Philadelphia chromosome-like acute lymphoblastic leukemia (Ph-like or BCR-ABL1-like ALL) is a common and genetically heterogeneous subtype of B-acute lymphoblastic leukemia (B-ALL) associated with high relapse rates and poor clinical outcomes with standard chemotherapy treatment.1,2 Rearrangements in erythropoietin receptor gene (EPOR) comprise 2-5% of Ph-like ALL cases across the pediatric-to-adult age spectrum and are associated with constitutive JAK/STAT signaling activation. 3,4 A recent preclinical study showed sensitivity of EPOR-overexpressing Ba/F3 cell lines and human EPOR-rearranged ALL cells to JAK inhibitors (JAKi),5 a strategy now under clinical investigation in patients with Ph-like ALL.3 Herein, we report three adolescent/young adult (AYA) patients with de novo IGH-EPOR Ph-like ALL with high end-induction measurable residual disease (MRD) treated with post-induction chemotherapy in combination with the JAKi ruxolitinib or multi-tyrosine kinase inhibitor (TKI) ponatinib. We further demonstrate in vitro and in vivo activity of these inhibitors in primary patient leukemia cells or patient-derived xenograft (PDX) models of IGH-EPOR Ph-like ALL (Table 1).
Patient #1 (PAYDRD): An 18 year-old Hispanic/Latina female was diagnosed with National Cancer Institute high-risk B-ALL (NCI HR B-ALL) in December 2016 with an initial white blood cell (WBC) count of 79,000 with 62% peripheral blasts. Cerebrospinal fluid (CSF) showed microscopic evidence of leukemia involvement (CNS2b). Cytogenetics were notable for 46,XX and t(14;19), but fluorescent in situ hybridization (FISH) probes did not identify specific translocation breakpoints. Low density microarray (LDA) analysis of RNA expression demonstrated the kinase-activated Ph-like ALL signature with positive 8-gene and 15-gene scores of 0.739 and 0.956, respectively,3,6 and moderately elevated EPOR expression (Online Supplementary Table S1). ArcherDX FusionPlex (anchored multiplex polymerase chain reaction [PCR]) analysis and next-generation sequencing (NGS) detected IGH-EPOR fusion and partial deletions of IKZF1 (7p12.2) and PAX5 (9p13.2), respectively. The patient was treated with a four-drug induction chemotherapy regimen on the Children’s Oncology Group (COG) AALL1131 phase III clinical trial (clinicaltrials gov. Identifier: NCT02883049) with end-induction flow cytometry (FC) MRD 48%, consistent with induction failure. She received post-induction chemotherapy with ruxolitinib 20 mg/m2 twice-daily 14-days-on/14-days-off/month (DL-2) on the COG AALL1521 phase II clinical trial (clinicaltrials gov. Identifier: NCT02723994)7 with end-consolidation MRD 9.5% and end-interim maintenance I MRD 7.3%. Chemotherapy-associated complications included steroid-induced hyperglycemia and central venous catheter-associated thrombosis and infection. Given her persistently chemorefractory disease, the patient was subsequently treated with autologous CD19 chimeric antigen receptor T-cell immunotherapy tisagenlecleucel in August 2017 on an institutional phase I clinical trial (clinicaltrials gov. Identifier: NCT02906371) and achieved MRD-negative remission that was electively consolidated with a matched-sibling donor (MSD) allogeneic hematopoietic stem cell transplant (HSCT) in April 2018. HSCT complications included chronic pulmonary and skin graft-versus-host disease (GvHD). She remains in continued MRD-negative leukemia remission with 100% donor chimerism at >3 years post-HSCT. PDX modeling from the patient’s diagnostic ALL specimen was attempted and unsuccessful.
Patient #2 (PAZLFZ): A 13 year-old female was diagnosed with NCI HR B-ALL in February 2019 with WBC 201,400 with 69% peripheral blasts. CSF was negative for leukemia (CNS1). Cytogenetics showed high hyperdiploidy (56,XX with +X,+2,+5,+6,+8,+9,+10,+19,+21, +22) in 20% of cells and 46,XX in 80% of cells. LDA analysis was positive for the Ph-like ALL signature3,6 with 8-gene and 15-gene scores of 0.776 and 0.956, respectively, and high EPOR expression (Online Supplementary Table S1). Moderate CRLF2 overexpression was detected without CRLF2 rearrangement and was attributed to hyperdiploidy with +X. ArcherDX FusionPlex and NGS analysis demonstrated IGH-EPOR rearrangement and subclonal KRASG12D mutation. The patient received four-drug induction chemotherapy on the COG AALL1131 trial with end-induction FC MRD 5.7%. She received post-induction chemotherapy with ruxolitinib 50 mg/m2 twice-daily for 14-days-on/14-days-off/month (DL2) on the COG AALL1521 phase II clinical trial7 and achieved remission with end-consolidation MRD <0.01% and end-interim maintenance 1 MRD 0%. Chemotherapy-associated complications included methotrexate-associated neurotoxicity with successful intrathecal chemotherapy rechallenge, pulmonary nodules treated with posaconazole, malnutrition requiring supplemental nasogastric feeding, and humeral avascular necrosis requiring discontinuation of prednisone chemotherapy in maintenance cycle 5. She remains in clinical remission on the AALL1521 trial with end-oftherapy in June 2021. Her diagnostic ALL specimen was not available for PDX modeling.
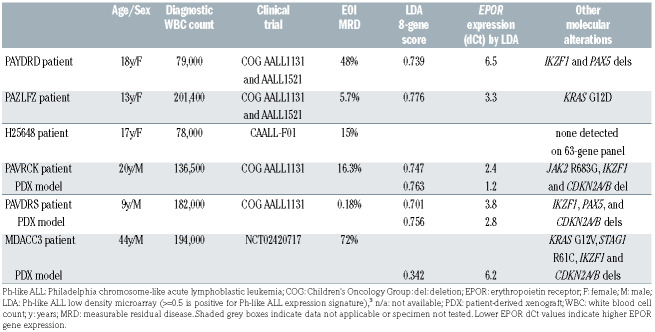
Table 1.
Genetic and demographic characteristics of IGH-EPOR Philadelphia chromosome-like acute lymphoblastic leukemia patients and patient-derived xenograft models.
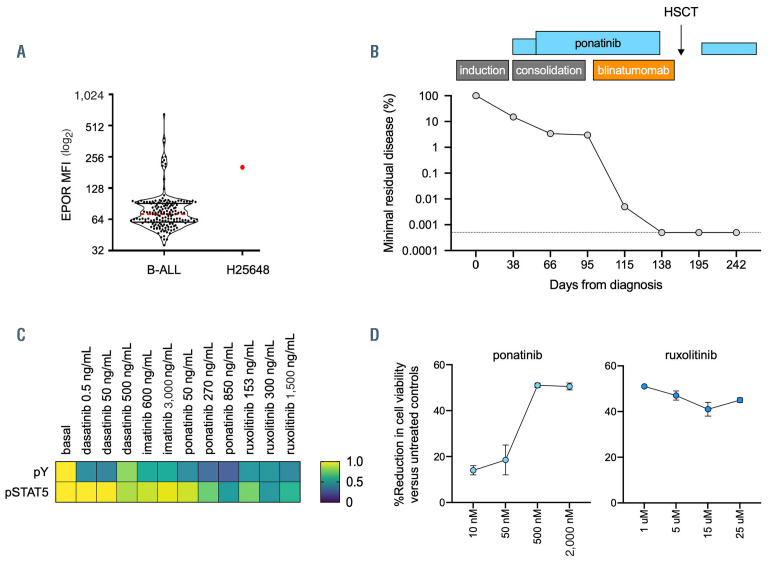
Patient #3 (H25648): A 17 year-old Caucasian female was diagnosed with NCI HR B-ALL in February 2019 with WBC 78,000 with 82% peripheral blasts. CSF was negative for leukemia (CNS1). Cytogenetics were normal with 46,XX. RNA-sequencing identified an IGH-EPOR rearrangement with confirmed high EPOR expression by reverse transcriptase-PCR and high EPOR surface protein expression by FC (Figure 1A). She had a poor prednisone response8 (9730 blasts/mm3 peripheral blood after 7 days’ therapy) and was thus classified as high-risk, received a four-drug induction on the CAALL-F01 phase III trial (clinicaltrials gov. Identifier: NCT02716233), and was refractory at end-induction with MRD 15%, as measured by immunoglobulin/T-cell receptor rearrangement PCR assay (Figure 1B). She was removed from study and received consolidation therapy with cyclophosphamide, cytarabine, 6-mercaptopurine, and ponatinib 45 mg daily for 14 days based upon in vitro phosphoflow cytometry and viability analyses of banked diagnostic ALL cells demonstrating preferential sensitivity to ponatinib and ruxolitinib (Figure 1C and D). Ponatinib was increased to 30 mg twice-daily given persistent mid-induction 1B/consolidation MRD 3.4%, which did not improve by end-1B/consolidation (TP2) with MRD 3% (Figure 1B). Chemotherapy-associated complications included vincristine- induced peripheral neuropathy, steroid-induced hyperglycemia, and mild transaminitis and coagulation parameter impairment. The patient then received one cycle of blinatumomab with continued ponatinib and achieved negative MRD (<10-5) prior to receipt of MSD allogeneic HSCT in May 2019, which was complicated by mild chronic oral and vaginal GvHD. Ponatinib 30 mg daily was begun at day +80 post-HSCT. She remains in continued MRD-negative remission and completed ponatinib maintenance therapy in May 2021 at 2 years posttransplant.
Figure 1.
Assessment of potential tyrosine kinase inhibitor activity in IGH-EPOR Philadelphia chromosome-like acute lymphoblastic leukemia. (A) Increased EPOR surface protein staining was detected in the leukemia blasts of patient H25648 with Philadelphia chromosome-like acute lymphoblastic leukemia (Ph-like ALL) and IGH-EPOR re-arrangement versus other B-acute lymphoblastic leukemia (B-ALL) cases (n=174) sequentially analysed at the Hôpital Robert Debré flow cytometry laboratory as research testing outside of the CAALL-F01 clinical trial. MFI: mean fluorescence intensity. Clinical flow cytometry analysis was performed on a FACS Canto II flow cytometer and analyzed with DIVA software (version 8.0.2; Becton-Dickinson) and demonstrated an immunophenotype profile with bright CD10/CD19/CD20, partial dim CD34, partial positive CD22, and dim CD24/CD58/CD38/CD123 staining with aberrant expression of CD21/CD25/CD27 and absence of myeloid markers CD11b/CD13/CD33/CD66c (not shown). (B) Clinical minimal residual disease levels in patient H25648 during chemotherapy (induction and consolidation; grey bars), ponatinib (blue bars; bar height bars depicts relative ponatinib dosing), and immunotherapy (blinatumomab; orange bar) and allogeneic hematopoietic stem cell transplantation (HSCT; black arrow) showed initial chemoresistance and subsequent measurable residual disease (MRD)-negative remission following blinatumomab therapy with continued ponatinib therapy that was also utilized subsequently at lower dosing as post-HSCT maintenance therapy. Dashed grey line shows undetectable MRD threshold. (C) In vitro exposure of fresh primary ALL cells from patient H25648 to various tyrosine kinase inhibitors (TKI) at the indicated concentrations for 72 hours at 37°C resulted in potent inhibition of phosphorylated pan-tyrosine and STAT5Y694 by phosphoflow cytometry (performed on a Navios flow cytometer) gated on CD45+/CD19+ blasts using Kaluza software (version 2.1; Beckman Coulter). Data are shown as percent inhibition (green-to-purple) of normalized basal phosphoprotein levels (yellow) with TKI exposure via colorimetric heatmap display. (D) In vitro viability of Ficoll-separated diagnostic primary bone marrow ALL cells from patient H25648 with ponatinib or ruxolitinib exposure was assessed via MTT (3-(4,5-di methylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) assay. Data analysis and display were performed in Prism.
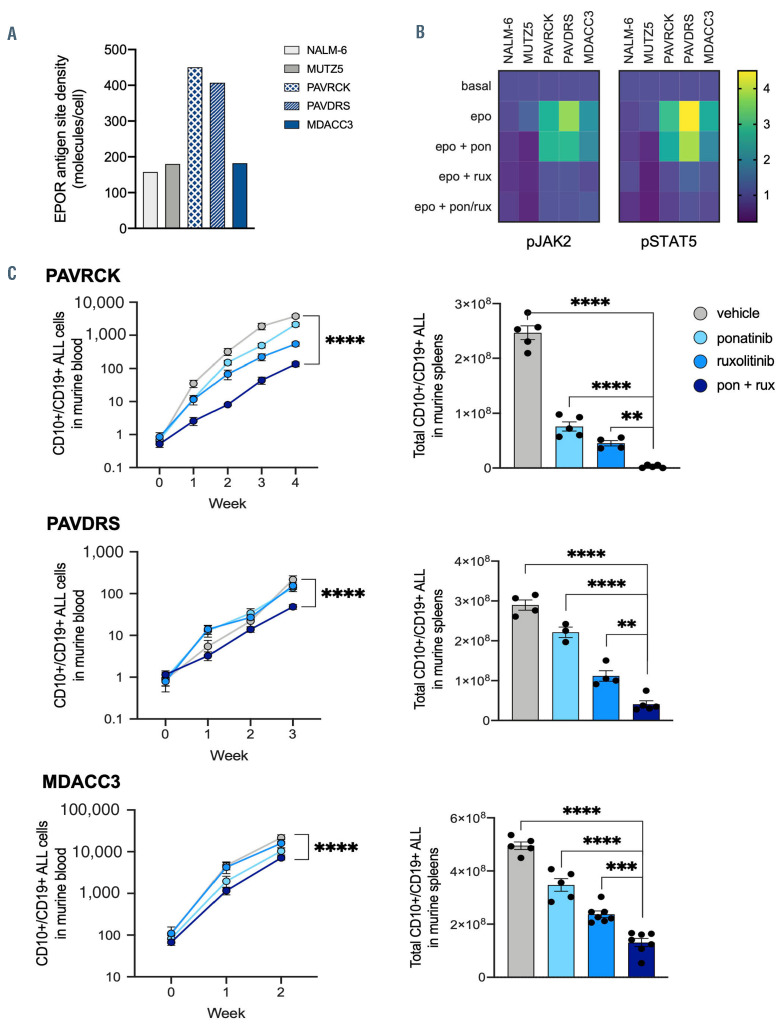
Figure 2.
Enhanced in vivo activity of combined ponatinib and ruxolitinib in patient-derived xenograft models of IGH-EPOR Philadelphia chromosome-like acute lymphoblastic leukemia. Tertiary patient-derived xenograft (PDX) models from pediatric (PAVRCK, PAVDRS) or adult (MDACC3) patients with IGH-EPOR Philadelphia chromosome-like acute lymphoblastic leukemia (Ph-like ALL) were established in NSG mice as described.5,9,11 (A) Increased surface EPOR protein expression was detected by flow cytometry (BD FACSVerse) in two of three tested IGH-EPOR Ph-like ALL PDX specimens (blue bars) versus non-Ph-like NALM-6 or Ph-like CRLF2-rearranged MUTZ5 ALL cell line controls (grey bars). IGH-EPOR fusions were confirmed in all three PDX specimens by ArcherDX FusionPlex and fluorescence in situ hybridization assays (not shown), including in the MDACC3 model without increased EPOR surface protein staining. (B) In vitro phosphoflow cytometry analysis of thawed viably-cryopreserved CD10+/CD19+/CD45+ IGH-EPOR Ph-like ALL PDX cells harvested from NSG murine spleens demonstrates ruxolitinib (rux)-induced inhibition of human erythropoietin (epo)-stimulated phosphorylated (p) JAK2Y1007/1008 and STAT5Y694 signaling. Conversely, erythropoietin co-stimulation effectively rescued potential ponatinib (pon)-induced JAK/STAT signaling inhibition. Both kinase inhibitors were used at 1 mM with simultaneous 5 units/mL erythropoietin cytokine stimulation for 60 minutes at 37°C in a 5% CO2 incubator. NALM-6 and MUTZ5 cells were used as non-Ph-like and JAK pathway- activated Ph-like ALL signaling controls, respectively. Data are normalized to basal phosphoprotein levels (level =1, purple) for each cell line or PDX model with colorimetric display of increased phosphorylation >1 (green-to-yellow) and decreased phosphorylation <1 (deep purple). (C) Engrafted IGH-EPOR Ph-like ALL PDX mice were randomized upon >1% peripheral blood engraftment to treatment with vehicle, ponatinib 25 mg/kg orally once daily for 5 days/week, ruxolitinib 2 g/kg chow orally ad libitum, or both ponatinib and ruxolitinib for 2-4 weeks depending upon rate of leukemia progression in control animals requiring sacrifice. Human CD10+/CD19+/CD45+ ALL cells were assessed weekly in murine retro-orbital venous peripheral blood (left panels) and end-study spleens by quantitative flow cytometry analysis as described.9-11 Combination ponatinib and ruxolitinib treatment induced superior inhibition of leukemia proliferation versus tyrosine kinase inhibitors (TKI) monotherapies in all three tested models. Flow cytometry analysis was performed in Cytobank. Statistical analysis and data display were performed in Prism (*P<0.05, **P<0.01, ***P<0.001, ****P<0.0001 by two-way [blood] or one-way [spleen] ANOVA with Dunnett’s post-test for multiple comparisons).
Given observed decreased MRD in these three highrisk patients treated with ruxolitinib or ponatinib and post-induction chemotherapy or immunotherapy, we conducted additional in vitro and in vivo laboratory studies to confirm and isolate the therapeutic potential of the specific TKI without multi-agent chemotherapy in IGH-EPOR Ph-like ALL PDX models (performed as described9-11). Primary B-ALL specimens used in these studies were obtained via COG or institutional biobanking research protocols via informed consent in accordance with the Declaration of Helsinki. PDX model studies were conducted via Institutional Animal Care and Use Committee-approved research protocols. We detected increased FC surface EPOR staining in two of three IGH-EPOR ALL PDX models versus non-EPORrearranged B-ALL NALM-6 (non-Ph-like) and MUTZ5 (CRLF2-rearranged Ph-like) cells (Figure 2A), as well as TKI-induced inhibition of erythropoietin-stimulated signaling in vitro via phosphoflow cytometry analyses (Figure 2B). As predicted,5,11 ponatinib or ruxolitinib monotherapy potently inhibited in vivo leukemia proliferation in two pediatric IGH-EPOR ALL PDX models (PAVRCK, PAVDRS) with superior activity observed with dual TKI treatment (Figure 2C). Interestingly, we also saw partial single-agent ponatinib and ruxolitinib activity in a third PDX model (MDACC3) established from an adult with relapsed IGH-EPOR ALL who was resistant to ruxolitinib 25 mg twice-daily and hyper-CVAD (cyclophosphamide, vincristine sulfate, doxorubicin hydrochloride, and dexamethasone) chemotherapy on an institutional phase II/III clinical trial (clinicaltrials gov. Identifier: NCT02420717).12 As in the de novo pediatric ALL PDX models, combined ponatinib and ruxolitinib more potently reduced leukemia burden in end-study murine spleens versus TKI monotherapy (Figure 2C), although this relapsed adult ALL model’s lack of LDA positivity or increased FC EPOR surface staining remains puzzling given our confirmation of IGH-EPOR fusion by both FISH and ArcherDX FusionPlex analyses. The previously- unknown sensitivity of IGH-EPOR Ph-like ALL to ponatinib in our preclinical PDX models and potentially clinically in patient H25648 is consistent with the observed sensitivity of CRLF2-rearranged Ph-like ALL to the SRC/ABLi dasatinib recently reported by our group.11 We posit that IGH-EPOR Ph-like ALL may also be driven by activated BCR-like and associated downstream SRC family kinase signaling in addition to known constitutive JAK/STAT signaling that merits further study.
Leukemia-associated IGH-EPOR fusions were first reported in 2009 by Russell and colleagues in a child with newly-diagnosed B-ALL transplanted in first remission for chemoresistance and in a young adult with very early medullary-relapsed B-ALL who underwent HSCT in second remission after salvage chemotherapy.13 Recent analyses of large cohorts of often-cytogenetically-cryptic high-risk childhood and adult B-ALL cases identified 3’ EPOR rearrangements most commonly with 5’ fusion partner immunoglobulin heavy locus (IGH) and less commonly with light chain genes immunoglobulin κ (IGK) and immunoglobulin l (IGL) or leukocyte-associated immunoglobulin-like receptor (LAIR) and associated kinase-activated Ph-like gene expression profiles.2-4 Our study confirms the clinically high-risk nature of IGH-EPOR Ph-like ALL in three AYA patients, all of whom had high end-induction MRD and two of whom required post-consolidation immunotherapy and allogeneic HSCT to overcome chemoresistance. While current clinical trials are assessing the potential efficacy of ruxolitinib addition to chemotherapy for patients with CRLF2-re-arranged and other JAK pathway-mutant Phlike ALL (including JAK2 or EPOR fusions), the potential success of this approach is not yet known,3 and ruxolitinib may also hinder desired post-HSCT graft-versus-leukemia effects.14 Ponatinib has shown early promise in adults with BCR-ABL1-rearranged (Ph+) ALL in combination with chemotherapy,15 but has not been explored specifically in Ph-like ALL. In summary, our data show that the JAKi ruxolitinib and multi-TKI ponatinib have activity against IGH-EPOR Ph-like ALL with enhanced effects of dual inhibitor treatment. Future clinical trials could explore the potential for combinatorial efficacy of ruxolitinib and ponatinib with chemotherapy in patients with IGH-EPOR fusions and other high-risk Ph-like ALL subtypes.
Acknowledgments
We gratefully acknowledge the Center for Biological Resources (‘CRB-cancer’) of the Robert Debré Hospital (BB-0033-00076; EL, AC-E, and HC), Drs I-Ming Chen and Richard Harvey at the University of New Mexico for performing Ph-like ALL low density microarray expression analysis of primary clinical and patient-derived xenograft (PDX) model ALL specimens, Ms Elizabeth Wagner at Nationwide Children’s Hospital for clinical annotation of COG ALL specimens, Dr Marilyn Li at CHOP for performing genetic characterisation of PDX models, and Dr Matthew Stubbs at Incyte Corporation for provision of ruxolitinib rodent chow for preclinical animal studies. We also kindly thank Dr Vandana Batra at the Children’s Hospital of Philadelphia, Dr Jing Chen at Hackensack University Medical Center, and Dr Michael Loschi at CHU de Nice for assisting in clinical patient care. This study is dedicated in honor of Miss Emily Herrera and Miss Ava Daisy Phillips.
Funding Statement
Funding: these studies were supported by United States National Institutes of Health (NIH)/National Institute of Child Health and Human Development award T32HD043021 (LMN), NIH/National Cancer Institute (NCI) award T32CA009615 (LMN), 1U01CA232486 (SKT), U01CA243072 (SKT), the ERA-NET TRANSCAN/Foundation ARC (EL, AC-E, HC), Department of Defense Translational Team Science award CA180683P1, the V Foundation for Cancer Research (SKT), the Sohn Monaco Foundation (PSR), and the PHRC program from the French Institut National du Cancer (PSR). Children’s Oncology Group (COG) specimen banking was supported by NCI U24CA114766 and U24CA196173. Childhood IGH-EPOR ALL PDX modeling was also supported by a Lady Tata Memorial Trust Award (II), St Jude Children’s Research Hospital Hematological Malignancies Program Garwood Fellowship (II), Leukemia and Lymphoma Society Specialized Center of Research (CGM), Stand up to Cancer Innovative Research Grant (CGM), St Baldrick’s Foundation Scholar award (CGM), NCI Outstanding Investigator Award R35CA197695 (CGM), and NIH Cancer Center Support Grant P30 CA21765 (CGM).
References
- 1.Tasian SK, Loh ML, Hunger SP. Philadelphia chromosome–like acute lymphoblastic leukemia. Blood. 2017;130(19):2064-2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roberts KG, Li Y, Payne-Turner D, et al. Targetable kinase-activating lesions in Ph-like acute lymphoblastic leukemia. N Engl J Med. 2014;371(11):1005-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harvey RC, Tasian SK. Clinical diagnostics and treatment strategies for Philadelphia chromosome-like acute lymphoblastic leukemia. Blood Adv. 2020;4(1):218-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roberts KG, Gu Z, Payne-Turner D, et al. High frequency and poor outcome of Philadelphia chromosomelLike acute lymphoblastic leukemia in adults. J Clin Oncol. 2017;35(4):394-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iacobucci I, Li Y, Roberts KG, et al. Truncating erythropoietin receptor rearrangements in acute lymphoblastic leukemia. Cancer Cell. 2016;29(2):186-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harvey RC, Kang H, Roberts KG, et al. Development and validation of a highly sensitive and specific gene expression classifier to prospectively screen and identify B-precursor acute lymphoblastic leukemia (ALL) patients with a Philadelphia chromosome-like (“Phlike” or “BCR-ABL1-Like”) signature for therapeutic targeting and clinical intervention. Blood. 2013;122(21):826-826. [Google Scholar]
- 7.Tasian SK, Assad A, Hunter DS, Du Y, Loh ML. A Phase 2 study of ruxolitinib with chemotherapy in children with Philadelphia chromosome- like acute lymphoblastic leukemia (INCB18424-269/AALL1521): dose-finding results from the Part 1 Safety Phase. Blood. 2018;132(Suppl 1):S555. [Google Scholar]
- 8.Schrappe M, Reiter A, Zimmermann M, et al. Long-term results of four consecutive trials in childhood ALL performed by the ALL-BFM study group from 1981 to 1995. Berlin-Frankfurt-Munster. Leukemia. 2000;14(12):2205-2222. [DOI] [PubMed] [Google Scholar]
- 9.Tasian SK, Teachey DT, Li Y, et al. Potent efficacy of combined PI3K/mTOR and JAK or ABL inhibition in murine xenograft models of Ph-like acute lymphoblastic leukemia. Blood. 2017;129(2):177-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tasian SK, Hurtz C, Wertheim GB, et al. High incidence of Philadelphia chromosome-like acute lymphoblastic leukemia in older adults with B-ALL. Leukemia. 2017;31(4):981-984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hurtz C, Wertheim GB, Loftus JP, et al. Oncogene-independent BCR-like signaling adaptation confers drug resistance in Ph-like ALL. J Clin Invest. 2020;130(7):3637-3653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jain N, Jabbour EJ, McKay PZ, et al. Ruxolitinib or dasatinib in combination with chemotherapy for patients with relapsed/refractory Philadelphia (Ph)-like acute lymphoblastic leukemia: a phase I-II trial. Blood. 2017;130(Suppl 1):S1322. [Google Scholar]
- 13.Russell LJ, De Castro DG, Griffiths M, et al. A novel translocation, t(14;19)(q32;p13), involving IGH@ and the cytokine receptor for erythropoietin. Leukemia. 2009;23(3):614-617. [DOI] [PubMed] [Google Scholar]
- 14.Zeiser R, von Bubnoff N, Butler J, et al. Ruxolitinib for glucocorticoid- refractory acute graft-versus-host disease. N Engl J Med. 2020;382(19):1800-1810. [DOI] [PubMed] [Google Scholar]
- 15.Jabbour E, Short NJ, Ravandi F, et al. Combination of hyper-CVAD with ponatinib as first-line therapy for patients with Philadelphia chromosome-positive acute lymphoblastic leukaemia: long-term follow-up of a single-centre, phase 2 study. Lancet Haematol. 2018;5(12):e618-e627. [DOI] [PMC free article] [PubMed] [Google Scholar]