Abstract
Type 2 diabetes is a chronic disease, requiring lifestyle management to prevent chronic complications. Increasing physical activity and reducing sedentary behavior is integral to maintaining glycemic control. The purpose of this study was to 1.) appraise and synthesize the literature about physical activity and sedentary behavior intervention delivery via telehealth strategies in adults with Type 2 Diabetes Mellitus and 2.) to evaluate what is known about the effectiveness of such interventions on physical activity, sedentary behavior, and glycemic control. An integrative literature review was carried out, including the electronic databases PubMed, CINAHL, and PsychInfo, searching for articles published within the past 10 years, meeting specified inclusion and exclusion criteria, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement guidelines. Seventeen studies were included. Significant improvements in physical activity and sedentary behavior were identified in web and mobile phone-based interventions. Modest improvements in glycemic control were reported. Theoretical framework use and integration was limited, and intervention length and follow-up varied greatly in the studies reviewed. Outcomes were measured using both self-report and objective measures, but objective measures were used less frequently. Further, few studies have been conducted in the United States or in rural populations. Web and mobile phone-based telehealth interventions to increase physical activity, reduce sedentary behaviors, and improve glycemic control have been supported by the literature. A need exists for future studies which are theory driven, include dose specific measures, self-report and objective measures, and long-term follow-up. Examining intervention effects in rural populations is needed.
Type 2 Diabetes Mellitus (T2DM) is a chronic disease process requiring lifestyle management to maintain normal glycemic levels, preventing and delaying the onset of chronic complications. In the United States (U.S.), 34.1 million adults, aged 18 or older, are living with known T2DM, with an estimated 7.3 million adults remaining undiagnosed (Centers for Disease Control and Prevention, 2020). Despite continued efforts in prevention, the prevalence of T2DM in U.S. adults is estimated to increase to 60.6 million by the year 2060 (Lin et al., 2018).
Physical activity (PA) is an integral lifestyle management component, which aids in maintaining glycemic control (GC) (American Diabetes Association [ADA], 2019b). The American Diabetes Association (2019b) recommends adults with T2DM participate in 150 minutes of moderate-to-vigorous PA weekly to reduce glycated hemoglobin (A1C) levels, triglycerides, blood pressure, and insulin resistance. Bouts of PA, specifically aerobic PAs, should last a minimum of 10 minutes, with the goal of reaching 30 minutes per day, most days of the week, not allowing for more than 2 days between activity sessions (ADA, 2016; ADA, 2019c).
Sedentary behavior (SB) is a separate, but equally important, component to maintain GC (ADA, 2016). Sedentary behaviors require low amounts of energy expenditure, which occur while lying or sitting (ADA, 2016). Reducing prolonged bouts of time spent sedentary every 20 – 30 minutes with light walking activity aids in improving GC (ADA, 2016). While there is strong evidence supporting the importance of increasing PA and decreasing SBs, many adults with T2DM continue to struggle to meet recommended guidelines (ADA, 2016; ADA, 2019c).
Telehealth is defined as the exchange of information using electronic communications to improve patient health and outcomes (Tuckson, Edmunds, & Hodgkins, 2017). The use of telehealth technology to improve monitoring, feedback, and high-quality healthcare access to patients is continuing to grow (Tuckson et al., 2017). Communication between patients and clinicians through videoconferencing, telephone calls, e-mail, remote wireless monitoring, and the internet can provide chronic disease management care (Tuckson et al., 2017). Wearable monitors, smartphones, mobile apps, videoconferencing, e-mail, and games can provide valuable health education and PA monitoring (Tuckson et al., 2017). Incorporating both internet and mobile technology-based interventions can reach a more diverse population than using an internet-based technology alone (ADA, 2019b).
Few systematic reviews have been conducted to explore the literature about PA and SB interventions delivered using a telehealth strategy to adults with T2DM. No identified reviews focused on SB interventions delivered using a telehealth strategy in this population exclusively. Two systematic reviews examined the use of telehealth strategies to promote PA in adults with T2DM, identifying the use of telehealth strategies to deliver PA interventions in adults with T2DM as effective (Connelly, Kirk, Masthoff, MacRury, 2013; Kongstad et al., 2019). Connelly et al. (2013) reviewed literature published between January 1991 and March 2013 and Kongstad et al. (2019) reviewed literature published prior to May 2017. Both systematic reviews provided evidence to support the need for tailored feedback delivered in a format the participant finds meaningful and the inclusion of self-monitoring features, such as a logbook (Connelly et al., 2013; Kongstad et al., 2019). While both systematic reviews identified a relationship between studies with a strong methodology (i.e., full theoretical integration, intervention descriptions, use of objective and subjective outcome measures) and clinically important outcomes, there has been little description of how interventions were developed, including the content included, full theoretical concept integration in the intervention or outcome measures, and the use of both objective and subjective outcome measures by the studies reviewed (Connelly et al., 2013; Kongstad et al., 2019). To provide additional insight into the current state of the literature the purpose of this integrative review was to 1.) appraise and synthesize the literature about PA and SB intervention delivery via telehealth strategies in adults with T2DM and 2.) evaluate what is known about the effectiveness of such interventions on PA adherence, SB reduction, and GC.
Methods
Search Methods
To be included in this literature review, a health behavior intervention designed to increase PA, and/or reduce SBs must have been delivered using a telehealth strategy to community-dwelling adults with T2DM with the aim of improving GC. “Telehealth” is defined as the use of technology to communicate an intervention using the internet through websites and mobile device technologies. “Physical activity” is defined as activities produced through skeletal muscle contraction which result in energy expenditure above a basal level, measured as levels of PA, time spent physically active, or steps taken (U.S. Department of Health and Human Services, 2018). “Sedentary behaviors” are defined as activities which require low amounts of energy expenditure, which occur while sitting, reclining or lying measured as time spent sedentary, the number of sedentary bouts, breaks in sedentary time, and as time spent is specific sedentary activities (U.S. Department of Health and Human Services, 2018). “Glycemic control” is defined as an A1C <7% and/or pre-prandial blood glucose levels of 80 – 130 mg/dL (ADA, 2019a).
The literature search of databases was conducted in October 2019. The following databases were included in the search: PubMed, CINAHL, and PsychInfo. Ancestry searches of eligible publication reference lists were performed to identify additional relevant publications not identified through the original database search. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines were followed (Moher, Liberati, Tetzlaff, Altman & The PRISMA Group, 2009).
The search strategy was limited to include articles published within the past 10 years, English language only, and full text available. The key terms “diabetes”, “intervention” and “internet or website or web-based or mobile or phone” were entered into the database search box with the term “physical activity or exercise”. Then the three key terms were reentered with the following search term, “sedentary or sitting time”. Articles were initially screened by reading the title, then the abstracts of relevant publications were read to determine eligibility. If eligibility could not be determined by reading the abstract, the full text was reviewed.
To determine study eligibility, the following specific inclusion and exclusion criteria were applied to make final publication selections. Specific inclusion criteria include: (a) community-dwelling adults (age ≥ 18 years); (b) access to full report; (c) participants diagnosed with T2DM; (d) PA and/or SB intervention delivered via telehealth strategy; (e) outcome measures for PA (levels of PA, time spent active, and steps taken) and/or SB (time spent sedentary, the number of sedentary bouts, breaks in sedentary time, and as time spent in specific sedentary activities); (f) available in English language; (g) published after January 1, 2009. Study exclusion criteria include: (a) non-community dwelling participants; (b) under the age of 18 (age ≤ 17 years); (c) diabetes diagnosis other than T2DM; (d) interventions focused on diabetes self-management behaviors that did not include PA or SB.
Study Selection
Initial database searches yielded 946 articles, with an additional 7 articles identified through ancestry searches. After removing duplicate articles, several articles were excluded by reading the title. The abstracts of 94 articles were screened for potential inclusion based on eligibility criteria, with 45 full text articles reviewed.
Primary study quality was assessed using the Physiotherapy Evidence Database (PEDro) scale, a scale commonly used in PA research (Maher, Sherrington, Herbert, Moseley, & Elkins, 2003; Morton, 2009; Verhagen et al., 1998). The PEDro Scale contains 11 criteria to appraise external validity (Criterion 1), internal validity (Criteria 2–9), and the presence of sufficient inferential statistical data (Criteria 10–11) (Maher et al., 2003). External validity (Criterion 1) was evaluated based on the inclusion of specific eligibility criteria (Maher et al., 2003; Verhagen et al., 1998). Internal validity (Criteria 2 – 9) was evaluated by assessing subjects random allocation to groups, group allocation concealment, group similarity at baseline, blinding of subjects, blinding of interventionist, blinding of assessors who measured at least one key outcome, obtaining at least one key outcome from 85% of subjects initially allocated to groups, and using an intention to treat analysis on at least one key outcome (Maher et al., 2003; Verhagen et al., 1998). Presence of sufficient inferential statistical data (Criteria 10 – 11) was evaluated based on the presence of between-group statistical comparisons reported on at least one key outcome and the presence of both point measures and measures of variability for at least one key outcome (Maher et al., 2003; Verhagen et al., 1998). Seventeen articles met the inclusion criteria for the literature review; see Figure 1. for PRISMA flow diagram.
Figure 1.
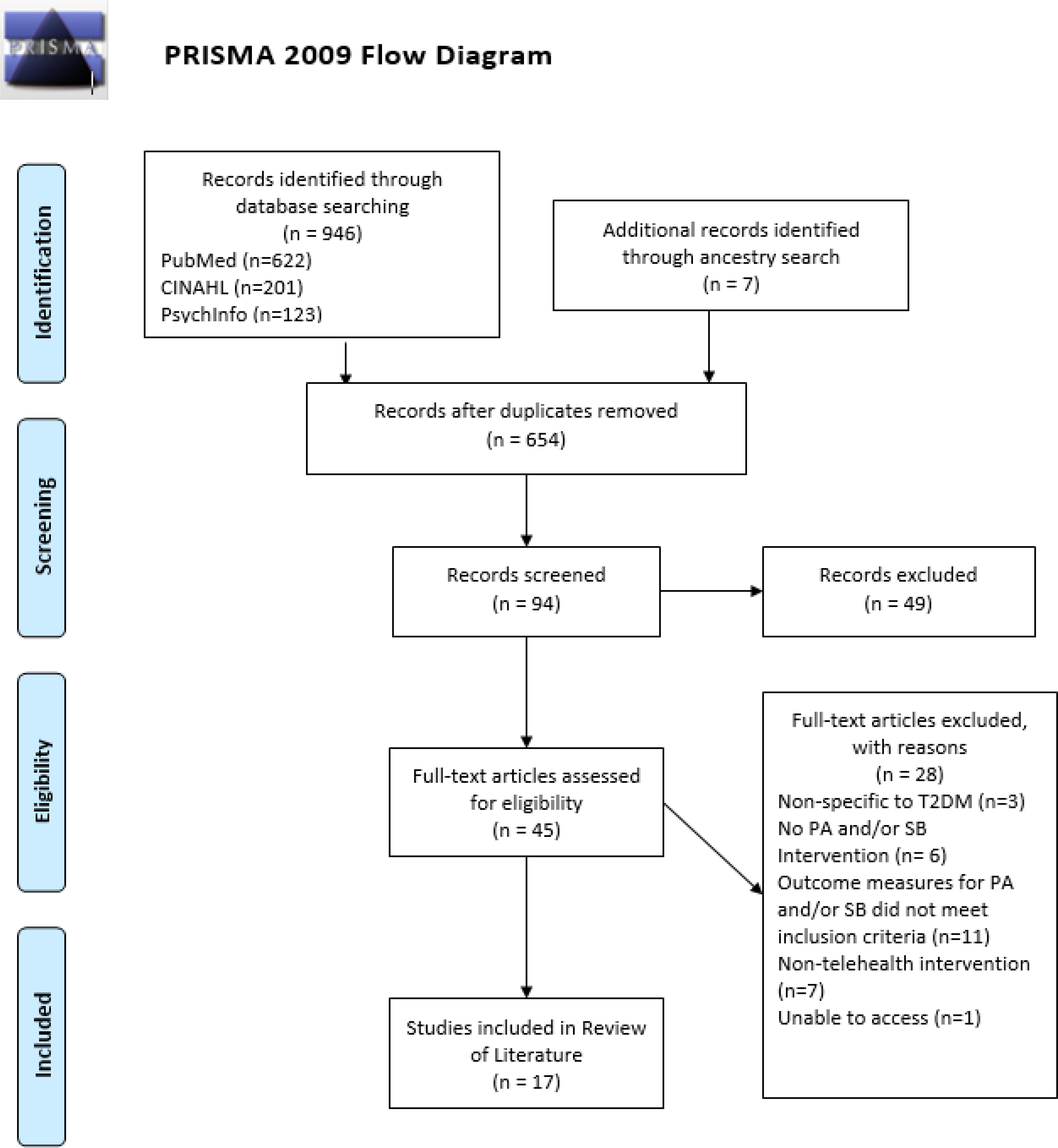
PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyses) Diagram detailing the process of study selection (Moher et al., 2009).
Data Extraction
The primary author (CH) independently extracted all data from the articles included; the second author (BJW) independently reviewed and confirmed the data extraction. Discrepancies between authors were resolved through discussion; the two authors discussed discrepancies and came to a consensus. The following data were extracted: theoretical framework, study design type, sampling method, sample size, attrition rates, study location(s), inclusion and exclusion criteria, participant characteristics, measurement duration and follow-up timeframes, intervention design and telehealth delivery format, outcome measures specific to PA, SB, and GC, other outcomes measures pertinent to the study, and study findings. Table 1. provides an overview of articles included in the review.
Table 1.
Table of Studies
| Study | Theoretical Framework | Sample Characteristics | Intervention Description | Control Description | PA, SB, and/or GC Related Outcome Measurement | Results | Conclusions |
|---|---|---|---|---|---|---|---|
| Akinci et al., 2018 | None reported. | Adults with T2DM for at least 1 year, an A1C greater than 6.5 – 11%, aged 40 – 65 years old, who had high-speed internet access in their homes, from an Endocrinology clinical in Turkey. n = 65 Mean Age (SD): 52.5 (6.4) years Female: 80% Race/Ethnicity: Not reported |
An 8-week intervention comparing supervised aerobic and resistance exercise training, under physical therapist supervision, 3 times per week, in 50 – 60 minutes bouts, with 4 – 6 other study subjects (n=22) with internet-based aerobic and resistance exercise videos, 3 times per week, available through a study website (n=21). The internet-based exercise group submitted reports of exercise electronically and received a short telephone message on Mondays as a reminder to exercise. | An educational brochure about the importance and benefits of PA and exercise in people with T2DM with practical lifestyle tips provided during a one-time counseling session (n=22). | Baseline and 8-week measurements. Steps per day, 6-minute walking distance, A1C, and fasting glucose. |
Found a significant increase in steps per day (Supervised: 1298.67 steps, p=0.04; Internet: 1258.05 steps, p=0.001), increase in 6-minute walking distance (Supervised: 29.32 m, p<0.001; Internet: 30.5 m, p<0.05), decrease in A1C (Supervised: 0.8%, p<0.001; Internet: 0.91%, p<0.05) and decrease in fasting glucose (Supervised: 39.45 mg/dL, p=0.001; Internet: 35.4 mg/dL, p<0.001) in both intervention groups at 8 weeks. | Results support the use of a web-based exercise program. |
| Chang et al., 2018 | Minimal Psychological Intervention | Adults with T2DM, with no serious complications, aged 20 years or older in China. n = 30 Mean Age (SD): 46 (8.9) years Female: 80% Race/Ethnicity: Not reported |
A 10-week intervention, using a mobile phone app (Facebook), within a closed community, including education and quizzes, and a forum to share experiences with other members, structured around cognitive, affective, psychological, and behavioral themes. | One group pre-post design. | Baseline and 10-week measurements. 32-item Diabetes Self Care Behavior Scale, measuring foot care, diet control, exercise, medication compliance, and self-monitoring blood sugar. |
Found an overall significant increase in Diabetes Self Care Behaviors (p=0.01), with a significant increase in exercise self-care behavior (p=0.017) and non-significant findings in self-monitoring blood sugar (p=0.185). | Results support the use of a mobile phone app-based intervention to improve diabetes self-care behaviors, but were limited due to a small sample size, and need for a more robust methodology. |
| Connelly et al., 2017 | Transtheoretical Model | Adults with T2DM, managed with oral medications, aged 18 years or older, who had computer and internet access, living in rural Scotland. n = 31 Mean Age (SD): 66.7 years Female: 41.9% Race/Ethnicity: Not reported |
A 6-month intervention comparing a website with PA education (n=10) and a website with PA education and interactive features, including a PA logbook, activity tracker, virtual coach, goal development, challenges, and local activities (n=11). | Written PA educational materials similar to website materials (n=10). | Baseline, 3- and 6-months measurements. Minutes/week in levels of PA, step counts, time spent sedentary, sedentary bouts, A1C, and fasting glucose. |
Found an increase in MVPA in the website only group (20.3 m/wk, d=0.15), decreases in total sedentary time in all groups (Website only: 147 m/wk, d=0.18; Website with interactive features: 271 m/wk, d=0.5; Control: 160 m/wk, d=0.2), increases in light activity in the website with interactive feature group (23.6 m/wk, d=0.1), and decreases in A1C in website with interactive features and control groups (0.4%, d=0.34; 0.4%, d=0.45) at 3 and 6 months. | Results support the use of a web-based PA intervention but demonstrated the addition of interactive features do not increase activity more than a web-based intervention alone. |
| Glasgow et al., 2010; Glasgow et al., 2012 | Social-Ecological Theory, 5 A’s Self-Management Model | Adults with T2DM, with a BMI ≥ 25 kg/m2, with at least 1 risk factor for heart disease, aged 25 – 75 years old, who had telephone and internet access, in Colorado, U.S. n = 463 Mean Age (SD): 58.4 (9.2) years Female: 49.8% Race/Ethnicity: 6.7% American Indian/Alaskan Native, 1.6% Asian, 15.4% Black or African American, 72% White; 21.5% Latino |
A 12-month intervention comparing a website with PA education, action plans and goal setting for medication adherence, exercise, and food choices, a logbook for 3 daily goals and immediate feedback based on goal success in the past 7 days, graphic displays of physiologic measures, a moderated forum, quizzes, motivational tips, community resources, and periodic prompting providing motivational information (n=169) with a group receiving the website with the addition of follow-up calls from an interventionist and group attendance with other participants (n=162). | Enhanced usual care with computer-based health risk appraisal feedback and recommended preventative care behaviors (n=132). | Baseline, 4- and 6-months measurements. Community Health Activities Model Program for Seniors Questionnaire (total weekly caloric expenditure in PA) and A1C. |
Found a significant increase in weekly total weekly caloric expenditure in both intervention groups at 4 and 12 months (149±356 cal/wk, p=0.019; 677±46 cal/wk, p<0.05). Modest, non-significant improvements in A1C at 4 and 12 months. | Results support the use of a web-based PA intervention but demonstrate the need a more intensive we-based program to see long-term effects. |
| Hansel et al., 2017 | None reported. | Adults with T2DM, receiving stable medication therapy, with an A1C 5.6 – 8.5%, with an email address and internet access in France. n = 120 Mean Age (SD): 56.6 (9.2) years Female: 66.7% Race/Ethnicity: Not reported |
A 4-month intervention using a web-based nutritional support tool to improve lifestyle habits for diet and PA using 4 modules which could be accessed simultaneously, including a diet and daily steps logbook, weekly menu and shopping list development, PA education, and brief PA videos (n=60). | Usual Care described as continuing care with general practitioner (n=60). | Baseline and 4-months measurements. IPAQ – S (self-reported duration and frequency of PA), aerobic fitness levels, A1C, and fasting glucose. |
Found a significant reduction in A1C in the intervention group (0.3%, p<0.001). No significant differences in self-reported PA, aerobic fitness levels, or fasting glucose. | Results support the use of a web-based nutritional support tool to improve glycemic control, but demonstrate the need for a more focused PA intervention to see improvements in PA. |
| Jennings et al., 2014 | Theory of Planned Behavior | Adults with T2DM, who are not receiving diabetes education or meeting national PA guidelines, over 18 years old, with email and internet access in Australia. n = 397 Mean Age: 58 years Female: 47.6% Race/Ethnicity: Not reported |
A 3-month intervention using a PA website, including educational modules, social support, positive reinforcement, personalized feedback, goal setting, and planning activities (n=195). | Usual care with limited access to PA website; home page and contact information only (n=202). | Baseline, 3- and 9-month measurements. IPAQ-L (self-reported duration and frequency of PA and SB in m/wk) |
Found a significant increase in self-reported total PA (370.6 m/wk, p<0.01) at 3 months, increase in moderate-intensity PA at 3 months (189.5 m/wk, p<0.05), and decreases in weekday and weekend sitting (110.9 m/wk, p<0.001; 100.3 m/wk, p<0.001) at 3 months and (67.2 m/wk, p<0.05) at 9 months. | Results support the use of a web-based PA and SB intervention. |
| Kooiman et al., 2018 | Social Cognitive Theory | Adults with T2DM, with an A1C ≥7.5%, who are 18 years or older, with computer and internet access in the Netherlands. n = 72 Mean Age (SD): 56.3 (11.4) years old Female: 47.2% Race/Ethnicity: Not reported |
A 3-month intervention using a Fitbit activity tracker and access to an online self-tracking program, aimed to optimize knowledge about living a healthy lifestyle, increase awareness of individual PA, and self-efficacy, through information about health consequences, setting behavioral and outcome goals, identifying barriers and problem solving, action planning, behavioral self-monitoring, receiving feedback, and habit formation (n=40). | Usual care described as visits every 3 months with a nurse or primary care provider (n=32). | Baseline and 3-month measurements. Steps per day, a 1-item PA questionnaire measuring engagement in 30 minutes of MVPA per day, A1C, and advanced glycation end products. |
Found a significant increase in self-reported MVPA (1.5±3 d/wk, p=0.047) and steps per day (1255±1500 steps, p=0.01) in the intervention group. There were no significant changes in A1C or advanced glycation end products. | Results support the use of a pedometer and web-based PA intervention but would benefit from including additional long-term follow-up. |
| Liebreich et al., 2009 | Social Cognitive Theory | Adults with T2DM, with no contraindications to PA, who are 18 years or older, with email and internet access in Canada. n = 49 Mean Age: 54.1 (10.3) years old Female: Not reported Race/Ethnicity: Not reported |
A 3-month intervention using a PA website based on SCT which provided education using five sections including a weekly topic, education, research, fitness tips, and PA myths, a PA logbook, community message forum, and email counseling with a study coordinator (n=25). | Received access to control group website with static links to Canadian Diabetes Association Clinical Practice Guidelines; no specific direction on physical activity was given (n=24). | Baseline and 3-month measurements. Godin Leisure Time Exercise Questionnaire (self-reported leisure time PA) |
Found a significant increase in leisure time MVPA (35 m/wk, p=0.052) and MET-minutes PA adjusted for BMI (171 MET-minutes, p=0.043). | Results support the use of a web-based PA intervention, driven by SCT but would benefit from including additional long-term follow-up. |
| Lorig et al., 2010 | None reported. | Adults with T2DM, who are 18 years or older, with internet access in the U.S. n = 761 Mean Age: 54.3 years old Female: 76% Race/Ethnicity: 14.5% American Indian/Alaska Natives; Others not reported |
A 6-month intervention compared an IBDSM Program, with 6 weekly sessions, including PA education, a weekly questionnaire, action plan development, a discussion center with interactive threaded bulletin boards, interactive measures, including a medication and exercise log, audio relaxation exercises, meal planning, glucose monitoring tools, and links to diabetes related websites, a private messaging center, and a copy of a book to use as a reference (n=259) with an IBDSM program plus two peer facilitators reminded participants to log on, provided modeling of action planning and problem solving, offered encouragement, posted on bulletin boards, and monitored posts for inappropriate content (n=232). | Usual care was not described (n=270). | Baseline, 6- and 18-month measurements. Self-report PA scale measured total minutes per week of aerobic exercise and A1C. |
Found no significant improvements in self-reported PA and significant improvement of A1C in the IBDSM only group at 6 months (0.034±0.844%, p=0.036). Identified stronger improvements in A1C in participants with a baseline A1C >7% (p<0.01) during subgroup analysis. | Results support the use of an IBDSM to improve PA but demonstrated no improvement when reinforcement features were added. Identified participants with elevated A1C demonstrated greater improvements than others. |
| Lorig et al., 2016 | None reported. | Adults with T2DM, aged 18 years or older, who are affiliated with an Anthem Health Plan in the U.S. n = 1229 Mean Age: 57.7 years old Female: 66.5% Race/Ethnicity: 74.4% Non-Hispanic White, 12.4% Black, Hispanic 7.4% |
A 6-week intervention which made comparisons between a face to face (n=1000) and web-based diabetes self-management program (n=229), including education about enhancing self-efficacy, healthy eating, exercise, understanding glucose monitoring, communication with family, friends, and healthcare providers, hypoglycemia, depression, emotional difficulties, sick day, medication management, problem solving, decision making, and action planning, with 2 peer facilitators. | No control group; two intervention groups were compared. | Baseline and 12-month measurements. Self-report PA scale measured total minutes per week of aerobic exercise and A1C. |
Found significant decrease in A1C (0.447%, p<0.001) and increases in aerobic exercise (16.7 m/wk, p<0.001) in combined groups. No significant differences were found between face to face and web-based groups. | Results support the use of a web-based diabetes self-management program, demonstrating similar efficacy to traditional face to face programs; however, self-enrollment and a lack of control group limit the generalizability of this study. |
| Muller et al., 2017 | None reported. | Adults with T2DM, aged 18 years or older, with access to the internet, who were able to read in English, German, or Mandarin, in the United Kingdom, Austria, Germany, Ireland, and Taiwan. n = 1045 Mean Age: 62 years old Female: 36.4% Race/Ethnicity: Not reported |
An intervention (length not included in publication) comparing two web-based PA interventions, using a static plain text version (n=497), and an interactive version with personalized audio-visual features (n=548), including sequences demonstrating lifestyle and PA activities, a PA planner, tailored feedback, and images based on responses to questions. Both versions included 5 sections about knowledge of PA benefits, advice on the selection of PA, advice of planning PA, success stories, and access to additional information about PA. | No control group; two intervention groups were compared. | Baseline and post-intervention measurements. IPAQ – S (self-reported duration and frequency of PA and SB) and self-reported beliefs, confidence, and intention related to PA |
Found significant increases in beliefs in benefits of PA (Interactive: 0.22, p<0.001; Static: 0.10, p=0.01), greater confidence in undertaking PA (Interactive: 0.35, p<0.001; Static: 0.34, p=0.001), and stronger intention to increase PA (Interactive: 0.49, p<0.001; Static: 0.35 p<0.001). No significant differences between the interactive and plain text versions. | Results support the use of web-based diabetes PA intervention and demonstrated the impact of using person-based approaches to design. |
| Poppe et al., 2019 | Self-regulation framework, Health Action Process Approach Model | Adults with T2DM, who are literate in Dutch, able to use a computer with internet access, and having not participating in the MyPlan 2.0 qualitative study in Belgium. n = 54 Mean Age: 62.7 years old Female: 37% Race/Ethnicity: Not reported |
A 5-week web and mobile-phone based intervention using 5 weekly sessions about PA or SB and the creation and evaluation of personal goals with an optional mobile app including 5 modules for daily support, with a gamification element. During the first week, participants selected either a PA (n=24) or SB (n=12) intervention group. | Usual Care, but not described (n=18). | Baseline and 5-week measurements. IPAQ – L (self-reported duration and frequency of PA and SB), LASA-SB (self-reported total sedentary time on weekdays), and objectively measured number of breaks from sedentary time, sedentary bouts, total sedentary time, number of steps, levels of PA, and total PA. |
Found significant increases in objectively measured moderate PA (8.48 m/d, p=0.05) and MVPA (8.43 m/d, p=0.049) in the PA intervention group and increases in breaks in sedentary time in the SB group (0.62 breaks/day, p=0.005). | Results support the use of self-regulated choice of a PA or SB web-based intervention on improving PA and SBs. |
| Richardson et al., 2010 | Social Cognitive Theory, Social Influence Theory | Adults with T2DM or coronary artery disease, with a BMI ≥ 25 kg/m2, with a valid email address, email access weekly, an internet connected computer using Windows XP or Vista, who lead a sedentary lifestyle in Michigan, U.S. n = 324 Mean Age (SD): 52 (11.4) years old Female: 66% Race/Ethnicity: 1% American Indian, 3% Asian, 6% Black, 86% 2% Other, 86% White; 2% Hispanic |
A 4-month web-based intervention, including components to upload pedometer data, receive step-count feedback, individually assigned and gradually increasing step-counts, and individually tailored motivational messages (n=70) compared to a group which received the web-based intervention with access to an online community (n=254). | No control group; two intervention groups were compared. | Baseline and 4-month measurements. Daily step counts |
Found a significant increase in daily step counts in both groups (No online community: 1579 steps, p<0.001; With online community: 1974 steps, p<0.001). No differences between groups on daily step counts. | Results support the use of a web-based intervention to increase daily steps but demonstrated that online community features did not have an influence. |
| Van der Weegen et al., 2015 | Not reported. | Adults with T2DM or COPD, aged 40 – 70 years old, who participate in less than 30 minutes per day MVPA on 5 or more days of the week, with a BMI ≥ 26 kg/m2 for T2DM or stable respiratory functioning for COPD in the Netherlands n = 199 Mean Age: 57.9 (7.6) years old Female: 51.3% Race/Ethnicity: 6% Non-Dutch |
A 3-month web and mobile phone-based intervention comparing a group receiving a nurse delivered Self-Support Program, which includes 4 nurse consultations, education, and local activities, an activity monitor tool that included a mobile and web-app, and monitored feedback (n=65) with a group receiving only the Self-Support Program (n=66). | Usual Care but not described (n=68). | Baseline, 4 – 6 and 9-months measurements. Minutes per day MVPA |
Found a significant increase in MVPA in the web and mobile-phone added group compared to the control group (11.73 m/d, p<0.001) and self-support program only group (7.86 m/d, p<0.003) at the 4-month and 9-month points (10.59 m/d, p<0.001; 9.41 m/d, p<0.001 respectively). | Results support the use of an interactive web and mobile phone-based intervention to increase PA in addition to a traditional self-support program. |
| Verwey et al., 2014 | Not reported. | Adults with T2DM or COPD, over age 40, with a BMI ≥ 25 kg/m2 for T2DM and Gold Criteria 2 or 3 for COPD in the Netherlands. n = 20 Mean Age: 60 years old Female: 45% Race/Ethnicity: Not reported |
A 3-month mixed-methods pilot study of a web and mobile phone-based intervention with a nurse delivered Self-Support Program, which includes 4 nurse consultations, education, and local activities, with a monitoring and web and mobile-phone based feedback tool, with qualitative interviews after each nurse consultation. | One group pre-post design. | Baseline, 2- and 3-months measurements. Minutes per day MVPA |
Found a significant increase in mean activity levels (10.6 m/d, p=0.02). | Results support the use of an interactive web and mobile phone-based intervention to increase PA in additional to a traditional self-support program. |
| Yom-Tov et al., 2017 | Not reported. | Adults with T2DM, with an A1C over 6.5%, leading a sedentary lifestyle with no dedicated PA program, with an Android based smartphone and data connection plan from an endocrinology and diabetes outpatient clinic in Israel. n = 27 Mean Age: 56.9 years old Female: 33.3% Race Ethnicity: Not reported |
A 26-week intervention of a mobile phone app that collects data about PA performed and uses a reinforcement learning algorithm to provide personalized text messages that would most likely increase PA the next day (n=20). | Once weekly unchanging reminder to exercise (n=7). | Baseline and 6 months measurements. Amount and rate of walking, and A1C. |
Found significant A1C reductions in participants allocated to the personalized text message group, those with a higher baseline A1C, and lower baseline activity levels (R 2=0.405, p<0.01). The personalized text message group had a non-significant increase in walking rates compared to the control group. | Results support the use of a personalized text message, based on activity performance, to increase PA. |
Note. A1C: Glycated Hemoglobin; BMI: Body Mass Index; cal/wk: Calories per Week; COPD: Chronic Obstructive Pulmonary Disorder; d/wk: Days per Week; GC: Glycemic Control; IBDSM: Internet Based Diabetes Self-Management; IPAQ-L: International Physical Activity Scale – Long Version; IPAQ-S: International Physical Activity Scale – Short Version; LASA-SB: Longitudinal Ageing Study Amsterdam – Sedentary Behavior; m: Meters; MET: Metabolic Equivalent; m/d: Minutes per Day; m/wk: Minutes per Week; MVPA: Moderate-to-vigorous physical activity; PA: Physical Activity; SB: Sedentary Behavior; SCT: Social Cognitive Theory; SD: Standard Deviation; T2DM: Type 2 Diabetes Mellitus: U.S.: United Stated
Results
Study Characteristics
Characteristics of the seventeen studies are summarized in Table 1. Sample sizes ranged from 20 – 1229. The mean age of participants ranged from 46 – 66.7 years. In seven studies there were more females than males enrolled in the study (Akinci et al., 2018; Chang et al., 2018; Hansel et al., 2017; Lorig et al., 2010; Lorig et al., 2016; Richardson et al., 2010; Van der Weegen et al., 2015). One study did not report the number of female or male participants enrolled (Liebreich et al., 2009). Race and/or ethnicity were not reported in most studies, but when reported the majority of participants were Non-Hispanic, White (Glasgow et al., 2010; Glasgow et al., 2012; Lorig et al., 2016; Richardson et al., 2010).
Quality assessment.
Findings from the study quality assessment are presented in Table 2. The PEDro scale does not indicate specific cut-points to identify level of quality; that said, the more criteria present, the greater the study quality (Maher et al., 2003; Verhagen et al., 1998). Twelve of the seventeen studies scored at least seven on the PEDro scale (Akinci et al., 2018; Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2012; Hansel et al., 2017; Jennings et al., 2014; Kooiman et al., 2018; Liebreich et al., 2009; Lorig et al., 2010; Muller et al., 2017; Richardson et al., 2010; Yom-Tov et al., 2017). All studies included specific details about eligibility criteria and included point measurements. Fourteen studies included a between groups statistical comparisons on at least one outcome measure. Twelve studies clearly specified random group allocation and the inclusion of intention to treat analysis on at least one outcome measure. Ten studies had similar groups at baseline and blinded assessors. Seven studies concealed group allocation. Due to the nature of the studies included, participants and interventionists were not blinded to their group allocation. However, in four studies (Connelly et al., 2017; Hansel et al., 2017; Muller et al., 2017; Yom-Tov et al., 2017) the interventions were completely online without an interventionist.
Table 2.
Study Quality Assessment
| PEDro Criteria | Eligibility specified | Random-isation | Allocation concealed | Groups similar at baseline | Subjects blinded | Interventionist blindeda | Assessors blindedb | Key outcome obtained from 85% | Intention to treat analysis | Between group statistical outcome | Point measure | Total Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Akinci et al., 2018 | Y | Y | Y | Y | N | N | Y | N | Y | Y | Y | 8 |
| Chang et al., 2018 | Y | N | N | N | N | N | N | N | N | N | Y | 2 |
| Connelly et al., 2017 | Y | Y | Y | Y | N | Y | N | N | N | Y | Y | 7 |
| Glasgow et al., 2010; Glasgow et al., 2012 | Y | Y | Y | Y | N | N | Y | N | Y | Y | Y | 8 |
| Hansel et al., 2017 | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 10 |
| Jennings et al., 2014 | Y | Y | Y | Y | N | N | Y | N | Y | Y | Y | 8 |
| Kooiman et al., 2018 | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 7 |
| Liebreich et al., 2009 | Y | Y | N | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Lorig et al., 2010 | Y | Y | N | Y | N | N | Y | N | Y | Y | Y | 7 |
| Lorig et al., 2016 | Y | N | N | N | N | N | N | N | Y | Y | Y | 4 |
| Muller et al., 2017 | Y | Y | N | Y | N | Y | Y | Y | Y | Y | Y | 9 |
| Poppe et al., 2019 | Y | Y | Y | N | N | N | N | N | N | Y | Y | 5 |
| Richardson et al., 2010 | Y | Y | N | Y | N | N | Y | N | Y | Y | Y | 7 |
| Van der Weegen et al., 2015 | Y | N | N | N | N | N | Y | N | Y | Y | Y | 5 |
| Verwey et al., 2014 | Y | N | N | N | N | N | N | N | N | N | Y | 2 |
| Yom-Tov et al., 2017 | Y | Y | Y | N | N | Y | Y | N | Y | Y | Y | 8 |
Note. The Physiotherapy Evidence Database (PEDro) scale was used to rate the quality of studies included in this review (Maher et al., 2003; Verhagen et al., 1998). N: No; Y: Yes.
Four studies were completed online without the involvement of an interventionist (Connelly et al., 2017; Hansel et al., 2017; Muller et al., 2017; Yom-Tov et al., 2017).
Five study outcome assessments were completed online without the involvement of an assessor (Glasgow et al., 2010; Glasgow et al., 2012; Jennings et al., 2014; Liebreich et al., 2009; Lorig et al., 2010).
Research design.
Thirteen articles were randomized controlled trials, randomizing participants to groups, using simple random assignment or block randomization (Akinci, Yeldan, Satman, Dirican, & Ozdincler, 2018; Glasgow et al., 2010; Glasgow et al., 2012; Hansel et al., 2017; Jennings, Vandelanotte, Caperchione, & Mummery, 2014; Kooiman et al., 2018; Liebreich, Plotnikoff, Courneya, & Boule, 2009; Lorig et al., 2010; Muller et al., 2017; Poppe et al., 2019, Richardson et al., 2010, Van der Weegen et al., 2015; Yom-Tov et al., 2017). Five randomized controlled trials compared two levels of the intervention with a control group (Akinci et al., 2018; Glasgow et al., 2010; Glasgow et al., 2012; Lorig et al., 2010; Van der Weegen et al., 2015). Two studies used a quasi-experimental design (Chang, Chang, Chen, & Yen, 2018; Lorig et al., 2016). Two studies used a mixed-methods design, with a qualitative component used for intervention development, with one including a randomized controlled trial and one a quasi-experimental design component as pilot studies (Connelly, Kirk, Masthoff, & MacRury, 2017; Verwey et al., 2014).
Location of studies.
Only one study was conducted in an exclusively rural population (Connelly et al., 2017). Five studies were conducted in the U.S., with one in Michigan, two in Colorado, and two with non-specified locations (Glasgow et al., 2010; Glasgow et al., 2012; Lorig et al., 2010; Lorig et al., 2016; Richardson et al., 2010). Twelve studies included were conducted internationally (Akinci et al., 2018; Chang et al., 2018; Connelly et al., 2017; Hansel et al., 2017; Jennings et al., 2014; Kooiman et al., 2018; Liebreich et al., 2009; Muller et al., 2017; Poppe et al., 2019; Van der Weegen et al., 2015; Verwey et al., 2014; Yom-Tov et al., 2017). Studies conducted internationally did not disclose if U.S. populations had been included in their sample (Akinci et al., 2018; Chang et al., 2018; Connelly et al., 2017; Hansel et al., 2017; Jennings et al., 2014; Kooiman et al., 2018; Liebreich et al., 2009; Muller et al., 2017; Poppe et al., 2019; Van der Weegen et al., 2015; Verwey et al., 2014; Yom-Tov et al., 2017).
Theoretical frameworks.
Eight studies did not include a theoretical framework to guide the intervention (Akinci et al., 2018; Hansel et al., 2017; Lorig et al., 2010; Lorig et al., 2016; Muller et al., 2017; Van der Weegen et al., 2015; Verwey et al., 2014; Yom-Tov et al., 2017). Chang et al. (2018) developed an intervention driven by Minimal Psychological Intervention design features. Eight studies included theoretical frameworks to guide intervention development, including: the Transtheoretical Model, Social-Ecology Theory, 5 A’s Self-management Model, Theory of Planned Behavior, Social Cognitive Theory, Self-Regulation Framework, Health Action Process Approach model, and Social Influence Theory (Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2012; Jennings et al., 2014; Kooiman et al., 2018; Liebreich et al., 2009; Poppe et al., 2019; Richardson, 2010). Social Cognitive Theory was included in three studies (Kooiman et al., 2018; Liebreich et al., 2009; Richardson et al., 2010). Commonalities in the theoretical frameworks used to guide intervention development included partial to full integration of the framework within the intervention design and addressing health behavior change constructs, such as, social support, self-efficacy, perceived behavioral control, action planning, self-monitoring (Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2012; Jennings et al., 2014; Kooiman et al., 2018; Liebreich et al., 2009; Poppe et al., 2019; Richardson, 2010). Through theoretical framework integration, four common intervention components were identified, education, planning, self-monitoring logbooks, and tailored feedback, in studies with improvement in outcome measures (Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2012; Jennings et al., 2014; Kooiman et al., 2018; Liebreich et al., 2009; Poppe et al., 2019; Richardson et al., 2010).
Intervention Design and Length
Types of telehealth interventions.
Ten studies delivered the intervention in only a web-based format (Akinci et al., 2018; Connelly et al., 2017; Hansel et al., 2017; Jennings et al., 2014; Kooiman et al., 2018; Liebreich et al., 2009; Lorig et al., 2010; Lorig et al., 2016; Muller et al., 2017; Richardson et al., 2010). Two studies used a mobile app for intervention delivery (Chang et al., 2018; Yom-Tov et al., 2017). Three studies used a combined web and mobile device delivered intervention (Poppe et al., 2019; Van der Weegen et al., 2015; Verwey et al., 2014). Two studies supplemented a web-based intervention delivery format with telephone calls (Glasgow et al., 2010; Glasgow et al., 2012).
Intervention components.
Thirteen common components were identified in the seventeen studies included, see Table 3. The most common intervention feature is education about diabetes self-management and/or physical activity (Chang et al., 2018; Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2012; Hansel et al., 2017; Jennings et al., 2014; Kooiman et al., 2018; Liebreich et al., 2009; Lorig et al., 2010; Lorig et al., 2016; Muller et al., 2017; Poppe et al., 2019; Van der Weegen et al., 2015; Verwey et al., 2014). A logbook for self-monitoring was included in eleven studies, planning or goal setting was addressed in nine studies, and tailored feedback was included in nine studies (Chang et al., 2018; Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2012; Hansel et al., 2017; Jennings et al., 2014; Kooiman et al., 2018; Liebreich et al., 2009; Lorig et al., 2010; Lorig et al., 2016; Muller et al., 2017; Poppe et al., 2019; Richardson et al., 2010; Van der Weegen et al., 2015; Verwey et al., 2014; Yom-Tov et al., 2017). Additional intervention components included videos, quizzes, barrier identification, local activities, peer support, reminder messages, professional facilitators, and peer facilitators.
Table 3.
Intervention Components
| Study | Intervention Components | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Education | Videos | Quizzes | Planning (Goal Setting) | Barrier Identification | Self-Monitoring Logbook | Tailored Feedback | Local Activities | Peer Support | Reminder Message | Professional Facilitator | Peer Facilitator | |
| Akinci et al., 2018 | x | x | ||||||||||
| Chang et al., 2018 | x | x | x | x | x | x | ||||||
| Connelly et al., 2017 | x | x | x | x | x | x | ||||||
| Glasgow et al., 2010; Glasgow et al., 2012 | x | x | x | x | x | x | x | |||||
| Hansel et al., 2017 | x | x | x | |||||||||
| Jennings et al., 2014 | x | x | x | x | ||||||||
| Kooiman et al., 2018 | x | x | x | x | x | |||||||
| Liebreich et al., 2009 | x | x | x | x | ||||||||
| Lorig et al., 2010 | x | x | x | x | x | x | x | |||||
| Lorig et al., 2016 | x | x | x | |||||||||
| Muller et al., 2017 | x | x | x | |||||||||
| Poppe et al., 2019 | x | x | x | x | x | x | x | |||||
| Richardson et al., 2010 | x | x | x | x | ||||||||
| Van der Weegen et al., 2015 | x | x | x | |||||||||
| Verwey et al., 2014 | x | x | x | |||||||||
| Yom-Tov et al., 2017 | x | |||||||||||
Intervention length and contact frequency.
The duration of interventions ranged from 2 to 6 months. Availability and delivery of intervention content varied between studies. One study provided daily intervention contact, through daily feedback, to participants (Yom-Tov et al., 2017). A single study delivered intervention content three times per week (Akinci et al., 2018). Seven studies delivered intervention content or provided feedback weekly (Glasgow et al., 2010; Glasgow et al., 2012; Hansel et al., 2017; Liebreich et al., 2009; Lorig et al., 2010; Lorig et al., 2016; Poppe et al., 2015). Eight studies provided open access to intervention content (Chang et al., 2018; Connelly et al., 2017; Jennings et al., 2014; Kooiman et al., 2018; Muller et al., 2017; Richardson et al., 2010; Van der Weegen et al., 2015; Verwey et al., 2014).
Follow-up periods.
Most studies reported only post-intervention measurements, with no additional follow-up period. Two studies included an additional 9-month follow-up (Jennings et al., 2014; Van der Weegen et al., 2015). A 12-month follow-up was measured by three studies (Glasgow et al., 2012; Lorig et al., 2010; Lorig et al., 2016).
Outcome Measurement
Physical activity and sedentary behavior measures.
The primary method of PA outcome measurement was by self-report; which was used in 11 studies (Chang et al., 2018; Glasgow et al., 2010; Glasgow et al., 2012; Hansel et al., 2017; Jennings et al., 2014; Kooiman et al., 2018; Leibreich et al., 2009; Lorig et al., 2010; Lorig et al., 2016; Muller et al., 2017; Poppe et al., 2019). Physical activity self-report measures used include the Diabetes Self-Care Behaviors Scale, the Community Health Activities Model Program for Seniors Questionnaire, the International Physical Activity Questionnaire, the Godin Leisure Time Exercise Questionnaire, and a 1-item Physical Activity Questionnaire (Chang et al., 2018; Glasgow et al., 2010; Glasgow et al., 2012; Hansel et al., 2017; Jennings et al., 2014; Kooiman et al., 2018; Leibreich et al., 2009; Muller et al., 2017; Poppe et al., 2019). Two studies did not disclose the PA tool used (Lorig et al., 2010; Lorig et al., 2016). Objective measures of PA were used less frequently, in only eight studies. Pedometers, waist worn accelerometers, and a cell phone accelerometer were used to collected objective PA measures (Akinci et al., 2018; Connelly et al., 2017; Hansel et al., 2017; Poppe et al., 2019; Richardson et al., 2010; Van der Weegen et al., 2015; Verwey et al., 2014; Yom-Tov et al., 2017). Sedentary behavior was reported in two studies using an accelerometer and three studies using the International Physical Activity Questionnaire and the Longitudinal Ageing Study Amsterdam – Sedentary Behavior Scale (Connelly et al., 2017; Jennings et al., 2014; Muller et al., 2017; Poppe et al., 2019).
Glycemic control.
Glycated hemoglobin levels were most frequently measured to evaluate GC (Akinci et al., 2018; Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2012; Hansel et al., 2017; Kooiman et al., 2018; Lorig et al., 2010; Lorig et al., 2016; Yom-Tov et al., 2017). Glycated hemoglobin lab specimens were primarily collected in clinic or laboratory settings (Akinci et al., 2018; Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2012; Hansel et al., 2017; Kooiman et al., 2018; Yom-Tov et al., 2017). High performance liquid chromatography methods were used to analyze blood specimen in three studies (Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2010). Two studies mailed specimen collection kits to participants who self-collected blood specimens, one using a BIOSAFE kit (Lorig et al., 2010) and the other not disclosing the specific kit (Lorig et al., 2016), before returning the kit to researchers. All studies measuring GC also measured PA. Fasting glucose was included in 3 studies as a measure of GC in addition to glycated hemoglobin levels (Akinci et al., 2018; Connelly et al., 2017; Hansel et al., 2017). Glycated hemoglobin levels are the gold-standard measurement to evaluate average glycemic control over approximately 3 months, using fasting glucose levels alone would be considered a limitation as they provide minimal information about overall glycemic control (ADA, 2019a).
Other outcome measures.
Multiple other outcome measures were included in studies. Outcome measures related to website usage were included in six studies (Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2012; Jennings et al., 2014; Muller et al., 2017; Richardson et al., 2010). Additional biomarkers and anthropometric measures were included in six studies (Akinci et al., 2018; Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2012; Hansel et al., 2017; Kooiman et al., 2018). Several studies included additional outcomes measures evaluating diabetes knowledge, quality of life, health literacy and resource utilization, behavioral self-management, and mental health (Akinci et al., 2018; Chang et al., 2018; Glasgow et al., 2010; Glasgow et al., 2012; Hansel et al., 2017; Kooiman et al., 2018; Liebreich et al., 2009; Lorig et al., 2010; Lorig et al., 2016; Poppe et al., 2019; Van der Weegen et al., 2015; Verwey et al., 2014; Yom-Tov et al., 2017).
Attrition from Telehealth Interventions
Three studies reported overall attrition rates ranging from 10.8 – 30.3% (Hansel et al., 2017; Lorig et al., 2010; Lorig et al., 2016). Attrition rates for intervention groups ranged dramatically from 0.7% to 57.9%, with most studies falling between 20 – 40% (Akinci et al., 2018; Chang et al., 2018; Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2012; Jennings et al., 2014; Kooiman et al., 2018; Liebreich et al., 2009; Muller et al., 2017; Poppe et al., 2019; Richardson et al., 2010; Van der Weegen et al., 2015; Verwey et al., 2014). In two studies with attrition rates of 31.4% (Glasgow et al., 2012) and 52.3% (Akinci et al., 2018) a commonality identified was a lack of feedback or interventionist involvement. Longer study lengths was also identified a commonality in studies with higher attrition rates; with attrition rates of 31.4% being reported at 12 months (Glasgow et al., 2012) and 57.9% at 9 months (Jennings et al., 2014). Control group attrition rates were overall lower, ranging from 1.5 – 39.6%, with most studies falling between 10 – 16% (Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2012; Jennings et al., 2014; Kooiman et al., 2018; Liebreich et al., 2009; Richardson et al., 2010; Van der Weegen et al., 2015). One study did not report attrition rates (Yom-Tov et al., 2017).
Intervention Impact
Physical activity and sedentary behavior impact.
Significant improvements in PA were observed in ten studies (Akinci et al., 2018; Glasgow et al., 2010; Glasgow et al., 2012; Jennings et al., 2014; Kooiman et al., 2018; Liebreich et al., 2009; Lorig et al., 2016; Richardson et al., 2010; Van der Weegen et al., 2015; Verwey et al., 2014). Connelly et al. (2017) reported small effects on moderate to vigorous PA when using a Transtheoretical Model Driven web-based PA intervention. Using the Theory of Planned Behavior to drive the intervention, Jennings et al. (2014) found significant increases in self-reported total and moderate-intensity PA and decreases in weekday and weekend sitting. Significant long-term improvement in PA was identified at the 9-month and 12-month follow-up points in two studies (Lorig et al., 2016; Van der Weegen et al., 2015). Improvement in sedentary time was reported as a small to moderate effect (Connelly et al., 2017). One study identified significant improvements in PA and SB, using a Health Action Process Approach model and Self-Regulation Theory driven intervention (Poppe et al., 2019).
Impact on glycemic control.
Four studies reported significant improvements in GC, with one reporting moderate effects (Akinci et al., 2018; Connelly et al., 2017; Hansel et al., 2017; Lorig et al., 2016; Yom-Tov et al., 2017). Akinci et al. (2018) demonstrated significant improvements in both A1C and fasting glucose. Lorig et al. (2010) noted stronger improvements in A1C in participants with a baseline A1C >7%. At a 12-month follow-up Lorig et al. (2016) identified significant decreases in A1C. Clinically relevant, non-significant improvements in A1C were identified in two studies (Glasgow et al., 2010; Glasgow et al., 2012).
Discussion
This review supports the use of web and mobile phone-based strategies to delivery PA and SB interventions to adults with T2DM. However, many of the studies reviewed did not include a theoretical framework to drive intervention development, intervention components specific to SB, or use objective outcome measures. Additionally, few studies reviewed were conducted with a focus on rural populations in the U.S.
Intervention Design
Web and mobile phone-based interventions have demonstrated the ability to improve outcome measures. Health behavior change interventions which focused on PA and SB specifically resulted in greater improvements than interventions targeted towards diabetes self-management overall (Akinci et al., 2018; Connelly et al., 2017; Glasgow et al., 2010; Glasgow et al., 2012; Jennings et al., 2014; Kooiman et al., 2018; Liebreich et al., 2009; Muller et al., 2017; Poppe et al., 2019; Richardson et al., 2010; Van der Weegen et al., 2015; Verwey et al., 2014). Additionally, only three studies used a combined web and mobile phone-based delivery system (Poppe et al., 2019; Van der Weegen et al., 2015; Verwey et al., 2014). While 81% of U.S. households were reported to have a computer with an internet subscription in 2016, it was identified that households which only had internet access via a smartphone device were more likely to be low-income, Black, or Hispanic (Ryan, 2018). Using a combined web and mobile phone-based delivery system will increase intervention accessibility to diverse populations who do not own a computer. While several studies have been presented which include an intervention focused on improving PA and reducing SBs, further research is needed to provide additional support for interventions which combine a web and mobile-phone delivery system or compare the effects of combined interventions.
This review identified only one study which included an intervention specific to SB (Poppe et al., 2019). Sedentary behavior has been identified as a separate, while equally relevant, component to diabetes self-management (ADA, 2016). Therefore, interventions focused solely on improving PA are not adequate to produce improvements in SBs (Martin et al., 2015; Prince, Saunders, Gresty, & Reid, 2014). Sedentary behavior must be included in future research studies as a separate component, to better understand the ability of web and mobile phone-based health behavior change interventions to make changes in SBs.
To further improve web and mobile phone-based interventions, additional studies, which are clearly driven by theoretical constructs must be conducted. Nearly half of the reviewed studies did not include any theoretical framework, making it difficult to fully understand the health behavior change mechanisms which resulted in study outcomes. Of the studies that did include a theoretical framework, few made full framework integration clear. By developing interventions which are theory driven, mechanisms of change and resultant outcomes can be better understood.
Outcome Timeframes and Measurement
Studies identified by this review included a broad range of intervention timeframes and measurement periods. No studies included elucidated a dose specific intervention period, which would be beneficial to better understand the minimum required intervention and point where additional intervention delivery does not affect the outcome. Few studies reviewed included long-term follow-up measures after the post-intervention outcome measures. Including long-term follow-up measures would provide evidence of the study interventions ability to produce long-term health behavior change. To further improve long-term outcome measurement, identifying methods to reduce attrition rates is necessary, to reduce internal validity threats.
Evaluating outcome measures of studies reviewed revealed that self-report measures are most commonly used to measure PA and SBs. Differences between self-report measures of PA and objective measures have been identified (Arvidsson, Fridolfsson, & Borjesson, 2019; Prince et al., 2008). Prince et al. (2008) found both under- and over-reporting of self-reported PA compared to objective measures. While no clear trends in under- or over-reporting have been identified, self-report measures which categorize PA by level of intensity demonstrate a trend with larger differences in self-report and objective measures when higher intensity levels (i.e., vigorous activity) are reported (Prince et al., 2008). Additionally, PA self-report measures are not adequate to fully examine SBs. It is necessary to include measurement tools specific to SB, to understand the domains and modes which SBs occur (Prince, LeBlanc, Colley, & Saunders, 2017).
The inclusion of accelerometry to provide objectively measured PA and SB is the most used method in clinical and epidemiological research (Arvidsson et al., 2019). However, accelerometry has not been widely used to evaluate web and mobile phone-based interventions in adults with T2DM. This may be due to the high cost associated with accelerometers and complex data processing and analysis required (Arvidsson et al., 2019). That said, to most accurately evaluate PA and SB it is integral to include objective measures in future studies. While objective measures provide important data, it is important to include self-report measures to better understand contextual factors related to PA and SB, such as domains and modes of activity. Using a combined measurement approach will provide a more comprehensive understanding of participant behaviors. In addition, further research is needed to determine the relationship between specific study characteristics and outcome measures.
Technologies Used
The focus of this review on web and mobile phone-based interventions for PA and sedentary behavior self-management in adult with T2DM identified four categories of technologies used: web only, mobile phone (application) only, web and mobile phone (application), and web and telephone. While four distinct categories emerged, a common thread remained amongst studies, the incorporation of personalized feedback with education and self-monitoring activities, delivered as either an automated feature based on participant responses or through discussion with peers, professionals, and study facilitators. Hanlon et al. (2017) identified improvements in glycemic control in people with T2DM with telehealth systems that incorporated feedback and some educational and lifestyle interventions. In another systematic review of reviews, the most effective interventions for diabetes self-management were identified as including tailored education, analyzing patient data, and providing individualized feedback (Greenwood, Gee, Fatkin, & Peeples, 2017). Regardless of the type of technology used, providing individualized feedback and using a person-centered design is necessary to engage participants and create sustainable health behavior change.
Rural Populations
This review has demonstrated a lack of research performed in rural communities. Rural adults are disproportionally affected by T2DM, having a 17% higher prevalence rate than urban adults (Massey, Appel, Buchanan, & Cherrington, 2010). Unique barriers faced by rural adults, including long travel distances, cultural barriers, a lack of health care providers, and reduced access to diabetes self-management education (Bolin et al., 2015). Telehealth technologies can be used to improve access to diabetes self-management education in rural adults (Bolin et al., 2015). Due to the increased need and feasibility of web and mobile phone-based interventions, it is necessary to conduct future studies in rural adults with T2DM to better understand the effectiveness in this population.
Limitations
Although a systematic approach was taken, it is possible that relevant studies were missed if they were not indexed in a computerized database. It is unknown if additional research studies were conducted but not published or if any data was excluded from the published studies included. Further, there is a potential for missed studies, due to 10-year limit, use of articles only published in English, and inclusion of only articles available in full-text format. Another limitation of this study is the inclusion of studies that did not have a primary focus on improving PA and/or reducing SBs, with non-specific outcome measures, due to the limited amount of literature published on the topic.
Conclusion
This integrative literature review adds to the literature by identifying positive outcomes for participants who receive PA and/or SB interventions using web and mobile phone-based technologies. This evidence provides integral support for diabetes education practices, elucidating necessary evidence to drive the use of web and mobile phone-based PA and SB strategies, which will improve access to invaluable diabetes self-management resources to diverse populations. It provides evidence of the need for additional studies that are theory driven, targeted specifically towards PA and SB, studies with specified intervention doses, in time or number of telehealth visits, and include long-term follow-up with both objective and self-report measures. Further, the need for interventions in rural populations has been revealed.
Funding Information
The work for this study was supported in part by the National Institute for Health [Grant Number T32NR025426] awarded to the Sinclair School of Nursing, University of Missouri.
Footnotes
Conflict of Interest
The authors declare no conflicts of interest.
References
- Akinci B, Yeldan I, Satman I, Dirican A, & Ozdincler AR (2018). The effects of internet-based exercise compared with supervised group exercise in people with type 2 diabetes: A randomized controlled study. Clinical Rehabilitation, 32(6), 799–810. doi: 10.1177/0269215518757052 [DOI] [PubMed] [Google Scholar]
- American Diabetes Association. (2016). Physical activity/exercise and diabetes: a position statement of the American diabetes association. Diabetes Care, 39, 2065–2079. doi: 10.2337/dc16-1728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Diabetes Association. (2019a). Glycemic targets: Standards of medical care in diabetes – 2019. Diabetes Care 2019, 42(1), s61–s70. doi: 10.2337/dc19-s006 [DOI] [PubMed] [Google Scholar]
- American Diabetes Association. (2019b). Improving care and promoting health in populations: standards of medical care in diabetes – 2019. Diabetes Care, 42(1), s7–s12. doi: 10.2337/dc19-s001 [DOI] [PubMed] [Google Scholar]
- American Diabetes Association. (2019c). Lifestyle management: Standards of medical care in diabetes – 2019. Diabetes Care, 42(1), s7–s12. doi: 10.2337/dc19-s005 [DOI] [PubMed] [Google Scholar]
- Arvidsson D, Fridolfsson J, & Borjesson M (2019). Measurement of physical activity in clinical practice using accelerometers. Journal of Internal Medicine, 286, 137–153. doi: 10.1111/joim.12908 [DOI] [PubMed] [Google Scholar]
- Bolin JN, Bellamy G, Ferdinand AO, Kash BA, & Helduser JW (2015). Rural healthy people 2020 (Vol. 1). College Station, Texas: Texas A&M Health Science Center School of Public Health, Southwest Rural Research Center. [Google Scholar]
- Centers for Disease Control and Prevention. (2020). National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services. Retrieved from https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf [Google Scholar]
- Chang HY, Chang HL, Chen AC, & Yen CH (2018). The impact of m-health on self-management of diabetes: A preliminary study. Studies in Health Technology and Informatics, 252, 39–44. doi: 10.3233/978-1-61499-890-7-39 [DOI] [PubMed] [Google Scholar]
- Connelly J, Kirk A, Masthoff J, & MacRury S (2013). The use of technology to promote physical activity in type 2 diabetes management: A systematic review. Diabetic Medicine, 30, 1420–1432. doi: 10.1111/dme.12289 [DOI] [PubMed] [Google Scholar]
- Connelly J, Kirk A, Masthoff J, & MacRury S (2017). A website to promote physical activity in people with type 2 diabetes living in remote or rural locations: Feasibility pilot randomized controlled trial. Journal of Medical Internet Research Diabetes, 2(2), e26. doi: 10.2196/diabetes.6669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Kurz D, King D, Dickman JM, Faber AJ, Halterman E, … Ritzwoller D (2010). Outcomes of minimal and moderate support version of an internet-based diabetes self-management support program. Journal of General Internal Medicine, 25(12), 1315–1322. doi: 10.1007/s11606-010-1480-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Kurz D, King D, Dickman JM, Faber AJ, Halterman E, … Ritzwoller D (2012). Twelve- month outcomes of an internet-based diabetes self-management support program. Patient Education and Counseling, 87(1), 81–92. doi: 10.1016/j.pec.2011.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwood DA, Gee PM, Fatkin KJ, & Peeples M (2017). A systematic review of reviews evaluating technology-enabled diabetes self-management education and support. Journal of Diabetes Science and Technology, 11(5), 1015–1027. doi: 10.1177/1932296817713506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanlon P, Daines L, Campbell C, McKinstry B, Weller D, & Pinnock H (2017). Telehealth interventions to support self-management of long-term conditions: A systematic metareview of diabetes, heart failure, asthma, chronic obstructive pulmonary disease, and cancer. Journal of Medical Internet Research, 19(5), e172. doi: 10.2196/jmir.6688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansel B, Giral P, Gambotti L, Lafourcade A, Peres G, Filipecki C, … Roussel R (2017). A fully automated web-based program improves lifestyle habits and HbA1c in patients with type 2 diabetes and abdominal obesity: randomized trial of patient e-coaching nutritional support (the ANODE study). Journal of Medical Internet Research, 19(11), e360. doi: 10.2196/jmir.7947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings CA, Vandelanotte C, Caperchione CM, & Mummery WK (2014). Effectiveness of a web-based physical activity intervention for adults with type 2 diabetes – a randomized controlled trial. Preventative Medicine, 60, 33–40. doi: 10.1016/j/ypmed.2013.12.011 [DOI] [PubMed] [Google Scholar]
- Kongstad MB, Valentiner LS, Ried-Larsen M, Walker KC, Juhl CB, & Langberg H (2019). Effectiveness of remote feedback on physical activity in persons with type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Journal of Telemedicine and Telecare, 25(1), 26–34. doi: 10.1177/1357633X17733772 [DOI] [PubMed] [Google Scholar]
- Kooiman TJM, de Groot M, Hoogenberg K, Krijnen WP, van der Schans CP, & Kooy A (2018). Self-tracking of physical activity in people with type 2 diabetes: A randomized controlled trial. Computers, Informatics, Nursing, 36(7), 340–349. doi: 10.1097/CIN.0000000000000443 [DOI] [PubMed] [Google Scholar]
- Liebreich T, Plotnikoff RC, Courneya KS, & Boule N (2009). Diabetes netPLAY: a physical activity website and linked email counselling randomized intervention for individuals with type 2 diabetes. International Journal of Behavioral Nutrition and Physical Activity, 6(18), 1–15. doi: 10.1186/1479/5868-6-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J, Thompson TJ, Cheng YJ, Zhuo X, Zhang X, Zhang P, … Rolka DB (2018). Projection of the future diabetes burden in the United States through 2060. Population Health Metrics, 16(9), 1–9. doi: 10.1186-s12963-018-0166-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig K, Green M, Ritter PL, Jernigan VBB, Laurent DD, Case S, & Plant K (2010). Online diabetes self-management program: A randomized study. Diabetes Care, 33(6), 1275–1281. doi: 10.2337/dc09-2153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig K, Ritter PL, Turner RM, English K, Laurent DD, & Greenberg J (2016). A diabetes self-management program: 12-month outcome sustainability from a nonreinforced pragmatic trial. Journal of Medical Internet Research, 18(12), e322. doi: 10.2196/jmir.6484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher CG, Sherrington C, Herbert RD, Moseley AM, & Elkins M (2003). Reliability of the PEDro scale for rating quality of randomized controlled trials. Physical Therapy, 83, 713–721. [PubMed] [Google Scholar]
- Martin A, Fitzsimons C, Jepson R, Saunders d. H., van der Ploeg HP, Teixeira PJ, … EuroFIT consortium. (2015). Interventions with potential to reduce sedentary time in adults: Systematic review and meta-analysis. British Journal of Sports Medicine, 49(16), 1056–1063. doi: 10.1136/bjsports-2014-094524 [DOI] [PubMed] [Google Scholar]
- Massey CN, Appel SJ, Buchanan KL, & Cherrington AL (2010). Improving diabetes care in rural communities: An overview of current initiatives and a call for renewed efforts. Clinical Diabetes, 28(1), 20–27. doi: 10.2337/diaclin.28.1.20 [DOI] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & The PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLos Med, 6(7), e1000097. doi: 10.1371/journal.pmed1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton NA (2009). The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Australian Journal of Physiotherapy, 55, 129–133. [DOI] [PubMed] [Google Scholar]
- Muller I, Rowsell A, Stuart B, Hayter V, Little P, Ganahl K, … Yardley L (2017). Effects of engagement and health literacy outcomes of web-based materials promoting physical activity in people with diabetes: An international randomized trial. Journal of Medical Internet Research, 19(1), e21. doi: 10.2196/jmir.6601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poppe L, de Bourdeaudhuij I, Verloigne M, Shadid S, van Cauwenberg J, Compernolle S, & Crombez G (2019). Efficacy of a self-regulation-based electronic and mobile health intervention targeting an active lifestyle in adults having type 2 diabetes and adults aged 50 years or older: Two randomized controlled trials. Journal of Medical Internet Research, 21(8), e13363. doi: 10.2196/13363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince SA, Adamo KB, Hamel ME, Hardt J, Gorber SC, & Tremblay M (2008). A comparison of direct versus self-report measures for assessing physical activity in adults: A systematic review. International Journal of Behavioral Nutrition and Physical Activity, 5(56), 1–24. doi: 10.1186/1479-5868-5-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince SA, LeBlanc AG, Colley RC, & Saunders TJ (2017). Measurement of sedentary behaviour in population health surveys: A review and recommendations. PeerJ, 5(e4130), 1–22. doi: 10.7717/peerj.4130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince SA, Saunders TJ, Gresty K, & Rei RD (2014). A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: A systematic review and meta-analysis of controlled trials. Obesity Reviews: An Official Journal of the International Association for the Study of Obesity, 15(11), 905–919. doi: 10.1111/obr.12215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson CR, Buis LR, Janney AW, Goodrich DE, Sen A, Hess ML, … Piette JD (2010). An online community improves adherence in an internet-mediated walking program. Part 1. results of a randomized controlled trial. Journal of Medical Internet Research, 12(4), e71. doi: 10.2196/jmir.1338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan C (2018). Computer and Internet Use in the United States: 2016. American Community Survey Reports. Washington, D.C., U.S. U.S. Census Bureau. [Google Scholar]
- Tuckson RV, Edmunds M, & Hodgkins ML (2017). Telehealth. The New England Journal of Medicine, 377(16), 1585–1592. doi: 10.1056/NEJMsr1503323 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2018). Physical Activity Guidelines for American (2nd ed.). Washington, D.C., U.S. Department of Health and Human Services. [Google Scholar]
- Van der Weegen S, Verwey R, Spreeuwenberg M, Tange H, Van der Weijden T, & de Witte L (2015). It’s life! mobile and web-based monitoring and feedback tool embedded in primary care increases physical activity: A cluster randomized controlled trial. Journal of Medical Internet Research, 17(7), e184. doi: 10.2196/jmir.4579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhagen AP, de Vet HCW, de Bie RA, Kessels AGH, Boers M, Bouter LM, & Knipschild PG (1998). The delphi list: A criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by the delphi consensus. Journal of Clinical Epidemiology, 51(12), 1235–1241. [DOI] [PubMed] [Google Scholar]
- Verwey R, Van der Weegen S, Spreeuwenberg M, Tange H, Van der Weijden T, & de Witte L (2014). A pilot study of a tool to stimulate physical activity in patients with COPD or type 2 diabetes in primary care. Journal of Telemedicine and Telecare, 20(1), 29–34. doi: 10.1177/1357633X13519057 [DOI] [PubMed] [Google Scholar]
- Yom-Tov E, Feraru G, Kozdoba M, Mannor S, Tennenholtz M, & Hockberg I (2017). Encouraging physical activity in patients with diabetes: Intervention using a reinforcement learning system. Journal of Medical Internet Research, 19(10), e338. doi: 10.2196/jmir.7994 [DOI] [PMC free article] [PubMed] [Google Scholar]


