Abstract
Background
Opioids are often used to treat pain after traumatic injury, but patient education on safe use of opioids is not standard. To address this gap, we created a video-based opioid education program for patients. We hypothesized that video viewing would lead to a decrease in overall opioid use and morphine equivalent doses (MEDs) on their penultimate hospital day. Our secondary aim was to study barriers to video implementation.
Methods
We performed a prospective pragmatic cluster randomized pilot study of video education for trauma floor patients. One of two equivalent trauma floors was selected as the intervention group; patients were equally likely to be admitted to either floor. Nursing staff were to show videos to English-speaking or Spanish-literate patients within one day of floor arrival, excluding patients with GCS < 15. Opioid use and MEDs taken on the day before discharge were compared. Intention to treat (ITT, intervention vs. control) and per-protocol groups (PP, video viewers vs. non-viewers) were compared, alpha=0.05. Protocol compliance was also assessed.
Results
In ITT analysis, there was no difference in percent of patients using opioids or MEDs on the day before discharge. In PP analysis, there was no different in percent of patients using opioids on the day before discharge. However, video-viewers still on opioids took significantly fewer MEDs than patients who did not see the video (26 vs 38, p<0.05). Protocol compliance was poor; only 46% of the intervention group saw the videos.
Conclusions
Video-based education did not reduce inpatient opioid consumption, although there may be benefits in specific subgroups. Implementation was hindered by staffing and workflow limitations, and staff bias may have limited the effect of randomization. We must continue to establish effective methods to educate patients about safe pain management and translate these into standard practices.
Level of Evidence:
Level IV, therapeutic
Keywords: Opioids, traumatic injury, video-based patient education, pain management
Introduction
In January 2019, the National Institute on Drug Abuse estimated that more that more than 130 people died every day by overdosing on opioids (1). Prescription opioid use is linked with opioid abuse – legitimately obtained prescriptions from health care providers are one of the three most common sources of opioids for nonmedical use (2) and three-quarters of recent heroin users were introduced to opioids through prescription drugs (3). Because of this, significant efforts have been made to reduce opioid use in the medical setting, with more than half of the states enacting laws limiting the prescribing of opioids for acute pain (4).
Unfortunately, after traumatic injury, patients have unavoidable pain, and opioids are often appropriately prescribed in conjunction with non-opioids as the first-line treatment for pain management. The incidence of post-hospitalization pain in trauma patients has been estimated as high as 97% (5). It is clear that adequate pain control is crucial to recovery, but it must be achieved in ways that minimize sustained opioid use. While clinicians are becoming more attuned to the importance of limiting opioids, patients must also become educated about the safe use of opioids. It is unknown whether structured education around safe use of opioids as well as safe storage and disposal would affect a patient’s narcotic use after traumatic injury.
In our trauma division, we have decisively moved to reduce opioids prescribed to injured patients to combat this epidemic and comply with our state’s acute pain prescribing limit (6). However, it remains unclear what clinicians can do to influence patients’ perception of pain and educate them on safe opioid use. We performed a pilot study of a short, video-based opioid education program for traumatically injured patients to determine the feasibility and effect of such a program on inpatient opioid use. We hypothesized that individuals who received the video intervention program would have significantly lower morphine equivalent doses (MEDs) compared to individuals who were not assigned to view the videos. Our second aim was to measure the feasibility of our video program by measuring compliance of video watching as well as reasons for noncompliance.
Methods
We performed a pragmatic prospective cluster randomized pilot study of opioid education videos for all trauma floor patients from January to April of 2019 at an urban academic Level 1 trauma center. One of two equivalent trauma-credentialed regular nursing floors (RNF) was selected to show the videos to all trauma patients within one day of floor admission. Patients were equally likely to be admitted to either floor, and were admitted to the RNF from the emergency department, operating room, or intensive care unit. Patients were excluded if they had died, had a Glasgow Coma Score (GCS) of less than 15 at the time of video inclusion, were not English-speaking or Spanish-literate, had a hospital length of stay (LOS) of less than 2 midnights, were on contact precautions, or were transferred to a non-trauma service at any point in the hospitalization.
Video Education Initiative
Two videos were created for this initiative. The first, entitled “Managing Your Pain,” is 6 minutes long and was designed to educate patients about expectations and management of pain and included testimony from trauma survivors as well as physician experts. The second video, entitled “Leaving the Hospital with a Narcotic Prescription,” is 3 minutes long, and was created to educate patients about leaving the hospital with an opioid prescription, including weaning, safe storage, and disposal of opioids. The content of the video scripts was reviewed by clinicians for medical accuracy and appropriateness. Funding to produce the videos was provided through a grant from the Best Practices in Pain Medication Use and Patient Engagement program run by the Cardinal Health Foundation’s Generation Rx program, which had no input on video content. Videos were produced by a local video production company and were subtitled in both English and Spanish. After review by our institution’s legal team, the videos were then uploaded to our institution’s YouTube channel (available at https://www.youtube.com/playlist?list=PL6lCc8oqoexnDIsuvO4RtyiWkWYUFeZM_).
Our institution has two regular nursing trauma floors which are adjacent to one another, staffed by one nursing team and the same secretarial staff. The same criteria are used to place patients on these floors, and patients are equally likely to be admitted to either floor, contingent upon bed availability. There is one supervisor for the nursing staff, and nurses float between the two floors so that trauma protocols and trauma care are uniformly provided to all floor patients.
Nursing and secretarial staff were educated about the project and the video content over the course of two weeks during twice-weekly staff meetings. The nursing and secretarial staff were asked to show the videos to eligible patients using the YouTube app on Apple iPads within one day of RNF arrival. Patients could refuse to watch the videos. Staff documented which patients had been offered the videos, who had agreed to watch them, and who had refused, to avoid showing the videos more than once to the same patient. Staff did not supervise the videos being watched. Logs of which patients agreed to watch the videos were kept in a locked room along with the iPads. After approximately 1 month of showing videos on one RNF, crossover was performed so that the floor that had shown videos previously stopped doing so and the floor that had not shown videos began to do so; the purpose of this crossover was to isolate the effect of these educational videos and minimize any potential bias based on the RNF to which a patient was admitted.
Data Collection
Patient clinical characteristics were extracted from our institutional trauma registry, including age, mechanism of injury, and injury severity score (ISS). Chart review was performed for study-specific information about medications and follow-up. Patient-stated “acceptable pain level” was recorded, as well as serum blood alcohol level and urine toxicology. Opioid medications and route were identified using patient medication administration record in the electronic medical record and included both oral, intravenous, and patient-controlled analgesia (PCA) opioids. All opioid doses were converted into Morphine Equivalent Doses (MEDs) and totaled for each hospital day.
The primary outcome of interest was opioid use on the day prior to discharge. For patients taking opioids, MEDs given on the day prior to discharge were compared between groups. Secondary outcomes included percentage of patients who were discharged with prescriptions for opioids or ancillary medications, and MEDs prescribed at discharge. All patient records were assessed for 30 days post-discharge to determine whether patients contacted trauma providers, consultants, emergency medicine teams, or other physicians for further pain-related prescriptions; late prescriptions and MEDs were also collected. Intention to treat (intervention vs. control) and per-protocol groups (videos vs. no videos) were compared. Assuming that the baseline MEDs would be 45 (equivalent to 30 mg of oxycodone, or 5 mg given q4h) and a standard deviation of 25, a sample size of approximately 44 patients per group would be needed to detect a 30% difference at an α=0.05 and power of 0.8. To assess the effect of time on discharge MEDs, we examined a Pearson correlation coefficient and simple linear regression between number of days between video watching and discharge MEDs, as well as an assessment of total length of stay to discharge MEDs.
To assess success of our intervention, protocol compliance was also assessed. Video education information was collected from the nursing and secretarial team weekly by the surgery research team. Need for staff education and staff changes were noted as part of identifying feasibility and implementation of this project.
Statistical analyses were performed using STATA/MP (version 16.1). Data are presented as median (interquartile range). Continuous variables were compared using Wilcoxon ranksum/Mann-Whitney U tests and categorical variables were compared using Chi-Square tests, with Fisher’s exact tests used for comparisons where the expected values would be less than 5. Analyses were performed in both intention-to-treat and per-protocol fashions. The MetroHealth Medical Center Institutional Review Board approved the study.
Results
During the study period, 483 patients were screened, with 198 patients meeting inclusion criteria (Figure 1). The most common reasons for exclusion were patients with short hospital stays, non-trauma patients on study RNFs (i.e. emergency general surgery patients), and trauma patients admitted to a non-study RNF. Of 198 patients eligible to view the video, 96 were assigned to view the videos, and 44 patients (46%) were ultimately given the videos for viewing.
Figure 1.
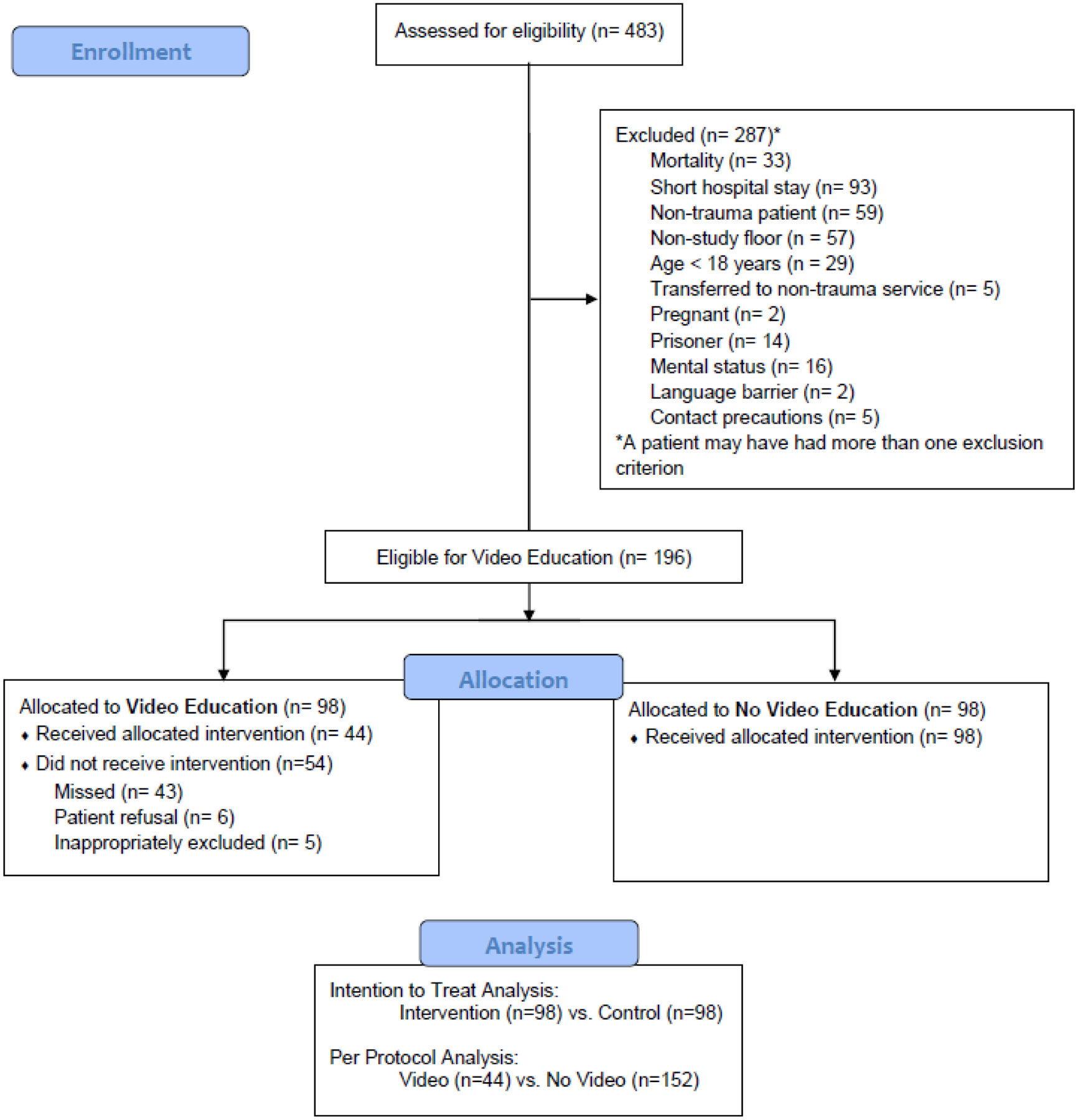
CONSORT flow diagram of study participants
Patients in the two groups were relatively balanced (Table 1), although patients in the intervention group were slightly younger (59 [37–72] vs. 69 [44–81], p=0.03) and were more likely to have had a penetrating mechanism (15 (15%) vs 5 (5%), p=0.02). More than half of patients were male (64%) and white (80%). Seventy-five (38%) of patients underwent an operation during their hospital admission, and 94 (48%) of patients were admitted to the ICU at any point during hospital admission. Fewer than 20% of participants had a urine toxicology performed and this data point was not analyzed.
Table 1:
Patient Demographics
| Factor | Total N=196 |
Intervention N=96 |
Control N=96 |
p-value |
|---|---|---|---|---|
| Patient Factor | ||||
| Age | 62 [43–77] | 59 [37–72] | 69 [44–81] | 0.03* |
| Male | 123 (63%) | 62 (63%) | 61 (52%) | 0.88 |
| White Race | 156 (80%) | 76 (78%) | 80 (82%) | 0.49 |
| Hospitalization Factors | ||||
| Penetrating Mechanism | 20 (10%) | 15 (15%) | 5 (5%) | 0.02* |
| ISS | 40 (20%) | 22 (22%) | 18 (17%) | 0.48 |
| Required Operative Intervention | 75 (38%) | 39 (40%) | 36 (37%) | 0.66 |
| First Hospital Day on Trauma Floor | 2 [1–4] | 2 [2–4] | 2 [1–4] | 0.69 |
| ICU Length of Stay | N=94 2 [1–4] |
N=47 2 [1–5] |
N=47 2 [1–4] |
0.97 |
| Total Length of Stay | 6 [4–9] | 5 [4–9] | 6 [4–9] | 0.98 |
| Study-Specific Risk Factors | ||||
| Self-Reported Acceptable Pain Level | 4 [0–5] | 4 [0–5] | 4 [1–5] | 0.57 |
| Blood Alcohol Level | 0 [0–9] | 0 [0–96] | 0 [0–7] | 0.18 |
| Discharge Disposition+ | 0.73 | |||
| Home | 93 (47%) | 50 (51%) | 43 (44%) | |
| Inpatient Rehabilitation | 32 (16%) | 15 (15%) | 17 (17%) | |
| Skilled Nursing | 66 (34%) | 30 (31%) | 36 (37%) | |
| Other | 5 (3%) | 3 (3%) | 2 (2%) |
ISS=Injury Severity Scale. ICU= Intensive Care Unit. Continuous data are presented as median [IQR], comparison via two-sample Wilcoxon Rank-sum/Mann-Whitney test with exact p-value. Categorical data are presented as n (%), comparison via Chi-square or Fisher’s exact test where noted (+)
Intention-to-Treat Analysis
In intention-to-treat analysis (Table 2), 96 patients in the intervention group were compared to 96 patients on the trauma floor where the videos were not offered. Injury severity, intensive care unit length of stay, hospital length of stay, self-reported accepted pain level, blood alcohol level, and discharge disposition were not significantly different between groups. On average, patients in both groups had their first day on a regular nursing floor on hospital day 2 (2 [2–4] vs. 2 [1–4], p=0.69). Groups were similar by gender, ISS, ICU LOS, and total LOS. The intervention group was slightly younger than the control group (59 [37–72] vs. 69 [44–81], p = 0.03) and more likely to have suffered a penetrating mechanism of injury (15% vs 5%, p = 0.02).
Table 2 –
Intention-to-Treat Analysis of Outcomes
| Outcome | Intervention N=96 |
Control N=96 |
p-value |
|---|---|---|---|
| Viewed Video | 44 (46%) | 0 (0%) | N/A |
| Medications on Day Prior to Discharge | |||
| Opioids | 68 (69%) | 58 (59%) | 0.14 |
| Patient-Controlled Analgesia or Epidural+ | 1 (1%) | 2 (2%) | 0.5 |
| Morphine Equivalent Doses, mg | 35 [15–61] | 38 [15–75] | 0.76 |
| Ancillary Medication | 97 (99%) | 98 (100%) | 0.32 |
| Pain Level on Day Prior to Discharge | |||
| Maximum Documented Pain Level | 8 [5–9] | 7 [4–9] | 0.39 |
| Minimum (not Asleep) Documented Pain Level | 3 [0–5] | 2 [0–5] | 0.12 |
| Medications at Discharge | |||
| Opioids | 57 (58%) | 54 (55%) | 0.67 |
| Morphine Equivalent Doses, mg | 210 [150–225] | 210 [140–210] | 0.20 |
| Ancillary Medication | 71 (72%) | 80 (82%) | 0.13 |
| After Discharge Prescriptions (n=183) | |||
| Opioids | 9/90 (10%) | 10/93 (11%) | 0.87 |
| Morphine Equivalent Doses, mg | 113 [90–210] | 210 [140–420] | 0.23 |
Continuous data are presented as median [IQR], comparison via two-sample Wilcoxon Rank-sum/Mann-Whitney test with exact p-value. Categorical data are presented as n (%), comparison via Chi-square or Fisher’s exact test where noted (+)
Outcome comparisons between groups are presented in Table 2. There was no difference in MEDs consumed on the day before discharge (17.5 vs 15, p = 0.446), the percentage of patients who received an opioid prescription at time of discharge (60.0% vs. 57.1%, p = 0.759), or MEDS prescribed at discharge (210 vs 210, p = 0.264). There was also no difference in patients who received additional opioid prescriptions after discharge. Among patients eligible for video viewing, those who were given the video were significantly younger (54 [33–71] vs 63 [52–73], p=0.03).
Per Protocol Analysis
In per-protocol analysis (Table 3), 44 patients who viewed the videos were compared to 152 patients who did not view the videos. There were no statistical differences between video viewers and non-viewers with regards to age, gender , race , first hospital day on a regular floor, need for operation, ICU LOS, total LOS, self-reported acceptable pain level, blood alcohol level, or discharge disposition (all p>0.05). Significantly more patients who had a penetrating mechanism (8 (18%) vs. 12 (8%), p=0.049) viewed the video, and patients who viewed the video had a lower ISS (10 [5–14] vs. 16 [9–17], p=0.01).
Table 3 –
Per-Protocol Analysis
| Outcome | Saw Video N=44 |
No Video N=96 |
p-value |
|---|---|---|---|
| Medications on Day Prior to Discharge | |||
| Opioids | 28 (64%) | 98 (64%) | 0.92 |
| Patient-Controlled Analgesia or Epidural+ | 1 (2%) | 2 (1%) | 0.54 |
| Morphine Equivalent Doses, mg | 26 [15–45] | 38 [15–75] | 0.04 * |
| Ancillary Medication | 44 (100%) | 151 (99%) | 0.59 |
| Pain Level on Day Prior to Discharge | |||
| Maximum Documented Pain Level | 7 [4–8] | 8 [5–9] | 0.14 |
| Minimum (not Asleep) Documented Pain Level | 3 [0–4] | 3 [0–5] | 0.86 |
| Medications at Discharge | |||
| Opioids | 28 (64%) | 83 (55%) | 0.29 |
| Morphine Equivalent Doses, mg | 210 [165–218] | 210 [135–210] | 0.15 |
| Ancillary Medication | 32 (73%) | 119 (78%) | 0.44 |
| After Discharge Prescriptions (n=183) | |||
| Opioids | 5/41 (12%) | 14/142 (10%) | 0.67 |
| Morphine Equivalent Doses, mg | 113 [90–140] | 210 [100–420] | 0.26 |
Continuous data are presented as median [IQR], comparison via two-sample Wilcoxon Rank-sum/Mann-Whitney test with exact p-value. Categorical data are presented as n (%), comparison via Chi-square or Fisher’s exact test where noted (+)
Outcome comparisons are presented in Table 3. There was no statistically significant difference in percent of individuals who took opioids on the day before discharge, but patients who watched the videos who consumed opioids on the day before discharge took significantly fewer MEDs (26 [15–45] vs. 38 [15–75], p=0.04). There were no differences in the percentage who received an opioid prescription at time of discharge, MEDs prescribed at discharge, opioids prescribed after discharge, or MEDs given after discharge.
Timing of Video and Discharge MEDs
The median number of days between video watching and discharge was 2 [IQR 1–4, range 0–21]. The Pearson correlation coefficient between number of days between video and discharge and the MEDs taken on the day prior to discharge was −0.4, suggesting a weak negative correlation; in other words, the MEDs taken in the hospital decreased slightly for patients who stayed longer on the floor. In unadjusted linear regression, each additional day on the floor post-video was associated with a 2 mg decrease in MEDs on the day prior to discharge (beta-coefficient −2.0, 95% CI −3.8 to −0.2, p-value=0.03). To test whether the decrease in MEDs was simply an effect of a longer hospitalization, we also examined corresponding Pearson’s correlation coefficients and regressions for non-video watchers, examining the relationship between regular nursing floor length of stay and the MEDs on the day prior to discharge. For non-video watchers, the number of days on the floor was 3 [1–5]; correlation between floor length of stay was 0.13, suggesting no correlation. In unadjusted linear regression, number of days on the floor was not associated with a change in MEDs on the day prior to discharge (beta-coefficient 1.7, 95% CI −0.9 to 4.3, p-value=0.2).
Implementation and Feasibility
Over the course of two weeks, four staff education sessions were held to share the aims of the study and protocols with the nursing and secretarial staff. Sessions were held at different times of day to ensure capture of staff working different shifts. Trauma staff, the research team, nursing leadership, nurses, and secretaries were involved in the planning of the project to help with adequate implementation. During the study period, the two floors went from two unit secretaries to one, who was largely in charge of identifying eligible patients and bringing the iPads to each room. Of the 49 patients who were supposed to view the videos but did not, 6 were due to patient refusal and 5 eligible patients were recorded in the log as ineligible by nursing staff. Three of these reasons for ineligibility included that it was “too late” with no further explanation, that the patient was asleep, and that there were too many family members in the room. The reasons for inappropriate exclusion were not recorded for the other two patients. The remaining patients did not have a documented reason for not viewing the videos. Compliance decreased over time, specifically decreasing after the video intervention crossed over to the second unit.
Discussion
As the scope of opioid crisis in the United States has grown, the urgent need to develop strategies to combat this scourge has become apparent. In the last decade there has been a trend away from criminal justice approaches with an increase in plans involving treatment, harm reduction, and prevention (7). Since there is a dose-dependent effect between opioid use and the incidence of long-term harm (8), many prevention strategies have focused on reducing the amount of opioids that clinicians provide to patients. However, approaches that attempt to reduce the amount of opioids patients take to treat their pain are not well-described. Here we demonstrate that a short video-based opioid education intervention was not associated with decreased opioid use in an intention-to-treat analysis. We continue to believe that this intervention may be promising, as there was a small subset of patients who had lower opioid use. We also found that patients who watched the video and stayed in the hospital longer used fewer opioids by the time they were discharged; for patients who did not watch the video, opioid use was not lower for patients who stayed in the hospital longer. We also demonstrate that implementation of a new video education program can be challenging, as only 45% of eligible patients saw the videos. Pain, once considered the “fifth vital sign,” is difficult to treat. Although pain can be psychologically distressing, the perception of pain in response to injury is highly individualized and is influenced by the extent of injury, genetics, ethnicity, and socioeconomics (9–12). There is evidence that educational attainment and health literacy also affect the experience of pain (13, 14). Despite multidimensional causes that lead to the experience of pain, opioids have long been the first-line treatment for acute pain after trauma. Indeed, opioids are often a necessary adjunct to allow patients to cope with the acute traumatic injury. However, it is known that there are non-physical attributes that lead to opioid use. Patients who have more psychological distress, “catastrophic thinking,” and less effective coping strategies are more likely to take opioids in the long-term (15). In order to combat the opioid epidemic and allow physicians to prescribe fewer opioids without leading to patient distress, a multimodal approach to pain control must be developed.
Video-based education has been demonstrated to improve patients’ knowledge and self-efficacy (16). It has also been shown to serve as a source of effective role-modeling in well-defined, self-limited situations; to decrease anxiety, pain, and sympathetic arousal; and to improve coping ability (17). Watching videos online is also a familiar and non-intimidating medium for most patients to use and does not require a minimum reading level. Our videos sought to capitalize on these strengths by featuring clinicians who shared medical information about opioids and trauma survivors who related their experiences with pain and pain management after injury. Education can also be a powerful tool for patients with either acute post-surgical or chronic pain and has been shown to decrease opioid use and improve knowledge about opioids and safe storage practices (18–20). Peer mentors have also been shown to help patients with a variety of domains of recovery including increasing self-efficacy and decreasing rehospitalizations (21), as peer mentors can serve as a “trusted and credible source of hope and support” (22). We hoped that viewing the videos would help patients develop realistic expectations about pain after traumatic injury and also to learn about safe use of pain medications after discharge. We hypothesized that once life-threatening problems and urgent surgical issues had been addressed, the use of this educational tool would result in patients using less opioids while in the hospital. The intervention was also meant to be minimally disruptive to nursing and secretarial staff’s pre-existing workflow. Trauma patients are an extremely heterogeneous group, with wide variation in age, injury mechanisms, pain level, and hospital courses. Our clustered crossover study was designed to equalize the risk of being in the “intervention” group, to decrease the likelihood of bias related to the intervention. Patients are placed in any available bed on either floor; clinical factors do not dictate placement into a bed or a room. The six patients who refused the video ranged in age from 22 to 86; we did not see evidence that age was a barrier to video viewing. Despite these efforts, the intervention and control groups were not perfectly balanced. In addition, compliance with offering the videos was poor; our analysis also suggests that there was some provider bias in administering the video to eligible patients which affected intervention rates. Penetrating trauma patients, younger patients, and those with lower injury severity scores were given the videos to watch more often, which suggests that the nursing and secretarial staff may have found it easier to remember to administer the video to patients who fit a specific risk profile. These differences in groups may have contributed to our findings.
Despite the multidisciplinary planning phase of this intervention, workflow issues on our floor limited protocol compliance. Nurses and secretarial staff floated between the two RNFs but because we only had two iPads, we were only showing the videos on one of the units at any given time – this made it difficult for the staff to remember if they were to show the videos to their patients on that day they were working. Staff also reported challenges keeping track of where the iPads were to prevent theft or loss of the devices, ensuring that the iPads were charged, and consistently documenting which patients had been offered the videos. In order to intervene before patients had become habituated to opioid use, we attempted to show the videos within 24 hours of admission to the floor. This short time frame likely limited our ability to be compliant. Attempting to isolate the effect of the video through crossover, we changed the RNF that was assigned to show videos to patients, which additionally increased the distance between the RNF and the iPad storage location. This coincided with seasonal increase in trauma volume, likely creating a situation in which busy staff were more likely to forget to show the videos to patients or simply did not have time to do so. Our study also identified a gap in knowledge and practice in regards to opioid prescribing. With or without the videos, the median opioid prescription was 210 MEDs, which is equal to 28 tablets of 5 mg of oxycodone. Of note, this dose is equal to the state limit for acute opioid prescriptions in the state of Ohio.
In conclusion, our study on video education for opioids was unable to show a decrease in inpatient opioid use, but compliance was poor likely due to implementation issues. Our primary outcome was opioid use on the patient’s last full inpatient day; many patients were not taking opioids by this time. For patients who were still taking opioids prior to discharge, MEDs taken on the day before discharge was lower in patients who had seen the videos. Also, we saw some evidence that patients who viewed the videos tapered their MEDs over time compared with patients who did not view the videos. We continue to believe that video education may be a useful tool for patients. Our study also highlights that clinician education at multiple points is not only important but is an essential part of a successful program, from the secretarial staff to nursing to prescribers such as physician assistants, residents, and attending physicians. More work is necessary to determine the ideal patient population, timing of video viewing, and improve implementation to evaluate potential effects on both opioid use and the overall patient experience of pain and recovery.
Acknowledgements
We thank the manager of our trauma regular nursing floor, April Largent, RN, and the staff of 7B and 7C for their assistance with this project and their dedication to the care of our trauma patients.
Conflicts of Interest and Sources of Funding:
VPH is supported by the Case Western Reserve University/Cleveland Clinic Clinical and Translational Science Award through the KL2 TR002547. There are no other potential conflicts of interest.
The creation of the videos in this project were funded by a grant from the Cardinal Health Foundation Generation Rx’s Best Practices in Pain Medication Use and Patient Engagement program.
This publication was made possible by the Clinical and Translational Science Collaborative of Cleveland, KL2 TR002547 from the National Center for Advancing Translational Sciences component of the National Institutes of Health and NIH roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
This abstract was presented as a QuickShot at the 33rd EAST Annual Scientific Assembly, January 14–18, 2020 in Orlando, Florida.
References
- 1.Opioid Overdose Crisis | National Institute on Drug Abuse (NIDA) https://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis#one [November 12, 2019].
- 2.Lankenau SE, Teti M, Silva K, Jackson Bloom J, Harocopos A, Treese M. Initiation into prescription opioid misuse amongst young injection drug users. Int J Drug Policy. 2012;23(1):37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71(7):821–6. [DOI] [PubMed] [Google Scholar]
- 4.Davis CS, Lieberman AJ, Hernandez-Delgado H, Suba C. Laws limiting the prescribing or dispensing of opioids for acute pain in the United States: A national systematic legal review. Drug Alcohol Depend. 2019;194:166–72. [DOI] [PubMed] [Google Scholar]
- 5.Archer KR, Castillo RC, Wegener ST, Abraham CM, Obremskey WT. Pain and satisfaction in hospitalized trauma patients: the importance of self-efficacy and psychological distress. J Trauma Acute Care Surg. 2012;72(4):1068–77. [DOI] [PubMed] [Google Scholar]
- 6.Zolin SJ, Ho VP, Young BT, Harvey AR, Beel KT, Tseng ES, Brown LR, Claridge JA. Opioid prescribing in minimally injured trauma patients: Effect of a state prescribing limit. Surgery. 2019;166(4):593–600. [DOI] [PubMed] [Google Scholar]
- 7.McGinty EE, Stone EM, Kennedy-Hendricks A, Sanders K, Beacham A, Barry CL. U.S. news media coverage of solutions to the opioid crisis, 2013–2017. Prev Med. 2019;126:105771. [DOI] [PubMed] [Google Scholar]
- 8.Dunn KM, Saunders KW, Rutter CM, Banta-Green CJ, Merrill JO, Sullivan MD, Weisner CM, Silverberg MJ, Campbell CI, Psaty BM, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fillingim RB. Individual differences in pain responses. Curr Rheumatol Rep. 2005;7(5):342–7. [DOI] [PubMed] [Google Scholar]
- 10.Edwards RR. Genetic predictors of acute and chronic pain. Curr Rheumatol Rep. 2006;8(6):411–7. [DOI] [PubMed] [Google Scholar]
- 11.Rahim-Williams FB, Riley JL 3rd, Herrera D, Campbell CM, Hastie BA, Fillingim RB. Ethnic identity predicts experimental pain sensitivity in African Americans and Hispanics. Pain. 2007;129(1–2):177–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stanaway FF, Blyth FM, Cumming RG, Naganathan V, Handelsman DJ, Waite LM, Sambrook PN, Creasey HM, Seibel MJ, Le Couteur DG. Back pain in older male Italian-born immigrants in Australia: the importance of socioeconomic factors. Eur J Pain. 2011;15(1):70–6. [DOI] [PubMed] [Google Scholar]
- 13.Lanitis S, Mimigianni C, Raptis D, Sourtse G, Sgourakis G, Karaliotas C. The Impact of Educational Status on the Postoperative Perception of Pain. Korean J Pain. 2015;28(4):265–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koppen PJ, Dorner TE, Stein KV, Simon J, Crevenna R. Health literacy, pain intensity and pain perception in patients with chronic pain. Wien Klin Wochenschr. 2018;130(1–2):23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Helmerhorst GT, Vranceanu AM, Vrahas M, Smith M, Ring D. Risk factors for continued opioid use one to two months after surgery for musculoskeletal trauma. J Bone Joint Surg Am. 2014;96(6):495–9. [DOI] [PubMed] [Google Scholar]
- 16.Denny MC, Vahidy F, Vu KY, Sharrief AZ, Savitz SI. Video-based educational intervention associated with improved stroke literacy, self-efficacy, and patient satisfaction. PLoS One. 2017;12(3):e0171952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gagliano ME. A literature review on the efficacy of video in patient education. J Med Educ. 1988;63(10):785–92. [DOI] [PubMed] [Google Scholar]
- 18.Yajnik M, Hill JN, Hunter OO, Howard SK, Kim TE, Harrison TK, Mariano ER. Patient education and engagement in postoperative pain management decreases opioid use following knee replacement surgery. Patient Educ Couns. 2019;102(2):383–7. [DOI] [PubMed] [Google Scholar]
- 19.Chakravarthy B, Somasundaram S, Mogi J, Burns R, Hoonpongsimanont W, Wiechmann W, Lotfipour S. Randomized pilot trial measuring knowledge acquisition of opioid education in emergency department patients using a novel media platform. Subst Abus. 2018;39(1):27–31. [DOI] [PubMed] [Google Scholar]
- 20.de la Cruz M, Reddy A, Balankari V, Epner M, Frisbee-Hume S, Wu J, Liu D, Yennuraialingam S, Cantu H, Williams J, et al. The Impact of an Educational Program on Patient Practices for Safe Use, Storage, and Disposal of Opioids at a Comprehensive Cancer Center. Oncologist. 2017;22(1):115–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gassaway J, Jones ML, Sweatman WM, Hong M, Anziano P, DeVault K. Effects of Peer Mentoring on Self-Efficacy and Hospital Readmission After Inpatient Rehabilitation of Individuals With Spinal Cord Injury: A Randomized Controlled Trial. Arch Phys Med Rehabil. 2017;98(8):1526–34 e2. [DOI] [PubMed] [Google Scholar]
- 22.Kersten P, Cummins C, Kayes N, Babbage D, Elder H, Foster A, Weatherall M, Siegert RJ, Smith G, McPherson K. Making sense of recovery after traumatic brain injury through a peer mentoring intervention: a qualitative exploration. BMJ Open. 2018;8(10):e020672. [DOI] [PMC free article] [PubMed] [Google Scholar]


