Abstract
Background:
The oesophageal hiatus is a long and oblique opening in the diaphragm where the thoracic section of the oesophagus passes into the abdomen. Enlarged hiatal surface and insufficiency are considered to be associated with gastroesophageal reflux disease (GERD) and hiatal hernia (HH). In this study, we aimed to retrospectively evaluate the relationship and the presence of GERD with HH by performing hiatal surface area (HSA) and other hiatal measurements at the thorax and abdominal computed tomography (CT) images in cases without any intra-abdominal or oesophageal surgery history.
Patients and Methods:
A total of 192 patients of GERD+ and 173 cases with GERD− as a control group were included in the study. In CT examinations of 365 patients included in the study, measurements and comments were made by an experienced radiologist in abdominal radiology. In CT scans, the following were evaluated for each case; HSA, hiatus anterior–posterior (A-P) diameter, hiatus transverse diameter, and HH types. The HSA measurement was made with the freehand region of interest in the picture archiving and communication system.
Results:
A total of 365 cases were included in this study; there was a significant difference between the median HSA, A-P diameter, and transverse diameter measurements between GERD− and GERD+ groups (P < 0.001). A statistically significant difference was found between the presence of GERD and HH types (P < 0.001).
Conclusions:
CT imaging helps investigate the presence of HH at GERD+ patients. In addition, pre-operative valuable data can be obtained from the detection of HH types and HSA measurements in cases with HH.
Keywords: Computed tomography, gastroesophageal reflux disease, hiatal hernia, hiatal surface area, oesophageal hiatus
INTRODUCTION
The oesophageal hiatus is a long and oblique opening in the diaphragm where the thoracic section of the oesophagus passes into the abdomen. The edges of the hiatus are adjacent to the diaphragmatic crura and may show some variations between individuals.[1,2] Besides, the oesophageal hiatus has a sphincter mechanism independent of the lower oesophageal sphincter.[3] Enlarged hiatal surface area (HSA) and insufficiency are considered associated with gastroesophageal reflux disease (GERD) and hiatal hernia (HH).[4,5] Further, in most patients with HHs, GERD is detected compared to patients without hernia.[4,6] In symptomatic GERD cases referred to laparoscopic anti-reflux surgery, pre-operative measurement of oesophageal hiatus defect and HSA has been recommended to prevent HH recurrence and intra-thoracic wrap migration.[7,8]
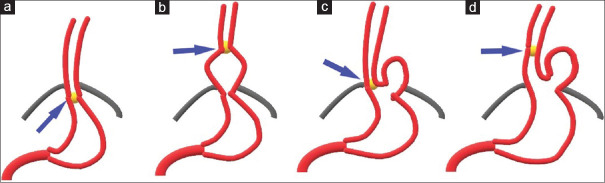
When the stomach extends partially or totally to the thorax regardless of swallowing, this finding is called a common medical condition, the HH. HH is classified into three types: type 1 sliding, type 2 para-oesophageal and type 3 mixed.[9,10,11] Type 1 sliding HH is defined when the stomach and oesophagogastric junction (EGJ) are above the diaphragmatic hiatus and EGJ is above the gastric fundus. Type 2 para-oesophageal HH is defined when EGJ is at the diaphragmatic hiatus level and the part of the stomach by more than 2 cm is above the diaphragm next to the oesophagus. Type 3 mixed HH can be roughly considered the total of sliding and para-oesophageal hernia [Figure 1].
Figure 1.
In the picture representing hiatal hernia types, blue arrows indicate the oesophagogastric junction; (a) normal oesophagus and stomach, (b) type 1 sliding hiatal hernia, (c) type 2 para-oesophageal hiatal hernia, (d) type 3 mixed hiatal hernia
Hiatal defect size and volumetric measurements in pre-operative computed tomography (CT) are helpful and determinative at the operative technique concerning the need for a relaxing incision on the diaphragm or rescue gastropexy. Therefore, knowing this information preoperatively helps decide and determine surgical complexity and operative approach.[12] Until a few years ago, data published in the literature on HSA mostly used calculations based on gross measurements obtained during surgery or cadaver.[11,13,14] In one study, assuming that the hiatus was shaped like a circle slice, it indirectly determined HSA by using linear measurements during surgery.[15]
In this study, we aimed to retrospectively evaluate the relationship and presence of GERD with HH by performing HSA and other hiatal measurements at the thorax and abdominal CT images in cases without any intra-abdominal and oesophageal surgery history.
PATIENTS AND METHODS
Patient selection
This retrospective study was evaluated and approved by the local ethics committee. Between September 2018 and February 2020, all thorax and abdominal computed tomography scans performed at the department of radiology were retrospectively analysed. Abdominal and/or oesophageal surgical history, cirrhosis and portal hypertension, known congenital anomaly-genetic disease, mediastinal fibrosis, body mass index (BMI) ≥35 and age younger than 18 were the exclusion criteria. Finally, 192 cases of GERD+ and 173 cases with GERD− as a control group were included in the study. GERD+ patients included in the study had clinical diagnoses and upper gastrointestinal endoscopy results, and medication treatments were available. In the CT images of 365 patients included, measurements were made by an experienced radiologist in abdominal radiology.
Computed tomography protocol and measurements
Images of all cases were obtained using 40 slices CT scanner (Siemens, SOMATOM Sensation 40). CT parameters of the thorax and abdominal tomography scanning included 0.4 s portal rotation time, 120 kVp, 200 mA, 1.25 mm section thickness and 512 × 512 matrix size. All CT images were reconfigured using the “picture archiving and communication system” (PACS) INFINITT: 3.0.11.4 (BN11) program and analysed. Analysis and measurements for each case were performed in axial, sagittal and coronal planes, respectively. Besides, additional data were obtained by providing three-dimensional post-processing, including maximum density projections and multi-plane image reformatting in all cases.
In CT scans, the following were evaluated for each case; HSA, hiatus anterior–posterior (A-P) diameter, hiatus transverse diameter, and HH types [Figure 2]. The HSA measurement was made with the freehand region of interest in PACS, as it provides convenience and gives more accurate results.
Figure 2.
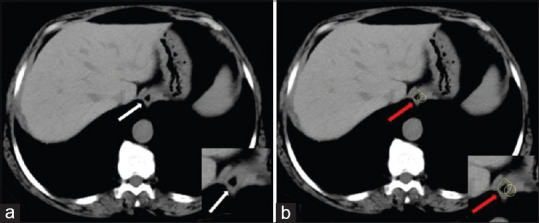
On the axial computed tomographic section view of the case without hiatal hernia; (a) the white arrows show the hiatus oesophagus and (b) the red arrows show the HSA measurement made at this level using the freehand region of interest method
Statistical analysis
Statistical analysis was performed using SPSS software (IBM SPSS version 22.0, IBM, Armonk, NY, USA). Descriptive statistical methods (median, frequency, percentage, minimum and maximum) were used to define the study data. Kolmogorov–Smirnov test assessed the normality of quantitative data distribution. Pearson’s Chi-square test was used to compare categorical variables, and Fisher’s exact test was applied if the number of subgroups was low. Spearman’s correlation analysis was used to evaluate the relationship between the parameters. Kruskal–Wallis test was applied to compare HSA and other diameter CT scan measurements between different groups (GERD+, GERD − and HH types). According to the results of the analysis, a P < 0.05 was considered statistically significant.
RESULTS
Of the 365 cases involved in this study, 179 were male and 186 were female. The youngest case was 18 years old and the oldest case was 94 years old, both males. In females, the youngest case was 19 years old and the oldest case was 89 years old. The mean age in all cases was 50.88 ± 17.11, 50.43 ± 17.32 for males and 51.32 ± 16.95 for females.
In addition to gender, there was no statistically significant difference between GERD− and GERD+ groups and BMI measurements (P = 0.68, P = 0.76). Hiatus measurements were compared in both groups; median HSA was measured as 4.89 cm2 in GERD− group and 19.11 cm2 in GERD+ group. In GERD − cases, the median A-P diameter was measured as 7.07 mm and the median transverse diameter was 7.58 mm. In GERD+ patients, it was measured as 15.48 mm and 16.55 mm, respectively. There was a significant difference between the median HSA, A-P diameter and transverse diameter measurements between the two groups (P < 0.001). Demographic data and CT measurements associated with GERD are summarized in Table 1.
Table 1.
Demographics, measurements of mean hiatal surface area and other diameters
| n | Mean age | Mean BMI±SD | Median HSA (cm2) | Median A-P diameter (mm) | Median transverse diameter (mm) | |
|---|---|---|---|---|---|---|
| GERD− | 173 | 43.85±14.88 | 28.1±5.1 | 4.89 (2.45-12.80) | 7.07 (4.48-13.06) | 7.58 (5.29-14.19) |
| GERD+ | 192 | 57.22±16.54 | 26.2±4.8 | 19.11 (2.92-87.76) | 15.48 (4.8437.18) | 16.55 (5.26-42.52) |
BMI: Body mass index, SD: Standard deviation, HSA: Hiatal surface area, GERD: Gastroesophageal reflux disease, A-P: Anterior-posterior
When the relationship between gender and GERD and between gender and HH types was evaluated using the Chi-square test, no statistically significant difference was found (P = 0.65, P = 0.99). The distribution and frequency of HH types by gender are shown in Table 2.
Table 2.
Distribution of hiatal hernia types by gender
| HH types | Total | ||||
|---|---|---|---|---|---|
|
| |||||
| None | Type 1 | Type 2 | Type 3 | ||
| Gender | |||||
| Male | |||||
| n | 88 | 59 | 21 | 11 | 179 |
| Percentage HH | 48.6 | 49.6 | 48.8 | 50.0 | 49.0 |
| Female | |||||
| n | 93 | 60 | 22 | 11 | 186 |
| Percentage HH | 51.4 | 50.4 | 51.2 | 50.0 | 51.0 |
| Total | |||||
| n | 181 | 119 | 43 | 22 | 365 |
| Percentage HH | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
HH: Hiatal hernia
The distribution of age, HSA and diameter measurements by gender were evaluated, respectively [Table 3]. There was no statistically significant difference between gender and age, HSA, A-P diameter and transverse diameter measurements (P > 0.05).
Table 3.
Distribution of age, hiatal surface area and diameter measurements by gender
| n | Minimum age | Maximum age | Mean±SD | |
|---|---|---|---|---|
| Male | ||||
| Age | 179 | 18 | 94 | 50.43±17.326 |
| HSA (cm2) | 179 | 2.45 | 84.54 | 12.7269±12.77487 |
| A-P (mm) | 179 | 4.48 | 37.18 | 11.5668±6.03150 |
| Transverse (mm) | 179 | 5.26 | 42.52 | 12.4156±6.81297 |
| Female | ||||
| Age | 186 | 18 | 89 | 51.32±16.952 |
| HSA (cm2) | 186 | 2.52 | 87.76 | 12.0263±12.24114 |
| A-P (mm) | 186 | 5.01 | 36.52 | 11.4291±6.34350 |
| Transverse (mm) | 186 | 5.34 | 37.81 | 12.1834±6.64914 |
SD: Standard deviation, HSA: Hiatal surface area, A-P: Anterior-posterior
According to the Spearman’s correlation, there was a moderate positive correlation between age and HH types, HSA, A-P diameter and transverse diameter (ρ: 0.391–0.430). Thirteen of the GERD− cases had type 1 HH, whereas type 2 and type 3 HH were not. In GERD+ patients, 106 type 1 HH, 43 type 2 HH and 22 type 3 HH were present. A statistically significant difference was found between the presence of GERD and HH types (P < 0.001). The relationship between GERD− and GERD+ groups and HH types and the distribution of cases are shown in Table 4.
Table 4.
Relationship between gastroesophageal reflux disease and hiatal hernia types
| HH types | Total | ||||
|---|---|---|---|---|---|
|
| |||||
| None | Type 1 | Type 2 | Type 3 | ||
| GERD | |||||
| − | |||||
| n | 160 | 13 | 0 | 0 | 173 |
| Percentage HH | 88.4 | 10.9 | 0.0 | 0.0 | 47.4 |
| + | |||||
| n | 21 | 106 | 43 | 22 | 192 |
| Percentage HH | 11.6 | 89.1 | 100.0 | 100.0 | 52.6 |
| Total | |||||
| n | 181 | 119 | 43 | 22 | 365 |
| Percentage HH | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
HH: Hiatal hernia, GERD: Gastroesophageal reflux disease
DISCUSSION
The oesophageal hiatus is an opening limited by the tissue that is continuous with the diaphragmatic crura in the diaphragm. The pathological expansion of the hiatus has clinical consequences. The size of the hiatus affects the surgeon’s choice of the hernia repair method, predicting the long-term success rate.[8,16] In addition, some studies have shown that there may be a significant relationship between low hiatus area, decreased the lower esophageal sphincter pressure and increased acid reflux in patients with GERD.[7,14]
Koch et al. showed that the hiatal area size was negatively correlated with low oesophageal sphincter (LES) pressure and positively correlated with acid reflux as observed by pH monitoring.[8] Similarly, Batirel et al. showed a negative correlation of the size of the hiatal area obtained from surgical measurements and the LES pressure, as well as a positive correlation between acid reflux and HSA obtained by pH monitoring.[7] A previous similar study also showed that GERD is associated with larger HH sizes measured by high-resolution manometry and pH monitoring.[17]
Granderath et al. described a method for the quantitative estimation of HSA using surgical measurements and suggested that the type of surgical repair is based on the size of the hiatal defect. Patients with HSA ≤4 cm2 were operated with sutures only, and patients with HSA >8 cm2 mesh were placed.[15] Similarly, another study has shown a relationship between the benefits of HSA-based surgical technique selection and the long-term success rate of repair surgery with the size of the hiatus.[16] Shamiyeh et al. found mean HSA by working with cadavers. Considering post-mortem changes, a formula was used to calculate HSA.[13]
HH can be easily identified on a CT scan as a soft tissue structure that extends in front of and to the right or opposite of the aorta.[18] Ouyang et al. reported that subjects with larger HSA and mixed-type hernias in GERD+ cases had larger hiatus than subjects without a hernia. However, in patients with GERD+ without hernia, it was not detected a significantly larger hiatus oesophagus than the control group.[4] Moten et al. compared preoperative CT images with intraoperative measured HSA values in patients undergoing laparoscopic HH repair and found that the calculated HSA value on CT was more accurate.[19] Kumar et al. evaluated the HH morphology by CT and found a significant increase in HSA in patients with different HH types compared to the control group.[20] Boru et al. compared the preoperative CT and intraoperative HSA measurements in obese patients with ‘bariatric surgery + posterior cruroplasty history’ and showed that CT gave more accurate results. The difficulty of evaluation of intra-operative hiatus oesophagus and insufficient measurement technique made HSA measurement difficult. In the same study, a significant decrease in HSA dimensions was observed in 1st -year control the thorax and abdominal CT.[21]
We used PACS software in this study since it is accessible, easy to use and measurements can be made in a short time. Furthermore, unlike some studies, we evaluated the non-obese group that was previously evaluated in a few publications.[4,19,20] This study has one of the largest case numbers in the literature.[4,20,21] Besides, our study has the second largest number of cases in the literature regarding the evaluation of hiatus oesophagus measurements with CT imaging.[4] We determined the relationship between GERD and HH with more data by measuring other diameters besides HSA. Finally, we compared the relationship between gender and GERD and HH types, respectively.
Limitations of our study include the lack of special algorithms and CT evaluation and measurements by a radiologist. Second limitation is the lack of pH monitoring measurements in GERD+ cases. Furthermore, taking measurements without using a workstation can be considered another limitation. We think that with the new studies, this problem can be overcome and the measurements can be standardised with PACS software.
CONCLUSIONS
CT imaging helps investigate the presence of HH in GERD+ patients. In addition, preoperative valuable data can be obtained from the detection of HH types and HSA measurements in cases with HH.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Collis JL, Kelly TD, Wiley AM. Anatomy of the crura of the diaphragm and the surgery of hiatus hernia. Thorax. 1954;9:175–89. doi: 10.1136/thx.9.3.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costa MM, Pires-Neto MA. Anatomical investigation of the esophageal and aortic hiatuses: Physiologic, clinical and surgical considerations. Anat Sci Int. 2004;79:21–31. doi: 10.1111/j.1447-073x.2004.00060.x. [DOI] [PubMed] [Google Scholar]
- 3.Mittal RK, Rochester DF, McCallum RW. Sphincteric action of the diaphragm during a relaxed lower esophageal sphincter in humans. Am J Physiol. 1989;256:G139–44. doi: 10.1152/ajpgi.1989.256.1.G139. [DOI] [PubMed] [Google Scholar]
- 4.Ouyang W, Dass C, Zhao H, Kim C, Criner G COPDGene Investigators. Multiplanar MDCT measurement of esophageal hiatus surface area: Association with hiatal hernia and GERD. Surg Endosc. 2016;30:2465–72. doi: 10.1007/s00464-015-4499-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gryglewski A, Pena IZ, Tomaszewski KA, Walocha JA. Unsolved questions regarding the role of esophageal hiatus anatomy in the development of esophageal hiatal hernias. Adv Clin Exp Med. 2014;23:639–44. doi: 10.17219/acem/37247. [DOI] [PubMed] [Google Scholar]
- 6.Wright RA, Hurwitz AL. Relationship of hiatal hernia to endoscopically proved reflux esophagitis. Dig Dis Sci. 1979;24:311–3. doi: 10.1007/BF01296546. [DOI] [PubMed] [Google Scholar]
- 7.Batirel HF, Uygur-Bayramicli O, Giral A, Ekici B, Bekiroglu N, Yildizeli B, et al. The size of the esophageal hiatus in gastroesophageal reflux pathophysiology: Outcome of intraoperative measurements. J Gastrointest Surg. 2010;14:38–44. doi: 10.1007/s11605-009-1047-8. [DOI] [PubMed] [Google Scholar]
- 8.Koch OO, Asche KU, Berger J, Weber E, Granderath FA, Pointner R. Influence of the size of the hiatus on the rate of reherniation after laparoscopic fundoplication and refundopilication with mesh hiatoplasty. Surg Endosc. 2011;25:1024–30. doi: 10.1007/s00464-010-1308-3. [DOI] [PubMed] [Google Scholar]
- 9.Jones FA. Diagnosis of hiatus hernia. Proc R Soc Med. 1952;45:277–9. doi: 10.1177/003591575204500508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol. 2008;22:601–16. doi: 10.1016/j.bpg.2007.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gordon C, Kang JY, Neild PJ, Maxwell JD. The role of the hiatus hernia in gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2004;20:719–32. doi: 10.1111/j.1365-2036.2004.02149.x. [DOI] [PubMed] [Google Scholar]
- 12.Kao AM, Ross SW, Otero J, Maloney SR, Prasad T, Augenstein VA, et al. Use of computed tomography volumetric measurements to predict operative techniques in paraesophageal hernia repair. Surg Endosc. 2020;34:1785–94. doi: 10.1007/s00464-019-06930-8. [DOI] [PubMed] [Google Scholar]
- 13.Shamiyeh A, Szabo K, Granderath FA, Syré G, Wayand W, Zehetner J. The esophageal hiatus: What is the normal size? Surg Endosc. 2010;24:988–91. doi: 10.1007/s00464-009-0711-0. [DOI] [PubMed] [Google Scholar]
- 14.Koch OO, Kaindlstorfer A, Antoniou SA, Asche KU, Granderath FA, Pointner R. Influence of the esophageal hiatus size on the lower esophageal sphincter, on reflux activity and on symptomatology. Dis Esophagus. 2012;25:201–8. doi: 10.1111/j.1442-2050.2011.01238.x. [DOI] [PubMed] [Google Scholar]
- 15.Granderath FA, Schweiger UM, Pointner R. Laparoscopic antireflux surgery: Tailoring the hiatal closure to the size of hiatal surface area. Surg Endosc. 2007;21:542–8. doi: 10.1007/s00464-006-9041-7. [DOI] [PubMed] [Google Scholar]
- 16.Grubnik VV, Malynovskyy AV. Laparoscopic repair of hiatal hernias: New classification supported by long-term results. Surg Endosc. 2013;27:4337–46. doi: 10.1007/s00464-013-3069-2. [DOI] [PubMed] [Google Scholar]
- 17.Franzén T, Tibbling L. Is the severity of gastroesophageal reflux dependent on hiatus hernia size? World J Gastroenterol. 2014;20:1582–4. doi: 10.3748/wjg.v20.i6.1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lindell MM, Jr, Bernardino ME. Diagnosis of hiatus hernia by computed tomography. J Comput Tomogr. 1981;5:16–9. doi: 10.1016/0149-936x(81)90051-5. [DOI] [PubMed] [Google Scholar]
- 19.Moten AS, Ouyang W, Hava S, Zhao H, Caroline D, Abbas A, et al. In vivo measurement of esophageal hiatus surface area using MDCT: Description of the methodology and clinical validation. Abdom Radiol (NY) 2020;45:2656–62. doi: 10.1007/s00261-019-02279-7. [DOI] [PubMed] [Google Scholar]
- 20.Kumar D, Zifan A, Ghahremani G, Kunkel DC, Horgan S, Mittal RK. Morphology of the esophageal hiatus: Is it different in 3 types of hiatus hernias? J Neurogastroenterol Motil. 2020;26:51–60. doi: 10.5056/jnm18208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boru CE, Rengo M, Iossa A, De Angelis F, Massaro M, Spagnoli A, et al. Hiatal surface area’s CT scan measurement is useful in hiatal hernia’s treatment of bariatric patients. Minim Invasive Ther Allied Technol. 2021;30:86–93. doi: 10.1080/13645706.2019.1683033. [DOI] [PubMed] [Google Scholar]