Abstract
Background and Aims
The Coronavirus disease 2019 (COVID‐19) pandemic globally changed the priorities of medical and surgical procedures. It has caused many healthcare systems to stop performing their routine screenings. Altering medical clinics to COVID‐19 referral centers, lockdowns, and the public fear to refer to medical centers caused a significant reduction in the referral rate; especially in the elderly. This short review article highlights the transform in clinical practice during the post‐COVID era and the need for future medical revolutions.
Methods
A comprehensive literature search was separately performed by both authors. The articles published between 2019 and August 2021 were included in this study and selected according to a quality appraisal method.
Results
We have summarized the possible corresponding changes in the diagnosis and treatment of all fields of medical care including internal medicine, surgical, and minor subcategories after the COVID‐19 pandemic. We have also discussed the potential impacts of the pandemic on all these different categories and subcategories of medicine, including the outpatient setting and clinical work. We do believe that the lack of routine check‐ups has led to an increase in the stage of disease in patients with a previously diagnosed problem. On the other hand, the dramatic change in the lifestyle of the population including restricted mobility and increased consumption of unhealthy food has caused metabolic syndrome and other new diseases that have not been diagnosed and properly managed.
Conclusion
Our findings revealed the urgent need for public health awareness. It indicated the need to carry out both psychological and screening approaches in the post‐COVID era to not miss patients with a chronic disease and new cases who were undiagnosed during the COVID pandemic.
Keywords: COVID‐19 pandemic, epidemiology, morbidity, SARS‐CoV‐2
1. INTRODUCTION
The Coronavirus disease 2019 (COVID‐19) pandemic as an unprecedented global crisis immediately affected healthcare services. Patients with COVID‐19 infection may initially suffer from flu‐like symptoms; however, nearly 50% to 75% of the subjects with positive PCR results may remain asymptomatic.1 However, the disease could be severe in some cases.2
The impact of COVID‐19 on the health care system has been dramatic as it had to undergo major changes such as postponement of elective surgeries and non‐urgent medical care, and acceptance of telehealth to achieve pandemic preparedness. Patients have had difficulty reaching the hospital through ambulances and those with a chronic disease would rather postpone their follow‐ups, outpatients' hospital activities were limited to urgent cases, and all scheduled activities were interrupted. As a result, telephonic consultations and messenger services were applied to not lose communication with patients. Despite all benefits of telemedicine during the COVID‐19 pandemic, the telemedical examination does not seem to be able to replace personal consultation fully. In addition, training programs have been affected by the COVID‐19 pandemic to the highest degree.3
In this review, we aimed to discuss the health system should have in mind the post‐pandemic care both in patients with a chronic disease and those healthy individuals who may confront a new undiagnosed disease.
2. METHODS
A systematic narrative review of research published between 2019 and August 2021 was performed. Keywords were selected for each subsection including internal medicine, surgical, and minor subcategories and used to search PubMed, Medline, and google scholar as reliable bibliographic databases. Results of each different subsection were then subject to review; using a quality appraisal method and the most related articles were selected. Accordingly, the titles and abstracts of the retrieved articles were screened and the full text of potentially relevant articles was printed and read by both authors.
2.1. COVID‐19 and cardiology
COVID‐19 is associated with myocarditis, myocardial ischemia, and abnormal host immune response, leading to arrhythmias.4, 5, 6 COVID‐19 can cause heart failure (HF) or even make it worse.6 Acute HF had a higher incidence among patients who did not survive.5 Older age may increase the risk of cardiovascular events leading to death.7 In a retrospective cohort study, cardiovascular‐associated death accounted for 5% of the 28 969 deaths and increased by 8%.8
Lockdowns and the fear to refer to healthcare centers prevented the identification of new patients as well as appropriate treatment of prior patients. This reduction in patient referrals overshadowed cardiac surgery training.9 There will be an increase in elective procedures and delayed elective procedures after the pandemic.10 Post‐MI complications will increase, which will potentially have a considerable effect on the healthcare economy, especially for developing countries.10, 11 (Figure 1).
FIGURE 1.
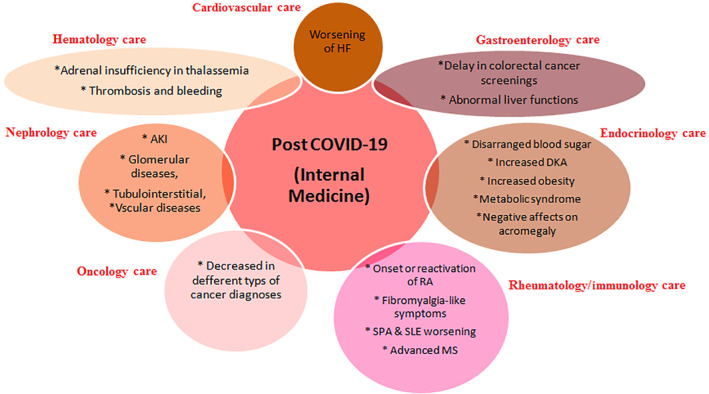
The consequences of COVID‐19 on internal medicine care after the pandemic
Pediatrics: Children often have cardiovascular involvement including myocardial dysfunction (MI), valvulitis, and coronary artery dilation or aneurysms.12 Pediatric and congenital heart disease (CHD) may cause an increased risk for severe MI.13
2.2. COVID‐19 and endocrinology
Physical activity has beneficial effects on blood sugar control. During the COVID‐19 period, social distance reduced physical activity and diet control, resulting in changes in glucose control, parallel to anxiety and sleep disturbance.14 In a retrospective study on gestational diabetes mellitus in France, there was a decrease in blood sugar control.15 As a result, this could lead to maternal and neonatal morbidity.15 While patient and society educations were focused on COVID‐19, maintaining regular education on other aspects of health, especially symptoms of diabetes, may be helpful to lower the prevalence of diabetic ketoacidosis (DKA).16
In terms of hypothyroidism, it has been reported in a recent study that compliance to levothyroxine treatment is decreased during the pandemic.17
After lockdown in Italy, there was a dramatic increase in obesity prevalence from 37% to 51%, metabolic syndrome from 14% to 27%, and dyslipidemia from 28% to 48%.18 In a survey among pituitary disease patients, delay or changes in planned care was observed in 64% of individuals.19
COVID‐19 negatively affected acromegaly care based on endocrinologists' respond.20 Moreover, there was an increase in delayed surgical procedures for acromegaly patients due to a lack of personal protective equipment and COVID‐19 testing provision.20 Additional effects of these delayed and impaired treatments are unknown, and researchers should focus on these impacts and implications. (Figure 1).
Pediatrics: COVID‐19 outbreak has been thought to modify type 1 diabetes management by the use of telemedicine; however, psychological aspects deserve attention in future researches.21 Interestingly, a cross‐sectional study revealed that the DKA rate has raised to 12% in children with more severe cases which may be attributed to changes in social limitations.16 Regelmann et al have confirmed the need for research assessing the impact of telemedicine on pediatric care outcomes.22
2.3. COVID‐19 and gastroenterology
COVID‐19 has caused several countries to suspend their colorectal cancer screenings.23 A study based on the UK national endoscopy database, including over 2.5 million records, showed an 88% decrease in endoscopy activities.24 Moreover, weekly cancer detection reduced to 58% compared to the pre‐COVID period; ranging from 19% (pancreaticobiliary cancers) to 72% (colorectal cancers).24 In another study in the Netherlands, gastroscopy activities declined by 57% and colonoscopies by 45%, with no change in the endoscopic retrograde cholangiopancreatography (ERCP) rate.25 In a survey among gastroenterologists in India, endoscopic training has decreased to 10% of its capacity.26 In addition, 98% of endoscopists in France had to cancel procedures, with a 91% decrease in procedures during this pandemic.27
COVID‐19 can be associated with abnormal liver functions due to viral infection in liver cells, drug toxicity, and systemic inflammation.28, 29 (Figure 1).
Pediatrics: Particular populations of children and adolescents may be at greater risk of COVID‐19 including those suffering from chronic liver disease.30 Children presented with gastrointestinal symptoms are found to be at higher risk of the need for pediatric intensive care unit (PICU) admission.31 Pediatrics are confronted with delays in the presentation of gastrointestinal problems and reduction in endoscopic studies have caused reduced opportunities for clinical and research training.32
2.4. COVID‐19 and hematology
A variety of hemogram parameters including the mean platelet volume, red cell distribution width (RDW), and neutrophil/lymphocyte ratio have been suggested to be increased in COVID‐19 patients.33 Patients with preexisting chronic morbidities such as those with hemoglobin disorders (sickle cell disease [SCD] or thalassemia) are expected to be more severely affected by COVID‐19.34, 35, 36
COVID‐19 infection may result in ICU admissions in older age and cases with lymphopenia, so that, these immunosuppressed patients may likely experience more significant morbidity and mortality and may require long‐term follow‐up.37 Inherited or acquired benign hematological disorders may increase the risk of developing severe complications from COVID‐19, so that changes to the usual treatment may be required in these patients.38 (Figure 1).
On the other hand, thrombosis and bleeding may occur as a consequence of COVID‐19, even in patients with no underlying disease. However, its severity is affected by age, coagulation profile, immobility state, and comorbidities.39 (Figure 1).
Pediatrics: Children with SCD are at an increased risk of Vaso‐occlusive crisis (VOC) and ACS with an increased need in blood requirement and intensive care unit admission.40
2.5. COVID‐19 and nephrology
In a study in the United States, 36% of COVID‐19 patients developed acute kidney injury (AKI), and 14.3% needed kidney replacement therapy.41 AKI incidence among hospitalized patients was higher in patients with COVID‐19 (56% vs 37.2%) and these patients needed kidney replacement therapy more than in other cases (4.6% vs 1.6%).42, 43, 44 Similar results were obtained in the study of Pei et al., showing a high frequency of renal abnormalities in COVID‐19 patients (75.4%), with 65.8% of them having proteinuria and 41.7% presenting hematuria.45
The direct influence of the SARS‐Cov2 in the renal damage or the innate and adaptive immune response activating cytokine and procoagulant cascades have been found to trigger glomerular diseases, principally collapsing focal segmental glomerulosclerosis, tubulointerstitial, and vascular diseases.46, 47 (Figure 1).
Pediatrics: Key areas of glomerular disease care in children that may be affected by the COVID‐19 pandemic include limitations in the clinic visit scheduling and provision of multidisciplinary care as well as restrictions in renal biopsy and patient education and support.48 AKI; caused by inflammatory storm and complement‐mediated injury, is prevalent in critically ill children with COVID‐19; especially in those with gastrointestinal symptoms.49 Rhabdomyolysis and AKI with no fever or respiratory symptoms were reported as the presenting symptoms of an adolescent affected with COVID‐19.50
2.6. COVID‐19 and oncology
According to the study of Bertuzzi et al, oncologic patients with COVID‐19 were older, had a higher neutrophil‐to‐lymphocyte ratio, fatality rate (1.92× risk of death), and were more commonly affected with diabetes, hypertension, coronary artery disease, and dyslipidemia.51
A notable decrease in cancer diagnoses was observed in the Netherlands after the chaos wreaked by the COVID‐19 outbreak.52 Similarly, a very steep decline was observed in breast cancer diagnoses among women aged 50 to 74 years. It remained lower than the expected number of diagnoses in the study of Dinmohamed et al.53 The results of another study on colorectal cancer screening programs in Australia, Canada, and the Netherlands revealed that short‐term disruption to colorectal cancer screening would have a noticeable impact on colorectal cancer incidence and deaths between 2020 and 2050.47 (Figure 1).
Pediatrics: Two‐thirds of the pediatric patients with cancer experienced treatment delays to the postponement of the planned treatment that was not caused by the complications of COVID‐19 infection.54 Ferrari et al suggest that no major adjustments are required in anticancer treatments of pediatric patients with no need to postpone it during the COVID‐19 pandemic.55
2.7. COVID‐19 and rheumatology/immunology
Rheumatic patients may fight back with the consequences of lengthened immobilization, lack of physiotherapy, consultations, and treatment adaption as well as depression caused by social isolation.56, 57, 58, 59 A recent survey performed on spondyloarthritis (SPA) patients, confirmed worsening of the disease and reduction or postponement of medication intake due to the home confinement linked to the COVID‐19 pandemic.60 The COVID‐19 outbreak had a significant effect on the psychological state of patients with systemic lupus erythematosus (SLE) with increased levels of stress, anxiety, and depression.61
Coronavirus may induce autoimmune diseases caused by a considerable increase in proinflammatory cytokines and chemokines in the infected person's serum.62 Accordingly, a virus‐triggered immunopathology may advance demyelinating disorders, such as multiple sclerosis (MS).63 Similar results were obtained in animal models confirming the role of coronaviruses in demyelination and intracranial axonal degeneration.64 (Figure 1).
Pediatrics: No sufficient evidence exists that pediatric patients with the rheumatic disease have higher risks of developing COVID‐19.65 Because the uncontrolled disease is a crucial risk factor for COVID‐19 infection, patients should not withdraw their medications, unless there is a contradiction.66, 67 COVID‐19 may result in multisystem inflammatory syndrome in children (MIS‐C) which is a very rare complication in pediatrics and is characterized by high fever, organ dysfunction, and strongly elevated markers of inflammation.68
2.8. COVID‐19 and dermatology
Skin changes related to the application of protective equipment and disinfection including de novo contact reactions and exacerbation of preexisting dermatologic conditions have been revealed in recent studies.69, 70
Although respiratory symptoms are the most common presentation of COVID‐19, skin manifestations including maculopapular rash, urticaria, vesicular rash, petechia, purpura, chilblains, livedo racemosa, and distal ischemia have been reported.71, 72 (Figure 2).
FIGURE 2.
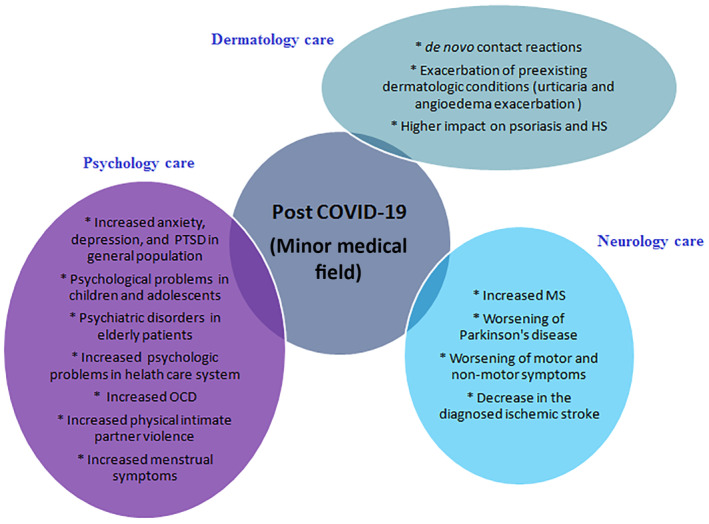
The consequences of COVID‐19 on minor medical fields after the pandemic
Increased release of pro‐inflammatory cytokines such as interleukin‐6 and tumor necrosis factor‐α are promoted by hypertrophied adipocytes and can lead to skin inflammation.73, 74 Besides the hyper inflammation state, drugs including hydroxychloroquine have been suggested to be triggering or exacerbating factors for psoriasis.75 Forced quarantine has negative impacts on psoriasis due to the psychological consequences affecting the quality of life as well as preventive discontinuation of effective treatment.76
Pediatrics: Chilblain‐like lesions located on acral regions distributed on hands and feet may be associated with COVID‐19 infection in the pediatric population; resulting in possible dermatological complications.77 The robust immune system in children may cause protection against respiratory symptoms of COVID‐19 but also may result in MIS‐C with macular, papular, morbilliform, vesicular, urticarial, and vascular morphologies.78
2.9. COVID‐19 and general surgery
COVID‐19 has the potentials to complicate the perioperative period with diagnostic challenges and a potential high fatality rate.79 Several studies reported considerable adverse effects on trainees.80, 81, 82, 83
In another survey, among 535 vascular surgeons, 91% noted the cancellation of elective surgical procedures.84 In a study in Auckland city's hospital, the admission decreased by 26%.85 Accordingly, patients presenting with trauma decreased by 57%. In addition, there was a 44% reduction in performed operations. Although there was a decrease in patients admissions, no statistical difference was found in discharge diagnosis.85 This effect is seen even in referrals with acute abdominal complaints. There was a 46% decrease in acute appendicitis admissions.86 Acute appendicitis and cholecystectomy decreased by 32% and 30%,87 while bariatric surgeries and hiatal hernia repairs dropped by 98% and 96%, respectively.88 In another survey among breast cancer patients awaiting surgery, more than half of them claimed that COVID‐19 pandemics increased their existing oncologic fears.89 According to a study in the UK, 3 to 6 months delay in cancer surgeries could have terrible effects on life‐years gained (LYG's) from cancer surgery which would cause the attributable death of 4755 out of 10 760 cases.90, 91 (Figure 3).
FIGURE 3.
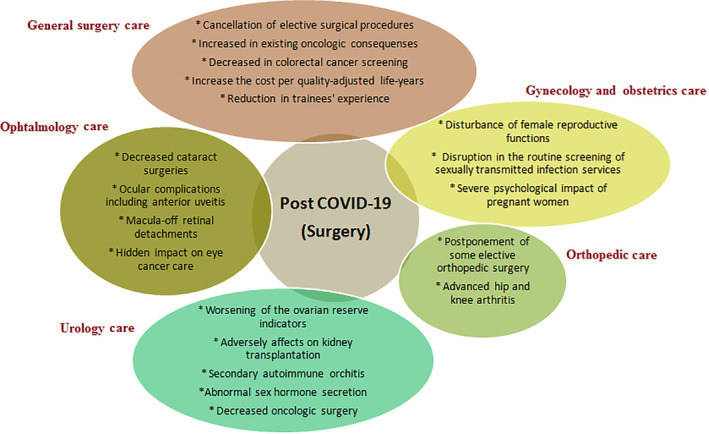
The consequences of COVID‐19 on surgery care after the pandemic
Pediatrics: Pediatric tumors require intensive treatment with no postponing or modification in the therapies to not reduce their efficacy and patient cure rates.92, 93 Considering the time‐sensitive nature of many pediatric craniofacial interventions these types of surgeries must be balanced according to the risks of postponing a surgical procedure with the risk of the COVID‐19 outbreak for the child.92
2.10. COVID‐19 and gynecology
ACE2 is widely expressed in the female reproductive system including the ovary, uterus, vagina, and placenta so that follicle development and ovulation, luteal angiogenesis and degeneration as well as regular changes in endometrial tissue and embryo development may be influenced by COVID‐19.94 Considering the disturbance of female reproductive functions,95 following‐up and evaluation of fertility are recommended in patients with a menstrual disorder or those with a delay in pregnancy. Menstrual data analysis of women of childbearing age diagnosed with COVID‐19 revealed that a menstrual volume decrease or cycle prolongation in one‐fifth of patients as a consequence of transient sex hormone changes.96 Moreover, the COVID‐19 pandemic has disrupted the routine screening of sexually transmitted infection services.97 As a result, an increase in syndromic sexually transmitted infection testing along with a raised number of missed asymptomatic cases is expected in the post‐COVID era. So, regular periodic following‐up strategies will be needed to recompense the long‐term gap of missed screening opportunities.
Saccone et al found that more than half of the pregnant women; especially those in the first trimester of pregnancy, suffered from the severe psychological impact of the COVID‐19 outbreak which was caused by high anxiety regarding the vertical transmission of the disease.98 So it seems that psychological interventions along with routine clinical screening should be formulated to improve both the mental and physical health after the COVID‐19 epidemic. (Figure 3).
2.11. COVID‐19 and neurology
A total of 64% of patients with multiple sclerosis (MS) canceled their medical visits, 11% canceled their MRI, and 10% changed their DMT due to COVID‐19.99, 100
In another study in the US, among 1342 patients with Parkinson's disease, the symptoms have been worsened in half of the patients.101 In a similar study, anxiety and depression had a higher prevalence in advanced Parkinson's disease patients.102 In a survey in Turkey, 31% of Parkinson's disease patients reported worsening of motor and non‐motor symptoms during the lockdown which is related to physical inactivity.103 Physical inactivity and increased stress may worsen motor symptoms and non‐motor symptoms in Parkinson's disease patients.104
There was a decrease in the mean weekly volume of newly diagnosed ischemic stroke.105, 106 In another similar study in Germany, there was a significant decrease in transient ischemic strokes (85%, 46%, and 42%) in three different hospitals.107 As patients with chronic neurological diseases suffer from a disability and restricted mobility, undiagnosed strokes, untreated strokes, delays in patients' treatment, and psychological effects could have serious consequences on the lifestyle of patients along with costs for the healthcare system.108, 109 (Figure 2).
Pediatrics: It has been indicated that neurological diseases of pediatrics such as Guillain‐Barre syndrome, multiple sclerosis, infantile spasms, acute disseminated encephalomyelitis, and febrile seizures are associated with COVID‐19.110, 111 Recent reports described emerging pediatric cases diagnosed with MIS‐C with an unexpectedly high incidence (34%) of neurological involvement.112
2.12. COVID‐19 and ophthalmology
According to a study performed in New York City, the majority of patients had increased anxiety regarding the suspended ophthalmic care.113 The COVID‐19 pandemic has been shown to reduce the institution's surgical rate to approximately 10%s, affecting the type of procedures.114 COVID‐19 may be associated with ocular complications, including anterior uveitis, which is usually leading to intraocular pressure.115 Orbital myositis in the absence of typical systemic COVID‐19 manifestations was reported in a 10‐year‐old boy; alarming the possible association of this event with coronavirus.116 According to an investigation performed in 104 confirmed COVID‐19 who required mechanical ventilation, 21.9% had eye lesions with a similar rate of intraocular lesions in patients in both the ward or intensive care unit.117 A higher proportion of macula‐off retinal detachments has been reported the delayed presentation of which may cause additional pressures on emergency eye department services due to complications and associated morbidity.118 Prioritizing intravitreal injections for neovascular age‐related macular degeneration and retinal vein occlusions have been announced during the COVID‐19 pandemic; as these eyes may experience the greatest loss of vision with treatment delay.119 COVID‐19 pandemic has a hidden impact on eye cancer care as fewer uveal melanoma cases with more advanced diseases were diagnosed during the national lockdowns.120 (Figure 3).
Pediatrics: Ocular involvement in children presented with episcleritis, retinal vasculitis, and neuro‐ophthalmological manifestations including optic neuritis or cranial nerve paresis may be associated with COVID‐19.121 In addition, fever, gastrointestinal, and dermatological symptoms may be signs of MIS‐C in pediatrics COVID‐19 involvement.122
2.13. COVID‐19 and orthopedy
Restarting elective orthopedic services during the COVID‐19 pandemic is still a major challenge as only 56% of patients were prepared to continue their planned surgical care.123 Opposite results were obtained in the study of Dittman et al suggesting the willingness of patients to undergo elective total hip and knee replacement.124 Whatever the desire of patients is, postponement of some elective orthopedic surgery may cause an irrecoverable worsening situation.
Even though patients with COVID‐19 who undergo urgent and emergent surgery are at increased risk for perioperative morbidity and mortality,125 a fine balance should be kept by considering the pros and cons of urgent vs postponed surgery to keep the patients safe and treat the disability associated with advanced hip and knee arthritis.126
The withdraws of different modalities are the longer time it takes and the impossibility of functional testing for ligament injuries.127 Despite the hope that mass vaccination will bring the previous routine healthcare system back, the orthopedic community must readjust its strategies to assemble the challenge of massive backlogs in elective caseloads.128 (Figure 3).
Pediatrics: COVID‐19 pandemic has led to a decrease in the number of acute pediatric trauma referrals with a decline in operations that may result in malformations of traumatic fractures by missing the golden weeks.129 However, in the study of Iliadis et al patients across different orthopedic subspecialties underwent the surgery without respiratory complications in the early postoperative period.130
2.14. COVID‐19 and psychology
Quarantine and social isolation have increased fear‐related disorders and widespread mental health problems.131 Unfavorable long‐term effects both on patients with previous psychiatric disorders and the general population are inevitable during the COVID‐19 pandemic.132, 133 Similar results were found in Brazil, as the country with the second‐highest number of COVID‐19 cases in the world; confirming the negative impact of the COVID‐19 pandemic on the mental health of the general population.134 In elderly patients with psychiatric disorders and suggested the consideration of patients' needs to ensure their well‐being throughout the current and future pandemics.135 Kovner et al have found the same results in frontline nurses during the first wave of the COVID‐19 pandemic in New York City.136 Psychological fatigue during a pandemic scenario is more prevalent in mothers of asthmatic children.137 The increase and persistence of obsessive‐compulsive symptoms have shown the importance of close monitoring of the public's mental health.138 The incidence and severity of physical intimate partner violence have also been increased during the COVID‐19 pandemic, and the victims were not referred to health care services until the late stages.139
According to the study of Demir et al, an increase in anxiety scores and women's menstrual symptoms were detected; while the length of periods was decreased.140 Impaired physiologic and emotional states during the forced quarantine may worsen several psychological or psoriasis conditions.141 (Figure 2).
Pediatrics: According to a study performed on quality of life and psychological state of children and adolescents in Germany, low socioeconomic status, migration background, and restricted living space were the main triggers of psychological problems.142
2.15. COVID‐19 and urology
Due to the COVID‐19 pandemic, low priority surgeries such as fertility procedures have been delayed, resulting in worsening of the ovarian reserve indicators caused by the increase in the average age of women as well as progressive testicular damage.143
The SCQ‐score has been suggested as a new quantitative system for prioritizing elective stone surgeries, which may probably remain of interest in the post‐COVID‐19 era.144 The kidney transplantation curriculum has been also adversely affected by the COVID‐19 pandemic with a drop in the operations of 72% of living and 84% of deceased donor programs.145
The male gonadal function may be impaired after COVID‐19 infection caused by even secondary autoimmune orchitis triggered by SARS‐CoV‐2 infection or segmental vasculitis caused by abnormal blood clotting.146, 147 Other studies have also confirmed the presence of leukocyte infiltration that could affect the function of Leydig cells, harm the blood‐testis barrier, and devastate the seminiferous epithelium.148, 149, 150 A dramatic decrease was found in the testosterone‐to‐luteinizing hormone ratio in patients with COVID‐19 compared to age‐matched healthy controls.151 An abnormal sex hormone secretion has also been confirmed; suggesting special attention to the reproductive function evaluation in the post‐COVID‐19 follow‐ups.152
Prostate cancer (PCa) needs to be managed by surgery as the gold‐standard treatment compared to radiation therapy alone; while oncologic surgery has been reduced.153 (Figure 2).
Pediatrics: The COVID‐19 pandemic has caused an extreme change in pediatric urology care. According to the study of Charnaya et al COVID‐19 pandemic had primarily reduced kidney transplantation among pediatrics with no sustained effect.154
2.16. Pulmonary involvement
Interestingly, patients with severe asthma did not show higher rates of exacerbations during the pandemic outbreak that may be contributed to the self‐administration of biological drugs.155 A significant reduction in asthma exacerbation was detected during COVID‐19 compared with previous years despite they were more expected to avoid or delay medical visits due to fear of referring to medical facilities.156, 157, 158
Similar results were found in the case of chronic obstructive pulmonary disease (COPD) with the most substantial reductions ever seen across Scotland and Wales which is hypothesized to have resulted from the decreased transmission of respiratory infection and exposure to outdoor pollution as well as possible enhanced COPD self‐management.159
Pediatrics: Studies are needed that go beyond to identify whether childhood asthma or any other kind of pediatric respiratory disease such as allergic manifestations constitute risk factors for COVID‐19 severity.160
3. CONCLUSION
Lockdown strategies during the COVID‐19 pandemic era may have negative effects on diagnostic and screening programs. To date, little is known about the possible incidence of new cases with a chronic disease in whom the diagnosis has been delayed because of the fear to refer to healthcare centers during the COVID‐19 pandemic. Similarly, it is unclear how those with an underlying disease have suffered from the condition due to the loss of patient‐clinician interaction, discontinuity of treatment, and lack of previously scheduled follow‐ups.
The major point of this review is that the bias of telehealth was not evaluated. Future directions in telehealth use and quality measures have still to be explored considering the changes in health care practice which is unlikely to resemble the prior era in the post‐COVID‐19 world. In addition, adherence to medication and the risk of flares are not yet assessed. As a result, further cooperative efforts are required to unfold this information. Direct engagement of multidisciplinary stakeholders should be considered to meet known and new patients' needs. This study highlighted the importance of being prepared to support families with special needs and mitigate the burden caused by COVID‐19. Containment policies and behavioral preventive modalities are suggested to limit the impact of COVID‐19 in patients with chronic underlying diseases. Furthermore, both the health systems and individual clinicians must be arranged to propose specific interventions to identify and treat psychiatric issues.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not‐for‐profit sectors.
CONFLICT OF INTEREST
The author does not have any conflict of interest and will sign the Disclosing Form. The [lead author: Nastaran Sabetkish] affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
AUTHOR CONTRIBUTIONS
Conceptualization: Nastaran Sabetkish.
Literature review: Nastaran Sabetkish, Alireza Rahmani.
Writing–Original Draft Preparation: Nastaran Sabetkish, Alireza Rahmani.
Writing–Review and Editing: Nastaran Sabetkish, Alireza Rahmani.
All authors have read and approved the final version of the manuscript.
Nastaran Sabetkish had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
Sabetkish N, Rahmani A. The overall impact of COVID‐19 on healthcare during the pandemic: A multidisciplinary point of view. Health Sci Rep. 2021;4:e386. doi: 10.1002/hsr2.386
REFERENCES
- 1.Aktas G. A comprehensive review on rational and effective treatment strategies against an invisible enemy; SARS Cov‐2 infection. Exp Biomed Res. 2020;3:293‐311. [Google Scholar]
- 2.Wu Z, McGoogan J. Outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323:1001.32154847 [Google Scholar]
- 3.Yiasemidou M, Tomlinson J, Chetter I, et al. Impact of the SARS‐CoV‐2 (COVID‐19) crisis on surgical training: global survey and a proposed framework for recovery. BJS Open. 2021;5:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Long B, Brady WJ, Koyfman A, et al. Cardiovascular complications in COVID‐19. Am J Emerg Med. 2020;38:1504‐1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahajan K, Chandra KS. Cardiovascular comorbidities and complications associated with coronavirus disease 2019. Med J Armed Forces India. 2020;76:253‐260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ullah M, Islam AM, Akanda MAK, et al. Post COVID cardiovascular care‐a review. Cardiovasc J. 2021;13:189‐199. [Google Scholar]
- 7.Mehra MR, Desai SS, Kuy S, et al. Cardiovascular disease, drug therapy, and mortality in Covid‐19. N Engl J Med. 2020;382:e102. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 8.Wu J, Mamas MA, Mohamed MO, et al. Place and causes of acute cardiovascular mortality during the COVID‐19 pandemic. Heart. 2021;107:113‐119. [DOI] [PubMed] [Google Scholar]
- 9.Shafi AM, Atieh AE, Harky A, et al. Impact of COVID‐19 on cardiac surgical training: our experience in the United Kingdom. J Card Surg. 2020;35:1954‐1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bandyopadhyay D, Akhtar T, Hajra A, et al. COVID‐19 pandemic: cardiovascular complications and future implications. Am J Cardiovasc Drugs. 2020;20:1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singh AK, Misra A. Impact of COVID‐19 and comorbidities on health and economics: focus on developing countries and India. Diabetes Metab Syndr Clin Res Rev. 2020;14:1625‐1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Niaz T, Hope K, Fremed M, et al. Role of a pediatric cardiologist in the COVID‐19 pandemic. Pediatr Cardiol. 2021;42:19‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alsaied T, Aboulhosn JA, Cotts TB, et al. Coronavirus disease 2019 (COVID‐19) pandemic implications in pediatric and adult congenital heart disease. J Am Heart Assoc. 2020;9:e017224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schofield J, Leelarathna L, Thabit H. COVID‐19: impact of and on diabetes. Diabetes Ther. 2020;11:1429‐1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ghesquière L, Garabedian C, Drumez E, et al. Effects of COVID‐19 pandemic lockdown on gestational diabetes mellitus: a retrospective study. Diabetes Metab. 2021;47:101201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dżygało K, Nowaczyk J, Szwilling A, et al. Increased frequency of severe diabetic ketoacidosis at type 1 diabetes onset among children during COVID‐19 pandemic lockdown: an observational cohort study. Pediatr Endocrinol Diabetes Metab. 2020;26:167‐175. [DOI] [PubMed] [Google Scholar]
- 17.Bilgin S, Tel BMA, Duman TT, et al. Комплаєнс до лікування левотироксином хворих на гіпотиреоз під час пандемічної ери SARS‐CoV‐2. Int J Endocrinol (Ukraine). 2021;17:103‐107. [Google Scholar]
- 18.Auriemma R, Pirchio R, Liccardi A, et al. Metabolic syndrome in the era of COVID‐19 outbreak: impact of lockdown on cardiometabolic health. J Endocrinol Investig. 2021;May 26:1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graf A, Marcus HJ, Baldeweg SE. The direct and indirect impact of the COVID‐19 pandemic on the care of patients with pituitary disease: a cross sectional study. Pituitary. 2021;24:262‐268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Giustina A, Legg E, Cesana BM, et al. Results from ACROCOVID: an international survey on the care of acromegaly during the COVID‐19 era. Endocrine. 2021;71:273‐280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.d'Annunzio G, Maffeis C, Cherubini V, et al. Caring for children and adolescents with type 1 diabetes mellitus: Italian Society for Pediatric Endocrinology and Diabetology (ISPED) statements during COVID‐19 pandemia. Diabetes Res Clin Pract. 2020;168:108372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Regelmann MO, Conroy R, Gourgari E, et al. Pediatric endocrinology in the time of COVID‐19: considerations for the rapid implementation of telemedicine and management of pediatric endocrine conditions. Horm Res Paediatr. 2020;93:343‐350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gralnek IM, Hassan C, Dinis‐Ribeiro M. COVID‐19 and endoscopy: implications for healthcare and digestive cancer screening. Nat Rev Gastroenterol Hepatol. 2020;17:444‐446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rutter MD, Brookes M, Lee TJ, et al. Impact of the COVID‐19 pandemic on UKendoscopic activity and cancer detection: a national endoscopy database analysis. Gut. 2021;70:537‐543. [DOI] [PubMed] [Google Scholar]
- 25.Lantinga MA, Theunissen F, Ter Borg PC, et al. Impact of the COVID‐19 pandemic on gastrointestinal endoscopy in The Netherlands: analysis of a prospective endoscopy database. Endoscopy. 2021;53:166‐170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goenka MK, Afzalpurkar S, Ghoshal UC, et al. Impact of COVID‐19 on gastrointestinal endoscopy practice in India: a cross‐sectional study. Endosc Int Open. 2020;8:E974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Belle A, Barret M, Bernardini D, et al. Impact of the COVID‐19 pandemic on gastrointestinal endoscopy activity in France. Endoscopy. 2020;52:1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bajaj JS, Garcia‐Tsao G, Biggins SW, et al. Comparison of mortality risk in patients with cirrhosis and COVID‐19 compared with patients with cirrhosis alone and COVID‐19 alone: multicentre matched cohort. Gut. 2021;70:531‐536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sarin SK, Choudhury A, Lau GK, et al. Pre‐existing liver disease is associated with poor outcome in patients with SARS CoV2 infection; the APCOLIS study (APASL COVID‐19 liver injury Spectrum study). Hepatol Int. 2020;14:690‐700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor R, Mallon D. COVID‐19 and pediatric gastroenterology. Pediatr Clin. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gonzalez Jimenez D, Rodríguez‐Belvís MV, Gonzalez PF, et al. COVID‐19 gastrointestinal manifestations are independent predictors of PICU admission in hospitalized pediatric patients. Pediatr Infect Dis J. 2020;39:e459–e462. [DOI] [PubMed] [Google Scholar]
- 32.Mallon D, Pohl JF, Phatak UP, et al. Impact of COVID‐19 on pediatric gastroenterology fellow training in North America. J Pediatr Gastroenterol Nutr. 2020;71:6‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aktas G. Hematological predictors of novel coronavirus infection. Rev Assoc Med Bras. 2021;67:1‐2. [DOI] [PubMed] [Google Scholar]
- 34.Taher AT, Bou‐Fakhredin R, Kreidieh F, et al. Care of patients with hemoglobin disorders during the COVID‐19 pandemic: an overview of recommendations. Am J Hematol. 2020;95:E208–E210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.de Sanctis V, Canatan D, Corrons JLV, et al. Preliminary data on COVID‐19 in patients with hemoglobinopathies: a multicentre ICET‐a study. Mediterr J Hematol Infect Dis. 2020;12:e2020046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beerkens F, John M, Puliafito B, et al. COVID‐19 pneumonia as a cause of acute chest syndrome in an adult sickle cell patient. Am J Hematol. 2020;95:E154–E156. [DOI] [PubMed] [Google Scholar]
- 37.Fan BE, Chong VCL, Chan SSW, et al. Hematologic parameters in patients with COVID‐19 infection. Am J Hematol. 2020;95:E131–E134. [DOI] [PubMed] [Google Scholar]
- 38.Noun P, Ibrahim A, Hodroj MH, et al. COVID‐19 in benign hematology: emerging challenges and special considerations for healthcare professionals. Expert Rev Hematol. 2020;13:1081‐1092. [DOI] [PubMed] [Google Scholar]
- 39.Patell R, Bogue T, Koshy A, et al. Postdischarge thrombosis and hemorrhage in patients with COVID‐19. Blood. 2020;136:1342‐1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vilela TS, Braga JAP, Loggetto SR. Hemoglobinopathy and pediatrics in the time of COVID‐19. Hematol Transfus Cell Ther. 2021;43:87‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hirsch JS, Ng JH, Ross DW, et al. Acute kidney injury in patients hospitalized with COVID‐19. Kidney Int. 2020;98:209‐218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hassanein M, Radhakrishnan Y, Sedor J, et al. COVID‐19 and the kidney. Cleve Clin J Med. 2020;87:619‐631. [DOI] [PubMed] [Google Scholar]
- 43.Fisher M, Neugarten J, Bellin E, et al. AKI in hospitalized patients with and without COVID‐19: a comparison study. J Am Soc Nephrol. 2020;31:2145‐2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cummings MJ, Baldwin MR, Abrams D, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID‐19 in new York City: a prospective cohort study. Lancet. 2020;395:1763‐1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pei G, Zhang Z, Peng J, et al. Renal involvement and early prognosis in patients with COVID‐19 pneumonia. J Am Soc Nephrol. 2020;31:1157‐1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.de Oliveira P, Cunha K, Neves P, et al. Renal morphology in coronavirus disease: a literature review. Medicina (Kaunas). 2021;57:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.de Jonge L, Worthington J, van Wifferen F, et al. Impact of the COVID‐19 pandemic on faecal immunochemical test‐based colorectal cancer screening programmes in Australia, Canada, and The Netherlands: a comparative modelling study. Lancet Gastroenterol Hepatol. 2021;6:304‐314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Robinson C, Ruhl M, Kirpalani A, et al. Management of Canadian pediatric patients with glomerular diseases during the COVID‐19 pandemic: recommendations from the Canadian association of pediatric nephrologists COVID‐19 rapid response team. Can J Kidney Health Dis. 2020;7:2054358120970713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang X, Chen X, Tang F, et al. Be aware of acute kidney injury in critically ill children with COVID‐19. Pediatr Nephrol. 2021;36:163‐169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tram N, Chiodini B, Montesinos I, et al. Rhabdomyolysis and acute kidney injury as leading COVID‐19 presentation in an adolescent. Pediatr Infect Dis J. 2020;39:e314–e315. [DOI] [PubMed] [Google Scholar]
- 51.Bertuzzi AF, Ciccarelli M, Marrari A, et al. Impact of active cancer on COVID‐19 survival: a matched‐analysis on 557 consecutive patients at an academic Hospital in Lombardy, Italy. Br J Cancer. 2021;125:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dinmohamed AG, Visser O, Verhoeven RHA, et al. Fewer cancer diagnoses during the COVID‐19 epidemic in The Netherlands. Lancet Oncol. 2020;21:750‐751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dinmohamed AG, Cellamare M, Visser O, et al. The impact of the temporary suspension of national cancer screening programmes due to the COVID‐19 epidemic on the diagnosis of breast and colorectal cancer in The Netherlands. J Hematol Oncol. 2020;13:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gampel B, Troullioud Lucas AG, Broglie L, et al. COVID‐19 disease in New York City pediatric hematology and oncology patients. Pediatr Blood Cancer. 2020;67:e28420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ferrari A, Zecca M, Rizzari C, et al. Children with cancer in the time of COVID‐19: an 8‐week report from the six pediatric onco‐hematology centers in Lombardia, Italy. Pediatr Blood Cancer. 2020;67:e28410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Antony A, Connelly K, De Silva T, et al. Perspectives of patients with rheumatic diseases in the early phase of COVID‐19. Arthritis Care Res. 2020;72:1189‐1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Figueroa‐Parra G, Aguirre‐Garcia GM, Gamboa‐Alonso CM, et al. Are my patients with rheumatic diseases at higher risk of COVID‐19? Ann Rheum Dis. 2020;79:839‐840. [DOI] [PubMed] [Google Scholar]
- 58.Favalli EG, Ingegnoli F, Cimaz R, et al. What is the true incidence of COVID‐19 in patients with rheumatic diseases? Ann Rheum Dis. 2021;80:e18. [DOI] [PubMed] [Google Scholar]
- 59.Arora G, Kassir M, Jafferany M, et al. The COVID‐19 outbreak and rheumatologic skin diseases. Dermatol Ther. 2020;33:e13357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Roux CH, Brocq O, Gerald F, et al. Impact of home confinement during the COVID‐19 pandemic on medication use and disease activity in Spondyloarthritis patients. Arthritis Rheumatol. 2020;72:1771‐1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Santos‐Ruiz A, Montero‐López E, Ortego‐Centeno N, et al. Effect of COVID‐19 confinement on the mental status of patients with systemic lupus erythematosus. Med Clin (Engl Ed). 2021;156:379‐385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhou SY, Zhang C, Shu WJ, et al. Emerging roles of coronavirus in autoimmune diseases. Arch Med Res. 2021;Apr 8:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cheng Y, Skinner DD, Lane TE. Innate immune responses and viral‐induced neurologic disease. J Clin Med. 2018;8:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mangale V, McIntyre LL, Walsh CM, et al. Promoting remyelination through cell transplantation therapies in a model of viral‐induced neurodegenerative disease. Dev Dyn. 2019;248:43‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Haşlak F, Yıldız M, Adrovic A, et al. Childhood rheumatic diseases and COVID‐19 pandemic: an intriguing linkage and a new horizon. Balkan Med J. 2020;37:184‐188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Favalli EG, Ingegnoli F, De Lucia O, et al. COVID‐19 infection and rheumatoid arthritis: faraway, so close! Autoimmun Rev. 2020;19:102523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen J, Zhang ZZ, Chen YK, et al. The clinical and immunological features of pediatric COVID‐19 patients in China. Genes Dis. 2020;7:535‐541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Grazioli S, Tavaglione F, Torriani G, et al. Immunological assessment of pediatric multisystem inflammatory syndrome related to COVID‐19. J Pediatric Infect Dis Soc. 2020;10:706‐713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Darlenski R, Kazandjieva J, Tsankov N. Prevention and occupational hazards for the skin during COVID‐19 pandemic. Clin Dermatol. 2021;39:92‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Darlenski R, Tsankov N. COVID‐19 pandemic and the skin: what should dermatologists know? Clin Dermatol. 2020;38:785‐787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gottlieb M, Long B. Dermatologic manifestations and complications of COVID‐19. Am J Emerg Med. 2020;38:1715‐1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Criado PR, Criado RFJ, Pincelli TP, et al. Chronic spontaneous urticaria exacerbation in a patient with COVID‐19: rapid and excellent response to omalizumab. Int J Dermatol. 2020;59:1294‐1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Budu‐Aggrey A, Brumpton B, Tyrrell J, et al. Evidence of a causal relationship between body mass index and psoriasis: a mendelian randomization study. PLoS Med. 2019;16:e1002739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Marasca C, Ruggiero A, Napolitano M, et al. May COVID‐19 outbreaks lead to a worsening of skin chronic inflammatory conditions? Med Hypotheses. 2020;143:109853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ozaras R, Berk A, Ucar DH, et al. Covid‐19 and exacerbation of psoriasis. Dermatol Ther. 2020;33:e13632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Patsatsi A, Kyriakou A. Impact of the COVID‐19 pandemic on the course and management of chronic inflammatory immune‐mediated skin diseases: what's the evidence? Clin Dermatol. 2021;39:52‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Garcia‐Lara G, Linares‐González L, Ródenas‐Herranz T, et al. Chilblain‐like lesions in pediatrics dermatological outpatients during the COVID‐19 outbreak. Dermatol Ther. 2020;33:e13516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yozgat CY, Uzuner S, Bursal Duramaz B, et al. Dermatological manifestation of pediatrics multisystem inflammatory syndrome associated with COVID‐19 in a 3‐year‐old girl. Dermatol Ther. 2020;33:e13770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Aminian A, Safari S, Razeghian‐Jahromi A, et al. COVID‐19 outbreak and surgical practice: unexpected fatality in perioperative period. Ann Surg. 2020;272:e27–e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Aziz H, James T, Remulla D, et al. Effect of COVID‐19 on surgical training across the United States: a national survey of general surgery residents. J Surg Educ. 2021;78:431‐439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hope C, Reilly J‐J, Griffiths G, et al. The impact of COVID‐19 on surgical training: a systematic review. Tech Coloproctol. 2021;25:1‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Johnson AP, Wohlauer MV, Mouawad NJ, et al. The impact of the COVID‐19 pandemic on vascular surgery trainees in the United States. Ann Vasc Surg. 2021;72:182‐190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Al‐Ghunaim TA, Johnson J, Biyani CS, et al. Psychological and occupational impact of the COVID‐19 pandemic on UKsurgeons: a qualitative investigation. BMJ Open. 2021;11:e045699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mouawad NJ, Woo K, Malgor RD, et al. The impact of the COVID‐19 pandemic on vascular surgery practice in the United States. J Vasc Surg. 2021;73:772‐779.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.McGuinness MJ, Hsee L. Impact of the COVID‐19 national lockdown on emergency general surgery: Auckland City Hospital's experience. ANZ J Surg. 2020;90:2254‐2258. [DOI] [PubMed] [Google Scholar]
- 86.Kamer E. The decrease of non‐complicated acute appendicitis and the negative appendectomy rate during pandemic. European Journal of Trauma and Emergency Surgery. 2021;Jun 17:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kurihara H, Marrano E, Ceolin M, et al. Impact of lockdown on emergency general surgery during first 2020 COVID‐19 outbreak. Eur J Trauma Emerg Surg. 2021;47:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Purdy AC, Smith BR, Hohmann SF, et al. The impact of the novel coronavirus pandemic on gastrointestinal operative volume in the United States. Surg Endosc. 2021;19:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Magno S, Linardos M, Carnevale S, et al. The impact of the COVID‐19 pandemic on breast cancer patients awaiting surgery: observational survey in an Italian university hospital. Breast J. 2020;26:1597‐1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sud A, Jones ME, Broggio J, et al. Collateral damage: the impact on outcomes from cancer surgery of the COVID‐19 pandemic. Ann Oncol. 2020;31:1065‐1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Karimuddin A, Albanese CM, Crump T, et al. Measuring the impact of delayed access to elective cholecystectomy through patient's cost‐utility: an observational cohort study. Int J Qual Health Care. 2021;33:mzab018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schoenbrunner A, Sarac B, Gosman A, et al. Considerations for pediatric craniofacial surgeons during the COVID‐19 outbreak. J Craniofac Surg. 2020;31:e618–e620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.DeFazio JR, Kahan A, Fallon EM, et al. Development of pediatric surgical decision‐making guidelines for COVID‐19 in a New York City children's hospital. J Pediatr Surg. 2020;55:1427‐1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Jing Y, Run‐Qian L, Hao‐Ran W, et al. Potential influence of COVID‐19/ACE2 on the female reproductive system. Mol Hum Reprod. 2020;26:367‐373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wilkins J, Al‐Inizi S. Premature ovarian insufficiency secondary to COVID‐19 infection: an original case report. Int J Gynaecol Obstet. 2021;154:179‐180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Li K, Chen G, Hou H, et al. Analysis of sex hormones and menstruation in COVID‐19 women of child‐bearing age. Reprod Biomed Online. 2021;42:260‐267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pinto CN, Niles JK, Kaufman HW, et al. Impact of the COVID‐19 pandemic on chlamydia and gonorrhea screening in the U.S. Am J Prev Med. 2021;61:386‐393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Saccone G, Florio A, Aiello F, et al. Psychological impact of coronavirus disease 2019 in pregnant women. Am J Obstet Gynecol. 2020;223:293‐295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Vogel AC, Schmidt H, Loud S, et al. Impact of the COVID‐19 pandemic on the health care of >1,000 people living with multiple sclerosis: a cross‐sectional study. Mult Scler Relat Disord. 2020;46:102512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Motolese F, Rossi M, Albergo G, et al. The psychological impact of COVID‐19 pandemic on people with multiple sclerosis. Front Neurol. 2020;11:1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Feeney MP, Xu Y, Surface M, et al. The impact of COVID‐19 and social distancing on people with Parkinson's disease: a survey study. NPJ Parkinsons Dis. 2021;7:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Montanaro E, Artusi CA, Rosano C, et al. Anxiety, depression, and worries in advanced Parkinson disease during COVID‐19 pandemic. Neurol Sci. 2021;May 4:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Balci B, Aktar B, Buran S, et al. Impact of the COVID‐19 pandemic on physical activity, anxiety, and depression in patients with Parkinson's disease. Int J Rehabil Res. [Internationale Zeitschrift Fur Rehabilitationsforschung. Revue Internationale De Recherches De Readaptation]. 2021;44:173‐176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Helmich RC, Bloem BR. The impact of the COVID‐19 pandemic on Parkinson's disease: hidden sorrows and emerging opportunities. J Parkinsons Dis. 2020;10:351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ortega‐Gutierrez S, Farooqui M, Zha A, et al. Decline in mild stroke presentations and intravenous thrombolysis during the COVID‐19 pandemic: the society of vascular and interventional neurology multicenter collaboration. Clin Neurol Neurosurg. 2021;201:106436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Siegler J, Heslin M, Thau L, et al. Falling stroke rates during COVID‐19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis. 2020;29:104953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hoyer C, Ebert A, Huttner HB, et al. Acute stroke in times of the COVID‐19 pandemic: a multicenter study. Stroke. 2020;51:2224‐2227. [DOI] [PubMed] [Google Scholar]
- 108.Bhaskar S, Bradley S, Israeli‐Korn S, et al. Chronic neurology in COVID‐19 era: clinical considerations and recommendations from the REPROGRAM consortium. Front Neurol. 2020;11:664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Heneka MT, Golenbock D, Latz E, et al. Immediate and long‐term consequences of COVID‐19 infections for the development of neurological disease. Alzheimers Res Ther. 2020;12:1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Christy A. COVID‐19: a review for the pediatric neurologist. J Child Neurol. 2020;35:934‐939. [DOI] [PubMed] [Google Scholar]
- 111.Gupta J, Madaan P, Chowdhury SR, et al. COVID‐19 and pediatric neurology practice in a developing country. Pediatr Neurol. 2020;113:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chen TH. Neurological involvement associated with COVID‐19 infection in children. J Neurol Sci. 2020;418:117096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Dar S, De Moraes CG, Karani R, et al. Patient concerns regarding suspended ophthalmic care due to COVID‐19. J Glaucoma. 2021;30:750‐757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Al‐Khersan H, Kalavar MA, Tanenbaum R, et al. Emergent ophthalmic surgical care at a tertiary referral center during the COVID‐19 pandemic. Am J Ophthalmol. 2021;222:368‐372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Alonso RS, Alonso FOM, Fernandes BF, et al. COVID‐19‐related ocular hypertension secondary to anterior uveitis as part of a multisystemic inflammatory syndrome. J Glaucoma. 2021;30:e256–e258. [DOI] [PubMed] [Google Scholar]
- 116.Eleiwa T, Abdelrahman SN, ElSheikh RH, et al. Orbital inflammatory disease associated with COVID‐19 infection. J AAPOS. 2021;25:232‐234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Marinho PM, Marcos AAA, Branco AMC, et al. COVID‐19 retinal findings in patients admitted to intensive care units and wards. Ocul Immunol Inflamm. 2021;May 12:1‐4. [DOI] [PubMed] [Google Scholar]
- 118.Poyser A, Deol SS, Osman L, et al. Impact of COVID‐19 pandemic and lockdown on eye emergencies. Eur J Ophthalmol. 2020;Nov 19:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Stone LG, Grinton ME, Talks JS. Delayed follow‐up of medical retina patients due to COVID‐19: impact on disease activity and visual acuity. Graefes Arch Clin Exp Ophthalmol. 2021;259:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang H, Elsheikh M, Gilmour K, et al. Impact of COVID‐19 pandemic on eye cancer care in United Kingdom. Br J Cancer. 2021;124:1357‐1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Alcalde CF, Fernández MG, Moreno MN, et al. COVID‐19 ocular findings in children: a case series. World J Pediatr. 2021;17:329‐334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Coll‐Vela LE, Zamudio‐Aquise MK, Nuñez‐Paucar H, et al. COVID‐19‐associated multisystem inflammatory syndrome in children: case series at a pediatric hospital in Peru. Rev Peru Med Exp Salud Publica. 2020;37:559‐565. [DOI] [PubMed] [Google Scholar]
- 123.Chang J, Wignadasan W, Kontoghiorghe C, et al. Restarting elective orthopaedic services during the COVID‐19 pandemic: do patients want to have surgery? Bone Jt Open. 2020;1:267‐271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Dittman LE, Johnson JD, Trousdale RT. COVID‐19 and elective joint arthroplasty: patient perspectives and considerations. J Orthop. 2021;25:179‐185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Knisely A, Zhou ZN, Wu J, et al. Perioperative morbidity and mortality of patients with COVID‐19 who undergo urgent and emergent surgical procedures. Ann Surg. 2021;273:34‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Liang ZC, Chong MSY, Sim MA, et al. Surgical considerations in patients with COVID‐19: what orthopaedic surgeons should know. J Bone Joint Surg Am. 2020;102:e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Scheidt S, Kehrer M, Jaenisch M, et al. A feasibility pilot study on the use of telemedicine for the examination of the knee joint. Z Orthop Unfall. 2020;Nov 24:1–5. [DOI] [PubMed] [Google Scholar]
- 128.Madanipour S, Iranpour F, Goetz T, et al. COVID‐19: lessons learnt and priorities in trauma and orthopaedic surgery. Ann R Coll Surg Engl. 2021;103:390‐394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sugand K, Park C, Morgan C, et al. Impact of the COVID‐19 pandemic on paediatric orthopaedic trauma workload in Central London: a multi‐centre longitudinal observational study over the “golden weeks”. Acta Orthop. 2020;91:633‐638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Iliadis AD, Eastwood DM, Bayliss L, et al. Providing a paediatric trauma and orthopaedics service during the peak of the COVID‐19 pandemic: the Royal National Orthopaedic Hospital experience. Bone Jt Open. 2020;1:287‐292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Amsalem D, Dixon LB, Neria Y. The coronavirus disease 2019 (COVID‐19) outbreak and mental health: current risks and recommended actions. JAMA Psychiat. 2021;78:9‐10. [DOI] [PubMed] [Google Scholar]
- 132.Belz M, Hessmann P, Vogelgsang J, et al. Evolution of psychosocial burden and psychiatric symptoms in patients with psychiatric disorders during the Covid‐19 pandemic. Eur Arch Psychiatry Clin Neurosci. 2021;May 3:1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Hossain MM, Rahman M, Trisha NF, et al. Prevalence of anxiety and depression in South Asia during COVID‐19: a systematic review and meta‐analysis. Heliyon. 2021;7:e06677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Goularte JF, Serafim SD, Colombo R, et al. COVID‐19 and mental health in Brazil: psychiatric symptoms in the general population. J Psychiatr Res. 2021;132:32‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Seethaler M, Just S, Stötzner P, et al. Psychosocial impact of COVID‐19 pandemic in elderly psychiatric patients: a longitudinal study. Psychiatry Q. 2021;26:1‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kovner C, Raveis VH, Van Devanter N, et al. The psychosocial impact on frontline nurses of caring for patients with COVID‐19 during the first wave of the pandemic in New York City. Nurs Outlook. 2021;Apr 5:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Di Riso D, Spaggiari S, Cambrisi E, et al. Psychosocial impact of Covid‐19 outbreak on Italian asthmatic children and their mothers in a post lockdown scenario. Sci Rep. 2021;11:9152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Loosen AM, Skvortsova V, Hauser TU. Obsessive‐compulsive symptoms and information seeking during the Covid‐19 pandemic. Transl Psychiatry. 2021;11:309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Gosangi B, Park H, Thomas R, et al. Exacerbation of physical intimate partner violence during COVID‐19 pandemic. Radiology. 2021;298:E38–E45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Demir O, Sal H, Comba C. Triangle of COVID, anxiety and menstrual cycle. J Obstet Gynaecol. 2021;May 6:1‐5. [DOI] [PubMed] [Google Scholar]
- 141.Megna M, Ruggiero A, Marasca C, Fabbrocini G. Biologics for psoriasis patients in the COVID‐19 era: more evidence, less fears. J Dermatol Treat. 2020;31:328‐329. [DOI] [PubMed] [Google Scholar]
- 142.Ravens‐Sieberer U, Kaman A, Erhart M, et al. Impact of the COVID‐19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur Child Adolesc Psychiatry. 2021;Jan 25:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Ribal MJ, Cornford P, Briganti A, et al. European Association of Urology guidelines office rapid reaction group: an organisation‐wide collaborative effort to adapt the European Association of Urology guidelines recommendations to the coronavirus disease 2019 era. Eur Urol. 2020;78:21‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Fentes DP, Baltar CF, Otero JN, Gil RD, Sampedro FG. The SCQ‐SCORE: initial validation of a new scoring system for elective stone surgery prioritization in the COVID‐19 era. Cent European J Urol. 2021;74:81‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Boyarsky BJ, Po‐Yu Chiang T, Werbel WA, et al. Early impact of COVID‐19 on transplant center practices and policies in the United States. Am J Transplant. 2020;20:1809‐1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Pan F, Xiao X, Guo J, et al. No evidence of severe acute respiratory syndrome‐coronavirus 2 in semen of males recovering from coronavirus disease 2019. Fertil Steril. 2020;113:1135‐1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Wang S, Zhou X, Zhang T, et al. The need for urogenital tract monitoring in COVID‐19. Nat Rev Urol. 2020;17:314‐315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Youssef K, Abdelhak K. Male genital damage in COVID‐19 patients: are available data relevant? Asian J Urol. 2020;8:324‐326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Xu J, Qi L, Chi X, et al. Orchitis: a complication of severe acute respiratory syndrome (SARS). Biol Reprod. 2006;74:410‐416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Gralinski LE, Menachery VD. Return of the coronavirus: 2019‐nCoV. Viruses. 2020;12:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ma L, Xie W, Li D, et al. Effect of SARS‐CoV‐2 infection upon male gonadal function: a single center‐based study. MedRxiv, 2020.
- 152.Ma L, Xie W, Li D, et al. Evaluation of sex‐related hormones and semen characteristics in reproductive‐aged male COVID‐19 patients. J Med Virol. 2021;93:456‐462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Moschovas MC, Sighinolfi MC, Rocco B, et al. Balancing the effects of COVID‐19 against potential progression and mortality in high‐risk prostate cancer. Eur Urol. 2020;78:e14–e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Charnaya O, Chiang TP, Wang R, et al. Effects of COVID‐19 pandemic on pediatric kidney transplant in the United States. Pediatr Nephrol. 2021;36:143‐151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Caruso C, Colantuono S, Urbani S, et al. Real‐life survey on severe asthma patients during COVID‐19 lockdown in Italy. Expert Rev Respir Med. 2021;15:1‐4. [DOI] [PubMed] [Google Scholar]
- 156.de Boer G, Braunstahl GJ, Hendriks R, et al. Asthma exacerbation prevalence during the COVID‐19 lockdown in a moderate‐severe asthma cohort. BMJ Open Respir Res. 2021;8:e000758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Salciccioli JD, She L, Tulchinsky A, et al. Effect of COVID‐19 on asthma exacerbation. J Allergy Clin Immunol Pract. 2021;9:2896‐2899.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Chan KPF, Kwok WC, Ma TF, et al. Territory‐wide study on hospital admissions for asthma exacerbation in COVID‐19 pandemic. Ann Am Thorac Soc. 2021;Feb 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Alsallakh MA, Sivakumaran S, Kennedy S, et al. Impact of COVID‐19 lockdown on the incidence and mortality of acute exacerbations of chronic obstructive pulmonary disease: national interrupted time series analyses for Scotland and Wales. BMC Med. 2021;19:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Castro‐Rodriguez JA, Forno E. Asthma and COVID‐19 in children: a systematic review and call for data. Pediatr Pulmonol. 2020;55:2412‐2418. [DOI] [PMC free article] [PubMed] [Google Scholar]


