The severe acute respiratory syndrome coronavirus (SARS-CoV-2) has caused global lockdowns with severe mobility restrictions and social isolation measures to contain the epidemic. COronaVIrus Disease 19 (COVID-19) has put unprecedented tests and strain on the resilience of global healthcare systems, resulting in the unavoidable deprioritisation of oncological activities [1,2]. Numerous centres have implemented stringent measures to minimise the risk of exposure to cancer patients. However, the benefits of these actions must be weighed against the costs, as COVID-19 should also be held accountable for future worsened oncological survival outcomes. Surprisingly, the most relevant risk factors of COVID-19 severity in lung cancer patients were not cancer or cancer-directed therapies but lung cancer risk factors and associated chronic medical conditions [3].
Additionally, the risks associated with COVID-19 and resource reallocation have altered the risk-benefit ratio of lung cancer screening and lung nodule management. In a risk-mitigation pandemic scenario, care should be taken not to jeopardise the lung cancer patient's prognosis. With the relaxation of the lockdown measures, it should be critical to restore case volumes whilst balancing the clinical needs of surgical patients against the available local offer of healthcare services. It is likely that diverting resources away from routine treatments, combined with months of daily bulletins warning people to avoid hospitals as much as possible, contributed to adverse lung cancer outcomes. Several initiatives and boards are being established to define ethical, organisational, and technical principles that will guide the catch up on thousands of missed surgical procedures and ensure continuity of diagnostic and therapeutic services to oncology patients.
We assessed COVID-19's impact on lung cancer screening and distribution of lung cancer stages at our institution by analysing the rates of pathological staging review by a multidisciplinary tumour board. We compared the baseline period (January to July 2019) and the COVID-19 waves in the first semesters of 2020 and 2021.
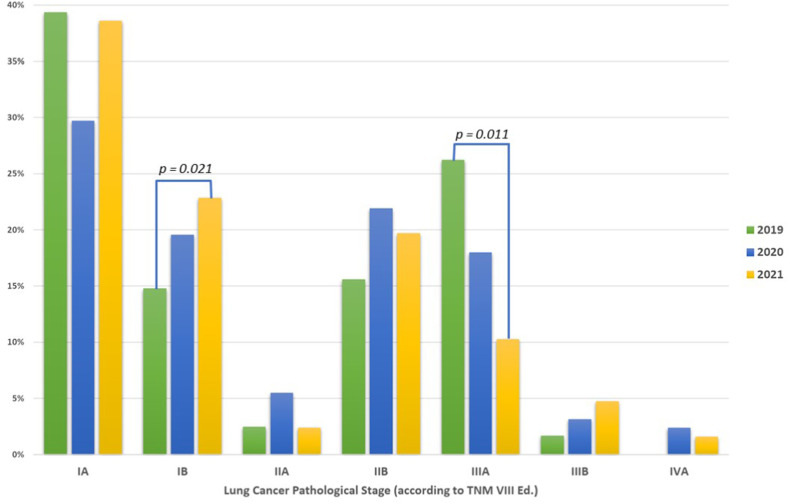
During the first semesters of 2019, 2020, and 2021, we respectively performed 122, 128, and 127 lobectomies for lung cancer. The main characteristics were reported in Table 1 . Among the cohorts, there were no statistically significant differences between the surgical approaches (thoracotomy versus minimally-invasive approaches, p = 0.78) and between the resected lobes (p = 0.90). While there were no significant differences in the number of patients with advanced-stage disease, there was a significantly (p = 0.014) lower number of patients treated in 2020 at the early stage when compared to the same six-month period in 2019. The number of early-stage lung cancers treated in 2021 rose to a value similar to 2019, probably due to the activation of digital health and telemedicine protocols at our institution in the second half of 2020. A statistically significant (p = 0.021) increase in the number of IB – IIB stages was observed. Unfortunately, there was a statistically significant decrease (p = 0.011) in the number of operable locally advanced tumours (stage IIIA) due to disease upstaging (Fig. 1 ).
Table 1.
Surgical characteristics. Data were shown as number (percentage) if not otherwise defined.
| 2019 (No. = 122) | 2020 (No. = 128) | 2021 (No. = 127) | p-value | |
|---|---|---|---|---|
| Age, median (range) | 66 (42–90) | 69 (38–84) | 68 (33–86) | 0.90 |
| Surgical approach | ||||
| Thoracotomy | 59 (48.36%) | 52 (40.63%) | 33 (25.98%) | 0.78 |
| Robotic-Assisted Thoracic Surgery | 59 (48.36%) | 53 (41.41%) | 76 (59.84%) | |
| Video-Assisted Thoracic Surgery | 4 (3.28%) | 23 (17.97%) | 18 (14.17%) | |
| Type of Lobectomy | ||||
| Right Upper Lobectomy | 35 (28.69%) | 49 (38.28%) | 39 (30.71%) | 0.99 |
| Right Middle Lobectomy | 7 (5.74%) | 6 (4.69%) | 13 (10.24%) | |
| Right Lower lobectomy | 24 (19.67%) | 23 (17.97%) | 28 (22.05%) | |
| Left Upper Lobectomy | 32 (26.23%) | 33 (25.78%) | 37 (29.13%) | |
| Left Lower Lobectomy | 24 (19.67%) | 17 (13.28%) | 10 (7.87%) | |
Fig. 1.
Distribution of the patients according to the pathological stage.
We observed a significant decrease in early-stage cases at our national oncological referral centre for thoracic surgery and lung cancer screening. This cannot plausibly be ascribed to a lower lung cancer incidence. On the other end, the impact of lockdown measures on the reduction of early-stage lung cancer and other malignancies diagnoses should be investigated and addressed. People's fear of hospitals resulted in a diagnostic delay, whose most severe effects occurred in the first months of 2022. The COVID-19 pandemic has accelerated the need for a digital revolution in health care [4]. The World Health Organization has emphasised the importance of integrating technologies into health systems. The availability of unprecedented qualitative and quantitative data, the application of advanced analytics, the pervasive digital innovation have the potential to revolutionise cancer treatment and prevention in the light of the challenges posed by the ongoing pandemic.
Declaration of competing interest
None.
Acknowledgments
This work was partially supported by the Italian Ministry of Health with Ricerca Corrente and 5x1000 funds.
References
- 1.Kaufman H.W., et al. Changes in newly identified cancer among US patients from before COVID-19 through the first full year of the pandemic. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collaborative C. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bertolaccini L., et al. Paying another tribute to the COVID-19 pandemic: the decrease of early lung cancers. Ann Thorac Surg. 2021;111:745–746. doi: 10.1016/j.athoracsur.2020.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petracca F., et al. Harnessing digital health technologies during and after the COVID-19 pandemic: context matters. J Med Internet Res. 2020;22 doi: 10.2196/21815. [DOI] [PMC free article] [PubMed] [Google Scholar]