Abstract
Individuals with heart failure (HF) typically live in the community and are cared for at home by family caregivers. These caregivers often lack supportive services and the time to access those services when available. Technology can play a role in conveniently bringing needed support to these caregivers. The purpose of this article is to describe the implementation of a virtual health coaching intervention with caregivers of HF patients (“Virtual Caregiver Coach for You”—ViCCY). A randomized controlled trial is currently in progress to test the efficacy of the intervention to improve self-care. In this trial, 250 caregivers will be randomly assigned to receive health information via a tablet computer (hereafter, tablet) plus 10 live health coaching sessions delivered virtually (intervention group; n = 125) or health information via a tablet only (control group; n = 125). Each tablet has specific health information websites preloaded. To inform others embarking on similar technology projects, here we highlight the technology challenges encountered with the first 15 caregivers who received the ViCCY intervention and the solutions used to overcome those challenges. Several adaptations to the implementation of ViCCY were needed to address hardware, software, and network connectivity challenges. Even with a well-designed research implementation plan, it is important to reexamine strategies at every step to solve implementation barriers and maximize fidelity to the intervention. Researcher and interventionist flexibility in adapting to new strategies is essential when implementing a technology-based virtual health coaching intervention.
Keywords: health coach, heart failure, nursing informatics, self-care, telehealth/mHealth, video conferencing
1 |. INTRODUCTION
1.1 |. Family caregivers
Approximately 41 million people in the United States are unpaid family caregivers for an adult at the cost of $470 billion dollars annually (National Alliance for Caregiving & AARP, 2015; Reinhard et al., 2019). These family caregivers—defined as spouses/partners, relatives, and friends who provide a broad range of assistance and support (hereafter, caregivers)—have the majority of the responsibility to care for ill, disabled, and elderly individuals (Family Caregiver Alliance, 2014; Hoefman et al., 2017). Caregivers have more stress, worse health status, poorer self-care, and a higher risk of death than noncaregivers (National Academies of Sciences, Engineering, and Medicine, 2016; Van Houtven et al., 2017). These caregivers often report having to cope with problems alone, thereby accentuating stress and leaving them less motivated to focus on themselves (Dionne-Odom, Demark-Wahnefried, et al., 2017; Wang et al., 2015).
Caregivers of adults living with heart failure (HF) experience many of the same issues as caregivers of adults with other illnesses and conditions. HF patients often have other chronic conditions resulting in complex care regimens that can complicate caregiving (Kitko et al., 2020). The natural disease course for a person with HF is highly variable with a decline in function over a period of time that may be long (Virani et al., 2020). Coping with the patient’s HF symptoms and supporting their own self-care can be difficult for caregivers as the role often involves supervising and monitoring adherence to complicated care management treatments (Alpert et al., 2017; Sevilla-Cazes et al., 2018). The caregiving role is further complicated by comorbidities and functional deficits (e.g., depression, cognitive impairment, physical limitations) and coordinating frequent hospitalizations for the person with HF (Buck et al., 2015; Wingham et al., 2015). Similar to other populations, caregivers of persons with HF often are burdened, stressed, and follow a poor regimen of self-care (Dionne-Odom, Hooker, et al., 2017).
1.2 |. Interventions for caregivers of patients with HF
The few intervention studies conducted with caregivers of patients with HF have focused on improving caregiver burden, stress, or health status (Evangelista et al., 2016; Liljeroos et al., 2017; Pressler et al., 2016; Srisuk et al., 2017). Among these studies, the most common interventions involve psychoeducational approaches based on a variety of methods such as face-to-face sessions, home visits, telephone calls, and/or virtual monitoring (Evangelista et al., 2016). Although some investigators have focused on helping caregivers support patient self-care, none have focused on improving caregiver self-care (Piette et al., 2015; Srisuk et al., 2017).
1.3 |. Using virtual approaches to support caregivers
Successful implementation of potentially effective interventions is impeded when caregivers are homebound with caregiving duties (Grant et al., 2003; Saunders, 2012). Yet, such isolated caregivers may be among the most stressed and in need of support (Hayes et al., 2015). Providing a virtual intervention that is convenient, requires limited time commitment, has no travel costs, is flexible, and can accommodate caregiver preferences, seems like an optimal solution to improve caregiver self-care.
Chi and Demiris (2015), who conducted a review of virtual interventions to support caregivers of both adults and children with a variety of conditions, concluded that caregivers were satisfied and comfortable with virtual support. In another review of eight open-label trials and 16 randomized controlled trials, the authors concluded that Internet-based interventions were effective in reducing caregiver stress and improving caregiver well-being (Hu et al., 2015). This finding is important because caregiving responsibility often confines caregivers to the home in close proximity to the patient with HF, limiting caregivers’ ability to attend in-person sessions (Saunders, 2012).
Developing a support intervention that can be delivered virtually wherever the caregiver maybe is a reasonable approach to supporting caregivers. Although there is literature suggesting a “digital divide” among older adults based on race, ethnicity, and socioeconomic status, technology access among older adults and caregivers has been steadily increasing (Anderson & Perrin, 2017; Yoon et al., 2020; Young et al., 2014). Leveraging the growing availability of technology, broadband accessibility, and overall declining costs of technology, we developed a live, virtual intervention. Given the recent coronavirus pandemic, a technology solution for homebound caregivers is all the more significant and relevant.
1.4 |. Purpose
The purpose of this article is to describe the implementation of a virtual health coaching intervention with caregivers of HF patients (“Virtual Caregiver Coach for You”—ViCCY [pronounced “Vicky”]). The intervention is part of a current randomized controlled trial testing the efficacy of ViCCY to improve self-care. We detail (a) application of the ViCCY health coaching intervention using specific technology, (b) challenges experienced delivering the intended intervention, and (c) solutions the health coaches used to implement the intervention when technological challenges occurred. The early lessons learned can inform others embarking on similar technology interventions about the specifications, procedures, and technology challenges encountered when designing and delivering a virtual intervention.
2 |. DESCRIPTION OF INNOVATION
2.1 |. Testing the virtual caregiver coach for you
In preparation for the trial, three pilot studies were conducted to adapt the intervention for caregivers. We first enrolled seven homebound female spouse caregivers of patients with HF and interviewed them to identify stressors associated with caregiving. The plan for the health coaching intervention was described, all participants were receptive to the electronic intervention, and five of the seven women wanted to participate, indicating they were desperate for help (Sigafus & Riegel, 2010). In the second pilot study, four methods of communication were tested—telephones, tablet computers (iPads) with video, laptop computers with video, and a detachable webcam, and touchscreen videophones. The iPad facilitated privacy by allowing the caregiver to move away from the person with HF while conversing and was preferred over other devices. In the third study, the feasibility of our planned methods was assessed, and we pilot tested the ViCCY intervention (Riegel et al., 2013). Four caregivers of patients with HF (white, female spouses, mean age 66 ± 8.5 years) were each given an iPad. Study interventionists, referred to as health coaches, engaged each caregiver in eight support sessions over a 3-month period. Each session lasted approximately 1 h. Data were collected at enrollment and 3 months later. Technology problems were more common among coaches than caregivers and were quickly resolved with assistance. Together these pilot studies illustrated that caregivers were interested in participating, they were comfortable with the tablet computer technology (hereafter referred to as tablet), and our proposed methods were feasible. We learned to hire health coaches adept with technology and to ensure that participants had a strong Internet connection (Riegel et al., 2013).
The content of the ViCCY intervention is based on the Transactional Model of Stress and Coping (Lazarus & Folkman, 1984). A full description of the theoretical underpinnings of the intervention has been published elsewhere (Riegel et al., 2019). Briefly, the intervention is designed to be delivered over a 6-month period through 10 virtual sessions with a trained health coach. The same coach delivers the intervention for all 10 sessions. The intervention covers evaluating caregiving demand, assessing stressors and coping resources, using self-care to support coping, getting better sleep, recognizing and changing automatic thoughts, learning relaxation techniques, building confidence, and evaluating the implementation and effectiveness of the sessions (Riegel et al., 2019). ViCCY sessions are designed to be provided using video-conferencing technology and can easily be deployed in any location. Periodically two members of the study team review audio recordings from ViCCY intervention health coaching sessions for fidelity to the session content.
2.2 |. Description of a study testing the innovation
The study is designed as a single-center phase II randomized controlled trial in which enrolled caregivers of persons living with HF are randomized into an intervention or control group (Riegel et al., 2019). Caregivers in both the intervention and control group receive a tablet pre-programmed with health information websites (e.g., patient education materials from the Heart Failure Society of America, self-care websites on relaxation and meditation techniques, nutrition, exercise). In addition, caregivers in the intervention group receive ViCCY intervention. Caregivers receive a call at 1-month after enrollment to answer questions about health care resource use and to receive a reminder to use their tablet. At 3, 6, 9 and 12 months after enrollment, caregivers are contacted by phone to complete survey items on self-care, stress, coping strategies, self-rated health, and work status. The specific aims of the trial are to (a) compare the efficacy of ViCCY to standardized health information alone in improving self-care and (b) estimate the cost and cost-effectiveness of the ViCCY intervention. The study is registered with ClinicalTrials.gov (NCT03988621) and the full research protocol description is available online (Riegel et al., 2019).
2.3 |. Study enrollment
A total of 250 caregivers will be enrolled in the trial (125 per group). All participants will be recruited from the largest outpatient HF clinic in southeastern Pennsylvania and from the affiliated academic tertiary medical center’s main hospital. Patients and their caregivers travel from hundreds of miles away to receive care at this outpatient HF clinic. Because the intervention is virtual, there are no restrictions on where the caregivers reside. As of April 30, 2020, 40 caregivers had enrolled in the trial.
Once enrollment and baseline data are collected, caregivers are randomized into groups using a process to achieve equal distribution on key participant characteristics (i.e., gender, relationship to the patient) known to influence perceived caregiving burden and receptivity to interventions (Schrank et al., 2016). The study project manager notifies the caregiver of his or her group assignment (intervention or control) by telephone, email, or message (based on the caregiver’s preference). This trial and evaluation were reviewed and approved by the University of Pennsylvania Institutional Review Board.
2.4 |. Technology
All enrolled caregivers, regardless of group assignment, are provided with a Samsung Galaxy Tab A tablet with an embedded camera capable of full two-way duplex video and real-time audio transmission. To reduce any equity, inclusion, or access barriers, all tablets were set up with mobile connectivity using a major cellular network provider. The Samsung tablet was chosen over the iPad that was tested in the pilot study based on cost. The tablet serves two purposes: (a) provides equal access to the targeted HF and self-care websites and (b) supports providing the virtual health coaching intervention using video conferencing software embedded in the tablet (required bandwidth: 800 kbps/1.0 Mbps for high-quality video; receiving 1080p high definition video requires 2.5 Mbps; sending 1080p high definition video requires 3.0 Mbps).
The tablets for both groups are identical with the same links and software. The tablets are configured so that all other features of the tablet are locked. This choice was based on the belief that tablets with limited function (e.g., blocking all non-study functions: no email, inability to connect to a Wi-Fi network, or search freely on the Internet) would maintain software integrity, deter unwanted use, and increase the likelihood of having the tablet returned after 6 months. All technology is managed by a group hired specifically to purchase and set up the tablets. This technology support team manages the hardware and software purchased for the study tablets, providing team training and ongoing one-on-one consultation with health coaches, remote trouble-shooting, and group support to the team related to the tablets.
2.4.1 |. Using the tablet
Directly after enrollment, all caregivers are given the study tablet. Trained staff provide instructions on how to turn on the tablet, how best to set it up at home (e.g., plugged in charging, case open), how to access the links on the home page (including what to do if they are assigned to the intervention group), and who to contact if they have any problems with the tablet. The study staff also provide the caregiver with a step-by-step manual on the use of the tablet and trouble-shooting guide.
Regardless of group, caregivers are encouraged at enrollment and then at the 1 month during a check-in, a follow-up call to spend a minimum of 30 min each week using the tablet to access the Internet sites on the tablet. In addition, all participants receive digital newsletters pushed out to their tablets, which provide useful self-care information. Time spent accessing the Internet sites is not collected in either group. Each caregiver signs an agreement to keep the tablet in good working order and return it to the study team at the end of the 6-month active intervention. A prepaid postage padded envelope is provided for returning the tablet at the completion of 6 months.
2.5 |. Health coaches
Health coaches are individuals who are credentialed to safely guide clients in behavioral change to promote wellness (Huffman, 2016). Experienced health coaches with skills in health coaching, motivational interviewing, basic knowledge about HF, and comfort using technology were hired to deliver the intervention. To prepare for the role, the three health coaches joined the full study team for a 2-day in-person intensive training about the health coaching intervention. The health coaches were provided with the ViCCY standardized treatment manual that specifies the format and questions to guide each intervention session. In addition, health coaches were trained on how to log into the cloud-based video conferencing platform. They practiced using the intervention virtual conference rooms during the health coaching sessions and accessed websites on tablets provided to the caregivers in the trial. Standardized training and routine study group meetings at 2-week intervals are used to ensure that the intervention is conducted similarly by all the health coaches.
2.6 |. ViCCY intervention
Evidence suggests that delivering an intervention virtually supports building rapport between the health coach and caregiver (Wakefield et al., 2008). The intervention, therefore, is designed to provide 10 virtual support sessions to caregivers, using audio and video, during the first 6 months of the study. Coaching and motivational interviewing are used in all sessions (Huffman, 2014).
ViCCY sessions are provided by Health Insurance Portability and Accountability Act (HIPAA)-compliant video conferencing technology embedded in the tablets. Three separate accounts were created to allow each of the three health coaches to access the video conferencing software. Each account is set up with five unique virtual conference “rooms” that can be used to provide the intervention. The video conferencing platform resides in the cloud. Each coach uses their own computer (PC or MAC) to log into one of the three accounts that provides access to 1 of the 15 virtual conference rooms (3 accounts with 5 rooms each = 15 private virtual conference rooms).
To launch a session, the health coach logs into the secure cloud account from a computer (i.e., laptop or desktop). The health coaches have a list of all the tablets and their assigned virtual conference room number. When a caregiver selects the icon for the virtual conference room on the tablet, the caregiver goes directly into that specific virtual conference room associated with the tablet.
When the health coach is assigned a new caregiver, the health coach contacts the caregiver by phone, email, or text within 2 days to set up the initial session (to occur ideally within 1 week of enrollment). The health coach asks the caregiver how comfortable they are with the tablet and works with the caregiver to test the video conferencing software before the first session. The health coaches are provided with images of what the caregiver sees when using the tablet to assist them with navigation. See Figure 1.
FIGURE 1.
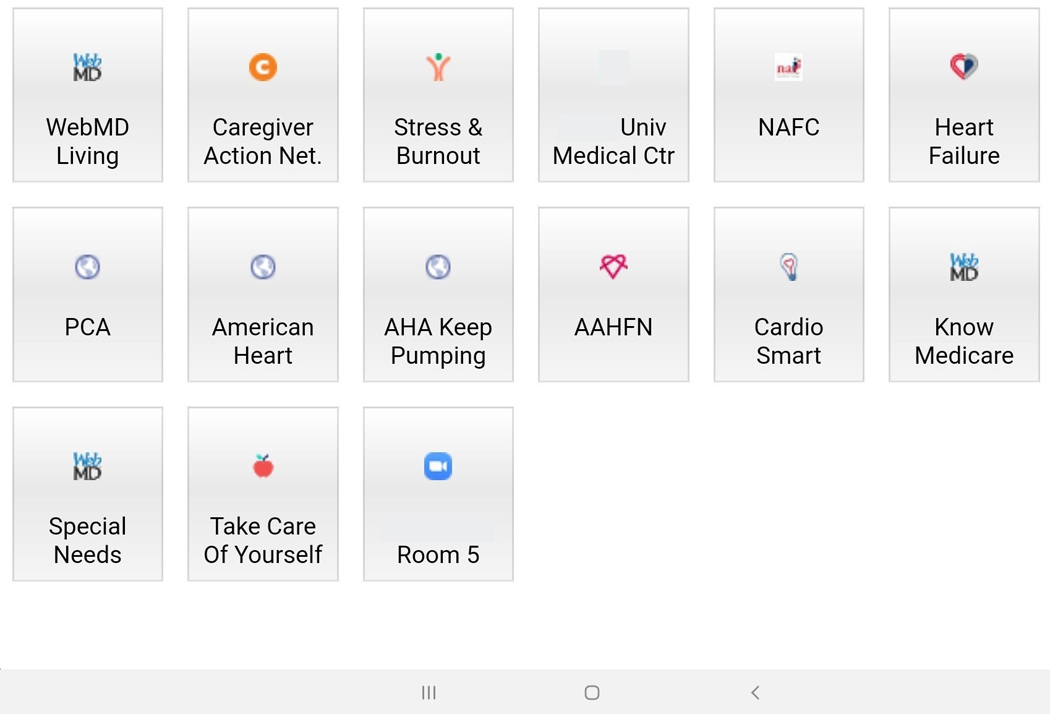
The image is of the home screen on the tablet for all study participants
2.7 |. Intervention session documentation
The health coaches are expected to complete 10 intervention sessions over 6 months. Although originally planned to be front-loaded, because of caregiver scheduling issues, the health coach and caregiver identify a mutually agreed upon schedule (e.g., clustered weekly and then spaced out over the remaining time or scheduled every other week). Health coaches document the total number of completed intervention sessions with each caregiver and take notes on what topics are discussed, details of the session goals, overall perception of how the session went, and rate the session’s audio and video quality (Excellent, Fair, Poor). For any session where the rating was fair or poor, the health coach provides a brief one- to two-sentence comment on what happened and, if the tablet was not used, what technology was used to complete the session (e.g., telephone, cell phone). In addition to the ViCCY intervention session ratings, health coach sessions are discussed in the routine study team meetings. During these meetings, we discuss strategies used to engage caregivers, handle common problems, and alternative strategies used to deliver the intervention.
3 |. IMPLEMENTATION OF THE VICCY INTERVENTION
3.1 |. Intervention sessions
Of the first 21 caregivers assigned to the intervention group, 3 were unable to be reached, 1 decided not to participate in the intervention, and 2 patients died before the caregivers received the complete intervention. Of the 15 caregivers who had the opportunity to receive the intervention, the median number of sessions received was 10 (average: 7, range: 0–11). Although health coaches were available for all sessions, caregivers missed sessions because of the demands of caregiving, the dynamic state of their family member’s illness, and priorities other than research. Six caregivers completed fewer than 10 sessions each due to issues such as lack of time to participate and lack of interest, explaining why 41 of a possible 60 sessions for these 6 caregivers were not completed.
Among the 109 sessions completed, health coaches rated the quality of the video used during a session as poor 44% of the time and use of audio as poor 13% of the time. The average length of a session was 59 min (range = 10–155 min). Table 1 presents the number of sessions completed.
TABLE 1.
Counts of intervention sessions for 15 caregiversa
| Session number | Number of completed health coach sessions |
|---|---|
| 1 | 15 |
| 2 | 14 |
| 3 | 12 |
| 4 | 11 |
| 5 | 9 |
| 6 | 9 |
| 7 | 9 |
| 8 | 9 |
| 9 | 9 |
| 10 | 9 |
| Booster | 3 |
| Total count of sessions | 109 |
Of the first 21 caregivers randomly assigned to the intervention, 6 caregivers completed no sessions for the following reasons: unable to reach the caregiver after enrollment (n = 3), the patient died before the caregiver started the intervention (n = 2), and one caregiver reported wanting a different type of intervention.
Reliable use of the video conferencing technology was a challenge. Overall, the video conferencing software was successfully used for the whole session (n = 28) or most of a session (n = 10) in 38 of 109 sessions. Among the remaining 71 sessions, the health coach had to adapt the implementation of the intervention due to the tablet failing to connect to the network (see Table 2). An adaptation (FaceTime either in addition to starting with the video conferencing software [n = 17] or alone [n = 18]) supported compliance in using virtual technology to deliver the health coaching intervention over two-thirds of the time (73 out of 109 sessions).
TABLE 2.
Audio and video connectivity
| Session technology used | ||
|---|---|---|
| Video conferencing on tablet | N | % |
| Both audio and video (start to finish) | 28 | 25.7 |
| Video for a portion then audio only | 10 | 9.2 |
| Attempted but switched to FaceTime | 17 | 15.6 |
| Attempted but switched to telephone | 7 | 6.4 |
| Total | 62 | 56.9 |
| FaceTime only | 18 | 16.5 |
| Phone only | 29 | 26.6 |
| Total | 109 | 100.0 |
3.2 |. Lessons learned
Examination of the first 21 randomly assigned intervention participants highlights some important lessons learned for scholars embarking on this type of technology-driven research. Three major areas to examine on a continuous basis include connectivity, software maintenance, and hardware issues. Examples of each challenge and potential solutions are presented below.
3.2.1 |. Connectivity
A frequently encountered challenge was achieving or maintaining connectivity. Health coaches reported video sessions dropping connection anywhere from 3 to 30 min into a session. Sometimes the audio remained clear, but the video was lost. Other times the audio and video both stopped working and, when the caregiver tried to reconnect, they were met with the message “no network connection.” For some caregivers, the tablet would not connect to the cellular network to enable the use of the video conferencing software. Rebooting did not resolve the problem.
Solutions
When connectivity was the challenge, the health coaches asked the caregivers to move to a different room or location in his or her home to improve the mobile signal strength. For some caregivers, the ability to change rooms was not feasible (e.g., no place to move to for privacy) and for others, moving rooms did not result in improvement. If they were unable to resolve the problem, to maintain the virtual face-to-face intent of the study protocol, the health coaches offered switching to the iPhone application FaceTime, if the caregiver had an iPhone. This occurred in almost one-third of the sessions (35/109). If the caregiver did not have a compatible smartphone, health coaches offered to skip the video and use the telephone to complete the session. In some cases, if there had been any level of connectivity, the health coaches continued to encourage the use of video conferencing software. If the caregiver was never able to enter the video conferencing session, however, and use of the alternative method worked, all future sessions often migrated to the alternative.
The selected video conferencing software was chosen to provide a private space and a secure setting to deliver the intervention. When the video conference room software worked, the health coaches reported that the sessions ran smoothly, and the quality of the video and audio quality were usually rated as excellent. Likely these issues were directly related to variability in the mobile connectivity of the tablet to the wireless provider. We chose a wireless carrier with a large coverage area, but still encountered problems.
Another possible issue is that the video conferencing software chosen requires 2.5–3.0 Mbps—maximum data transfer rate expressed in bits per second (bps). The level of bandwidth required for high definition video coupled with poor connectivity may be a cause for the challenges experienced by some intervention group caregivers. One solution that we are trying is to use video conferencing software that requires less bandwidth (<2.0 Mbps). For caregivers with an iPhone, the switch to using FaceTime has worked well, most likely due to the caregiver’s iPhone being connected to a local Wi-Fi network.
3.2.2 |. Software maintenance
Software maintenance became an issue about 5 months into the trial. This manifested as broken links to websites and users received notification from the operating software about the need for an update. Because the tablets were locked, the caregivers were unable to complete the updates.
Solutions
The technology support team pushed out updates to the tablets to fix the broken or outdated links and to install the operating system and software updates. This solution is time-consuming. It entails contacting each caregiver in the study for both the intervention and control groups to remind them to keep the tablet plugged in and the case open to allow remote software updating and programing. The time may be worth-while, however, because there is an indication the updates also may improve the aforementioned connectivity issues.
3.2.3 |. Hardware
Hardware challenges presented as both user maintenance (e.g., battery not charged) as well as unexpected tablet responses such as the tablet “going to sleep” even with a full battery charge. During individual sessions, caregivers and health coaches noted the tablet could not connect properly to the data plan if there was a low battery or the tablet would shut down during a session if it was not fully charged. The exact nature of the tablet “going to sleep” was less clear, although we suspect it relates to a timer setting on the tablet system.
Solution
To deal with hardware challenges, the coaches scheduled special sessions with the caregiver using the tablet while a member of the technology support team tried to remote into the tablet to evaluate the problem. When battery charge was determined to be a major issue, the technology support team provided specific guidance on best practices for keeping the tablets working properly, and this content was added to the caregiver training and manual. In addition, the health coaches now remind the caregivers before, during, and after sessions to leave the tablet plugged in and charging at all times, a strategy that has resolved the problem for some caregivers.
The tablet “going to sleep” during a session, however, was not solved completely by the battery charge solution. All tablets with this problem were remoted into and the screen “sleep” timer setting checked. This setting was the same on all tablets and did not appear to be the problem, thus no specific solution has been identified. The solution identified by the caregiver was to keep touching the tablet during the session to keep it “awake.”
4 |. DISCUSSION
Challenges encountered early in the trial provide several important lessons. Although using video technology to deploy a virtual intervention may not be new (Chi & Demiris, 2015), using technology to support caregivers of persons with HF is not common. With each enrolled caregiver and completed ViCCY session, the health coaches and team developed a set of standard adaptations to try to address common technology problems faced during a structured clinical trial. The lessons learned presented here have three important implications.
First, the use of a tablet to deliver standardized health information and the virtual health coaching intervention is feasible but requires flexibility. Most sessions required the health coach to adapt the implementation of the intervention to complete the intervention session. About 26% of intervention sessions (Table 2) were conducted as originally specified with both video and audio. Both the intervention and control groups have had problems related to broken health information links. Although it is not common for the main website links to change, it does occur indicating the need to routinely check the links.
Other design considerations include providing mobile connectivity and choosing a cellular plan with a broad network to provide everyone with access. We did not consider, however, that the video conferencing software bandwidth parameters might exceed what some areas can provide. In this trial, caregivers’ tablets are blocked from connecting to a personal or public Wi-Fi network, which limits the caregiver in using alternative networks to improve connectivity. Allowing connectivity to personal or public Wi-Fi networks should be considered to decrease this potential challenge.
Second, both the control and intervention groups receive a tablet already configured with standardized health information and virtual health coaching video conferencing software. This approach was chosen to eliminate disparities noted in previous studies (Yoon et al., 2020). Yet, not all barriers are eradicated. The current COVID-19 pandemic has highlighted the potential widening of the digital divide due to health and economic disparities and lack of infrastructure in some communities (Almufleh & Givertz, 2020; Bakhtiar et al., 2020; Hirko et al., 2020; Khilnani et al., 2020; Nouri et al., 2020; Wosik et al., 2020). As many aspects of life in the United States moved online, older adults and those with greater economic disparities were unprepared for the impact and the resulting isolation (Conger & Griffith, 2020). Offering virtual supports to individuals requires access to both hardware and connectivity. In the United States, free Wi-Fi was one quick solution implemented to bridge this divide, but without adequate hardware (e.g., smartphone, tablet, or computer), this solution is incomplete. From a research perspective, the COVID-19 pandemic altered the way in which traditional research has been conducted (Verna et al., 2020), yet virtual interventions, such as the one described here, have been able to continue. A highlight of this intervention is the provision of both hardware and connectivity as well as a person caregivers can connect with for support while isolated at home.
For the intervention group, the sessions are still being delivered to the caregivers by the health coaches but not always using the original video conferencing software installed on the tablets. From the start, we anticipated problems and had a strong system in place to document the challenges, discuss them, and troubleshoot with the coaches and caregivers. Close monitoring and flexibility are key to recognize that issues are occurring so that the team can quickly adapt, resolve, or accept novel ways to solve them. These technical challenges will continue to be monitored over the remainder of the trial. Modifications will be made as needed. At this point, we are trying different video conferencing software and considering the use of a different tablet (e.g., iPads). The challenges associated with poor connectivity due to the structure of the home or the mobile cellular carrier, however, cannot be modified.
Third, while the technology was piloted in prior work, the exact tablet model and video conferencing platform modifications used are slightly different. Newer models of tablets, operating systems and software improvements, and greater mobile connectivity, although seen as advances, appear to have created a challenge in the startup of this trial. Testing all hardware and software again, especially if modified from the pilot study, in as many possible scenarios before the start of a trial should be considered, if feasible. Setting up a schedule for pushing out updates to tablets is essential. Once updates were sent out to the tablets many issues were resolved among the newer enrolled caregivers.
Reliable and responsive technology support is critical. Having a good relationship with your technology support team is essential to keep tablets in optimal working order throughout the study. Developing standardized processes to document the tablet problems, the solutions implemented by the technology support (e.g., updating the operating system, fixing broken links), and the time required to make the modifications are essential. This information facilitates examining the root cause of an adaptation to the delivery of the intervention as well as determining the cost of an intervention. In addition, having computer savvy health coaches with the ability to work together and develop a set of adaptations to meet the intervention group’s collective needs has been critical to moving the intervention forward. Developing early consensus on acceptable, standardized procedures to adapt the delivery of the intervention and collect data about all modifications is an essential element to the design of a study.
There are several pros and cons to the decisions made in the setup of the tablets for the current study. The pros are that by standardizing the tablets everyone received the same technology, mobile connectivity, and health information intervention, as well as the same problems with the need for operating system updates, poor connectivity, and broken health information web links. In addition, all caregivers received a digital copy of the caregiver manual that has all the same health information links on the table in the manual, thereby allowing the caregiver to access those links through their own devices.
Some cons are that by locking down the tablet, the caregivers are unable to print any material they may find and wish to keep, nor can they email the information to themselves or others. Only mass emails pushed out to all tablets by the technology team are possible. Having individual email available on each tablet may have been useful in pushing out reminders for follow-up interviews, setting up calendar invites, and connecting with the study team electronically. One aspect that is not being tracked in this study but may be of interest to others designing similar work, is the frequency of accessing the health and self-care links made available to all study subjects. Tracking sites accessed and the time spent on specific sites might be useful to determine if the site or time spent has an impact on self-care.
There is limited research comparing virtual interventions to telephone interventions. In a recently published study, the main differences between the two groups were that the video intervention had greater odds of connectivity difficulties at the start of the study, connection loss during sessions, and trouble hearing the study participant, in comparison to the telephone group (Byaruhanga et al., 2020). Most of the available literature compares telephone to usual care (e.g., in person or health information only) or virtual to usual care, often lacking a description of challenges encountered and solutions used (Gately et al., 2019; O’Brien et al., 2018; Waller et al., 2017). More research examining the relative value of using video versus telephone interventions with caregivers is greatly needed.
When developing and launching interventions using technology, teams need to closely monitor technical issues and be prepared to implement solutions that best support the delivery as intended. The findings here inform readers of the challenges and solutions to consider. Balancing the cost of the technology, and the time it takes to troubleshoot, with the quality of the intended delivery of the intervention will be explored with findings from this trial.
ACKNOWLEDGMENTS
Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number Research (NINR) R01NR018196. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding information
NINR/National Institutes of Health (NIH), Grant/Award Number: R01NR018196
Footnotes
DESCRIPTION
Special Issue: Telehealth/mHealth; Research Methods Paper.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
REFERENCES
- Almufleh A, & Givertz MM (2020). Virtual health during a pandemic. Circulation: Heart Failure, 13(8), e007317. https://www.pewresearch.org/internet/wp-content/uploads/sites/9/2017/05/PI_2017.05.17_Older-Americans-Tech_FINAL.pdf [DOI] [PubMed] [Google Scholar]
- Alpert CM, Smith MA, Hummel SL, & Hummel EK (2017). Symptom burden in heart failure: Assessment, impact on outcomes, and management. Heart Failure Reviews, 22(1), 25–39. 10.1007/s10741-016-9581-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson M, & Perrin A. (2017). Tech adoption climbs among older adults. Retrieved from https://www.pewinternet.org/2017/05/17/tech-adoption-climbs-among-older-adults/
- Bakhtiar M, Elbuluk N, & Lipoff JB (2020). The digital divide: How Covid-19’s telemedicine expansion could exacerbate disparities. Journal of the American Academy of Dermatology, 83(5), E345–E346. 10.1016/j.jaad.2020.07.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buck HG, Harkness K, Wion R, Carroll SL, Cosman T, Kaasalainen S, Kryworuchko J, McGillion M, O’Keefe-McCarthy S, Sherifali D, Strachan PH, & Arthur HM (2015). Caregivers’ contributions to heart failure self-care: A systematic review. European Journal of Cardiovascular Nursing, 14(1), 79–89. 10.1177/1474515113518434 [DOI] [PubMed] [Google Scholar]
- Byaruhanga J, Paul CL, Wiggers J, Byrnes E, Mitchell A, Lecathelinais C, & Tzelepis F. (2020). Connectivity of real-time video counselling versus telephone counselling for smoking cessation in rural and remote areas: An exploratory study. International Journal of Environmental Research and Public Health, 17(8), 2891. 10.3390/ijerph17082891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi NC, & Demiris G. (2015). A systematic review of telehealth tools and interventions to support family caregivers. Journal of Telemedicine and Telecare, 21(1), 37–44. 10.1177/1357633X14562734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger K, & Griffith E. (2020. March 27). As Life Moves Online, an Older Generation Faces a Digital Divide. New York Times. Retrieved from https://www.nytimes.com/2020/03/27/technology/virus-older-generation-digital-divide.html [Google Scholar]
- Dionne-Odom JN, Demark-Wahnefried W, Taylor RA, Rocque GB, Azuero A, Acemgil A, Martin MY, Astin M, Ejem D, Kvale E, Heaton K, Pisu M, Partridge EE, & Bakitas MA (2017). The self-care practices of family caregivers of persons with poor prognosis cancer: Differences by varying levels of caregiver well-being and preparedness. Supportive Care in Cancer, 25(8), 2437–2444. 10.1007/s00520-017-3650-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dionne-Odom JN, Hooker SA, Bekelman D, Ejem D, McGhan G, Kitko L, Strömberg A, Wells R, Astin M, Metin ZG, Mancarella G, Pamboukian SV, Evangelista L, Buck HG, Bakitas MA, & IMPACT-HF National Workgroup (2017). Family caregiving for persons with heart failure at the intersection of heart failure and palliative care: A state-of-the-science review. Heart Failure Reviews, 22(5), 543–557. 10.1007/s10741-017-9597-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evangelista LS, Stromberg A, & Dionne-Odom JN (2016). An integrated review of interventions to improve psychological outcomes in caregivers of patients with heart failure. Current Opinion in Supportive and Palliative Care, 10(1), 24–31. 10.1097/SPC.0000000000000182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Family Caregiver Alliance. (2014). Definitions. Retrieved from https://www.caregiver.org/definitions-0
- Gately ME, Trudeau SA, & Moo LR (2019). In-home video telehealth for dementia management: Implications for rehabilitation. Current Geriatrics Reports, 8(3), 239–249. 10.1007/s13670-019-00297-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant I, McKibbin CL, Taylor MJ, Mills P, Dimsdale J, Ziegler M, & Patterson TL (2003). In-home respite intervention reduces plasma epinephrine in stressed Alzheimer caregivers. American Journal of Geriatric Psychiatry, 11(1), 62–72. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12527541 [PubMed] [Google Scholar]
- Hayes L, Hawthorne G, Farhall J, O’Hanlon B, & Harvey C. (2015). Quality of life and social isolation among caregivers of adults with schizophrenia: Policy and outcomes. Community Mental Health Journal, 51(5), 591–597. 10.1007/s10597-015-9848-6 [DOI] [PubMed] [Google Scholar]
- Hirko KA, Kerver JM, Ford S, Szafranski C, Beckett J, Kitchen C, & Wendling AL (2020). Telehealth in response to the Covid-19 pandemic: Implications for rural health disparities. Journal of the American Medical Informatics Association, 27, 1816–1818. 10.1093/jamia/ocaa156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoefman RJ, Meulenkamp TM, & De Jong JD (2017). Who is responsible for providing care? Investigating the role of care tasks and past experiences in a cross-sectional survey in the Netherlands. BMC Health Services Research, 17(1), 477. 10.1186/s12913-017-2435-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu C, Kung S, Rummans TA, Clark MM, & Lapid MI (2015). Reducing caregiver stress with internet-based interventions: A systematic review of open-label and randomized controlled trials. Journal of the American Medical Informatics Association, 22(e1), e194–e209. 10.1136/amiajnl-2014-002817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman MH (2014). Using motivational interviewing: Through evidence-based health coaching. Home Healthcare Nurse, 32(9), 543–548. 10.1097/nhh.0000000000000139 [DOI] [PubMed] [Google Scholar]
- Huffman MH (2016). Advancing the practice of health coaching: Differentiation from wellness coaching. Workplace Health Saf, 64(9), 400–403. 10.1177/2165079916645351 [DOI] [PubMed] [Google Scholar]
- Khilnani A, Schulz J, & Robinson L. (2020). The COVID-19 pandemic: New concerns and connections between eHealth and digital inequalities. Journal of Information, Communication and Ethics in Society, 18(3), 393–403. 10.1108/JICES-04-2020-0052 [DOI] [Google Scholar]
- Kitko L, McIlvennan CK, Bidwell JT, Dionne-Odom JN, Dunlay SM, Lewis LM, Meadows G, Sattler ELP, Schulz R, & Strömberg A. (2020). Family caregiving for individuals with heart failure: A scientific statement from the American Heart Association. Circulation, 141(22), e864–e878. 10.1161/CIR.0000000000000768 [DOI] [PubMed] [Google Scholar]
- Lazarus R, & Folkman S, & (1984. & Stress, appraisal and coping, New York, NY: Springer. 10.1007/978-1-4419-1005-9 [DOI] [Google Scholar]
- Liljeroos M, Agren S, Jaarsma T, Arestedt K, & Stromberg A. (2017). Long-term effects of a dyadic psycho-educational intervention on caregiver burden and morbidity in partners of patients with heart failure: a randomized controlled trial. Quality of Life Research, 26(2), 367–379. 10.1007/s11136-016-1400-9 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2016). Families caring for an aging America, Washington, DC: The National Academies Press. 10.17226/23606 [DOI] [PubMed] [Google Scholar]
- National Alliance for Caregiving & AARP. (2015). Research Report: Caregiving in the US. Retrieved from https://assets.aarp.org/rgcenter/il/us_caregiving_1.pdf
- Nouri S, Khoong E, Lyles C, & Karliner L. (2020). Addressing Equity in Telemedicine for Chronic Disease Management During the Covid-19 Pandemic. New England Journal of Medicine Catalyst Innovation in Care Delivery, May 4, 2020 (Commentary). 10.1056/CAT.20.0123 [DOI] [Google Scholar]
- O’Brien KM, Hodder RK, Wiggers J, Williams A, Campbell E, Wolfenden L, Yoong SL, Tzelepis F, Kamper SJ, & Williams CM (2018). Effectiveness of telephone-based interventions for managing osteoarthritis and spinal pain: A systematic review and meta-analysis. PeerJ, 6, e5846. 10.7717/peerj.5846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piette JD, Striplin D, Marinec N, Chen J, & Aikens JE (2015). A randomized trial of mobile health support for heart failure patients and their informal caregivers: Impacts on caregiver-reported outcomes. Medical Care, 53(8), 692–699. 10.1097/MLR.0000000000000378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pressler SJ, Jung M, & Friedman J. (2016). Heart failure and debilitating cardiovascular problems. In Burgio LD, Gaugler JE, & Hilgeman MM (Eds.), The spectrum of family caregiving for adults and elders with chronic illness. Oxford University Press. [Google Scholar]
- Reinhard SC, Feinberg LS, Houser A, Choula R, & Evans M, AARP Public Policy Institute. (2019). Valuing the invaluable, 2019 update: Charting a path forward. Washington, DC: AARP Public Policy Institute. Retrieved from https://www.aarp.org/content/dam/aarp/ppi/2019/11/valuing-the-invaluable-2019-update-charting-a-path-forward.doi.10.26419-2Fppi.00082.001.pdf [Google Scholar]
- Riegel B, Christiansen K, Fontana S, Lillo E, Lillo J, Patey M, & Tkacs N. (2013). Cognitive behavioral therapy by iPad for caregivers: A pilot study. Electrophysiology and Rhythm Devices (Journal of Cardiac Failure), 19(8), S40. (abstract # 115). [Google Scholar]
- Riegel B, Hanlon AL, Coe NB, Hirschman KB, Thomas G, Stawnychy M, Wald JW, & Bowles KH (2019). Health coaching to improve self-care of informal caregivers of adults with chronic heart failure—iCare4Me: Study protocol for a randomized controlled trial. Contemporary Clinical Trials, 85, 105845. 10.1016/j.cct.2019.105845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders MM (2012). Perspectives from family caregivers receiving home nursing support: Findings from a qualitative study of home care patients with heart failure. Home Healthcare Nurse, 30(2), 82–90. 10.1097/NHH.0b013e3182429337 [DOI] [PubMed] [Google Scholar]
- Schrank B, Ebert-Vogel A, Amering M, Masel EK, Neubauer M, Watzke H, Zehetmayer S, & Schur S. (2016). Gender differences in caregiver burden and its determinants in family members of terminally ill cancer patients. Psycho-Oncology, 25(7), 808–814. 10.1002/pon.4005 [DOI] [PubMed] [Google Scholar]
- Sevilla-Cazes J, Ahmad FS, Bowles KH, Jaskowiak A, Gallagher T, Goldberg LR, Kangovi S, Alexander M, Riegel B, Barg FK, & Kimmel SE (2018). Heart failure home management challenges and reasons for readmission: A qualitative study to understand the patient’s perspective. Journal of General Internal Medicine, 33(10), 1700–1707. 10.1007/s11606-018-4542-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigafus M, & Riegel B. (2010). Riding the roller-coaster: Experiences of caregivers of adults with heart failure. Paper presented at the Penn-ICOWHI 18th International Congress on Women’s Health; “Cities and Women’s Health: Global Perspectives”, University of Pennsylvania, Philadelphia, PA, USA. [Google Scholar]
- Srisuk N, Cameron J, Ski CF, & Thompson DR (2017). Randomized controlled trial of family-based education for patients with heart failure and their carers. Journal of Advanced Nursing, 73(4), 857–870. 10.1111/jan.13192 [DOI] [PubMed] [Google Scholar]
- Van Houtven CH, Smith VA, Stechuchak KM, Shepherd-Banigan M, Hastings SN, Maciejewski ML, Wieland GD, Olsen MK, Miller KEM, Kabat M, Henius J, Campbell-Kotler M, & Oddone EZ (2017). Comprehensive support for family caregivers: Impact on veteran health care utilization and costs. Medical Care Research and Review, 76(1), 89–114. 10.1177/1077558717697015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verna EC, Serper M, Chu J, Corey K, Fix OK, Hoyt K, Page KA, Loomba R, Li M, Everson GT, Fried MW, Garcia-Tsao G, Terrault N, Lok AS, Chung RT, & Reddy KR (2020). Clinical research in hepatology in the COVID-19 pandemic and post-pandemic era: Challenges and the need for innovation. Hepatology, 72, 1819–1837. 10.1002/hep.31491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, … Tsao CW (2020). Heart Disease and Stroke Statistics 2020 Update: A report from the American Heart Association. Circulation, 141(9), e139–e596. 10.1161/CIR.0000000000000757 [DOI] [PubMed] [Google Scholar]
- Wakefield BJ, Bylund CL, Holman JE, Ray A, Scherubel M, Kienzle MG, & Rosenthal GE (2008). Nurse and patient communication profiles in a home-based telehealth intervention for heart failure management. Patient Education and Counseling, 71(2), 285–292. 10.1016/j.pec.2008.01.006 [DOI] [PubMed] [Google Scholar]
- Waller A, Dilworth S, Mansfield E, & Sanson-Fisher R. (2017). Computer and telephone delivered interventions to support caregivers of people with dementia: A systematic review of research output and quality. BMC Geriatrics, 17(1), 265–265. 10.1186/s12877-017-0654-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Robinson KM, & Hardin HK (2015). The impact of caregiving on caregivers’ medication adherence and appointment keeping. Western Journal of Nursing Research, 37(12), 1548–1562. 10.1177/0193945914533158 [DOI] [PubMed] [Google Scholar]
- Wingham J, Frost J, Britten N, Jolly K, Greaves C, Abraham C, & Dalal H. (2015). Needs of caregivers in heart failure management: A qualitative study. Chronic Illness, 11(4), 304–319. 10.1177/1742395315574765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, Curtis S, Roman M, Poon EG, Ferranti J, Katz JN, & Tcheng J. (2020). Telehealth transformation: COVID-19 and the rise of virtual care. Journal of the American Medical Informatics Association, 27(6), 957–962. 10.1093/jamia/ocaa067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon H, Jang Y, Vaughan PW, & Garcia M. (2020). Older adults’ Internet use for health information: Digital divide by race/ethnicity and socioeconomic status. Journal of Applied Gerontology, 39(1), 105–110. 10.1177/0733464818770772 [DOI] [PubMed] [Google Scholar]
- Young R, Willis E, Cameron G, & Geana M. (2014). “Willing but Unwilling”: Attitudinal barriers to adoption of home-based health information technology among older adults. Health Informatics Journal, 20(2), 127–135. 10.1177/1460458213486906 [DOI] [PubMed] [Google Scholar]


