Abstract
Introduction
Diabetes-related distress is present in a high proportion of people with type 2 diabetes mellitus. We hypothesized that complexity of the antidiabetic medication regimen is a factor that is associated with diabetes-related distress.
Research design and methods
This was a retrospective study including a group of 74 patients managed at a tertiary care center. Patients with type 1 diabetes mellitus, steroid-induced diabetes, post-transplant diabetes, and other types of diabetes were excluded. Patients were screened using the Diabetes Distress Scale-2 (DDS-2). A Diabetes Medication Complexity Scoring (DMCS) system was developed to objectively assess the diabetes medication complexity. Based on DMCS, participants were categorized into three groups: low (n=26), moderate (n=22), and high (n=26) medication complexity.
Results
Complexity groups were similar in sociodemographic characteristics, diabetes duration, body mass index, and blood pressure as well as the prevalence of hypertension, hyperlipidemia and hypoglycemic episodes. However, there were significant differences for HbA1c with higher HbA1c in the high and moderate complexity groups than in the low group (p=0.006). The microvascular complications were also more common in higher complexity groups (p=0.003). The prevalence of diabetes-related distress (DDS-2 ≥6) was 34.6% in the low, 36.4% in the moderate and 69.2% in the high complexity groups (p=0.021). There were significant differences in DDS-2 score among complexity groups (p=0.009), with higher DDS-2 score in the high complexity group compared with the moderate (p=0.008) and low complexity groups (p=0.009). The difference in DDS-2 score remained significant after adjusting for HbA1c (p=0.024) but did not reach statistical significance after controlling for both HbA1c and microvascular complications (p=0.163).
Conclusions
A complex antidiabetic medication regimen may be associated with high levels of diabetes-related distress.
Keywords: medication, diabetes mellitus, type 2, psychology
Significance of this study.
What is already known about this subject?
Almost 50% patients with diabetes have high levels of diabetes-related distress when screened using a validated questionnaire.
Patients positive for diabetes-related distress also have high HbA1c.
What are the new findings?
This study includes a new method of evaluating complexity of antidiabetic medication regimen.
High complexity of medication regimen was associated with high likelihood of screening positive for diabetes-related distress.
High complexity of medication regimen was also associated with higher diabetes-related distress score independent of HbA1c.
How might these results change the focus of research or clinical practice?
Patients with complex antidiabetic treatment regimens may need more psychological support.
If the medication regimen can be simplified without compromising glycemic control, there is a potential to decrease diabetes-related distress that may also improve glycemic control.
Introduction
Diabetes is a complex chronic disease affecting multiple aspects of human life. Patients with diabetes often report high levels of psychological distress. Diabetes-related distress refers to the negative psychological reactions that are specific to living with diabetes rather than other psychological disorders.1 The prevalence of diabetes-related distress is reported to be as high as 48% in patients with type 2 diabetes mellitus (T2DM).1 2 High levels of distress significantly impact medication adherence and are associated with disease severity, high self-care burden, suboptimal care, and high HbA1c.3–5 Increased severity of disease or high HbA1c are likely to impose higher treatment burden, including the need for complex medication regimens, that may in turn increase diabetes-related distress.
Medication regimen complexity index (MRCI) is a validated tool for quantifying drug regimen complexity based on the quantity of medications, dosage form, dosage frequency, and additional instructions.6 Recent studies using the MRCI score have shown that high medication regimen complexity (including all prescribed drugs) is associated with poor glycemic control and decreased medication adherence.7 8 However, there are few studies to evaluate the impact of complexity of only the antidiabetic medication regimen on psychological health of people with T2DM.
Due to the progressive nature of T2DM, patients often need more medications over time.9 The antidiabetic medication regimen can become highly complex with the years unless conscious efforts are made to simplify the regimen and discontinue the ineffective or less effective medications. The American Diabetes Association recommends deintensification or simplification of treatment regimens in older people with multiple comorbidities to reduce the treatment burden and to prevent hypoglycemia.10 Psychological impact of highly complex treatment regimens for diabetes has not been studied.
We hypothesized that complexity of antidiabetic medication regimen in people with T2DM is a factor that may contribute to increased diabetes-related distress. If true, these patients may need considerations for additional psychological support or deintensification of the treatment regimen. Therefore, we conducted a study to evaluate the association between antidiabetic medication complexity score and diabetes-related distress.
Methods
This was a retrospective study including a group of patients with T2DM managed by one provider at a major academic diabetes center. The study was reviewed by the University of Miami Institutional Review Board (IRB ID: 20180060) and waiver of informed consent was approved. Patients were given a printed questionnaire with the two item Diabetes Distress Scale (DDS-2) at the time of check-in and asked to return it with answers to the provider at the start of visit. Patients with type 1 diabetes mellitus (T1DM), steroid induced diabetes, post-transplant diabetes, and other types of diabetes were excluded. Patients presenting for their first visit were also excluded to minimize the contribution of new visit related stress on diabetes-related distress. Consecutive adult patients with T2DM who completed DDS-2 screening at the start of their follow-up visits while receiving consistent antidiabetic medications for 6–12 weeks were included in the study. If a patient had more than one follow-up visits during the study period, only the first follow-up visit was taken into account. Demographic data, medications and laboratory data were obtained from electronic medical records. For this study, data values available on the date of the visit when the DDS-2 was completed (and before the patient was seen by the provider) were taken into account. Thus, antidiabetic medication regimen complexity was drawn from the chart from the same time as the diabetes distress was assessed and medication changes made on that visit were not included. In addition, medical records were manually reviewed for comorbidities, hypoglycemic episodes, and diabetes complications. Manual chart reviews were conducted using a data collection sheet by one investigator (HA) and checked for accuracy by another investigator (ML) with random checks by a third investigator (RG). Data were collected for consecutive patients seen from January 2019 to July 2019.
The DDS is a validated self-report questionnaire including 17 items that assesses emotional burden, physician-related distress, regimen-related distress, and interpersonal distress to quantify diabetes-related distress.11 12 The DDS-2 is a brief two-item version used as a more practical screening tool in diabetes clinics.13 We used the DDS-2 in this study to reduce patient burden and because it does not include questions about medications. Relative to the full scale, the DDS-2 correctly screens 92.7% of patients.6 A total score of 6.0 or higher on the DDS-2 is considered positive for high diabetes distress.
While MRCI has been used to quantify overall drug regimen complexity, it was not designed specifically for diabetes medications.6 Thus, to objectively assess the medication complexity of antidiabetic regimen, we developed a Diabetes Medication Complexity Score that was modeled after the published literature on MRCI6 and a published study that used MRCI to calculate complexity of medication regimen in patients with diabetes.14 Each oral medication was given one point that was multiplied by the number of times the medication was to be administered daily. One time a week glucagon-like peptide-1 receptor agonist (GLP-1RA) injection was given 2 points and one time a day GLP-1RA injection was given 3 points. One time a day insulin injection was given 4 points. Using this scoring system, we defined low, moderate, and high complexity scores as follows, modeled after the published study:14
-
Low complexity regimen: ≤4. One or two oral medications, each given up to two times a day or ≤1 injection daily.
Examples: Metformin two times a day (score=2); Metformin two times a day+Empagliflozin one time a day (score=3); Metformin two times a day+Glipizide two times a day (score=4); Metformin two times a day+one time a week GLP-1RA injection (score=4); one time a day basal insulin alone (score=4).
-
Moderate complexity regimen: 5–8. More than two oral medications given more than two times a day or two oral medications+basal insulin or insulin injection two times a day.
Examples: Metformin two times a day+Long acting insulin one time a day (score=6); Metformin two times a day+Empagliflozin one time a day+one time a week GLP-1RA injection (score=5).
High complexity regimen: >8. More than three injections a day of insulin: (basal+meal time insulin) or Insulin Pump.
The scoring system was validated for accuracy by independent investigators. A random sample of 21 unidentified patient charts was evaluated for Diabetes Medication Complexity Scoring by two independent investigators, who were not involved in the study. The final scores were reviewed and compared for consistency, with high agreement between the two investigators’ ratings of patients’ medication complexity (Cohen’s kappa=0.944, p<0.001).
Statistical analysis
All data were extracted from medical records and deidentified. Data were tested and found to have normal distributions. Therefore, continuous data are presented as means with SD and categorical data are presented as number with percentages. Data analyses was prespecified to test the hypothesis that medication complexity is a predictor of diabetes distress and thus, high complexity group would be more likely to screen positive for diabetes-related distress as well as score higher on the DDS-2. We compared patients who were classified as having either low, moderate, or high complexity scores to identify factors that were significantly different between the three groups. The three groups were compared using one-way analysis of variance (ANOVA) and analysis of covariance for continuous variables and χ² tests for categorical variables. Variables that were significantly different between the groups on one-way ANOVA or known to affect DDS-2 were included as covariates.5 15 16 The least squares difference test was used for multiple comparisons in posthoc analyses. Statistical significance was determined by p<0.05. We used SPSS V.25 (IBM, New York, USA) for statistical analysis.
Results
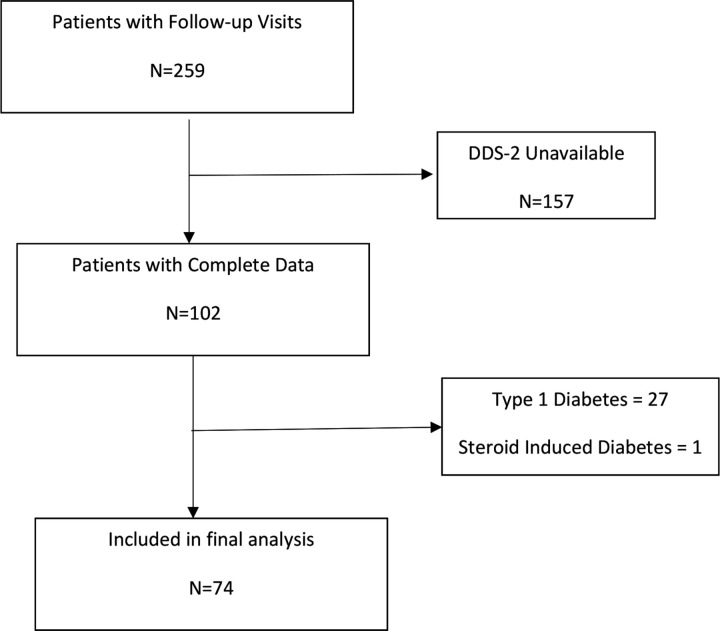
Patient inclusion for the study is shown in figure 1. We found 259 patients who had completed one or more follow-up visits during the study period and 102 of them had completed the DDS-2 questionnaire. We excluded 27 patients with type 1 diabetes and 1 patient with steroid induced diabetes from analysis. Thus, 74 patients with T2DM who met the inclusion criteria were included in the final analysis. The mean age of patients was 59±10 years and mean duration of diabetes was 13±9 years. The sample included 51% men, 50% Hispanic patients, and 35% Spanish speaking patients; 76% of patients reported living with family or partner. The majority of patients had hypertension (78%), hyperlipidemia (70%), and a family history of diabetes (72%). Half the sample had one or more microvascular complications (50%) but very few had macrovascular complications (12%). Diabetes medication complexity score ranged from 0 to 19, with low scores in 26 (35%), moderate scores in 22 (30%), and high scores in 26 (35%) patients. The mean DDS-2 was 5.36±2.97; with 35 patients screened positive (DDS-2 ≥6) and 39 patients screened negative (DDS-2=0–5) for diabetes-related distress.
Figure 1.
Patient inclusion for analysis. DDS-2, Diabetes Distress Scale-2.
The demographic and medical characteristics of the patients compared by medication complexity groups are shown in table 1.
Table 1.
Comparison of patients’ demographic and medical characteristics by medication complexity
| Low complexity | Moderate complexity | High complexity | P value | |
| Age (years) | 62.6±10.4 | 58.9±10.2 | 56.7±10.3 | 0.13 |
| Gender | 0.51 | |||
| Male | 15 (57.7) | 12 (54.5) | 11 (42.3) | |
| Female | 11 (42.3) | 10 (45.5) | 15 (57.7) | |
| Race/ethnicity (self-reported)* | 0.38 | |||
| White or Caucasian | 4 (15.4) | 4 (20) | 2 (7.7) | |
| Black/African American | 2 (15.4) | 5 (25) | 2 (7.7) | |
| Hispanic | 18 (69.2) | 11 (55) | 21 (80.8) | |
| Native Hawaiian/Pacific Islander | 0 | 0 | 1 (3.8) | |
| BMI (kg/m2) | 31.3±5.2 | 32.1±6.5 | 34.6±5.2 | 0.09 |
| Systolic BP (mm Hg) | 132±15.3 | 127.6±13.5 | 131.8±17.3 | 0.56 |
| Diastolic BP (mm Hg) | 70.1±10.9 | 71.3±10.9 | 70.5±10.8 | 0.93 |
| Duration of diabetes (years) | 11.4±9.8 | 13.6±9.1 | 13.8±7.6 | 0.55 |
| HbA1c (%)† | 7.4±1.2 | 8.7±1.5 | 8.6±2 | 0.006 |
| Creatinine (mg/dL)‡ | 0.88±0.24 | 0.9±0.27 | 1.0±0.32 | 0.5 |
| eGFR (mL/min)§ | 79.4±17.9 | 84.7±24.5 | 83.1±19.9 | 0.72 |
| LDL (mg/dL)¶ | 92.8±38.1 | 97.8±25.2 | 85±33.9 | 0.59 |
| Diabetes distress score (range 2–12) | 4.7±2.8 | 4.6±2.8 | 6.8±2.9 | 0.009 |
| Diabetes distress | 0.02 | |||
| DDS-2<6 | 17 (65.4) | 14 (63.6) | 8 (30.8) | |
| DDS-2≥6 | 9 (34.6) | 8 (36.4) | 18 (69.2) | |
| Hypertension | 0.36 | |||
| No | 4 (15.4) | 7 (31.8) | 5 (19.2) | |
| Yes | 22 (84.6) | 15 (68.2) | 21 (80.8) | |
| Hyperlipidemia* | 0.97 | |||
| No | 7 (29.2) | 6 (27.3) | 8 (30.8) | |
| Yes | 17 (70.8) | 16 (72.7) | 18 (69.2) | |
| Hypoglycemia | 0.1 | |||
| No | 21 (80.8) | 13 (59.1) | 14 (53.8) | |
| Yes | 5 (19.2) | 9 (40.9) | 12 (46.2) | |
| Microvascular complications** | 0.003 | |||
| No | 18 (72) | 11 (55) | 6 (24) | |
| Yes | 7 (28) | 9 (45) | 19 (76) | |
| Macrovascular complications†† | 0.43 | |||
| No | 20 (87) | 20 (95.2) | 19 (82.6) | |
| Yes | 3 (13) | 1 (4.8) | 4 (17.4) |
*n=72.
†n=73.
‡n=61.
§n=54.
¶n=47.
**n=70.
††n=67.
BMI, body mass index; BP, blood pressure; DDS-2, Diabetes Distress Scale-2; eGFR, estimated glomerular filtration rate; LDL, low density lipoprotein.
Complexity groups were similar on sociodemographic characteristics, diabetes duration, body mass index, and blood pressure as well as the prevalence of hypertension, hyperlipidemia, and hypoglycemic episodes over the last year. The prevalence of microvascular complications varied as a function of low (28%), moderate (45%), and high (76%) regimen complexity (χ2 (2)= 11.8, p = 0.003). One-way ANOVA also revealed significant complexity group differences for HbA1c with higher HbA1c in the high and moderate complexity groups than in the low complexity group (F(2,70) = 5.47, p=0.006). The prevalence of diabetes-related distress (DDS-2 ≥6) was 34.6% in the low, 36.4% in the moderate, and 69.2% in the high complexity groups (χ2(2)=7.75, p=0.021).
One-way ANOVA showed significant differences in DDS-2 score among medication complexity group (F(2,71) = 4.99, p=0.009). Posthoc analyses showed that diabetes-related distress was significantly greater in the high complexity group compared with the moderate complexity group (p=0.008) as well as the low complexity group (p=0.009) (see table 1).
Analysis of covariance adjusting for HbA1c showed that DDS-2 score significantly differed as a function of complexity group (F(2,69) = 3.93, p=0.024). The model explained 16.2% of the variance in diabetes-related distress (R2=0.162). The adjusted DDS-2 was significantly greater for the high complexity group (adjusted DDS-2=6.61) compared with the moderate complexity group (adjusted DDS-2=4.46; p=0.01) and the low complexity group (adjusted DDS-2=4.98; p=0.049). When the presence of microvascular complications was added as a control variable in addition to HbA1c in a univariate general linear model to analyze the relationship between DDS-2 and medication complexity score, the adjusted DDS-2 means were 6.44 for the high complexity group, 4.8 for the moderate complexity group, and 5.16 for the low complexity group (F(2,64) = 1.87, p=0.163).
Discussion
This study shows that antidiabetic medication complexity is associated with high levels of diabetes-related distress. Patients with higher antidiabetic regimen complexity also had poor diabetes control and high prevalence of microvascular complications. However, medication complexity was found to be an important factor associated with diabetes distress. The association between antidiabetic medication complexity and diabetes-related distress persisted after adjusting for HbA1c, but was not significant when controlling for both HbA1c and microvascular complications. Our study highlights the points that patients on complex treatment regimens may need more psychological support and if the medication regimen can be simplified without compromising glycemic control, there is potential to partially decrease the diabetes-related distress.
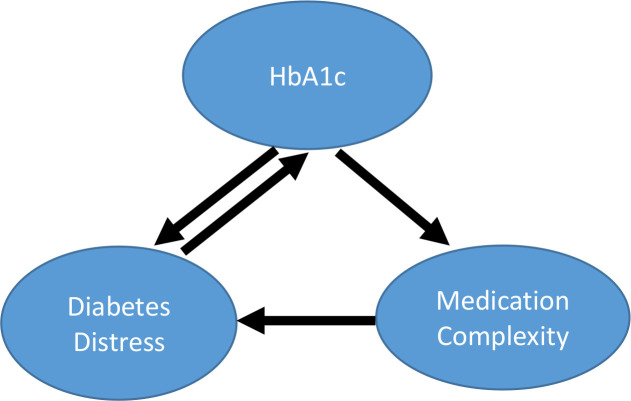
Patients with T2DM require more medications or changes in the medication regimen over time due to progressive nature of this disease.9 Patients with poorly controlled diabetes are likely to receive more medications, especially in the presence of complications of diabetes. There is a natural tendency among providers to add more medications in attempts to improve glycemic control, making the treatment regimen more complex. Moreover, clinical practice guidelines recommend intensification of medication regimen when HbA1c target is not being met.9 Data show that clinical inertia is a factor among providers not adjusting medications when indicated, often leading to poor glycemic control.17 However, more complex treatment regimens are harder to implement for patients and cause more distress. In a previous study, higher diabetes-specific medication regimen complexity was associated with poorer glycemic control and the authors suggested that simplifying antidiabetic medication regimens, especially where the treatment guidelines give no preference, could be a step toward achieving treatment goals.14 We propose that patients with T2DM get into a cycle of poor glycemic control, increased medication complexity, and increased distress (figure 2). One of the ways to break this cycle may be simplifying the treatment regimen if possible. This may include discontinuing ineffective or less effective medications, which could result in an improvement in medication adherence. Our hypothesis is supported by a recent study showing that patients with less complex diabetes-specific medication regimens have better adherence, and that patients with complex regimens, have worse adherence and poor glycemic control.7 We have also reported that de-escalating from multiple subcutaneous insulin injections to one time a day basal insulin is associated with improvement in glycemic control and decrease in rates of hypoglycemia, which could be related to an improvement in medication adherence.18 However, the simplification of medication regimen is uncommon in clinical practice. In a previous study, we found that even in elderly patients at high risk of hypoglycemia, antidiabetic medication regimen was simplified less than half the time.19 We propose that simplification of medication regimen when possible may improve the psychological well-being of the patient. Another important intervention could be psychological and behavioral support for patients on complex medication regimens who also have increased distress. Previous studies have shown an improvement in medication adherence with slightly improved HbA1c with these intervention.20
Figure 2.
Interaction between medication complexity, HbA1c and diabetes-related distress.
Our study is consistent with limited existing data that evaluated the correlates of diabetes distress in T2DM.21 22 Previous studies have also shown that use of insulin is associated with high diabetes distress in T2DM.23 Insulin use, especially multiple insulin injection regimen that requires frequent blood glucose monitoring and insulin dose adjustments, can be highly distressing to a patient with T2DM. This may be partly due to lower emphasis on education and support for insulin use in T2DM than in T1DM. Main components of diabetes education at the onset of T1DM include carbohydrate counting, blood glucose monitoring, and insulin administration. However, major emphasis of diabetes education in patients with new onset T2DM focuses on lifestyle changes (diet and exercise) for weight reduction. Patients with T2DM often receive insulin after a few years of being on oral agents and may not receive the same education for injection therapy as patients with T1DM. Diabetes education, psychological, and social support may help lower diabetes distress in patient with T2DM.24
There are several limitations of our study. First, it was a retrospective study that used available data; only DDS-2 was available and DDS-17 was not available. Second, we did not take into account all the medications for calculating medication complexity score because our goal was to focus on antidiabetic regimen, with the hope of future interventions to lower complexity of antidiabetic medication regimens for T2DM. Patients with T2DM often take multiple other medications that may confound the relationship between diabetes-related distress and antidiabetic medication complexity. While it may not be possible to decrease overall medication complexity, it may be possible to simplify antidiabetic treatment in certain patients. Last, our study did not establish whether or not it is feasible to reduce the antidiabetic medication complexity and what will be its consequences in terms of glycemic control and diabetes distress.
In conclusion, antidiabetic medication complexity is associated with high levels of diabetes distress and poor diabetes control. Psychological well-being of patients with diabetes being an important goal of treatment of diabetes, future studies should evaluate whether simplifying antidiabetic medication complexity leads to decreased diabetes distress without compromising glycemic control.
Footnotes
Contributors: ML: conception of the work, data collection. RL: data analysis and interpretation. HA: data collection. PGS: data analysis and interpretation, critical revision of the article. RG: conception of the work, data analysis and interpretation, critical revision of the article, guarantor of this work and takes full responsibility for the work as a whole, including the study design, access to data, and the decision to submit and publish the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: RG is an editorial board member of the BMJ Open Diabetes Research & Care.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Young-Hyman D, de Groot M, Hill-Briggs F, et al. Psychosocial care for people with diabetes: a position statement of the American diabetes association. Diabetes Care 2016;39:2126–40. 10.2337/dc16-2053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perrin NE, Davies MJ, Robertson N, et al. The prevalence of diabetes-specific emotional distress in people with type 2 diabetes: a systematic review and meta-analysis. Diabet Med 2017;34:1508–20. 10.1111/dme.13448 [DOI] [PubMed] [Google Scholar]
- 3.Fisher L, Mullan JT, Arean P, et al. Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care 2010;33:23–8. 10.2337/dc09-1238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pandit AU, Bailey SC, Curtis LM, et al. Disease-Related distress, self-care and clinical outcomes among low-income patients with diabetes. J Epidemiol Community Health 2014;68:557–64. 10.1136/jech-2013-203063 [DOI] [PubMed] [Google Scholar]
- 5.Nanayakkara N, Pease A, Ranasinha S, et al. Depression and diabetes distress in adults with type 2 diabetes: results from the Australian National diabetes audit (ANDA) 2016. Sci Rep 2018;8:7846. 10.1038/s41598-018-26138-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hirsch JD, Metz KR, Hosokawa PW, et al. Validation of a patient‐level medication regimen complexity index as a possible tool to identify patients for medication therapy management intervention. Pharmacotherapy 2014;34:826–35. 10.1002/phar.1452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ayele AA, Tegegn HG, Ayele TA, et al. Medication regimen complexity and its impact on medication adherence and glycemic control among patients with type 2 diabetes mellitus in an Ethiopian General Hospital. BMJ Open Diabetes Res Care 2019;7:e000685. 10.1136/bmjdrc-2019-000685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boye KS, Mody R, Lage MJ, et al. Chronic Medication Burden and Complexity for US Patients with Type 2 Diabetes Treated with Glucose-Lowering Agents. Diabetes Ther 2020;11:1513–25. 10.1007/s13300-020-00838-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Diabetes Association . 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes-2021. Diabetes Care 2021;44:S111–24. 10.2337/dc21-S009 [DOI] [PubMed] [Google Scholar]
- 10.American Diabetes Association . 12. Older Adults: Standards of Medical Care in Diabetes-2021. Diabetes Care 2021;44:S168–79. 10.2337/dc21-S012 [DOI] [PubMed] [Google Scholar]
- 11.Polonsky WH, Anderson BJ, Lohrer PA, et al. Assessment of diabetes-related distress. Diabetes Care 1995;18:754–60. 10.2337/diacare.18.6.754 [DOI] [PubMed] [Google Scholar]
- 12.Polonsky WH, Fisher L, Earles J. Assessing psychosocial distress in diabetes. Development of the Diabetes Distress Scale 2005;28:626–31. [DOI] [PubMed] [Google Scholar]
- 13.Fisher L, Glasgow RE, Mullan JT, et al. Development of a brief diabetes distress screening instrument. Ann Fam Med 2008;6:246–52. 10.1370/afm.842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yeh A, Shah-Manek B, Lor KB. Medication regimen complexity and A1c goal attainment in underserved adults with type 2 diabetes. Ann Pharmacother 2017;51:111–7. 10.1177/1060028016673652 [DOI] [PubMed] [Google Scholar]
- 15.Winchester RJ, Williams JS, Wolfman TE, et al. Depressive symptoms, serious psychological distress, diabetes distress and cardiovascular risk factor control in patients with type 2 diabetes. J Diabetes Complications 2016;30:312–7. 10.1016/j.jdiacomp.2015.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang Q-Q, Sun J-W, Shao D, et al. The association between diabetes complications, diabetes distress, and depressive symptoms in patients with type 2 diabetes mellitus. Clin Nurs Res 2021;30:293–301. 10.1177/1054773820951933 [DOI] [PubMed] [Google Scholar]
- 17.Khunti K, Wolden ML, Thorsted BL, et al. Clinical inertia in people with type 2 diabetes: a retrospective cohort study of more than 80,000 people. Diabetes Care 2013;36:3411–7. 10.2337/dc13-0331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.ARUNACHALAM A, GARG R. 880-P: insulin regimen and glycemic control in people with type 2 diabetes mellitus. Am Diabetes Assoc 2021. [Google Scholar]
- 19.Pirela DV, Garg R. De-intensification of diabetes treatment in elderly patients with type 2 diabetes mellitus. Endocr Pract 2019;25:1317–22. 10.4158/EP-2019-0303 [DOI] [PubMed] [Google Scholar]
- 20.Perrin N, Bodicoat DH, Davies MJ, et al. Effectiveness of psychoeducational interventions for the treatment of diabetes-specific emotional distress and glycaemic control in people with type 2 diabetes: a systematic review and meta-analysis. Prim Care Diabetes 2019;13:556–67. 10.1016/j.pcd.2019.04.001 [DOI] [PubMed] [Google Scholar]
- 21.Wardian J, Sun F. Factors associated with diabetes-related distress: implications for diabetes self-management. Soc Work Health Care 2014;53:364–81. 10.1080/00981389.2014.884038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wardian JL, Tate J, Folaron I, et al. Who's distressed? A comparison of diabetes-related distress by type of diabetes and medication. Patient Educ Couns 2018;101:1490–5. 10.1016/j.pec.2018.03.001 [DOI] [PubMed] [Google Scholar]
- 23.Delahanty LM, Grant RW, Wittenberg E, et al. Association of diabetes-related emotional distress with diabetes treatment in primary care patients with type 2 diabetes. Diabet Med 2007;24:48–54. 10.1111/j.1464-5491.2007.02028.x [DOI] [PubMed] [Google Scholar]
- 24.Baek RN, Tanenbaum ML, Gonzalez JS. Diabetes burden and diabetes distress: the buffering effect of social support. Ann Behav Med 2014;48:145–55. 10.1007/s12160-013-9585-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on reasonable request.