Abstract
Background
As populations age, the possible consequences of increased frailty are a major concern for the health sector. Here, we investigate how life expectancy with and without frailty has changed during a 10–11-year-period across Europe.
Methods
The Sullivan method was used to investigate changes in life expectancy with and without frailty in 10 European countries. Frailty status (non-frail, pre-frail and frail) was determined by use of the Survey of Health, Ageing and Retirement in Europe Frailty Instrument (SHARE-FI). Data on frailty prevalence was obtained from 21 698 individuals in wave 1 (2004–05) and 38 859 individuals in wave 6 (2015) of the SHARE. Information on mortality was obtained from the Eurostat Database.
Results
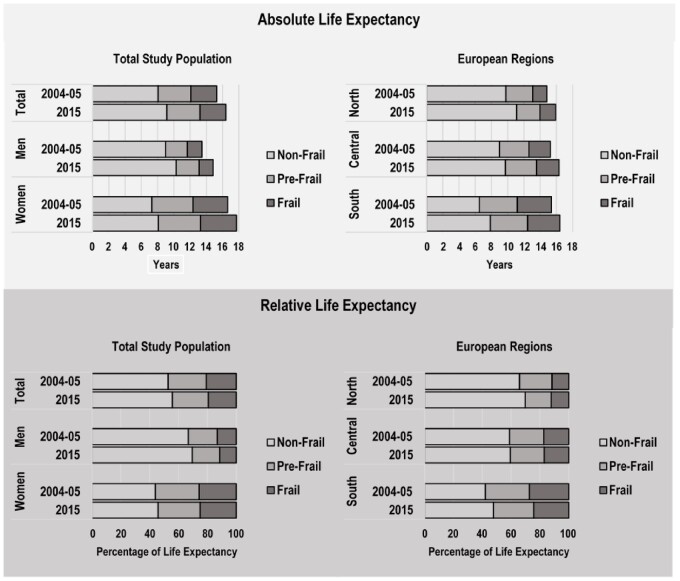
In 2015, women aged 70 spent 25.0% (95% CI: 24.0–26.1) of their remaining life expectancy in a frail state, and the number for men was 11.5% (95% CI: 10.7–12.3). Southern Europeans spent 24.2% (95% CI: 22.9–25.4) of their remaining life expectancy in a frail state and the numbers for Central Europeans and Northern Europeans were 17.0% (95% CI: 16.0–17.9) and 12.2% (95% CI: 10.9–13.5), respectively. From 2004–05 to 2015, life expectancy increased by 1.1 years (from 15.3 to 16.4 years) for 70-year-old Europeans. Similarly, non-frail life expectancy increased by 1.1 years (95% CI: 0.8–1.4), whereas no significant changes in life expectancy in frail states were observed.
Conclusions
This study suggests that Europeans today spend more years in a non-frail state than Europeans did 10–11 years ago. Our findings reflect a considerable inequality by gender and region.
Introduction
In high-income countries, mortality at older ages has fallen dramatically and record life expectancy (LE) has risen for more than a centuryby three months per year in low-mortality countries.1,2 The reason for the rise in LE has, since the 1950s, mostly been caused by declining mortality rates at older ages.1 The social and economic implications associated with ageing have been discussed extensively. A key concern is whether the years gained in LE are healthy years or years spent in a disabled and unhealthy state.3,4
In the late 1970s and early 1980s, three alternative scenarios of future health trends in ageing populations were proposed.5–7 Gruenberg argued that as mortality rates are declining, partly as a product of better health care, individuals who previously would have died are kept alive but in a less than healthy state.5 According to Gruenberg, the proportion of unhealthy elderly people will increase as LE increases. This projection is often referred to as the failure-of-success theory or the expansion of morbidity theory.4,5,8. Fries proposed a contrasting projection, namely that improved health care will postpone the onset of morbidity and disability to a higher age, so that time spent in an unhealthy state will be compressed into a shorter period before death—a theory known as the success-of-success theory or the compression of morbidity theory.4,6,8 An intermediate theory, the dynamic equilibrium theory, proposed by Manton, suggests that the proportion of unhealthy elderly people will increase, but that there will be a shift towards less severe morbidities and disabilities.7
As data on measures of health in the ageing population has become increasingly available, these theories have been tested widely with a considerable amount of research suggesting that people are living longer and healthier lives.4 However, current evidence shows that many older community-dwelling people have risk factors for major health-related events, and this has caused the frailty-syndrome to be recognized as a condition to be given high priority in public health prevention and research.9
Frailty has been defined as a state of increased physiological vulnerability and is associated with an increased risk for negative health outcomes (e.g. falls, hospitalization, long-term care, institutionalization and mortality).9–11 Frailty may represent a transition phase between successful ageing and disability, and with the gradually increasing number of elderly, there is growing global awareness on preventing and delaying the onset of frailty.9,12
While numerous definitions of frailty have been proposed, the one that has gained most recognition is the definition given by Fried et al.13 Fried’s method requires the measurement of five frailty criteria: weakness, slowness, low level of physical activity, low energy or self-reported exhaustion and unintentional weight loss.13
Romero-Ortuno et al. were the first to investigate LE with and without frailty across Europe, in 15 countries participating in the Survey of Health, Ageing and Retirement in Europe (SHARE) in wave 4 in 2011.14 Among 50 351 Europeans aged 50+, they found that LE in a frail state at age 70 was 0.7 years for men and 1.8 years for women; however, the estimates varied by country, with a higher proportion of pre-frailty and frailty in Southern Europe than in Northern Europe.14 A similar study in a French population of 2350 individuals aged 70+ by Herr et al., found that LE at age 70 in a frail state was 1.2 years for men and 3.4 years for women, confirming the known gender differences in health expectancy.15
To our knowledge, no studies have evaluated the development in LE with frailty over time in the European population. In this study, we estimate LE in different frailty states for the European population in 2004–05 and 2015, respectively, to assess the change over time and evaluate whether LE with and without frailty has increased, decreased or stagnated in the European population. Moreover, we explore gender and regional differences in frailty during the observation period.
Methods
Study population
This study was based on data from SHARE, a cross-national panel survey, collecting data on health, socioeconomic status and social networks of people aged 50+ and their spouses/partners, living in Europe. The data were collected by trained interviewers in the participants’ homes using computer-assisted personal interviews. To increase sample size and compensate for attrition, SHARE continuously adds refresher samples in each wave.16
The present study included respondents aged 50+ from wave 1 (2004–05)17 and wave 6 (2015).18 A total of 10 European countries were part of both waves. These countries were classified into three regions: Northern Europe (Denmark and Sweden), Central Europe (Austria, Germany, France, Switzerland and Belgium) and Southern Europe (Italy, Spain and Greece). Response rates for baseline/refreshment interviews at the household level varied from 40.3% in Belgium to 97.6% in France in wave 1 and from 45.0% in Italy to 69.3% in Greece in wave 6.19
Frailty classification
To classify the study population according to frailty status, the SHARE Frailty Instrument (SHARE-FI)20–22 was applied. The SHARE-FI is based on five items in the SHARE questionnaire (exhaustion, weight loss, weakness, slowness, and low physical activity) which have been identified to be the best approximation to Fried’s frailty criteria.23
Exhaustion was identified as a ‘yes’ to the question: ‘In the last month, have you had too little energy to do the things you wanted to do’?
Weight loss was defined as a ‘Diminution in desire for food’ in response to: ‘What has your appetite been like?’ or, if the response was non-specific or not codable, by responding ‘less’ to: ‘So, have you been eating more or less than usual?’
Weakness was assessed by handgrip strength in kilograms using a dynamometer. Two measurements were taken from both hands, with the highest value being selected.
Slowness was identified by answering ‘yes’ to one or both of the following questions: ‘Because of a health problem, do you have difficulty (expected to last more than 3 months) walking 100 meters?’ or ‘… climbing one flight of stairs without resting?’.
Low physical activity was assessed by the question: ‘How often do you engage in activities that require a low or moderate level of energy such as gardening, cleaning the car, or doing a walk?’ The answer was measured on an ordinal scale: more than once a week; once a week; one to three times a month; or hardly ever or never.
Based on the answers to these questions, the SHARE-FI formula calculates a frailty score from which individuals can be classified according to three categories: non-frail, pre-frail and frail.20 Detailed information on the SHARE-FI formula can be found in the original paper by Romero-Ortuno et al.20
Statistical analysis
LE in different frailty states and 95% confidence intervals (CIs) were measured by application of the Sullivan method with direction from the practical guide by Jagger et al.24 The required data for calculating healthy life expectancy (HLE) by the Sullivan method is the age-specific prevalence of the population in healthy and unhealthy states (i.e. the prevalence of non-frail, pre-frail and frail individuals in the two SHARE waves) as well as age-specific mortality information provided from a period life table.24 Mortality data from the respective 10 SHARE countries in 2004 and 2015 were obtained from period life tables at Eurostat.25
The age-specific prevalence’s of frailty was assessed in five-year age groups for the total study population and investigated separately by gender and regions and weighted using the calibrated individual probability weights provided in the SHARE dataset, designed to reduce the impact of non-response and attrition.16
LE in the different frailty states was estimated using STATA and Microsoft Excel.
In order to evaluate which of the proposed theories fitted the development in time spent with and without frailty in the European population, the classification proposed by Nusselder26,27 was applied (table 1). The classification distinguishes between absolute and relative compression and expansion of morbidity, based on changes observed in healthy and unhealthy LE over time. We defined ‘healthy LE’ as non-frail LE and ‘unhealthy LE’ as pre-frail and frail LE. For instance, if healthy LE (i.e. years spent in a non-frail state) increases during the observation period, while at the same time unhealthy LE (i.e. years spent in a pre-frail and frail state) decreases, there will be evidence of absolute compression of unhealthy LE. Contrarily, if unhealthy LE increases over time, there will be evidence of absolute expansion of unhealthy LE. In case of no changes observed in unhealthy LE, there will be evidence of an equilibrium between absolute expansion and compression. Relative compression of unhealthy LE is observed if the proportion of healthy LE increases during the observation period, while there will be a relative expansion if the proportion of healthy LE decreases (table 1). There is evidence for the dynamic equilibrium theory if an absolute and relative expansion of unhealthy LE is observed together with a shift from more to less severe unhealthy life years (i.e. a shift towards increasing pre-frail LE and decreasing frail LE).7,27
Table 1.
Classification of absolute and relative compression and expansion of morbidity (as proposed by Nusselder26)
| Life expectancy (LE) | Healthy LE | Unhealthy LE |
% Healthy LE
in LE |
Classification |
|
|---|---|---|---|---|---|
| Absolute | Relative | ||||
| ↑ | ↑ | ↓ | ↑ | Compression | Compression |
| ↑ | ↑ | = | ↑ | Equilibrium compression-expansion | Compression |
| ↑ | ↑ | ↑ | ↑ | Expansion | Compression |
| ↑ | ↑ | ↑ | = | Expansion | Equilibrium compression-expansion |
| ↑ | ↑ | ↑ | ↓ | Expansion | Expansion |
| ↑ | = | ↑ | ↓ | Expansion | Expansion |
| ↑ | ↓ | ↑ | ↓ | Expansion | Expansion |
Results
The study population comprised 21 698 individuals in wave 1 and 38 859 in wave 6. The average age was 64.3 (SD 9.8) years in 2004–05 and 67.0 (SD: 9.8) years in 2015. There was a slightly higher proportion of participating women than men (53.6% in 2004–05 and 54.1% in 2015). The proportion of frail individuals increased from 7.1% to 7.9% for 50+ yearolds and decreased from 15.6% to 15.0% for 70+ yearolds from 2004–05 to 2015. The highest proportion of frail individuals was observed in the Southern European population (table 2).
Table 2.
Demographic characteristics of the study population (50+yearold), SHARE waves 1 (2004–05) and 6 (2015)
| Total study population |
Northern Europe |
Central Europe |
Southern Europe |
|||||
|---|---|---|---|---|---|---|---|---|
| 2004–05 (n = 21 698) |
2015 (n = 38 859) |
2004–05 (n = 4282) |
2015 (n = 7145) |
2004–05 (n = 10 835) |
2015 (n = 18 391) |
2004–05 (n = 6581) |
2015 (n = 13 323) |
|
| Gender (n (%)) | ||||||||
| Men | 10 074 (46.4) | 17 815 (45.9) | 2031 (47.4) | 3336 (46.7) | 5042 (46.5) | 8332 (45.3) | 3001 (45.6) | 6147 (46.1) |
| Women | 11 624 (53.6) | 21 044 (54.1) | 2251 (52.6) | 3809 (53.3) | 5793 (53.5) | 10 059 (54.7) | 3580 (54.4) | 7176 (53.9) |
| Age interval (n (%)) | ||||||||
| 50–54 | 4057 (18.7) | 3896 (10.0) | 775 (18.1) | 677 (9.5) | 2093 (19.3) | 1920 (10.4) | 1189 (18.1) | 1299 (9.8) |
| 55–59 | 4102 (18.9) | 6090 (15.7) | 870 (20.3) | 976 (13.7) | 2014 (18.6) | 3035 (16.5) | 1218 (18.5) | 2079 (15.6) |
| 60–64 | 3716 (17.1) | 7046 (18.1) | 750 (17.5) | 1224 (17.1) | 1818 (16.8) | 3360 (18.3) | 1148 (17.4) | 2462 (18.5) |
| 65–69 | 3345 (15.4) | 7029 (18.1) | 609 (14.2) | 1434 (20.1) | 1705 (15.7) | 3224 (17.5) | 1031 (15.7) | 2371 (17.8) |
| 70–74 | 2726 (12.6) | 5585 (14.4) | 494 (11.5) | 1148 (16.1) | 1329 (12.3) | 2535 (13.8) | 903 (13.7) | 1902 (14.3) |
| 75–79 | 2000 (9.2) | 4430 (11.4) | 411 (9.6) | 809 (11.3) | 1014 (9.4) | 2051 (11.2) | 575 (8.7) | 1570 (11.8) |
| 80–84 | 1183 (5.5) | 2846 (7.3) | 221 (5.2) | 500 (7.0) | 619 (5.7) | 1294 (7.0) | 343 (5.2) | 1052 (7.9) |
| 85+ | 569 (2.6) | 1937 (5.0) | 152 (3.6) | 377 (5.3) | 243 (2.2) | 972 (5.3) | 174 (2.6) | 588 (4.4) |
| Age in years (mean (SD)) | ||||||||
| 64.3 (9.8) | 67.0 (9.8) | 64.4 (10.0) | 67.5 (9.7) | 64.2 (9.7) | 66.8 (9.9) | 64.4 (9.7) | 67.0 (9.7) | |
| Frailty status (n (%)) | ||||||||
| 50+-year-old | ||||||||
| Non-Frail | 16 875 (77.8) | 29 521 (76.0) | 3617 (84.5) | 6049 (84.7) | 8689 (80.2) | 14 352 (78.0) | 4625 (69.3) | 9120 (68.5) |
| Pre-Frail | 3291 (15.2) | 6251 (16.1) | 482 (11.3) | 759 (10.6) | 1469 (13.6) | 2731 (14.9) | 1363 (20.4) | 2761 (20.7) |
| Frail | 1532 (7.1) | 3087 (7.9) | 183 (4.3) | 337 (4.7) | 677 (6.3) | 1308 (7.1) | 684 (10.3) | 1442 (10.8) |
| 70+-year-old | ||||||||
| Non-Frail | 3905 (60.3) | 9247 (62.5) | 897 (70.2) | 2129 (75.1) | 2039 (63.6) | 4417 (64.5) | 969 (48.6) | 2701 (52.8) |
| Pre-Frail | 1564 (24.1) | 3329 (22.5) | 256 (20.0) | 441 (15.6) | 710 (22.2) | 1487 (21.7) | 598 (30.0) | 1401 (27.4) |
| Frail | 1009 (15.6) | 2222 (15.0) | 125 (9.8) | 264 (9.3) | 456 (14.2) | 948 (13.8) | 428 (21.4) | 1010 (19.8) |
In the following, results for the age group of individuals aged ‘70–74’ are reported. LE for all age groups in each frailty state and across gender and regional area can be found in the supplementary file, table A1–12.
In 2004–05 as well as in 2015, we observed disparity in healthy (non-frail) and unhealthy (pre-frail and frail) LE between men and women and across regions. Women had a higher LE compared with men but spent a considerably higher proportion of their remaining LE in an unhealthy state. In 2015, a 70-year-old woman could expect to live a further 17.7 years, of which 29.2% (95% CI: 28.1–30.3) would be in a pre-frail state and 25.0% (95% CI: 24.0–26.1) would be in a frail state. In comparison, a 70-year-old man could expect to further live 14.8 years, of which 19% (95% CI: 18.0–20.0) would be in a pre-frail state and 11.5% (95% CI: 10.7–12.3) would be in a frail state (table 3, figure 1). Across regions, Northern Europeans had the lowest LE (15.9 years in 2015) and the lowest proportion of unhealthy LE [pre-frail LE: 18.0% (95% CI: 16.4–19.5) and frail LE: 12.2% (95% CI: 10.9–13.5)] while Southern Europeans had the highest LE (16.4 years in 2015) and the highest proportion of unhealthy LE [pre-frail LE: 28.0% (95% CI: 26.7–29.4) and frail LE: 24.2% (95% CI: 22.9–25.4)] (table 3, figure 1).
Table 3.
Life expectancy by frailty state at age 70 across European regions and gender in SHARE Waves 1 (2004–05) and 6 (2015)
| Population | Calendar year | Total life expectancy |
Absolute life expectancy
Years (95% CI) |
Relative life expectancy
% (95% CI) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Healthy |
Unhealthy |
Healthy |
Unhealthy |
||||||||||
| Years | (Changea) | Non-frail | (Changeb) | Pre-frail | Frail | (Changec) | Non-frail | (Changeb) | Pre-frail | Frail | (Changec) | ||
| Total | |||||||||||||
| Total Study Population | 2004–05 | 15.3 | 8.1 (7.9–8.3) | 4.0 (3.8–4.2) | 3.2 (3.0–3.4) | 52.8 (51.5–54.1) | 26.4 (25.3–27.6) | 20.9 (19.7–22.0) | |||||
| 2015 | 16.4 | (1.1) ↑ | 9.2 (9.0–9.3) | (1.1) ↑ | 4.1 (4.0–4.2) | 3.2 (3.1–3.3) | (0.1) ↑ | 55.7 (54.9–56.5) | (2.9) ↑ | 24.9 (24.1–25.6) | 19.4 (18.7–20.1) | (–3.0) ↓ | |
| Northern Europe | 2004–05 | 14.8 | 9.8 (9.4–10.2) | 3.3 (3.0–3.7) | 1.7 (1.4–2.0) | 66.0 (63.3–68.6) | 22.5 (20.0–24.9) | 11.6 (9.6–13.5) | |||||
| 2015 | 15.9 | (1.1)↑ | 11.1 (10.8–11.4) | (1.3) ↑ | 2.9 (2.6–3.1) | 1.9 (1.7–2.2) | (–0.2) ↓ | 69.8 (68.1–71.6) | (3.8) ↑ | 18.0 (16.4–19.5) | 12.2 (10.9–13.5) | (–3.9) ↓ | |
| Central Europe | 2004–05 | 15.2 | 9.0 (8.7–9.3) | 3.6 (3.3–3.9) | 2.6 (2.4–2.9) | 59.0 (57.1–60.9) | 23.7 (21.9–25.4) | 17.4 (15.8–18.9) | |||||
| 2015 | 16.3 | (1.1) ↑ | 9.7 (9.5–9.9) | (0.7) ↑ | 3.8 (3.7–4.0) | 2.8 (2.6–2.9) | (0.4) ↑ | 59.5 (58.4–60.7) | (0.5) ↑ | 23.5 (22.4–24.6) | 17.0 (16.0–17.9) | (–0,6) ↓ | |
| Southern Europe | 2004–05 | 15.4 | 6.5 (6.1–6.8) | 4.7 (4.3–5.0) | 4.2 (3.9–4.5) | 42.2 (40.0–44.4) | 30.5 (28.3–32.8) | 27.2 (25.0–29.5) | |||||
| 2015 | 16.4 | (1.0) ↑ | 7.8 (7.6–8.0) | (1.3) ↑ | 4.6 (4.4–4.8) | 4.0 (3.8–4.2) | (–0.3) ↓ | 47.8 (46.4–49.2) | (5.6) ↑ | 28.0 (26.7–29.4) | 24.2 (22.9–25.4) | (–5.5) ↓ | |
| Women | |||||||||||||
| Total Study Population | 2004–05 | 16.6 | 7.3 (7.0–7.6) | 5.1 (4.8–5.3) | 4.3 (4.0–4.6) | 43.9 (42.2–45.6) | 30.4 (28.7–32.1) | 25.7 (24.1–27.4) | |||||
| 2015 | 17.7 | (1.1) ↑ | 8.1 (7.9–8.3) | (0.8) ↑ | 5.2 (5.0–5.4) | 4.4 (4.2–4.6) | (0.2) ↑ | 45.8 (44.7–46.9) | (1.9) ↑ | 29.2 (28.1–30.3) | 25.0 (24.0–26.1) | (–1.9) ↓ | |
| Northern Europe | 2004–05 | 16.1 | 9.2 (8.7–9.8) | 4.6 (4.0–5.2) | 2.2 (1.8–2.7) | 57.5 (53.8–61.1) | 28.5 (24.9–32.1) | 14.0 (11.1–16.8) | |||||
| 2015 | 17.0 | (0.9) ↑ | 10.6 (10.1–11.0) | (1.4) ↑ | 4.0 (3.6–4.4) | 2.5 (2.1–2.8) | (–0.3) ↓ | 62.2 (59.7–64.7) | (4.7) ↑ | 23.3 (21.0–25.7) | 14.5 (12.5–16.5) | (–4.7) ↓ | |
| Central Europe | 2004–05 | 16.5 | 8.5 (8.1–8.9) | 4.5 (4.1–4.9) | 3.5 (3.2–3.9) | 51.5 (49.0–54.0) | 27.2 (24.9–29.6) | 21.3 (19.0–23.5) | |||||
| 2015 | 17.6 | (1.1) ↑ | 9.1 (8.8–9.3) | (0.6) ↑ | 4.7 (4.5–5.0) | 3.8 (3.6–4.1) | (0.5)↑ | 51.5 (49.9–53.1) | (0.0) = | 26.9 (25.4–28.4) | 21.6 (20.2–23.0) | (0.0) = | |
| Southern Europe | 2004–05 | 16.8 | 5.2 (4.7–5.7) | 5.9 (5.4–6.4) | 5.8 (5.2–6.3) | 30.8 (28.1–33.6) | 35.0 (31.8–38.2) | 34.2 (31.0–37.4) | |||||
| 2015 | 18.0 | (1.2) ↑ | 6.1 (5.8–6.4) | (0.9) ↑ | 6.1 (5.7––6.5) | 5.8 (5.4–6.1) | (0.2) ↑ | 33.9 (32.1–35.6) | (3.1) ↑ | 33.9 (31.9–36.0) | 32.2 (30.2–34.2) | (–3.1) ↓ | |
| Men | |||||||||||||
| Total Study Population | 2004–05 | 13.5 | 9.0 (8.7–9.2) | 2.7 (2.5–2.9) | 1.8 (1.6–2.0) | 66.8 (64.9–68.6) | 20.1 (18.5–21.7) | 13.2 (11.8–14.6) | |||||
| 2015 | 14.8 | (1.3)↑ | 10.3 (10.1–10.5) | (1.3) ↑ | 2.8 (2.7–3.0) | 1.7 (1.6–1.8) | (0.0) = | 69.5 (68.4–70.6) | (2.7) ↑ | 19.0 (18.0–20.0) | 11.5 (10.7–12.3) | (––2.8) ↓ | |
| Northern Europe | 2004–05 | 13.3 | 10.4 (9.9–10.8) | 1.8 (1.4–2.2) | 1.1 (0.8––1.4) | 78.2 (74.8–81.7) | 13.7 (10.8–16.6) | 8.1 (5.7–10.4) | |||||
| 2015 | 14.6 | (1.3)↑ | 11.7 (11.4–12.0) | (1.3) ↑ | 1.6 (1.4–1.9) | 1.3 (1.1–1.6) | (0.0) = | 79.9 (77.7–82.2) | (1.7)↑ | 11.1 (9.3–12.8) | 9.0 (7.4–10.6) | (–1.7) ↓ | |
| Central Europe | 2004–05 | 13.4 | 9.7 (9.3–10.0) | 2.4 (2.1–2.7) | 1.4 (1.2–1.7) | 71.9 (69.2–74.5) | 17.6 (15.3–19.9) | 10.5 (8.6-12.3) | |||||
| 2015 | 14.7 | (1.3) ↑ | 10.5 (10.3–10.7) | (0.8)↑ | 2.8 (2.6–3.0) | 1.5 (1.3–1.6) | (0.5)↑ | 71.2 (69.6–72.8) | (–0.7) ↓ | 18.8 (17.4–20.2) | 10.0 (8.9–11.1) | (0.7) ↑ | |
| Southern Europe | 2004–05 | 13.5 | 8.0 (7.5–8.4) | 3.3 (2.8–3.7) | 2.3 (1.9–2.7) | 58.8 (55.5–62.1) | 24.1 (21.0–27.2) | 17.1 (14.3-19.9) | |||||
| 2015 | 15.0 | (1.5) ↑ | 9.8 (9.5–10.1) | (1.8) ↑ | 3.1 (2.8–3.3) | 2.1 (1.9–2.3) | (–0.4) ↓ | 65.3 (63.4–67.2) | (6.5)↑ | 20.6 (18.9–22.2) | 14.1 (12.6–15.6) | (–6.5) ↓ | |
Note: Sum of life expectancy in different frailty states (absolute and relative) does not always add to total life expectancy due to rounding.
Change in life expectancy from 2004–05–2015.
Change in healthy (non–frail) life expectancy from 2004–05–2015.
Change in unhealthy (pre-frail + frail) life expectancy from 2004–05–2015.
Figure 1.
Remaining life expectancy at age 70 by frailty state in the Total Study Population and across European regions in 2004–05 and 2015 in absolute (years) and relative (proportion) measures.
During the observation period from 2004–05 to 2015, we observed an increase in remaining LE for a 70-year-old individual in the total study population of 1.1 years, from 15.3 years in 2004–05 to 16.4 years in 2015. Northern women had the smallest increase of 0.9 years from 16.1 years in 2004–05 to 17.0 years in 2015, while Southern men had the highest increase of 1.5 year from 13.5 years in 2004–05 to 15.0 years in 2015 (table 3).
In the total study population, healthy LE increased by 1.1 years from 8.1 years (95% CI: 7.9–8.3) in 2004–05 to 9.2 years (95% CI: 9.0–9.3) in 2015, while unhealthy LE increased by 0.1 years, as a result of a non-significant increase in years spent in a pre-frail state [4.0 years (95% CI: 3.8–4.2) in 2004–05 to 4.1 years (95% CI: 4.0–4.2 in 2015)] (table 3). In relative measures, the proportion of healthy LE increased by 2.9 percentage points from 52.8% (95% CI: 51.5–54.1) in 2004–05 to 55.7% (95% CI: 54.9–56.5) in 2015, resulting in a relative compression of unhealthy LE during the period (tables 1and 3).
Healthy LE increased from 2004–05 to 2015 for both men and women in each regional area. However, overlap in 95% CIs of healthy LE for the period 2004–05 and 2015 was observed for Central European women (table 3). Varying trends in changes in unhealthy LE were observed across gender and region. Generally, the changes were minor compared with the changes observed in healthy LE, and in all cases, the 95% CI overlapped (table 3).
A trend of absolute compression of unhealthy LE was observed among Northern women and Southern men, while a trend of absolute expansion was observed among Southern women and Central women and men. Among Northern men, an equilibrium between absolute compression and expansion was detected, as there were no changes in overall unhealthy LE during the period. A trend of relative compression of unhealthy LE was observed among Northern and Southern men and women, while relative expansion was detected among Central men and an equilibrium between relative compression and expansion was detected among Central women (tables 1and 3). Central European men were the only population group in which an inclination towards the dynamic equilibrium was observed, as there was a trend of absolute as well as relative expansion of unhealthy LE together with a shift from severe (i.e. frail) to moderate (i.e. pre-frail) ill health. The proportion of remaining LE in a frail state decreased from 10.5% (95% CI: 8.6–12.3) to 10.0% (95% CI: 8.9–11.1) while the proportion of remaining LE in a pre-frail state increased from 17.6% (95% CI: 15.3–19.9) to 18.8% (95% CI: 17.4–20.2) (table 3).
Discussion
In this paper, we focused on evaluating the development in time spent with and without frailty over a 10–11-year period, and we assessed gender and regional differences in the European population of older adults.
Our analysis showed that a minority of the European population of 70+ yearolds were frail in 2004–05 (15.6%), and that there was a slight decrease in 2015 (15.0%).
We found disparity in healthy LE (non-frail) and unhealthy LE (pre-frail and frail) across gender, with women spending more time in an unhealthy state compared with men, and across regions, with Southern Europeans spending considerably more time in an unhealthy state compared with Northern and Central Europeans. From 2004–05 to 2015, we found that healthy LE increased along with total LE for men as well as women in each European regional area. However, during the observation period, unhealthy LE did also increase for some groups in the study population, revealing disparity across gender and regions. Northern European women and Southern European men had the most positive development during the 10–11-year period, compressing absolute as well as relative unhealthy LE, while Central European men were worse off expanding absolute and relative unhealthy LE.
To our knowledge, this study is the first to investigate the development in HLE spent in different states of frailty over time in the European population. While other studies have looked at the development in HLE in Europe with respect to other health indicators, comparison across results is difficult due to differences in methods (e.g. observation period, health indicator, agerange).27–29 In general, these studies report an increase in years spent in good health, but only in some populations does the increase in healthy life years exceed the increase in total LE during the observation period.27–29
The observed differences in time spent with and without frailty between men and women are consistent with findings from other comparable studies. Romero-Ortuno et al. found that LE at age 70 in a non-frail state was 8.1 years for men and 6.0 years for women, for the total study population of 15 European countries participating in the fourth wave (2010–11) of SHARE.14 Another study, conducted in a French population of 70+ yearolds in 2008–2010, found that women could expect to live 5.1 years in a non-frail state, while men could expect to live 6.4 years.15 These observations of women living longer lives but in poor health were also found in studies investigating HLE with respect to other health measures than frailty.28,30,31 The phenomenon has been termed the male–female health-survival paradox, and despite being studied extensively, the underlying mechanisms for these observed gender differences in LE and health are still poorly understood.32 Gender differences in biological, social and lifestyle risk factors as well as selection and information bias in surveys have been proposed as being potentially explanatory reasons for the phenomenon.32 A study in a French population found that women’s higher LE with disability compared with that of men was attributed to lower mortality from diseases as well as higher disability prevalences from mainly musculoskeletal diseases.33 The close connection between frailty and musculoskeletal diseases10 might explain some of the gender differences observed in time spent with and without frailty in this study.
Cross-country differences in frailty distribution in the European region have been documented in other studies as well. Santos-Eggimann et al. found that Southern European countries had a higher prevalence of frailty compared with Northern European countries.23 Similarly, another study among centenarians residing in five countries found that the Central European countries (France and Switzerland) had higher frailty prevalences compared with the Northern European countries (Denmark and Sweden).34Romero-Ortuno et al. found that LE in a pre-frail and frail state was highest in Southern countries like Spain and Italy and shortest in Northern and Central countries like Denmark, Sweden, Germany and the Netherlands.14 These disparities in frailty distribution across European countries are consistent with findings of a north-south gradient with respect to other health indicators in the European population.35,36 A study investigating the association between national economic gross domestic product and frailty in the SHARE countries found that higher-income countries (e.g. Denmark, Sweden, France, Germany, Belgium) had lower prevalence of frailty compared with lower-income countries (e.g. Spain and Italy),37 suggesting that the observed country differences in frailty may be caused by socioeconomic factors.14 The north-south gradient observed with respect to LE (lowest LE in Northern Europe and highest LE in Southern Europe), might be partly explained by the north-south gradient in cardiovascular diseases across Europe. Cardiovascular disease is the main cause of death in Europe, and Southern European countries have for several decades reported lower age-standardized death rates from ischaemic heart disease compared with the rest of Europe—most likely due to dietary differences.38
The strength of this study is the large national sample of people from 10 European countries interviewed 10–11 years apart, making it possible to compare trends in LE in different frailty states across European regions. A limitation of the SHARE-FI score is that four out of the five items included are based on self-reporting, which makes the measurement vulnerable towards misclassification. Additionally, since nursing home residents are underrepresented in SHARE, it is likely that the prevalence of the population in a frail state is underestimated.18
Despite being the most widely used method for estimating HLE, the Sullivan method has been criticized for its assumptions of stationary mortality and disability rates.39 The Multi State Life Table (MSLT) model, in which transition rates between different states of health and ultimately death are calculated in a longitudinal setting, has been highlighted as being superior to the Sullivan method for estimating HLE over time.39 However, as the MSLT model requires mortality data on an individual level, and as it has been documented that SHARE’s mortality follow-up systematically underestimates real mortality,40 we considered the Sullivan method to be the most appropriate considering the data.
Based on our findings, we cannot decisively conclude which of the three theories proposed by Fries (compression of morbidity),6 Gruenberg (expansion of morbidity)5 and Manton (dynamic equilibrium of morbidity)7 is true for the European population as a whole, as we found different trends across regional areas. However, our findings are encouraging in demonstrating that, generally, most of the extra years added to life in the European population from 2004–05 to 2015 are years spent in a non-frail state. Although there were substantial differences in LE with and without frailty among men and women in the three European regions, an improvement in years spent in a non-frail state was demonstrated for all groups.
HLE is a comprehensive public health indicator as it adds information about the quality of years lived in a population. As our analysis has shown, high LE does not necessarily equal a healthy life. Estimating and comparing the development of HLE across the ageing European population is of public health importance as it serves as an indicator of the process of promoting healthy and active ageing in the European region.
Further research into the development in HLE across gender and European regions is needed in order to decisively evaluate on whether Europeans are living longer and healthier lives and to gain further knowledge on what is driving the gender- and regional differences observed in HLE in Europe.
Supplementary data
Supplementary data are available at EURPUB online.
Funding
This paper uses data from SHARE Waves 1 and 6 (DOIs: 10.6103/SHARE.w1.6.1.1.and 10.6103/SHARE.w6.6.1.1.), see Börsch-Supan et al. (2013) for methodological details.15 The SHARE data collection has been primarily funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812) and FP7 (SHARE-PREP: N°211909, SHARE-LEAP: N°227822, SHARE M4: N°261982). Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Key points
A fundamental question in ageing research is whether longer life results in more years spent in good versus bad health.
Whether life expectancy with and without frailty has changed over time in Europe has so far received little attention.
We observed a general trend of increasing years spent in a non-frail state from 2004–05 to 2015 across European regions and sex.
We found disparity in years spent in a non-frail state across sex and regions.
Data availability statement
The data underlying this article were provided by the Survey of Health, Ageing and Retirement in Europe (SHARE) (http://www.share-project.org/home0.html) by permission.
Conflicts of interest: None declared.
Supplementary Material
References
- 1.Rau R, Soroko E, Jasilionis D, Vaupel JW.. Continued reductions in mortality at advanced ages. Popul Dev Rev 2008;34:747–68. [Google Scholar]
- 2.Oeppen J, Vaupel JW.. Broken limits to life expectancy. Science 2002;24:251–6. [DOI] [PubMed] [Google Scholar]
- 3.Beltrán-Sánchez H, Soneji S, Crimmins EM.. Past, present, and future of healthy life expectancy. Cold Spring Harb Perspect Med 2015;5:a025957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Christensen K, Doblhammer G, Rau R, Vaupel JW.. Ageing populations: the challenges ahead. Lancet 2009;374:1196–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gruenberg EM.The Failues of Success. 1977. Milbank Q 2005;83:779–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fries J.Aging, natural death, and the compression of the morbidity. N Engl J Med 1980;303: 130–8. [DOI] [PubMed] [Google Scholar]
- 7.Manton KG.Changing concepts of morbidity and mortality in the elderly population. Milbank Mem Fund Q Health Soc 1982;60:183. [PubMed] [Google Scholar]
- 8.Jagger C.Compression or expansion of morbidity – what does the future hold. Age Ageing 2000;29:93–4. [DOI] [PubMed] [Google Scholar]
- 9.Cesari M, Prince M, Thiyagarajan JA, et al. Frailty: an emerging public health priority. J Am Med Dir Assoc 2016;17:188–92. [DOI] [PubMed] [Google Scholar]
- 10.Chen X, Mao G, Leng SX.. Frailty syndrome: an overview. Clin Interv Aging 2014;9:433–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clegg A, Young J, Iliffe S, et al. Frailty in elderly people. Lancet 2013;381:752–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Puts MTE, Toubasi S, Andrew MK, et al. Interventions to prevent or reduce the level of frailty in community-dwelling older adults: a scoping review of the literature and international policies. Age Ageing 2017;46:383–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146–56. [DOI] [PubMed] [Google Scholar]
- 14.Romero-Ortuno R, Fouweather T, Jagger C.. Cross-national disparities in sex differences in life expectancy with and without frailty. Age Ageing 2014;43:222–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herr M, Arvieu J-J, Ankri J, Robine J-M.. What is the duration of life expectancy in the state of frailty? Estimates in the SIPAF study. Eur J Ageing 2018;15:165–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Börsch-Supan A, Brandt M, Hunkler C, et al. Data resource profile: the survey of health, ageing and retirement in Europe (share). Int J Epidemiol 2013;42:992–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Börsch-Supan A, Jürges H.. The Survey of Health, Ageing and Retirement in Europe – Methodology. Mannheim, Germany: MEA,2005. [DOI] [PMC free article] [PubMed]
- 18.Malter F, Börsch-Supan A. SHARE wave 6: panel innovations and collecting Dried Blood Spots. Munich, Germany: MEA,2017.
- 19.Bergmann M, Kneip T, de Luca G, Scherpenzeel A. Survey participation in the Survey of Health, Ageing and Retirement in Europe (SHARE), Wave 1-6. Munich, Germany: MEA, 2019.
- 20.Romero-Ortuno R, Walsh CD, Lawlor BA, Kenny RA.. A frailty instrument for primary care: findings from the Survey of Health, Ageing and Retirement in Europe (SHARE). BMC Geriatr 2010;10:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Romero-Ortuno R, Kenny RA.. The frailty index in Europeans: association with age and mortality. Age Ageing 2012;41:684–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Romero-Ortuno R, O’Shea D, Kenny RA.. The SHARE frailty instrument for primary care predicts incident disability in a European population-based sample. Qual Prim Care 2011;19:301–9. [PubMed] [Google Scholar]
- 23.Santos-Eggimann B, Cuenoud P, Spagnoli J, Junod J.. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. Journals Gerontol – Ser A Biol Sci Med Sci 2009;64A: 675–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jagger C, Oyen HV, Robine J-M.. Health expectancy calculation by the Sullivan method: a practical guide. Newcastle University Institute of Ageing,2014;1–40. [Google Scholar]
- 25.Eurostat. EUROSTAT Database.2015. Available at: http://epp.eurostat.cec.eu.int(14 February 2021, date last accessed).
- 26.Nusselder W. Compression or expansion of morbidity? A life table approach. Erasmus University, Rotterdam,1998;1–253.
- 27.Van Oyen H, Cox B, Demarest S, et al. Trends in health expectancy indicators in the older adult population in Belgium between 1997 and 2004. Eur J Ageing 2008;5:137–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jagger C, Matthews FE, Wohland P, et al. A comparison of health expectancies over two decades in England: results of the Cognitive Function and Ageing Study I and II. Lancet 2016;387:779–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sundberg L, Agahi N, Fritzell J, Fors S.. Trends in health expectancies among the oldest old in Sweden, 1992–2011. Eur J Public Health 2016;26:1069–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van Oyen H, Nusselder W, Jagger C, et al. Gender differences in healthy life years within the EU: an exploration of the “health-survival” paradox. Int J Public Health 2013;58:143–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jagger C, Matthews F.. Gender differences in life expectancy free of impairment at older ages. J Women Aging 2002;14:85–97. [DOI] [PubMed] [Google Scholar]
- 32.Oksuzyan A, Brønnum-Hansen H, Jeune B.. Gender gap in health expectancy. Eur J Ageing 2010;7:213–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nusselder WJ, Cambois EM, Wapperom D, et al. Women’s excess unhealthy life years: disentangling the unhealthy life years gap. Eur J Public Health 2019;29:914–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Herr M, Jeune B, Fors S, et al. ;5-COOP group. Frailty and associated factors among centenarians in the 5-COOP countries. Gerontology 2018;64:521–31. [DOI] [PubMed] [Google Scholar]
- 35.Ahrenfeldt LJ, Scheel-Hincke LL, Kjærgaard S, et al. Gender differences in cognitive function and grip strength: a cross-national comparison of four European regions. Eur J Public Health 2019;29:667–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scheel-Hincke LL, Möller S, Lindahl-Jacobsen R, et al. Cross-national comparison of sex differences in ADL and IADL in Europe: findings from SHARE. Eur J Ageing 2020;17:69–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Theou O, Brothers TD, Rockwood MR, et al. Exploring the relationship between national economic indicators and relative fitness and frailty in middle-aged and older Europeans. Age Ageing 2013;42:614–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mladovsky P, Allin S, Masseria C, et al. Health in the European Union: trends and analysis. European Observatory on Health Systems and Policies. 2009.
- 39.Imai K, Soneji S.. On the estimation of disability-free life expectancy: Sullivan’smethod and its extension. J Am Stat Assoc 2007; 102:1199–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schulz A, Doblhammer G.. Validity of the mortality follow-up in SHARE. Princeton. 2010. Available at: https://epc2010.princeton.edu/papers/100401 (15 February 2021, date last accessed). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article were provided by the Survey of Health, Ageing and Retirement in Europe (SHARE) (http://www.share-project.org/home0.html) by permission.
Conflicts of interest: None declared.