Abstract
Background
The COVID-19 pandemic has witnessed a reduction in asthma exacerbations across the United Kingdom. Several factors may underpin this, including reduced transmission of seasonal viruses and improved adherence to inhaled corticosteroids (ICS). However, little is known about how ICS use has changed during the pandemic.
Objective
To identify prescribing patterns for asthmatics during the pandemic.
Methods
Using the OpenPrescribing database, we retrospectively analyzed prescribing patterns of ICS, salbutamol and peak flow meters from January 2019 to January 2021 across England. In addition, using a sample asthma cohort at 3 primary care practices in London, we assessed individual prescription patterns.
Results
A sharp increase in national ICS prescriptions occurred in March 2020 representing a 49.9% increase compared with February 2020. The sample cohort included 1132 patients (762 ICS treated across both years). Overall ICS adherence improved in 2020 (P < .001), with the proportion of patients meeting “good adherence” (≥75%) increasing from 33.9% to 42.0% (P < .001). The March 2020 spike predominantly reflected improved adherence rather than a hoarding effect of multiple inhalers. Female gender and increasing age were associated with the most significant improvements in adherence. A similar spike in salbutamol occurred in March 2020; however, an overall reduction in salbutamol prescriptions occurred in 2020 (P = .039). National figures highlighted a progressive increase in prescription of peak flow meters over 2020.
Conclusion
ICS adherence rates remain low; however, a modest improvement in adherence was observed during the first year of the COVID-19 pandemic. Salbutamol prescription rates reduced over the same time period, whereas prescriptions for peak flow meters have steadily increased.
Key words: COVID-19, Asthma, Inhaler devices, Adherence
Abbreviations used: COPD, Chronic obstructive pulmonary disease; GINA, Global Initiative for Asthma; ICS, Inhaled corticosteroids; OCS, Oral corticosteroids; PAAP, Personalized asthma action plan; SD, Standard deviation
What is already known about this topic? A reduction in asthma exacerbations has been recorded over the COVID-19 pandemic. It is unknown whether there was a change in medication use over the first year of the pandemic compared with the previous year.
What does this article add to our knowledge? The COVID-19 pandemic has witnessed an improvement in adherence to inhaled corticosteroids (ICS), a reduction in salbutamol use, and an increase in prescription of peak flow meters for home monitoring compared with the previous year.
How does this study impact management guidelines? Ongoing efforts to improve ICS adherence, reduce reliance on salbutamol, and use peak flow meters for remote monitoring and self-management of asthma are needed.
The World Health Organization declared COVID-19 a global pandemic on March 11, 2020, and over 100 million cases had been reported by March 2021.1 It is well documented that people with asthma are at risk of exacerbation with seasonal respiratory tract viruses.2 , 3 However, over the pandemic, a reduction in asthma exacerbations has been reported.4 , 5 Possible explanations include reduced transmission of other respiratory viruses through hand washing and mask wearing, a change in prescribing patterns of asthma medications, or a change in patient behavior with improved adherence to inhaled corticosteroids (ICS).
Data remain somewhat conflicted on whether asthma is a risk factor for worse outcomes with COVID-19.6 , 7 Early in the pandemic, the Center for Disease Control and Prevention8 and the Global Initiative for Asthma (GINA)9 recommended that patients continue their ICS to reduce the theoretical risk of an exacerbation with COVID-19. However, poor adherence to ICS is well recognized with rates frequently recorded at <25%.10 Reasons include both intentional (eg, due to economic cost) and unintentional factors (eg, forgetfulness).11
In March 2020, a surge in all prescription medication was seen in England.12 In the United States, an increase in controller medication use for patients with airways disease was reported in the last week of March 2020.13 It remains unknown whether this pattern of behavior may have persisted beyond this early phase of the pandemic. We therefore investigated whether there was evidence of a persistent change in prescribing of asthma therapies beyond the first wave of the pandemic.
Using the UK National database, OpenPrescribing,12 we compare prescribing patterns of ICS and salbutamol in 2019 with rates across the first year of the pandemic. In addition, we report prescribing patterns of a sample asthma cohort to identify any demographic characteristics associated with differential changes in behavior.
Methods
Monthly data for all ICS, salbutamol inhalers, and peak-flow meters from January 1, 2019, to January 1, 2021, were extracted from OpenPrescribing.12 However, as neither the indication (eg, asthma vs chronic obstructive pulmonary disease [COPD]) nor differentiation by strength is accessible, a sample asthma cohort was generated of all patients with asthma registered at 3 primary care practices in London, United Kingdom, to explore the driver(s) for any change in prescription rate. All data were anonymized and included demographic (gender, age, and ethnicity) and individual ICS and salbutamol prescription data. Local Caldicott Guardian ethical approval was granted for data collection by GSTT NHSFT (approval number 11434).
Prescription records were used as a surrogate measure of adherence to ICS. The ICS medication possession ratio was calculated as the number of doses of ICS issued/expected for each patient and is reported in a continuous and categorical manner. Adherence has been defined as good (≥75%), suboptimal (50%-74%), poor (25%-49%), and nonadherence (<25%).14 , 15 Salbutamol use was reported as the total number of salbutamol inhalers issued for each patient. The treatment step at the time of review was defined according to GINA 2020.9
Data were analyzed using SPSS (v26; IBM, Chicago, Ill) and figures generated using Graphpad Prism (v8). Kolmogorov-Smirnov tests were used to analyze data distribution. Results are given as mean (standard deviation [SD]) if normally distributed or median (interquartile range) if nonparametric. Parametric variables were compared using t tests (paired or independent) and nonparametric variables using the Mann-Whitney U test (unrelated) or the Wilcoxon signed rank test (related). Parametric and nonparametric analysis of variance was performed for analysis of 3 or more groups. Categorical variables were analyzed by the χ2 test or the Fisher exact test. For nonparametric testing, differences are represented by test statistic, z, and considered significant at P < .05. All P values are 2-sided.
Results
Prescribing of inhaled corticosteroids
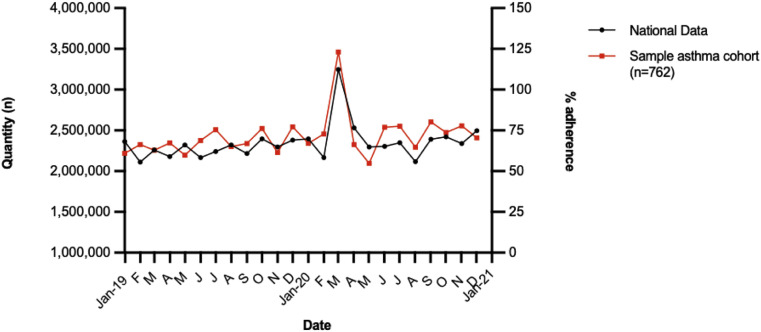
In 2019, the mean (SD) number of monthly ICS prescriptions in England was 2,270,869 (91,057), increasing by 6.6% to 2,421,130 (286,101) in 2020 (P = .11). A sharp increase to 3,247,030 was observed in March 2020, representing a 49.9% increase compared with February 2020 (2,166,316) and a 43.8% increase compared with March 2019 (2,110,503), after which rates of ICS prescribing appear to return to normal levels (Figure 1 ).
Figure 1.
National prescribing of inhaled corticosteroids (ICS) in England (left axis) and ICS adherence rate of the sample asthma cohort (right axis).
Demographic and clinical characteristics of the sample asthma cohort
A total of 1132 patients with a diagnosis of asthma were identified across the 3 general practices (combined list size of 24,633 patients). The mean age was 39.9 (18.0) years. A total of 762 (67.3%) were prescribed GINA step 2-5 treatment with an ICS ± additional controller medication(s) across both 2019 and 2020 allowing comparisons of usage before and during the pandemic. An additional 120 (10.6%) patients were newly initiated on ICS in 2020. The remaining 250 patients (22.1%) were treated with salbutamol alone across the 2-year period of study (Table I ).
Table I.
Baseline demographic and clinical characteristics of the sample asthma cohort (n = 1132)
| Characteristic | Value |
|---|---|
| Age (y), mean ± SD | 39.9 ± 18.0 |
| Sex, n (%) | |
| Female | 630 (55.7) |
| Age groups (y), n (%) | |
| 5-17 | 103 (9.1) |
| 18-39 | 545 (48.1) |
| 40-64 | 360 (31.8) |
| ≥65 | 124 (11.0) |
| Ethnicity, n (%) | |
| White | 641 (56.6) |
| Black | 267 (23.6) |
| Asian | 137 (12.1) |
| Not specified | 87 (7.7) |
| GINA step, n (%) | |
| Salbutamol only | 250 (22.1) |
| Step 2 | 498 (44.0) |
| Step 3 | 150 (13.2) |
| Step 4 | 184 (16.3) |
| Step 5 | 50 (4.4) |
| Smoking status, n (%) | |
| Never smoker | 824 (72.8) |
| Current smoker | 149 (13.2) |
| Previous smoker | 159 (14.0) |
GINA, Global Initiative for Asthma; ICS, inhaled corticosteroid; LABA, long-acting β-agonist; SD, standard deviation.
Salbutamol only: patients prescribed salbutamol only since 2017; Step 2: daily low-dose ICS; Step 3: low-dose ICS/LABA or medium-dose ICS; Step 4: medium-dose ICS/LABA or high-dose ICS; Step 5: high-dose ICS/LABA.
Patterns of adherence to ICS
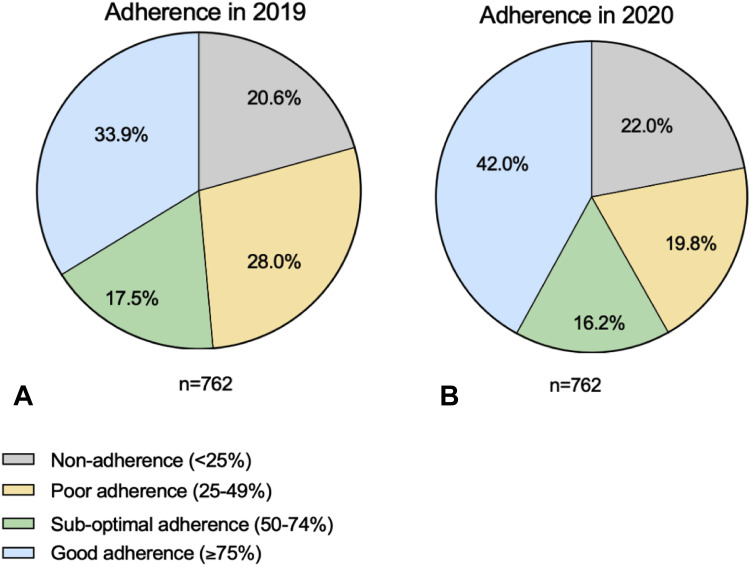
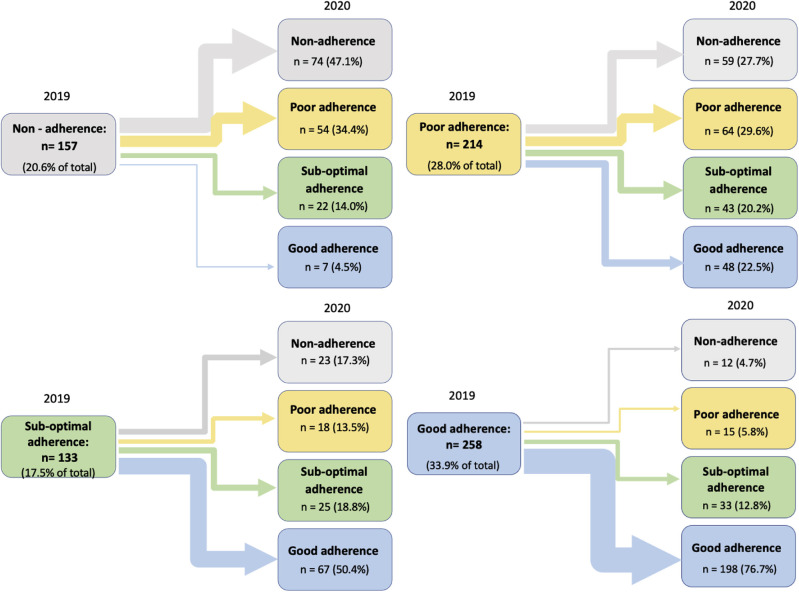
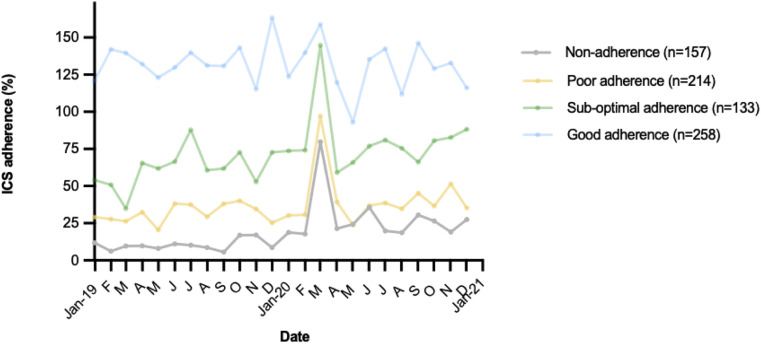
The median levels of ICS adherence was 54.8% (27.4%-95.9%) in 2019 and 54.8% (27.4%-106.8%) in 2020. Despite an identical median value, this difference was statistically significant highlighting an increase in 2020 (P < .001). More specifically, the proportion of patients who met the ≥75% threshold for “good adherence” increased from 33.9% to 42% in 2020 (P < .001), whereas the proportion of patients with <50% ICS adherence reduced from 48.6% to 41.8% in 2020 (P < .001) (Figure 2 ). Overall, adherence levels increased for 31.6%, decreased for 21.0%, and remained consistent for 47.4% patients (Figure 3 ), particularly for those with good adherence preceding the onset of the pandemic in 2019 (Figure 4 ).
Figure 2.
Overall levels of adherence to inhaled corticosteroids in (A) 2019 and (B) 2020.
Figure 3.
Change in level of adherence to inhaled corticosteroids from 2019 to 2020. The size of the arrow relates to the relative change from 2019 to 2020.
Figure 4.
Patterns of adherence to inhaled corticosteroids (ICS) in the sample asthma cohort according to the adherence level in 2019.
Relationship between patient characteristics and ICS adherence
Gender
Levels of ICS adherence were similar between females and males in 2019 with a median of 52.1% and 54.8%, respectively (P = .54). In 2020, a small but significant increase to 54.8% in adherence rate was observed for females only (P < .001), equaling adherence levels with males in 2020 (Table II ).
Table II.
Adherence to inhaled corticosteroids in 2019 to 2020 according to baseline demographic and clinical characteristics
| Characteristic | n | 2019 (n = 762) | 2020 (n = 762) | z | P value∗ |
|---|---|---|---|---|---|
| Overall adherence to ICS | 54.8 (27.4-95.9) | 54.8 (27.4-106.8) | 3.923 | <.001 | |
| Sex | |||||
| Female | 428 | 52.1 (27.4-95.9) | 54.8 (27.4-108.9) | 3.834 | <.001 |
| Male | 334 | 54.8 (27.4-92.5) | 54.8 (27.4-98.6) | 1.597 | .110 |
| Age | |||||
| 5-17 | 64 | 41.1 (16.4-78.8) | 41.1 (16.4-82.2) | 0.201 | .841 |
| 18-39 | 322 | 32.9 (16.4-65.8) | 42.5 (13.7-82.2) | 2.365 | .018 |
| 40-64 | 267 | 65.8 (32.9-98.6) | 76.7 (32.9-109.6) | 2.580 | .010 |
| ≥65 | 109 | 82.2 (42.5-109.6) | 93.2 (49.2-134.2) | 1.964 | .05 |
| Ethnicity | |||||
| White | 421 | 54.8 (27.4-98.6) | 54.8 (27.4-98.6) | 2.203 | .028 |
| Black | 200 | 54.7 (27.4-98.6) | 67.1 (27.4-109.6) | 3.013 | .003 |
| Asian | 89 | 41.1 (16.4-82.2) | 54.8 (16.4-95.9) | 1.262 | .207 |
| Not specified | 52 | 45.2 (17.8-78.8) | 42.5 (14.4-94.5) | 1.140 | .254 |
| GINA treatment step | |||||
| Salbutamol only | – | – | – | – | – |
| Step 2 | 416 | 41.1 (27.4-82.2) | 54.8 (13.7-100.7) | 1.777 | .075 |
| Step 3 | 131 | 54.8 (27.4-98.6) | 71.2 (32.9-109.6) | 2.655 | .008 |
| Step 4 | 168 | 62.3 (32.9-98.6) | 75.3 (32.9-106.8) | 2.568 | .010 |
| Step 5 | 47 | 65.8 (32.9-98.6) | 74.0 (49.3-98.6) | 1.307 | .191 |
| Smoking status | |||||
| Never smoker | 543 | 49.3 (27.4-82.2) | 54.8 (27.4-98.6) | 3.709 | <.001 |
| Current smoker | 102 | 54.8 (27.4-98.6) | 61.6 (15.8-98.6) | 0.621 | .535 |
| Previous smoker | 117 | 65.8 (27.4-109.6) | 82.2 (30.1-109.6) | 1.259 | .208 |
GINA, Global Initiative for Asthma; ICS, inhaled corticosteroids.
Data presented as number (n) and median (interquartile range).
Wilcoxon signed rank test.
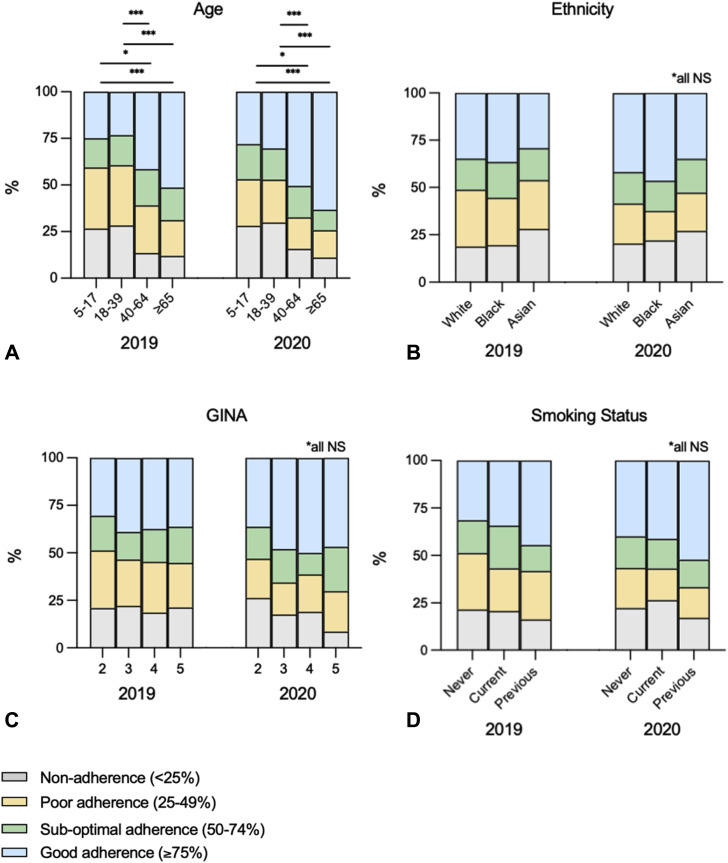
Age
Increasing age was associated with improved levels of ICS adherence in both 2019 and 2020. Compared with 2019, significant improvements in adherence were observed for patients aged 18-64 (all P < .05) with a strong trend in the ≥65 age group (P = .05), a subgroup who already demonstrated high levels of adherence in 2019 of 82.2%. In contrast, adherence in the 5-17 age group was low at 41.1% (16.4%-78.8%) in 2019 and failed to improve in 2020 (Table II; Figure E1, A, available in this article's Online Repository at www.jaci-inpractice.org).
Figure E1.
Levels of adherence to inhaled corticosteroids. Adherence is categorized as “nonadherence,” “poor,” “suboptimal,” and “good” and is shown for the asthma cohort in 2019 and 2020 according to (A) age, (B) ethnicity, (C) GINA treatment step, and (D) smoking status. GINA, Global Initiative for Asthma.
Ethnicity
Adherence rates were similar across the reported ethnicities in 2019 and 2020. An improvement in adherence in 2020 was observed in White (P = .028) and Black (P = .003) patients, but not in Asian patients; however, the size of the Asian subgroup was smaller than either the White or Black subgroups (Table II; Figure E1, B, available in this article's Online Repository at www.jaci-inpractice.org).
Treatment step
Adherence rates were similar comparing GINA treatment steps in 2019 and 2020. However, significant improvements in adherence during the pandemic were only evident for patients receiving step 3 (54.8%-71.2%, P = .008) and step 4 (62.3%-75.3%, P = .01) treatment (Table II; Figure E1, C, available in this article's Online Repository at www.jaci-inpractice.org).
Smoking status
Adherence rates were similar across categories of smoking status, with improvements in adherence in 2020 observed for never-smokers only (49.3%-54.8%, P < .001). However, this was by far the largest group (71.3% of the cohort), and numerically large albeit nonsignificant improvements were also seen in previous smokers (65.8%-82.2%, P = .208) (Table II; Figure E1, D, available in this article's Online Repository at www.jaci-inpractice.org).
Prescribing of ICS during March 2020
In March 2020, 391 of 882 (44.3%) patients received an ICS prescription (882 includes all patients receiving an ICS in 2019 and 2020, including 120 steroid-naïve patients), a figure twice the 195 patients in March 2019. This included 41 patients who received ICS for the first time in March 2020. Analysis of individual ICS prescriptions highlighted that 112 of 391 (28.6%) were issued the March 2020 ICS before their previous ICS prescription was due to run out. However, the average length of ICS supply issued per prescription in March 2020 did not significantly differ from March 2019 (P = .89).
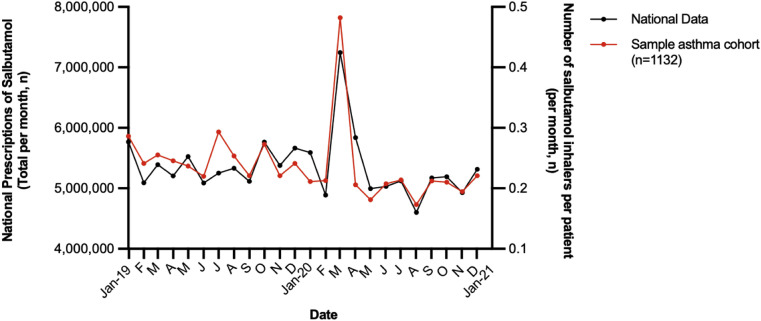
Patterns of salbutamol use
The number of salbutamol prescriptions in England in 2020 was similar to 2019 with a monthly mean of 5,381,409 (250,871) versus 5,326,557 (685,756) in 2020 (P = .79). As seen with ICS, a spike in salbutamol prescriptions occurred in March 2020 with a 34.4% increase compared with the same month in 2019 (Figure 5 ). Analysis of the sample asthma cohort of 1132 patients highlighted an equivalent spike as seen nationally, with prescription rates of 0.48 inhalers/patient in March 2020, compared with 0.26 inhalers/patient issued in March 2019. A total of 72 of 1132 (6.4%) were issued salbutamol for the first time in March 2020, of whom 22 patients were issued 2 salbutamol inhalers. Taken together, 17.2% of the salbutamol prescribed in March 2020 could be attributed to formerly salbutamol-naïve patients. Even allowing for this, the remaining 452 salbutamol prescriptions in March 2020 still represented a 56.4% increase compared with March 2019.
Figure 5.
Prescriptions of salbutamol. Total prescriptions per month are shown for all patients in England (left axis) as well as per patient per month for the sample asthma cohort (n = 1132, right axis) from 2019 to 2021.
Interestingly, despite the March peak, overall salbutamol prescriptions decreased in 2020 (P = .039) including the number prescribed >3 inhalers/year (P < .001). A significant reduction was observed for the 40-64 age group (P = .027) as well as in Black patients (P < .001) but not in other age or ethnic groups. When analyzing according to the GINA treatment step, a reduction in salbutamol was only seen in patients on GINA step 4 treatment (P < .012) (Table III ).
Table III.
Salbutamol prescription rates in 2019 to 2020
| Characteristic | n | 2019 (n = 1132) Median (IQR) |
2020 (n = 1132) Median (IQR) |
z | P value∗ |
|---|---|---|---|---|---|
| Overall salbutamol use (inhalers/patient) | 2.0 (0.0-4.0) | 2.0 (1.0-4.0) | −2.069 | .039 | |
| Sex | |||||
| Female | 630 | 2.0 (0.0-4.0) | 2.0 (1.0-4.0) | −1.318 | .187 |
| Male | 502 | 2.0 (0.0-4.0) | 2.0 (0.0-3.0) | −1.648 | .099 |
| Age | |||||
| 5-17 | 103 | 2.0 (1.0-4.0) | 2 (1.0-4.0) | −1.346 | .178 |
| 18-39 | 545 | 1.0 (0.0-2.0) | 1 (0.0-2.0) | 0.478 | 633 |
| 40-64 | 360 | 2.0 (1.0-6.0) | 2 (1.0-5.0) | −2.218 | .027 |
| ≥65 | 124 | 4.0 (2.0-7.0) | 3 (1.0-6.0) | −1.553 | .121 |
| Ethnicity | |||||
| White | 641 | 1.0 (0.0-4.0) | 2.0 (1.0-3.0) | −0.404 | .686 |
| Black | 267 | 2.0 (1.0-6.0) | 2.0 (1.0-4.0) | −3.718 | <.001 |
| Asian | 137 | 2.0 (0-3.0) | 1.0 (0.0-4.0) | −0.199 | .842 |
| Not specified | 87 | 1.0 (0.0-4.0) | 2.0 (1.0-4.0) | .445 | |
| GINA treatment step | |||||
| Salbutamol only | 250 | 1.0 (0.0-2.0) | 1.0 (0.0-2.0) | 1.331 | .183 |
| Step 2 | 498 | 2.0 (1.0-4.0) | 2.0 (1.0-3.0) | −1.167 | .243 |
| Step 3 | 150 | 1.0 (0.0–4.3) | 1.0 (0.0-4.0) | −1.628 | .104 |
| Step 4 | 184 | 4.0 (1.0-7.0) | 3.0 (1.0-7.0) | −2.509 | .012 |
| Step 5 | 50 | 3.5 (2.0-8.3) | 4.0 (2.0-7.3) | −0.169 | .866 |
| Smoking status | |||||
| Never smoker | 824 | 2.0 (0.0-4.0) | 2.0 (1.0-3.0) | −1.824 | .068 |
| Current smoker | 149 | 2.0 (1.0-4.0) | 2.0 (1.0-4.0) | −1.647 | .100 |
| Previous smoker | 2.0 (0.0-5.0) | 2.0 (1.0-5.0) | .962 | ||
| No. of patients, n (%) | |||||
| 0 inhalers | 159 | 311 (27.4) | 268 (23.7) | −0.047 | .001 |
| 1-3 inhalers | 479 (42.3) | 565 (49.9) | <.001 | ||
| >3 inhalers | 342 (30.3) | 299 (26.4) | <.001 |
GINA, Global Initiative for Asthma; IQR, interquartile range.
Data presented as number (n) and median (interquartile range).
Wilcoxon signed rank test.
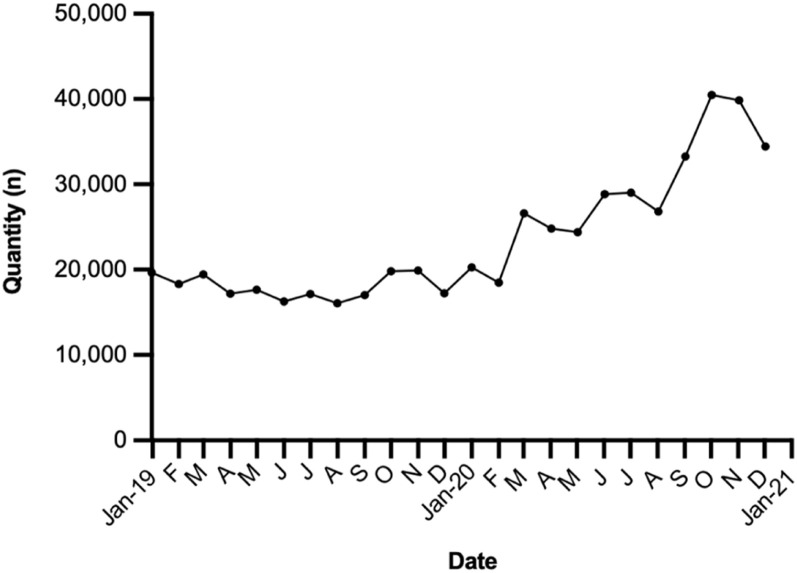
Peak flow meters
National prescribing of peak flow meters, a tool frequently used for self-monitoring and part of personalized asthma action plans (PAAPs), remained stable throughout 2019 with a mean monthly rate of 17,972 (±1399). A 43.8% rise was then observed in March 2020. However, unlike the prescription patterns of ICS and salbutamol that saw rates return to near normal levels, prescriptions of peak flow meters continued to rise steadily over the second half of 2020, peaking in October 2020 at 40,459 representing a 125% increase from the 2019 mean (Figure E2, available in this article's Online Repository at www.jaci-inpractice.org).
Figure E2.
National prescribing of peak flow meters.
Discussion
We report the prescribing patterns of asthma therapies before and during the COVID-19 pandemic in England and offer novel insights into the underlying factors that may have led to the observed patterns. We demonstrate an overall increase in prescribing of ICS from 2019 to 2020, a finding that primarily appears to have been driven by improved adherence to ICS during the pandemic. Alongside this, we report a reduction in salbutamol prescribing, with certain patient demographic and clinical characteristics associated differentially with this change. Lastly, we report that the prescription of peak flow meters has progressively increased during the pandemic.
The most substantial change in the prescription rates occurred in March 2020, when an approximate doubling in both ICS and salbutamol was seen. Our results suggest that the reason for this was likely multifactorial with some evidence of a hoarding effect, resulting from premature ICS prescribing as well as a contribution from a small proportion of ICS-naïve patients being prescribed ICS for the first time. However, the dominant driver appears to be an effort (on the part of either the health care professional, the patient, or both) to optimize ICS adherence in a large group of patients with a demonstrably poor track record of regular ICS use. Indeed, in the year before the pandemic, only a third of patients in the sample asthma cohort received sufficient ICS prescriptions to achieve good adherence, whereas almost half received fewer than 50% of the intended ICS prescriptions.
The prevalence and clinical implications of poor adherence in asthma are well described.16 , 17 In 2001, a study by Suissa et al18 highlighted a direct relationship between ICS prescription rate and risk of death from asthma, whereas in the United Kingdom, the National Review of Asthma Deaths19 described poor ICS adherence as a leading preventable factor in the fatalities. Although we observed an improvement in ICS adherence in 2020, 58% of patients still fell short of “good adherence” reflecting the continuing unmet need in this population.
It is unclear where the impetus for a new prescription in March 2020 came from. At that point in time, no data had emerged for or against the possibility that individuals with asthma may be at increased risk with COVID. However, it is probable that from their own personal experience, most patients and their clinicians would have been familiar with the decline in asthma control that follows the onset of respiratory viruses, so it is likely that there will have been a degree of apprehension on both sides driving the observed increase.
Conversely, we also observed a decline in ICS adherence in approximately a quarter of patients during the pandemic. There are no published data to help explain this finding; however, possibilities might include unintentional factors such as difficulty in obtaining a new prescription due to shielding or intentional factors including concerns about the immunosuppressive properties of ICS. Another potential explanation for the decline in ICS adherence may be a reduced symptom burden relating to decreased exposure to respiratory viruses and environmental triggers.
Older patients, and in particular those over 65 years, consistently demonstrated better ICS adherence than younger patients, a finding consistent with previous reports.20 Older age was one of the earliest risk factors to emerge in relation to COVID-19, and these patients are also more likely to have other relevant comorbidities further increasing their risk with COVID-19.21 , 22 It is possible that older patients were therefore additionally incentivized to take their ICS regularly as opposed to younger patients considered lower risk.
Epidemiological studies have similarly identified individuals of Black ethnicity as a high-risk group compared with age-matched White subjects after infection with COVID-19.23 Although we report a statistically significant improvement in ICS adherence for both White and Black patients with asthma, the magnitude of the improvement was numerically greater for Black patients, with adherence rates of 67% compared with 55% in White patients in 2020.
Before the pandemic, incremental increases in ICS adherence levels with increasing treatment step were seen, ranging from 41% (GINA 2) to 66% (GINA 5). During 2020, adherence levels were on average >70% across GINA steps 3-5; however, patients on GINA step 2 (low-dose ICS) did not significantly improve their adherence, possibly relating to an overall lower level of perceived risk.
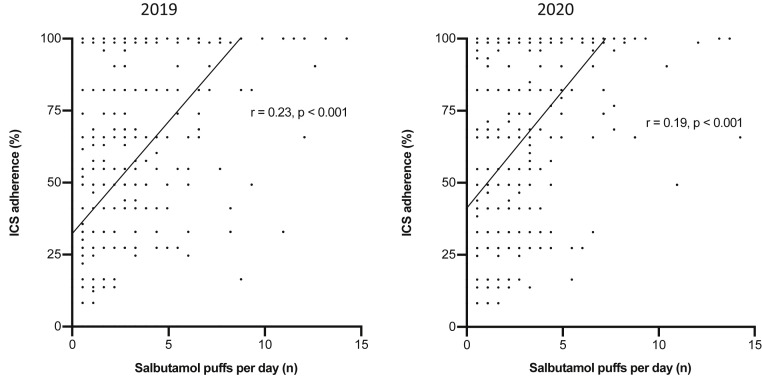
It was interesting that despite an acute surge in salbutamol prescribing in March 2020, the overall level across 2020 was lower than in 2019. This was particularly so in older patients (aged 40-64), Black patients, and those on step 4 treatment, making it tempting to relate this to the notable improvements in ICS adherence seen in these groups. However, this was not a consistent pattern across the cohort. Indeed, there was a weak positive correlation between ICS adherence and salbutamol use in both 2019 and 2020 (Figure E3, available in this article's Online Repository at www.jaci-inpractice.org), possibly driven by underlying asthma severity and/or concomitant prescribing habits driving both variables in the same direction.
Figure E3.
Correlation between adherence to inhaled corticosteroids (ICS) and salbutamol use.
Our finding of a steady increase in the prescription of peak flow meters across England has not been previously reported. We believe that the progressive increase over 2020 may reflect a move to more remote asthma consultations during the pandemic, necessitating an objective measure of disease control in the patient's home. A recent European survey describing the impact of the COVID-19 pandemic highlighted that 79% of follow-up consultations for asthma took place remotely.24 Peak flow measurements are a key component of a PAAP, empowering patients to manage their own symptoms. In addition, concern about aerosol-generating procedures will have meant that peak flow meters are likely to have been provided to patients in instances of diagnostic uncertainty.
Our analysis has 2 main limitations. The National OpenPrescribing data do not distinguish between conditions, meaning that the rates reflect patients with asthma as well as COPD for which these medications are licensed. We have attempted to overcome this by using an asthma sample cohort; however, we acknowledge that this may not precisely reflect the national picture. Secondly, in the absence of direct e-monitoring of inhaler use for our cohort, we have had to use prescription frequency as a surrogate for drug administration. At the same time, we appreciate that some patients may receive automated prescription refills, and some may receive 2 or even 3 months' worth of treatment in a single prescription. In either case, adherence will likely be overestimated. We have not reported oral corticosteroid (OCS) use as it was not possible to confirm whether the OCS was for asthma, or whether it represented an acute course or a “rescue pack” for a possible future event.
In summary, we describe patterns of ICS and salbutamol use in asthma before and during the first year of the COVID-19 pandemic. We report evidence of improved ICS adherence, lower salbutamol use, and an increase in the provision of peak expiratory flow meters enabling remote disease monitoring. Future research is required to explore the level of persistence in ICS adherence, as well as whether this has in part contributed to the recent reports of reduced acute asthma exacerbations.
Acknowledgments
H. Dhruve contributed to study design, data collection, analysis, and manuscript preparation. D. J. Jackson, G. d’Ancona, A. M. Nanzer, J. Dhariwal, and S. Holmes contributed to data analysis and manuscript preparation.
Footnotes
No funding was received for this work.
Conflicts of interest: The authors declare that they have no relevant conflicts of interest.
Online Repository
References
- 1.World Health Organization (WHO) 2020. Coronavirus disease (COVID-19) pandemic. Accessed May 3, 2021. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. [Google Scholar]
- 2.Jackson D.J., Johnston S.L. The role of viruses in acute exacerbations of asthma. J Allergy Clin Immunol. 2010;125:1178–1187. doi: 10.1016/j.jaci.2010.04.021. quiz: 88-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jackson D.J., Trujillo-Torralba M.B., del-Rosario J., Bartlett N.W., Edwards M.R., Mallia P., et al. The influence of asthma control on the severity of virus-induced asthma exacerbations. J Allergy Clin Immunol. 2015;136:497–500.e3. doi: 10.1016/j.jaci.2015.01.028. [DOI] [PubMed] [Google Scholar]
- 4.Davies G.A., Alsallakh M.A., Sivakumaran S., Vasileiou E., Lyons R.A., Robertson C., et al. Impact of COVID-19 lockdown on emergency asthma admissions and deaths: national interrupted time series analyses for Scotland and Wales. Thorax. 2021;76:867–873. doi: 10.1136/thoraxjnl-2020-216380. [DOI] [PubMed] [Google Scholar]
- 5.Shah S.A., Quint J.K., Nwaru B.I., Sheikh A. Impact of COVID-19 national lockdown on asthma exacerbations: interrupted time-series analysis of English primary care data. Thorax. 2021;76:860–866. doi: 10.1136/thoraxjnl-2020-216512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bloom C.I., Drake T.M., Docherty A.B., Lipworth B.J., Johnston S.L., Nguyen-Van-Tam J.S., et al. Risk of adverse outcomes in patients with underlying respiratory conditions admitted to hospital with COVID-19: a national, multicentre prospective cohort study using the ISARIC WHO Clinical Characterisation Protocol UK. Lancet Respir Med. 2021;9:699–711. doi: 10.1016/S2213-2600(21)00013-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith S.J., Busby J., Heaney L.G., Pfeffer P.E., Jackson D.J., Yang F., et al. The impact of the first COVID-19 surge on severe asthma patients in the UK. Which is worse: the virus or the lockdown? ERJ Open Res. 2021;7:00768–2020. doi: 10.1183/23120541.00768-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention Coronovirus disease 2019 (COVID-19) https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/asthma.html Accessed May 3, 2020.
- 9.Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention; 2020. Accessed May 4, 2021. https://ginasthma.org
- 10.Bender B.G., Pedan A., Varasteh L.T. Adherence and persistence with fluticasone propionate/salmeterol combination therapy. J Allergy Clin Immunol. 2006;118:899–904. doi: 10.1016/j.jaci.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 11.Heaney L.G., Horne R. Non-adherence in difficult asthma: time to take it seriously. Thorax. 2012;67:268–270. doi: 10.1136/thoraxjnl-2011-200257. [DOI] [PubMed] [Google Scholar]
- 12.EBM DataLab, Department of Primary Care Health Services, University of Oxford. Home ǀ OpenPrescribing; 2021. Accessed May 1, 2021. https://openprescribing.net/
- 13.Kaye L., Theye B., Smeenk I., Gondalia R., Barrett M.A., Stempel D.A. Changes in medication adherence among patients with asthma and COPD during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8:2384–2385. doi: 10.1016/j.jaip.2020.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee J., Tay T.R., Radhakrishna N., Hore-Lacy F., Mackay A., Hoy R., et al. Nonadherence in the era of severe asthma biologics and thermoplasty. Eur Respir J. 2018;51:1701836. doi: 10.1183/13993003.01836-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams L.K., Peterson E.L., Wells K., Ahmedani B.K., Kumar R., Burchard E.G., et al. Quantifying the proportion of severe asthma exacerbations attributable to inhaled corticosteroid nonadherence. J Allergy Clin Immunol. 2011;128:1185–1191.e2. doi: 10.1016/j.jaci.2011.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Engelkes M., Janssens H.M., de Jongste J.C., Sturkenboom M.C., Verhamme K.M. Medication adherence and the risk of severe asthma exacerbations: a systematic review. Eur Respir J. 2015;45:396–407. doi: 10.1183/09031936.00075614. [DOI] [PubMed] [Google Scholar]
- 17.d’Ancona G., Kent B.D. Practical applications of FeNO measurement and inhaler monitoring technologies in the management of difficult asthma. J Allergy Clin Immunol Pract. 2021;9:1539–1540. doi: 10.1016/j.jaip.2021.01.001. [DOI] [PubMed] [Google Scholar]
- 18.Suissa S., Ernst P. Inhaled corticosteroids: impact on asthma morbidity and mortality. J Allergy Clin Immunol. 2001;107:937–944. doi: 10.1067/mai.2001.115653. [DOI] [PubMed] [Google Scholar]
- 19.Royal College of Physicians . RCP; London: 2014. Why asthma still kills: the National Review of Asthma Deaths (NRAD) Confidential Enquiry report. [Google Scholar]
- 20.Dima A.L., Hernandez G., Cunillera O., Ferrer M., de Bruin M. Asthma inhaler adherence determinants in adults: systematic review of observational data. Eur Respir J. 2015;45:994–1018. doi: 10.1183/09031936.00172114. [DOI] [PubMed] [Google Scholar]
- 21.Williamson E.J., Walker A.J., Bhaskaran K., Bacon S., Bates C., Morton C.E., et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Docherty A.B., Harrison E.M., Green C.A., Hardwick H.E., Pius R., Norman L., et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perkin M.R., Heap S., Crerar-Gilbert A., Albuquerque W., Haywood S., Avila Z., et al. Deaths in people from Black, Asian and minority ethnic communities from both COVID-19 and non-COVID causes in the first weeks of the pandemic in London: a hospital case note review. BMJ Open. 2020;10:e040638. doi: 10.1136/bmjopen-2020-040638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eguiluz-Gracia I., van den Berge M., Boccabella C., Bonini M., Caruso C., Couto M., et al. Real-life impact of COVID-19 pandemic lockdown on the management of pediatric and adult asthma: a survey by the EAACI Asthma Section. Allergy. 2021;76:2776–2784. doi: 10.1111/all.14831. [DOI] [PMC free article] [PubMed] [Google Scholar]