Abstract
Objectives: To describe the profile of hospital deaths in Brazil according to cause of admission during the pre-pandemic (2019) and pandemic periods (2020).
Methods: Descriptive study based on individual-level records of all hospital admissions with death outcomes reimbursed by the Brazilian National Health System in 2019 and 2020.
Results: The number of hospital deaths increased by 16.7% in 2020 compared with 2019 (522,686 vs 609,755). Coronavirus disease 2019 (COVID-19) was associated with 19.5% (118,879) of all hospital deaths in 2020, surpassing diseases of the circulatory system (15.4%, 93,735) and diseases of the respiratory system (14.9%, 91,035).
Conclusions: COVID-19 was the main cause of death in public hospitals in Brazil in 2020.
Keywords: COVID-19, SARS-CoV-2l, Hospital mortality, Cause of death, Unified health system, Brazil
Introduction
As a consequence of the high death toll of coronavirus disease 2019 (COVID-19), some countries, such as the USA, have already reported COVID-19 as one of the leading causes of death in 2020 (Ahmad and Anderson, 2021). Since the beginning of the COVID-19 pandemic, Brazil has experienced a rapidly increasing number of cases and deaths (Castro et al., 2021b). In addition, COVID-19 has spread asymmetrically and unequally across social and economic groups, as well as geographic regions, in Brazil, with the most vulnerable populations and the Northeastern and Northern regions being the most affected (Dall'Alba and Rocha, 2021; Rocha et al., 2021). On this basis, this article presents and discusses data on the leading causes of death in public hospitals in Brazil in 2019 and 2020.
Methods
After extracting 1,132,441 records from all in-hospital deaths in 2019 and 2020 from the National Hospital Information System (SIH/SUS), deaths were classified by cause of admission based on the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10). Any admission including ICD-10 (‘U07.1’, ‘U07.2’, ‘B97.2’ or ‘B34.2’) (Tanno et al., 2020) or specific COVID-19 medical procedure codes (‘0802010296’, ‘0802010300’, ‘0802010318’ or ‘0303010223’) (Brasil, Ministério da Saúde, Departamento de Informática do SUS, 2021) was classified as a ‘COVID-19’ admission. The data cover all the hospital deaths that occurred in 2019 and 2020 (from January to December). Descriptive statistics on patient characteristics (sex, age, ethnicity), severity of hospital admission (length of stay, intensive care unit admission) and geographic region are presented by cause of admission in 2019 and 2020.
All analyses were conducted in R language and based on de-identified individual-level data available on the hospitalization authorization repository (ftp://ftp.datasus.gov.br/dissemin/publicos/SIHSUS/200801_/Dados) at the end of August 2021.
Results
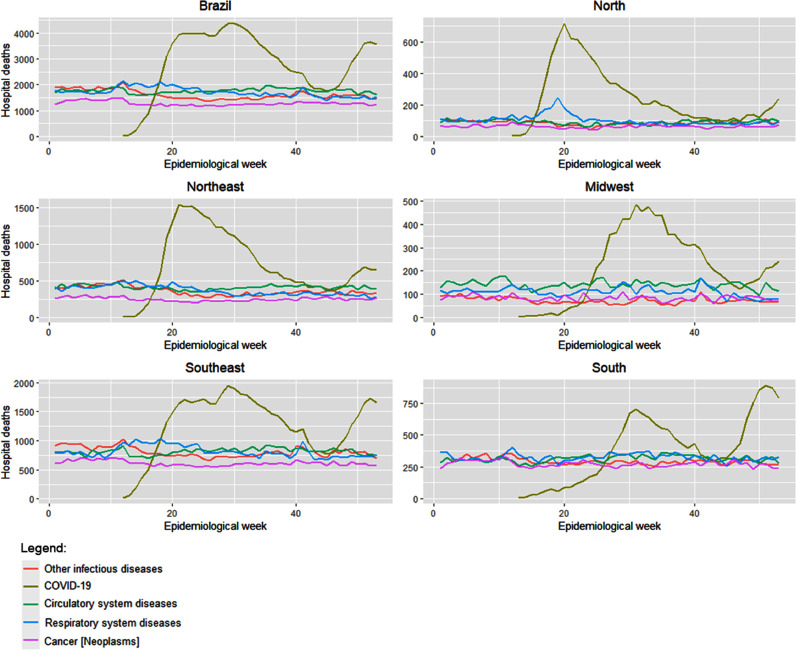
Diseases of the circulatory system were the leading cause of hospital death in 2019 (18.7%, 97,867), followed by infectious diseases (18.7%, 97,842), diseases of the respiratory system (18.7%, 97,585) and cancer (13.7%, 71,550) (Table 1 ). Compared with 2019, the total number of hospital deaths increased by 16.7% in 2020 (522,686 vs 609,755, respectively). Although this increase follows the trend of deaths related to COVID-19, there was a slight decrease in other causes of death, ranging from a 4.2% decrease in diseases of the circulatory system to a 12.3% decrease in other infectious diseases (excluding COVID-19). Figure 1 shows that although the death trends from other causes remained relatively stable throughout 2020, COVID-19 was the main cause of hospital death in Brazil by the 20th epidemic week (10–16 May 2020), except in the South and Midwest regions. By the end of 2020, COVID-19 was the main cause of hospital death (19.5%, 118,879), followed by diseases of the circulatory system (15.4%, 93,735), diseases of the respiratory system (14.9%, 91,035), other infectious diseases (14.1%, 85,830) and cancer (11.1%, 67,808).
Table 1.
Number of hospital deaths by cause of admission in public hospitals in Brazil in 2019 and 2020.
| 2019 |
2020 |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cause | Circulatory system diseases | Infectious diseases | Respiratory system diseases | Cancer (neoplasms) | Other causes | Total | COVID-19 | Circulatory system diseases | Respiratory system diseases | Infectious diseases | Cancer (neoplasms) | Other causes | Total |
| Sex | |||||||||||||
| Female | 50,674 | 51,017 | 50,643 | 36,142 | 89,532 | 278,008 | 68,323 | 49,083 | 49,263 | 45,044 | 33,818 | 86,775 | 332,306 |
| Male | 47,193 | 46,825 | 46,942 | 35,408 | 68,310 | 244,678 | 50,556 | 44,652 | 41,772 | 40,786 | 33,990 | 65,693 | 277,449 |
| Age range (years) | |||||||||||||
| 0–19 | 983 | 3719 | 3055 | 1396 | 17,896 | 27,049 | 754 | 912 | 2072 | 2898 | 1272 | 17,257 | 25,165 |
| 20–39 | 3154 | 6094 | 3669 | 4200 | 13,551 | 30,668 | 5020 | 3320 | 4034 | 5519 | 3993 | 13,924 | 35,810 |
| 40–59 | 18,013 | 18,067 | 13,270 | 20,963 | 31,812 | 102,125 | 23,633 | 17,859 | 13,673 | 16,614 | 20,147 | 31,639 | 123,565 |
| 60–79 | 48,721 | 41,644 | 40,295 | 36,155 | 59,059 | 225,874 | 59,728 | 46,494 | 39,253 | 36,985 | 34,258 | 56,520 | 273,238 |
| ≥80 | 26,996 | 28,318 | 37,296 | 8836 | 35,524 | 136,970 | 29,744 | 25,150 | 32,003 | 23,814 | 8138 | 33,128 | 151,977 |
| Ethnicity | |||||||||||||
| Black | 4574 | 5268 | 3985 | 3704 | 7227 | 24,758 | 6905 | 4746 | 4998 | 4980 | 3977 | 7545 | 33,151 |
| Brown | 32,596 | 31,469 | 29,539 | 24,663 | 55,339 | 173,606 | 40,401 | 31,336 | 28,300 | 28,180 | 23,082 | 53,213 | 204,512 |
| Native Brazilian | 78 | 121 | 200 | 42 | 255 | 696 | 243 | 62 | 186 | 113 | 38 | 269 | 911 |
| White | 35,351 | 35,340 | 39,696 | 30,795 | 54,616 | 195,798 | 37,435 | 33,887 | 35,167 | 31,028 | 29,425 | 52,363 | 219,305 |
| Yellow | 2112 | 2504 | 2224 | 1046 | 3255 | 11,141 | 3968 | 2029 | 2204 | 2113 | 1026 | 3436 | 14,776 |
| Not informed | 23,156 | 23,140 | 21,941 | 11,300 | 37,150 | 116,687 | 29,927 | 21,675 | 20,180 | 19,416 | 10,260 | 35,642 | 137,100 |
| Length of stay (days) | |||||||||||||
| ≤7 | 64,998 | 53,658 | 61,475 | 43,874 | 102,199 | 326,204 | 60,051 | 63,440 | 59,117 | 48,174 | 43,185 | 100,637 | 374,604 |
| 7–14 | 17,550 | 22,034 | 19,814 | 14,686 | 29,235 | 103,319 | 32,204 | 16,495 | 17,859 | 19,100 | 13,884 | 27,729 | 127,271 |
| >14 | 15,319 | 22,150 | 16,296 | 12,990 | 26,408 | 93,163 | 26,624 | 13,800 | 14,059 | 18,556 | 10,739 | 24,102 | 107,880 |
| ICU admission | |||||||||||||
| No | 61,832 | 58,812 | 70,708 | 57,661 | 98,519 | 347,532 | 50,694 | 57,395 | 63,190 | 49,880 | 54,346 | 92,573 | 368,078 |
| Yes | 36,035 | 39,030 | 26,877 | 13,889 | 59,323 | 175,154 | 68,185 | 36,340 | 27,845 | 35,950 | 13,462 | 59,895 | 241,677 |
| Region | |||||||||||||
| Midwest | 7525 | 4512 | 6383 | 4534 | 10,020 | 32,974 | 8841 | 7485 | 5834 | 3841 | 4445 | 9669 | 40,115 |
| Northeast | 23,530 | 22,679 | 22,436 | 14,115 | 39,851 | 122,611 | 30,534 | 21,597 | 19,384 | 19,032 | 13,086 | 38,412 | 142,045 |
| North | 5138 | 4529 | 5365 | 3182 | 9698 | 27,912 | 10,374 | 4761 | 5414 | 4480 | 3280 | 9512 | 37,821 |
| Southeast | 44,636 | 48,809 | 43,352 | 34,925 | 72,821 | 244,543 | 53,192 | 43,318 | 43,166 | 42,794 | 32,591 | 69,759 | 284,820 |
| South | 17,038 | 17,313 | 20,049 | 14,794 | 25,452 | 94,646 | 15,938 | 16,574 | 17,237 | 15,683 | 14,406 | 25,116 | 104,954 |
| Total | 97,867 | 97,842 | 97,585 | 71,550 | 157,842 | 522,686 | 118,879 | 93,735 | 91,035 | 85,830 | 67,808 | 152,468 | 609,755 |
ICU, intensive care unit.
aExcluding coronavírus disease 2019.
Figure 1.
Timeline of leading causes of admission for deaths in public hospitals in Brazil from January 2020 to December 2020. COVID-19, coronavirus disease 2019.
Compared with 2019, the greatest increase in deaths was observed in patients aged 40–60 years and 60–79 years, representing 20.3% (123,565) and 44.8% (272,238) of all deaths in 2020, respectively. The number of hospital deaths related to COVID-19 among children and teenagers (0–19 years old) represented the smallest group compared with all other causes of death in 2020. Regarding ethnicity, the main increases in deaths were observed among blacks (33.9%), yellows (32.6%) and native Brazilians (30.9%). The black/brown group represented 39.8% (47,306) of the COVID-19 hospital deaths. The number of deaths in all length-of-stay groups increased in 2020, but a more pronounced increase was observed for admissions lasting 7–14 days (23.2%) and intensive care unit admissions (38,0%). However, it is noteworthy that half of the deaths due to COVID-19 occurred in hospitalizations with length of stay ≤7 days. Although the Southeast region had the highest proportion (44.3%) of hospital deaths due to COVID-19, the Northern region showed the greatest increase (31.58%) in the total number of hospital deaths.
Discussion
COVID-19 was the main cause of hospital death in public hospitals in Brazil in 2020, surpassing diseases of the circulatory system, diseases of the respiratory system, other infectious diseases and cancer. Although accounting for hospital death data alone, this finding is in line with wider studies in other contexts, such as the study conducted by Ahmad and Anderson (2021) with provisional death records from the USA. However, instead of being the main cause of death, COVID-19 was the third leading cause of death in 2020 in the USA. This is a very worrying scenario, and the emergence of new variants may make the scenario even more worrying in 2021 (Abdool Karim and de Oliveira, 2021). As well as COVID-19, the number of hospital deaths due to diseases of the respiratory system was also important in 2020, suggesting the consequences of weak preparedness, such as low numbers of beds at public hospitals. Indeed, as a result of failing to mitigate the spread (Castro et al., 2021b), estimates also show the high impact of COVID-19 in terms of reducing overall life expectancy by 1.3 years in Brazil, highlighting the impact of local inequities (Castro et al., 2021a). In addition, the present results show disparities between ethnicities, which were observed and related to socio-economic status in previous analyses (Baqui et al., 2020; Castro et al., 2021b).
COVID-19 is likely to remain as one of the leading causes of death in 2021. In fact, civil registration data (ARPEN, 2021) already report COVID-19 as the main cause of death in Brazil in March 2021. None of the 2019 death records were classified as deaths due to COVID-19, suggesting a lack of misclassification. However, the study data are restricted to deaths that occurred in hospitals reimbursed by the SUS, and deaths that occurred in private hospitals, at home or in other settings were not included. These estimates can shed some light on the leading causes of hospital death in Brazil, and indicate the need for better strategies to prevent the direct and indirect effects of COVID-19 on the Brazilian population.
Conflict of interest statement
None declared.
Funding
This study was funded by the Call for Proposals MCTIC/CNPq/FNDCT/MS/SCTIE/Decit No. 07/2020 – research to address the COVID-19 pandemic, its consequences, and other severe acute respiratory syndromes, under the coordination of LMPS. GSF and LCA received a research grant from CNPq during the study. The study sponsor had no role in the study design, data collection, data analysis, data interpretation or report writing. The authors had full access to all study data and were responsible for the decision to submit this work for publication.
Ethical approval
All analyses were based on public data sets available to the public at large and not restricted to researchers. The records were all de-identified before being made public, and are available in SIH/SUS repository at ftp://ftp.datasus.gov.br/dissemin/publicos/SIHSUS/200801_/Dados.
Author contributions
Conceptualization: IRZ, MNS, ENS and LMPS.
Data curation: IRZ and LCA.
Formal analysis: IRZ and LCA.
Validation: FVC, GSF, IRZ, JJCE, MNS, ENS and LMPS.
Writing: FVC, GSF, IRZ, JJCE, MNS, ENS and LMPS.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Abdool Karim SS, de Oliveira T. New SARS-CoV-2 variants – clinical, public health, and vaccine implications. N Engl J Med. 2021;384:1866–1868. doi: 10.1056/NEJMc2100362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad FB, Anderson RN. The leading causes of death in the US for 2020. JAMA. 2021;325:1829–1830. doi: 10.1001/jama.2021.5469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ARPEN. Portal de Transparência do Registro Civil 2021. Available at: https://transparencia.registrocivil.org.br (accessed 8 October 2021).
- Baqui P, Bica I, Marra V, Ercole A, van der Schaar M. Ethnic and regional variations in hospital mortality from COVID-19 in Brazil: a cross-sectional observational study. Lancet Glob Heal. 2020;8:e1018–e1026. doi: 10.1016/S2214-109X(20)30285-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brasil Ministério. Medicamentos e OPM do SUS; 2021. da Saúde, Departamento de Informática do SUS. SIGTAP – Sistema de Gerenciamento da Tabela de Procedimentos. Available at http://sigtap.datasus.gov.br/tabela-unificada/app/sec/inicio.jsp. [Google Scholar]
- Castro MC, Gurzenda S, Turra CM, Kim S, Andrasfay T, Goldman N. Reduction in life expectancy in Brazil after COVID-19. Nat Med. 2021;27:1629–1635. doi: 10.1038/s41591-021-01437-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro MC, Kim S, Barberia L, Ribeiro AF, Gurzenda S, Ribeiro KB, et al. Spatiotemporal pattern of COVID-19 spread in Brazil. Science. 2021;372:821–826. doi: 10.1126/science.abh1558. [DOI] [PubMed] [Google Scholar]
- Dall'Alba R, Rocha DG. Brazil's response to COVID-19: commercial determinants of health and regional inequities matter. Lancet Glob Heal. 2021;9:E726–E727. doi: 10.1016/S2214-109X(21)00146-7. [DOI] [PubMed] [Google Scholar]
- Rocha R, Atun R, Massuda A, Rache B, Spinola P, Nunes L, et al. Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: a comprehensive analysis. Lancet Glob Heal. 2021;9:E782–E792. doi: 10.1016/S2214-109X(21)00081-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanno LK, Casale T, Demoly P. Coronavirus Disease (COVID)-19: World Health Organization definitions and coding to support the allergy community and health professionals. J Allergy Clin Immunol Pract. 2020;8:2144–2148. doi: 10.1016/j.jaip.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]