Singapore diagnosed its first cases of coronavirus disease of 2019 (COVID-19) in travelers in January 2020, and responded with very thorough contact tracing and extensive testing without lockdowns. However, from April 7th to June 1st 2020 Singapore went into a shutdown called “circuit breaker” due to a surge in unlinked community cases. Schools and all non-essential businesses were closed, with only limited healthcare and food stores open. The most draconian measures were lifted gradually in June, and currently restaurants, entertainment venues and most businesses are still restricted to reduced capacity. Safe distancing and mandatory universal masking in public continue to be strictly enforced since early April 2020.
The National University Hospital is a tertiary-care, academic medical center in Singapore with 1200 inpatient beds. The Epidemiology unit tracks incidence of key pathogens of importance including respiratory viruses, so we can identify clusters of infections either in the hospital or community.
Respiratory viral laboratory testing is ordered at the discretion of the attending physician for patients in whom there is clinical suspicion, using one of the following: (1) D3 Ultra™ DFA Respiratory Virus Screening and Identification Kit (Diagnostic Hybrids, Inc., USA), (2) cobas® Influenza A/B & RSV Nucleic acid test (Roche Diagnostics, GmbH, Germany), (3) up till April 2020: Luminex NxTAG Respiratory Pathogen Panel (Luminex Corporation, USA), and from April 2020 onwards: BioFire FilmArray Respiratory Panel 2 (Biofire Diagnostics, France). As of March 2021, the BioFire FilmArray Respiratory Panel 2.1 has included SARS-CoV-2 virus.
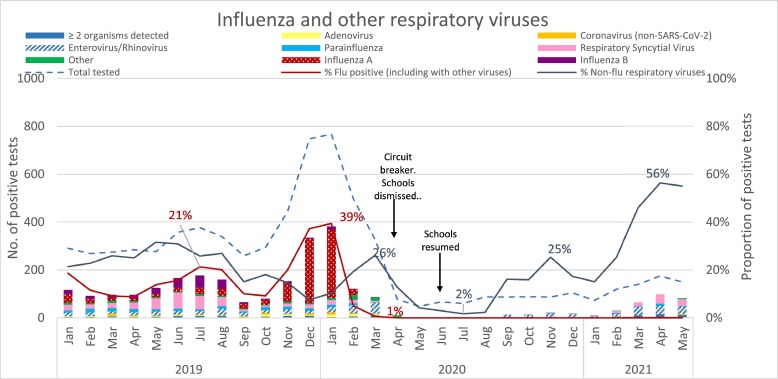
We reviewed the results of these respiratory tests at NUH between January 2019 and May 2021 to determine the impact of COVID-19 on the incidence of influenza and other respiratory viruses. Since the number of tests varied with reagent supply, hospital and community policies and other factors, we focused on test positivity. The usual bimodal peaks of influenza, in pre-COVID-19 July and August (20% – 21% positivity of all samples tested), and December 2019 – January 2020 (37% – 39% positivity of all samples tested) were present (Fig. 1 ). However, influenza disappeared completely in March 2020 just before the introduction of tight non-pharmaceutical interventions, masking, social distancing, and other restrictions nationally. This is similar to what has been seen in other places, and may be due to the population already practicing personal behavior changes in line with public health messaging, or may be due to the abrupt stop in global travel [1], [2], [3], [4].
Fig. 1.
Influenza and other respiratory viruses
50% of those tested in the post-COVID-19 period (June 2020 – May 2021), were aged 16 and below, with 32% 2 years of age or younger. Surprisingly, after a steep decline in all respiratory viral test positivity rates from April through June 2020 during Singapore's “circuit breaker”, a resurgence in other, non-influenza, respiratory viruses occurred (Fig. 1). Our data in April 2021 shows a return to pre-COVID-19 highs of 56% positivity of all samples tested in April 2021, after schools re-opened in July and August 2020, although the absolute number of tests ordered is lower than 2019 (Table 1 in Supplementary). This pattern was seen for rhinoviruses, parainfluenza viruses, respiratory syncytial viruses and other viruses as well but strikingly not for influenza. In fact, there have been no cases of influenza diagnosed at NUH or detected by national surveillance up until May 2021 [5]. In Singapore, individuals with upper respiratory tract symptoms, are encouraged to seek medical attention at designated clinics for proper testing, and given a mandated 3 – 5 day Medical Certificate to stay home even if the test is negative [6]. Under the Singapore Infectious Disease Act, all persons who test positive for SARS-CoV-2, must be admitted to hospital or a community isolation facility. With the Infectious Disease Act being strictly enforced to penalize non-compliance, there might be individuals who avoid seeking medical attention, bringing down the numbers of respiratory infections being diagnosed. The actual number of cases of upper respiratory tract infection seen in government polyclinics is higher than during circuit breaker but remains at about half the level it was before the pandemic [7,8].
The continued disappearance of influenza while other respiratory viruses returned post COVID-19 is striking, particularly since non–pharmaceutical interventions have continued. The reasons for this difference need to be explored. In Hong Kong, school outbreaks of rhinoviruses and enteroviruses without significant influenza activity were reportedly related to school reopening [9]. Other possibilities include the near complete shutdown in global travel which may have broken the chain of transmission of influenza from the Northern Hemisphere through the tropics to the Southern Hemisphere and back which is believed to sustain global seasonal influenza [10]. Alternatively, there may be some degree of viral cross protection between SARS-CoV-2 and influenza as has been suggested for adenoviruses and influenza [11], or due to some interaction at the receptor level between influenza virus and SARS-CoV-2 which has been observed in animal models [12]. There are differences in modes of transmission and current measures may be more effective for larger respiratory viruses such as influenza and coronaviruses, than for small viruses such as rhinovirus [13].
This phenomenon may be a global one and needs to be better understood through careful epidemiological and animal model studies. There is an urgent need to better understand the virology and the non-adaptive and adaptive immune responses to these important respiratory viruses with pandemic potential before the next pandemic strikes.
Declaration of Competing Interest
All authors report no direct conflict of interest. Paul Ananth Tambyah has received research support from Roche, Shionogi, Johnson and Johnson and Arcturus paid to the institution.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jcv.2021.104992.
Appendix. Supplementary materials
References
- 1.Soo R.J.J., Chiew C., Ma S., Pung R., Lee V. Decreased influenza incidence under COVID-19 control measures, Singapore. Emerg. Infect. Dis. 2020;26(8):1933–1935. doi: 10.3201/eid2608.201229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chow A., Hein A.A., Kyaw W.M. Unintended consequence: influenza plunges with public health response to COVID-19 in Singapore. J. Infect. 2020;81:e68–e69. doi: 10.1016/j.jinf.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tan J.Y., Conceicao E.P., Sim X.Y.J., Wee L.E.I., Aung M.K., Venkatachalam I. Public health measures during COVID-19 pandemic reduced hospital admissions for community respiratory viral infections. J. Hosp. Infect. 2020;106:387–389. doi: 10.1016/j.jhin.2020.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poole S., Brendish N.J., Tanner A.R., Clark T.W. Physical distancing in schools for SARS-CoV-2 and the resurgence of rhinovirus. Lancet Respir. Med. 2020;8:e92–e93. doi: 10.1016/S2213-2600(20)30502-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singapore. Ministry of Health Weekly infectious diseases bulletin [Internet] Singapore: Ministry Health. 2021 https://www.moh.gov.sg/resources-statistics/infectious-disease-statistics/2021/weekly-infectious-diseases-bulletin [cited 2021 Mar 14] Available from. [Google Scholar]
- 6.Tang L. Jail for woman who broke Covid-19 law by going to funeral while on MC for acute respiratory infection. Today Online. 2021 https://www.todayonline.com/singapore/jail-woman-who-broke-covid-19-law-going-funeral-while-mc-acute-respiratory-infection [Google Scholar]
- 7.Singapore. Ministry of Health Weekly infectious diseases bulletin [Internet] Singapore: Ministry Health. 2021 https://www-moh-gov-sg-admin.cwp.sg/docs/librariesprovider5/diseases-updates/2019_week_5216305221bf6e4296b8bfc51c33fc143f.pdf [cited 2021 Jun 24] Available from. [Google Scholar]
- 8.Singapore. Ministry of Health Weekly infectious diseases bulletin [Internet] Singapore: Ministry Health. 2021 https://www-moh-gov-sg-admin.cwp.sg/docs/librariesprovider5/diseases-updates/2021_week_23.pdf [cited 2021 Jun 24] Available from. [Google Scholar]
- 9.Fong M.W., Leung N.H.L., Cowling B.J., Wu P. Upper respiratory infections in schools and childcare centers reopening after COVID-19 dismissals, Hong Kong. Emerg. Infect. Dis. 2021;27:5. doi: 10.3201/eid2705.210277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nelson M.I., Simonsen L., Viboud C., Miller M.A., Holmes E.C. Phylogenetic analysis reveals the global migration of seasonal influenza A viruses. PLoS Pathog. 2007;3(9):e131. doi: 10.1371/journal.ppat.0030131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen I.M., Loh J.P., Chuah C.X.P., et al. Evidence for cross-protection against subsequent febrile respiratory illness episodes from prior infections by different viruses among Singapore military recruits 2009–2014. J. Infect. Dis. 2019;219:1913–1923. doi: 10.1093/infdis/jiz046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bai L., Zhao Y., Dong J., et al. Coinfection with influenza A virus enhances SARS-CoV-2 infectivity. Cell Res. 2021;0:1–9. doi: 10.1038/s41422-021-00473-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leung N.H.L., Chu D.K.W., Shiu E.Y.C., et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.