% (41) | |
| Essential worker | 42.5% (85) | 47.14% (66) | 31.67% (19) | |
| Education, % (n) | 0.86 | |||
| No education/primary/incomplete middle | 34.94% (94) | 37.5% (72) | 28.57% (22) | |
| Middle/incomplete high school | 32.34% (87) | 33.85% (65) | 28.57% (22) | |
| Highschool/Higher any or technical career | 32.71% (88) | 28.65% (55) | 42.86% (33) | |
| Health status | ||||
| Self-reported health status, % (n) | 0.003 | |||
| Fair or bad | 45.11% (120) | 49.74% (94) | 33.77% (26) | |
| Good | 36.09% (96) | 36.51% (69) | 35.06% (27) | |
| Excellent or very good | 18.8% (50) | 13.76% (26) | 31.17% (24) | |
| Number of diagnosed comorbidities, mean, (s.d) | 0.59 (0.86) | 0.59 (0.82) | 0.57 (0.93) | 0.416 |
| Diagnosed comorbidities, % (n) | ||||
| Diabetes | 11.48% (31) | 11.4% (22) | 11.69% (9) | 1.00 |
| Hypertension | 10.74% (29) | 11.92% (23) | 7.79% (6) | 0.389 |
| Depression | 7.04% (19) | 6.74% (13) | 7.79% (6) | 0.794 |
| Other | 27.04% (73) | 26.94% (52) | 27.27% (21) | 1.00 |
| Healthcare access and utilization | ||||
| Has valid health insurance in the U.S., % (n) | 0.493 | |||
| No | 56.93% (152) | 58.33% (112) | 53.33% (40) | |
| Yes | 43.07% (115) | 41.67% (80) | 46.67% (35) | |
| Frequency of visits for regular medical care when needed in the last 6 months, % (n) | 0.022 | |||
| Never | 29.15% (72) | 30.73% (59) | 23.64% (13) | |
| Sometimes | 19.43% (48) | 20.83% (40) | 14.55% (8) | |
| Usually | 12.55% (31) | 14.58% (28) | 5.45% (3) | |
| Always | 38.87% (96) | 33.85% (65) | 56.36% (31) | |
| Contextual variables | ||||
| Household food security scale (ELCSA), % (n) | 0.464 | |||
| Food secure | 74.23% (193) | 74.32% (136) | 74.03% (57) | |
| Mild food insecurity | 19.62% (51) | 20.77% (38) | 16.88% (13) | |
| Moderate food insecurity | 3.85% (10) | 2.73% (5) | 6.49% (5) | |
| Severe food insecurity | 2.31% (6) | 2.19% (4) | 2.60% (2) | |
| Mean score of trust and safety (s.d) | 12.06 (3.09) | 11.97 (3.06) | 12.26 (3.15) | 0.43 |
Fisher exact test for categorial variables and Mann–Whitney test for non-normally distributed data
Source: Data collected by authors
Almost half of our survey respondents recounted that they never or only sometimes got regular non-urgent care in the last 6 months. While it reached 51.5% in NYC, in LA this proportion was significantly lower (38%), although still inadequate. A consistent vulnerability across both cities was food insecurity. Around one quarter of the respondents reported some level of food insecurity: 19.6% reported mild insecurity, 3.8% moderate, and 2.3% severe food insecurity. This is a high proportion compared to estimates from the U.S. Department of Agriculture [45], which reported that 10.5% of all U.S. households and 15.6% of Hispanic households were food insecure in 2019. The social capital score, which accounts for subjective perceptions of trust and safety, was around 12 in both cities, indicating a moderate response.
Place of residence is a source of inequity in COVID-19 morbidity and mortality. Thus, we used zip code data provided by survey respondents to map their neighborhoods of residence using morbidity and mortality adjusted data at two different time points. Figure 1 corresponds to NYC and Fig. 2 to LA. The top panels show morbidity and mortality COVID-19 rates per 100,000 population in both cities up to August 2020, while the lower panels show the same information updated to January 2021. In the second morbidity map, the scale varies, as testing increased, and more cases were added. The Consulates’ personnel validated both samples with expressions like “good sample”, “it is very well represented”, “coincides with the strongest outbreaks” and were able to pinpoint where Mexican immigrants live and where the pandemic struck.
Fig. 1.
COVID-19 morbidity and mortality by zip code of residence of Mexican immigrants in New York City (August 2020 and January 2021)
Fig. 2.
COVID-19 morbidity and mortality by zip code of residence of Mexican immigrants in Los Angeles (August 2020 and January 2021)
Across the NYC maps, the circles show a consistent pattern of higher COVID-19 case and mortality rates in the zip codes where Mexican immigrants lived. Some specific clusters in each of the boroughs can be identified. In Manhattan a cluster is visible in the east Harlem and Washington Heights. In the Bronx the morbidity trends concentrate in areas such as Soundview, Morrisiana, and Morris and University Heights. In Queens, the area comprised of the neighborhoods of Jackson Heights, Corona and Elmhurst, is a particularly worrisome cluster for Mexican immigrants due to persistent higher rates of morbidity and mortality. In Brooklyn we observed a cluster around Sunset Park and Greenwood Heights, although more concerning in terms of morbidity than mortality. Finally, in Staten Island, a point in the neighborhood of Port Richmond shows high rates of cases in the two time periods.
Figure 2 zooms into the central and southern region of LA country. Most respondents were clustered in the East Los Angeles, Vernon Central and in Miracle Mile-La Brea. LA portrays a similar pattern compared to NYC, as respondents resided in areas with high COVID-19 morbidity and mortality. The bottom left panel shows that the City of Vernon had the county’s highest case rate. Over 10% of survey respondents lived close to this area. Like NYC, cases and deaths were concentrated in areas with lower income, i.e., closer to the east, portraying a geographical disparity.
We interviewed key informants from the VDS to triangulate our findings, examine system factors faced by Mexican immigrants and discuss their response to the COVID-19 pandemic in both cities. The summary of the key themes that emerged is available in Table 2. The VDS in NYC and LA confirmed that the Mexican immigrant population they serve is mostly employed in low-wage and front-line jobs in activities classified as “essential services” (i.e., “farming”, “transportation”, supermarkets”, “restaurants”, and “deliveries”). Importantly, they explained that Mexican immigrants were highly exposed to the COVID19 virus through their jobs, often working without protective gear, fearing losing their jobs if they complained about their working conditions. An informant summarized the increased risk as a combination of “the economic needs and misinformation, the language barrier, they don’t know how to keep protecting themselves, and believing that taking one aspirin will keep fever away”. Both cities provided free testing and emergency insurance during the pandemic, however, health care use was restrained due to mistrust in the health system and concerns over the use of personal data. The constant fear of generating a “public charge”, even if unwarranted, was a key obstacle [46]. In NYC, for example, some eligible individuals refrained from accepting the economic support for restaurant employees.
Table 2.
Golden quotes from in depth interviews with key informants from Los Angeles and New York City
| Theme | New York City | Los Angeles |
|---|---|---|
| Types of employment of population served by the Mexican consulates | The problem with our population is that the industries of construction, restaurant, deliveries and the jobs of the Mexicans here, did not suspend and worked when the contagion was at the highest. They really were the ones who kept the City going | Here the majority of the population works in services; supermarkets, transport, and everything that has to do with the food chain. In other counties, like Ventura, 95% work on farms because it is a very rural area; we are definitely in the essential sectors |
| Exposure associated with essential workers | The risk they were exposed to was when they were working at the supermarkets or delivering food without the adequate protection, even feeling sick, they didn’t stop working because they couldn’t. The fact that they are more exposed is linked with the economic needs and misinformation, the language barrier, they don’t know how to keep protecting themselves, and believing that taking one Aspirin will keep fever away | Unfortunately, our community can’t give the luxury to stop working. The sick and diagnosed person has to do it, but with the risk of losing his job. Many have informal employment and reactions are diverse. They are those who keep working with their relatives sick in the next bed and also the proper sick person who can’t have the privilege to isolate himself |
| Access to health services | The emergency was paid to people with COVID, but many of them thought they had to pay and didn’t seek care. We explained that emergency Medicaid would be activated. To all the people with COVID who entered at hospitals we applied the emergency Medicaid and the state of NY and Trump care paid for it. The problem now is that COVID health consequences aren’t being paid | Here the option is My Health LA, and in case that you’re not eligible, there’s the community clinic, the cost of healthcare is really low and they provide basic healthcare services. Specifically, for COVID, the test is free for people without health insurance. For intensive hospitalizations they use emergency MediCal, which has financial consequences for the family |
| Distrust in health system | They think they have no rights, they believe access to healthcare can mark their immigration status. The pandemic was so big that you needed to survive, to eat. People had to go to the hospital or they would die. It was really important to highlight that going for food didn’t breach a health burden. The fear existed but the need was bigger | Many times, people are afraid even to receive a service; if they have to fill out forms, they ask us “where is this going?” and we tell them that their information is completely private, but there is always the fear about who has access to it, and that it may be a deportation cause |
| Fear of generating “public charge” | Yes, there were special programs and financial aid; the restaurants and rental costs were important. The problem is that they don’t ask for this back up for fear that it could generate future problems. We announced the NY students’ card and the questions were about public charge or the consequences of taking it | The fear is much greater with the pandemic because they know that there will be unaffordable medical costs. And they fear they’re gonna be a public charge. Even though the person could only become a public charge with specific medical coverage and certain programs for which they are not eligible due to their immigration status, the fear is always there |
| VDS as a key source of trusted information | We went from face-to-face to a permanent telephone service, a 24/7 number was set up for any health issue. Then the COVID resource guide for the community was made; they were receiving information in Spanish verified by people from the consulate, in which they could see where to find food and the different measures to take. They were also helped to find funeral homes, when they reached the limit and were no longer serving. We use Facebook a lot; now we do seminars and online talks to improve health. The challenge comes to re-explain how to access services, explain navigation in the health system and that they do have access, and integrate telemedicine | We replaced normal activities with more presence on social media, educating the community about different programs to keep them afloat during the pandemic. We focus on COVID-19 symptoms, where to go, where to get tested, and everything related to that topic. People could contact the consulate with very specific questions. They had endless needs that showed up, we helped by giving information about county programs; how to access health coverage, how to find out where the nearest food bank was, how to apply for unemployment insurance, etc. Now we are doing other kind of workshops, such as nutrition, how effective telemedicine is and much more |
| Emergency support from VDS | The mobile service window is doing COVID tests and influenza vaccination days. They keep with pantry deliveries, they were the first. The pantries, the food, were the basic needs. And we partner to have tests on community centers or churches. Many of the VDS partners stayed on and gave us the details to work online or by phone. What we did was have clinicians, two doctors and two nurses, who spoke to people to see their health problem and then made the corresponding referral, to a primary health service in person or with allies that we know, whether to receive medical service or for COVID | A COVID test center opened at the consulate with a capacity for 1400 tests by week; people considered it a safe space, they know they can come without appointment, because it’s an obstacle that people don’t know how to schedule one, not even online and other processes aren’t user-friendly. We also start doing influenza vaccination days. And we have been distributing COVID-19 protective equipment to peddlers in the area for two weeks. Besides, we do medical advisory services through appointments |
| Mental health needs and support | We interviewed people with the VDS system about their emotional status, and we basically found anxiety, stress, fear, sadness and depression. And the part of domestic violence, which the city has detached a lot. Access to mental health in your language has been a very important challenge, in addition to breaking the myth that exists “I'm not bad, I don’t need to.” The line to make referrals in health services was opened and calls to relatives of the deceased were increased to provide emotional support directly; it was a volunteer program. It wasn’t exactly a line of support; we put them in contact with a shrink who can follow up with them. The major advantage is that it was direct, in Spanish, and delivered by culturally appropriate staff | We began to have virtual workshops about the impact of the pandemic on the emotional well-being of the community, which consisted of giving them tools to get through those difficult times that they had to be at home with their children, often without work. Then we went with other closely related issues that we knew were going to increase, such as loss and grief, family violence, suicide prevention, alcohol, and substance use. And about stigma because in the community there was a lot of stigma around mental health. The LA County Department of Mental Health has lines in Spanish and English that, right now, due to the pandemic, were activated 24/7 days a week; not just for crisis cases, but for people who are experiencing anxiety or stress, or who just want to talk |
| Maps’ validation | Where Mexicans live it seems to me a good sample. Where the circles are, there is a larger Mexican population. And yes, it really is how we are distributed, they are well located, which is the south of the Bronx, Corona, Queens, Sunset Park, Staten island, which are the areas where the community is and where there were more cases. Staten Island is the zone, not by quantity but by presence. I think there could be more population there, the Port Richmond area. It was a very good sample, it does coincide, also was where the strongest outbreaks were seen | All of Los Angeles County is full of Mexicans, but I believe that most of them are concentrated in the southern area and I think that it is very well represented with what you show us. It reveals the situation we are discussing. It's most likely the central and south-southeast area of Los Angeles, the cities where we have the largest Hispanic population, also where there are more productive plants. In that area are the cities of Commerce, Industry, Huntington Park, in all those cities there is a lot of Mexican population and there are also many food manufacturing companies, a large part of the companies has plants there, so it makes sense to us what you are saying |
VDS Ventanillas de Salud (Health Windows)
The VDS had a vital role in the response to the COVID-19 pandemic. This health outreach program provided information about the virus, testing, how to navigate the health system if symptoms appeared and referred relatives to consular services for funeral arrangements and repatriation of remains. They were able to convert most of their services to telephone and online modalities– both the physical site and the mobile consulate. VDS became a reliable, trusted, and accessible source of information for migrants, ranging from basic explanations of transmission mechanisms and protective measures to specialized information such as health care eligibility and economic support. Moreover, VDS provided direct services like free COVID-19 testing, influenza vaccination, and health information. At a critical point of economic inactivity, they became food pantries, which underscores food insecurity as a critical need. In addition, the VDS helped identify anxiety, depression, grief, and domestic violence as serious consequences of the lockdown measures and were able to connect users with Spanish-speaking mental health providers.
Discussion
In this study we sought to complement existing literature that has documented the impact of COVID-19 on the Hispanic community as a high-risk population [2, 3, 6]. Our study used three different data sources to investigate individual, systems and area levels of vulnerability faced by low-income Mexican immigrants during the COVID-19 pandemic. We used primary data to assess pre-pandemic vulnerabilities among Mexican immigrants in NYC and LA. From our survey data, we observed statistically significant differences between cities in terms of age, proportion of essential workers, which was above 30% in both cities, health status, health care utilization and average length of residence in the U.S. Despite these differences, we identified some commonalities: (i) study participants had a high share of uninsured individuals that exceeded the uninsured rates in California and NY (9% and 6.2% respectively) [47]. (ii) Vulnerability factors were low health care access, high food insecurity [48], and high T2D diagnoses [49], with a prevalence higher than the U.S. and Mexican prevalence, in spite of respondents’ young average age.
These pre-COVID vulnerabilities partially result from health and migratory polices that limit immigrants’ access to health care, constrain health insurance options [25], and alienate them from the health system through lack of eligibility, fear of detention, deportation, and public charge [20, 50]. In addition, social determinants of health faced by low-income Mexican immigrants such as residential segregation, overcrowded housing, and exposure to food deserts, could contribute to health conditions such as obesity and overweight, T2D and related comorbidities that might explain why, despite having a young sample (of about 40 years), self-reported health status was overwhelmingly poor. Low-income Mexican immigrants are particularly vulnerable to unfavorable area-level social determinants of health [17, 51].
Our study showed a close correspondence between area-level COVID-19 morbidity and mortality rates with respondents’ zip codes of residence. The geospatial distribution of Mexican immigrants places them in areas of residence with disproportionally high COVID-19 cases and deaths. Our findings are consistent with previous research [1, 2, 4, 52], and with the narrative described in our KII. In addition to access to care barriers, occupation emerged as a key risk factor. In our sample, a large share of the migrants, had a job that placed them at higher risk of infection, as were customer-facing occupations and sectors that did not allow for remote work. This has been previously highlighted [8, 15] and also emerged as a central topic when interviewing key informants.
Three important lessons emerge from this research. First, the study confirmed the vulnerability of Mexican immigrants in terms of limited access to health care and health insurance, and low self-reported health status especially considering their average age. Mexican immigrants contribute to the NYC and LA local economies and are disproportionately employed in low-wage essential services [17]. Despite their contribution, they are fearful of deportation and somehow distrustful of their communities [20]. Second, our study underscores the importance of understanding how such vulnerabilities transform into challenges for reaching low-income and noncitizen migrants with low or non-English fluency during the pandemic. Reaching these populations requires trusted and culturally sensitive navigation resources to facilitate access to COVID-19 testing, treatment, and vaccination, as well as prevention services of common side effects of the pandemic such as mental health conditions and increased food insecurity. Our research shows the importance of VDS at the onset of the pandemic. Through a rapid adaption response in NYC and LA, VDS were able to offer culturally tailored information about COVID-19 and remote clinical assessments of symptoms with the aid of health professionals. They also helped immigrants to navigate administrative services; verify in Spanish information received; explain how to access health services during the pandemic including telemedicine, testing and vaccination sites; and access local government support programs and food pantries [53]. The use of social media (i.e. Facebook) was fundamental in the adaptation of such services.
The Mexican government should continue to invest and expand this health outreach programs that are closely coordinated with local U.S. health care providers, U.S. governments (federal, state, local), health care providers, stakeholders, and advocates [54]. Lastly, vulnerable communities should not be stigmatized for having higher rates of infection and mortality. Such outcomes are driven by structural inequalities and area-level social determinants of health which are manifest, amongst others, through residential segregation [55].
Among our limitations are statistical representation, including sample size, and potential self-selection into Consular visits. However, we aim to describe, not to make causal claims. The external validity of our study findings is also limited, since our findings apply to low-income Mexican migrants from two large U.S. metropolitan areas labeled as “sanctuary cities”. Foreign-born migrants from other countries, those working in rural areas, or in smaller cities and towns in non-sanctuary cities or states are not represented in this study. Two important strengths of our study are the triangulation of three different data sources to show the different levels of vulnerability faced by low-income Mexican immigrants to COVID-19. Moreover, we worked with Mexican interviewers from within the Mexican Consulates, which have the trust of migrants regardless of their legal status. Likewise, we obtained relevant information about the ongoing challenges that this population has faced during the pandemic, through our KII with the front-line consular officers of VDS that have provided a culturally appropriate health information and navigation resources. Further studies would benefit from including the perspectives of the staff in the Consulates performing other tasks, the organizations supporting the VDS, and the users of VDS. In addition, while the KII helped triangulating the other sources of data, it would be beneficial to have a more detailed description of the adaptations and services provided by the VDS during the pandemic through an implementation science perspective.
Conclusions
In this study we analyze individual, area-level and systemic levels of vulnerability faced by low-income Mexican immigrants during the COVID-19 pandemic. We argued that prior vulnerabilities linked to immigration such as type of employment, food insecurity status, chronic conditions, health status, and access to care barriers, placed low-income Mexican immigrants at higher risk of COVID-19. Our study shows a close correspondence between the zip codes where respondents lived with areas disproportionately affected by COVID-19 morbidity and mortality in both cities. These findings suggest unfavorable area-level social determinants of health that reinforce the pre-Covid-19 individual and systemic vulnerabilities faced by the study population. Health outreach programs such as VDS have been key to disseminate information about the virus, testing, health care navigation, and handling of the deceased. The VDS model may be used by other countries as a blueprint for community outreach and eventually as a network to expand health care access and promote healthy lifestyles nationwide [22]. Further investments in culturally appropriate programs and coordination with local health care providers, advocates and stakeholders is needed to reduce health disparities.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We acknowledge the valuable contribution of Isabel Ferré and Annel Lozano-Marrufo for their contributions in coordinating the field work, David Tamayo for his support in the data management, Wilfrido A. Gómez Arias for his support in the geospatial analysis, and the Mexican General Consulates in New York City, NY and Los Angeles, CA.
Funding
UC-Mexus.
Footnotes
The Health Department classifies the start of the outbreak in NYC as the date of the first laboratory-confirmed case, February 29, 2020.
Zip code boundaries and names are established by the U.S. Postal Service (USPS). Zip code boundaries do not necessarily follow established municipal, community, and other district boundaries. Therefore, while a zip code name usually reflects the municipality or community that predominates that area, it does not necessarily coincide entirely with the established municipal, community, or other district boundaries. Thus, a zip code name may include parts of other communities and/or districts not reflective of its name. Moreover, the sum of counts by modified zip codes may not match values in Citywide tables because of records with missing geographic information.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Neelon B, Mutiso F, Mueller NT, Pearce JL, Benjamin-Neelon SE. Spatial and temporal trends in social vulnerability and COVID-19 incidence and death rates in the United States. medRxiv. 2020;47:37. doi: 10.1371/journal.pone.0248702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strully K, Yang T-C, Liu H. Regional variation in COVID-19 disparities: connections with immigrant and Latinx communities in US counties. Ann Epidemiol. 2021;53:56–62. doi: 10.1016/j.annepidem.2020.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karmakar M, Lantz PM, Tipirneni R. Association of social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Netw Open. 2021;4(1):e2036462. doi: 10.1001/jamanetworkopen.2020.36462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodriguez-Diaz CE, Guilamo-Ramos V, Mena L, Hall E, Honermann B, Crowley JS, et al. Risk for COVID-19 infection and death among Latinos in the United States: examining heterogeneity in transmission dynamics. Ann Epidemiol. 2020;52:46–53. doi: 10.1016/j.annepidem.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Macias Gil R, Marcelin JR, Zuniga-Blanco B, Marquez C, Mathew T, Piggott DA. COVID-19 pandemic: disparate health impact on the Hispanic/Latinx population in the United States. J Infect Dis. 2020;222(10):1592–1595. doi: 10.1093/infdis/jiaa474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogedegbe G, Ravenell J, Adhikari S, Butler M, Cook T, Francois F, et al. Assessment of racial/ethnic disparities in hospitalization and mortality in patients with COVID-19 in New York City. JAMA Netw Open. 2020;3(12):e2026881. doi: 10.1001/jamanetworkopen.2020.26881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arias E, Tejada-Vera B, Ahmad F. Vital statistics rapid release: provisional life expectancy estimates for January through June, 2020. CDC Vital Stat Rapid Release. 2021 doi: 10.15620/cdc:100392. [DOI] [Google Scholar]
- 8.Hooper MW, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perez-Escamilla R, Garcia J, Song D. Health care access among Hispanic immigrants: ¿Alguien Esta Escuchando? [Is anybody listening?] NAPA Bull. 2010;34(1):47–67. doi: 10.1111/j.1556-4797.2010.01051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bureau USC. Health insurance: tables 2018- forward. Health insurance coverage in 2019. 2019.
- 11.Vargas Bustamante A, Fang H, Garza J, Carter-Pokras O, Wallace SP, Rizzo JA, et al. Variations in healthcare access and utilization among Mexican immigrants: the role of documentation status. J Immigr Minor Health. 2012;14(1):146–155. doi: 10.1007/s10903-010-9406-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bustamante AV, Chen J, McKenna RM, Ortega AN. Health care access and utilization among US immigrants before and after the affordable care act. J Immigr Minor Health. 2018;21:211–218. doi: 10.1007/s10903-018-0741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bustamante AV, McKenna RM, Viana J, Ortega AN, Chen J. Access-to-care differences between Mexican-heritage and other Latinos in California after the affordable care act. Health Aff. 2018;37(9):1400–1408. doi: 10.1377/hlthaff.2018.0416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bustamante AV, Chen J, Felix Beltran L, Ortega AN. Health policy challenges posed by shifting demographics and health trends among immigrants to the United States. Health Aff. 2021;40(7):1028–1037. doi: 10.1377/hlthaff.2021.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Solis J, Franco-Paredes C, Henao-Martínez AF, Krsak M, Zimmer SM. Structural vulnerability in the US revealed in three waves of COVID-19. Am J Trop Med Hyg. 2020;103(1):25–27. doi: 10.4269/ajtmh.20-0391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ross J, Diaz CM, Starrels JL. The disproportionate burden of COVID-19 for immigrants in the Bronx, New York. JAMA Intern Med. 2020;180(8):1043–1044. doi: 10.1001/jamainternmed.2020.2131. [DOI] [PubMed] [Google Scholar]
- 17.Martinez L, Bustamante AV, Balderas-Medina Y, Dominguez R, Diaz S, Hayes-Bautista D. COVID-19 in vulnerable communities: an examiniation by race & ethnicity in Los Angeles and New York City. CA: UCLA Latino Policy & Politics Initiative; 2020. [Google Scholar]
- 18.Krebs C. Advisory memorandum on identification of essential critical infrastructure workers during Covid-19 response. Washington: United States Department of Homeland Security; 2020. [Google Scholar]
- 19.Brenes F. Immigrants and the right to health care in the era of COVID-19. Hisp Health Care Int. 2020;18(4):178–179. doi: 10.1177/1540415320958614. [DOI] [PubMed] [Google Scholar]
- 20.Guerrero A, Felix L, Dominguez R, Bustamante AV. Foregoing healthcare in a global pandemic: the chilling effects of the public charge rule on health access among children in California. Los Angeles: UCLA Latino Policy & Politics Initiative; 2021. [Google Scholar]
- 21.Flores-Yeffal NY. English proficiency and trust networks among undocumented Mexican migrants. Ann Am Acad Pol Soc Sci. 2019;684(1):105–119. [Google Scholar]
- 22.Vilar-Compte M, Bustamante AV, Lopez-Olmedo N, Gaitan-Rossi P, Torres J, Peterson KE, et al. Migration as a determinant of childhood obesity in the United States and Latin America. Obes Rev. 2021;22:e13240. doi: 10.1111/obr.13240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bustamante AV, Vilar-Compte M, Lagunas AO. Social support and chronic disease management among older adults of Mexican heritage: a US-Mexico perspective. Soc Sci Med. 2018;216:107–113. doi: 10.1016/j.socscimed.2018.09.025. [DOI] [PubMed] [Google Scholar]
- 24.Vilar-Compte M, Macinko J, Weitzman BC, Avendaño-Villela CM. Short relative leg length is associated with overweight and obesity in Mexican immigrant women. Int J Equity Health. 2019;18(1):103. doi: 10.1186/s12939-019-0988-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Data NO. Housing & development: shapefile of footprint outlines of buildings in New York City 2020. https://data.cityofnewyork.us/Housing-Development/Shapefiles-and-base-map/2k7f-6s2k. Accessed 2 Feb 2021.
- 26.Health N. COVID-19 data by zip code 2021. https://www1.nyc.gov/site/doh/covid/covid-19-data-totals.page#zip. Accessed 1 Feb 2021.
- 27.Codes USZ. ZIP codes in California 2021. https://www.unitedstateszipcodes.org/ca/#zips-list. Accessed 2 Feb 2021.
- 28.LA Co. Master zip codes 2021. https://lacounty.gov/government/geography-statistics/zip-codes/. Accessed 2 Feb 2021.
- 29.County L. COVID-19 surveillance dashboard 2021. http://dashboard.publichealth.lacounty.gov/covid19_surveillance_dashboard/. Accessed 3 Feb 2021.
- 30.Miilunpalo S, Vuori I, Oja P, Pasanen M, Urponen H. Self-rated health status as a health measure: the predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. J Clin Epidemiol. 1997;50(5):517–528. doi: 10.1016/s0895-4356(97)00045-0. [DOI] [PubMed] [Google Scholar]
- 31.Burström B, Fredlund P. Self rated health: is it as good a predictor of subsequent mortality among adults in lower as well as in higher social classes? J Epidemiol Community Health. 2001;55(11):836–840. doi: 10.1136/jech.55.11.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stenholm S, Kivimäki M, Jylhä M, Kawachi I, Westerlund H, Pentti J, et al. Trajectories of self-rated health in the last 15 years of life by cause of death. Eur J Epidemiol. 2016;31(2):177–185. doi: 10.1007/s10654-015-0071-0. [DOI] [PubMed] [Google Scholar]
- 33.Greer S, Naidoo M, Hinterland K, Archer A, Lundy De La Cruz N, Crossa A, et al. Health of Latinos in New York City. New York City; 2017.
- 34.Hayes SL, Riley P, Radley DC, McCarthy D. Reducing racial and ethnic disparities in access to care: has the affordable care act made a difference? Issue Brief. 2017;2017:1–14. [PubMed] [Google Scholar]
- 35.Cain CL, Wallace SP, Ponce NA. Helpfulness, trust, and safety of neighborhoods: Social capital, household income, and self-reported health of older adults. Gerontologist. 2017;58(1):4–14. doi: 10.1093/geront/gnx145. [DOI] [PubMed] [Google Scholar]
- 36.Hoffman EE, Mair TT, Hunter BA, Prince DM, Tebes JK. Neighborhood sexual violence moderates women's perceived safety in urban neighborhoods. J Community Psychol. 2018;46(1):79–94. doi: 10.1002/jcop.21917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Assari S, Caldwell CH, Zimmerman MA. Perceived neighborhood safety during adolescence predicts subsequent deterioration of subjective health two decades later; gender differences in a racially-diverse sample. Int J Prev Med. 2015;6:117. doi: 10.4103/2008-7802.170431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stokes JE. Trajectories of perceived neighborhood quality across the life course: sociodemographic determinants and implications for well-being. Soc Sci Res. 2019;79:181–193. doi: 10.1016/j.ssresearch.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 39.Beyer KM, Malecki KM, Hoormann KA, Szabo A, Nattinger AB. Perceived neighborhood quality and cancer screening behavior: evidence from the survey of the health of Wisconsin. J Community Health. 2016;41(1):134–137. doi: 10.1007/s10900-015-0078-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pérez-Escamilla R, Vilar-Compte M, Gaitan-Rossi P. Why identifying households by degree of food insecurity matters for policymaking. Global Food Secur. 2020;26:100459. [Google Scholar]
- 41.StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC; 2017.
- 42.Pebesma EJ. Simple features for R: standardized support for spatial vector data. R J. 2018;10(1):439. [Google Scholar]
- 43.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2021. https://www.R-project.org/.
- 44.CDC. National diabetes statistcis report 2020. Estimates of diabetes and its burden in the United States. 2020. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed 2 Mar 2021.
- 45.USDA. Food security status of US households in 2019. 2019. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2019, ERR-275, U.S. Department of Agriculture, Economic Research Service. 2020.
- 46.Bustamante AV, Diaz S. Advancing health equity [Internet]. New York, NY: The commonwealth fund. 2021 [cited 2021]. Available from: https://www.commonwealthfund.org/blog/2021/can-changing-public-charge-rule-improve-health-and-lives-children. Accessed 15 Apr 2021.
- 47.Tolbert J, Orgera K, Damico A. Key facts about the uninsured population. California: KFF; 2020. [Google Scholar]
- 48.Payán DD, Rios KD, Ramírez AS, De Trinidad Young M-E. Structural barriers influencing food insecurity, malnutrition, and health among Latinas during and after COVID-19: considerations and recommendations. J Acad Nutr Diet. 2021;121:837–843. doi: 10.1016/j.jand.2021.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rosenthal N, Cao Z, Gundrum J, Sianis J, Safo S. Risk factors associated with in-hospital mortality in a US national sample of patients with COVID-19. JAMA Netw Open. 2020;3(12):e2029058. doi: 10.1001/jamanetworkopen.2020.29058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bernstein H, Gonzalez D, Karpman M, Zuckerman S. One in seven adults in immigrant families reported avoiding public benefit programs in 2018. Washington: Urban Institute; 2019. [Google Scholar]
- 51.Ingram E, Ledden S, Beardon S, Gomes M, Hogarth S, McDonald H, et al. Household and area-level social determinants of multimorbidity: a systematic review. J Epidemiol Community Health. 2021;75(3):232–241. doi: 10.1136/jech-2020-214691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bilal U, Barber S, Tabb LP, Diez-Roux AV. Spatial inequities in COVID-19 testing, positivity, confirmed cases and mortality in 3 US cities: an ecological study. medRxiv. 2021;80:10–34. doi: 10.7326/M20-3936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Balderas-Medina Y, Martinez LE, Bustamante AV, Diaz S, Hayes-Bautista D. Telehealth & COVID-19: policy considerations to improve access to care. Los Angeles: UCLA Latino Policy & Politics Initiative; 2020. [Google Scholar]
- 54.Dominguez-Villegas R, Bustamante AV. Health insurance coverage in Mexico among return migrants: differences between voluntary return migrants and deportees. Health Aff. 2021;40(7):1047–1055. doi: 10.1377/hlthaff.2021.00051. [DOI] [PubMed] [Google Scholar]
- 55.Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59(1):137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.