August 30, 2021
Authors note: The authors are grateful to have been involved in many conversations with providers, health care systems, and jurisdictions about crisis standards of care (CSC) issues during COVID-19. Statements in this paper are often based on or buttressed by these accounts, although the authors are not able to share the specific details, as some of these colleagues have suffered professional retribution for raising these issues or being willing to have open and honest discussion of the tactics that were implemented. The authors of this manuscript hope that discussion about CSC can become akin to root cause analysis and other no-fault learning environments. Until then, the authors are thankful for our colleagues’ honesty and desire to clarify and improve our frameworks.
Introduction
COVID-19 has fundamentally challenged the delivery of health care services across the world, forcing difficult choices on health professionals and laying bare many preexisting health, medical, and public health sector frailties. Extreme shortages of key resources and worries that patients would not receive the care they needed were frequent features of the response beginning in the spring of 2020 and were recurrent during subsequent regional and national peaks.
Crisis standards of care (CSC) occur when the degree of resource shortage requires decisions that place a patient or provider at risk of a poor outcome. These situations arose in most jurisdictions and required a systematic, coordinated response [1]. Often, state and health care CSC plans were used or revised, or they did not apply to the situations encountered. In several critical instances, potentially useful CSC plans were ignored or actively subverted. The authors of this paper describe some of the successes and shortfalls of CSC principles and practices during COVID-19 and identify issues to be addressed for future events.
This paper focuses on hospital application of CSC, though emergency medical services (EMS) experienced similar issues. EMS and health care planning and response must be linked to ensure consistency of expectations as well as optimal patient distribution and redistribution. Both EMS and hospital resources and staff require stewardship during disasters, particularly ones that are protracted in nature. Recognition of clinical care interdependency (long-term care, EMS, hospitals, outpatient care) in planning and response is critical for avoiding CSC conditions and improving consistency across the spectrum of care as well as across any given geographic region.
Revision of CSC doctrine is needed and should be a focus for health care institutions and local, state, and federal governments alike to ensure that the best care possible is delivered when the next disaster strikes. In the following sections, the authors discuss some key CSC domains as well as successes, issues, and action steps.
CSC Areas of Focus
Equity
CSC planning has been predicated upon the importance of ensuring unbiased, fair, and consistent triage decisions. However, COVID-19 laid bare the structural inequities of our current health care system that made such aspirational goals largely unachievable and highlighted that some elements of CSC planning may unfairly penalize certain groups [2]. COVID-19 disproportionately affected communities of color and at-risk individuals, such as those in skilled nursing facilities, detention facilities, and essential workplaces. Further, preexisting comorbidities, multigenerational housing, use of public transit, and essential worker occupations magnified poor outcomes and accelerated transmission in historically disadvantaged communities [3,4,5,6,7,8].
When resources are in shortage, fairness demands extra effort to reach and serve the hardest hit communities, including tailored connection and communication strategies, as many historically marginalized communities have limited connection with, and significant distrust of, the medical system and government initiatives. Unfortunately, for resources such as COVID-19 diagnostic testing kits and access to vaccines and monoclonal antibodies, there was widespread use of online registration systems and implementation of mass testing or vaccination sites, with the aim of speeding the process and rapidly making progress, but these choices further disadvantaged those with diminished access to information, computers, and transportation [9,10].
Equity clearly requires that resources be balanced in a community to ensure a consistent level of care—such as patient load-balancing between hospitals (discussed later in this paper). The more difficult task is to ensure equitable access to information, basic medical care, testing, vaccination, and early treatment for underserved communities. While several racial and ethnic minority groups have seen dramatically higher COVID-19 infection, hospitalization, and death rates, the direct use of race as a prioritizing factor for resource allocation has been controversial, with only Vermont and Montana doing so for vaccination prioritization [11]. Arguments against the use of race in medical resource allocation include operational concerns of defining members of racial groups, ethical concerns of fairness at the individual level, social concerns of stoking racial resentment, and legal concerns of equal protection [12]. The use of multifactor risk tools that include race, such as the Centers for Disease Control and Prevention’s (CDC’s) Social Vulnerability Index, has been less contentious in theory and has been recommended by a National Academies of Sciences, Engineering, and Medicine committee and the CDC’s Advisory Committee on Immunization Practices [13,14,15]. However, such tools have rarely been implemented in practice for vaccine allocation—and where they have been used, they have sometimes been challenged [13,14,15]. Rather, the focus on equity, where it has been explicitly addressed, has been through strategies like establishing pop-up clinics in churches serving communities of color and through outreach strategies targeting underserved communities.
The potential for structural racism in CSC plans is not the only concern. Risks of ageism and discrimination against the disabled must also be addressed [16,17,18]. This is especially true given the catastrophic impact on residents of long-term care facilities, whose life circumstances often present a high risk of implicit triage decisions by providers to withhold usual medical care, sometimes cloaked in the language of medical futility (i.e., presenting a triage decision, based on a resource shortage, as a decision to withhold the resource because it offers no benefit).
The authors suggest:
CSC protocols that will be used for making urgent allocation decisions in a disaster cannot be expected to remedy historic and structural inequity. However, they should not exacerbate underlying disparities. Public and private partnerships are required to address structural inequity, trust, and access to care issues prior to an incident.
During a disaster, resource allocation for community-based interventions (such as vaccination clinics and testing sites) should be weighted to ensure equitable access to resources for communities according to their risk of illness and mortality, including access to transportation, personal protective equipment (PPE), diagnostics, safe housing for quarantine, and treatment for those who become ill.
Ethicists and clinicians should agree concretely on priority mechanisms of both allocation (e.g., when random number, lottery, weighted lottery, or first-come-first-served are most appropriate) and clinical prioritization (e.g., according to likelihood of benefit) when novel therapies are in shortage (e.g., monoclonal antibodies, vaccine). Templated baseline strategies and thresholds for their use would also be helpful, in light of the apparent reticence of some political and clinical leaders to acknowledge crisis conditions (discussed further later in this paper).
Politics and Declarations of CSC
Both the 2009 and 2012 Institute of Medicine (IOM) (now National Academy of Medicine) reports on CSC (Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations: A Letter Report and Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response, respectively) defined CSC as requiring a “formal declaration,” and, in fact, many hospital and state plans rely on a state declaration to trigger CSC protocols [19,20]. This threshold was included largely based on the assumption that many resources would come into scarcity at the same time, including ventilators and other life-saving resources, but it did not consider that some resources might be in sustained shortage, yet not require formal state action. For example, during the early phase of COVID-19, health care systems experienced critical shortages of PPE, requiring implementation of crisis strategies developed by the CDC—but usually without required state action. Although shortages no longer require crisis strategies, many facilities are still not able to use conventional PPE strategies at the time of this writing [21].
Only Arizona and New Mexico formally declared CSC, allowing for triage of ventilators and other intensive care resources using state CSC plans. But the decision to implement ventilator triage was left to health care facilities, none of which apparently did so [39]. Waxing and waning conditions over time created significant difficulty in determining when a crisis situation began or ended for a given resource in a given area. Many jurisdictions reached a point where staff and resources such as dialysis were spread critically thin, with confusion as to whether the system was in crisis or not. Some jurisdictions declared CSC at a county or state level without having leveraged patient transfer mechanisms that could have unloaded their affected facilities (in the end, none of these wound up performing overt triage). In addition, some areas that were clearly in crisis related to ventilators, oxygen, or other resources, where painful triage decisions had to be made, never received a formal declaration authorizing CSC [22,23]. It appears that some states ignored their own CSC plans to declare crisis conditions. This reticence is likely attributable to multiple factors, including political concerns as well as practical concerns about scope, authorities, and liability in addition to issues defining which specific conditions or shortages were worthy of a declaration and which were not. Most state plans at least tacitly indicate that a declaration would be made to support such decisions as ventilator triage in a catastrophic situation, but prior guidance has generally reflected a blanket invocation and not accounted for more limited declarations or actions. Clearly, crisis conditions and the need to make decisions to prioritize services and asset allocation can arise regardless of any jurisdictional declaration.
The authors suggest:
State leadership (public health, governors, attorneys general, and regulatory entities) should identify ways in which mitigation and surge strategies can be implemented and supported at the state or regional level, including promoting communication and coordination of resources to reduce the need for CSC, in addition to regulatory, administrative, and executive actions to support providers and facilities and reduce liability.
Offices of governors and state attorneys general, health care systems, and state health departments should negotiate more explicit expectations of legal, regulatory, and policy support during crisis conditions, including consideration of specific triggers and requests that would automatically invoke CSC legal protections and clinical guidance. These should recognize that while a state declaration may be part of support for clinical activities, crisis conditions can arise whether declared or not, and ad hoc clinical problem-solving will likely still be required. Facilities and health care systems must coordinate care and mitigate crisis conditions as quickly and consistently as possible, and states have a duty to support providers making difficult choices.
States should clarify the role of state health department and governors’ offices in the public recognition of the aspects of the health care system that are in crisis, the support of strategies to mitigate the situation, and the provision of best practice guidance when rationing becomes necessary.
Planning efforts should focus on developing and promulgating tools for managing specific resources that may be in extreme shortage (e.g., PPE, dialysis, oxygen, sedatives) rather than seeking an overarching declaration of crisis conditions. These should include public, patient, and family messaging, legal and regulatory tools to support necessary health care rationing actions, and proactive guidance for those situations.
Box 1. Definitions.
Conventional care: usual resources and level of care provided through maximal use of the facilities’ usual beds, staff, and resources.
Contingency care: provision of functionally equivalent care—care provided is adapted from usual practices (e.g., boarding critical care patients in post-anesthesia care areas).
Crisis care: inadequate resources are available to provide equivalent care—care is provided to the level possible given the resource gap. Increased risk of morbidity and mortality defines the care provided in this phase—this risk can be minimized by implementing consistent proactive resource use strategies.
Health care facilities and systems should work together to agree on information they will share and actions that they will take to avoid crisis situations as well as coordinate efforts when CSC implementation is unavoidable, regardless of governmental action.
When legislative protections are not available, legal protections for providers under executive order should be sought but confined to address the specific issue and time frame (i.e., broad immunity for prolonged periods of time should be avoided). If neither legislative nor executive protections are available despite the need to make triage decisions, professional associations, hospital associations, health care coalitions, and other entities that span jurisdictional boundaries should bring together health care systems, public health departments, EMS, and emergency management agencies to craft guidance, which is likely to establish a reasonable provider legal standard for the circumstances.
Education should be provided to clinicians about the circumstances under which life-saving resources may be ethically withheld from patients without patient or surrogate consent, and these processes must have the support of the providers as well as the state.
Categories and Nomenclature
The CSC spectrum of care recognizes that health care surge occurs on a continuum across conventional, contingency, and crisis response (see Box 1) [20]. This nomenclature was generally helpful in surge planning at the health care facility level and was used early in the response to COVID-19 by the CDC in its guidance for health care worker PPE [21]. However, problems arose from the CDC’s use of these categories as the progression across them was unfamiliar to clinicians and health care administrators. For example, a recommendation that health care workers could use bandanas and other protections of last resort during extreme shortages of PPE resulted in misunderstanding by health care workers that the CDC considered such protective measures adequate (which was clearly not the case) [23]. This was indicative of a much larger issue—the near-absence of education and training of the US health care workforce to operate under disaster conditions. As a result, the authors frequently observed an excessive fixation on worst-case scenarios that generated significant emotional response but that rarely occurred, such as complete absence of PPE, ventilators, or critical medications. Though this may have resulted in the public and providers taking precautions more seriously because of the potential extreme consequences, it was not effective in focusing health care planning.
Illustrations of the spectrum of CSC usually represent the transition between contingency and crisis as a sharp vertical line between the two; however, this is not typically the case. Although some resource shortages (e.g., ventilators) pose such a risk as to automatically represent crisis conditions, incremental changes to staffing or the performance of dialysis do not fall squarely within either the contingency or crisis category, and the lack of established triggers and protocols for allocating these resources created confusion. In prior documents, including the 2012 IOM report, transitions from conventional to contingency and contingency to crisis have been described as incremental, but it was difficult for providers to translate this concept from graphical representation of a dividing line to knowing when the strategy used crossed the boundary from contingency to crisis based on the increased risk to the patient of a given strategy [20]. One way this was addressed was to denote the transition from conventional care to contingency care as crossing a resource shortage threshold, when a particular resource was noted to be in short supply. In a sustained or severe disaster, clinical decision making might further be impacted if supplies continue to dwindle, now crossing a resource triage threshold at which point decisions related to their specific allocation were required, denoting the transition from contingency to crisis care [20]. The transition of risk between contingency and crisis is a gray area, particularly when a resource is elastic, and is less important than a common understanding of the progression of changes that will be made and an ability to compare those adaptations to the ones required at other facilities in the area.
However, multiple examples (see Figure 1) during COVID-19 demonstrated the ability of clinicians to implement graded changes in services provided, thus minimizing risks to patients [20,24]. In many cases, these were developed on an ad hoc basis but represent examples that need to be preserved. Titrating the minimum change required to the resources available across this continuum satisfies the proportionality tenet of CSC. What constitutes significant risk to the patient that indicates a transition to crisis care is often open to interpretation, but the use of a graduated progression ensures that the right thing is done clinically for the circumstances. In general, the setting of triggers as a threshold for crisis (e.g., no ICU beds remaining) at the state level has failed because when this threshold is crossed, either adaptive strategies allow contingency care beyond that number, or some facilities have crossed that threshold, but others have not. At the coalition or regional level, agreeing on a threshold (such as staffing ratios) that is recognized as “in crisis” allows improved communication of circumstances and coordination, and can drive additional facility, coalition, and state actions to support the affected facilities.
FIGURE 1. Examples of Graduated Changes Across the Care Continuum.
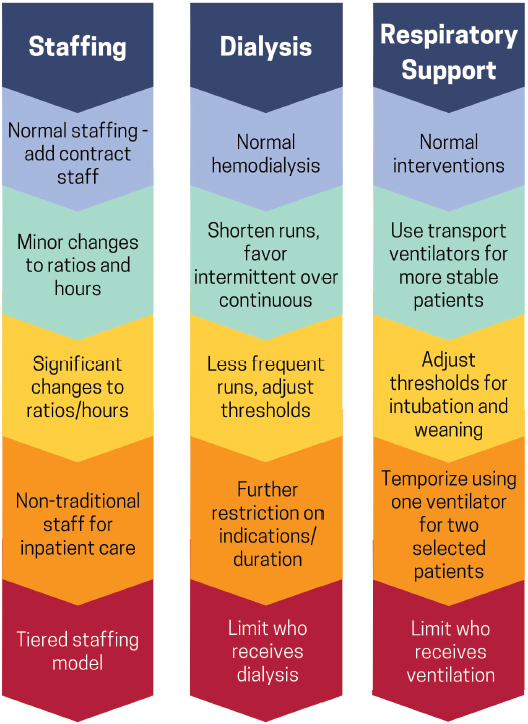
SOURCE: Developed by authors.
NOTE: Examples only. Does not represent all potential adjustments. Increasing risk for poor patient outcome as changes implemented from top to bottom. Regional agreement on what constitutes ‘significant risk’ and therefore crisis conditions is needed to facilitate communications, resource distribution, and guide response strategy.
The authors suggest:
Mandatory clinical staff education should be provided about the spectrum of disaster care, which was a recommendation laid out in prior reports related to CSC calling for provider engagement [19,20].
Casebooks with examples of stepwise degradation of services should be created (e.g., extension of dialysis, using transport ventilators for patients with stable respiratory parameters).
When the significant risk (i.e., crisis) threshold is not clear, regional definitions should be adopted to facilitate resource allocation/movement decisions—for example, what level of staffing constitutes crisis vs. contingency.
Emphasis should be on planning and effort to avoid crisis conditions (i.e., stay in contingency).
Understanding of Surge
Insights gained from the management of a large, sustained flow of patients to U.S. hospitals greatly advanced understanding of actual surge capacity and highlighted those factors (e.g., staffing, oxygen supply) that may limit the expansion of critical care in disasters. If properly documented, this understanding of surge capacity can greatly advance regional and national disaster planning. In many cases, hospital surge plans did not reflect a graded progression of strategies across the spectrum of conventional, contingency, and crisis. In some cases, crisis surge plans were separate documents.
The authors suggest:
States, health care systems, public health agencies, and health care coalitions capture and share available surge data and capacity data to better understand daily system capacity as well as for use in future events of all hazard types. Accurate, accessible, relevant data are critical to understanding the impact of patient surges and the need for intervention.
Health care facilities should update surge capacity plans for all-hazards response that include CSC strategies as part of the spectrum of a graded surge response, not as a separate plan.
Future architectural remodeling and health care facility capital improvement projects, including plans for new building construction, should anticipate and accommodate disaster surge needs.
Coordination of Care and Information Sharing
Community and regional (i.e., in a health care catchment area) consistency in the delivery of care is crucial to avoiding pockets of crisis care and assuring fairness, particularly given recent work illustrating the increased mortality at hospitals experiencing COVID-19 surge [25]. In many communities, COVID-19 forced health care coalitions, hospital associations, and health care systems to refine data collection and information sharing for system status monitoring. Such data coordination permitted coalition/state actions such as load-balancing (i.e., medical operations coordination cells [MOCC]) that contributed greatly in many areas to maximal use of critical care beds by facilitating transfers from overwhelmed facilities [26,27]. Some shortfalls involved patients being refused transfer due to insurance status [28,29]. Close coordination with EMS is required to ensure that adequate resources are available for transfers and to maintain emergency response capacity. Regional and interstate coordination of EMS assets may be required.
Additionally, in some areas, health care coalitions and state entities were critical in allocating resources to facilities most in need, including PPE, ventilators, and staffing. These coordination and prioritization mechanisms have been articulated and encouraged by the Department of Health and Human Services (HHS) Office of the Assistant Secretary for Preparedness and Response (ASPR) Hospital Preparedness Program (HPP) requirements, which may be refined in future iterations to further support this important role [30].
Between 2009 and 2020, the U.S. health care system failed to define essential elements of information that could be shared between hospitals, across and between states, and with federal partners to assess the impact of an event in real time and to support load-balancing of patients, staff, and resources. During the COVID-19 crisis, this led to implementation of ad hoc systems (e.g., awarding of de novo contracts to private sector parties), which created full-time obligations at hospitals to fulfill data requirements, yet often provided low visibility on how this data affected federal decisions [31]. States and health care coalitions also had diverse interpretations of the data points requested, which further limited the utility of the data (e.g., critical care beds available—some reporting staffed vs. unstaffed beds).
The authors suggest:
All jurisdictions should have access to a MOCC [26] that can facilitate patient placement and redistribution. All hospitals should be required to participate, and expectations for patient distribution/acceptance should be agreed upon prior to an incident.
HHS should better define opportunities and expectations for interstate coordination of information sharing and patient movement. A process for interstate regional prioritization of transportation and other assets to support these activities should be in place.
Each state should have documented processes to reallocate available staff and material resources and compare relevant indicators of impact and need across requesting facilities (e.g., percent usual occupancy in addition to staffing strategies implemented).
Essential elements of information with standard definitions that support system monitoring and load-balancing should be developed and adopted by all states.
Federal grant programs should adopt specific requirements for patient transfer coordination, including MOCC operations and essential elements of information.
Patient transfer decisions should be made irrespective to patient insurance status and other nonclinical factors and should be based on patient loads and clinical needs only.
A national system for health care system information sharing in disasters should be developed and implemented, with consultation from major electronic health record (EHR) providers and other health care information technology companies, coalition leaders, clinicians, state health departments, and health care system stakeholders.
Passive data collection should be ongoing to establish daily and seasonal baselines for health care systems (i.e., direct feed from the EHR) that will better demonstrate the impact of patient surges on a geographic area when an incident occurs including hospital capacity, morbidity, and, to a degree, mortality [32]. An information chain powered by advanced analytics allowing for forecasting, modeling, and predictions should be built into these capabilities.
Facilities should create regional indicators of crisis conditions to improve communication and coordination (e.g., the health care coalition will consider a facility in crisis and will implement the regional MOCC, when patient loads, staffing, or restriction of nonemergency procedures differ significantly between facilities) that help create consistency, direct regional patient movement, or prioritize a facility for resources.
Alternate Care Sites
Prior to COVID-19, many jurisdictions did not have robust plans for establishing community-based alternate care sites (ACS). This was a focus across the nation during the early months of the pandemic for the U.S. Army Corps of Engineers and FEMA [33]. Yet, very few of these sites contributed significantly to the overall number of patients cared for, and they often wound up with disproportionate numbers of uninsured and difficult-to-place long-term care patients, suggesting dumping practices by hospitals onto publicly funded sites [34]. Staffing was a pervasive problem for these facilities, and most of the larger facilities were staffed with federal resources, which is not an option for a majority of jurisdictions in most disasters. Often, successful ACS were in jurisdictions that did not have robust inpatient resources or were geographically isolated [35]. ACS may also be helpful in specific types of events when local health care infrastructure is damaged or insufficient, and COVID-19 significantly advanced this planning.
Planning for hospital-based ACS (e.g., tents in a parking lot near the emergency department (ED) with services limited to assessment and triage, or utilization of non-patient care areas for inpatient care) may offer significant advantages compared to community-based sites, due to proximity to medical resources and personnel. Many hospitals developed plans and set aside assets to ensure maximal care expansion on their campuses prior to activating community-based sites.
The authors suggest:
ACS plans should be updated based on best practices from COVID-19.
Hospitals should plan to maximize alternate care areas at their facilities, as this can often be done more quickly and effectively than opening a community site.
Each state should have defined thresholds for when a community ACS would be opened and how it will be staffed, licensed (if applicable), and operated. This should assume that all available hospital beds will be used first, elective procedures will be halted, and hospitals will have maximized on-site alternate care areas on their campuses.
Clinical Decision Making
Unfortunately, clinicians experienced multiple information deficits throughout the pandemic, including lack of knowledge of the status of their facility, their roles and responsibilities during a disaster, when and how to seek consultations, and an understanding of the foundational elements of CSC and principles of ethical decision making in disasters.
Though many of these issues were addressed by just-in-time education, in many cases clinicians felt disconnected from the formal incident response and felt forced to make ad hoc decisions at the bedside. In some cases, lack of communication about plans or recommendations from the facility level resulted in implicit or covert triage decisions being made by clinicians who believed that the resource situation was worse than it was, and/or determined on their own accord that a patient should not be offered certain interventions. Some of these ad hoc triage decisions were conflated with thinking on medical futility, (i.e., that the treatment would not benefit the patient) though the interventions would have been offered under usual circumstances. Many such decisions were not within their usual scope of practice, though clinicians rarely felt they rose to the level of needing to consult a triage team as outlined in the 2012 CSC guidance [20]. There was often a disconnect between “bedside and boardroom,” as senior leaders were not always aware of the decisions clinical staff were being forced to make, while clinical staff were not well integrated into command-level decisions and did not receive adequate information about available resources.
A key way to avoid or minimize the need for resource triage is to minimize resources expended on unwanted care, including for those who might altruistically decline services in the event of an extreme shortage. However, typical do not resuscitate (DNR) discussions rarely capture these issues. More nuanced discussion and documentation of the wishes of patients, including those around prolonged ventilation, tracheostomy, feeding, renal replacement therapy, and overall goals of care were critical to helping clinicians understand what the patient and family prioritize and helping orient and reorient care during hospitalizations for severe COVID-19. Engagement of family members using digital technology promoted frequent conversation about these issues during COVID-19 but, on the other hand, drastically hampered the development of trust and understanding between family and health professionals that these encounters usually rely on. There is ongoing ethical debate on whether and how to engage patients or family members in conversations about altruistically forgoing services voluntarily in the event of a severe shortage [36,37,38].
The authors suggest:
Health care systems should develop clearer understandings of the required elements of CSC that cover three levels of activity—from the clinician at the bedside, to the health care facility, and finally the coordination level (coalition/state). These levels share requirements across three domains in CSC: information, command/coordination, and policy/practice.
If the required information is not available, or if clinical practice, policy, and system components are not aligned, it is not possible to provide regionally consistent care or to mitigate the crisis effectively (see Figure 2). Planning, education, and exercises are needed to ensure that the required elements are in place and interface successfully with each other.
Critical care and other specialty physicians (e.g., burn, pediatric, infectious disease, trauma surgeons) should be involved in both planning for and response to disasters, as well as integrating directly with the incident command system so that clinical and administrative decisions can be informed together.
FIGURE 2. Key Domains and Requirements in Crisis Standards of Care.
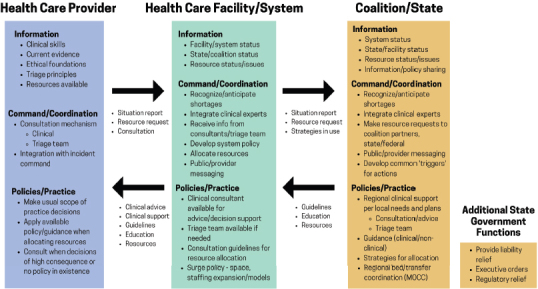
SOURCE: Developed by authors.
Incident command should be aware of all current or impending rationing decisions and work directly with clinical staff and appropriate regional/coalition entities on mitigation strategies and creation of proactive guidance.
Critical care and other physicians should be encouraged to share information in structured and informal communications with clinicians at other facilities to share situational and best practice information.
All clinicians should receive real-time information that is sufficient to understand whether or not they should be triaging specific resources.
All health care practitioners should receive training in basic disaster ethics and decision making, including an understanding of implicit bias.
Clinicians should promote discussion of end-of-life wishes with patients and their families, including the completion of formal advance directives before critical events arise. Health systems should support these conversations through appropriate financing, EHR supports, and fostering a culture of routine advance directive conversations with all adult patients.
Clinicians should discuss with patients and families the consequences of potential interventions, including an honest assessment of likely outcomes, as best they can be ascertained. These assessments should include details such as how likely the patient is to return to baseline functioning, and to elicit what tradeoffs of intervention/discomfort/rehabilitation the patient and family feel would be appropriate. The patient’s wishes should be documented in the EHR and reassessed as the clinical situation changes.
Patients that voluntarily raise the possibility of foregoing services or resources that are in shortage have the legal and ethical right to decline services, but extreme caution must be exercised not to pressure patients into “altruistic” acts that are not consistent with their underlying values.
Facilities should ensure that their legal counsel supports the CSC processes and procedures and understands when and how they will be used. This should include a commitment to providers that they will be legally defended by the health care entity if they are following the facility processes.
Legal and medical associations, as well as public agencies such as the Assistant Secretary for Preparedness and Response should provide education about the increased legal risk for ad hoc rationing decisions versus creating plans and expectations for how the health care system adapts to increased demand, how help is obtained, and how services will be rationed when necessary.
Health care systems should maintain multimodal and transparent communication to staff, particularly nurses and physicians, about the current situation, resources, strategies, trends, and coordination with outside agencies/coalitions, including what steps are being taken to address current and future issues.
Professional and specialty groups should develop brief, targeted educational materials on ethical and procedural CSC principles to be integrated into teaching curricula and adapted by facilities with their specific information embedded. These professional standards can provide both clinical and ethical guidance and may offer some legal protection to practitioners adhering to professional standards in an emergency, even if CSC has not been formally declared by the state.
Triage
Though no health care facility was forced to triage ventilators proactively and overtly, many examples of implicit or covert triage were communicated to the authors in confidence, in which physicians decided, based on their assessment, that they would not offer mechanical ventilation to patients who would have been offered this resource under non-crisis conditions. These decisions were often based on limited initial data suggesting extremely high mortality in the elderly from COVID-19 or limited ventilator resources at the facility. One example highlighting this issue is a case in which multiple ventilators had just been delivered by the state to the facility, but the provider was unaware of the delivery. Fortunately, the provider was alerted to this availability in time to prevent potentially tragic decisions.
Triaging patients for critical care interventions sometimes reflects failures at the provider, facility, health care coalition, or government levels. Often, it suggests the need to plan and coordinate better, and CSC implementation should be limited to situations where no other options exist. In some cases during the COVID-19 pandemic, unfortunately, the solutions either chosen or available to clinicians facing immediate bedside resource shortages resulted in morally injurious bedside decisions—the opposite of the proactive, consistent approach advocated by CSC guidance. Rationing access to extracorporeal membrane oxygenation (ECMO) provides an example of a uniquely limited resource with high staffing demands, and this intervention may require rationing even under routine system conditions (or seasonal conditions such as influenza) [39]. Regional systems for ECMO prioritization have been described in at least one jurisdiction [40].
During the COVID-19 pandemic, triage of critical care resources more often involved not initiating ICU-level care rather than withdrawing or reallocating services. This resulted in higher acuity care sometimes being provided in non-ICU environments or, at an extreme, not receiving usual interventions, such as a ventilator. A reallocation decision (taking a needed resource from a patient to give to another) is different than not initiating care. Reallocation is so clinically, emotionally, and ethically challenging, that those decisions should be made by agreement of multiple providers that the degree of difference in prognosis warrants the reallocation, and only if the initial patient has had appropriate duration of therapy to demonstrate a lack of benefit. The CSC triage team approach in this case continues to have relevance. However, concerns have been raised that the triage team construct espoused in previous IOM/NAM publications was too limited in scope and too restrictive for dynamic environments, and that the described appeals process would not be achievable [20,41]. There is agreement that triage decisions likely to result in death should not be made by a single provider, particularly when there is no accepted guidance for the situation.
Even if statewide CSC plans had been implemented, many contained outdated triage tools. Very few encouraged consideration of disease-/condition-specific prognostic variables, and many relied heavily on Sequential Organ Failure Assessment (SOFA) scores. Limitations of the SOFA score have been recognized and publicized prior to COVID-19 [42,43,44]. The SOFA score should not be used as a significant variable for COVID-19 or other primarily respiratory diseases, as scores are significantly lower than for disease states such as sepsis [45,46,47]. The assignment of points based on the creatinine measurement does not differentiate between preexisting and acute renal disease, particularly penalizes renal failure/dialysis patients, and can exacerbate racial disparities even if race corrections for creatinine are not used [48]. Though the SOFA score may be helpful to compare relative acuity between patients or critical care units, it should play a very limited role in triage methods compared to disease- or injury-specific knowledge. At present, there is no widely available prognostic tool that is reliable enough to exclude individuals from critical care [47,48], and in any event, the need to use such a tool should only apply to binary resources such as ECMO and mechanical ventilation. Such tools are of limited or no utility when considering allocation of elastic resources like medications and dialysis that can be titrated, substituted, and more gracefully degraded.
In many cases, clinicians made decisions to withhold interventions based on the patient’s age and assumed COVID-19 mortality risk. Even though age has direct correlation with risk of death from COVID-19 [51], the initial assessment of that risk was far more grim than later data revealed [52], particularly in the 60- to 70-year-old age group—illustrating the need to have the best available data possible and make it rapidly available to clinicians. Some of the very high early mortality rates among older patients during surge conditions may have been influenced by implicit or covert triage decisions, raising mortality rates among patients from whom resources were withheld. Monitoring and updating practice guidelines with the latest information can help ensure consistency of decision making and avoid incorporation of age-related and other bias.
Discrimination against people with disabilities was found in several clinical situations and state CSC plans. The HHS Office of Civil Rights (OCR) created guidance that patients needed to be assessed as individuals and that providers could only use age in determining resource allocation when there were no better measures available to assess mortality risk and when there was a clear correlation of age with mortality for the specific condition [16,17,18]. The same considerations apply for disabilities. The notion of life-cycle prioritization of younger patients over older is controversial because it is based on ethical norms not held by all cultural groups, and it is not supported by current OCR directives.
Prioritization of specific social groups for critical care triage is highly controversial. Some states include essential worker status in tiebreaking situations (e.g., Colorado), and some did not include them after debate (e.g., Minnesota). Others (e.g., Pennsylvania) have considered including geographic deprivation indices in tiebreakers despite these being based on community and not individual factors. No triage process is value-neutral, and all may have effects on underlying social, economic, and health disparities. Though there is broad agreement that saving lives is an important goal of triage systems, there remains debate on how best to optimize overall benefits while prioritizing attention to those hardest hit in a disaster [46,53].
The authors suggest:
The availability of rapid expert consultation must be ensured for rationing decisions outside of the provider’s normal practice for which there is no practice guideline. This expert or group should have visibility on hospital and regional resources and be able to push the decision and the consequences up to incident command to facilitate both optimal decision making and development of proactive strategies to avoid the ongoing need for triage.
Improved prognostic tools should be prioritized for use and widespread deployment. These should be both generic systems for organ failure assessment as well as condition-specific assessment tools. The marked improvements in data science, including the application of artificial intelligence (AI) and machine learning to improve predictive analytics, should be leveraged to create more accurate triage scoring systems, while monitoring closely for inadvertent creation or exacerbation of inequities (a recognized ethical risk of AI risk prediction algorithms) [54].
In the absence of more accurate scoring systems, state and coalition CSC plans should emphasize coordination of care, access to rapid expert consultation, and situational awareness rather than score-based triage. There should be a review of state triage decision tools, and scoring systems that do not perform well at the individual patient level should be eliminated or minimized. Scoring systems should be used only as a contributing factor in an individualized assessment process, and they should use disease- and injury-specific factors rather than using a generic scoring system. These plans should incorporate routine regional coordination for therapies such as ECMO that may require rationing in non-disaster situations.
The triage process should specifically exclude consideration of age, race, gender, disability, and other inappropriate discriminators, and those conducting triage should be trained on implicit bias with the aim of mitigating the inadvertent exacerbation of disparities.
The state or region’s attorney general’s office should review the state plans with specific attention to civil rights protections.
The critical care triage processes should exclude factors not related to medical prognosis or resource utilization (e.g., status as a health care worker, location of residence, status as a parent, status as an essential worker, status as a child) unless these are shown to be socially and legally accepted by the community and supported by the state.
Social factor incorporation must be procedurally sound, address the target goal, and be easily addressed and implemented by the bedside clinician. Geographical and other population-based determinants of impact have significant value for prioritizing interventions prior to hospitalization but are controversial to use in prioritizing assignment of critical care resources, as there is no assurance that the goals of the intended correction are met at the individual level. That is, a privileged resident of an area scoring high on a social vulnerability index may be inappropriately prioritized over a disadvantaged individual that lives outside a prioritized area. This is not an issue in community-based interventions where the community at large benefits from targeted assignment of assets but is problematic when assigning life-saving resources [55,56].
Plans and education should acknowledge that withholding usual interventions is triage and should only be performed in circumstances that require such restrictions. Providers must be transparent with patients and family members when a care decision is being made because the therapy will confer no benefit (i.e., futility) versus when resource triage is required based on scarcity.
Plans should specify that the threshold for reallocating lifesaving resources should not be merely a “possible better chance of survival,” as might be appropriate during an allocation between two patients not yet receiving the intervention. There should be a significant difference in likelihood of survival agreed upon by more than one expert provider.
Health care facilities should define the situations in which an appeals process may be reasonable and develop a different model to ensure that bias is avoided when time-sensitive decisions are needed— particularly if multiple appeals are occurring simultaneously. Ensure appropriate documentation to support quality assurance review, including by the consulting provider.
Hospitals and health systems should develop policies and processes for discontinuation of potentially non-beneficial therapies. These should explicitly address resources that may be in shortage, such as ECMO, and should emphasize accurate and complete communication with patients and families when a resource is being provided as a trial of therapy rather than as a resource indefinitely assigned to a patient.
Supplies
COVID-19 illustrated in graphic fashion that a just-in-time supply chain struggles in the face of global demand. Some of the biggest supply problems faced could have been anticipated based on the 2009 H1N1 experience, but solutions were often avoided because they involved too much perceived effort, lacked market drivers (e.g., reusable PPE would generate less revenue than disposable), or were judged too expensive (e.g., extra ventilators). Shortages of PPE were a known risk after the 2009 H1N1 pandemic, so the scope and the duration of shortages and their effects on provider health, well-being, and workplace morale should have been no surprise during the COVID-19 pandemic. Also, not surprisingly, nations (including the United States) often prevented export of PPE, medications, and vaccines, keeping these for domestic use regardless of international contracts and obligations, and sometimes against public health best practices to stop the pandemic most efficiently worldwide.
In some cases, there were problems with both resource availability and distribution. For instance, high-flow nasal cannula oxygen emerged as a key therapy for COVID-19 but placed extraordinary demands on hospital oxygen systems. Flow limitations for existing oxygen plumbing, freezing of vaporizers, and inability to obtain timely delivery created numerous problems. In some cases, oxygen conservation strategies were not enacted in facilities despite low pressure alarms. The authors suggest:
A systematic examination of U.S. medical supply chain resiliency, with a focus on disasters and likely shortages during disasters, what can be learned from routine medication shortages to inform disaster preparedness and response, and strategies for prevention and mitigation of supply disruptions. This should include an analysis of U.S. reliance on international resources, and reliance of our international partners on U.S. resources to fully assess the benefits and risks of the current push for onshoring medical supply manufacturing.
A new approach to PPE development, design, and willingness to use, including respirators with cleanable surfaces, elastomeric models designed specifically for health care markets, standardizing the testing and assessment of simple masks, and refining categorization of barrier materials.
Improving caches of materials (including agreeing on reasonable surplus stocks of ventilators, PPE, and medications to support all-hazards critical care) at the facility, health system, state, and federal level.
Dedicated planning around oxygen, as it represents a key vulnerability for hospitals, including changes to hospital design to allow higher volume delivery to inpatient units, developing strategies for emergency conservation measures when demand is high, and explicit triggers for implementation of specific conservation strategies.
Staffing
Availability of staff, particularly nursing and respiratory therapy, to support expanded COVID-19 critical care was a pervasive issue and the subject of a rapid expert consultation by the National Academies of Sciences, Engineering, and Medicine [57]. In many cases, contract personnel, federal and state disaster team members, and others played a crucial role enabling care expansion. Severe financial impact on health care systems was not an expected consequence of a pandemic but resulted in widespread furloughs and layoffs driven by reduced ED, outpatient, and procedural visits. [58].
Nurse-to-patient ratios often remained stretched for months at a time, contributing to burnout. Ironically, at the same time, many health professionals involved in outpatient and surgical care were furloughed or laid off, though some transitioned from surgical and outpatient roles to inpatient roles. Some hospitals used nontraditional staff to provide care in intensive care environments, supervised by critical care staff and nurses in ratios that expanded and contracted to meet the demands with available staff. Many states and facilities made requests for staffing assistance that were difficult to prioritize without shared data on the types of staffing contingencies invoked (e.g., facilities pronounced themselves in crisis to seek assistance despite wildly different availability of staff).
Just-in-time training and mentoring helped providers adjust to new roles, but the mental health impacts of high acuity, contagion, long duration surges, and often new or expanded responsibilities was immense and likely will cause workforce repercussions for years. Staff are not infinitely expandable, and in some cases, states inferred that triage of patients would occur (or did occur) due to staffing issues, but binary types of triage (e.g., critical care vs. palliative care) should be avoided when staffing is the limiting factor [57]. Instead, prioritization of the sickest patients to be cared for by the staff with the highest level of training/competency is appropriate, as are other strategies to try to match staff to patient needs when staffing is constrained.
The authors suggest:
Hospitals should include the possibility of extreme staffing shortages in their surge capacity and CSC planning, and educate staff about the plans, new roles, and necessary competencies.
Health care facilities should ensure dialogue with their unions and appropriate flexibility in collective bargaining agreements to allow a safe and flexible disaster response.
National curricula should be refined and implemented by hospitals to improve nursing and physician staff comfort in stepping up to provide a higher level of care in contingency or crisis scenarios. This should be reinforced by just-in-time training.
Health care coalitions and states should agree on commonly accepted definitions for crisis staffing (e.g., use of nontraditional providers in critical care environments, increase in nurse-to-patient ratios beyond a particular percentage, use of tiered supervised staffing) to enable better situational awareness and improved load-balancing of patients and allocation of available staff.
Concluding Suggestions
The prior CSC work and its contributions during COVID-19 to policy and practice should be revisited and updated in collaboration with national experts in medicine, ethics, law, and other disciplines, with an emphasis on the need to avoid crisis conditions by planning for systems of care that maintain consistency across regions through patient and resource movement.
Documents such as this one and those that result from future workshops and committees should be used as discussion drivers at the hospital, health care system, health care coalition, state, and federal levels to change policy and process, and optimally be written into federal preparedness program expectations (e.g., requirements of facilities and coalitions under the HHS/ASPR Hospital Preparedness Program). There is also a clear need to include public health departments and officials, as well as state governors, in discussions to understand when CSC may be invoked and what the state role is relative to declarations, legal protections, best practices, and other CSC domains. The actions of the states during COVID-19 were diverse and varied, from overly broad declarations of CSC with long-duration immunity for providers, to no action or acknowledgment of the situation in the face of overwhelming patient volumes that required triage of resources such as dialysis. In many states, no specific legal protection was afforded to physicians forced to make triage decisions, which contributed to opaque decision processes. States and health care systems should emphasize transparency and facilitate better decision making by providing consultation and clinical advice in scarce resource situations.
Prior to COVID-19 there was a recognized gap in clinician (physician, advanced practice providers, nursing staff) understanding of the ethics and process around resource triage and allocation. Building off scarcity thinking and everyday challenges around medication shortages, providers should receive foundational education on the basics of rationing, triage, the shared duty to steward resources, and current weaknesses in assessing individual prognosis (with limited disease- and injury-specific exceptions). The total time commitment should be relatively small, but a shared understanding of health care workers’ obligations, limitations, plans, and processes to address shortages would help tremendously to improve consistency and reduce provider moral distress.
The authors believe that specialty societies, major health care systems, and private sector health information technology partners should work together to leverage AI to assist in developing better prognostic tools for critical illness in general, as well as for disease- and injury-specific situations, and to develop systems for tracking the effects of using these algorithms on key measures of equity. The ability to leverage AI will also offer opportunity during a novel event to determine risk factors and treatment efficacy, as well as to improve supply chain decision making, including the proactive steps necessary to supplement resources anticipated to be in short supply.
The authors hope that technological advances will result in meaningful improvements to PPE and will also drive changes in critical medical equipment. Ventilators will be cheaper and easier to use, with standard circuits and next generation autonomous systems that can augment the role of respiratory therapists by using machine-learning algorithms to adjust ventilator settings. Both software and hardware changes to devices as well as increased integration of remote patient monitoring, the use of wearables, sensors, and other means of virtual health care could help reduce the strain on overburdened health care facilities by honing decision-making skills about who needs to seek care and when. The use of such tools can also help to standardize care (through greater use of checklists and care plans), reduce nursing workload (by allowing medication drips and ventilators to integrate with patient monitoring and auto-titrate within specified ranges of hemodynamic or respiratory parameters), and prioritize attention in busy units by having graded alarms and notifications, among other improvements.
When the initial CSC recommendations were first created in anticipation of the second wave of the 2009 H1N1 influenza pandemic, the authors recognized that future events and learnings would surely result in improvements and revisions to those initial recommendations [19]. While there have been some incremental changes made in the ensuing eleven years, informed by research as well as discrete events such as the Haiti earthquake, COVID-19 provides the emergency preparedness and response community a distillation of experiences that allows health care planners and providers to systematically incorporate CSC learnings, successes, and failures. Unless the time is dedicated to engage the providers, do the planning, perform the research, develop the systems, test the assumptions, and ensure availability of the key resources needed to meet the next challenge, the public will face dangerous shortages and inequities in the future, yet health care providers will be no better prepared. The toll of COVID-19 has been high enough. Health care providers and organizations cannot afford to ignore the lessons and risk additional provider and patient losses in future events that are sure to happen. It is quite apparent that the age of epidemics is upon us, and that the threats of climate change and geologic instability, let alone risks due to geopolitical threats, continue to make planning for catastrophic emergencies a matter of national security, not simply something to put off to another time. The time is now to do something with what we have learned.
Acknowledgments
The authors would like to acknowledge Peter Pons, Denver Health Medical Center; Vicki Sakata, Northwest Healthcare Response Network; and Vikramjit Mukherjee, Bellevue Medical ICU and the New York University School of Medicine for their valuable contributions to this paper.
Funding Statement
The views expressed in this paper are those of the authors and not necessarily of the authors’ organizations, the National Academy of Medicine (NAM), or the National Academies of Sciences, Engineering, and Medicine (the National Academies). The paper is intended to help inform and stimulate discussion. It is not a report of the NAM or the National Academies. Copyright by the National Academy of Sciences. All rights reserved.
Footnotes
Conflict-of-Interest Disclosures: Dr. Wynia reports receiving grants from ASPR and NIH (CTSA).
Contributor Information
John L. Hick, Hennepin Healthcare and University of Minnesota.
Dan Hanfling, In-Q-Tel and George Washington University.
Matthew K. Wynia, University of Colorado.
Eric Toner, Johns Hopkins Center for Health Security.
References
- 1.National Academies of Science, Engineering, and Medicine. Rapid expert consultation on crisis standards of care for the COVID-19 pandemic (March 28, 2020) Washington, DC: The National Academies Press; 2021. [DOI] [PubMed] [Google Scholar]
- 2.Manchanda EC, Couillard C, Sivashanker K. Inequity in crisis standards of care. New England Journal of Medicine. 2020;383(4):e16. doi: 10.1056/NEJMp2011359. [DOI] [PubMed] [Google Scholar]
- 3.Kosar CM, White EM, Feifer RA, Blackman C, Gravenstein S, Panagiotou OA, McConeghy K, Mor V. COVID-19 mortality rates among nursing home residents declined from March to November 2020. Health Affairs. 2021;40(4):655–663. doi: 10.1377/hlthaff.2020.02191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh GK, Lin CCC. Area deprivation and inequalities in health and health care outcomes. Annals of Internal Medicine. 2019;171(2):131–132. doi: 10.7326/M19-1510. [DOI] [PubMed] [Google Scholar]
- 5.Gould E, Wilson V. Economic Policy Institute. 2020. [August 25, 2021]. Black workers face two of the most lethal preexisting conditions for coronavirus—racism and economic inequality. https://www.epi.org/publication/black-workers-covid/ [Google Scholar]
- 6.Wadhera RK, Wadhera P, Gaba P, Figueroa JF, Joynt Maddox KE, Yeh RW, Shen C. Variation in COVID-19 Hospitalizations and Deaths Across New York City Boroughs. JAMA. 2020;323(21):2192–2195. doi: 10.1001/jama.2020.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Webb Hooper M, Nápoles AM, PérezStable EJ. COVID-19 and Racial/Ethnic Disparities. JAMA. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. https://doiorg/10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nau C, Bruxvoort K, Navarro RA, Chevez SG, Hogan TA, Ironside KR, Ludwig SM, Ngo-Metzger Q, Mourra NR, Young DR, Sangha N, Turner BP, Li IX, Padilla A, Chen A, Hong V, Yau V, Tartof S. Annals of Internal Medicine. 2020. COVID-19 inequities across multiple racial and ethnic groups: results from an integrated health care organization. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jean-Jaques M, Bauchner H. Vaccine distribution—Equity left behind? JAMA. 2021;325(9):829–830. doi: 10.1001/jama.2021.1205. [DOI] [PubMed] [Google Scholar]
- 10.National Academies of Science, Engineering, and Medicine. Rapid Expert Consultation on Allocating COVID-19 Monoclonal Antibody Therapies and Other Novel Therapeutics (January 29, 2021) Washington, DC: The National Academies Press; 2021. [DOI] [Google Scholar]
- 11.Galewitz P. Kaiser Health News. 2021. [August 25, 2021]. Vermont to give minority residents vaccine priority. https://khn.org/news/article/vermont-gives-blacks-and-other-minority-residents-vaccine-priority/ [Google Scholar]
- 12.Schmidt H, Gostin LO, Williams MA. Is it lawful and ethical to prioritize minorities for COVID-19 vaccines? JAMA. 2020;324(20):2023–2024. doi: 10.1001/jama.2020.20571. [DOI] [PubMed] [Google Scholar]
- 13.Schmidt H. Stat News. 2021. [August 25, 2021]. Disadvantage indices can help achieve equitable vaccine allocation. https://www.statnews.com/2021/02/01/disadvantage-indices-can-help-achieve-equitable-vaccine-allocation/ [Google Scholar]
- 14.Centers for Disease Control and Prevention. CDC/ATSDR Social Vulnerability Index. 2021. [August 25, 2021]. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html. [Google Scholar]
- 15.Plathoff E, Garnham JP. Texas Tribune. 2021. Jan 20, [August 25, 2021]. Dallas County axes plan to prioritize vaccinating communities of color after state threatens to slash allocation. https://www.texastribune.org/2021/01/20/dallas-vaccine-plan-communities-of-color/ [Google Scholar]
- 16.U.S. Department of Health and Human Services, Office for Civil Rights. OCR reaches early case resolution with Alabama after it removes discriminatory ventilator triaging guidelines. 2020. [August 25, 2021]. https://www.hhs.gov/guidance/document/ocrreaches-early-case-resolution-alabama-after-it-removes-discriminatory-ventilator. [Google Scholar]
- 17.U.S. Department of Health and Human Services, Office for Civil Rights. Civil rights and COVID-19. Washington, DC: 2020. [August 25, 2021]. https://www.hhs.gov/civil-rights/for-providers/civil-rights-covid19/index.html. [Google Scholar]
- 18.HHS Office for Civil Rights in Action. BULLETIN: Civil Rights, HIPAA, and the Coronavirus Disease 2019 (COVID-19) 2020. [August 25, 2021]. https://www.hhs.gov/sites/default/files/ocr-bulletin-3-28-20.pdf. [Google Scholar]
- 19.Institute of Medicine. Guidance for establishing crisis standards of care for use in disaster situations: A letter report. Washington, DC: The National Academies Press; 2009. [DOI] [PubMed] [Google Scholar]
- 20.Institute of Medicine. Crisis standards of care: A systems framework for catastrophic disaster response: Volume 1: Introduction and CSC framework. Washington, DC: The National Academies Press; 2012. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Summary for healthcare facilities: Strategies for optimizing the supply of PPE during shortages. 2020. [August 25, 2021]. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/strategies-optimize-ppe-short-ages.html. [Google Scholar]
- 22.Grisham ML. New Mexico Governor’s Executive Order 2020-083. 2020. [August 25, 2021]. https://cv.nmhealth.org/wp-content/uploads/2020/12/Executive-Order-2020-083.pdf. [Google Scholar]
- 23.Koop C. Fort Worth Star Telegram. 2020. Jul 24, [August 25, 2021]. COVID-19 patients will be “sent home to die” if deemed too sick, Texas county says. https://www.star-telegram.com/news/coronavirus/article244443257.html. [Google Scholar]
- 24.Hick JL, Barbera JA, Kelen GD. Refining surge capacity: Conventional, contingency, and crisis capacity. Disaster Medicine and Public Health Preparedness. 2009;3(Suppl 1):S59–S67. doi: 10.1097/DMP.0b013e31819f1ae2. [DOI] [PubMed] [Google Scholar]
- 25.Kadri SS, Sun J, Lawandi A, Strich JR, Busch LM, Keller M, Babiker A, Yek C, Malik S, Krack J, Dekker JP, Spaulding AB, Ricotta E, Powers III JH, Rhee C, Klompas M, Athale J, Boehmer TK, Gundlapalli AV, Bentley W, Datta SD, Danner RL, Warner CYS. Annals of Internal Medicine. 2020. Association between caseload surge and COVID-19 survival in 558 US hospitals, March to August 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Response Coordination Center Healthcare Resilience Task Force. Medical Operations Coordination Cell Toolkit. 2020. [August 25, 2021]. https://files.asprtracie.hhs.gov/documents/fema-mocc-toolkit.pdf. [Google Scholar]
- 27.Valin JP, Gulley S, Keidan B, Perkins K, Price CS, Neff W, Winfield G, Tad-y D. NEJM Catalyst. 2020. Physician executives guide a successful COVID-19 response in Colorado. [DOI] [Google Scholar]
- 28.Evans M, Berzon A, Hernandez D. Wall Street Journal. 2020. Oct 19, [August 25, 2021]. Some California hospitals refused COVID-19 transfers for financial reasons, state emails show. https://www.wsj.com/articles/some-california-hospitalsrefused-covid-19-transfers-for-financial-reasons-state-emails-show-11603108814. [Google Scholar]
- 29.Fink S. The New York Times. 2021. Feb 8, [August 25, 2021]. Dying of COVID in a “separate and unequal” LA hospital. https://www.nytimes.com/2021/02/08/us/covid-los-angeles.html. [Google Scholar]
- 30.U.S. Department of Health and Human Services, Office of the Assistant Secretary for Preparedness and Response. Hospital Preparedness Program. 2021. [August 25, 2021]. https://www.phe.gov/Preparedness/planning/hpp/Pages/default.aspx. [Google Scholar]
- 31.U.S. Department of Health and Human Services. COVID-19 Guidance for Hospital Reporting and FAQ for Hospitals, Hospital Laboratories, and Acute Care Facility Data Reporting. 2021. [August 25, 2021]. https://www.hhs.gov/sites/default/files/covid-19-faqs-hospitals-hospital-laboratory-acute-care-facility-data-reporting.pdf. [Google Scholar]
- 32.National Academies of Science, Engineering, and Medicine. A framework for assessing mortality and morbidity after large-scale disasters. Washington, DC: 2020. [DOI] [PubMed] [Google Scholar]
- 33.U.S. Department of Health and Human Services, Office of the Assistant Secretary for Preparedness and Response. Federal Healthcare Resilience Task Force Alternate Care Site Toolkit Third Edition. 2020. [August 25, 2021]. https://files.asprtracie.hhs.gov/documents/acs-toolkit-ed1-20200330-1022.pdf. [Google Scholar]
- 34.Curwen T. Los Angeles Times. 2020. May 19, [August 25, 2021]. LA surge hospital for COVID-19 patients to close by the end of June. https://www.latimes.com/california/story/2020-05-19/la-surge-hospi-tal-coronavirus-covid-19-closing-end-of-june. [Google Scholar]
- 35.Breyre AM, Sloane B, Herring C, Backer H, McGinnis T, Staats K. Establishment of an Alternate Care Site (ACS) in Imperial County During COVID-19. Western Journal Emergency Medicine. 2021;22(3):608–613. doi: 10.5811/westjem.2020.12.49237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Span P. The New York Times. 2020. Jul 31, [August 25, 2021]. Should youth come first in coronavirus care? https://www.nytimes.com/2020/07/31/health/coronavirus-ethics-rationing-elderly.html. [Google Scholar]
- 37.Savulescu J, Wilkinson D. Journal of Medical Ethics. 2020. [August 25, 2021]. Extreme altruism in a pandemic (blog post) https://blogs.bmj.com/medical-ethics/2020/04/23/extreme-altruism-in-a-pandemic/ [Google Scholar]
- 38.Doukas DJ, Stout N. Altruism discussions in the time of pandemic: May we ask, may they tell? [August 25, 2021];Journal of Clinical Ethics. 2021 32(1):13–19. https://pubmed.ncbi.nlm.nih.gov/33416515/ [PubMed] [Google Scholar]
- 39.Fink S. The New York Times. 2021. Jul 12, [August 25, 2021]. The rationing of a last-resort COVID treatment. https://www.nytimes.com/2021/07/12/us/covidtreatment-ecmo.html. [Google Scholar]
- 40.Prekker ME, Brunsvold ME, Bohman JK, Fischer G, Gram KL, Litell JM, Saavedra-Romero R, Hick JL. Regional planning for extracorporeal membrane oxygenation during coronavirus disease 2019. Chest. 2020;158(2):603–607. doi: 10.1016/j.chest.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Supady A, Curtis JR, Abrams D, Lorusso R, Bein T, Boldt J, Brown CE, Duerschmied D, Metaxa V, Brodie D. Allocating scarce intensive care resources during the COVID-19 pandemic: practical challenges to theoretical frameworks. Lancet Respiratory Medicine. 2021;9(4):430–434. doi: 10.1016/S2213-2600(20)30580-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rubinson L, Knebel A, Hick JL. MSO-FA: An important step forward, but are we spending too much time on the SOFA? Disaster Medicine and Public Health Preparedness. 2010;4(4):270–272. doi: 10.1001/dmp.2010.41. [DOI] [PubMed] [Google Scholar]
- 43.U.S. Department of Health and Human Services. SOFA score what is it and how to use it in triage. 2017. [August 25, 2021]. https://files.asprtracie.hhs.gov/documents/aspr-tracie-sofa-score-fact-sheet.pdf. [Google Scholar]
- 44.Kahn Z, Hulme J, Sherwood N. An assessment of the validity of SOFA score based triage in H1N1 critically ill patients during an influenza pandemic. Anaesthesia. 2009;64(12):1283–1288. doi: 10.1111/j.1365-2044.2009.06135. [DOI] [PubMed] [Google Scholar]
- 45.Wunsch H, Hill AD, Bosch N, Adhikari NKJ, Rubenfeld G, Walkey A, Ferreyro BL, Tillmann BW, Amaral ACKB, Scales DC, Fan E, Cuthbertson BH, Fowler RA. Comparison of 2 triage scoring guidelines for allocation of mechanical ventilators. JAMA Network Open. 2020;3(12):e2029250. doi: 10.1001/jamanetworkopen.2020.29250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Raschke RA, Agarwal A, Rangan P, Heise CW, Curry SC. Discriminant accuracy of the SOFA score for determining the probable mortality of patients with COVID-19 pneumonia requiring mechanical ventilation. JAMA. 2021;325(14):1469–1470. doi: 10.1001/jama.2021.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wynia M. Crisis triage: attention to values in addition to efficiency. JAMA Network Open. 2020;3(12):e2029326. doi: 10.1001/jamanetworkopen.2020.29326. [DOI] [PubMed] [Google Scholar]
- 48.Schmidt H. The New York Times. 2020. Apr 15, [August 25, 2021]. The way we ration ventilators is biased. https://www.nytimes.com/2020/04/15/opinion/covid-ventilator-rationing-blacks.html. [Google Scholar]
- 49.Wynia M, Sottile PD. Ethical triage demands a better triage survivability score. American Journal of Bioethics. 2020;20(7):75–77. doi: 10.1080/15265161.2020.1779412. [DOI] [PubMed] [Google Scholar]
- 50.Maves RC, Downar J, Dichter JR, Hick JL, Devereaux A, Geling JA, Kissoon N, Hupert N, Niven AS, King MA, Rubinson LL, Hanfling D, Hodge JG, Jr., Marshall MF, Fischkoff K, Evans LE, Tonelli MR, Wax RS, Seda G, Parrish JS, Truog RD, Sprung CL, Christian MD ACCP Task Force for Mass Critical Care. Triage of Scarce Critical Care Resources in COVID-19 - An Implementation Guide for Regional Allocation: An Expert Panel Report of the Task Force for Mass Critical Care and the American College of Chest Physicians. Chest. 2020;158(1):212–225. doi: 10.1016/j.chest.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Centers for Disease Control and Prevention. Risk for COVID-19 infection, hospitalization, and death by age group. 2021. [August 25, 2021]. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html. [Google Scholar]
- 52.King CS, Sahjwani D, Brown AW, Feroz S, Cameron P, Osborn E, Desai M, Djurkovic S, Kasarabada A, Hinerman R, Lantry J, Shlobin OA, Ahmad K, Khangoora V, Aryal S, Collins AC, Speir A, Nathan S. PLoS One. 2020. Outcomes of mechanically ventilated patients with COVID-19 associated respiratory failure. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wasserman D, Persad G, Millum J. Setting priorities fairly in response to COVID-19: identifying overlapping consensus and reasonable disagreement. Journal of Law and the Biosciences. 2020;7(1):Isaa044. doi: 10.1093/jlb/lsaa044. https://dx.doi.org/10.1093%2Fjlb%2Flsaa044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Richens JG, Lee CM, Johri S. Improving the accuracy of medical diagnosis with causal machine learning. Nature Communications. 2020;11(3923) doi: 10.1038/s41467-02017419-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Blitzer D, Regan S, Fischkoff D, Fischkoff K. Why health care workers should receive priority care for COVID-19. 2020. [August 25, 2021]. https://www.thehastingscenter.org/why-health-care-workers-should-receive-priority-care-for-covid-19/ [Google Scholar]
- 56.Rothstein MA. Should health care providers get treatment priority in an influenza pandemic? Journal of Law, Medicine, & Ethics. 2010;38(2):412–419. doi: 10.1111/j.1748-720X.2010.00499.x. https://dx.doi.org/10.1111%2Fj.1748-720X.2010.00499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.National Academies of Science, Engineering, and Medicine. Rapid expert consultation on staffing considerations for crisis standards of care for the COVID-19 pandemic (July 28, 2020) Washington, DC: The National Academies Press; 2021. [DOI] [Google Scholar]
- 58.Lagasse J. Healthcare Finance. 2021. Feb 22, [August 25, 2021]. U.S. hospitals and health systems face a long road to recovery. https://www.healthcarefinancenews.com/news/us-hospitals-and-health-systems-face-long-road-recovery. [Google Scholar]


