Abstract
Coronaviruses can cause multiple systemic infections respiratory complications are the most recognizable symptoms similar to severe acute respiratory syndrome coronavirus (SARS-CoV). Aspiration pneumonia was the most common reason for the Emergency admission of patients with PD.Here we report the case a patient with Parkinson’s disease admitted for respiratory insufficiency secondary to Covid-19 and aspiration pneumonia.
A 78-years- old male patient, treated for Parkinson’s disease, was admitted to the emergency department with symptoms of acute respiratory insufficiency. Four days before his admission, the patient suffered from solid dysphagia. On physical examination, the patient was obnibulated, febrile at 39 °, with clinical signs of respiratory insuffisiency. Computed tomography of the neck and Chest showed patchy areas of subpleural ground glass opacities with vascular dilatation associated with bilateral posterobasal and anterior consolidations with air overlapping imaging characteristics of aspiration and covid 19 pneumonia. The CT scan also showed an oesophageal hypodensity consistant with endoluminal foreign body.
Reverse transcription-polymerase chain reaction (RT-PCR) for COVID-19 was positive.The diagnosis of Sars-cov 19 associated with aspiration pneumonia were retained. An esophagoscopy was realized, a foreign body visualized in the upper sphincter of the esophagus and an impacted food bolus was retracted.
We would like to emphasize the challenging differential diagnosis of pneumonia caused by aspiration of different materials and Sars-cov 19. Definite discrimination of the two diagnoses might be impossible. Some radiologic features may suggest one diagnos over the other. While lobar or segmental pneumonia, lung abscess, and empyema have been reported as Complications of aspirations pneumonia these outcomes are rarely Considered Complications of COVID-19 pneumonia. Centrilobular nodules and tree-in-bud sign are commonly seen in cases with aspiration. Interestingly, these CT findings are not frequent in COVID-19 pneumonia and have been categorized as “Atypical” by the Radiological Society of North America (RSNA), and therefore could be of some Value in proposing a differential diagnosis. Bilateral subpleural patches of ground-glass opacity (GGO), especially in basal distribution, have been described as typical for the diagnosis of COVID-19 pneumonia in suspected Cases. Such a presentation is also fairly common in aspiration Pneumonia.
Keywords: Sars-Cov-19, Coronavirus, Aspiration pneumonia, Dyspnea, Foreign body ingestion, Parkinson's disease
1. Introduction
On 31 December 2019, a novel coronavirus (COVID-19) was detected in Wuhan City, Hubei Province of China. The symptoms of COVID-19 are dependent on age and the patient’s underlying medical illness and also the condition of the immune system [1]. Coronaviruses can cause multiple systemic infections that respiratory complications are the most recognizable symptoms similar to severe acute respiratory syndrome coronavirus (SARS-CoV). The most prevailing symptoms at the onset of disease, after an incubation period of approximately 5−2 days, are Fever, cough, dyspnea, myalgia, headache, and diarrhea.
Parkinson’s disease is a progressive nervous system disorder that affects movement. Symptoms start gradually. Tremors are common, but the disorder also commonly causes stiffness or slowing of movement, loss of automatic movements, impaired posture, and balance. The cause of Parkinson's disease is unknown, but several factors appear to play a role, including genetic and environmental causes. The treatment options vary and include medications and surgery. While Parkinson’s itself is not fatal, disease complications can be serious [2]. Gastrointestinal abnormalities in Parkinson’s disease(PD) have been known since 1817. Aspiration pneumonia was the most common reason for the Emergency admission of patients with PD.
Here we report the case of a patient with Parkinson’s disease admitted for respiratory insufficiency secondary to Covid-19 and aspiration pneumonia, and discuss the diagnosis challenges and the radiological features of each etiology of pneumonia.
2. Case report
A 78-years- old male patient, was admitted to the emergency department with symptoms of acute respiratory insufficiency. Four days before his admission, the patient suffered from solid dysphagia with no other symptom associated, the evolution was towards worsening of the symptomatology, and the development of dyspnea. In the past medical history, the patient is treated for Parkinson’s disease for ten years, with two episodes of aspiration pneumonia in the last two years, the patient is on medical treatment : Levodopa. The patient is also a well-known type 2 diabetes mellitus treated with insulin.
On physical examination, the patient was obnibulated, febrile at 39 °, with blood pressure :100−85 mm/hg, heart rate :120 beats/minute, respiratory rate 37/minute, and oxygen saturation of 75 % on room air. Given the instability of the patient, no further clinical examination was done.
The laboratory examination results were as follows: serum glucose 160 mg/dL; blood urea nitrogen : 19 mg/dL ;creatinine 0.13 mg/dL ; alanine aminotransferase 35 IU/L ; aspartate aminotransferase 47 IU/L ; sodium 140 mmol/L ; potassium 3.8 mmol/L, hemoglobin 11.6 g/ dL and white blood cell count 14,700 cells per microliter (neutrophils = 82.7 % ; lymphocytes = 10.4%) ; C-reactive protein :64 mg/l, negative glucose and ketone in complete urinalysis.
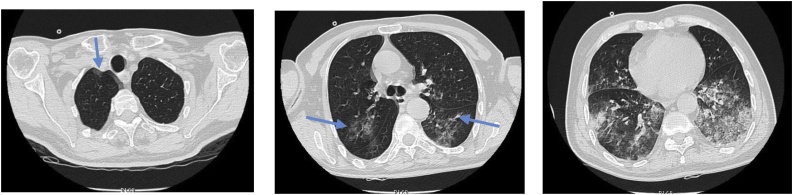
Computed tomography of the neck and Chest showed patchy areas of subpleural ground glass opacities with vascular dilatation associated with bilateral posterobasal and anterior consolidations with air bronchogram (Fig. 1), Featuring overlapping imaging characteristics of aspiration and covid 19 pneumonia. The CT scan also showed an oesophageal hypodensity consistant with endoluminal foreign body (Fig. 2).
Fig. 1.
Computed tomography of the neck and Chest, axial slices: patchy areas of subpleural ground glass opacities with vascular dilatation associated with bilateral anterior and posterobasal, consolidations with air bronchogram, Featuring overlapping imaging characteristics of aspiration and covid 19 pneumonia.
Fig. 2.
Computed tomography of the neck and Chest: oesophageal endoluminal foreign body.
Reverse transcription-polymerase chain reaction (RT-PCR) for COVID-19 was positive.The diagnosis of Sars-cov 19 associated with aspiration pneumonia were retained. The treatment regimen was ventilatory support, high-flow oxygen, the patient was treated with hydroxychloroquine, Lopinavir/Ritonavir (LPV/RTV), and Azythromycin.Under general anesthesia and following the Safety Recommendations for Evaluation and Surgery of the Head and Neck During the COVID-19 pandemic [6], an esophagoscopy was realized, a foreign body visualized in the upper sphincter of the esophagus and an impacted food bolus was retracted (Fig. 3).
Fig. 3.
Picture of the foreign body retracted from the oesophagus: impacted food bolus.
3. Discussion
Aspiration pneumonia is the most common reason for the Emergency admission of patients with PD whose disease the ratio was >5 years [10]. Most of them showed cognitive impairment and a history of psychiatric symptoms. Our protocol at patient admission recommended screening for SARS-Cov2 in patients presenting respiratory symptoms and Epidemiologic risk of contact with the infected or contagious individual, Besides, correct triage of these patients is obligatory to reduce the risk of spread of infection and to protect the medical personnel from inadvertent exposure to The virus. On the other hand, early administration of Antibiotics in the presumed cases of aspiration pneumonia is Urgent to prevent morbidity and mortality [8,3]. In immunocompromised populations, COVID-19 infection should be considered in the presence of an atypical presentation and screening, protocols may be needed to be re-evaluated. Therefore, and since the increase in the number of cases and evidence of asymptomatic transmission among the community, contact with infected individuals was no longer mandatory. The fact that our patient did not have any epidemiologic risk factor for COVID-19 infection, made the diagnosis more likely to be aspiration pneumoniaI [2]. Our patient had Typical symptoms of gastrointestinal complications of Parkinson’s disease that had been begun four days before the appearance of respiratory symptoms even though the patient was under medical treatment. Dopaminergic medication does not necessarily improve swallowing function [5]. PD patients often show an improved swallowing function and reduction in other symptoms after the adjustment of medications. Some Studies have suggested that dysphagia in PD is statistically resistant to dopaminergic stimulation. Another study Suggested that the risk of aspiration may remain unchanged with levodopa. Further studies are nnecessary to confirm the difference in the risk of aspiration between on and off states of levodopa [7,9,10].
We would like to emphasize the challenging differential diagnosis of pneumonia caused by aspiration of different materials and Sars-cov 19. The Interpretation of chest findings may not be necessarily easy for the Emergency radiologists in the setting of e exact diagnosid. Although the go standard for the diagnosis of COVID Infection is PCR testing, radiologic outcomes together with the clinical data have also been implied at least for initial decision-making. In some cases, definite discrimination of the two diagnoses might be impossible. Some radiologic features may suggest One diagnos over the other. While lobar or segmental pneumonia, lung abscess, and empyema have been reported as Complications of aspirations pneumonia these outcomes are rarely Considered Complications of COVID-19 pneumonia. Centrilobular nodules and tree-in-bud sign are commonly seen in cases [1].
With aspiration. Interestingly, these CT findings are not frequent in COVID-19 pneumonia and have been categorized as “Atypical” by the Radiological Society of North America (RSNA), and therefore could be of some Value in proposing a differential diagnosis. Bilateral subpleural patches of ground-glass opacity (GGO), especially in basal distribution, have been described as typical for the diagnosis of COVID-19 pneumonia in suspected Cases [4,8]. Such a presentation is also fairly common in aspiration Pneumonia. Although posterodorsal lung Involvement is the most common distribution pattern in both Conditions, anterior lung involvement has rarely been reported in aspiration pneumonia, thus detection of radioLogic findings in anterior parts is more suggestive of COVID Pneumonia rather than aspiration pneumonia.
4. Conclusion
In summary, this study demonstrates, despite possible radiologic and clinical similarities between aspiration and COVID pneumonia, one Could suggest a correct diagnosis by careful examination of The CT images together with attention to the clinical scenario and judicious utilization of laboratory tests. Timely Diagnosis and treatment positively influence prognosis and Reduce mortality.
Ethical statement for solid state ionics
1) This material is the authors' own original work, which has not been previously published elsewhere.
2) The paper is not currently being considered for publication elsewhere.
3) The paper reflects the authors' own research and analysis in a truthful and complete manner.
4) The paper properly credits the meaningful contributions of co-authors and co-researchers.
5) The results are appropriately placed in the context of prior and existing research.
6) All sources used are properly disclosed (correct citation). Literally copying of text must be indicated as such by using quotation marks and giving proper reference.
7) All authors have been personally and actively involved in substantial work leading to the paper, and will take public responsibility for its content.
Funding statement
No funding to declare.
Declaration of Competing Interest
The authors report no declarations of interest.
References
- 1.Monte Francisca Sueli, da Silva-Junior Francisco Pereira. Mov. Disord. 2005;20(4):457–462. doi: 10.1002/mds.20342. [DOI] [PubMed] [Google Scholar]
- 2.Guillain Barre syndrome associated with COVID-19 infection: A case Report Zahra Sedaghat a, Narges Karimi Case Reports / Journal of Clinical Neuroscience. [DOI] [PMC free article] [PubMed]
- 3.Chaumartin N., Monville M., Lachaux B. Dysphagia or dysphagias during neuroleptic medication? LEncphale. 2011 doi: 10.1016/j.encep.2011.07.002. Paris. [DOI] [PubMed] [Google Scholar]
- 4.Forster A., Samaras N., Notaridis G., Morel P., Hua-Stolz J., Samaras D. Assessment and screening of deglutition disorders in geriatric patients. NPG Neurol. - Psychiatr. – Geriatr. 2013 [Google Scholar]
- 5.Sutton James P. Point of view Dysphagia in Parkinson’s disease is responsive to levodopa. Parkinsonism Relat. Disord. 2013;19:282e284. doi: 10.1016/j.parkreldis.2012.11.007. Pacific Neuroscience Medical Group, Oxnard, CA 93030, United States. [DOI] [PubMed] [Google Scholar]
- 6.Givi Babak. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngol. Neck Surg. 2020;(March (31)) doi: 10.1001/jamaoto.2020.0780. [DOI] [PubMed] [Google Scholar]
- 7.Dysphagia in Parkinson’s disease is responsive to levodopa, James P. Sutton, Pacific Neuroscience Medical Group. [DOI] [PubMed]
- 8.Aspiration Pneumonia or COVID-19 Infection: A Diagnostic Challenge, Fariba Zarei, MD, Letter to the Editor. [DOI] [PMC free article] [PubMed]
- 9.Oropharyngeal Dysphagia and Aspiration Pneumonia Following Coronavirus Disease 2019: A Case Report, Yoichiro Aoyagi1. [DOI] [PMC free article] [PubMed]
- 10.Springer Science+Business Media; New York: 2015. Dysphagia in Parkinson’s DiseaseInga Suttrup. [Google Scholar]