Abstract
Background
The effect of coronavirus disease 2019 (COVID-19) on a developing nation is sparsely reported and, more importantly, the discrepancies in public and private sectors are underexplored.
Methods
We retrospectively investigated the data on the effect of COVID-19 on renal transplantation between 2019 and 2020 in a nationwide analysis from 8 public and 10 private sector hospitals of India.
Results
On comparing the yearly data, the number of living-related transplants and deceased donor transplants declined by 48% (2610 vs 1370) and 49% (194 vs 99), respectively. The outpatient numbers and in-center admissions decreased by 40.4% (616,741 vs 367,962) and 30.8 % (73,190 vs 49,918). respectively. There was no increase in the number of renal or graft biopsies in the COVID-19 era. The number of waitlisted patients on hemodialysis was higher in public (304,898 vs 338,343) when compared with private (163,096 vs 150,292) in the last 2 years. Similarly, the number of waitlisted patients on peritoneal dialysis (4655 vs 3526) was higher in the public sector compared with private sector (932 vs 745). The decline in living transplants during the pandemic was higher in public sectors (58%) compared with the private (49%). However, the decline in deceased donation was higher in private (57.9%) relative to public (50.6%).
Conclusions
COVID-19 has adversely affected the transplantation activities across the Indian transplantation centers, with a disproportionately higher impact on waitlisted patients in public sector programs. A sound prioritization of health care resources is mandated to safeguard the most deprived and high-risk waitlisted patients during the pandemic.
Coronavirus disease 2019 (COVID-19) has reshaped transplantation activities across all parts of the world [1,2].Various high-level data depict the multidomain effect of COVID-19 on transplantation practices [3,4]. During the pandemic, an optimal assessment of the risk-benefit ratio for performing surgeries with an overburdened health care system is the most demanding step [5]. The next challenging step is to resume emergency transplantation in crisis, at least for the most vulnerable waitlisted patients. Numerous such reports have been published in developed nations, but there is a definite lack of such data from the developing world, where pandemic consequences were worse owing to underdeveloped health care resources. This study aimed to analyze the crude impact of COVID-19 in transplantation services in India, where living donation predominates, unlike in the Western world. This report will provide a general illustration of the landscape of living renal transplantation in developing nations amid the COVID-19 pandemic. Hence, this report will help prioritize care for those sections of the transplantation system most prone to being negatively impacted.
Materials and Methods
India has a predominant living-related transplant program; deceased donation is in its infancy, and the bulk of transplantation occurs in the private sector [6]. To measure the effect of the ongoing COVID-19 pandemic on transplantation and nephrology services in India, a nationwide call to 36 transplant centers was made. The data of 18 willing centers were received and explored in this retrospective observational study, which included 8 public sector institutions (Institute of Kidney Disease and Research Center, Ahmedabad; Jeevandan, Government of Telangana; Department of Renal Transplant Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh; Osmania General Hospital, India, Hyderabad; Nizam's Institute of Medical Sciences Panjagutta, Hyderabad; Indira Gandhi Institute of Medical Sciences, Patna; Institute of Postgraduate Medical Education and Research, Kolkata; Sawai Man Singh Hospital, Jaipur) and 10 private hospitals (Muljibhai Patel Urological Hospital, Nadiad, Gujarat; Christian Medical College, Vellore, Tamil Nadu; Narayana Health (Rabindranath Tagore International Institute of Cardiac Sciences), Kolkata; Indraprastha Apollo Hospital, New Delhi; Manipal Hospital, Bangalore; Kovai Medical Center and Hospital, Coimbatore, Tamil Nadu; Jaslok Hospitals, Mumbai; Venkateshwar Hospital, New Delhi; Center Yashoda Hospitals, Secunderabad; Lakeshore Hospital, Kochi, Kerala). We collected the monthly data of outpatient department patients, in-center patients, and renal transplants in 2019 and 2020. We also collected the number of COVID-19 transplant and dialysis patients in respective centers. For measuring the effect on nephrology services, data about procedures such as the number of double lumen catheter insertions, arteriovenous fistula, and renal biopsies were collected and analyzed. The sample size was not predefined, and data from all willing centers were added. A larger number of private sector hospitals contributed to the study, which is a potential source of bias. The data were collected electronically from all the centers by 2 of the authors (V.B.K and H.S.M) for final interpretation. The data were expressed as numbers and percentages, and no statistical analysis was required in the study.
Ethical Statement
The study was approved by the institutional ethical committee (Registration number: ECRJI43/InstlGJI2013/RR-19). The study followed the Strengthening The Reporting of OBservational Studies in Epidemiology guidelines. We abided by the norms and regulations of the declaration of Helsinki, the declaration of Istanbul, and the Tissue and Organ Transplantation Act.
Results
Data from 18 centers (8 public and 10 private sector hospitals) were received and analyzed in the study. Because of the nationwide lockdown from April to June, there was an extremely steep decline in transplant and renal care activities (Fig. 1 -4 ). Many of the participating transplant centers (n = 6) were converted to designated COVID-19 centers during the lockdown period. Compared with the previous year, during the lockdown period the number of living transplants (103 vs 643) and deceased transplants (6 vs 34) decreased by 84% and 83%, respectively. The in-center admissions during lockdown declined by 61% (18,339 vs 7251) along with the out-patient department numbers 63% (15,6458 vs 59,088). However, there was a mere 6% difference (145,926 vs 138,554) in the number of patients undergoing hemodialysis even in the lockdown. When comparing the yearly data, the number of living-related transplants declined by 48% (2610 vs 1370) in the calendar year 2019 vs 2020. The decline in deceased donor transplants was 49% (194 vs 99), which was similar to the live donations. The outpatient department showed a decreased number of registrations by 40.4% (61,6741 vs 36,7962), whereas the in-center admissions declined further by 31.8% (73,190 vs 49,918). There was an insignificant decline in the number of dialysis patients by only 1% (589,261 vs 590,692) in the calendar year 2019 vs 2020. Data accumulated from 5 centers showed a decrease in the numbers of renal biopsies performed by 43% (3861 vs 2225) in the 2 years. There was no increase in the number of renal or graft biopsies in the COVID-19 era. As the threshold for elective surgery was universally kept higher in the COVID-19 era, the number of arteriovenous fistulae (3055 vs 2063) declined by 32.5% between the 2 years. A secondary analysis of the difference in public and private sectors was also done. Most of the living-related transplantations were performed in the private sector (1736 vs 885) compared with the public (735 vs 309) sector in the 2 years, whereas the opposite was true for deceased donation, where the public sector (308 vs 152) led over the private sector (76 vs 32). The number of waitlisted patients on hemodialysis was higher in the public sector (304,898 vs 338,343) when compared with the private sector (163,096 vs 150,292) in the last 2 years. Similarly, the number of waitlisted patients on peritoneal dialysis (4655 vs 3526) was higher in public sector compared with the private sector (932 vs 745). During the 2 years, the number of waitlisted patients on dialysis increased in public sectors (1.1%), whereas it declined for the private (0.92%), although the difference was very small. The decline in living transplants during the pandemic was higher in public sectors (58%) compared with the private sectors (49%). However, the decline in deceased donation was higher in private (57.9%) relative to the public (50.6%) sector. Table 1 compares the impact of COVID-19 between public and private transplant centers.
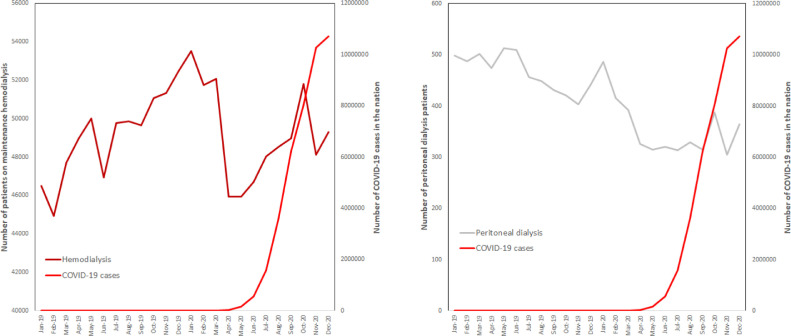
Fig 2.
Comparison of the number of patients receiving hemodialysis (right) and peritoneal dialysis (left) in the years 2019 vs 2020. COVID-19, coronavirus disease 2019.
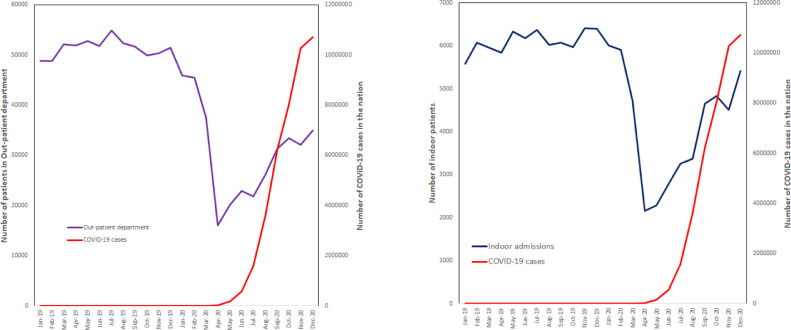
Fig 3.
Comparison of out-patient department admissions (right) and indoor admissions (left) in the years 2019 vs 2020. COVID-19, coronavirus disease 2019.
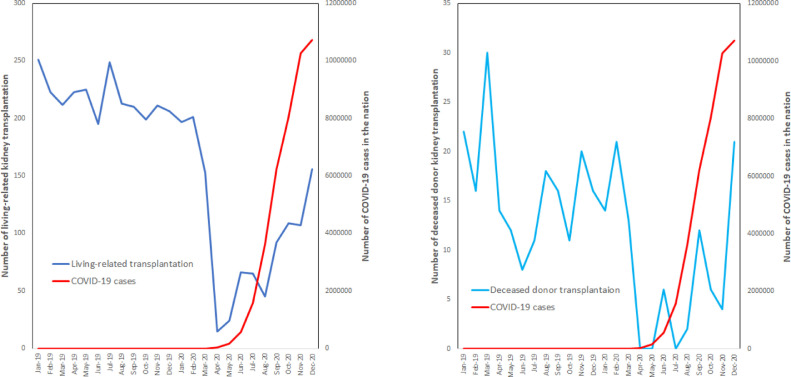
Fig 1.
Comparison of living-related transplantation (right) and deceased donor transplantation (left) in the years 2019 vs 2020. COVID-19, coronavirus disease 2019.
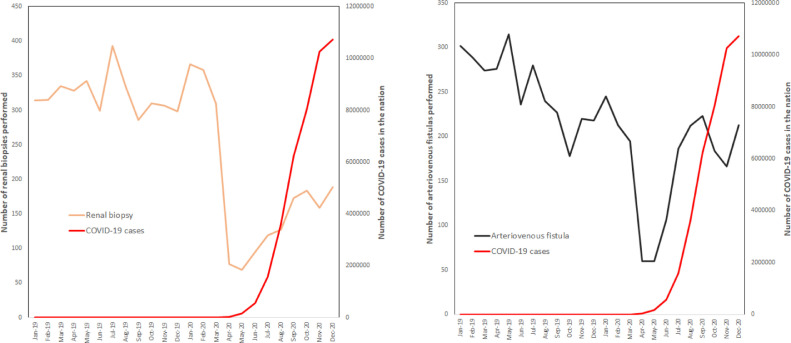
Fig 4.
Comparison of renal biopsies (right) and arteriovenous fistulas performed (left) in the years 2019 vs 2020. COVID-19, coronavirus disease 2019.
Table 1.
Comparison of the Effect of COVID-19 on Transplantation and Waitlist Patients in Public and Private Sectors
| Months | Jan2019 | Feb2019 | Mar2019 | Apr2019 | May 2019 | Jun 2019 | Jul2019 | Aug 2019 | Sep 2019 | Oct 2019 | Nov 2019 | Dec 2019 | Jan 2020 | Feb 2020 | Mar2020 | Apr2020 | May 2020 | Jun 2020 | Jul 2020 | Aug 2020 | Sep2020 | Oct2020 | Nov 2020 | Dec 2020 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LRKT | ||||||||||||||||||||||||
| Public sectors | 67 | 65 | 66 | 62 | 68 | 48 | 66 | 52 | 59 | 66 | 60 | 56 | 61 | 65 | 36 | 2 | 2 | 9 | 20 | 11 | 18 | 30 | 21 | 34 |
| Private sectors | 170 | 144 | 129 | 153 | 152 | 132 | 167 | 145 | 137 | 124 | 145 | 138 | 128 | 132 | 110 | 13 | 22 | 57 | 43 | 33 | 71 | 77 | 84 | 115 |
| DDKT | ||||||||||||||||||||||||
| Public sectors | 30 | 22 | 45 | 23 | 22 | 21 | 22 | 23 | 23 | 16 | 34 | 27 | 23 | 30 | 20 | 0 | 0 | 9 | 5 | 7 | 16 | 9 | 7 | 26 |
| Private sectors | 5 | 7 | 7 | 3 | 8 | 4 | 7 | 8 | 9 | 5 | 7 | 6 | 10 | 4 | 6 | 0 | 1 | 1 | 0 | 5 | 2 | 0 | 2 | 1 |
| HD | ||||||||||||||||||||||||
| Public sectors | 22541 | 21606 | 24139 | 24653 | 25829 | 24268 | 26582 | 26857 | 26100 | 27209 | 27135 | 27979 | 29357 | 28390 | 29425 | 27067 | 27038 | 26960 | 28831 | 28164 | 28205 | 29371 | 27798 | 27737 |
| Private sectors | 13839 | 13237 | 13455 | 14230 | 14069 | 12548 | 13066 | 12886 | 13462 | 13782 | 14119 | 14403 | 14860 | 14067 | 13769 | 11005 | 11125 | 11893 | 11331 | 12373 | 12782 | 13468 | 11350 | 12269 |
| PD | ||||||||||||||||||||||||
| Public sectors | 423 | 410 | 425 | 397 | 435 | 432 | 378 | 371 | 353 | 342 | 325 | 364 | 418 | 347 | 332 | 266 | 255 | 261 | 255 | 268 | 252 | 327 | 243 | 302 |
| Private sectors | 76 | 77 | 77 | 77 | 78 | 78 | 78 | 78 | 78 | 79 | 78 | 78 | 68 | 69 | 60 | 60 | 60 | 59 | 59 | 61 | 63 | 61 | 62 | 63 |
COVID-19, coronavirus disease 2019; DDKT, deceased donor kidney transplantation; HD, hemodialysis; LRKT, living-related kidney transplantation; PD, peritoneal dialysis. Data presented as number of patients.
Discussion
There have been reports from the transplantation societies of many developed nations [7], but the magnitude of COVID-19 on the Indian subcontinent is underexplored. Overall, the number of waitlisted patients in the pandemic year remained static when compared with the gross decline in transplantation activity. Additionally, the number of waitlisted patients increased in the public sector programs compared with the private sector. The long-term impact of the increased waiting time is also not known. The discrepancy found between public and private transplant centers has important implications and was previously understudied. Thus, our report shows that the lower socioeconomic transplant candidates suffered more from the pandemic. Furthermore, there was an absolute shut down of the activities in all centers at the peak of the pandemic. The contribution of deceased donation to Indian transplantation is already minuscule and was among the most affected from the pandemic. Kidney paired donation is predominately a single-center experience in Indian settings [8]. During the pandemic, kidney paired donation rates also saw a drastic decline. One of the most remarkable achievements of all the transplant centers was the successful transplantation of recovered patients, which has been published in our previous reports [5]. Another highlight analysis from our report is the decline in in-center patients, which is attributed to the effective implementation of telemedicine in all the centers for tackling this pandemic, which proved an excellent tool in a densely populated nation with high transmission of COVID-19. There was no increase in the number of graft biopsies performed in the pandemic, which also suggests that COVID-19 may not have the postulated direct effects on kidneys [9] on a large scale. There was also no substantial increase in the number of patients on peritoneal dialysis, which shows the barriers of implementation and acceptability of this mode of dialysis that is regarded as having a theoretical advantage over hemodialysis in such a pandemic surge.
The limitation of the report is that the detailed analysis of the mortality and in-hospital admission characteristics is not studied. In summary, our report highlights the impact of COVID-19 in transplantation in a developing nation and calls for channelizing the resources to the most deprived and high-risk patients to lessen the lethality of future pandemics.
Conclusions
In this nationwide analysis, the public sector hospitals are more affected by the pandemic than private sector ones. Our report would help better allocate resources by focusing on the most vulnerable part of the transplantation practices, especially in living donation. This will help create better preparedness and minimize the damage in case of a next COVID-19 wave.
References
- 1.Alasfar S, Avery RK. The impact of COVID-19 on kidney transplantation. Nat Rev Nephrol. 2020;16:568–569. doi: 10.1038/s41581-020-00340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kute VB, Meshram HS, Navadiya VV, Chauhan S, Patel DD, Desai SN, et al. Consequences of the first and second COVID-19 wave on kidney transplant recipients at a large Indian transplant center [e-pub ahead of print]. Nephrology (Carlton) doi: 10.1111/nep.13961, accessed August 11, 2021. [DOI] [PMC free article] [PubMed]
- 3.Michel S, Witt C, Gottlieb J, Aigner C. Impact of COVID-19 on lung transplant activity in Germany: a cross-sectional survey. Thorac Cardiovasc Surg. 2021;69:92–94. doi: 10.1055/s-0040-1715436. [DOI] [PubMed] [Google Scholar]
- 4.Azzi Y, Bartash R, Scalea J, Loarte-Campos P, Akalin E. COVID-19 and solid organ transplantation: a review article. Transplantation. 2021;105:37–55. doi: 10.1097/TP.0000000000003523. [DOI] [PubMed] [Google Scholar]
- 5.Kute VB, Ray DS, Yadav DK, Pathak V, Bhalla AK, Godara S, et al. A multicenter cohort study from India of 75 kidney transplants in recipients recovered after COVID-19. Transplantation. 2021;105:1423–1432. doi: 10.1097/TP.0000000000003740. [DOI] [PubMed] [Google Scholar]
- 6.Kute V, Ramesh V, Shroff S, Guleria S, Prakash J. Deceased-donor organ transplantation in India: current status, challenges, and solutions. Exp Clin Transplant. 2020;18(Suppl 2):31–42. doi: 10.6002/ect.rlgnsymp2020.L6. [DOI] [PubMed] [Google Scholar]
- 7.Danziger-Isakov L, Blumberg EA, Manuel O, Sester M. Impact of COVID-19 in solid organ transplant recipients. Am J Transplant. 2021;21:925–937. doi: 10.1111/ajt.16449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kute VB, Patel HV, Modi PR, Rizvi SJ, Shah PR, Engineer DP, et al. Non-simultaneous kidney exchange cycles in resource-restricted countries without non-directed donation: a prospective single-center cohort study. Transpl Int. 2021;34:669–680. doi: 10.1111/tri.13833. [DOI] [PubMed] [Google Scholar]
- 9.Velez JCQ, Caza T, Larsen CP. COVAN is the new HIVAN: the re-emergence of collapsing glomerulopathy with COVID-19. Nat Rev Nephrol. 2020;16:565–567. doi: 10.1038/s41581-020-0332-3. [DOI] [PMC free article] [PubMed] [Google Scholar]