Abstract
Sialendoscopy is a minimally invasive technique that facilitates the diagnosis and treatment of sialolithiasis. This case series presents the novel use of sialendoscopy to treat sialodocholithiasis in six patients with a non-functional or surgically absent submandibular gland by a single surgeon at the University of Pennsylvania Health System between March 2013 and December 2019. The four female and two male patients had a median age of 56 years and mean follow-up of 16.2 months (range 1–44.5). All stones were successfully removed using sialendoscopy, and in 5 patients a combined approach was utilized. All patients remain asymptomatic at last clinical follow-up. We conclude that sialendoscopy is a viable, minimally invasive method for managing sialodocholithiasis in patients with prior submandibular gland excision or atretic gland. It is also useful as an assistive tool when approaching complex transcervical or transoral procedures in previously instrumented patients.
Keywords: Sialendoscopy, Sialodocholithiasis, Sialolithiasis, Salivary gland disease, Recurrent or retained sialolith
Introduction
With the advent of sialendoscopy, over 95% of sialoliths can be managed with gland preservation; however, gland excision sometimes remains necessary.1 Recurrent or persistent sialolithiasis following gland excision is a rare but recognized phenomenon and is thought to be related to functional activity in the residual submandibular gland (SMG) deep lobe.2 Herein we present six cases of sialodocholithiasis following prior SMG excision. A 1.3 mm Marchal sialendoscope (Karl Storz, Tuttlingen, Germany) was utilized in all cases. The University of Pennsylvania Institutional Review Board approved this research.
Case reports
Case 1
A 62-year-old male with distant history of poorly differentiated nasopharyngeal carcinoma treated with surgical resection and adjuvant radiation presented with floor of mouth (FOM) calcification on dental X-ray concerning for sialodocholithiasis. CT scan showed 6 mm sialodocholith in the mid-Wharton’s duct and an atretic SMG. Intraoperatively, the stone was removed with a 6-wire basket (Cook Medical, Bloomington, IN, USA), the duct was irrigated with steroids, and a sialodochoplasty was performed. The patient remained asymptomatic at six-month follow-up apart from dysphagia and xerostomia attributed to prior radiation.
Case 2
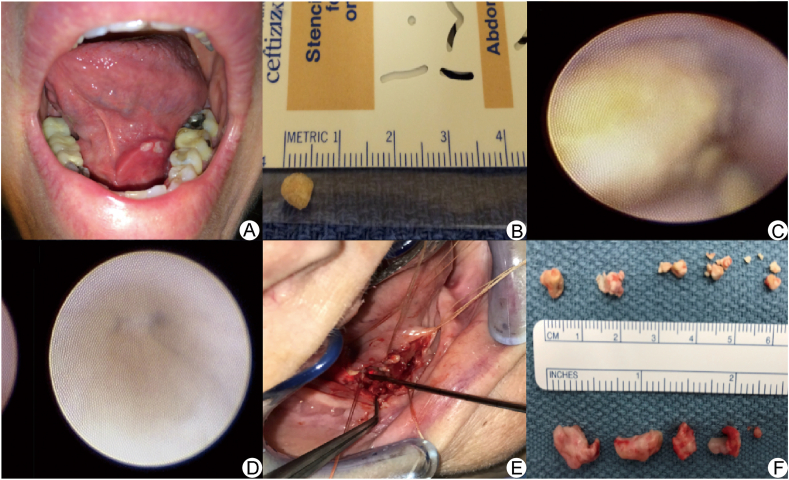
A 59-year-old female with history of SMG sialolithiasis one-year status-post gland excision and sialodochoplasty presented with recurrent FOM pain and swelling (Fig. 1A). CT scan showed 7 mm sialodocholith in the remnant mid-Wharton’s duct. Prior pathology showed ductal carcinoma in situ and with concern that chronic sialadenitis may promote ductal malignancy, sialendoscopy and excision of the residual SMG was performed (Fig. 1B).3 Pathology was negative for carcinoma and the patient remained asymptomatic at 3.7 year follow-up.
Figure 1.
A: Case 2, floor of mouth edema and area of stone extrusion from Wharton’s duct; B: Case 2, 6 mm sialolith; C: Case 4, sialendoscopy showing sialolith in situ with microbur; D: Case 4, clear ducts to the bifurcation post-extraction; E: Case 6, sialendoscopic transillumination assisting in stone removal after excision of extremely inflamed sublingual gland; F: Case 6, multiple calculi with largest diameter 9 mm.
Case 3
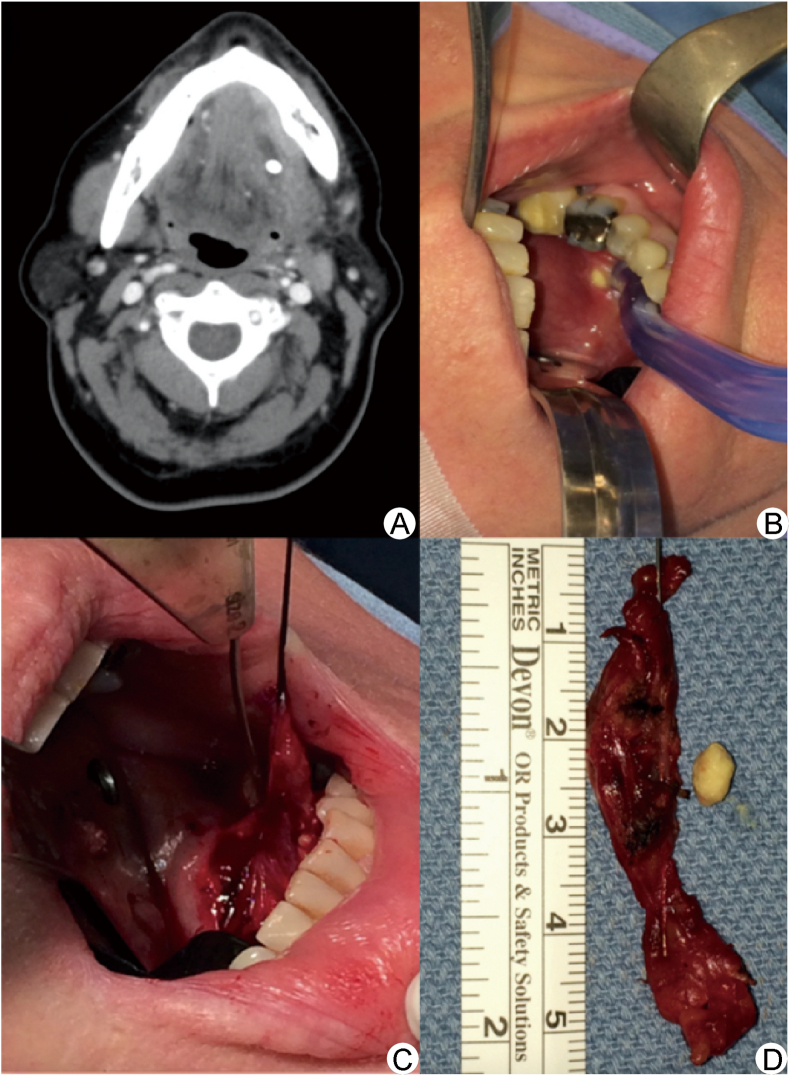
A 53-year-old female with history of SMG sialolithiasis five months status-post gland excision presented with oral swelling, drainage, and a visible FOM defect. CT scan showed 6.5 mm sialodocholith in the remnant mid-Wharton’s duct. Intraoperatively, the stone was found to have eroded the duct wall and was removed. Just posterior to the papillae, a second defect from stone extrusion was noted, obligating cannulation of the duct from this site. Excision of the residual SMG was performed due to extensive granulation tissue (Fig. 2). The patient remained asymptomatic at three-month follow-up.
Figure 2.
Case 3 (A): CT scan showing 5.5–6 mm sialodocholith in the remnant mid-Wharton’s duct with dilation of the left submandibular duct and adjacent soft tissue stranding; (B) and (C) intraoperative images of complete gland removal; (D) 8 mm sialolith and complete submandibular gland.
Case 4
A 50-year-old female with history of chronic sialadenitis and SMG sialolithiasis three years status-post gland excision presented with cervical lymphadenopathy and FOM pain. A CT scan showed two sialodocholiths (largest diameter 6.4 mm) in the remnant Wharton’s duct. Intraoperatively, the sialolith was mobilized using a microbur (Karl Storz, Tuttlingen, Germany) but subsequent basket extraction (Cook Medical, Bloomington, IN, USA) was unsuccessful (Fig. 1C). A combined FOM cut-down and endoscopic approach enabled stone removal (Fig. 1D). The patient remained asymptomatic at 3.7 year follow-up.
The following is the supplementary data related to this article:
Case 5
A 53-year-old male with history of chronic sialadenitis and SMG sialolithiasis ten months status-post gland excision presented with neck pain and swelling. A CT scan showed 11 mm sialodocholith in the remnant Wharton’s duct. Intraoperatively, an NCircle basket (Cook Medical, Bloomington, IN, USA) was used to stabilize the stone and a papillotomy was performed with basket extraction and sialodochoplasty. The patient remained asymptomatic at one-month follow-up.
Case 6
A 73-year-old female with history of SMG sialolithiasis seven years status-post gland excision presented with facial swelling and FOM pain. A CT scan showed proximal Wharton’s duct dilatation and multiple calculi in the remnant duct (largest diameter 6 mm). Intraoperatively, inability to dilate the papilla necessitated FOM cut-down. A distal stone was removed and an inflamed sublingual gland was excised (Fig. 1E). Sialendoscopy identified the blind end of the duct and allowed removal of remaining stones (Fig. 1F). The patient remained asymptomatic at one month follow up.
Discussion
This case report represents the largest series of patients with sialodocholithiasis following prior SMG excision (Table 1). Our experience shows that sialendoscopy, alone or as an adjunct to transoral approaches, is effective as definitive management for such cases. Although no specific quality of life measures were taken, all patients reported complete symptom resolution post-operatively. We were additionally successful in extracting moderately-sized (6–7 mm) sialodocholiths, larger than previously reported.4
Table 1.
Summary of presentation and management for patients with recurrent salivary gland disease following prior submandibular gland excision.
| Case | Age (years) | Sex | History | Presentation | Years post-excision | Stone location | Stone size (mm; CT, pathology) | Surgical approach | Deep lobe & duct remnant | Follow-up (months) | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 62 | M | Minor salivary gland carcinoma of NP, s/p resection and radiation with atretic R SMG | Minimal symptoms, thickened saliva | 15.67a | Mid-duct | 6, 6 | Sialendoscopy, steroid irrigation, basket extraction | Preserved | 6 | Asymptomatic |
| 2 | 59 | F | Sialolithiasis, s/p sialodochoplasty and L SMG excision, stone extruded pre-operatively | Recurrent FOM swelling and pain | 1.12 | Mid-duct | 7, 6 | Sialendoscopy | Excised | 44 | Asymptomatic |
| 3 | 53 | F | Sialolithotomy, s/p L SMG excision | Recurrent L FOM swelling and pain, odynophagia, visible FOM defect | 0.25 | Mid-duct | 6.5, 6 | Sialendoscopy with guide wire placement, complex repair | Excised | 3 | Asymptomatic |
| 4 | 50 | F | Sialadenitis and sialolithiasis, s/p R SMG excision | Pain, R FOM pinching sensation, right cervical lymphadenopathy | 2.25 | Proximal and distal duct | 6.4, 8b | Sialendoscopy with N-circle basket, papillotomy, sialodochoplasty | Preserved | 45 | Asymptomatic |
| 5 | 53 | M | Chronic sialadenitis, s/p L SMG excision | L neck swelling and pain | 0.75 | Distal, at papilla | 11, 13 | Sialendoscopy, microbur used to mobilize stone with combined open and endoscopic approach | Preserved | 1 | Asymptomatic |
| 6 | 73 | F | Chronic sialadenitis, s/p R SMG excision | R facial swelling, pain with chewing | 7 | Through-out duct | 6, 9b | Sialendoscopy, combined open and endoscopic approach, sublingual gland excision | Preserved | 1 | Asymptomatic |
FOM: floor of mouth; NP: nasopharynx; s/p: status post; SMG: submandibular gland.
Designates time after radiation treatment instead of gland excision in this patient.
Designates multiple stones; patient 4 had two stones, the other of which was 6 mm; patient 6 had multiple stones, five of which were >5 mm.
Transorally, an endoscopic approach offers improved visualization of the proximal duct and lingual nerve during dissection within a scarred surgical bed. Furthermore, retrograde sialendoscopy both during and following gland excision may help avoid retained sialoliths and prevent ongoing sialodocholithiasis.5 Intraoperative ultrasound guidance can serve as further confirmation of a lack of retained sialoliths. Stone removal with duct remnant preservation may be possible, but with chronically inflamed deep lobes (case 3) or the rare case of ductal premalignancy (case 2), excision of the residual SMG and duct remnant may be needed. We suggest that sialendoscopy be considered a viable first-line therapy for sialodocholithiasis following gland excision. It should also be considered at the time of SMG excision as a mechanism to reduce the likelihood of retained sialoliths. When a complex surgical approach is necessary, sialendoscopy can be an adjunct to open transcervical or transoral procedures.
Credit author statement
Jennifer Douglas: Data curation, Formal analysis, Writing (original draft, review, and editing); W. Walsh Thomas: Data curation, Formal analysis; Christopher Wen: Data curation, Writing (original draft, review, and editing), Laurie Loevner: Visualization; Writing (review and editing); Erica Thaler: Writing (review and editing); Ara Chalian: Writing (review and editing); Christopher H. Rassekh: Conceptualization, Supervision, Investigation, Writing (review and editing)
Funding sources
No funding was received for this research.
Author contributions
Jennifer Douglas: initial and revision authorship, conceptualization; W. Walsh Thomas: initial and revision authorship, conceptualization; Christopher Wen: revision authorship, video production; Laurie Loevner: neuroradiologist on cases, revision authorship; Erica Thaler: attending surgeon and referring provider of cases, revision authorship; Ara Chalian: attending surgeon and referring provider of cases, revision authorship; Christopher Rassekh: attending surgeon, managed the cases intra- and post-operatively, revision authorship, conceptualization.
Declaration of Competing Interest
The authors have no relevant conflicts of interest to disclose.
Acknowledgements
None.
Edited by Qiong Wu
Footnotes
Peer review under responsibility of Chinese Medical Association.
Contributor Information
Jennifer E. Douglas, Email: jennifer.douglas@pennmedicine.upenn.edu.
Christopher H. Rassekh, Email: Christopher.Rassekh@pennmedicine.uphs.upenn.edu.
References
- 1.Capaccio P., Torretta S., Ottavian F., Sambataro G., Pignataro L. Modern management of obstructive salivary diseases. Acta Otorhinolaryngol Ital. 2007;27:161–172. [PMC free article] [PubMed] [Google Scholar]
- 2.Markiewicz M.R., Margarone J.E., 3rd, Tapia J.L., Aguirre A. Sialolithiasis in a residual Wharton’s duct after excision of a submandibular salivary gland. J Laryngol Otol. 2007;121:182–185. doi: 10.1017/S0022215106003525. [DOI] [PubMed] [Google Scholar]
- 3.Gallego L., Junquera L., Calvo N., Fuente E., Rosado P. Bilateral carcinoma in situ of Wharton’s duct after chronic obstructive sialadenitis: inflammation as the cause of malignancy. Ann Otol Rhinol Laryngol. 2012;121:296–300. doi: 10.1177/000348941212100503. [DOI] [PubMed] [Google Scholar]
- 4.Luers J.C., Grosheva M., Stenner M., Beutner D. Sialoendoscopy: prognostic factors for endoscopic removal of salivary stones. Arch Otolaryngol Head Neck Surg. 2011;137:325–329. doi: 10.1001/archoto.2010.238. [DOI] [PubMed] [Google Scholar]
- 5.Potash A., Hoffman H.T. Retrograde sialendoscopy: a new technique for avoiding retained ductal stones. Ann Otol Rhinol Laryngol. 2012;121:38–43. doi: 10.1177/000348941212100107. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.