Abstract
Objective:
Spiritual well-being (SpWb) is an important dimension of health-related quality of life for many cancer patients. Accordingly, an increasing number of psychosocial intervention studies have included SpWb as a study endpoint, and may improve SpWb even if not designed explicitly to do so. This meta-analysis of randomized controlled trials (RCTs) evaluated effects of psychosocial interventions on SpWb in adults with cancer and tested potential moderators of intervention effects.
Methods:
Six literature databases were systematically searched to identify RCTs of psychosocial interventions in which SpWb was an outcome. Doctoral-level rater pairs extracted data using Covidence following Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines. Standard meta-analytic techniques were applied, including meta-regression with robust variance estimation and risk-of-bias sensitivity analysis.
Results:
Forty-one RCTs were identified, encompassing 88 treatment effects among 3883 survivors. Interventions were associated with significant improvements in SpWb (g = 0.22, 95% CI [0.14, 0.29], p < 0.0001). Studies assessing the FACIT-Sp demonstrated larger effect sizes than did those using other measures of SpWb (g = 0.25, 95% CI [0.17, 0.34], vs. g = 0.10, 95% CI [−0.02, 0.23], p = 0.03]. No other intervention, clinical, or demographic characteristics significantly moderated effect size.
Conclusions:
Psychosocial interventions are associated with small-to-medium-sized effects on SpWb among cancer survivors. Future research should focus on conceptually coherent interventions explicitly targeting SpWb and evaluate interventions in samples that are diverse with respect to race and ethnicity, sex and cancer type.
Keywords: cancer, interventions, meta-analysis, psycho-oncology, randomized controlled trials, spiritual well-being
1 |. INTRODUCTION
Religion and spirituality (R/S) are important aspects of many cancer patients’ lives and salient to coping with cancer and its treatment.1–5 Despite conceptual challenges in defining constructs within R/S,6,7 ‘spiritual well-being’ (SpWb) is one clinically useful way of describing this important area of life for many patients. SpWb refers to ‘the degree to which patients’ spirituality can help them make sense of their lives, and feel whole, hopeful and peaceful even in the midst of a serious illness.8 SpWb reflects patients’ spiritual health related to but distinct from religious behaviours and is often construed as a dimension of health-related quality of life.9 SpWb is associated with clinically relevant outcomes including depression, end of life coping and caregiver well-being.10,11
Several interventions have been developed to address SpWb in those with advanced disease.12 Other interventions, administered in a range of cancer settings, might also promote salutary changes in SpWb, even if this was not their primary aim. For example, even interventions that target seemingly removed outcomes such as physical activity may affect SpWb through the therapeutic process itself or through skill-building (e.g., emotion regulation and mindfulness). Further, given the known barriers many survivors face accessing psychological care, it is important to determine whether SpWb can be improved through an array of intervention approaches. Interventions have varied with respect to delivery (e.g., nurse and psychologist), format (e.g., individual and group) and cancer population of interest (e.g., advanced stage of disease and post-treatment survivorship).13,14 Whether these efforts generate significant improvements in SpWb remains an important question. Moreover, it is unclear whether intervention effects differ for patients at varying phases of the cancer care trajectory (i.e., active treatment and post-treatment survivorship), and whether different modes and formats of intervention delivery achieve distinct effects on SpWb.
To address these questions, we conducted a meta-analytic review of the existing evidence for psychosocial interventions that measure change in SpWb. Specifically, the present meta-analysis of randomized controlled trials (RCTs) evaluated the effects of psychosocial interventions on SpWb in adults with cancer and tested hypothesized moderators (e.g., primacy of SpWb outcome, cancer treatment phase and delivery) of intervention effects.
2 |. METHODS
This meta-analysis was conducted as part of a broader set of analyses of the effects of psychosocial interventions on positive psychological well-being in cancer survivors (defined as ‘survivor’ from the point of diagnosis on; meta-analysis project through R03CA184560). This research was exempt from Institutional Review Board review. See Park et al. for detailed description of overall meta-analysis methods used.15 Below, we briefly describe key methodological details specific to this study. The raw data (including effect size estimates, variance estimates and moderator variables) and code for replicating all reported analyses are available in the supplementary materials accompanying this article.
2.1 |. Search strategy
A health sciences librarian developed the database search strategies in consultation with two other authors (John M. Salsman, MAS). We searched MEDLINE (Ovid), PsycINFO (EBSCOhost), CINAHL with Full Text (EBSCOhost), EMBASE (Elsevier), The Cochrane Library (Wiley) and Web of Science (Clarivate Analytics). We ran the original database searches on 5 January 2015 and ran search updates on 9 January 2017 and 14 September 2018. For the MEDLINE search, we used the McMaster multi-term filters with the best balance of sensitivity and specificity for retrieving RCTs and systematic reviews.16,17 Detailed search strategies for each database are available in the supplementary materials accompanying this article.15
2.2 |. Eligibility criteria
Eligibility criteria included as follows: (a) evaluation of psychosocial intervention using a RCT, (b) written in English, (c) study sample included cancer survivors age 18 years or older and (d) included SpWb as an outcome. Psychosocial interventions included any non-medical or non-pharmacological intervention that targeted thoughts, feelings, or behaviours. See Park et al. for detailed description of potential interventions.15
2.3 |. SpWb outcomes
SpWb is conceptualized in multiple ways including affective, cognitive and belief domains. Some measures include aspects of religious behaviour (e.g. Church attendance and prayer) as well as assuming a particular religious affiliation (e.g. Judeo-Christian-specific wording). To increase clinical relevance and generalizability of findings, we included SpWb measures that were not restricted to a specific religious affiliation (e.g., SpWb Scale).18 Our search terms were not restricted by measure names. Rather, each returned article’s measure of SpWb, including item content, was reviewed for congruence with our operationalization of the SpWb construct. Measures included in our final analysis were the FACIT-Sp9 total score (studies that only analysed meaning or meaning/peace subscales excluded), expanded FACIT-Sp-EX,9,19 Quality of Life-Breast Cancer spiritual well-being subscale,20 Linear Analogue-Self Assessment—spiritual well-being item,21 Expressions of Spirituality Inventory and the Body-Mind-Spirit Well-Being Inventory.22
2.4 |. Study selection
See Park et al. for detailed description.15 Five doctoral-level investigators comprised the review team. Covidence, a Cochrane technology platform, was used to manage study reviews and coding. A pair of raters independently reviewed each abstract to determine whether it met inclusion criteria for full text review. A pair of raters then independently extracted data elements and resolved any discrepancies though consensus.
2.5 |. Data coding
Demographic (e.g., sample age and sex), clinical (cancer type, stage and phase of cancer care) and intervention study characteristics (intervention delivery format, modality, type of intervention, session number, comparison group, follow-up time and outcome measure, described below) were extracted. Delivery format included in-person, online, telephone, print, self-delivered, or a combination. Intervention modality included individual, dyad, or group-based. Psychosocial interventions included non-pharmacologic interventions targeting thoughts, feelings, or behaviour. Interventions incorporating physical activity (e.g., yoga) were included. Intervention-type included creative arts, education/healthy lifestyle behaviours, meaning/existential, mediation/yoga, skills-based/Cognitive Behavioural Therapy, or multimodal (i.e., a combination of category types). Intervention types were identified using a conceptual framework and based on previous meta-analyses and systematic review groupings.14 Laurie E. McLouth, C. Graham Ford and John M. Salsman coded intervention type, interventionist details (e.g., provider type and professional discipline), and comparison group type. Comparison groups included either active control (i.e., attention, education and component control), or wait-list or standard/usual care.23,24 Outcome factors included how SpWb was utilized in the study aims and analytic plan (i.e., primary, secondary or unspecified outcome) and what measure was used to assess SpWb (FACIT-Sp vs. other).
2.6 |. Assessment of risk of bias
Risk of bias (ROB) categories included: randomization sequence generation, allocation concealment, attrition and outcome reporting.25 Each was categorized as low, unclear or high ROB.25 We did not evaluate blinding of participants or blinding of outcome assessors, as blinding is often not feasible for psychosocial intervention trials.
2.7 |. Effect size calculations and meta-analytic procedures
We present key analytic information here; see Salsman et al. for detailed description of analytic procedures.26 Standardized mean differences, using Hedge’s g correction, between treatment and control groups were estimated. The estimated difference between treatment and control groups, adjusted for baseline differences (i.e., change-score or regression adjustment), was used for the numerator of the effect size estimate. Standard deviations, pooled across groups, in the baseline outcome measure were used for the denominator of the effect size estimate. See Salsman et al. for missing baseline data procedures.26 We calculated effect size estimates using reported mean and standard deviation estimates by group, or statistical tests (e.g., t- or F-statistics, p-values) when mean and SD estimates were missing. Before conducting further analysis, we examined the distribution of effect size estimates for outliers. None were identified. Additionally, we used leave-one-out sensitivity analyses to identify studies with a strong influence on overall results.
Many studies reported effects at multiple assessment points or compared multiple treatment groups to a common control group, leading to statistical dependence between effect sizes. Traditional methods of handling dependent effect sizes entail either aggregating effect size estimates, creating sub-groups, or selecting one effect size per study to avoid dependency,27 all of which make it difficult to conduct moderator analysis for characteristics that vary across effect sizes within study. To avoid this problem, we used the more recently developed approach of random effects meta-analysis with robust variance estimation.27–29 This approach allows for inclusion of all relevant effect sizes in the overall meta-analysis and moderator analysis, while estimating uncertainty using methods that are robust to statistical dependency among effect size estimates from common samples. Following best practices, we conducted sensitivity analyses to varying levels of assumed dependence between effect size estimates.27 We calculated restricted maximum likelihood estimates of the between-study SD () to describe the extent of heterogeneity among effect sizes as well as the I2 statistic to describe the extent to which heterogeneity among true effect sizes contributes to observed variation in effect size estimates.30 Moderators of intervention effect sizes were tested using a random effects meta-regression model that allowed for between-study variance components to vary across levels of the moderator.
ROB in meta-analytic results due to small-study effects was assessed using a funnel plot of estimates and a modified version of Egger’s regression test for plot symmetry.31 Robust variance estimation was used account for dependence of effect size estimates nested within studies.
Analyses were conducted in R using the metafor package and clubSandwich package.32,33 Results below follow the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines.34
3 |. RESULTS
3.1 |. Study selection
The search of the electronic databases retrieved 3457 citations (Figure 1). After removal of duplicates, 3407 remained and were evaluated on the basis of title and abstract. Of these, 2893 were discarded because they did not meet the inclusion criteria and were position or purely theoretical papers, review papers, descriptive or observational studies or qualitative studies. Five hundred and fourteen potentially relevant references were screened in more detail on the basis of the full texts. Of these, 41 met inclusion criteria (Table 1).35–75 Each study contributed between 1 and 8 effect size estimates, with a median of 2 effect sizes per study and a total of 88 effect size estimates. Studies contributing multiple effects involved multiple active intervention arms40,42,48,53 or assessed SpWb at multiple follow-up times.35–38,40,42,44,47,48,50–54,56,61–63,68,70–73
FIGURE 1.

Preferred reporting items for systematic reviews and meta-analyses flow diagram
TABLE 1.
Study characteristics of included 41 randomized controlled trials
| Author | Age (mean) | % Female | Cancer-type | Cancer stage | Cancer phase | Delivery format | Modality | Intervention-type | Control | Outcome | SpWb measure |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Badger36 | 66.99 | 0.00 | Prostate | Mixed | Mixed | Phone | Dyad | Skills based/CBT | A/E/C | Unspecified | QOL-BC SpWB |
| Badger35 | 47.34 | 100.00 | Breast | Mixed | PT | Phone | Dyad | Skills based/CBT | A/E/C | Secondary | QOL-BC SpWB |
| Breitbart38 | 60.10 | 51.10 | Mixed | Advanced | Mixed | In-person | Group | Meaning/Existential | A/E/C | Primary | FACIT-Sp |
| Breitbart39 | 54.40 | 60.50 | Mixed | Advanced | Mixed | In-person | Individual | Meaning/Existential | A/E/C | Primary | FACIT-Sp |
| Breitbart37 | 58.20 | 69.50 | Mixed | Advanced | NR | In-person | Group | Meaning/Existential | A/E/C | Primary | FACIT-Sp |
| Breitbart40 | 58.00 | 71.70 | Mixed | Advanced | Pal | In-person | Individual | Meaning/Existential | A/E/C | Primary | FACIT-Sp |
| Carlson41 | 54.66 | 100 | NR | NR | NR | In-person | Group | Meditation/Yoga | A/E/C | Secondary | FACIT-Sp |
| Cohen42 | 51.86 | 100.00 | Breast | Mixed | Cur | In-person | Individual | Education/HLB | A/E/C | Secondary | FACIT-Sp |
| Cook43 | 59.53 | 53.00 | Mixed | NR | NR | In-person | Individual | Creative arts | WL/SC | Primary | FACIT-Sp |
| Cramer44 | 68.26 | 38.90 | Colorectal | Mixed | Mixed | In-person | Group | Meditation/Yoga | A/E/C | Secondary | FACIT-Sp |
| Djuric45 | 55.50 | 100.00 | Breast | Early | PT | In-person | Individual | Meditation/Yoga | A/E/C | Unspecified | FACIT-Sp |
| Fauver46 | 64.15 | NR | Mixed | Mixed | Mixed | In-person | Group | Meaning/Existential | WL/SC | Unspecified | FACIT-Sp-EX |
| Ferguson47 | 50.28 | 100.00 | Breast | Early | PT | In-person | Individual | Skills Based/CBT | A/E/C | Primary | QOL-CS SpWb |
| Freeman48 | 55.40 | 100.00 | Breast | Mixed | PT | In-person | Group | Multimodal | WL/SC | Secondary | FACIT-Sp-EX |
| Guthrey49 | NR | 97.00 | Mixed | Mixed | PT | In-person | Group | Meaning/Existential | WL/SC | Unspecified | FACIT-Sp-EX |
| Hanser50 | 51.50 | 100.00 | Breast | Advanced | Cur | In-person | Individual | Creative arts | A/E/C | Primary | FACIT-Sp |
| Hawkes51 | 66.35 | 46.10 | Colorectal | Mixed | Mixed | In-person | Individual | Skills based/CBT | A/E/C | Primary | FACIT-Sp |
| Heiney52 | 50.40 | 100.00 | Breast | Early | Mixed | Phone | Group | Skills based/CBT | A/E/C | Unspecified | QOL-BC SpWB |
| Henderson53 | 49.80 | 100.00 | Breast | Early | Mixed | In-person | Group | Meditation/Yoga | A/E/C | Primary | FACIT-Sp |
| Hoogland54 | 51.40 | 100.00 | Mixed | Mixed | Mixed | In-person | Individual | Skills based/CBT | A/E/C | Primary | FACIT-Sp |
| Jafari55 | 48.00 | 100.00 | Breast | NR | NR | In-person | Group | Meaning/Existential | A/E/C | Primary | FACIT-Sp |
| Juarez56 | 49.65 | 100.00 | Breast | Mixed | PT | In-person | Individual | Education/HLB | A/E/C | Primary | QOL-BC SpWB |
| Kristeller57 | 59.98 | 55.06 | Mixed | NR | Mixed | In-person | Individual | Skills based/CBT | A/E/C | Unspecified | FACIT-Sp |
| Leal58 | 41.00 | 62.50 | Lymphoma | Mixed | Mixed | In-person | Group | Meditation/Yoga | A/E/C | Unspecified | FACIT-Sp |
| Liao59 | 61.82 | 50.00 | NR | NR | NR | NR | Individual | Multimodal | A/E/C | Primary | FACIT-Sp |
| Liu60 | 49.11 | 100.00 | Breast | Mixed | PT | In-person | Group | Multimodal | A/E/C | Unspecified | BMSWBI |
| Lo61 | 56.00 | 70.00 | Mixed | Advanced | NR | In-person | Individual | Skills based/CBT | A/E/C | Secondary | FACIT-Sp |
| Loerzel62 | 72.10 | 100.00 | Breast | Early | PT | In-person | Individual | Multimodal | A/E/C | Primary | QOL-BC SpWB |
| Meneses63 | 54.50 | 100.00 | Breast | Early | PT | In-person | Individual | Education/HLB | A/E/C | Secondary | QOL-BC SpWB |
| Milbury64 | 53.63 | 100.00 | Breast | Early | PT | In-person | Group | Meditation/Yoga | A/E/C | Secondary | FACIT-Sp |
| Moadel65 | 54.81 | 100.00 | Breast | Mixed | Mixed | In-person | Group | Meditation/Yoga | A/E/C | Primary | FACIT-Sp |
| Nidich66 | 63.84 | 100.00 | Breast | Mixed | NR | In-person | Individual | Meditation/Yoga | A/E/C | Secondary | FACIT-Sp |
| Olesen67 | 50.03 | 100.00 | Ovarian | Early | PT | In-person | Individual | Education/HLB | A/E/C | Primary | QOL-CS SpWb |
| Piderman68 | 59.30 | 34.52 | Mixed | NR | Cur | In-person | Dyad | Skills based/CBT | A/E/C | Secondary | FACIT-Sp |
| Puig69 | 51.40 | 100.00 | Breast | Early | Mixed | In-person | Individual | Creative arts | A/E/C | Unspecified | EOSI |
| Radl70 | 52.13 | 100.00 | Mixed | Mixed | Cur | In-person | Individual | Creative arts | A/E/C | Secondary | FACIT-Sp |
| Radl71 | 52.13 | 100.00 | Mixed | Mixed | Mixed | In-person | Individual | Creative arts | A/E/C | Secondary | FACIT-Sp |
| Rodin72 | 59.08 | 60.00 | NR | Advanced | NR | In-person | Individual | Multimodal | A/E/C | Secondary | FACIT-Sp |
| Roth73 | 76.00 | 53.00 | Mixed | Mixed | Mixed | Phone | Individual | Skills based/CBT | A/E/C | Secondary | FACIT-Sp |
| Rummans74 | 59.54 | 35.92 | Mixed | Advanced | NR | In-person | Group | Skills based/CBT | A/E/C | Secondary | LASA |
| Zernicke75 | 58.00 | 72.58 | Mixed | Mixed | PT | Online | Group | Meditation/Yoga | A/E/C | Secondary | FACIT-Sp |
Abbreviations: A/E/C, Attention/Education/Component control; BMSWBI, Body-Mind-Spirit Well-Being Inventory; CBT, Cognitive Behavioural Therapy; Cur, Curative; Education/HLB, Education/Healthy Lifestyle Behaviours; EOSI, Expressions of Spirituality Inventory; FACIT-Sp, FACIT-Sp Total Score; FACIT-Sp-Ex, Expanded FACIT-Sp; LASA, Linear Analogue-Self Assessment spiritual well-being item; NR, Not reported; Pal, Palliative; PT, Post-treatment; QOL-CS SpWb, Quality of Life-Breast Cancer Spiritual Well-Being subscale; WL/SC, Waitlist or standard care.
3.2 |. Overall description of studies and effects
See Table 2 for demographic, clinical and intervention characteristics of included studies. The average intervention length was 7.6 sessions (SD = 5.4). The majority were delivered in-person (83%) in the outpatient setting (93%). Twenty percent did not specify the provider background of the interventionist; 27% were delivered by a mental health provider and an additional 15% were co-led, often with a mental health provider. Sixty percent of studies included multiple assessments of SpWb. The average number of weeks from baseline after which SpWb was assessed was 18.2 (SD = 18.6; range = 0.43 – 104). Across 41 RCTs, 88 effect sizes, and a combined sample of 3883 participants (M age = 56.4, SD = 7.2), the weighted average effect of SpWb outcomes was estimated as g = 0.22, 95% CI = 0.14 – 0.29, p < 0.0001. The estimated between-study standard deviation was (I2 = 52%), indicating substantial heterogeneity of effects across studies.
TABLE 2.
Moderator analyses of demographic, clinical, intervention, study design, and outcome variables
| Mean (SD) | Number of studies | Number of effect size estimates | Average ES (95% Cl) | I2 (%) | F(df1, df2) | P | ||
|---|---|---|---|---|---|---|---|---|
| Demographic factors | ||||||||
| Average participant age | 56.4 (7.2) | 40 | 87 | −0.003 (−0.02. 0.01) | 0.13 | 55 | 0.27 (1, 12.7) | 0.612 |
| Average % female | 79.5 | 40 | 87 | 0.00 (−0.004, 0.004) | 0.14 | 56 | 0.00 (1, 12.3) | 0.988 |
| Clinical variables | ||||||||
| Cancer-type | - | - | - | - | - | 34 | 0.87 (1, 19.0) | 0.362 |
| Breast | - | 17 | 40 | 0.24 (0.10. 0.39) | 0.18 | - | - | - |
| Othera | - | 24 | 48 | 0.17 (0.10, 0.25) | 0.03 | - | - | - |
| Cancer stage | - | - | - | - | - | 53 | 1.34 (2. 10.2) | 0.311 |
| Early | - | 9 | 19 | 0.19 (0.02, 0.36) | 0.03 | - | - | - |
| Advanced | - | 8 | 19 | 0.27 (0.09, 0.44) | 0.07 | - | - | - |
| Mixed | - | 18 | 39 | 0.14 (0.07, 0.22) | 0.00 | - | - | - |
| Not reported | - | 6 | 11 | 0.42 (−0.31, 0.86) | 0.36 | - | - | - |
| Cancer phase | - | - | - | - | - | 39 | 0.07 (2. 5.5) | 0.937 |
| Curative | - | 4 | 19 | 0.17 (0.03, 0.30) | 0.00 | - | - | - |
| Mixed | - | 15 | 30 | 0.16 (0.06, 0.26) | 0.00 | - | - | - |
| Palliative | - | 1 | 6 | 0.21 (−1.72, 2.13) | 0.07 | - | - | - |
| Post-treatment | - | 12 | 21 | 0.19 (0.04, 0.34) | 0.02 | - | - | - |
| Not reported | - | 9 | 12 | 0.35 (0.08, 0.62) | 0.29 | - | - | - |
| Intervention characteristics | ||||||||
| Delivery format | - | - | - | - | - | 28 | 1.48 (1, 4.1) | 0.290 |
| In-person | - | 34 | 74 | 0.21 (0.14, 0.29) | 0.10 | - | - | - |
| Otherb | - | 7 | 13 | 0.15 (−0.02, 0.32) | 0.00 | - | - | - |
| Intervention modality | - | - | - | - | - | 45 | 2.50 (2, 4.7) | 0.182 |
| Individual | - | 22 | 49 | 0.16 (0.10, 0.22) | 0.00 | - | - | - |
| Dyad | - | 3 | 10 | 0.01 (−0.59, 0.62) | 0.14 | - | - | - |
| Group | - | 16 | 29 | 0.33 (0.17, 0.48) | 0.20 | - | - | - |
| Intervention-type | - | - | - | - | - | 55 | 2.15 (5. 9.4) | 0.147 |
| Creative arts | - | 5 | 10 | 0.32 (0.14, 0.50) | 0.00 | - | - | - |
| Education/Healthy lifestyle behaviours | - | 5 | 12 | 0.03 (−0.17, 0.22) | 0.08 | - | - | - |
| Meaning/Existential | - | 7 | 12 | 0.39 (0.09, 0.70) | 0.26 | - | - | - |
| Meditation/Yoga | - | 10 | 17 | 0.25 (0.09, 0.41) | 0.17 | - | - | - |
| Multimodal | - | 5 | 10 | 0.28 (−0.10, 0.67) | 0.17 | - | - | - |
| Skills-based/CBT | - | 12 | 27 | 0.14 (0.04, 0.23) | 0.00 | - | - | - |
| Intervention sessions | - | 39 | 85 | −0.001 (−0.02, 0.02) | 0.13 | 55 | 0.10 (1, 1.7) | 0.786 |
| Study design characteristics | ||||||||
| Control group type | - | - | - | - | - | 34 | 0.30 (1, 2.9) | 0.623 |
| Attention, education, or component control | - | 37 | 81 | 0.21 (0.14, 0.29) | 0.13 | - | - | - |
| Wait-list or standard care | - | 4 | 7 | 0.27 (−0.09. 0.63) | 0.00 | - | - | - |
| Outcome factors | ||||||||
| Spiritual well-being outcome | - | - | - | - | - | 30 | 2.88 (2, 14.2) | 0.089 |
| Primary | - | 17 | 39 | 0.31 (0.17, 0.46) | 0.20 | - | - | - |
| Secondary | - | 15 | 38 | 0.15 (0.06, 0.23) | 0.00 | - | - | - |
| Unspecified | - | 9 | 11 | 0.09 (0.08, 0.26) | 0.00 | - | - | - |
| Outcome measure | - | - | - | - | - | 42 | 6.27 (1, 9.7) | 0.032 |
| FACIT-Sp | - | 30 | 67 | 0.25 (0.17, 0.34) | 0.13 | - | - | - |
| Otherc | - | 12 | 21 | 0.10 (−0.02, 0.23) | 0.00 | - | - | - |
Abbreviations: CBT, Cognitive Behavioural Therapy; LASA, Linear Analogue-Self Assessment; QOL-CS SpWb, Quality of Life-Breast Cancer Spiritual Well-Being subscale.
Other cancer types included: Cervical, head/neck, prostate, leukemia, melanoma and mixed types.
Other delivery formats included: Online, telephone, print, self-delivered and combinations thereof.
Other outcome measures included: QOL-BC spiritual well-being subscale, QOL-CS spiritual well-being subscale, Body-mind-spirit well-being inventory (BMSWBI), LASA, spiritual well-being item, Expressions of Spirituality Inventory.
Summary effect estimates were not sensitive to the assumed sampling correlation between effect size estimates drawn from the same study, suggesting the level of dependency assumed did not have a strong impact on the magnitude of the overall effect size. Specifically, in sensitivity analyses that varied the assumed correlation between 0.0 and 0.9, weighted average effect estimates ranged from 0.20 (95% CI = 0.14 – 0.27) to 0.25 (95% CI = 0.16 – 0.34). Between-study standard deviation estimates ranged from 0.12 (assuming correlation of 0.4) to 0.18 (assuming correlation of 0.9). For correlations at 0.8 or below, the estimated between-study standard deviation was always 0.14 or less.
Leave-one-out sensitivity analyses suggested one study, Jafari55 strongly influenced the estimated effect size distribution (g = 0.99, SE = 0.18). Excluding the effect size estimate from Jafari reduced the overall average effect estimate to g = 0.17, 95% CI = 0.11–0.22, p < 0.0001, and the between-study heterogeneity estimate to .
3.3 |. ROB
We conducted sensitivity analysis examining how study risk-of-bias affected estimates of the overall average effect size and degree of heterogeneity with successively stronger inclusion criteria applied at each step. The first row of Table 3 shows the estimated distribution of effect sizes across all included studies. Rows that follow show the estimates for subsets of studies and how the overall average effect estimate is influenced by the stringency of inclusion criteria. Including only the 31 studies (69 effects) that were at low risk-of-bias for outcome reporting, the overall average effect size estimate was g = 0.23, 95% CI = 0.13, 0.33, . Including only the seven studies (13 effects) that were also at low risk-of-bias for allocation concealment, the overall average effect size estimate was g = 0.24, 95% CI = 0.01, 0.48, . Including only the six studies (10 effects) that were also low risk-of-bias for sequence generation, the overall average effect size estimate was g = 0.24, 95% CI = −0.02, 0.51, . This sensitivity analysis indicates that risk-of-bias factors were not associated with effect magnitude.
TABLE 3.
Risk-of-bias analysis using successive inclusion criteria
| Criteria | Studies (Effects) | Estimate (SE) | 95% CI | I2 (%) | |
|---|---|---|---|---|---|
| All studies | 41 (88) | 0.22 (0.04) | (0.14, 0.29) | 0.12 | 52 |
| + Low ROB outcome reporting | 31 (69) | 0.23 (0.05) | (0.13, 0.33) | 0.17 | 63 |
| + Low ROB allocation concealment | 7 (13) | 0.24 (0.09) | (0.01, 0.48) | 0.13 | 41 |
| + Low ROB sequence generation | 6 (10) | 0.24 (0.10) | (−0.02, 0.51) | 0.15 | 48 |
Abbreviation: ROB, risk-of-bias.
3.3.1 |. Small sample size:
See Figure 2 for a funnel plot of effect size estimates versus scaled standard errors. Using Egger’s regression test, the estimated slope for the scaled standard error was , 95% CI = −0.19, 1.11, p = 0.140, indicating there was not clear evidence for small-study effects. However, limiting the analytic sample to the 15 studies (27 effects) with post-test sample sizes larger than 80 led to decreased estimates of the overall average effect (g = 0.14, 95% CI = 0.09, 0.19) and decreased heterogeneity (, I2 = 0%).
FIGURE 2.
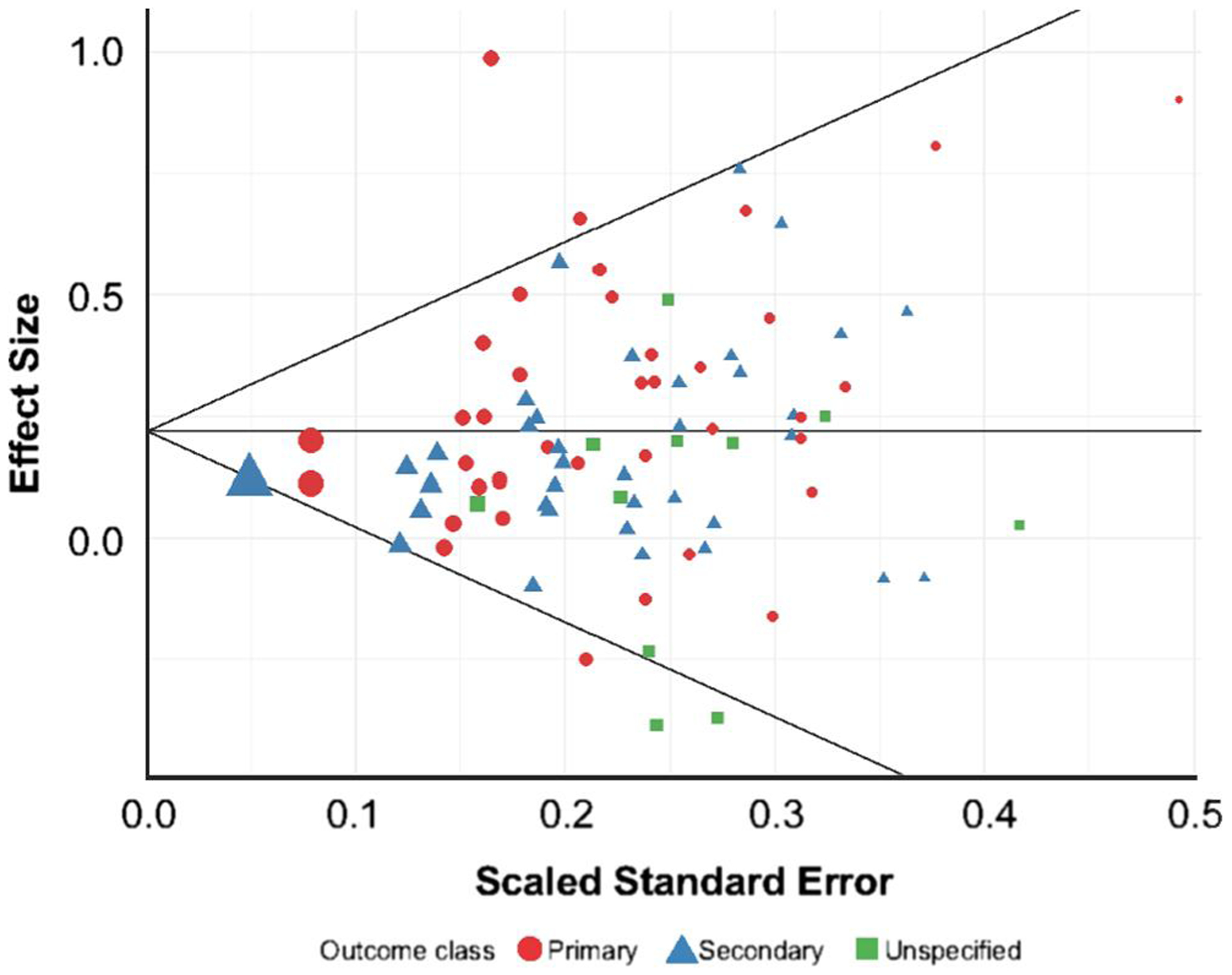
Funnel plot
3.3.2 |. Moderator Analyses
Moderator analyses were conducted on demographic factors, clinical variables, intervention characteristics, study design characteristics, as well as outcome factors.
See Table 2 for moderator results. There were not statistically significant differences in treatment effects on SpWb based on demographic, clinical, or intervention characteristics. The only variable that moderated the effect of interventions on SpWb was outcome measure. Studies that used the FACIT-Sp to measure SpWb showed larger effect sizes compared to studies that did not (g = 0.25, 95% CI = 0.17–0.34 FACIT-Sp vs. g = 0.10, 95% CI = −0.02–0.23 other measures of SpWb; p = 0.032). There was a non-statistically significant difference in effect sizes based on outcome type such that studies that assessed SpWb as the primary outcome showed larger effects (g = 0.31, 95% CI = 0.17–0.46) compared to studies that assessed SpWb as a secondary (g = 0.15, 95% CI = 0.06–0.23) or unspecified outcome (g = 0.09, 95% CI = −0.08–0.26). Moreover, there was a non-statistically significant difference in effect size magnitude based upon intervention type, with meaning/existential interventions demonstrating the largest effects (g = 0.39, 95% CI = 0.09, 0.70).
4 |. DISCUSSION
This is the first meta-analysis of the effects of psychosocial interventions on SpWb outcomes among cancer survivors. Results drawn from 41 RCTs encompassing 3883 participants suggest psychosocial interventions can increase SpWb in cancer patients. Results also suggest several considerations for future trial design and gaps in the literature on psychosocial interventions for SpWb in cancer.
The average effect of interventions on SpWb (g = 0.22) was modest, but comparable with the effects of interventions on other common concerns in cancer (e.g., fatigue g = 0.26–0.30)32 and other indicators of well-being (e.g., meaning/purpose = g = 0.37; positive affect = 0.35).12,26 Sensitivity analyses to examine risk-of-bias suggested interventions at low ROB yielded similar effect sizes; however, one study55 exerted strong influence on the effect size estimates. Omitting this study reduced the estimate to g = 0.17. We included this study in our overall effect size because study design characteristics (i.e., breast cancer sample, explicit focus on SpWb and use of meaning/existential therapy and six 2.5 h sessions) suggested the intervention’s large effect was anticipated.76,77 Even omitting this study, the effect of interventions on SpWb is noteworthy given known ceiling effects with SpWb measures.8 Further, no trials screened participants on the basis of low baseline levels of SpWB or room for improvement.
We conducted moderator analyses to test whether intervention effects varied depending upon patient, clinical or intervention characteristics or trial design factors. Only SpWb outcome measure significantly moderated the effect of interventions. A majority of studies (73%) used the FACIT-Sp as an outcome, and these studies yielded larger effects compared to those that used other measures of SpWb. This may be due in part to the FACIT-Sp’s robust psychometric properties.78–80 Other moderators, though not statistically significant, were in the expected direction. Studies which specified SpWb as the primary outcome, used in-person interventions, and used group-based settings trended towards larger effect sizes. Meaning/existential interventions, followed by creative arts interventions and yoga/meditation, had the largest effect size of different intervention classes, whereas interventions that focused on health education and lifestyle changes (concerns that seem more remote from SpWb) had the smallest effects. Our finding that even interventions seemingly removed from spiritual well-being interventions had some impact may be explained by therapeutic gain occurring from common factors in interventions (e.g., positive regard, mastery, empathy and self-reflection) or development of skills that improve a variety of psychological outcomes (e.g., emotion regulation).81 It is also possible that improvements in physical health, in the case of health education or lifestyle interventions, allowed for more participation in activities that may promote spiritual well-being such as leisure or social engagement.82,83 Such potential mediators should be evaluated in trials.
Although in the expected direction, moderators warrant further research. The effect of delivery mode, in particular, merits additional research given the growth of remote (e.g., telehealth) and technology-based interventions (e.g., applications). Future research should also evaluate the effect of interventionist type (e.g., nurse, counsellor). Roughly, 20% of studies did not report the interventionist type; however, a similar proportion utilized a Master’s level mental health provider, a psychologist, or a psychiatrist. To guide adoption into clinical practice and inform the scalability of an intervention, future trials need to provide detail on interventionist background and training.
4.1 |. Clinical implications
This study has several implications for clinical practice. First, SpWb may be improved through a variety of interventions. Although meaning/existential interventions exerted the largest effects, SpWb also improved through other psychosocial interventions. Thus, for survivors who do not have access to meaning/existential interventions (which have largely been delivered in-person via a mental health provider), other interventions (e.g., creative arts and yoga) may yield some benefit. These interventions may be more widely available as part of psycho-oncology services in cancer care. Second, clinicians might consider administering the FACIT-Sp to monitor treatment progress when targeting SpWb. The FACIT-Sp was the most commonly used measure of SpWb in reviewed trials and has been rigorously tested. However, the FACIT-Sp may be susceptible to ceiling effects, and is also confounded with emotional well-being. As such, additional measures (e.g., spiritual distress) may be needed to evaluate treatment progress. Similarly, as the FACIT-Sp is not routinely administered in cancer care, practices that wish to identify survivors who may benefit from a SpWb intervention may consider focussing on survivors who screen positive for spiritual distress.84,85 Spiritual distress is a closely related, albeit distinct, construct from SpWb that when present, is a significant indicator of poor psychosocial health outcomes.86,87 As such, identifying and intervening with patients experiencing spiritual distress, rather than low spiritual well-being, may be the most efficient and targeted way to identify patients in need of intervention.
4.2 |. Study limitations
This study is limited by heterogeneity in effects observed and small sample size within moderator strata. Study strengths include use of standard guidelines (PRISMA statement), search of six databases, and expertise of PhD reviewers, a medical librarian and statistician. Other limitations pertained to the studies themselves and included: failure to specify the primary study endpoint; underrepresentation of racial and ethnic minorities, men, and non-breast cancer survivors; and insufficient detail on the interventionist. There are also limitations related to conceptual distinction of SpWb from closely related constructs.15 Although SpWb may include selected features of other constructs (e.g., an attained sense of meaning in life, perceptions of comfort from religious or spiritual commitments, and so on), each carries separate meanings and represents a distinct, vibrant field of scholarship. Investigators should be clear about what outcomes they are targeting (e.g., meaning, peace, comfort and spiritual struggle) and how they are assessing them. Specifying the outcome and its relation to the theoretical underpinnings of the intervention designed to address it will help advance the science of spirituality in illness and hopefully inform more tailored interventions.
5 |. CONCLUSION
In summary, overall our results suggest SpWb can be increased through psychosocial intervention. As clinical practice incorporates measures of spiritual needs into cancer care, there may be opportunity to implement interventions to address SpWb. Beyond greater transparency of trial design (e.g., outcome specification, interventionist type and training), future trials should improve representation of understudied cancer populations, evaluate whether SpWb interventions need to be tailored to clinical characteristics (e.g., disease stage and phase of cancer care), differentiate SpWb from related constructs, and test equivalency of delivery strategies. Addressing these limitations will improve understanding of the efficacy and potential reach of interventions for SpWb.
Supplementary Material
ACKNOWLEDGMENTS
We thank Mark Berendson, for his contribution designing search strategies for the larger meta-analysis comprising this study R03CA184560 (PI: Salsman), and Craig Esposito, for his assistance in abstract reviews. Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under award number R03CA184560 (PI: Salsman). Dr. McLouth was supported by R25CA122061 (PI: Avis) and the University of Kentucky Markey Cancer Center (P30 CA177558).
Footnotes
DATA AVAILABILITY STATEMENT
The raw data (including effect size estimates, variance estimates and moderator variables) and code for replicating all reported analyses are available in the supplementary materials accompanying this article.
REFERENCES
- 1.Stefanek M, McDonald PG, Hess SA. Religion, spirituality and cancer: current status and methodological challenges. Psycho Oncol. 2005;14(6):450–463. [DOI] [PubMed] [Google Scholar]
- 2.Asgeirsdottir GH, Sigurbjornsson E, Traustadottir R, Sigurdardottir V, Gunnarsdottir S, Kelly E. To cherish each day as it comes: a qualitative study of spirituality among persons receiving palliative care. Support Care Canc. 2013;21(5):1445–1451. [DOI] [PubMed] [Google Scholar]
- 3.Puchalski CM. Spirituality in the cancer trajectory. Ann Oncol. 2012;23:49–55. [DOI] [PubMed] [Google Scholar]
- 4.Yeary KHK, Alcaraz KI, Ashing KT, et al. Considering religion and spirituality in precision medicine. Transl Behav Med. 2020;10(1):195–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chandra A, Shafrin J, Dhawan R. Utility of cancer value frameworks for patients, payers, and physicians. J Am Med Assoc. 2016;315(19):2069–2070. [DOI] [PubMed] [Google Scholar]
- 6.Moberg DO. Assessing and measuring spirituality: confronting dilemmas of universal and particular evaluative criteria. J Adult Dev. 2002;9(1):47–60. [Google Scholar]
- 7.Zinnbauer BJ, Pargament KI, Cole B, et al. Religion and spirituality: unfuzzying the fuzzy. J Sci Stud Relig. 1997;36(4):549–564. [Google Scholar]
- 8.Bredle JM, Salsman JM, Debb SM, Arnold BJ, Cella D. Spiritual well-being as a component of health-related quality of life: the functional assessment of chronic illness therapy—spiritual well-being scale (FACIT-Sp). Religions. 2011;2(1):77–94. [Google Scholar]
- 9.Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy--Spiritual Well-being Scale (FACIT-Sp). Ann Behav Med. 2002;24(1):49–58. [DOI] [PubMed] [Google Scholar]
- 10.Salsman JM, Pustejovsky JE, Jim HS, et al. A meta-analytic approach to examining the correlation between religion/spirituality and mental health in cancer. Cancer. 2015;121(21):3769–3778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McClain CS, Rosenfeld B, Breitbart W. Effect of spiritual well-being on end-of-life despair in terminally-ill cancer patients. Lancet. 2003;361(9369):1603–1607. [DOI] [PubMed] [Google Scholar]
- 12.Xing L, Guo X, Bai L, Qian J, Chen J. Are spiritual interventions beneficial to patients with cancer?: a meta-analysis of randomized controlled trials following PRISMA. Med Baltim. 2018;97(35):e11948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zimmermann T, Heinrichs N, Baucom DH. Does one size fit all? Moderators in psychosocial interventions for breast cancer patients: a meta-analysis. Ann Behav Med. 2007;34(3):225–239. [DOI] [PubMed] [Google Scholar]
- 14.Moyer A, Knapp-Oliver SK, Sohl SJ, Schnieder S, Floyd AH. Lessons to be learned from 25 years of research investigating psychosocial interventions for cancer patients. Cancer J. 2009;15(5):345–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park CL, Pustejovsky JE, Trevino K, et al. Effects of psychosocial interventions on meaning and purpose in adults with cancer: a systematic review and meta-analysis. Cancer. 2019;125(14):2383–2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haynes RB, McKibbon KA, Wilczynski NL, Walter SD, Werre SR, Hedges T. Optimal search strategies for retrieving scientifically strong studies of treatment from Medline: analytical survey. BMJ. 2005;330(7501):1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Montori VM, Wilczynski NL, Morgan D, Haynes RB, Hedges T. Optimal search strategies for retrieving systematic reviews from Medline: analytical survey. BMJ. 2005;330(7482):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ellison CW. Spiritual well-being: conceptualization and measurement. J Psychol Theol. 1983;11(4):330–338. [Google Scholar]
- 19.Cotton S, Puchalski CM, Sherman SN, et al. Spirituality and religion in patients with HIV/AIDS. J Gen Intern Med. 2006;21:S5–S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferrell BR, Dow KH, Grant M. Measurement of the quality of life in cancer survivors. Qual Life Res. 1995;4(6):523–531. [DOI] [PubMed] [Google Scholar]
- 21.Bretscher M, Rummans T, Sloan J, et al. Quality of life in hospice patients. A pilot study. Psychosomatics. 1999;40(4):309–313. [DOI] [PubMed] [Google Scholar]
- 22.Ng SM, Yau JK, Chan CL, Chan CH, Ho DY. The measurement of body-mind-spirit well-being toward multidimensionality and transcultural applicability. Soc Work Health Care. 2005;41(1):33–52. [DOI] [PubMed] [Google Scholar]
- 23.Freedland KE, Mohr DC, Davidson KW, Schwartz JE. Usual and unusual care: existing practice control groups in randomized controlled trials of behavioral interventions. Psychosom Med. 2011;73(4):323–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mohr DC, Spring B, Freedland KE, et al. The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychother Psychosom. 2009;78(5):275–284. [DOI] [PubMed] [Google Scholar]
- 25.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salsman JM, Pustejovsky JE, Schueller SM, et al. Psychosocial interventions for cancer survivors: a meta-analysis of effects on positive affect. J Cancer Surviv. 2019;13(6):943–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hedges LV, Tipton E, Johnson MC. Robust variance estimation in meta-regression with dependent effect size estimates. Res Synth Methods. 2010;1(1):39–65. [DOI] [PubMed] [Google Scholar]
- 28.Tipton E Small sample adjustments for robust variance estimation with meta-regression. Psychol Methods. 2015;20(3):375–393. [DOI] [PubMed] [Google Scholar]
- 29.Tipton E, Pustejovsky JE. Small-sample adjustments for tests of moderators and model fit using robust variance estimation in meta-regression. J Educ Behav Stat. 2015;40(6):604–634. [Google Scholar]
- 30.Borenstein M, Higgins JP, Hedges LV, Rothstein HR. Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Res Synth Methods. 2017;8(1):5–18. [DOI] [PubMed] [Google Scholar]
- 31.Pustejovsky JE, Rodgers MA. Testing for funnel plot asymmetry of standardized mean differences. Res Synth Methods. 2019;10(1):57–71. [DOI] [PubMed] [Google Scholar]
- 32.Pustejovsky J clubSandwich: Cluster-robust (sandwich) variance estimators with small-sample corrections. Version 0.2.3. 2017. Available at: https://CRAN.R-project.org/package=clubSandwich.
- 33.Viechtbauer W Conducting meta-analyses in R with the metafor package. Journal of Statistical Software. 2010;36(3):1–48. [Google Scholar]
- 34.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. [DOI] [PubMed] [Google Scholar]
- 35.Badger T, Segrin C, Pasvogel A, Lopez AM. The effect of psychosocial interventions delivered by telephone and videophone on quality of life in early-stage breast cancer survivors and their supportive partners. J Telemed Telecare. 2013;19(5):260–265. [DOI] [PubMed] [Google Scholar]
- 36.Badger TA, Segrin C, Figueredo AJ, et al. Psychosocial interventions to improve quality of life in prostate cancer survivors and their intimate or family partners. Qual Life Res. 2011;20(6):833–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Breitbart W, Rosenfeld B, Pessin H, Applebaum A, Kulikowski J, Lichtenthal WG. Meaning-centered group psychotherapy: an effective intervention for improving psychological well-being in patients with advanced cancer. J Clin Oncol. 2015;33(7):749–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Breitbart W, Rosenfeld B, Gibson C, et al. Meaning-centered group psychotherapy for patients with advanced cancer: a pilot randomized controlled trial. Psycho Oncol. 2010;19(1):21–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Breitbart W, Poppito S, Rosenfeld B, et al. Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. J Clin Oncol. 2012;30(12):1304–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Breitbart W, Pessin H, Rosenfeld B, et al. Individual meaning-centered psychotherapy for the treatment of psychological and existential distress: a randomized controlled trial in patients with advanced cancer. Cancer. 2018;124(15):3231–3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carlson LE, Tamagawa R, Stephen J, Drysdale E, Zhong L, Speca M. Randomized-controlled trial of mindfulness-based cancer recovery versus supportive expressive group therapy among distressed breast cancer survivors (MINDSET): long-term follow-up results. Psycho Oncol. 2016;25(7):750–759. [DOI] [PubMed] [Google Scholar]
- 42.Cohen L, Chandwani K, Raghuram N, et al. Effect of yoga on QOL, cortisol rhythm, and HRV for women with breast cancer undergoing radiotherapy. J Clin Oncol. 2011;29(15 Suppl):9009. [Google Scholar]
- 43.Cook EL, Silverman MJ. Effects of music therapy on spirituality with patients on a medical oncology/hematology unit: a mixed-methods approach. Arts Psychother. 2013;40(2):239–244. [Google Scholar]
- 44.Cramer H, Pokhrel B, Fester C, et al. A randomized controlled bicenter trial of yoga for patients with colorectal cancer. Psycho Oncol. 2016;25(4):412–420. [DOI] [PubMed] [Google Scholar]
- 45.Djuric Z, Mirasolo J, Kimbrough L, et al. A pilot trial of spirituality counseling for weight loss maintenance in African American breast cancer survivors. J Natl Med Assoc. 2009;101(6):552–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fauver R The Healing Wisdom within: A Preliminary Experimental Trial of Psycho-Spiritual Integrative Therapy for People with Cancer. Palo Alto, CA: Institute of Transpersonal Psychology; 2011. [Google Scholar]
- 47.Ferguson RJ, McDonald BC, Rocque MA, et al. Development of CBT for chemotherapy-related cognitive change: results of a waitlist control trial. Psycho Oncol. 2012;21(2):176–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Freeman LW, White R, Ratcliff CG, et al. A randomized trial comparing live and telemedicine deliveries of an imagery-based behavioral intervention for breast cancer survivors: reducing symptoms and barriers to care. Psycho Oncol. 2015;24(8):910–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Guthrey CR. An Empirical Study of the Effect of Psycho-Spiritual Integrative Therapy on the Spirituality of Cancer Patients. Palo Alto, CA: Institute of Transpersonal Psychology; 2015. [Google Scholar]
- 50.Hanser SB, Bauer-Wu S, Kubicek L, et al. Effects of a music therapy intervention on quality of life and distress in women with metastatic breast cancer. J Soc Integr Oncol. 2006;4(3):116–124. [DOI] [PubMed] [Google Scholar]
- 51.Hawkes AL, Pakenham KI, Chambers SK, Patrao TA, Courneya KS. Effects of a multiple health behavior change intervention for colorectal cancer survivors on psychosocial outcomes and quality of life: a randomized controlled trial. Ann Behav Med. 2014;48(3):359–370. [DOI] [PubMed] [Google Scholar]
- 52.Heiney SP, McWayne J, Hurley TG, et al. Efficacy of therapeutic group by telephone for women with breast cancer. Canc Nurs 2003;26(6):439–447. [DOI] [PubMed] [Google Scholar]
- 53.Henderson VP, Clemow L, Massion AO, Hurley TG, Druker S, Hebert JR. The effects of mindfulness-based stress reduction on psychosocial outcomes and quality of life in early-stage breast cancer patients: a randomized trial. Breast Canc Res Treat. 2012;131(1):99–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hoogland AI, Lechner SC, Gonzalez BD, et al. Efficacy of a Spanish-language self-administered stress management training intervention for Latinas undergoing chemotherapy. Psycho Oncol. 2018;27(4):1305–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jafari N, Farajzadegan Z, Zamani A, et al. Spiritual therapy to improve the spiritual well-being of Iranian women with breast cancer: a randomized controlled trial. Evid Base Compl Alternative Med. 2013;2013:353262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Juarez G, Hurria A, Uman G, Ferrell B. Impact of a bilingual education intervention on the quality of life of Latina breast cancer survivors. Oncol Nurs Forum. 2013;40(1):E50–E60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kristeller JL, Rhodes M, Cripe LD, Sheets V. Oncologist Assisted Spiritual Intervention Study (OASIS): patient acceptability and initial evidence of effects. Int J Psychiatr Med. 2005;35(4):329–347. [DOI] [PubMed] [Google Scholar]
- 58.Leal B, Engebretson J, Cohen L, Chaoul MA, eds. Qualitative and quantitative analyses of the effects of Tibetan yoga (TY) on patients quality of life and experience of lymphoma. San Francisco, CA: Psychosomatic Medicine; 2014. [Google Scholar]
- 59.Liao J, Wu Y, Zhao Y, et al. Progressive muscle relaxation combined with Chinese medicine five-element music on depression for cancer patients: a randomized controlled trial. Chin J Integr Med. 2018;24(5):343–347. [DOI] [PubMed] [Google Scholar]
- 60.Liu CJ, Hsiung PC, Chang KJ, et al. A study on the efficacy of body-mind-spirit group therapy for patients with breast cancer. J Clin Nurs. 2008;17(19):2539–2549. [DOI] [PubMed] [Google Scholar]
- 61.Lo C, Hales S, Nissim R, Rodin G, eds. Preliminary evidence of the effectiveness of CALM to alleviate distress in advanced cancer. Psychooncology; 2014. [Google Scholar]
- 62.Loerzel VW, McNees P, Powel LL, Su X, Meneses K. Quality of life in older women with early-stage breast cancer in the first year of survivorship. Oncol Nurs Forum. 2008;35(6):924–932. [DOI] [PubMed] [Google Scholar]
- 63.Meneses KD, McNees P, Loerzel VW, Su X, Zhang Y, Hassey LA. Transition from treatment to survivorship: effects of a psychoeducational intervention on quality of life in breast cancer survivors. Oncol Nurs Forum. 2007;34(5):1007–1016. [DOI] [PubMed] [Google Scholar]
- 64.Milbury K, Chaoul A, Biegler K, et al. Tibetan sound meditation for cognitive dysfunction: results of a randomized controlled pilot trial. Psycho Oncol. 2013;22(10):2354–2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Moadel AB, Shah C, Wylie-Rosett J, et al. Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: effects on quality of life. J Clin Oncol. 2007;25(28):4387–4395. [DOI] [PubMed] [Google Scholar]
- 66.Nidich SI, Fields JZ, Rainforth MV, et al. A randomized controlled trial of the effects of transcendental meditation on quality of life in older breast cancer patients. Integr Canc Ther. 2009;8(3):228–234. [DOI] [PubMed] [Google Scholar]
- 67.Olesen ML, Duun-Henriksen AK, Hansson H, Ottesen B, Andersen KK, Zoffmann V. A person-centered intervention targeting the psychosocial needs of gynecological cancer survivors: a randomized clinical trial. J Cancer Surviv. 2016;10(5):832–841. [DOI] [PubMed] [Google Scholar]
- 68.Piderman KM, Johnson ME, Frost MH, et al. Spiritual quality of life in advanced cancer patients receiving radiation therapy. Psycho Oncol. 2014;23(2):216–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Puig A, Lee SM, Goodwin L, Sherrard PAD. The efficacy of creative arts therapies to enhance emotional expression, spirituality, and psychological well-being of newly diagnosed Stage I and Stage II breast cancer patients: a preliminary study. Arts Psychother. 2006;33(3):218–228. [Google Scholar]
- 70.Radl DM. The Effects of Self-Book© Art Therapy on Emotional Distress in Female Cancer Patients: A Randomized Controlled Trial [Doctoral]. Philadelphia, PA: Drexel University; 2015. [Google Scholar]
- 71.Radl D, Vita M, Gerber N, Gracely EJ, Bradt J. The effects of Self-Book© art therapy on cancer-related distress in female cancer patients during active treatment: a randomized controlled trial. Psycho Oncol. 2018;27(9):2087–2095. [DOI] [PubMed] [Google Scholar]
- 72.Rodin G, Lo C, Rydall A, et al. Managing cancer and living meaningfully (CALM): a randomized controlled trial of a psychological intervention for patients with advanced cancer. J Clin Oncol. 2018;36(23):2422–2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Roth A A telephone psychotherapy to help achieve wisdom in older cancer patients: the care project. Psycho Oncol. 2017;26(S1):7. [Google Scholar]
- 74.Rummans TA, Clark MM, Sloan JA, et al. Impacting quality of life for patients with advanced cancer with a structured multidisciplinary intervention: a randomized controlled trial. J Clin Oncol. 2006;24(4):635–642. [DOI] [PubMed] [Google Scholar]
- 75.Zernicke KA, Campbell TS, Speca M, McCabe-Ruff K, Flowers S, Carlson LE. A randomized wait-list controlled trial of feasibility and efficacy of an online mindfulness-based cancer recovery program: the eTherapy for cancer applying mindfulness trial. Psychosom Med. 2014;76(4):257–267. [DOI] [PubMed] [Google Scholar]
- 76.Schnabel L More religious, less dogmatic: toward a general framework for gender differences in religion. Soc Sci Res. 2018;75:58–72. [DOI] [PubMed] [Google Scholar]
- 77.Ford CG, Vowles KE, Smith BW, Kinney AY. Mindfulness and meditative movement interventions for men living with cancer: a meta-analysis. Ann Behav Med. 2019;54(5):360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Brintz CE, Birnbaum-Weitzman O, Merz EL, et al. Validation of the functional assessment of chronic illness therapy-spiritual well-being-expanded (FACIT-Sp-Ex) across English and Spanish-speaking Hispanics/Latinos: results from the Hispanic community health study/study of Latinos sociocultural ancillary study. Psycholog Relig Spiritual. 2017;9(4):337–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lazenby M, Khatib J, Al-Khair F, Neamat M. Psychometric properties of the functional assessment of chronic illness therapy–spiritual well-being (FACIT-Sp) in an Arabic-speaking, predominantly muslim population. Psycho Oncol. 2013;22(1):220–227. [DOI] [PubMed] [Google Scholar]
- 80.Peterman AH, Reeve CL, Winford EC, et al. Measuring meaning and peace with the FACIT–spiritual well-being scale: distinction without a difference? Psychol Assess. 2014;26(1):127–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Park CL, Lee SY, Finkelstein-Fox L, Sanderson K. Yoga to promote physical, mental and spiritual well-being: self-regulation on and off the mat. In: Plante TG, ed. Healing with Spiritual Practices: Proven Techniques for Disorders from Addictions and Anxiety to Cancer and Chronic Pain. Santa Barbara, CA: Praeger; 2018:72–85. [Google Scholar]
- 82.Goyal NG, Ip EH, Salsman JM, Avis NE. Spirituality and physical health status: a longitudinal examination of reciprocal effects in breast cancer survivors. Support Care Cancer. 2019;27(6):2229–2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Leisure Heintzman P. and spiritual well-being relationships: a qualitative study. Loisir Société/Soc Leis. 2000;23(1):41–69. [Google Scholar]
- 84.Bahraini S, Gifford W, Graham ID, et al. The accuracy of measures in screening adults for spiritual suffering in health care settings: a systematic review. Palliat Support Care. 2020;18(1):89–102. [DOI] [PubMed] [Google Scholar]
- 85.King SD, Fitchett G, Murphy PE, Pargament KI, Harrison DA, Loggers ET. Determining best methods to screen for religious/spiritual distress. Support Care Canc. 2017;25(2):471–479. [DOI] [PubMed] [Google Scholar]
- 86.Sherman AC, Simonton S, Latif U, Spohn R, Tricot G. Religious struggle and religious comfort in response to illness: health outcomes among stem cell transplant patients. J Behav Med. 2005;28(4):359–367. [DOI] [PubMed] [Google Scholar]
- 87.Fitchett G, Murphy PE, Kim J, Gibbons JL, Cameron JR, Davis JA. Religious struggle: prevalence, correlates and mental health risks in diabetic, congestive heart failure, and oncology patients. Int J Psychiatr Med. 2004;34(2):179–196. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


