Abstract
The ergot alkaloid ergotamine is produced by Claviceps purpurea, a parasitic fungus that commonly infects crops and pastures of high agricultural and economic importance. In humans and livestock, symptoms of ergotism include necrosis and gangrene, high blood pressure, heart rate, thermoregulatory dysfunction and hallucinations. However, ergotamine is also used in pharmaceutical applications to treat migraines and stop post-partum hemorrhage. To define its effects, metabolomic profiling of the brain was undertaken to determine pathways perturbed by ergotamine treatment. Metabolomic profiling identified the brainstem and cerebral cortex as regions with greatest variation. In the brainstem, dysregulation of the neurotransmitter epinephrine, and the psychoactive compound 2-arachidonylglycerol was identified. In the cerebral cortex, energy related metabolites isobutyryl-L-carnitine and S-3-oxodecanoyl cysteamine were affected and concentrations of adenylosuccinate, a metabolite associated with mental retardation, were higher. This study demonstrates, for the first time, key metabolomic pathways involved in the behavioural and physiological dysfunction of ergot alkaloid intoxicated animals.
Subject terms: Biochemistry, Neuroscience
Introduction
Ergot alkaloids, the causative agents of ergotism, are commonly produced by fungi from the Clavicipitaceae family. In humans, symptoms of ergotism include gangrene, convulsions and hallucinations1. However, tightly controlled dosages of the ergot alkaloid, ergotamine is successfully applied in pharmaceutical applications2. Claviceps purpurea (Fries ex Fries) Tulasne, a commonly known parasitic fungus, that produces ergotamine, infects cereals and forage grasses with a wide host range of more than 400 plant species3. These include economically significant crops, such as rye, wheat and barley and temperate grasses such as tall fescue. The temperate grasses tall fescue and perennial ryegrass can also be infected with endophytic fungi of the Epichloë species which produces the major ergot alkaloid ergovaline. The asexual nonpathogenic species, in particular E. festucae var. lolii and E. coenophiala, are commonly utilised in pasture-based agriculture as they enhance disease and insect pest control and thus improve pasture performance3–6. However, ergovaline has well documented effects on animal welfare, including poor weight gain from reduced feed intake, decreased fertility, and poor milk production7.
Host plant-Clavicipitaceae fungi associations lead to production of ergot alkaloids that are known to cause ergotism in humans and other mammals who consume contaminated grains or pasture3. The most potent and abundant of the ergopeptides produced by C. purpurea and Epichloë sp. are ergotamine and ergovaline respectively. The physiological effects observed in animals exposed to ergotamine or ergovaline are comparable in intensity and duration. These include effects on blood pressure, heart rate and thermoregulatory dysfunction8–10. Furthermore, in vitro studies show the most potent contractile responses of veins and arteries occur in response to these two mycotoxins when compared to other ergopeptides produced by the fungi11–17.
Ergopeptides, such as ergotamine and ergovaline, are the most structurally complex ergot alkaloids, comprising D-lysergic acid linked via an amide bond to a three-membered peptide7. The alkaloids vary only in the composition of the peptide i.e. L-alanine, L-phenylalanine and L-proline in ergotamine and L-alanine, L-valine and L-proline in ergovaline.
Studies on the ergopeptides show they cause physiological dysfunction in respiratory, thermoregulatory, cardiac and vasomotor function as demonstrated in animal bioassays investigating the effects of ergovaline and ergotamine7–9,18. However, the simple ergoamide, ergine, with only a basic D-lysergic acid structure attached to an amide, is reported to possess psychotropic properties19.
Consumption of contaminated rye related products such as bread frequently caused ergotism epidemics throughout the Middle Ages3. Despite the major impact of these outbreaks, there are also historical reports of medicinal uses as well. For example, midwives used the ergot sclerotia to accelerate childbirth or initiate abortion in the sixteenth century. Later in the nineteenth century the ergot alkaloids were used to prevent excessive bleeding in childbirth and is used even today in developing countries, which contributes to the high rates of maternal mortalities3. Furthermore, in the latter half of the nineteenth century, controlled dosages of ergot alkaloids such as ergotamine were effectively used to treat severe and acute migraines2,20. In more recent times ergot alkaloids have been modified for pharmaceutical use and these include compounds such as pergolide and cabergoline which are used for neurological disorders including Parkinsons disease and Restless leg syndrome21.
Naturally occurring ergot alkaloids exert their effects on dopamine, serotonin and adrenaline neurotransmitter receptor sites, acting as partial agonists and in some cases as antagonists. Studies conducted on ergot alkaloid producing fungus, E. coenophialum, an endophyte associated with tall fescue grass (Lolium arundinaceum), have shown to disrupt brain dopaminergic and serotonergic mechanisms in the central nervous system22,23 as well as inhibit activity of Na+/K+ ATPase, essential for maintenance of neuronal membrane potential24.
Despite studies evaluating the effect of mycotoxins on the central nervous system, the mode of action of the ergot alkaloid family of toxins within the brain is still largely unknown. To address this, we investigate the effects of ergotamine on the metabolomic profile of the mouse brain and identify key metabolites associated with the physiological and behavioural effects elicited by animals exposed to ergot alkaloids.
Results
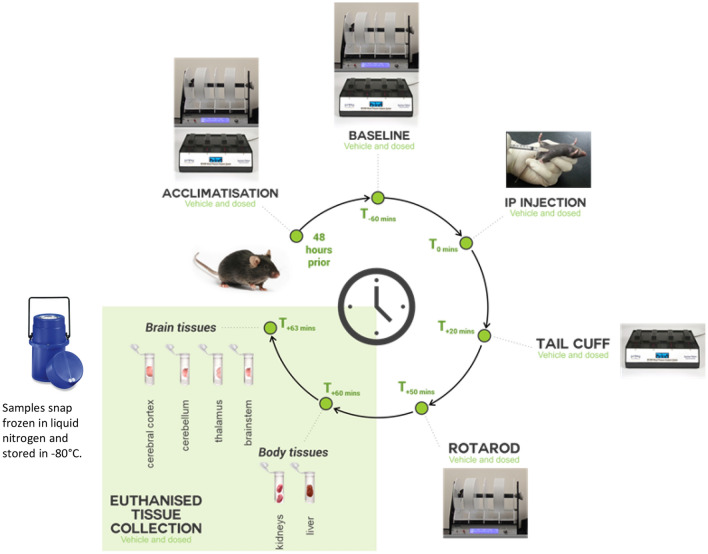
To investigate the effects on the central nervous system, various brain tissues (cerebral cortex, brainstem, thalamus and cerebellum) were harvested from vehicle control (ETVEH), ergotamine high dose (ETHIGH) and ergotamine low dose (ETLOW) treated mice 1 h post exposure (Fig. 1) and the metabolite extracts were analysed using ESI+ Liquid Chromatography-Mass Spectrometry (LCMS).
Figure 1.
Experimental design of mouse bioassay for ergot alkaloid intoxication.
PCA plots of untreated and treated brain tissues revealed separation of the four regions, with some overlap in the thalamus and cerebellum regions of the brain (Fig. 2). It is not unexpected that the metabolome of the individual regions of the brain are distinct due to their inherently unique functions. All subsequent analyses were conducted separately for each brain region.
Figure 2.
PCA scores plots of ESI + UHPLC-HRMS data coloured by (a) brain tissues: brainstem, cerebellum, cerebral cortex and thalamus and (b) treatments: ETHIGH (blue; 0.05 mg/kg; n = 8), ETLOW (green; 0.025 mg/kg; n = 6) and ETVEH (orange; 1% lactic acid; n = 8).
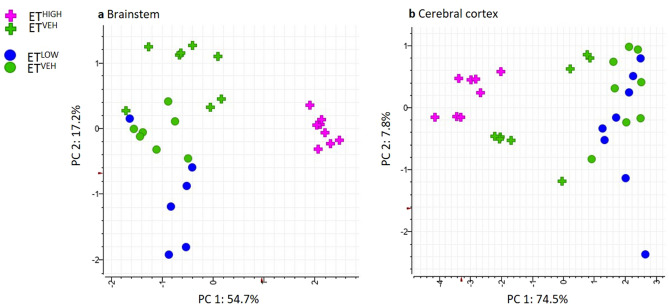
A total of 3096 features were extracted from all brain tissue samples. Prior to statistical analysis, PCA plots of individual brain regions were generated to assess the reproducibility of the Pooled Biological Quality Control (PBQC) samples (Supplementary Fig. S1) for intensity drifts along the batch. Data dimensionality reduction was achieved using N-Way ANOVA on each of the brain tissue regions based on the treatment effect. The Benjamini-Hochberg (BH) correction criteria was used to adjust the significance (p value) of each of the variables, and the subsequent adjusted p value is referred to as a Q-value. A data subset with features satisfying Q-value < 0.05 were represented by 19 significant features in the brainstem. PCA plots performed on the dataset (n = 32) resulted in separation between classes brainstem ETHIGH and ETVEH across Eigenrow (herein Principal Component, PC) 1. A PCA plot generated for the brainstem represented 72% of the total variance (Fig. 3a). Most metabolic variation occurred between classes ETHIGH and ETVEH (54.7%, PC 1) compared to ETLOW and ETVEH (17.2%, PC 2). An orthogonal projection to latent structure discriminant analysis (OPLS-DA) model was applied to full datasets of the brainstem comparing ETHIGH and ETLOW treatments to ETVEH. The OPLS-DA scores plot revealed discrimination between treatment groups compared to controls in the brainstem (Supplementary Fig. S2). However, evaluation of model performance indicated poor predictive performance and goodness of fit for ETHIGH vs ETVEH (Q2 = 0.150, R2Y = 0.755, R2X = 0.057) and ETLOW versus ETVEH (Q2 = 0.325, R2Y = 0.771, R2X = 0.078). The overall models were not significant, indicated by 100 different model permutations for ETHIGH vs ETVEH (p value = Q2: p = 0.18 and R2Y: p = 0.64) and ETLOW vs ETVEH (p value = Q2: p < 0.01 and R2Y: p = 0.48).
Figure 3.
PCA scores plot of significant features generated from N-Way ANOVA of (a) brainstem (Q < 0.05) acquired from ESI+ UHPLC-HRMS of aqueous tissue extracts, representing classes ETHIGH (pink; n = 8), ETLOW (blue; n = 6) and ETVEH (green; n = 8) and (b) cerebral cortex (Q < 0.01) acquired from ESI+ UHPLC-HRMS of aqueous tissue extracts, representing classes ETHIGH (pink; n = 8), ETLOW (blue; n = 8) and ETVEH (green; n = 8).
A data subset with features satisfying a more stringent Q-value (Q < 0.01) cut-off was applied to the N-Way ANOVA results of the cerebral cortex, to allow discrimination of treatment effects in the PCA model. The cerebral cortex region showed dysregulation of 26 metabolites with a generated PCA plot representing 82.3% of the total variance (Fig. 3b). Only the ETHIGH and ETVEH (74.5%, PC 1) treatments could be discriminated in the PCA model. An orthogonal projection to latent structure discriminant analysis (OPLS-DA) model was applied to full datasets of the cerebral cortex comparing ETHIGH and ETLOW treatments with ETVEH. The OPLS-DA scores plot revealed discrimination between treatment groups compared to controls in the cerebral cortex (Supplementary Fig. S3). However, evaluation of model performance indicated poor predictive performance and goodness of fit for ETHIGH vs ETVEH (Q2 = 0.137, R2Y = 0.690, R2X = 0.058) and ETLOW vs ETVEH (Q2 = − 0.032, R2Y = 0.744, R2X = 0.058). The overall models were not significant indicated by 100 different model permutations for ETHIGH vs ETVEH (p value = Q2: p = 0.12 and R2Y: p = 0.56) and ETLOW vs ETVEH (p value = Q2: p = 0.13 and R2Y: p = 0.83).
The cerebral cortex and brainstem regions shared 3 significantly dysregulated metabolites, these include a sterol lipid (Table 1) and 2 unknown compounds (Table 2).
Table 1.
Summary of identified metabolites altered in the brain tissue in mice treated with ergotamine compared to vehicle control.
| Identity | TR (min) | Mass (m/z) [M + H]+ | Molecular formula | Mass Error (ppm) | Tissue | ETHIGH versus ETVEH | ETLOW versus ETVEH | N-Way ANOVA | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Effect size | * | Effect size | * | Q-Value (BH adjusted p value) | MS2 and MS3 ions | Metabolite Level | ||||||
| 2-arachidonylglycerol | 11.29 | 379.2835 | C23H38O4 | − 2.0536 | brainstem | 1/3.59 | ↓ | 1/1.79 | ↓ | 0.014 | 287.2375, 269.2271, 203.1798 | 2 |
| Epinephrine | 2.96 | 184.0966 | C9H13NO3 | − 1.1178 | brainstem | 1.13 | ↑ | 1/1.57 | ↓ | 0.039 | 166.0867, 120.0808, 124.0759 | 1 |
| Pantetheine 4’-phosphate | 2.94 | 359.1032 | C11H23N2O7PS | − 4.3505 | brainstem | 1.03 | ↑ | 1/1.81 | ↓ | 0.039 | – | 3 |
| Sterol lipid | 8.72 | 415.2109 | C24H30O6 | − 1.5281 | brainstem | 7.36 | ↑ | 1.206 | ↑ | 3.23 × 10−6 | 303.1205, 264.1001 | 4 |
| cerebral cortex | 3.47 | ↑ | 1/1.89 | ↓ | 1.99 × 10−3 | |||||||
| Adenylosuccinate | 2.45 | 464.0808 | C14H18N5O11P | − 1.1775 | cerebral cortex | 1.94 | ↑ | 1.43 | ↑ | 0.002 | 252.0728, 162.0774, 97.0288 | 2 |
| Isobutyryl-L-carnitine | 3.36 | 232.1540 | C11H21NO4 | − 1.3549 | cerebral cortex | 1.79 | ↓ | 1.27 | ↑ | 0.002 | 173.0814, 85.0286 | 2 |
| S-3-oxodecanoyl cysteamine | 7.06 | 246.1517 | C12H23NO2S | − 2.2079 | cerebral cortex | 2.84 | ↑ | 1.25 | ↓ | 0.004 | 229.1263, 183.1204 | 2 |
*↑ = Up-regulated, ↓ = Down-regulated.
Table 2.
Summary of significant unknown metabolites altered in the brain (cerebral cortex and brainstem) in ergotamine treated mice compared to control.
| Group | TR (min) | Mass (m/z) [M + H]+ | Tissue | ETHIGH versus ETVEH | ETLOW versus ETVEH | N-Way ANOVA | ||
|---|---|---|---|---|---|---|---|---|
| Effect size | * | Effect size | * | Q-Value (BH adjusted p value) | ||||
| 1 | 8.27 | 623.3156 | brainstem | 1/70.85 | ↓ | 1/1.27 | ↓ | 0.014 |
| 2 | 2.48 | 86.09672 | brainstem | 1/1.00 | ↓ | 1/1.34 | ↓ | 0.039 |
| 3 | 4.96 | 199.0939 | brainstem | 9.81 | ↑ | – | – | 0.023 |
| 4 | 1.99 | 267.0585 | brainstem | 1.20 | ↑ | 1.43 | ↑ | 0.039 |
| 5 | 10.18 | 292.2992 | brainstem | 1/3.03 | ↓ | 1/1.41 | ↓ | 0.036 |
| 6 | 2.02 | 308.5818 | brainstem | 1.32 | ↑ | 1/1.52 | ↓ | 0.039 |
| 7 | 8.04 | 387.1794 | brainstem | – | – | 1/4.20 | ↓ | 3.23 × 10−6 |
| 8 | 12.5 | 387.1972 | brainstem | 1.50 | ↑ | 1/7.24 | ↓ | 0.006 |
| 9 | 2.39 | 408.1484 | brainstem | 1.13 | ↑ | 1/1.26 | ↓ | 0.039 |
| 10 | 8.04 | 425.1353 | brainstem | – | – | 1/4.59 | ↓ | 6.34 × 10−5 |
| cerebral cortex | – | – | 1/4.76 | – | 1.11 × 10−5 | |||
| 11 | 2.26 | 437.1332 | brainstem | 1.48 | ↑ | 1/1.44 | ↓ | 0.023 |
| 12 | 2.39 | 559.1500 | brainstem | 1.31 | ↑ | 1/2.15 | ↓ | 0.025 |
| 13 | 5.39 | 910.849 | brainstem | 1/1.40 | ↑ | 2.93 | ↑ | 0.039 |
| 14 | 1.18 | 258.1096 | cerebral cortex | 1/1.33 | ↓ | 1.04 | ↑ | 2.51 × 10−4 |
| 15 | 1.28 | 269.0875 | cerebral cortex | 1.71 | ↑ | 1/1.59 | ↓ | 5.05 × 10−4 |
| 16 | 2.39 | 269.0876 | cerebral cortex | 1.70 | ↑ | 1/1.31 | ↓ | 6.84 × 10−4 |
| 17 | 2.39 | 291.0695 | cerebral cortex | 1.45 | ↑ | 1/1.21 | ↓ | 5.05 × 10−4 |
| 18 | 16.7 | 123.0553 | cerebral cortex | 1/4.53 | ↓ | 1.22 | ↑ | 7.11 × 10−4 |
| 19 | 2.39 | 137.0456 | cerebral cortex | 1.70 | ↑ | 1/1.28 | ↓ | 5.05 × 10−4 |
| 20 | 1.82 | 159.0276 | cerebral cortex | 1.82 | ↑ | 1/1.41 | ↓ | 8.93 × 10−4 |
| 21 | 2.55 | 162.0581 | cerebral cortex | 2.73 | ↑ | 1/1.27 | ↓ | 6.88 × 10−3 |
| 22 | 4.99 | 204.1050 | cerebral cortex | 3.07 | ↑ | 1/1.31 | ↓ | 5.05 × 10−4 |
| 23 | 1.35 | 218.1384 | cerebral cortex | 1/2.10 | ↓ | 1.15 | ↑ | 2.19 × 10−4 |
| 24 | 2.61 | 218.1384 | cerebral cortex | 1/1.86 | ↓ | 1.19 | ↑ | 5.05 × 10−4 |
| 25 | 7.06 | 246.1517 | cerebral cortex | 2.84 | ↑ | 1/1.25 | ↓ | 4.37 × 10−3 |
| 26 | 1.25 | 276.1185 | cerebral cortex | 2.01 | ↑ | 1/1.40 | ↓ | 6.87 × 10−3 |
| 27 | 1.28 | 307.0434 | cerebral cortex | 1.75 | ↑ | 1/1.44 | ↓ | 5.05 × 10−4 |
| 28 | 9.63 | 315.1949 | cerebral cortex | 7.93 | ↑ | 1/1.37 | ↓ | 8.93 × 10−4 |
| 29 | 2.39 | 353.0399 | cerebral cortex | 2.14 | ↑ | 1/1.52 | ↓ | 1.99 × 10−3 |
| 30 | 2.39 | 369.0123 | cerebral cortex | 1.67 | ↑ | 1/1.30 | ↓ | 4.37 × 10−3 |
| 31 | 2.45 | 387.9961 | cerebral cortex | 1.97 | ↑ | 1/1.47 | ↓ | 1.99 × 10−3 |
| 32 | 1.28 | 464.0806 | cerebral cortex | 1.68 | ↑ | 1/1.51 | ↓ | 9.31 × 10−3 |
| 33 | 2.45 | 502.0274 | cerebral cortex | 2.09 | ↑ | 1/1.40 | ↓ | 9.95 × 10−4 |
| 34 | 8.04 | 409.1614 | brainstem | – | – | 1/4.20 | ↓ | 5.34 × 10−7 |
| cerebral cortex | – | – | 1/4.20 | ↓ | 1.51 × 10−9 | |||
*↑ = Up-regulated, ↓ = Down-regulated.
N-Way ANOVA of the treatments ETHIGH, ETLOW and ETVEH in the thalamus and brainstem region showed no significant impact at Q < 0.05.
Together these data demonstrate that ergotamine treated (ETHIGH and ETLOW) compared to ETVEH animals show significant metabolic variation only in the brainstem and cerebral cortex regions of the brain. PCA plots of the significant (19 metabolites; Q-value < 0.05) metabolites in the brainstem region revealed a dose related effect, with clear separation between ETHIGH and ETLOW. However, in the cerebral cortex region PCA of the significant metabolites (26 metabolites; Q-value < 0.01) showed that ETLOW clustered with the ETVEH, indicating that only ETHIGH had central effects.
Identification of significant features
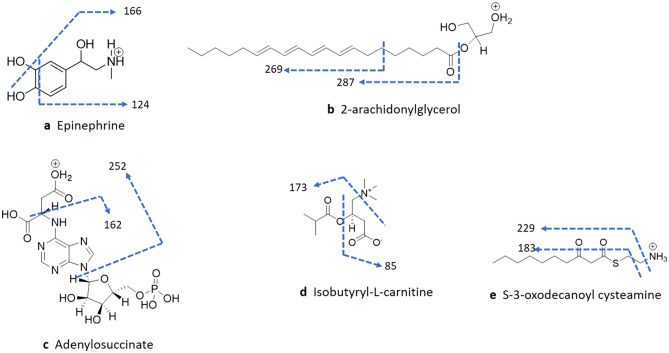
Identification of metabolites impacted in the brainstem and cerebral cortex of animals exposed to ergotamine 1 h post treatment was investigated. For this, accurate masses were compared to the Human Metabolome Database (HMDB). Identification of 7 of the 45 differentially expressed metabolites was confirmed using either MS or MSn fragmentation of the parent ion (Table 1, Fig. 4). There were 5 metabolites that achieved Level 2 identification and above (as defined by the Metabolomics Standards Initiative25,26); these include 2-arachidonylglycerol (Q-Value = 0.0386), epinephrine (Q-Value = 0.0386), adenylosuccinate (Q-Value = 0.0020), isobutyryl-L-carnitine (Q-Value = 0.0020) and S-3-oxodecanoyl cysteamine (Q-Value = 0.0004). MS2 fragmentation data of epinephrine and 2-arachidonylglycerol were consistent with those in the MzCloud database.
Figure 4.
MSn fragmentation confirm the identity of compounds differentially expressed in the brainstem and cerebral cortex regions of the brain.
To confirm identity of the compounds, targeted MS2 and MS3 was performed on the 7 analytes (Supplementary Figs. S4–S8).
The catecholamine, epinephrine eluted at 2.96 min ([M + H]+, m/z 184.0966) and the MS2 mass spectrum gave rise to the intense ion m/z 166.0867 indicating deoxygenation. Subsequent demethylation of the N-CH3 and loss of remaining hydroxyl groups resulted in the less intense ion m/z 120.0808. Further MS3 of the most intense MS2 ion (m/z 166.0867) resulted in fragmentation of the aromatic ring (m/z 124.0759), confirming the presence of the compound (Fig. 4a).
The monoacylglycerol, 2-arachidonylglycerol (2-AG) eluted at 11.29 min (m/z 379.2835), MS2 fragmentation led to loss of the glycerol moiety m/z 287.2375. The MS2 ion m/z 287.2375 fragmentation resulted in deoxygenation and dehydrogenation (m/z 269.2271) prior to loss of the alkyloxy chain and (m/z 203.1798). The elution time and fragmentation pattern confirmed the identification of the compound (Fig. 4b).
Adenylosuccinate eluted at 2.45 min (m/z 464.0808) and MS2 fragmentation of the ion resulted in loss of the dehydroxylated tetrahydrofuran phosphate moiety (m/z 252.0728). The smaller fragments m/z 162.0774 and m/z 97.0288 represented the purine ring attached to the secondary amine group and a dehydrogenated methyl hydroxy tetrahydrofuran ring, respectively (Fig. 4c).
Isobutyryl-L-carnitine eluted at 3.36 min (m/z 232.1540). MS2 fragmentation led to fragmentation of the tertiary amine, m/z 173.0814, subsequent MS3 of the ion resulted in loss of the isobutyric acid group, m/z 85.0286 (Fig. 4d).
S-3-oxodecanoyl cysteamine eluted at 7.06 min (m/z 246.1517), and MS2 resulted in loss of the amine (m/z 229.1263) and subsequent MS3 of the ion represented the alkyl sulfane group (m/z 183.1204) (Fig. 4e).
The predicted molecular formula for m/z 415.2109 (C24H30O6) together with the fragmentation pattern and retention time (8.72 min), strongly suggest that the group belongs to the sterol lipid class of compounds (Level 4 identification).
The retention time 2.94 min and accurate mass (m/z 359.1032) in addition to a HMDB match suggest Level 3 identification of the compound pantetheine 4’-phosphate.
There are another 34 unknown metabolites that were also significantly altered in the brain (Fig. 3), and the accurate mass and retention time are listed in Table 2.
Receiver-operating characteristic (ROC) curves were used to evaluate the specificity and sensitivity of disrupted metabolites in the brainstem and cerebral cortex exposed to ETHIGH compared to ETVEH. Sensitivity and 1-specificity corresponded to the true positive rate and false positive rate, respectively27. Areas under the curve (AUCs) have been applied as useful indices for discriminating the diagnostic values of features. If the AUC is greater than 0.7, the features are regarded as useful biomarkers28–31. AUC values greater than 0.7 are considered to be sensitive and specific. Using this criteria, 8 biomarkers in the brainstem (Supplementary Table S1) and 6 biomarkers in the cerebral cortex (Supplementary Table S2) were identified in ETHIGH when compared to ETVEH. AUC results demonstrated that predictive models could be generated to determine ergotamine exposure in brain tissue of animals.
To evaluate the predictive performance of sub-clinical exposure (ETLOW) to ergotamine, a combination of biomarkers for ETHIGH was tested and linear support vector machine (SVM) was applied. Based on the prediction performance of ETLOW, 2-arachidonylglycerol was selected to build a classification model for the brainstem region. The ROC curve generated from the model resulted in an AUC of 1.0 and 1–1 at 95% confidence interval with 50% sample hold-out (Fig. 5). The cross-validation accuracy of the model showed good prediction performance of 0.88 based on 100 cross validations. The predictive performance of the model was found to be significant with 100 permutations (p = 0.010). The reliability of the model was tested on ETLOW brain regions. The SVM model predicted with 67% (4 out of 6 replicates of ETLOW). These results indicate that the SVM model based on biomarkers confirms the importance of the metabolite 2-arachidonylglycerol in mild and severe cases of ergotamine intoxication in the brainstem.
Figure 5.
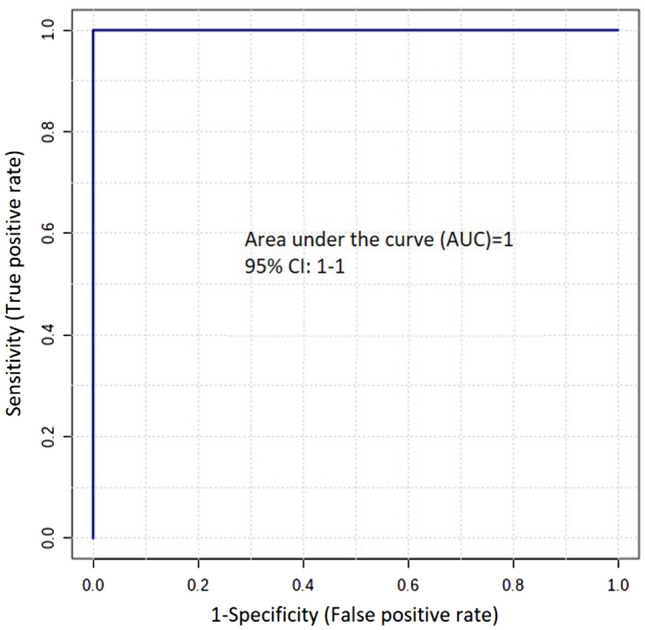
ROC curve of 2-arachidonylglycerol showing AUC—1.0 and sensitivity and specificity at a 95% confidence interval of 1–1.
Discussion
This study investigated the mode and site of action of ergot alkaloids using ESI+ LCMS metabolite profiling to determine the effect of ergotamine exposure on brain metabolism in male C57Bl/6J mice at 1 h post treatment. Our results demonstrate that ergotamine elicits region specific effects in the cerebral cortex and brainstem, but not the cerebellum and thalamus. Ergotamine treated mice at high doses exerted the greatest metabolic variation in the brainstem where clear dose-related effects were also observed in the metabolite 2-AG. This is further corroborated by the detection of ergotamine in this region as previously reported in these same mice7. Recently, the clinical signs presenting in animal models exposed to ergotamine have been attributed to physiological effects in both blood pressure and heart rate that are regulated by the autonomic nervous system of the brainstem7. However, the physiological profile in these same mice were not affected in a dose dependent manner. This may be due to the receptors mediating the effect are reaching a physiological threshold32.
Ergotism in humans and other mammals results in behavioural effects and motor incapacitation which is associated with central nervous stimulation33–37. Our findings suggest that only intoxication at high concentrations of ergotamine effects the cerebral cortex metabolome significantly. This is in agreement with early studies that have shown that only very high doses of ergotamine result in behavioural disorders and motor incoordination in animals, including rodents33.
Non-detectable levels of ergotamine in the cerebral cortices7 suggest that the resulting behavioural effects could likely occur via excitation of afferent fibres entering the cerebral cortex from the neuromodulatory or cranial nerve nuclei of the brainstem.
Metabolomic profiling identified 45 metabolites significantly altered in the brain by ergotamine, that may be responsible for exerting a major effect in the brain at 1 h post treatment. Seven of these were identified using either MS or MSn fragmentation of the parent ion.
The monoacylglycerol 2-AG is a key intermediate in multiple lipid metabolic pathways, and an endogenous endocannabinoid responsible for important physiological pathways such as locomotor activity, stress and anxiety38. A reduction of 2-AG in the brainstems of ergotamine treated mice relative to vehicle controls was found in this study. Decreased levels of 2-AG is linked to anxiety-like behaviour39, which is further supported by the behavioural phenotype elicited in mice exposed to high-levels of ergotamine33. The effect size of 2-AG compared to ETVEH in this study decreased in a dose-dependent manner. Thus, 2-AG is shown to be a key metabolite for ergot alkaloid toxicity and its importance is further demonstrated by its ability to predict mild and severe cases of ergotamine intoxication in the ROC curve analysis.
The physiological phenotype of animals exposed to ergotamine is characterised by vasoconstriction which is likely to be responsible for other symptoms including increased blood pressure as well as cardiovascular and respiratory effects7,9. Perturbation in epinephrine neurotransmitter levels is associated with vasoconstriction and also likely to disrupt blood pressure and heart rate40 similar to those observed in ergotamine intoxicated animals. Ergotamine exposed animals suffer from gastrointestinal41 and cerebral vessel dilation42 all of which are associated with alterations in epinephrine levels40 mediated primarily through α-adrenergic receptors33,43. Epinephrine is synthesized in the brainstem in the medulla oblongata region and is involved in regulation of physiological functions of the sympathetic nervous system44. Epinephrine neurons in the brain, particularly the brain stem and hypothalamus regions, are involved in regulation of body temperature, reflex bradycardia as well as motor performance45.
Furthermore, variation in the synthesis of the metabolite pantetheine 4’-phosphate, a key intermediate in the biosynthesis of Coenzyme A (CoA) can lead to disruption in metabolic systems46,47 as CoA plays a key role in carbohydrate, lipid and amino acid metabolism46,47.
Together these findings support the hypothesis that the disrupted levels of epinephrine in ergot alkaloid-intoxicated animals show a complex interaction with biogenic receptors, primarily an α-adrenergic mediated response. Furthermore, psychoactive effects present in the behavioural phenotype can be attributed to disruption of lipids, particularly 2-AG and downstream metabolic systems.
The cerebral cortex comprises regions that regulate emotion, cognition, language, memory, homeostasis as well as auditory and visual areas48. The perturbed metabolites at high doses of ergotamine in the cerebral cortices include the energy related metabolites isobutyryl-L-carnitine and S-3-oxodecanoyl cysteamine. Impairment in energy metabolism is known to occur as a consequence of stress and toxicity and typically in a pathological state, where there is increased demand for energy production. Furthermore, ergotamine exposed animals show increased levels of adenylosuccinate in the cerebral cortex. The accumulation of adenylosuccinate in bodily fluids occurs due to a deficiency of adenylosuccinase, the enzyme which catalyses the conversion of adenylosuccinate into AMP in the synthesis of purine nucleotides49. The metabolic defect which results in a deficiency of adenylosuccinase can occasion mental impairment, ranging from a slight delay to severe retardation49.
These studies indicate that behavioural effects and motor incoordination exhibited by ergot alkaloid intoxicated animals at high doses of the toxin could be attributed to the metabolic disruption in the cerebral cortex.
Conclusion
This is the first study exploring the effects of ergot alkaloid toxicity on the brain metabolome in a rodent model. Metabolomics profiling identified key differences in epinephrine, 2-AG and panthetheine 4′-phosphate in the brainstem region, which we suggest are linked to the physiological effects exhibited by animals exposed to the toxin. Furthermore, pathophysiological processes elicited only in response to high doses of the toxin in the cerebral cortex, could contribute to the behavioural dysfunction and motor incoordination exhibited in animals ingesting ergot alkaloids. Understanding the cause and biochemical consequences of toxicoses provide insight into potential treatments or pharmacological uses. Thus, future studies should be undertaken to determine the identification of the unknown metabolites in this study.
Materials and methods
Toxins
Ergotamine (98% pure) was purchased from Novachem Pty Ltd, (B-MYC3600-5). Ergotamine was administered by intraperitoneal (ip) injection in the vehicle carrier 1% lactic acid (neat lactic acid, Sigma Aldrich, diluted with ultrapure distilled water, Invitrogen).
Ergotamine was administered at 0.025 mg/kg bwt (ETLOW) and 0.05 mg/kg bwt (ETHIGH). These doses correspond to sub-clinical (low) and potent (high) doses that are calculated based on levels of feed intake of ruminants, concentrations in pasture and pharmacological aspects such as bioavailability of the toxin8. A negative control group was used for comparison of physiological and behavioural observations for each cohort, vehicle control (ETVEH) treated with 1% lactic acid via intraperitoneal (ip) injection.
Animal studies
All animal studies were approved by the La Trobe University Animal Ethics Committee (Protocol number 18–21) and were conducted in accordance with the Australian Code of Practice for the Care and Use of Animals for Scientific Purposes set out by the National Health and Medical Research Council of Australia. The research study was conducted in compliance with the ARRIVE (Animal Research: Reporting of In Vivo Experiments) guidelines50. Animal experimental procedures were as previously described7 and provided here in brief. The mice were housed in groups of two to four during the experimental period in individually ventilated cages (Tecniplast, Buguggiate, Italy) with standard pellet food and water available ad libitum. Ambient temperature of housing and testing rooms was 21 ± 2 °C and mice were housed under a 12-h light–dark cycle (lights on at 7am). A total of 48 male C57Bl/6J mice 8–12 weeks old were sourced from a breeding colony at the Walter and Eliza Hall Institute of Medical Research, Melbourne, Victoria. Animals were allowed to acclimatise to the facility conditions for a minimum of one week prior to the experiment phase. All animals underwent rotarod testing to examine effects of intoxication on movement and tail plethysmography to observe vasomotor effects7.
Metabolite extraction
Tissues of mice exposed to low (ETLOW; 0.025 mg/kg bwt, n = 6) or high (ETHIGH; 0.05 mg/kg bwt, n = 8) doses of ergotamine were collected at 1 h post-treatment and compared to vehicle injected controls (ETVEH; n = 8) by metabolomic analysis7. Animals were euthanized by cervical dislocation and brain tissues dissected into cerebral cortex, thalamus, cerebellum and brainstem were harvested. Samples were snap-frozen in liquid nitrogen before storage at − 80 °C for metabolomics analysis.
Frozen samples of thalamus and cerebral cortex were transferred into 4 mL polycarbonate tubes with 3/8" stainless steel grinding balls and kept frozen in liquid nitrogen. Sample tubes were placed into pre-frozen 24 well cryo-blocks on the Geno/Grinder 2010 (SPEX Sample Prep, Metuchen, NJ, USA) and the tissues were homogenised at 1700 rpm for 1–5 min7,51. The fine powder was stored at − 80 °C until weighed. Frozen cerebellum and brainstem tissues were hand-ground in a chilled mortar and pestle with liquid nitrogen. The fine powder was stored at – 80 °C until weighed.
Cerebral cortex, thalamus, cerebellum and brainstem (20–23 mg) samples were each weighed in 2 mL microcentrifuge tubes (Eppendorf SafeLock). Tissue samples were extracted using a 4:1 (v/v) MeOH/H2O mono-phasic methanol extraction7. Briefly, 500 μL chilled 80% methanol was added to frozen tissue powder and vortex-mixed (15 s). Samples were sonicated on ice for 10 min, incubated at room temperature for a further 10 min, then centrifuged for 5 min at 10,000 rpm (9503 × g). The extraction was repeated and supernatant pooled to give a final volume of 1 mL and stored at − 80 °C.
A volume of 50 μL was transferred into HPLC vials containing inserts ready for LCMS analysis of polar metabolites. Each extract of a tissue type (2 µl of each) was combined to generate a pooled biological quality control (PBQC) sample, which was used to monitor analytical reproducibility. The remaining supernatant was evaporated under a stream of nitrogen, re-constituted in 100 µL of 4:1 (v/v) MeOH/H2O, and transferred to HPLC vials containing 200 µL inserts for quantitative LCMS analysis.
Liquid chromatography-mass spectrometry (LCMS) analysis
Metabolite profiling was performed on the Vanquish Ultra-High Performance Liquid Chromatography (UHPLC) system (Thermo Fisher Scientific, Bremen) with a binary pump, autosampler and temperature-controlled column compartment coupled with a QExactive (QE) Plus mass spectrometer (Thermo Fisher, Waltham, MA, USA; Thermo, Bremen, Germany)7 for MS and MS2 analysis or a Thermo Scientific LTQ Orbitrap Velos ion trap MS system (Thermo Scientific, Waltham, MA, USA; Bremen, Germany) for MS3 analysis. Metabolites eluted on a Thermo Fisher Scientific Hypersil Gold 1.9 µm, 100 mm × 2.1 mm column. The initial conditions were 2% B before initiating a linear gradient to 100% B over 11 min, and this was maintained for 4 min before returning to the initial gradient conditions at a flow of 0.3 mL/min (total run time of 20 min).
The Thermo Fisher QExactive Plus mass spectrometer was used to acquire MS data and set at positive mode over a mass range of 70–1200 amu with resolution set at 17,000. Nitrogen was used as the sheath, auxiliary and sweep gas at a flow rate of 28, 15 and 4 L/min, respectively, and spray voltage was set at 3600 V (positive mode)52. Samples were randomized, and blanks (80% methanol) were injected every five samples. A PBQC was run every 10 samples. Prior to data acquisition, the system was calibrated with Pierce LTQ Velos ESI Positive and Negative Ion Calibration Solution (Thermo Fisher Scientific). Mass spectrometry data was acquired using Thermo Xcalibur V. 2.1 (Thermo Fisher Scientific Inc., USA). For MS2 analysis, data were acquired in full-scan MS/data-dependent MS2 (ddMS2) mode for selected samples. MS cycles were composed of 1 Full MS and up to 5 ddMS2. Ions within the inclusion list detected in the full MS survey scan (intensity threshold 4.0 × 104) triggered a MS2 event at the peak apex with an isolation window of 0.4 m/z. A 2.0 s delay was required for the same ion to trigger a new MS2 event (dynamic exclusion). Full MS scans were acquired from m/z 300 to 1200 with a resolution of 70,000 (full width at half maximum, FWHM, at m/z 200); automatic gain control (AGC) target was 3 × 106; maximum injection time (IT) 200 ms. Scans (ddMS2) were acquired at a resolution of 17,500, the AGC target was 1 × 105, and the maximum IT was 50 ms. Ions were fragmented with stepped collision energy (20, 40 and 60%).
Compound fragmentation using MS2 and MS3 analysis was performed using a Thermo Scientific LTQ Orbitrap Velos ion trap MS system (Thermo Scientific, Waltham, MA, USA; Bremen, Germany), with a heated electrospray ionisation (ESI) source. Data-dependent MS2 and MS3 spectra was acquired on target ions and selected samples with normalised collision energy of 35 V and an ion max time of 50 microseconds. Source heater temperature was maintained at 350 °C and the heated capillary was maintained at 320 °C. The sheath, auxiliary and sweep gases was 40, 15 and 8 units respectively, for ESI+ mode. Source voltage was set to 4.2 kV (positive) and with a capillary voltage of − 70 V. Sample injection volumes was 5 µL. Prior to data acquisition, the system was calibrated with Pierce LTQ Velos ESI Positive and Negative Ion Calibration Solution (Thermo Scientific). Spectra was inspected in Thermo Xcalibur Qual Browser v.2.3.26 (Thermo Fisher Scientific).
Prior to data analysis, individual samples were checked for column pressures, variations of PBQC and retention times for instrument stability along the batch.
Data processing and statistical analyses
The data files obtained following LCMS analyses were processed in the Refiner MS module of Genedata Expressionist 12.0 with the following parameters: (1) chromatogram chemical noise subtraction with removal of peaks with less than 4 scans, chromatogram smoothing using moving average estimator over 5 scans, and 70% quantile over 151 scans for noise subtraction, (2) intensity thresholding using a clipping method and a threshold of 100, (3) selection of positive mode data only, (4) chromatogram RT alignment using a pairwise alignment based tree and a maximum RT shift of 2 min, (5) chromatogram peak detection using a 5 scans summation window, a minimum peak size of 0.1 min, a maximum merge distance of 0.05 Da, a boundary merge strategy, a maximum gap/peak ratio of 70% with moving average smoothing over 10 scans for peak RT splitting (6) chromatogram isotope clustering using RT and m/z tolerance of 0.05 min and 0.05 Dalton respectively with a maximum charge of 2, (7) adduct detection using mainly M + H and allowable adducts (M + 2H, M + K, M + Na, M-H2O + H) and (8) singleton filter for removal of peaks that do not belong to a cluster, resulting in a total of 3096 number of features (Supplementary Fig. S9).
Statistical analyses were performed using the Analyst module of Genedata Expressionist 12.0. Principal component analyses (PCA) were performed to identify tissue and treatment differences. Overlay of the PBQC and samples allowed for the validation of the high-quality dataset by ensuring that RT variation, mass error and sensitivity changes throughout the run were consistent. Statistical significances between treatments within tissue types were assessed by N-Way ANOVA and sorted according to BH Q-Value. Levels of significance for brainstem (Q < 0.05) and cerebral cortex (Q < 0.01) were applied and PCA performed on significant metabolites.
An OPLSDA model was applied to the brainstem and cerebral cortex datasets using MetaboAnalyst 3.053 Prior to multivariate analysis missing value imputation was applied and features with > 50% missing values were removed and remaining missing values replaced by 1/5 of the minimum positive value for each feature. Subsequently, the data were log transformed and mean centered to achieve normality and homoscedasticity. A prediction model was also developed on MetaboAnalyst 3.0 to discriminate effects between control and treatment groups using ROC curve model. The significant features were evaluated and identified for each brain tissue for ergotamine high dose treatment. The ROC area under the curve (AUC) analyses for tissues brainstem and cerebral cortex were ranked based on AUC values (Supplementary Tables S1 and S2). All potential biomarker candidates were subjected to linear SVM (support vector machine) to establish a statistical prediction model.
Analyte identification of significant metabolites was performed by searching experimental MS1 data through the following databases: Human Metabolome DataBase (HMDB) (http://hmdb.ca); ChemSpider (http://chemspider.com); and Lipid Maps®(http://www.lipidmaps.org); . MS2 data was searched on MzCloud (http://mzcloud.org) and MetFragment®(http://ipb-halle.github.io/MetFrag/).
Supplementary Information
Acknowledgements
The authors thank the Molecular Phenomics group at Agriculture Victoria and La Trobe University Central Animal House for their assistance. The research described here was funded by Agriculture Victoria, Dairy Australia through the Dairy Futures Cooperative Research Centre and DairyBio.
Author contributions
P.R.: Conceptualization, Supervision, Resources, Project administration, Investigation, Formal analysis, Writing—Original Draft. D.V.: Formal analysis, Writing—Review and Editing. J.H.: Investigation, Writing—Review and Editing. V.E.: Writing—Review and Editing. K.G.: Conceptualization, Supervision, Resources, Writing—Review and Editing. G.C.S.: Conceptualization, Supervision, Resources, Writing—Review and Editing. S.J.R.: Conceptualization, Supervision, Resources, Writing—Review and Editing.
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-98870-4.
References
- 1.Alm T. The witch trials of Finnmark, Northern Norway, during the 17th century: Evidence for ergotism as a contributing factor. Econ. Bot. 2003;57:403–416. doi: 10.1663/0013-0001(2003)057[0403:TWTOFN]2.0.CO;2. [DOI] [Google Scholar]
- 2.Perrin VL. Clinical pharmacokinetics of ergotamine in migraine and cluster headache. Clin. Pharmacokinet. 1985;10:334–352. doi: 10.2165/00003088-198510040-00004. [DOI] [PubMed] [Google Scholar]
- 3.Haarmann T, Rolke Y, Giesbert S, Tudzynski P. Ergot: from witchcraft to biotechnology. Mol. Plant Pathol. 2009;10:563–577. doi: 10.1111/j.1364-3703.2009.00548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Panaccione DG. Origins and significance of ergot alkaloid diversity in fungi. FEMS Microbiol. Lett. 2005;251:9–17. doi: 10.1016/j.femsle.2005.07.039. [DOI] [PubMed] [Google Scholar]
- 5.Klotz JL, Smith DL. Recent investigations of ergot alkaloids incorporated into plant and/or animal systems. Front. Chem. 2015 doi: 10.3389/fchem.2015.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miedaner T, Geiger HH. Biology, genetics, and management of ergot (Claviceps spp.) in rye, sorghum, and pearl millet. Toxins. 2015;7:659–678. doi: 10.3390/toxins7030659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reddy P, et al. Ergot alkaloid mycotoxins: Physiological effects, metabolism and distribution of the residual toxin in mice. Sci. Rep. 2020;10:9714. doi: 10.1038/s41598-020-66358-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Browning R, Jr, Leite-Browning ML. Effect of ergotamine and ergonovine on thermal regulation and cardiovascular function in cattle. J. Anim. Sci. 1997;75:176–181. doi: 10.2527/1997.751176x. [DOI] [PubMed] [Google Scholar]
- 9.McLeay LM, Smith BL, Reynolds GW. Cardiovascular, respiratory, and body temperature responses of sheep to the ergopeptides ergotamine and ergovaline. Am. J. Vet. Res. 2002;63:387–393. doi: 10.2460/ajvr.2002.63.387. [DOI] [PubMed] [Google Scholar]
- 10.Jackson JA, et al. Physiological responses of rats fed loline and ergot alkaloids from endophyte-infected tall fescue. Drug Chem. Toxicol. 1996;19:85–96. doi: 10.3109/01480549609002198. [DOI] [PubMed] [Google Scholar]
- 11.Klotz JL, Bush LP, Strickland JR. A vascular contractility bioassay using bovine right ruminal artery and vein. J. Anim. Sci. 2011;89:1944–1951. doi: 10.2527/jas.2010-3532. [DOI] [PubMed] [Google Scholar]
- 12.Klotz JL, et al. Ergovaline-induced vasoconstriction in an isolated bovine lateral saphenous vein bioassay. J. Anim. Sci. 2007;85:2330–2336. doi: 10.2527/jas.2006-803. [DOI] [PubMed] [Google Scholar]
- 13.Foote AP, Harmon DL, Strickland JR, Bush LP, Klotz JL. Effect of ergot alkaloids on contractility of bovine right ruminal artery and vein. J. Anim. Sci. 2011;89:2944–2949. doi: 10.2527/jas.2010-3626. [DOI] [PubMed] [Google Scholar]
- 14.Klotz JL, Kirch BH, Aiken GE, Bush LP, Strickland JR. Contractile response of fescue-naïve bovine lateral saphenous veins to increasing concentrations of tall fescue alkaloids. J. Anim. Sci. 2010;88:408–415. doi: 10.2527/jas.2009-2243. [DOI] [PubMed] [Google Scholar]
- 15.Pesqueira A, Harmon DL, Branco AF, Klotz JL. Bovine lateral saphenous veins exposed to ergopeptine alkaloids do not relax. J. Anim. Sci. 2014;92:1213–1218. doi: 10.2527/jas.2013-7142. [DOI] [PubMed] [Google Scholar]
- 16.Klotz JL, Kirch BH, Aiken GE, Bush LP, Strickland JR. Effects of selected combinations of tall fescue alkaloids on the vasoconstrictive capacity of fescue-naïve bovine lateral saphenous veins. J. Anim. Sci. 2008;86:1021–1028. doi: 10.2527/jas.2007-0576. [DOI] [PubMed] [Google Scholar]
- 17.Foote AP, et al. Constriction of bovine vasculature caused by endophyte-infected tall fescue seed extract is similar to pure ergovaline. J. Anim. Sci. 2012;90:1603–1609. doi: 10.2527/jas.2011-4513. [DOI] [PubMed] [Google Scholar]
- 18.Browning R, Jr, Thompson FN, Sartin JL, Leite-Browning ML. Plasma concentrations of prolactin, growth hormone, and luteinizing hormone in steers administered ergotamine or ergonovine. J. Anim. Sci. 1997;75:796–802. doi: 10.2527/1997.753796x. [DOI] [PubMed] [Google Scholar]
- 19.Guerre P. Ergot alkaloids produced by endophytic fungi of the genus Epichloë. Toxins. 2015;7:773–790. doi: 10.3390/toxins7030773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Foster JB. Migraine. Traditional uses of ergot compounds. Postgrad. Med. J. 1976;52:12–14. [PubMed] [Google Scholar]
- 21.Jakubczyk D, Cheng JZ, O’Connor SE. Biosynthesis of the ergot alkaloids. Nat. Prod. Rep. 2014;31:1328–1338. doi: 10.1039/C4NP00062E. [DOI] [PubMed] [Google Scholar]
- 22.Porter JK, Stuedemann JA, Thompson FN, Jr, Lipham LB. Neuroendocrine measurements in steers grazed on endophyte-infected fescue. J. Anim. Sci. 1990;68:3285–3292. doi: 10.2527/1990.68103285x. [DOI] [PubMed] [Google Scholar]
- 23.Schillo KK, Leshin LS, Boling JA, Gay N. Effects of endophyte-infected fescue on concentrations of prolactin in blood sera and the anterior pituitary and concentrations of dopamine and dopamine metabolites in brains of steers. J. Anim. Sci. 1988;66:713–718. doi: 10.2527/jas1988.663713x. [DOI] [PubMed] [Google Scholar]
- 24.Moubarak AS, Piper EL, West CP, Johnson ZB. Interaction of purified ergovaline from endophyte-infected tall fescue with synaptosomal ATPase enzyme system. J. Agric. Food Chem. 1993;41:407–409. doi: 10.1021/jf00027a012. [DOI] [Google Scholar]
- 25.Schrimpe-Rutledge AC, Codreanu SG, Sherrod SD, McLean JA. Untargeted metabolomics strategies—Challenges and emerging directions. J. Am. Soc. Mass Spectrom. 2016;27:1897–1905. doi: 10.1007/s13361-016-1469-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sumner LW, et al. Proposed minimum reporting standards for chemical analysis: Chemical Analysis Working Group (CAWG) Metabolomics Standards Initiative (MSI) Metabolomics. 2007;3:211–221. doi: 10.1007/s11306-007-0082-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hajian-Tilaki K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Casp. J. Intern. Med. 2013;4:627–635. [PMC free article] [PubMed] [Google Scholar]
- 28.Greiner M, Pfeiffer D, Smith RD. Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev. Vet. Med. 2000;45:23–41. doi: 10.1016/S0167-5877(00)00115-X. [DOI] [PubMed] [Google Scholar]
- 29.Kottas M, Kuss O, Zapf A. A modified Wald interval for the area under the ROC curve (AUC) in diagnostic case-control studies. BMC Med. Res. Methodol. 2014 doi: 10.1186/1471-2288-14-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Graham SF, Holscher C, Green BD. Metabolic signatures of human Alzheimer’s disease (AD): 1H NMR analysis of the polar metabolome of post-mortem brain tissue. Metabolomics. 2014;10:744–753. doi: 10.1007/s11306-013-0610-1. [DOI] [Google Scholar]
- 31.Li Y, et al. A systematic strategy for screening and application of specific biomarkers in hepatotoxicity using metabolomics combined with ROC curves and SVMs. Toxicol. Sci. 2016;150:390–399. doi: 10.1093/toxsci/kfw001. [DOI] [PubMed] [Google Scholar]
- 32.Haddjeri N, Seletti B, Gilbert F, de Montigny C, Blier P. Effect of ergotamine on serotonin-mediated responses in the rodent and human brain. Neuropsychopharmacology. 1998;19:365–380. doi: 10.1016/S0893-133X(98)00038-4. [DOI] [PubMed] [Google Scholar]
- 33.Griffith RW, Grauwiler J, Hodel C, Leist KH, Matter B. Toxicological considerations. In: Berde B, Schild H, editors. Ergot Alkaloids and Related Compounds, Basic Pharmacological Properties. Springer; 1978. pp. 805–851. [Google Scholar]
- 34.Gröcer D, Floss HG. Biochemistry of ergot alkaloids - achievements and challenges. In: Cordell GA, editor. Alkaloids: Chemistry and Biology. Academic Press; 1978. pp. 171–218. [Google Scholar]
- 35.Panaccione DG, Schardl CL. Molecular genetics of ergot alkaloid biosynthesis. In: White JF Jr, Bacon CW, Hywel-Jones NL, Spatafora JW, editors. The Clavicipitalean Fungi: Evolutionary Biology, Chemistry, Biocontrol, and Cultural Impacts. CRC Press; 2003. pp. 399–424. [Google Scholar]
- 36.Pertz H, Eich E. Ergot alkaloids and their derivatives as ligands for serotoninergic, dopaminergic, and adrenergic receptors. In: Kren V, Cvak L, editors. Ergot: The Genus Claviceps. CRC Press; 1999. pp. 411–440. [Google Scholar]
- 37.Tudzynski P, Correia T, Keller U. Biotechnology and genetics of ergot alkaloids. Appl. Microbiol. Biotechnol. 2001;57:593–605. doi: 10.1007/s002530100801. [DOI] [PubMed] [Google Scholar]
- 38.Baggelaar MP, Maccarrone M, van der Stelt M. 2-Arachidonoylglycerol: A signaling lipid with manifold actions in the brain. Prog. Lipid Res. 2018;71:1–17. doi: 10.1016/j.plipres.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 39.Bluett RJ, et al. Endocannabinoid signalling modulates susceptibility to traumatic stress exposure. Nat. Commun. 2017 doi: 10.1038/ncomms14782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bhagavan NV. Endocrine metabolism III: adrenal glands. In: Bhagavan NV, editor. Medical Biochemistry. Academic Press; 2002. pp. 749–767. [Google Scholar]
- 41.Rogers DA, Mansberger JA. Gastrointestinal vascular ischemia caused by ergotamine. South. Med. J. 1989;82:1058–1059. doi: 10.1097/00007611-198908000-00034. [DOI] [PubMed] [Google Scholar]
- 42.Carpi A, Virno M. The action of ergotamine on the intracranial venous pressure and on the cerebral venous outflow of the dog. Br. J. Pharmacol. Chemother. 1957;12:232–239. doi: 10.1111/j.1476-5381.1957.tb00126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Badia A, Moron A, Cuffi L, Vila E. Effects of ergotamine on cardiovascular catecholamine receptors in the pithed rat. Gen. Pharmacol. 1988;19:475–481. doi: 10.1016/0306-3623(88)90051-1. [DOI] [PubMed] [Google Scholar]
- 44.Beart PM. Adrenaline The cryptic central catecholamine. Trends Neurosci. 1979;2:295–297. doi: 10.1016/0166-2236(79)90115-2. [DOI] [Google Scholar]
- 45.Tsai SH, Shih CJ, Lin MT. Effects of brain epinephrine depletion on thermoregulation, reflex bradycardia, and motor activity in rats. Exp. Neurol. 1985;87:428–438. doi: 10.1016/0014-4886(85)90173-6. [DOI] [PubMed] [Google Scholar]
- 46.Lane MD. Coenzyme A. In: Lennarz WJ, Lane MD, editors. Encyclopedia of Biological Chemistry. Academic Press; 2013. pp. 539–541. [Google Scholar]
- 47.Kohlmeier M. Pantothenate. In: Kohlmeier M, editor. Nutrient Metabolism. Academic Press; 2003. pp. 619–625. [Google Scholar]
- 48.Jessell, T. M., Siegelbaum, S. A. & Hudspeth, A. J. Principles of Neural Science, Vol. 5 (ed. Schwartz, J. H. & Kandel, E. R.) (McGraw-hill, 2012).
- 49.Van den Bergh F, Vincent MF, Jaeken J, Van den Berghe G. Residual adenylosuccinase activities in fibroblasts of adenylosuccinase-deficient children: Parallel deficiency with adenylosuccinate and succinyl-AICAR in profoundly retarded patients and non-parallel deficiency in a mildly retarded girl. J. Inherit. Metab. Dis. 1993;16:415–424. doi: 10.1007/BF00710291. [DOI] [PubMed] [Google Scholar]
- 50.Percie du Sert N, et al. The ARRIVE guidelines 2.0: Updated guidelines for reporting animal research. PLoS Biol. 2020;18:e3000410. doi: 10.1371/journal.pbio.3000410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Reddy P, et al. Tremorgenic effects and functional metabolomics analysis of lolitrem B and its biosynthetic intermediates. Sci. Rep. 2019;9:9364. doi: 10.1038/s41598-019-45170-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vassiliadis S, et al. A simple LC-MS method for the quantitation of alkaloids in endophyte-infected perennial ryegrass. Toxins. 2019 doi: 10.3390/toxins11110649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xia J, Sinelnikov IV, Han B, Wishart DS. MetaboAnalyst 3.0-making metabolomics more meaningful. Nucleic Acids Res. 2015;43:W251–W257. doi: 10.1093/nar/gkv380. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during the current study are available from the corresponding author on reasonable request.