The American Medical Association recently released a statement defining health equity as “optimal health for all,” and affirming the organization’s commitment to promote better health care access, diversity in the healthcare workforce, understanding of the social determinants of health, and equitable distribution of resources and high quality care.1 Unfortunately, according to a World Health Organization report in 2015, approximately 400 million individuals globally lack access to at least one of seven essential health services as a result of workforce shortages and uneven distributions of healthcare workers.2 In a statement published in 2001, the Institute of Medicine declared that “All health care organizations, professional groups, and private and public purchasers should adopt as their explicit purpose to continually reduce the burden of illness, injury, and disability, and to improve the health and functioning of the people of the United States.”3
Rural America
One in five individuals living in the United States resides in a rural area.4 Figure 1 depicts the distribution across the United States of urban clusters, defined by a population of 2,500 to less than 50,000 people, and urbanized clusters, defined by a population in excess of 50,000 people.5 In 2010, of approximately 4000 rheumatologists practicing in the US, 90% were in metropolitan regions (labor market areas centered on an urbanized cluster), 3% in micropolitan (labor market areas centered on an urban cluster), and 7% in rural parts of the US.5,6 In urban clusters, many patients travel in excess of 100 miles to see a rheumatologist.6 Interestingly, despite the declining rural population and pullulating urban population, and despite the greater density of physicians in more populous regions, the physician-to-patient ratio remains disparate and inadequate.
Figure 1.
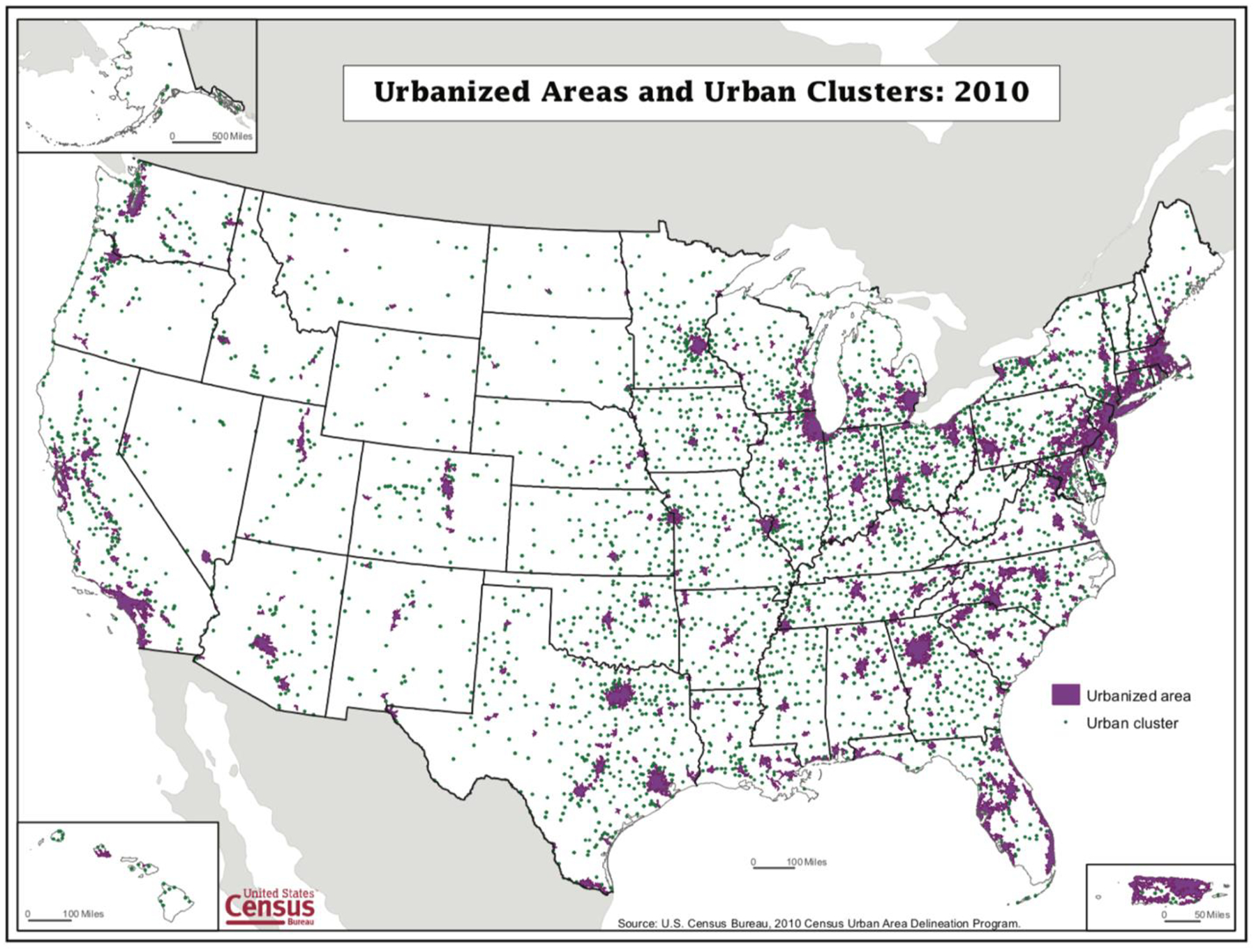
Urbanized Areas and Urban clusters, defined by population of 50,000 or more and 2,500 to less than 50,000, respectively5
In 2015, the American College of Rheumatology Workforce Study iterated that the percentage of internal medicine residents entering rheumatology has remained stable at approximately 4% from 2005 to 2015.7,8 With a retiring baby-boomer population of physicians, the challenge is the estimated disproportionate decrease of supply compared to demand for rheumatology services. With a baseline clinical full-time equivalent (FTE) of 4,997 in 2015, the 2025 projected supply will decrease by 27% to 3,645 FTE and the 2030 projected supply will further decrease by 30% from baseline to 3,455 FTE (Figure 2).8 There is also a significant shortage of pediatric rheumatologists. For the nearly 300,000 children with arthritis in the United States,9 we have less than 350 board-certified and practicing pediatric rheumatologists, 8 states without a single board-certified and practicing pediatric rheumatologist, and 4 states with only one.10 Interestingly, there is a significantly higher concentration of adult rheumatology training programs in the Northeast and Mid-Atlantic regions compared to areas west of the Mississippi (with the exception of California, Figure 3). These findings are in line with a study published by the American Association of Medical Colleges in early 2018 stating the projected shortage of physicians in the United States of approximately 43,000 to 121,000 by 2030.11 This same study demonstrated that, if individuals living in non-metropolitan areas and those without insurance utilized healthcare in the same way as those insured individuals living in metropolitan areas, the United States would have needed more than 30,000 additional physicians. While this may certainly represent, to some degree, overuse of the healthcare system in urban areas, there is no question of limited access to quality healthcare in rural areas. The Health Resources and Services Administration (HRSA) designates “Medically Underserved Areas” (MUAs), as areas with a shortage of primary care health services, high infant mortality, high poverty or a high elderly population,12 and Health Professional Shortage Areas (HPSAs), as geographic areas, facilities or populations with shortages of primary medical care, dental or mental health providers.12 and highlights the need for increased resource allocation in these areas. What is, however, less discussed, is the value and importance of medical education in these underserved areas.
Figure 2.
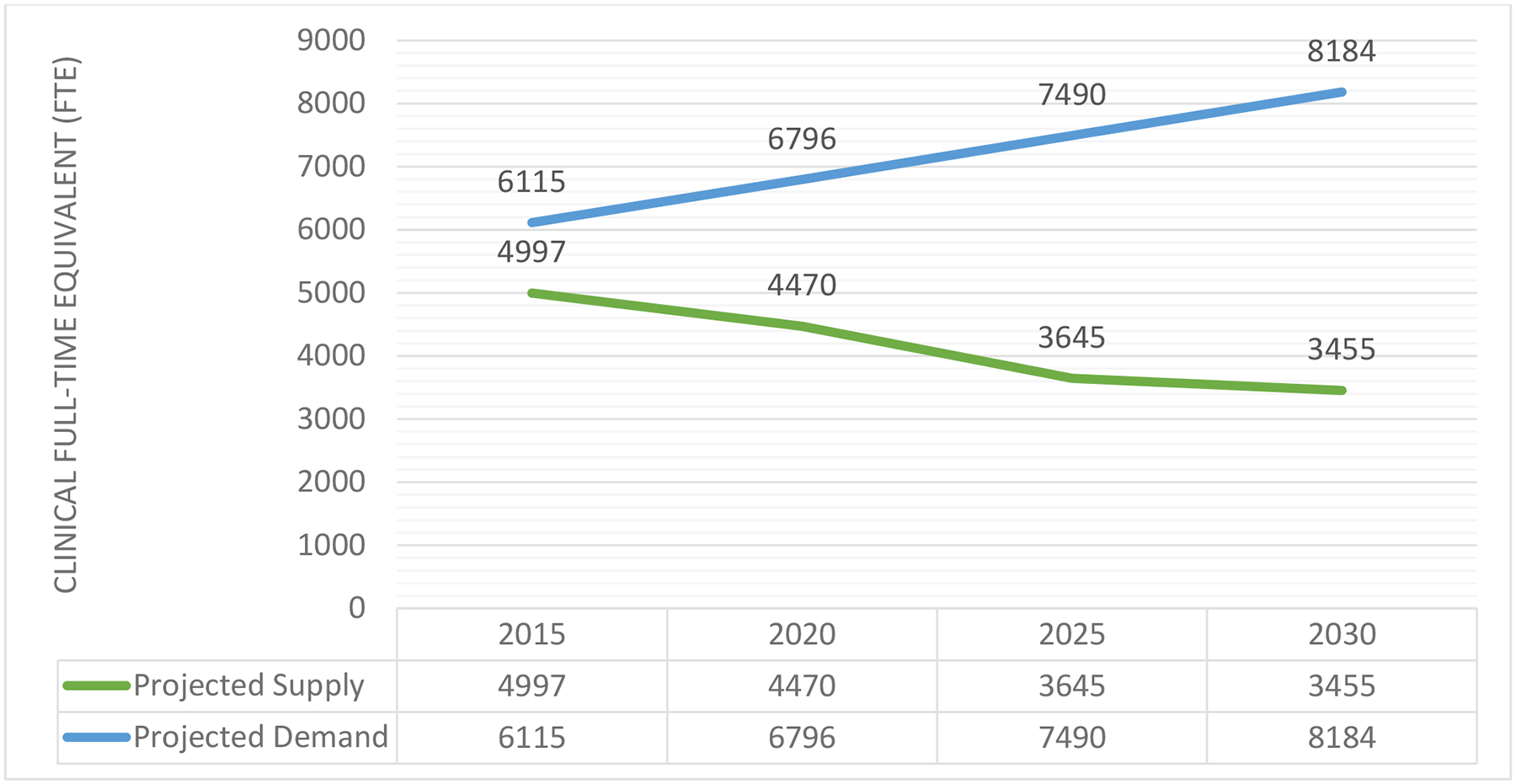
Supply and Demand of Adult Rheumatologists in the United States (clinical FTE), adapted from the ACR’s 2015 Rheumatology Workforce Study
Adapted from ACR 2015 Workforce Study Report8
Figure 3.
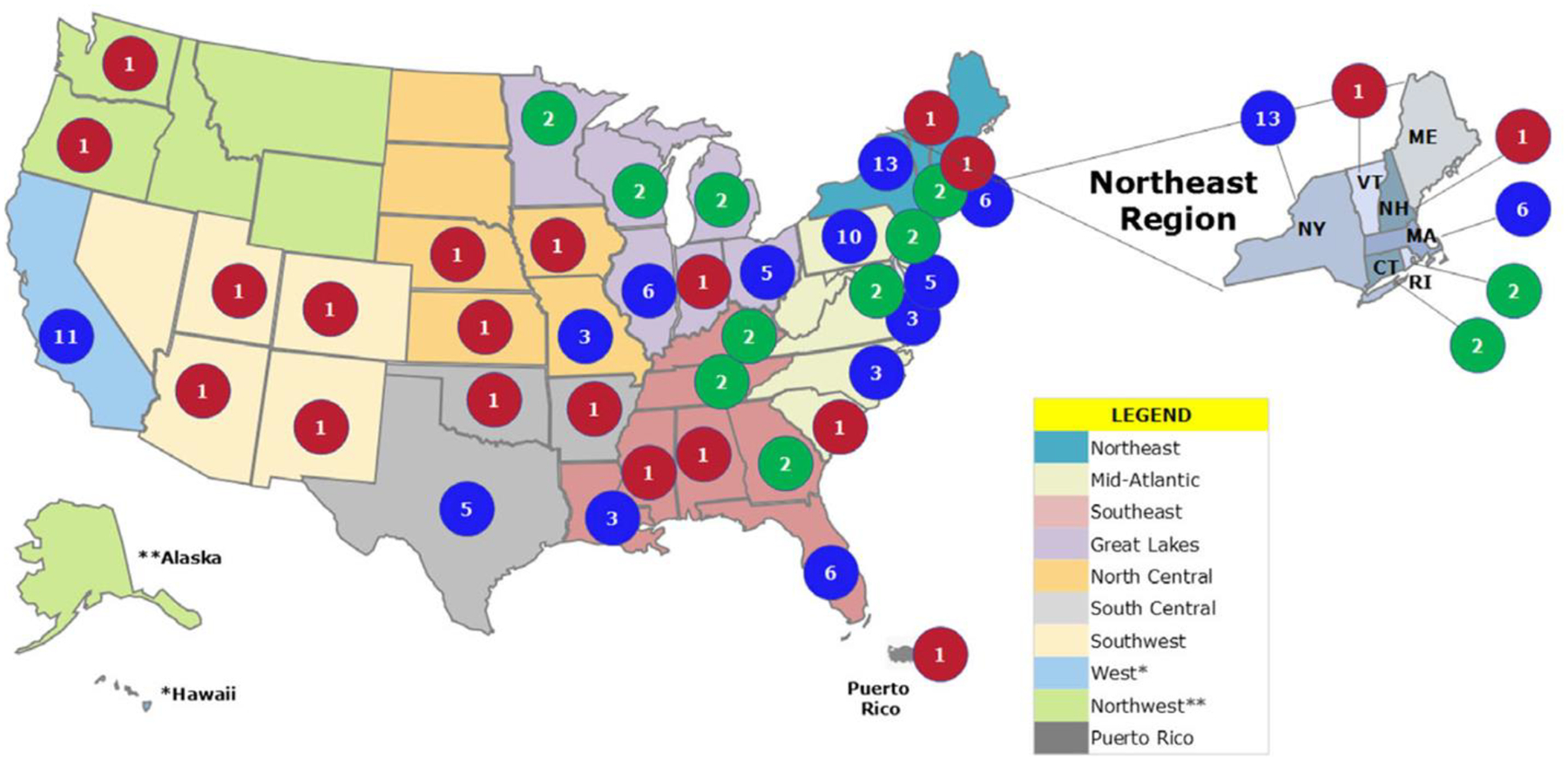
Number of adult rheumatology training programs in each US state in 2015.10
The responsibility of health equity: addressing workforce shortage
The National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP) states “Health equity is achieved when every person has the opportunity to ‘attain his or her full potential’ and no one is ‘disadvantaged from achieving this potential because of social position or other socially determined circumstances.’”13 Disparities in life expectancy, quality of life, rates of morbidity and mortality, disease severity and access to care, result in health inequities. To begin to address this, the Centers for Disease Control and Prevention (CDC) established programs like REACH – Racial and Ethnic Approaches to Community Health – which funds culturally appropriate interventions to reduce preventable risk behaviors such as poor nutrition and smoking.13
Achieving health equity requires a proper understanding of the community context. In underserved communities in particular it is important to appreciate the regional needs to provide high quality healthcare. It is in part the responsibility of health professional schools to train high-quality healthcare providers in underserved regions. Ferguson et al14 and Ko et al15 demonstrated that a student’s training, including their medical education experience, bears a large impact on the student’s intention to practice in an MUA.
Medical Training: Expanding to Medically Underserved Areas
Increasing residency and fellowship positions, as well as salary support through grant programs will certainly help with the physician shortage crisis we are experiencing. Federally Qualified Health Centers are community-based organizations that provide primary and preventive care services typically to MUAs. Involvement of specialty services like rheumatology in these organizations will provide an increase in healthcare access. This need for rheumatologic care was examined through surveys sent to Massachusetts community health center physician medical directors where >50% of directors felt that their patients needed better access to rheumatologic care.16 The majority of providers were uncomfortable starting a disease-modifying antirheumatic drug or immunosuppressive medication and language differences and insurance status were deemed as barriers to obtaining appropriate rheumatologic care.16 Placing trainees, including residents and fellows, in MUAs and HPSAs would then increase the likelihood of physician retention in both primary and subspecialty care, as residents tend to practice close to where they train.17
Socioeconomic incentives will also improve physician likelihood of practicing in rural settings. This can be carried out by increased federal funding for programs such as the Conrad 30 Waiver Program, Title VII/VIII workforce development, the National Health Service Corps, and similar programs directed toward encouraging provision of health services to underserved communities, particularly places where shortages of subspecialists exist.
Telemedicine
An emerging field of healthcare, telemedicine provides an alternative approach to enhancing both physician education and patient access to healthcare with a focus on MUAs and HPSAs. Chase and colleagues first reported the use of telemedicine in rheumatology at the Texas state prison where a remote-site examiner (physician on-site at the prison) was assigned as the “presenter”.18 While the study concluded that providers and prison staff were satisfied with the service and the consults were “equal” to on-site evaluation by a rheumatologist, critics note the concern with relying on proxy examinations by presenters with different levels of training.20–22 An additional factor that comes into play is the cost of equipment needed for telemedicine presentation and transmission to a specialist. According to a systematic review by McDougall and colleagues looking at 20 studies on the use of telemedicine in rheumatic diseases, the majority demonstrated cost-effectiveness but was noted that additional studies are warranted to justify its implementation for the diagnosis and management of rheumatic disease.22 In particular, diagnosing a new condition may require greater confidence in the physical examination, as well as identifying which rheumatic disease would most benefit from telemedicine services is warranted.22
Because of the scarcity of board-certified and practicing pediatric rheumatologists, telemedicine appears to be an excellent option for enhancing patient access. In a rural MUA in northern California, barriers in access to subspecialty care included traveling for more than 1 hour for appointments, missing work for appointments, and relying on emergency room visits.23 Provision of telemedicine consultations on 55 children with special healthcare needs in this same area resulted in a high satisfaction with telemedicine in providing accessible, family-centered and well-coordinated care with healthcare providers.23 However, in a separate study evaluating patient barriers to accessing pediatric rheumatologic care, in-person visits were preferred by 95% over the option of telemedicine, even in cases where travel to the pediatric rheumatology clinic exceeded 3 hours (28%).24
In telemedicine, an additional opportunity to be noted is for provider education. An example of this is Project Extension for Community Healthcare Outcomes (ECHO), where primary care providers in local communities are linked with specialists from academic institutions who provide feedback and mentoring to provide high quality care to patients with otherwise limited access to specialty services.25 Through telemedicine and internet-based tools, providers (nurse practitioners, primary care providers, physician assistants, pharmacists, and more) present patients through video- or telephone-conferencing in a patient-centered case-based format to university specialists. This method of patient care not only enhances the community-based provider’s medical knowledge but also bears potential to affect upon feelings of professional stagnation and isolation with excess workloads and lack of access to consultation services; all recipes for accelerated burnout. In addition, this is a capacity-building approach and strengthens the skills and knowledge of existing providers rather than relying on external, visiting volunteers that may be less sustainable.
Another approach to utilizing communication networks to improve patient access to healthcare services is electronic consultations – “e-consults.” E-consults are “an asynchronous communication between healthcare providers that occurs within a shared electronic health record or secure web-based platform.”26 While not designed for routine chronic care, e-consults may be helpful in triaging consultations from referring providers to specialists, who may either answer a clinical question, request additional information and/or schedule a face-to-face appointment. In addition to improving healthcare access, healthcare utilization services may be optimized by minimizing no-show rates, ensuring diagnostic testing is complete at the time of consultation services, and inclusion of learners in the e-consult experience will provide an avenue of medical learning that is likely to play a large role in healthcare in the coming years.
J-1 Visa Waiver Program
The J-1 visa waiver is a program typically handled by the US Department of Health and Human Services and/or the US Department of Veterans Affairs. Individuals carrying a J-1 visa are subject to a two-year home-country physical presence requirement if they participated in a program to receive graduate medical education or training.27 This requires a J-1 visa holder to return to their home country for a total of at least 2 years (cumulatively). Until this requirement is fulfilled, their J-1 visa status cannot be changed to an H-visa (nonimmigrant temporary worker) or intracompany transferee (L), nor can they receive an immigrant visa, a temporary worker (H), or fiancé (K) visa.27 However, through the US Citizenship and Immigration Services, a waiver may be requested by a designated State Public Health Department (or its equivalent) in what’s known as the Conrad State 30 Program, an opportunity limited to 30 waivers per department per federal fiscal year.27 If a medical graduate (typically after completing a portion of training i.e. residency/fellowship) has an offer of full-time employment for 40 hours a week for at least 3 years and is willing to begin employment within 90 days of receiving a waver in a designated HPSA or a facility serving patients from such an area, he or she can apply for the Conrad State 30 Program.27 Because more than 30% of rheumatology fellows in training are non-US medical school graduates,28 increasing the number of J-1 waiver slots in MUAs, as well as providing better resources for renewing visas in these individuals would likely help the ongoing shortage of rheumatologists.
The National Health Service Corps
The National Health Service Corps (NHSC) provides financial support through scholarships and loan repayment after graduation from some form of schooling for health professionals who provide primary care services in HPSAs.29 More than 50,0000 health professionals have served in the NHSC since 1972 and, with nearly 11,000 current members, the NHSC provides services to more than 11 million people at more than 5,000 urban, rural and tribal sites. The program enables health professionals who might have personal financial limitations to deliver care in MUAs and HPSAs. Additional resources offered by the NHSC include funding for more than 1,000 NHSC scholars who are currently either in school or residency.29
Benefits of Training in Medically Underserved Areas and Socially Accountable Health Professional Education
The Health Professional Schools in Service to the Nation Program was designed to reform medical education curriculum by defining service learning as “a structured learning experience that combines community service with explicit learning objectives, preparation and reflection,” enabling students to “provide direct community service but also to learn about the context in which service is provided, the connection between their service and their academic coursework, and their roles as citizens.”30 Twenty institutions participated in this program from 1995 to 1998 through the Center for the Health Professions at the University of California at San Francisco. On evaluation at the second year of the program’s commencement, service learning was deemed a powerful tool for influencing students in their outlook on the role of service in their lives as healthcare professionals.31 Additionally, community partners valued the ability to establish partnerships with academic institutions, particularly when their key role in shaping the education of these future healthcare professionals was recognized.31 Socially accountable health professional education programs are along this spectrum of service learning designed to connect medical education curriculum with research and service that is unique to the needs of the population they serve.32,33 It is through this community-based medical education that students are immersed within the community of their medical practice.34 These communities are essentially two-way streets of medical students learning through community immersion and the community learning through quality healthcare provision. Such community placements have demonstrated positive impacts on student competencies, including better clinical skills compared to those students learning in more traditional urban hospital-based settings.35
Student-run free clinics (SRFC) are another example of community-based medical education whereby health professional students offer free health services under the supervision of licensed healthcare professionals. The University of California, San Diego established the Student-Run Free Clinic Project to incorporate a curriculum of didactics in the philosophy and approach to working at a free clinic with taking on administrative and clinical roles in managing the clinic in the first two years of medical school followed by a primary-care clerkship experience in their third and fourth years.36 Loma Linda University has a program entitled “Street Medicine,” where students, under the supervision of licensed healthcare professionals, provide medical checkups, drug counseling, flu shots and routine medical care to homeless populations of San Bernardino, California.37
Graduate medical education offered in MUAs range from electives to clerkships and longitudinal tracks or pathways. Some schools offer a 4-year longitudinal track directed toward healthcare provision in underserved areas with a curriculum that is immersed within the community, including community-based projects and didactic seminars.38–39 The Albert Schweitzer Fellowship Program is an example of an extracurricular fellowship program funding leadership skills education and a health service project in the community.40 Another example is the Brigham and Women’s Hospital’s residency in global health equity, established in 2004 as a combined 4-year internal medicine residency with an advanced study of public health.41
The international consortium of Training for Health Equity Network has established global institutions set forth to carry out an integration of health professional education to meet local needs and undertake research that is meaningful to the community.42 This consortium evaluates the institutions through “The Framework for Social Accountability in Health Workforce Education,” which helps health professional schools to restructure and evaluate their programs to comply with goals of attaining health equity worldwide.42 In the Philippines, the socially accountable health professions education program, Ateneo de Zamboanga University School of Medicine (ADZU-SOM), has implemented these approaches, yielding not only a 55% increase in the number of municipalities in Zamboanga with a doctor, but also a decline in the under-five mortality from 89 per 1000 live births to 8 per 1000 since the initiation of the program.43
The Accreditation Council for Graduate Medical Education (ACGME) mandates all programs to teach trainees about health disparities. Interestingly, however, in a study exploring the perception of rheumatology fellows on their experience with health disparities education, it was noted that there was no formal health disparities curriculum and inadequate teaching of how to address health disparities in their patients.38 When five focus groups were established in New York and Pennsylvania to query fellows’ experiences with health disparities in their practices, 25 fellows in total endorsed feeling overwhelmingly frustrated with an inability to do enough for their patients – specifically not knowing what to do to address the disparities at hand.44 Additionally, fellows denied clear curriculum or training in addressing health disparities and reported lacking role models that regularly address health disparities.44 These findings emphasize the importance of establishing rheumatology-specific curriculum incorporated with service learning and community-based learning as approaches to formally train learners that will ultimate advocate for patients affected most by health disparities.
The Lupus Initiative’s (TLI) Teaching Fellows in Lupus Project is a program through which rheumatology fellows provide seminars to frontline primary care providers on the diagnosis and management of lupus.45 Since its inception in 2015, more than 900 non-rheumatologist providers have attended such seminars led by rheumatology fellows from 11 rheumatology programs in the US and Canada. In reviewing responses from 660 providers asked to evaluate these seminars, reported gains were noted in knowledge, confidence in lupus competencies, and overall success of rheumatology fellows as lupus educators – specifically that 96% of responding providers were satisfied with the seminar content.46 A similar program by TLI is the Expert Outreach Project, which provides online lupus education modules for rheumatology professionals to maintain rheumatology board certification (CARE:Lupus).47
Research in MUAs
Federal funding through programs like the Office of Minority Health Lupus Grants aim to begin the process of eliminating racial/ethnic disparities in adverse outcomes in rheumatic diseases, and specific in lupus.48 In one such project,, researchers across the United States will be developing culturally and linguistically appropriate education programs to encourage recruitment and enrollment in clinical trials as well as establishing education modules that are innovative and effective in improving confidence and provision of high quality healthcare by health care providers.48 Similarly the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) with joint efforts from other NIH components like the Office of Research on Minority Health, Office of Research on Women’s Health, Office of Disease Prevention, and with the Centers for Disease Control and Prevention, the Arthritis Foundation and the American College of Rheumatology express a commitment to addressing disparities of rheumatic disease in MUAs and HPSAs. Such programs not only encourage education and community-based research in MUAs and HPSAs to reduce barriers and improve health outcomes.
Discussion
In rheumatology, education and work in underserved areas is particularly important because of the racial/ethnic and socioeconomic disparities that exist in different rheumatic diseases in disease onset, burden, disease course, response to therapies, and long-term outcomes. The onus is on medical education institutions to train students to serve vulnerable communities to improve both healthcare access and the quality of medical school education.
Medical literature worldwide has repeatedly demonstrated a shortage of primary care and subspecialty providers in underserved regions. However, the value of education provided in and around MUAs and HPSAs is underrecognized. When health disparities are formally included in medical education curricula and the culture of medical education shifts to a service learning and community-based learning approach, patients and providers will reap the benefits. Improved healthcare capacity yields potential to improved healthcare quality services otherwise unattainable or difficult to attain, minority involvement in research will likely increase, and learners will possess a sense of understanding of health disparities that will allow for sustainable advocacy in the field with the ultimate goal of eliminating disparities altogether.
Synopsis:
The shortage of healthcare professionals is projected to worsen in the coming years. This is particularly concerning in underserved areas that are fraught with disparities in disease outcomes and life expectancy, quality of life, and healthcare access. The onus is on medical education institutions to train students to serve vulnerable communities to improve both healthcare access and the quality of medical school education. When health disparities are formally included in medical education curricula and the culture of medical education shifts to a community-based learning approach, patients and healthcare providers alike will reap the benefits.
Key points:
The disproportionate decrease in supply of rheumatology providers to anticipated demand in the coming years warrants a change in the education system.
Health equity is limited by disparities in life expectancy, quality of life, rates of morbidity and mortality, disease severity and access to healthcare.
Expanding medical training to medically underserved areas increases the likelihood of physician retention in primary and subspecialty care in these areas
Utilizing technologies to expand on healthcare access as well as medical education is a rapidly emerging field of healthcare.
Formal health disparities teaching in medical education curriculum will provide an environment dedicated to service learning in a community-based approach, benefiting patients and learners alike.
Acknowledgements:
NIH/NIAMS P30 AR072577 (VERITY).
Footnotes
Disclosures: The authors have no relevant financial disclosures.
References
- 1.Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US); 2001. [PubMed] [Google Scholar]
- 2.Global reference list of 100 core health indicators: Working version 5. Geneva: World Health Organization; 2014 [Google Scholar]
- 3.Robeznieks A. Health equity commitment being embedded in DNA of AMA’s work. AMA Association: Patient Support & Advocacy. January25, 2019. https://www.ama-assn.org/delivering-care/patient-support-advocacy/health-equity-commitment-being-embedded-dna-ama-s-work?&utm_source=BulletinHealthCare&utm_medium=email&utm_term=012819&utm_content=NON-MEMBER&utm_campaign=article_alert-morning_rounds_daily&utm_uid=&utm_effort.AccessedFebruary 13, 2019. [Google Scholar]
- 4.Ratcliff M, Burd C, Holder K, Fields A. Defining Rural at the US Census Bureau. ACSGEO-1, US Census Bureau, Washington, DC, 2016. [Google Scholar]
- 5.U.S. Census Bureau, Change in Rural and Urban Population Size: 1910–2010, https://www.census.gov/content/dam/Census/library/visualizations/2016/comm/acs-rural-urban.pdf.AccessedJanuary 28, 2019.
- 6.FitzGerald JD, Benford L, Battistone M et al. Regional distribution of adult rheumatologists. Arthritis Rheum 2013December;65(12):3017–25. [DOI] [PubMed] [Google Scholar]
- 7.ACGME. Rheumatology programs academic year 2015–2016. United States https://apps.acgme.org/ads/Public/Reports/ReportRun?ReportId=8&CurrentYear=2017&SpecialtyId=&AcademicYearId=2015.AccessedFebruary 1, 2019.
- 8.Battafarano DF, Ditmyer M, Bolster MB et al. 2015 Workforce Study: Supply and Demand of Adult Rheumatology Workforce, 2015–2030. Arthritis Care & Research 2018; 70(4):617–626. [DOI] [PubMed] [Google Scholar]
- 9.Sacks JJ, Helmick CG, Luo YH et al. Prevalence of and annual ambulatory health care visits for pediatric arthritis and other rheumatologic conditions in the United States in 2001–2004. Arthritis Rheum 2007;57:1439–45. [DOI] [PubMed] [Google Scholar]
- 10.Address Shortage of Pediatric Rheumatologists. https://www.arthritis.org/advocate/our-policy-priorities/access-to-care/increase-access-to-pediatric-rheumatologists.AccessedJanuary 29, 2019.
- 11.American Association of Medical Colleges. (2018). 2018 Update: The Complexities of Physician Supply and Demand: Projections from 2016 to 2030. https://aamc-black.global.ssl.fastly.net/production/media/filer_public/85/d7/85d7b689-f417-4ef0-97fb-ecc129836829/aamc_2018_workforce_projections_update_april_11_2018.pdf.AccessedJanuary 21, 2019.
- 12.MUA Find. https://data.hrsa.gov/tools/shortage-area/mua-find.AccessedJanuary 2, 2019.
- 13.REACH 2018. Division of Nutrition, Physical Activity, and Obesity. https://www.cdc.gov/nccdphp/dnpao/state-local-programs/reach/current_programs/index.html.Reviewed October 3, 2018. AccessedJanuary 29, 2019.
- 14.Ferguson WJ, Cashman SB, Savageau JA et al. Family medicine residency characteristics associated with practice in a health professions shortage area. Residency Education 2009;41(6):405–410. [PubMed] [Google Scholar]
- 15.Ko M, Edeksteub RA, Heslin KC et al. Impact of the University of California Los Angeles/Charles R. Drew University medical education program on medical students’ intention to practice in medically underserved areas. Academic Medicine 2005;80(9):803–808. [DOI] [PubMed] [Google Scholar]
- 16.Feldman CH, Hicks LS, Norton TL, Freeman E, Solomon DH. Assessing the need for improved access to rheumatology care: a survey of Massachusetts community health center medical directors. J Clin Rheumatol. 2013;19(7):361–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Talley RC. Graduate medical education and rural health care. Acad Med 1990;65:522–525. [DOI] [PubMed] [Google Scholar]
- 18.Chase JL, Llsse JR, Brecht RM. Rheumatology in the 21st Century - Telemedicine Leading the Way. Arthritis Rheum 1995; 38:R39–R39. [Google Scholar]
- 19.Sanders PA. Cyberclinic in rheumatology. J R Coll Physicians Lond. 1999; 33:400–401. [PMC free article] [PubMed] [Google Scholar]
- 20.Lewtas J. Telemedicine in rheumatology. J Rheum 2001; 28:1745–1746. [PubMed] [Google Scholar]
- 21.Rothschild B Telerheumatology: not ready for prime time. Intern Med J 2013; 43:468–469. [DOI] [PubMed] [Google Scholar]
- 22.McDougall JA, Ferucci ED, Glover J, Fraenkel L. Telerheumatology: A Systematic Review. Arthritis Care Res (Hoboken) 2017; 69(10): 1546–1557. doi: 10.1002/acr.23153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marcin JP, Ellis J, Mawis R et al. Using Telemedicine to Provide Pediatric Subspecialty Care to Children with Special Health Care Needs in an Underserved Rural Community. Pediatrics 2004;113(1). [DOI] [PubMed] [Google Scholar]
- 24.Bullock DR, Vehe RK, Zhang L, Correll CK. Telemedicine and other care models in pediatric rheumatology: an exploratory study of parents’ perceptions of barriers to care and care preferences. Pediatr Rheumatol Online J. 2017;15(1):55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arora S, Geppert CM, Kalishman S, et al. Academic health center management of chronic diseases through knowledge networks: Project ECHO. Acad Med 2007;82(2):154–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vimalananda VG, Gupte G, Seraj SM, et al. Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare. 2015;21(6):323–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eligibility for a Waiver of the Exchange Visitor Two-Year Home-Country Physical Presence Requirement. https://travel.state.gov/content/travel/en/us-visas/study/exchange/waiver-of-the-exchange-visitor/eligibility.html.AccessedFebruary 18, 2019.
- 28.National Resident Matching Program, Charting Outcomes in the Match, Specialties Matching Service, Appointment Year 2018. National Resident Matching Program, Washington, DC. 2018. [Google Scholar]
- 29.Physician workforce: the special case of health centers and the National Health Service Corps. Am Fam Physician 2005;72(2):235. [PubMed] [Google Scholar]
- 30.Seifer SD. Service-learning: community-campus partnerships for health professions education. Acad Med 1998;73(3):273–277. [DOI] [PubMed] [Google Scholar]
- 31.Gelmon SB, Holland BA, Shinnamon AF. Health Professions Schools in Service to the Nation. Conference Proceedings 1998:8. [Google Scholar]
- 32.Palsdottir B, Neusy A, Reed G. Building the evidence base: networking innovative socially accountable medical education programs. Education for Health 2008;8:177. [PubMed] [Google Scholar]
- 33.Larkins SL, Preston R, Matte MC et al. Measuring social accountability in health professional education: development and international pilot testing of an evaluation framework. Medical Teacher 2013;35:32–35. [DOI] [PubMed] [Google Scholar]
- 34.Magzoub ME, Schmidt HG. 2000. A taxonomy of Community-based Medical Education. Academic Medicine 75:699–707 [DOI] [PubMed] [Google Scholar]
- 35.Chang LW, Kaye D, Muhwezi WW et al. Perceptions and evaluation of a community-based education and service (COBES) program in Uganda. Med Teach 33:e9–e15. [DOI] [PubMed] [Google Scholar]
- 36.Marcin JP, Ellis J, Mawis R et al. Using Telemedicine to Provide Pediatric Subspecialty Care to Children With Special Health Care Needs in an Underserved Rural Community. Pediatrics 2004;113(1). [DOI] [PubMed] [Google Scholar]
- 37.Street Medicine; Loma Linda University Health: https://caps.llu.edu/volunteer-now/street-medicine.AccessedFebruary 18, 2019.
- 38.Huang W, Malinow A. Curriculum and evaluation results of a third-year medical student longitudinal pathway on underserved care. Teach Learn Med 2010;22(2):123–130. [DOI] [PubMed] [Google Scholar]
- 39.Smucny J, Beatty P, Grant W, Dennison T, Wolff LT. An evaluation of the Rural Medical Education Program of the State University of New York Upstate Medical University, 1990–2003. Acad Med. 2005;80(8):733–738. [DOI] [PubMed] [Google Scholar]
- 40.Schweitzer Albert Fellowship.Improving Health. Developing Leaders. Creating Change. http://www.schweitzerfellowship.org/about/ AccessedJanuary 15, 2019. [Google Scholar]
- 41.Doris and Howard Hiatt Residency in Global Health Equity ad Internal Medicine. https://www.brighamandwomens.org/medicine/global-health-equity/hiatt-residency-in-global-health-equity-and-internal-medicine.AccessedFebruary 18, 2019.
- 42.Training for Health Equity Around the World. https://thenetcommunity.org, AccessedDecember 18, 2018.
- 43.Cristobal F, Worley P. Can medical education in poor rural areas be cost-effective and sustainable: the case of the Ateneo de Zamboanga University School of Medicine. Rural Remote Health 2012;12:1835. [PubMed] [Google Scholar]
- 44.Blanco I, Gonzalez C. Current Rheumatology Fellows Experiences with Health Disparities and Disparity Education: A Qualitative Study [abstract] Arthritis Rheumatol 2018; 70(suppl 10). https://acrabstracts.org/abstract/current-rheumatology-fellows-experiences-with-health-disparities-and-disparity-education-a-qualitative-study.AccessedJanuary 30, 2019 [Google Scholar]
- 45.Caron A, Lim SS, Rene L et al. Teaching Fellows in Lupus: Rheumatology Fellows Are Successful Educators in Improving Lupus Recognition By Frontline Healthcare Providers. 2015Arthritis Rheumatol 2015:67. [Google Scholar]
- 46.Fellows Project: Demystifying Lupus. https://thelupusinitiative.org/educators-students/seminars/.AccessedFebruary 18, 2019.
- 47.St. Clair EW. The ACR’s Lupus Initiative Expands Training, Educational Resources. August2015. https://www.the-rheumatologist.org/article/the-acrs-lupus-initiative-expands-training-educational-resources/.AccessedFebruary 18, 2019. [Google Scholar]
- 48.US Department of Health and Human Services Office of Minority Health, Lupus Grants. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=2&lvlid=62.AccessedJanuary 30, 2019.


