Abstract
Background
Suicide and risk factors have been poorly studied in the Muslim‐majority countries that hinder the formulation of prevention strategies and affect suicide prevention eventually.
Objectives
We aimed at identifying and analyzing the psychological autopsy studies assessing the risk factors for suicide conducted in Muslim‐majority countries.
Methods
We did a search to trace all the available psychological autopsy studies in the Muslim countries with the search term “psychological autopsy study in Muslim countries.” We also checked the available bibliographies to identify the psychological autopsy studies in the Muslim countries so that all the possible studies could be included.
Results
Out of the Muslim countries, only eight psychological autopsy studies were identified in five countries (Bangladesh [1], Indonesia [1], Iran [1], Pakistan [2], and Turkey [3]). Six studies adopted a case‐control study design, and all were carried out in urban settings. The prevalence of psychiatric disorders among case‐control studies varied from 52.8% in Turkey to 96% in Pakistan. Psychiatric illness, self‐harm, and stressful life events were the commonly replicated risk factors for suicide across studies.
Conclusions
Psychological autopsy studies have been conducted only in five Muslim countries revealing that the risk factor for suicide is certainly under‐researched in the incumbent countries. This review identified a similar list of risk factors for suicide, namely, psychiatric disorder, past non‐fatal attempts, and adverse life events compared to the Western countries even though the rate varies.
Keywords: case‐control study, Muslim countries, psychological autopsy, risk factors, suicide
1. INTRODUCTION
Suicide is a public health problem affecting people of all religions and age groups all over the world.1, 2 Every year 7, 03000 people die by suicide, whilst someone is dying every 40 seconds.1 Suicide not only results in direct loss lives but also has disruptive psychosocial and adverse socioeconomic effects. However, with adequate services and timely interventions, it can be prevented.3 The determination of the actual rate and risk factors of suicide is an important step in preventing suicide, which is often complicated by cultural, social, and religious factors.4, 5, 6
Suicide is a multifaceted phenomenon that results from several risk factors, including a family history of suicide, genetic loading, traumatic life events,7 psychosocial stressors, socioeconomic factors, underlying psychiatric illnesses,8 personality traits, loss of social support,2 previous suicidal behaviors,5, 9 and cognitive distortions.10, 11, 12 However, variations have been noted in regard to the risk factors from culture to culture, time to time, and country to country.13
Suicide has been decriminalized in most of the Western countries or countries with the least number of Muslims, whereas in the Muslim‐majority countries, it is strictly condemned as per the Islamic law and considered as an illegal/criminal offense with financial/or imprisonment penalty. The majority of Muslim countries, namely, Afghanistan, Pakistan, Kuwait, Algeria, Morocco, Oman, Brunei Darussalam, Indonesia, Djibouti, Somalia, Bahrain, Qatar, Sudan, Albania, Iraq, United Arab Emirates, Malaysia, Saudi Arabia, and Bangladesh, follow the Islamic Shariah law.14, 15 The legally imposed punishment for suicidal behavior hinders help‐seeking due to the fear of legal procedures and inconsistent jurisprudence.14
Although suicide is a global public health priority, there is a dearth of research in suicide in the Muslim‐majority countries.16 In addition, very few Muslim countries such as Brunei Darussalam, Kazakhstan, Turkey, and Kyrgyzstan report suicide to WHO,4, 17, 18 whereas many other countries, such as Pakistan, Kuwait, Bangladesh, Oman, Algeria, Saudi Arabia, Sudan, Afghanistan, Indonesia, and Somalia, do not report suicide statistics to WHO.15, 16 Furthermore, they lack a proper country‐based suicide registration system.18 The existing religious, social, and legal taboos linked with suicidal behavior hinder the suicide disclosure.2
Psychiatric disorders have been identified as an important risk factor for suicide across the globe whilst mostly studied in the Western countries.3, 5, 10, 13, 19, 20 However, mental illness arises in every culture and it has progressively been recognized as a risk factor for suicidal behaviors in the Muslim countries also.21, 22 Studies from Muslim countries identified that psychological disorders such as depression, neuroticism, obsession‐compulsion, pessimism, and anxiety are comparatively higher in Muslims than those in the Western samples.23, 24, 25 It is obvious that in spite of all the cultural and religious barriers, being a Muslim does not prohibit one from having such suicidal tendencies along with psychiatric disorders.4, 24
There are approximately 1.9 billion Muslims globally, making Islam the second‐largest religion living in about 50 countries and territories clustered in Asia and Africa.26 It is important to review the risk factors and the actual rate of suicide in Muslim countries to better understand the phenomenon, which will further provide the path to future research and design intervention strategies, thus helping to curb the menace. Henceforth, we aimed at identifying and analyzing the psychological autopsy (PA) studies assessing the risk factors for suicide conducted in Muslim‐majority countries. The purpose of this study was not only to evaluate the magnitude of studies addressing the risk factors of suicide in Muslim countries but also to identify the domains of major risk factors responsible for suicide. Also, we opted to compare the prevalence of psychiatric disorders in suicides among the studies conducted in Muslim countries.
2. METHODS
2.1. Search strategy
A search was performed by the first author to identify the original PA studies from Muslim countries. The search was carried out in PubMed, PubMed Central, Scopus, Google Scholar, and Google with the search term “psychological autopsy study in Muslim countries,” “psychological autopsy study in… (individual country name)” (Data S1). Subsequently, two other authors (third and fourth authors) checked and validated the articles by separate searches. We also did a snow‐balling to identify all the studies in Muslim countries. The original articles of the PA study from Muslim countries published from inception till the end of 2020 were included (Figure 1).
FIGURE 1.
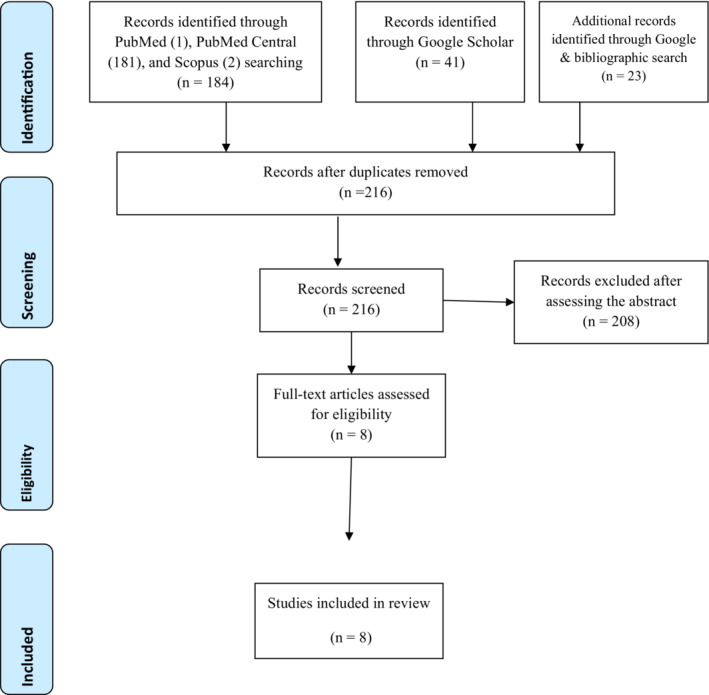
PRISMA 2009 flow diagram
2.2. Inclusion criteria
Original contributions, quantitative studies, articles published in the English language, PA studies from Muslim countries, and studies with full‐accessible text were included. The term “psychological autopsy” had to be identified in the title and/or abstract for the initial search.
2.3. Exclusion criteria
Studies other than the original contribution such as review, commentary, correspondence, viewpoints, editorials, and case studies were excluded. We also excluded qualitative studies.
2.4. Data extraction
We identified and reviewed eight original papers from Muslim countries. The studies were found in five countries (Bangladesh [1], Indonesia [1], Iran [1], Pakistan [2], and Turkey [3]). The characteristics are presented in Table 1.
TABLE 1.
Psychological autopsy studies in Muslim countries (n = 8)
| S. no | Study | Place of study | Study design | Study duration (mo) | Data collection method | Study population | Sample size | M:F | Age of suicide Mean (±SD) [range] |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Arafat et al27 | Dhaka, Bangladesh | Case‐control | 13 | Interview | General population | Case 100; control 100 | 0.96:1 | 26.30 (±12.36) [9‐75] |
| 2 | Kurihara et al28 | Bali, Indonesia | Case‐control | 4 | Interview | General population | Cases 60; controls 120 | 1.72:1 | 41.4 (±21.5) [13‐87] |
| 3 | Rasouli et al29 | Tehran, Iran | Case‐control | 6 | Interview | General population over 18 y of age | Case 40; control 40 | 4:1 | 39.4 (±16) [19‐75] |
| 4 | Khan et al30 | Karachi, Pakistan | Case‐control | 12 | Interview | General population | Case 100; control 100 | 4.88:1 | |
| 5 | Abdullah et al31 | Khyber Pakhtunkhwa, Pakistan | Case series | 6 | Interview and document review | Youth (12‐26 y) | 63 | 1.52:1 | 22.1 (±3.08) |
| 6 | Oguzhanoglu et al32 | Anatolia, Turkey | Case‐control | 24 | Interview and document review | General population | Case 53; control 31 | 6.57:1 | 46.6 (±26.10) |
| 7 | Taktak et al33 | Istanbul, Turkey | Case series | Interview and document review | General population | 124 | 2.02:1 | 35.4 (±16.5) | |
| 8 | Altindag et al34 | Anatolia, Turkey | Case‐control | 12 | Interview | General population | Case 26; control 25 | 0.58:1 | 24.2 (±11.3) |
2.5. Quality assessment
Two authors (VM and SAZA) independently assessed the methodological quality of included studies using the Newcastle‐Ottawa Quality Assessment Scale for case‐control studies (Data S2). The tool evaluates the quality of studies under the following broad perspectives: (a) selection of study groups (four items), (b) comparability of study groups (one item), and (c) ascertainment of exposure for the groups (three items). A maximum of one star is allocated for each numbered item except for the comparability item where a maximum of two stars can be allocated; thus, the total scores range from 0 to 9 where 0 to 3, 4 to 6, and 7 to 9 are considered as low‐, moderate‐, and high‐quality studies, respectively.35
2.6. Ethical aspects
As we reviewed publicly available already published papers, no institutional review board clearance was sought for conducting the study.
3. RESULTS
3.1. Psychological autopsy studies in Muslim countries
A total of eight PA studies have been identified in Muslim‐majority countries; of these, three were from Turkey, two from Pakistan, and one each from Iran, Indonesia, and Bangladesh. The earliest such study was carried out in 2005 in Turkey; four of the remaining seven studies have been conducted in the last 3 years. Except for two case series studies, all others used a case‐control design. The study duration ranged from 4 to 24 months. Males constituted the majority of the sample in most studies except for one study each from Turkey and Bangladesh (Table 1). All the studies in this review used semistructured interview method, supplemented by a review of additional documents to extract information. The study population was the general adult population in nearly all studies except one where the authors specifically studied suicide in adolescents and young adults.
3.2. Religion of the suicides
We searched and collected studies from Muslim‐majority countries. However, only one study explicitly mentioned the proportion of Muslim suicides (96%) in Pakistan.30 The Indonesian study was conducted in Bali, which is a Hindu majority area, and the proportion of suicides based on the religion was not mentioned.28
3.3. Psychiatric disorders among suicides in Muslim countries
All studies used a Diagnostic and Statistical Manual of Mental Disorders (DSM) classificatory instrument such as Structured Clinical Interview for DSM Axis‐I Disorders (SCID‐I), SCID‐II, DSM‐IV, and DSM‐V except for a study in Pakistan that used the International Classification of Diseases, Tenth Revision (ICD‐10), to identify the mental disorders (Table 2). All the studies were carried out in urban settings. More than half of the decedents, across all the studies in this review, were diagnosed with mental disorders and the figures ranged from 52.8% in Turkey to 96% in Pakistan. Personality disorder was assessed in only two case‐control studies from Bangladesh and Pakistan (Table 2). A past history of suicide attempts was found in 6% to 42.5% of decedents (Table 2). Six studies reported proportion under mental health services coverage; the figures were widely varying in the two studies from Pakistan and ranged from 3% to 71.4%; in other countries, figures were more consistent and ranged from 13% to 16.1% (Table 2).
TABLE 2.
Prevalence of psychiatric disorders among suicides in Muslim countries
| S. no | Study | Study setting | Instruments | Prevalence of psychiatric disorder | Assessment of personality disorder | Prevalence of past attempt | Proportion under mental health services |
|---|---|---|---|---|---|---|---|
| 1 | Arafat et al27 | urban, Bangladesh | SCID‐I (DSM‐IV‐TR); SCID‐II, Paykel's life events schedule | 61% | Yes | 14% | 13% |
| 2 | Kurihara et al28 | Urban, Indonesia | SCID‐I (DSM‐IV‐TR), duke social support index | 80% | 20% | 13.3% | |
| 3 | Rasouli et al29 | Urban, Iran | SCID‐I, SUPREMISS, Spielberger's state‐trait anger scale, Dickman impulsivity questionnaire | 82.5% | 42.5% | ||
| 4 | Khan et al30 | Urban, Pakistan | ICD‐10, personality assessment schedule, Paykel's life events schedule | 96% | Yes | 6% | 3% |
| 5 | Abdullah et al31 | Urban, Pakistan | Diagnostic statistic manual for mental disorders (DSM) 5 | 71.4% | Yes | 36.5% | 71.4% |
| 6 | Oguzhanoglu et al32 | Urban, Turkey | DSM‐IV, PERI life event scale | 52.8% | |||
| 7 | Taktak et al33 | Urban, Turkey | DSM‐IV | 61.3% | 12.9% | 16.1% | |
| 8 | Altindag et al34 | urban, Turkey | DSM‐IV, PERI life event scale | 69% | 15% |
3.4. Risk factors for suicide in Muslim countries
Pre‐existing psychiatric illness and stressful life events were the commonly replicated risk factors for suicide across studies in Muslim countries. A past suicide attempt was noted to be a risk factor in two studies each from Turkey and Pakistan, one each from Iran and Bangladesh. Unemployment and substance use were recorded as risk factors in a study each from Turkey, Pakistan, and Iran. Likewise, interpersonal conflicts were noted to be a risk factor in a study from Indonesia and Pakistan (Table 3). A low level of religious involvement was an observed risk factor in an Indonesian study, whereas a lack of support was noted by Turkish studies (Table 3).
TABLE 3.
Risk factors for suicide in Muslim countries
| S. no | Study | Study setting | Study design | Major risk factors |
|---|---|---|---|---|
| 1 | Arafat et al27 | Urban, Bangladesh | Case‐control | Psychiatric disorder, past attempt, life event, sexual abuse |
| 2 | Kurihara et al28 | Urban, Indonesia | Case‐control | Psychiatric disorder, low level of religious interest, severe interpersonal troubles |
| 3 | Rasouli et al29 | Urban, Iran | Case‐control | Psychiatric disorder, past attempt, smoking, unemployment |
| 4 | Khan et al30 | Urban, Pakistan | Case‐control | Psychiatric disorder, being married, unemployment, lower education, life event. |
| 5 | Abdullah et al31 | Urban, Pakistan | Case series | Psychiatric disorder, substance abuse, past attempt, irritability, low self‐esteem, non‐compliance, family disharmony, financial hardness |
| 6 | Oguzhanoglu et al32 | Urban, Turkey | Case‐control | Psychiatric disorder, past attempt, life event, lack of social support |
| 7 | Taktak et al33 | Urban, Turkey | Case series | Psychiatric disorder, past attempt, unemployment, substance abuse |
| 8 | Altindag et al34 | Urban, Turkey | Case‐control | Psychiatric disorder, life event |
3.5. Quality assessment
Risk of bias was noted in selected domains in all the included studies. All the included studies defined cases of suicide based on hospital or government records without independent validation (Data S2). Comparability of groups was lower among one study each from Turkey34and Indonesia.28 Although structured interviews were conducted in all the studies, the interviewer was not blinded to case‐control status and hence ascertainment bias was observed in all studies with a control group.27, 29, 30, 31, 32, 33 One study used different assessment methods for cases and controls (telephonic interview for all controls vs a mixture of face‐to‐face and telephonic interview for cases).32 Overall, two studies were rated as high‐quality and29, 30 four as moderate‐quality27, 31, 32, 34; two others could not be assessed on six of the eight items due to the lack of a control group, and hence, the overall quality cannot be commented upon.31, 33
4. DISCUSSION
We aimed at identifying the PA studies conducted in Muslim countries to assess the extent of the study followed by identifying the risk factors for suicide in Muslim countries from those studies to see whether there is any variation from the Western countries. We systematically searched to scrutinize the available eight studies from five Muslim countries. The major findings of this review include the extent of PA studies in Muslim countries, the prevalence of psychiatric disorders among the suicides and identification of major risk factors for suicide.
4.1. Psychological autopsy studies in Muslim countries
Among the all Muslim countries, PA studies have been identified in only five countries that undisguised an extreme lack of studies as well as attention towards risk factors for suicide. PA method basically uses two components: perusal of available medical, psychiatric, forensic, and police records and collateral interviews with key informants. The aim is to collect as much information on circumstances of death in order to arrive at a conclusion about the mode of death, with as high a degree of certainty as possible. Several studies have examined its validity in terms of diagnostic accuracy, with mostly positive reports although there are discordant voices too. Completeness of information, timing of interview following the event, and use of structured tools are some of the issues that affect the reliability and validity of a PA procedure.36, 37 The recent second‐generation autopsy studies usually utilize the structured objective instruments to diagnose the events and psychiatric disorders, which gives its credibility across settings. However, there are some unavoidable biases can affect that are attributed to whole PA method. It is worthy to consider that there are several methodological challenges to conducting such studies, namely, poor‐quality data, under‐reporting of suicide, criminal status of suicide in the legal system, existing stigma, and social taboos towards suicide. These include stigma in being interviewed for the suicide of a family member, a behavior that is strongly prohibited in Islam, which may affect their willingness to participate in the interviews. Besides, other barriers such as infrastructure and availability of data sources are important feasibility questions. Some suggestions to perform a PA in settings where a case‐control design is not possible due to resource constraints include a multi‐method approach, beginning with open, narrative questions, and moving to semistructured interviews to cover predefined topics, supplemented with questionnaires.38 Recently, Arensman and colleagues have described an optimized methodological approach to a PA that allows for investigating a range of risk and protective factors for suicide whilst also examining consistency across various information sources.39
4.2. Mental health and suicide in Muslim countries
The presence of a mental disorder has been identified as a universal risk factor across the studies in Muslim countries. The current study revealed a variation in the prevalence of psychiatric disorders in suicides among the eight studies those used either SCID/ICD as a assessment tool (Tables 2 and 3). It ranges from 52.8% in Turkey32 to 96% Pakistan.30 There are several possibilities we would like to mention here. First, these figures are in the same direction and highlight the fact that majority of those who die by suicide in Muslim countries have associated psychiatric morbidity. Second, the variations between countries may reflect the differences in the level of training and familiarity with the tool (SCID/ICD) of those who administered it as a fair amount of training is critical to the valid use of SCID, even by mental health professionals. Thirdly, it may also reflect actual differences between countries and cultures. Such differences have been identified by well‐designed systematic reviews.10, 19 However, the proportions are lower when compared to the Western countries except one study from Pakistan where the prevalence was 96%.30 However, criminal status, religious prohibition, lower mental health literacy, and a higher stigma could disguise the psychiatric morbidities among the suicides in the incumbent countries. According to the latest report of WHO, the rate of suicide has been found lower in the Muslim countries than the global rate. For example, the global age‐standardized rate of suicide was 9.0 per 100 000 population for 2019, whereas it was 3.9 for Bangladesh, 2.6 for Indonesia, 5.1 for Iran, 9.8 for Pakistan, and 2.3 for Turkey per 100 000 population for the same year.1 Therefore, it has been thought that religion has some sort of protective effect in Muslim countries. However, that protective effect of religious affiliation may be marred by the presence of psychiatric morbidity, which may cloud judgment and influence irrational behaviors. In this regard, it is pertinent to note that substance use, which may also impair judgment, was found to be a risk factor for suicide in some of the reviewed studies (Table 3). The proportion of suicide decedents utilizing mental health services were remarkably similar across the studies reviewed except for one outlier study. These results are consistent with global findings as well as country‐specific findings that suggest that over 70% of people with common and severe mental illness report do not seek professional help.40 Public stigma against mental illness remains a major barrier to seeking appropriate treatment for people with mental illness apart from structural barriers such as cost and accessibility due to distance. These findings have implications for the restructuring of mental health care service delivery; involving private and traditional health care providers, and training and supervising their ability to detect and manage common mental illness may help surmount barriers to service utilization; and preliminary evidence of these strategies is available from Asian settings and needs further evaluation in other regions.41 There may also be some merit in investigating the characteristics of “no‐contact suicides” in Muslim regions to aid referral and suicide prevention efforts.42 The use of mHealth strategies may also help to address structural barriers to care and the stigma associated with in‐person consults.43
4.3. Risk factors for suicide in Muslim countries
Pre‐existing psychiatric morbidity, past attempt, unemployment, triggering life events, and interpersonal troubles were the most common risk factors for suicide in studies from Bangladesh, Pakistan, Indonesia, and two studies from Turkey (Table 3). These findings concur with reports from Asian settings where life events and interpersonal conflicts have been noted to be major drivers of suicide, unlike the West where psychiatric morbidity remains the principal risk factor.8, 10, 19, 44 Previous studies from Turkey, a transcontinental country located both in Asia and in Europe, have shown the key role of stressful life events and poor social support in triggering suicidal behavior across age groups.45, 46 Our findings imply that suicide prevention efforts in Muslim nations must also focus adequately on the social determinants of suicide, apart from addressing barriers to seeking mental health services, to effectively tackle the menace of suicide.
4.4. What is already known
Suicide is a global problem. However, most of the review studies about the risk factors for suicide using a case‐control approach have been conducted in non‐Muslim countries.10, 19, 47, 48, 49 and the literature regarding the burden and risk factors for suicide using a case‐control PA approach in Muslim countries is limited.
4.5. What this study adds
The literature on PA from Muslim countries remains scanty even though, in recent years, studies are coming out. We could not find any PA study in any African Muslim country. This review identified the extent of PA studies across the Muslim countries. Also, it showed the major risk factors for suicides that are similar to the Western countries in regard to the areas of risk factors.
4.6. Strength of the study
This is the first review assessing the PA studies in Muslim countries identifying the risk factors, prevalence of mental disorders, and research gaps. We tried to include all the possible studies to include in the review.
4.7. Limitations of the study
We included the studies published only in the English language. There are variations in the methodology, study population, sample size, and prevalence of mental disorders. The articles did not clearly mention the suicides based on the religion. Personality disorders were assessed only in two countries (Bangladesh and Pakistan).
5. CONCLUSIONS
PA studies have been conducted only in five Muslim countries revealing that the risk factor for suicide is certainly under‐researched in Muslim countries. This review identified a similar list of risk factors for suicide, namely, psychiatric disorder, past non‐fatal attempts, and adverse life events compared to the Western countries. As Muslims comprised an important proportion of the global population with a lower suicide rate, a need arises to look into the risk and resilient factors for suicide based on the religion and religiosity.
CONFLICT OF INTEREST
The authors declare there is no conflict of interest.
TRANSPARENCY STATEMENT
The lead author S. M. Yasir Arafat affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
AUTHORS' CONTRIBUTIONS
Conceptulization: S. M. Yasir Arafat, Murad M. Khan, Mohsen Rezaeian.
Data Curation: S. M. Yasir Arafat, Syeda Ayat‐e‐Zainab Ali, Sheikh Shoib.
Formal Analysis: S. M. Yasir Arafat, Vikas Menon, Syeda Ayat‐e‐Zainab Ali, Sheikh Shoib.
Investigation: S. M. Yasir Arafat.
Methodology: S. M. Yasir Arafat.
Project Administration: S. M. Yasir Arafat.
Supervision: S. M. Yasir Arafat, Murad M Khan, Mohsen Rezaeian.
Validation: S. M. Yasir Arafat.
Visualization: S. M. Yasir Arafat.
Writing – Original Draft Preparation: S. M. Yasir Arafat, Vikas Menon, Syeda Ayat‐e‐Zainab Ali.
Writing – Review & Editing: S. M. Yasir Arafat, Murad M. Khan, Vikas Menon, Syeda Ayat‐e‐Zainab Ali, Mohsen Rezaeian, Sheikh Shoib.
All authors have read and approved the final version of the manuscript.
The corresponding author had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
Supporting information
Data S1. List of the Muslim countries
Data S2. Quality assessment of the articles by Newcastle‐Ottawa scale (NOS) (n = 8)
ACKNOWLEDGEMENT
None.
Arafat SMY, Khan MM, Menon V, Ali S‐Z, Rezaeian M, Shoib S. Psychological autopsy study and risk factors for suicide in Muslim countries. Health Sci Rep. 2021;4:e414. doi: 10.1002/hsr2.414
Funding information: None.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.
REFERENCES
- 1.World Health Organization . Suicide in the world: Global Health Estimates. Geneva, Switzerland: World Health Organization; 2019. [Google Scholar]
- 2.Al‐Harrasi A, Al Maqbali M, Al‐Sinawi H. Surviving a suicide attempt. Oman Med J. 2016;31(5):378‐380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawton K, Witt KG, Salisbury TLT, et al. Psychosocial interventions following self‐harm in adults: a systematic review and meta‐analysis. Lancet Psychiatry. 2016;3(8):740‐750. [DOI] [PubMed] [Google Scholar]
- 4.Pritchard C, Iqbal W, Dray R. Undetermined and accidental mortality rates as possible sources of underreported suicides: population‐based study comparing Islamic countries and traditionally religious Western countries. BJPsych Open. 2020;6(4):e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zalsman G, Hawton K, Wasserman D, et al. Suicide prevention strategies revisited: 10‐year systematic review. Lancet Psychiatry. 2016;3(7):646‐659. [DOI] [PubMed] [Google Scholar]
- 6.Arafat SMY, Kabir R. Suicide prevention strategies: which one to consider? SE Asia J Pub Health. 2017;7(1):1‐5. [Google Scholar]
- 7.Buchman‐Schmitt JM, Chu C, Michaels MS, et al. The role of stressful life events preceding death by suicide: evidence from two samples of suicide decedents. Psychiatry Res. 2017;256:345‐352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen YY, Wu KC, Yousuf S, Yip PS. Suicide in Asia: opportunities and challenges. Epidemiol Rev. 2012;34:129‐144. [DOI] [PubMed] [Google Scholar]
- 9.Nock MK, Millner AJ, Joiner TE, et al. Risk factors for the transition from suicide ideation to suicide attempt: results from the Army study to assess risk and resilience in Servicemembers (Army STARRS). J Abnorm Psychol. 2018;127(2):139‐149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cho SE, Na KS, Cho SJ, Im JS, Kang SG. Geographical and temporal variations in the prevalence of mental disorders in suicide: systematic review and meta‐analysis. J Affect Disord. 2016;190:704‐713. [DOI] [PubMed] [Google Scholar]
- 11.Costanza A, D'Orta I, Perroud N, et al. Neurobiology of suicide: do biomarkers exist? Int J Leg Med. 2014;128(1):73‐82. [DOI] [PubMed] [Google Scholar]
- 12.Eskin M. Suicidal behavior in the Mediterranean countries. Clin Pract Epidemiol Ment Health. 2020;16(Suppl‐1):93‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bachmann S. Epidemiology of suicide and the psychiatric perspective. Int J Environ Res Public Health. 2018;15(7):1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mishara BL, Weisstub DN. The legal status of suicide: a global review. Int J Law Psychiatry. 2016;44:54‐74. [DOI] [PubMed] [Google Scholar]
- 15.Pritchard C, Amanullah S. An analysis of suicide and undetermined deaths in 17 predominantly Islamic countries contrasted with the UK. Psychol Med. 2007;37(3):421‐430. [DOI] [PubMed] [Google Scholar]
- 16.Naveed S, Qadir T, Afzaal T, Waqas A. Suicide and its legal implications in Pakistan: a literature review. Cureus. 2017;9(9):e1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gal G, Goldberger N, Kabaha A, et al. Suicidal behavior among Muslim Arabs in Israel. Soc Psychiatry Psychiatr Epidemiol. 2012;47(1):11‐17. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization . WHO methods and data sources for country‐level causes of death 2000‐2016. Geneva, Switzerland: World Health Organization; 2018. [Google Scholar]
- 19.Milner A, Sveticic J, De Leo D. Suicide in the absence of mental disorder? A review of psychological autopsy studies across countries. Int J Soc Psychiatry. 2013;59(6):545‐554. [DOI] [PubMed] [Google Scholar]
- 20.Papaslanis T, Kontaxakis V, Christodoulou C, et al. Suicide in Greece 1992‐2012: a time‐series analysis. Int J Soc Psychiatry. 2016;62(5):471‐476. [DOI] [PubMed] [Google Scholar]
- 21.Eskin M, AlBuhairan F, Rezaeian M, et al. Suicidal thoughts, attempts and motives among university students in 12 Muslim‐majority countries. Psychiatry Q. 2019;90(1):229‐248. [DOI] [PubMed] [Google Scholar]
- 22.Khan MM, Naqvi H, Thaver D, Prince M. Epidemiology of suicide in Pakistan: determining rates in six cities. Arch Suicide Res. 2008;12(2):155‐160. [DOI] [PubMed] [Google Scholar]
- 23.Abdel‐Khalek AM. Neither altruistic suicide, nor terrorism but martyrdom: a Muslim perspective. Arch Suicide Res. 2004;8(1):99‐113. [DOI] [PubMed] [Google Scholar]
- 24.Gearing RE, Alonzo D. Religion and suicide: new findings. J Relig Health. 2018;57(6):2478‐2499. [DOI] [PubMed] [Google Scholar]
- 25.Lester D. Suicide and islam. Arch Suicide Res. 2006;10(1):77‐97. [DOI] [PubMed] [Google Scholar]
- 26.World Population Review . Muslim Majority Countries 2021. Available from https://worldpopulationreview.com/country-rankings/muslim-majority-countries. Accessed June 15, 2021.
- 27.Arafat SMY, Mohit MA, Mullick MSI, Kabir R, Khan MM. Risk factors for suicide in Bangladesh: case‐control psychological autopsy study. BJPsych Open. 2020;7(1):e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kurihara T, Kato M, Reverger R, Tirta IG. Risk factors for suicide in Bali: a psychological autopsy study. BMC Public Health. 2009;9:327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rasouli N, Malakouti SK, Rezaeian M, et al. Risk factors of suicide death based on psychological autopsy method; a case‐control study. Arch Acad Emerg Med. 2019;7(1):e50. [PMC free article] [PubMed] [Google Scholar]
- 30.Khan MM, Mahmud S, Karim MS, Zaman M, Prince M. Case‐control study of suicide in Karachi, Pakistan. Br J Psychiatry. 2008;193(5):402‐405. [DOI] [PubMed] [Google Scholar]
- 31.Abdullah M, Khalily MT, Ahmad I, Hallahan B. Psychological autopsy review on mental health crises and suicide among youth in Pakistan. Asia Pac Psychiatry. 2018;10(4):e12338. [DOI] [PubMed] [Google Scholar]
- 32.Oğuzhanoğlu NK, Uğurlu TT, Acar K, Atesci F. A psychological and social perspective on completed suicides in western Anatolia, Turkey: a case‐control psychological autopsy study. Dusunen Adam. 2018;31(4):331‐339. [Google Scholar]
- 33.Taktak Ş, Uzun İ, Balcıoğlu İ. Gender differences in completed suicides in Istanbul, Turkey. J Affect Disord. 2013;145(3):394‐399. [DOI] [PubMed] [Google Scholar]
- 34.Altindag A, Ozkan M, Oto R. Suicide in batman, southeastern Turkey. Suicide Life Threat Behav. 2005;35(4):478‐482. [DOI] [PubMed] [Google Scholar]
- 35.Wells GA, Shea B, O'Connell DA, et al. The Newcastle‐Ottawa Scale (NOS) for assessing the quality of non randomised studies in meta‐analyses. 2000. Available from http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed April 15, 2021.
- 36.Isometsä ET. Psychological autopsy studies‐a review. Eur Psychiatry. 2001;16(7):379‐385. [DOI] [PubMed] [Google Scholar]
- 37.Hjelmeland H, Dieserud G, Dyregrov K, Knizek BL, Leenaars AA. Psychological autopsy studies as diagnostic tools: are they methodologically flawed? Death Stud. 2012;36(7):605‐626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mérelle S, Van Bergen D, Looijmans M, et al. A multi‐method psychological autopsy study on youth suicides in The Netherlands in 2017: feasibility, main outcomes, and recommendations. PLoS One. 2020;15(8):e0238031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arensman E, Larkin C, McCarthy J, et al. Psychosocial, psychiatric and work‐related risk factors associated with suicide in Ireland: optimised methodological approach of a case‐control psychological autopsy study. BMC Psychiatry. 2019;19(1):275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Utz F, Böge K, Hahn E, et al. Public attitudes towards depression and schizophrenia in an urban Turkish sample. Asian J Psychiatr. 2019;45:1‐6. [DOI] [PubMed] [Google Scholar]
- 41.Patel V, Weiss HA, Chowdhary N, et al. Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): a cluster randomised controlled trial. Lancet. 2010;376(9758):2086‐2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hamdi E, Price S, Qassem T, et al. Suicides not in contact with mental health services: risk indicators and determinants of referral. J Ment Health. 2008;17(4):398‐409. [Google Scholar]
- 43.Brian RM, Ben‐Zeev D. Mobile health (mHealth) for mental health in Asia: objectives, strategies, and limitations. Asian J Psychiatr. 2014;10:96‐100. [DOI] [PubMed] [Google Scholar]
- 44.Arafat SMY, Menon V, Varadharajan N, Kar SK. Psychological autopsy studies of suicide in South East Asia. Indian J Psychol Med. 2021;1‐6. 10.1177/02537176211033643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.OkanIbiloglu A, Atli A, Demir S, et al. The investigation of factors related to suicide attempts in southeastern Turkey. Neuropsychiatr Dis Treat. 2016;12:407‐416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Terzi‐Unsal S, Kapci EG. Risk factors for suicidal behavior: psychosocial risk models with Turkish adolescents. Soc Behav Pers. 2005;33(6):593‐608. [Google Scholar]
- 47.Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33(3):395‐405. [DOI] [PubMed] [Google Scholar]
- 48.Mendez‐Bustos P, de Leon‐Martinez V, Miret M, et al. Suicide reattempters: a systematic review. Harv Rev Psychiatry. 2013;21(6):281‐295. [DOI] [PubMed] [Google Scholar]
- 49.Rukundo GZ, Kemigisha E, Ocan M, et al. A systematic review of the risk factors for suicidal ideation, suicidal attempt and completed suicide among children and adolescents in sub‐Saharan Africa between 1986 and 2018: protocol for a systematic review of observational studies. Syst Rev. 2018;7(1):230. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. List of the Muslim countries
Data S2. Quality assessment of the articles by Newcastle‐Ottawa scale (NOS) (n = 8)
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.


