Cotzias GC, Van Woert MH, Schiffer LM. Aromatic amino acids and modification of parkinsonism. N Engl J Med 1967;276:374–379.
Without any hesitation, my vote for the most important and impactful paper related to the treatment of movement disorders and published in the 20th Century is the one by George C. Cotzias and his colleagues,1 reporting on the dramatic effectiveness of high dosage DL‐dopa in treating Parkinsonʼs disease (PD). This was published in the February 16, 1967, issue of The New England Journal of Medicine. I'd add Cotzias' companion paper published 2 years later (February 13, 1969), showing that the benefit from DL‐dopa is solely due to the levorotatory isomer, levodopa.2 In between these two publications, Cotzias delivered an oral presentation at an international symposium in September 1967 in Montreal organized by André Barbeau, in which Cotzias showed movies of the dramatic improvement in his patients by both DL‐ and L‐dopa.3 This presentation likely spurred many clinical investigators sitting in the audience to embark on their own investigations of L‐dopa because there was a spate of publications that appeared shortly after Cotzias' February 1969 paper on high dosage levodopa.2 All these subsequent publications4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 corroborated Cotzias' findings. Melvin Yahr and colleagues4 published the first of these papers, a double‐blind clinical trial of levodopa appearing in October 1969. All the rest were open‐label studies, except for the paper by Nakano and Tyler.14
The work by Cotzias and his colleagues was immediately and widely recognized to be a new revolutionary treatment for PD. The Lasker Foundation named Cotzias as the recipient of its 1969 award for Clinical Medical Research.16 Levodopa was approved for the treatment of PD by the U.S. Food and Drug Administration in 1970.17 Interestingly, Cotzias revealed16 that his 1967 DL‐dopa paper had been initially rejected by prominent journals before being accepted by The New England Journal of Medicine. Cotzias suspected the rejections were because his dramatic beneficial results were difficult to be believed by the reviewers and editors of these other (unnamed) journals.
What about the outstanding contributions by others that provided laboratory and some clinical evidence for a role of levodopa in the treatment of PD (see review by Fahn18)? Let us start with the pioneering, Nobel prize‐winning work of Arvid Carlsson in Sweden who showed that a deficiency of a brain catecholamine was responsible for reserpine‐induced parkinsonism in animal models (mice and rabbits), and that DL‐dopa can reverse this parkinsonian state,19, 20 as illustrated in Figure 1.21 Carlsson showed that dopamine is present in the brain and that reserpine depletes the dopamine, which is restored by DL‐dopa administration.20 Graduate students22 in Carlsson's lab, as well as the neurologist Isamu Sano23 in Japan showed in regional distribution studies that dopamine is highly localized in the striatum in the brain. Based on all these investigations, Carlsson proposed that brain dopamine was somehow related to parkinsonism.24 Despite all this magnificent work in establishing a role for dopamine in brain function and implicating its role in PD, Carlsson's work appeared to have no influence on the subsequent clinical work of Cotzias, who never even cited any of Carlsson's publications in the DL‐ and L‐dopa clinical trials.1, 2 Carlsson's treatment of reserpine‐induced parkinsonism in animals19 was instrumental in initiating trials of L‐dopa in drug‐induced parkinsonian patients by Rudolf Degkwitz and his colleagues.25 As I will describe later, Cotzias' goal with DL‐dopa administration was not to restore brain dopamine with DL‐dopa but to restore neuromelanin in the substantia nigra.1
FIG. 1.
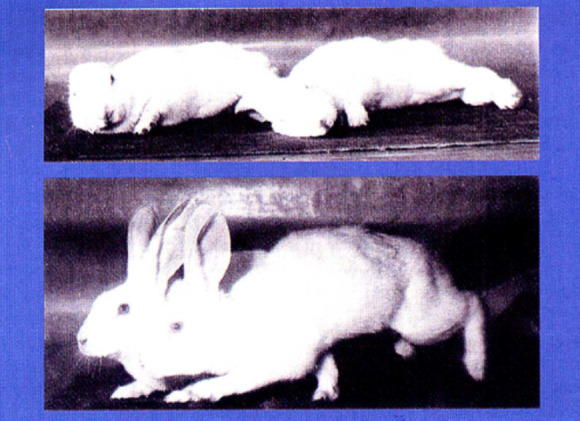
Rabbits that became immobile (akinetic) after being reserpinized (upper panel) and then were restored to good mobility after being treated with L‐dopa (lower panel) in an experiment by Carlsson, Lindqvist and Magnusson19 who showed that it was L‐dopa, and not L‐5‐HTP, that could reverse reserpine's parkinsonian effect. Figure from Carlsson's Nobel Lecture.21 Permission had been granted by Arvid Carlsson for future use of this figure.
Let us next consider the huge contributions by Oleh Hornykiewicz and his colleagues in Austria. In his own words26 Hornykiewicz described the influencing events that led him to measure dopamine levels in parkinsonian brains.27 First were Carlsson's discoveries that dopamine is in the brain, it is depleted by reserpine, and that DL‐dopa can both restore the brain dopamine and reverse reserpine‐induced parkinsonism.19, 20 Second, and perhaps of more importance to Hornykiewicz,26 were the reports that dopamine was highly selectively localized in the neostriatum,22, 23 a region known to be involved in extrapyramidal diseases. Hornykiewicz therefore decided to study regional brain dopamine concentrations in patients with a variety of extrapyramidal diseases. He proceeded to collect autopsied brains of 17 neurologically‐normal adults, 2 fetuses, and 14 brains of movement disorder cases; the latter group consisted of four with postencephalitic parkinsonism, two with PD, two with Huntingtonʼs disease, and six of an unknown cause. He measured the level of dopamine and norepinephrine in different brain regions, finding a marked depletion in striatal dopamine in only the six parkinsonian brains.27 Next, using a more sensitive analytical methodology, Hornykiewicz showed that dopamine was also severely reduced in the substantia nigra in PD brains.28 In 1966, Hornykiewicz published a review on dopamine's function in the brain and its relationship to PD. He concluded that striatal dopamine deficiency correlates with the parkinsonian motor features of rigidity and akinesia.29 With additional postmortem correlations of brain biochemistry and pathology, Hornykiewicz and his colleagues concluded that because of compensatory changes, such as supersensitivity of dopamine receptors and increased dopamine turnover, PD symptoms are manifested only when there is about an 80% reduction of dopamine concentration in the putamen or a loss of 60% of nigral dopaminergic neurons.30
Actually, Hornykiewicz was not the first person to demonstrate dopamine deficiency in the brains of people with PD (published in December 196027). Isamu Sano, a neurologist in Japan, reported dopamine deficiency in a single patient with PD at a neuropathology meeting earlier that year.31 The publication in Japanese of Sano's presentation of that work was of limited circulation and was not widely picked up by other scientists. Sano conceived of the idea of overcoming the dopamine deficiency by administering dopa to PD patients. He injected 200 mg of DL‐dopa intravenously into some patients with PD and found transient relief of rigidity and tremor. But the benefit lasted only a few minutes, and Sano concluded that this treatment was of no practical value.31
Hornykiewicz, similarly, after finding dopamine deficiency in parkinsonian brains,27 immediately conceived of the idea to treat parkinsonian patients with L‐dopa.26 Contributing his own personal small supply of L‐dopa, Hornykiewicz persuaded the neurologist, Walther Birkmayer, to inject L‐dopa intravenously into his patients with PD and postencephalitic parkinsonism. Following the procedure of Degkwitz,25 Birkmayer and Hornykiewicz began the injections in July 1961. They injected a total of 20 patients, and reported striking, transient benefit in mobility of their patients,32 with the greatest response in the postencephalitic patients. Benefit was enhanced if an oral monoamine oxidase (MAO) inhibitor was also given. Their collaboration lasted 5 years, testing many more patients and also testing oral doses of dopa. Dosing was limited by adverse effects of nausea and vomiting. By 1964, Birkmayer and Hornykiewicz had treated 200 parkinsonism patients with L‐dopa 25 mg i.v. (along with an oral MAO inhibitor) once or twice a week; 20% showed a general improvement of reduced akinesia, 30% had no improvement, and the other 50% had some improvement in speech or posture.33
While European investigators (Degkwitz in drug‐induced parkinsonism and Birkmayer in PD) were testing small doses of i.v. dopa, Patrick McGeer, a pharmacologist in Vancouver, teamed up with neurologists to test high dosage oral DL‐dopa. First, McGeer and his colleagues34 tested patients with drug‐induced parkinsonism (4 from reserpine, 18 from phenothiazines). They administered D,L‐dopa (4 to 32 g/day) orally and found mild improvement in two of the reserpine group and none in the phenothiazine group. Diphenhydramine 400 to 600 mg/d was also tested and was found to be beneficial in all 11 patients studied.34 Despite this disappointing result, McGeer and Zeldowicz subsequently tested high dosage oral DL‐dopa in six patients with PD and three with postencephalitic parkinsonism.35 They built the oral dose up gradually until 5 gm/d of DL‐dopa was reached. They treated 10 patients (six PD, three postencephalitic, and one arteriosclerotic) for several days. Two showed some benefit. The authors concluded in 1964 that dopa has little to offer as a therapeutic agent in the treatment of parkinsonism.
Hornykiewicz, himself, at a symposium in 1965, concluded that the role of L‐dopa in the treatment of PD is unsettled because of its side effects.36 Roger Duvoisin in New York, in his review on the therapy of PD in 1965, also did not place much therapeutic value to levodopa.37
Did the contributions by Hornykiewicz, Birkmayer or McGeer influence Cotzias to evaluate DL‐ or L‐dopa in PD? The answer is “no.” In Cotzias' 1967 DL‐dopa paper,1 he cites Hornykiewicz's report of brain dopamine depletion and wonders if that finding is related to the loss of neuromelanin in PD. Cotzias also cites the clinical results of Birkmayer and Hornykiewicz and those of McGeer and colleagues and points out that their results disagree with each other. So, why did Cotzias administer high dosage DL‐dopa? Cotzias had a hypothesis that PD is due to a loss of neuromelanin in the substantia nigra,38, 39 and if this pigment can be increased, perhaps this would ameliorate the symptoms of PD. The first drug Cotzias tested was not DL‐dopa but melanocyte‐stimulating hormone.1 Instead of improving the patients, however, this agent worsened their Parkinson condition. Cotzias speculated that the resulting stimulation of skin melanocytes may have diverted the supply of dopa from brain to skin. Cotzias next tested DL‐dopa because dopa is a precursor to neuromelanin. Cotzias knew that L‐dopa would be the active agent, but this amino acid would be enormously expensive, and therefore DL‐dopa was used. The dramatic results were mentioned above. After observing the benefits from DL‐dopa, Cotzias substituted DL‐phenylalanine for it because phenylalanine is a precursor of dopa, and this amino acid was also expected to provide benefit. However, the administration of phenylalanine resulted in an aggravation of PD. Today, we could interpret this result as providing a large amino acid that would compete against tyrosine for uptake into the brain via the active transport system. Tyrosine is the immediate direct precursor to dopa. In the discussion of the results, Cotzias did not fully accept the explanation that restoration of brain dopamine is the mechanism for the benefit provided by DL‐dopa, but he did not exclude this possibility either.
Cotzias attributed his successful result with DL‐dopa, in contrast to those of McGeer and others, to his ability to build up the dosage of DL‐dopa slowly over months by having his patients remain in a government research hospital, thereby avoiding the gastrointestinal side effects that occurs with a rapid increase in the dosage of dopa.
The impact of Cotzias' success with high dosage DL‐ and L‐dopa to treat PD and other forms of parkinsonism goes far beyond helping the people with parkinsonism. True, after more than 50 years of levodopa being commercially available for treating parkinsonism, levodopa remains the “gold standard” of therapy for the motor features of PD.40 The introduction of levodopa cut the 3‐fold elevated mortality rate in half for people with PD,41 although with long‐term usage of levodopa, the mortality rate has climbed back up somewhat.42 Beyond the importance of levodopa as a therapy for patients, the presence of levodopa therapy attracted more clinicians and scientists to join the study of dopamine in the nervous system. Further investigations have led to a more comprehensive understanding of brain physiology and function. They led to a realization of the role of dopamine in psychiatric conditions, addiction, and reward behavior. In neurology, dopamine was found to play a role not just in parkinsonism but also in hyperkinetic disorders such as dystonia, tardive dyskinesia, and chorea. The utilization of high‐dosage levodopa therapy was a key factor in the development of the subspecialty of movement disorders, leading to the founding of The Movement Disorder Society.
Author Roles
(1) Research Project: A. Conception, B. Organization, C. Execution; (2) Statistical Analysis: A. Design, B. Execution, C. Review and Critique; (3) Manuscript Preparation: A. Writing of the first draft, B. Review and Critique.
S.F.: 3A, 3B
Disclosures
Ethical Compliance Statement
The approval of an institutional review board was not required for this work, nor was informed patient consent. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Funding Sources and Conflicts of Interest
No funding was received for this work, and the author has no conflicts to report.
Financial Disclosures from Previous 12 Months
SF has received honoraria from Springer publishers as co‐editor and royalty from Elsevier publishers as book co‐author.
References
- 1.Cotzias GC, Van Woert MH, Schiffer LM. Aromatic amino acids and modification of parkinsonism. N Engl J Med 1967;276:374–379. [DOI] [PubMed] [Google Scholar]
- 2.Cotzias GC, Papavasiliou PS, Gellene R. Modification of parkinsonism—chronic treatment with L‐dopa. N Engl J Med 1969;280:337–345. [DOI] [PubMed] [Google Scholar]
- 3.Cotzias GC, Papavasiliou PS. Therapeutic studies in parkinsonian patients: Long‐term effects of DL‐ and L‐dopa. In: Barbeua A, Brunette J‐R, eds. Progress in Neuro‐Genetics. Amsterdam, The Netherlands: Excerpta Medica Foundation International Congress Series No. 175; 1969:357–365. [Google Scholar]
- 4.Yahr MD, Duvoisin RC, Schear MJ, Barrett RE, Hoehn MM. Treatment of parkinsonism with levodopa. Arch Neurol 1969;21(4):343–354. [DOI] [PubMed] [Google Scholar]
- 5.Klawans HL Jr, Garvin JS. Treatment of parkinsonism with L‐dopa (study of 105 patients). Dis Nerv Syst 1969;30(11):737–746. [PubMed] [Google Scholar]
- 6.Calne DB, Stern GM, Spiers AS, Laurence DR. L‐dopa in idiopathic parkinsonism. Lancet 1969;2(7628):973–976. [DOI] [PubMed] [Google Scholar]
- 7.Mones RJ, Elizan TS, Siegel GJ. Evaluation of L‐dopa therapy in Parkinson's disease. N Y State J Med 1970;70:2309–2318. [PubMed] [Google Scholar]
- 8.Mawdsley C. Treatment of parkinsonism with Laevo‐dopa. Br Med J 1970;1(5692):331–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rinne UK, Sonninen V, Siirtola T. L‐dopa treatment in Parkinson's disease. Eur Neurol 1970;4(6):348–369. [DOI] [PubMed] [Google Scholar]
- 10.Schwarz GA, Fahn S. Newer medical treatment in parkinsonism. Med Clin North Am 1970;54:773–785. [PubMed] [Google Scholar]
- 11.McDowell F, Lee JE, Swift T, Sweet RD, Ogsbury JS, Kessler JT. Treatment of Parkinson's syndrome with dihydroxyphenylalanine (levodopa). Ann Int Med 1970;72:29–35. [DOI] [PubMed] [Google Scholar]
- 12.Kofman O. Treatment of Parkinson's disease with L‐dopa: a current appraisal. Can Med Assoc J 1971;104(6):483–487. [PMC free article] [PubMed] [Google Scholar]
- 13.Treciokas LJ, Ansel RD, Markham CH. One to two year treatment of Parkinson's disease with levodopa. Calif Med 1971;114:7–14. [PMC free article] [PubMed] [Google Scholar]
- 14.Nakano KK, Tyler HR. A double‐blind study of the effects of levodopa in Parkinson's disease. Neurology 1971;21(10):1069–1074. [DOI] [PubMed] [Google Scholar]
- 15.Fehling C. Treatment of Parkinson's syndrome with L‐DOPA on an out‐patient basis. Z Neurol 1972;202(3):197–208. [DOI] [PubMed] [Google Scholar]
- 16. https://laskerfoundation.org/winners/l-dopa-for-treating-parkinsons-disease/
- 17.News Item . Parkinsonism: L‐Dopa goes commercial. Chem Eng News 1970;48:12. [Google Scholar]
- 18.Fahn S. The medical treatment of Parkinson disease from James Parkinson to George Cotzias. Mov Disord 2015;30(1):4–18. [DOI] [PubMed] [Google Scholar]
- 19.Carlsson A, Lindqvist M, Magnusson T. 3,4‐dihydroxyphenylalanine and 5‐hydroxytryptophan as reserpine antagonists. Nature 1957;180:1200. [DOI] [PubMed] [Google Scholar]
- 20.Carlsson A, Lindqvist M, Magnusson T, Waldeck B. On the presence of 3‐hydroxytyramine in brain. Science 1958;127:471. [DOI] [PubMed] [Google Scholar]
- 21.Carlsson A.A half‐century of neurotransmitter research: impact on neurology and psychiatry. Nobel Lecture, December 8, 2000. https://www.nobelprize.org/uploads/2018/06/carlsson-lecture.pdf [DOI] [PubMed]
- 22.Bertler A, Rosengren E. Occurrence and distribution of catechol amines in brain. Acta Physiol Scand 1959;47:350–61. [PubMed] [Google Scholar]
- 23.Sano I, Gamo T, Kakimoto Y, Taniguchi K, Takesada M, Nishinuma K. Distribution of catechol compounds in human brain. Biochim Biophys Acta 1959;32:586–587. [DOI] [PubMed] [Google Scholar]
- 24.Carlsson A. The occurrence, distribution and physiological role of catecholamines in the nervous system. Pharmacol Rev 1959;11:490–493. [PubMed] [Google Scholar]
- 25.Degkwitz R, Frowein R, Kulenkampff C, Mohs U. Über die Wirkungen des L‐DOPA beim Menschen und deren Beeinflussung durch Reserpin, Chlorpromazin, Iproniazid und Vitamin B6. [On the effects of L‐dopa in man and their modification by reserpine, chlorpromazine, iproniazid and vitamin B6]. Klin Wochenschr 1960;38:120–123. [DOI] [PubMed] [Google Scholar]
- 26.Hornykiewicz O. Dopamine miracle: from brain homogenate to dopamine replacement. Mov Disord 2002;17:501–508. [DOI] [PubMed] [Google Scholar]
- 27.Ehringer H, Hornykiewicz O. Verteilung von Noradrenalin und Dopamin (3‐Hydroxytryamin) im Gehirn des Menschen und ihr Verhalten bei Erkrankungen des extrapyramidalen Systems. [Distribution of noradrenaline and dopamine (3‐hydroxytyramine) in the human brain and their behavior in diseases of the extrapyramidal system]. Klin Wochenschr 1960;38:1236–1239. (English translation can be found in Parkinsonism Relat Disord. 1998;4:53–57.).13726012 [Google Scholar]
- 28.Hornykiewicz O. [The tropical localization and content of noradrenalin and dopamine (3‐hydroxytyramine) in the substantia nigra of normal persons and patients with Parkinson's disease]. Wien Klin Wochenschr 1963;75:309–312. [PubMed] [Google Scholar]
- 29.Hornykiewicz O. Dopamine (3‐hydroxytyramine) and brain function. Pharmacol Rev 1966;18:925–964. [PubMed] [Google Scholar]
- 30.Bernheimer H, Birkmayer W, Hornykiewicz O, Jellinger K, Seitelberger F. Brain dopamine and the syndromes of Parkinson and Huntington. J Neurol Sci 1973;20:415–455. [DOI] [PubMed] [Google Scholar]
- 31.Sano H. Biochemistry of the extrapyramidal system. Parkinsonism Relat Disord 2000;6(1):3–6. (English translation from original in Shinkei Kennkyu No Shinpo [Advances in Neurological Sciences]. 1960;5:42–48.). [DOI] [PubMed] [Google Scholar]
- 32.Birkmayer W, Hornykiewicz O. Der L‐3,4‐Dioxyphenylalanin (DOPA)‐Effekt bei der Parkinson‐Akinese. [The effect of L‐3,4‐dihydroxyphenylalanine (= DOPA) on akinesia in parkinsonism.]. Wien Klin Wochenschr 1961;73:787–788. (English translation available in Parkinsonism Relat Dis 1998;4:59–69.).13869404 [Google Scholar]
- 33.Birkmayer W, Hornykiewicz O. Weitere experimentelle Untersuchungen űber L‐DOPA beim Parkinson‐Syndrom und Reserpin‐Parkinsonismus. [Additional experimental studies on L‐dopa in Parkinson's syndrome and reserpine parkinsonism.]. Arch Psychiatr Nervenkr 1964;206:367–381. [DOI] [PubMed] [Google Scholar]
- 34.McGeer PL, Boulding JE, Gibson WC, Foulkes RG. Drug‐induced extrapyramidal reactions. Treatment with diphenhydramine hydrochloride and dihydroxyphenylalanine. JAMA 1961;177:665–670. [DOI] [PubMed] [Google Scholar]
- 35.McGeer PL, Zeldowicz LR. Administration of dihydroxyphenylalanine to parkinsonian patients. Can Med Assoc J 1964;90:463–466. [PMC free article] [PubMed] [Google Scholar]
- 36.Hornykiewicz O. Metabolism of brain dopamine in human parkinsonism: neurochemical and clinical aspects. In: Costa E, Côté LJ, Yahr MD, eds. Biochemistry and Pharmacology of the Basal Ganglia. Hewlett, NY: Raven Press; 1966:171–185. [Google Scholar]
- 37.Duvoisin RC. A review of drug therapy in parkinsonism. Bull N Y Acad Med 1965;41:898–910. [PMC free article] [PubMed] [Google Scholar]
- 38.Cotzias GC, Papavasiliou PS, Van Woert MH, Sakamoto A. Melanogenesis and extrapyramidal diseases. Fed Proc 1964;23:713–718. [PubMed] [Google Scholar]
- 39.Cotzias GC. Manganese, melanins and the extrapyramidal system. J Neurosurg 1966;24(1):170–180. [PubMed] [Google Scholar]
- 40.Jankovic J, Hallett M, Okun MS, Comella C, Fahn S. Medical treatment of the motor features of Parkinson disease. Principles and Practice of Movement Disorders. 3rd ed.London: Elsevier; 2021;164–203. [Google Scholar]
- 41.Yahr MD. Evaluation of long‐term therapy in Parkinson's disease: mortality and therapeutic efficacy. In: Birkmayer W, Hornykiewicz O, eds. Advances in Parkinsonism. Basel: Editiones Roche; 1976:435–443. [Google Scholar]
- 42.Morgan JC, Currie LJ, Harrison MB, Bennett JP Jr, Trugman JM, Wooten GF. Mortality in levodopa‐treated Parkinson's disease. Parkinsonʼs Dis 2014;2014:426976. 10.1155/2014/426976. [DOI] [PMC free article] [PubMed] [Google Scholar]


