Abstract
Objectives:
To evaluate the presence of migraine features in patients with persistent postural-perceptual dizziness (PPPD).
Methods:
In a retrospective survey study, consecutive patients presenting to a tertiary care neurotology clinic during an 18-month period were given questionnaires about headache and dizziness symptoms. The survey responses plus history and examination of the patient were used to diagnose patients with PPPD. The prevalence of migraine headache, vestibular migraine (VM), and migraine characteristics was evaluated.
Results:
In total, 36 subjects with PPPD were included in the study. The mean age of the subjects was 56±16 years with a female (72%) predominance. A total of 19 (53%) patients met the International Classification of Headache Disorders criteria for migraine headache, and 6 of those (17%) met the criteria for definite VM. Of the patients who did not meet full migraine headache criteria, 6 (17%) patients met 4 of 5 criteria, and 5 (14%) patients met 3 of 5 criteria. There was no significant difference between PPPD patients who fulfilled full migraine headache criteria and those who did not in sensitivity to light, sound, smells, weather changes, feelings of mental fog/confusion, and sinus pain/facial pressure.
Conclusions:
This study demonstrates that a majority of patients with PPPD fulfill the criteria for migraine headache. A large proportion of PPPD patients who do not meet the full criteria for migraine headache still meet a majority of the migraine headache criteria. This suggests an association between the two conditions. PPPD may be a part of the spectrum of otologic migraine, where migraine manifests as otologic symptoms.
Keywords: Persistent postural-perceptual dizziness, Migraine, Migraine headache, PPPD, Otologic migraine
Introduction
Persistent postural-perceptual dizziness (PPPD) is a functional vestibular disorder in which maladaptation typically to an inciting event causes a long-lasting sensation of motion, dizziness, and unsteadiness. Though only recently officially defined in 2015 in the International Classification of Diseases (ICD-11), the condition has been previously investigated for decades, and prior labels include phobic postural vertigo, space-motion discomfort, chronic subjective dizziness, and visual vertigo.1 The condition is characterized by 3 or more months of non-spinning vertigo, dizziness, or unsteadiness that is often initially triggered by an event that involves vestibular symptoms, psychological distress, or heightened awareness of posture (Table 1).2 The subsequent maladaptive response results in continued non-spinning vertigo or imbalance symptoms even after the inciting event has concluded. For example, a patient may develop vestibular neuritis and experience a continued sensation of motion even after the neuritis has resolved. Other inciting events include vestibular migraine, panic attacks, head injuries, autonomic dysfunction, and more.3
Table 1.
Diagnostic criteria for persistent postural-perceptual dizziness (PPPD) as defined by the International Classification of Vestibular Disorders (ICVD).
| All five criteria (A-E) must be fulfilled to make the diagnosis: |
|
PPPD has been found in association with migraine headache. A study by Bittar and Lins found that up to 26% of individuals with PPPD also experience migraine headaches.4 Episodes of migraine headache or vestibular migraine can additionally act as a trigger for PPPD. When individuals experience features of migraine headache alongside vestibular symptoms, they can be said to have vestibular migraine.5 However, PPPD, migraine headache, and vestibular migraine are thought to be distinct entities that can co-exist. Current treatment for PPPD generally consists of vestibular rehabilitation therapy, cognitive behavioral therapy, and medications including selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs).6–8 Interestingly, vestibular ocular reflex exercises may worsen vestibular symptoms or slow improvement in the setting of active migraine,9,10 prompting a need to elucidate the presence of migrainous features in those with PPPD in order to facilitate management of the condition. This study aims to determine the prevalence of migraine headache without aura, vestibular migraine, and migrainous features in a study population of PPPD patients. If an association exists between the two conditions, treatments for PPPD may potentially be expanded to include treatments for migraine headache as well.
Methods
Following institutional review board approval from the University of California, Irvine, electronic tablet surveys were administered to consecutive patients who presented to a tertiary care neurotology clinic from July 2018 to January 2020. Patients completed the surveys immediately after their clinical encounters with a neurotologist. The survey was a custom-designed questionnaire that included questions pertaining to the diagnostic criteria of migraine headache, vestibular migraine, and PPPD as defined by the International Classification of Vestibular Disorders (ICVD)2. Data from the completed surveys was uploaded onto a secure, clinical database using electronic data capture software (REDCap, Vanderbilt University, Nashville, TN, USA). Subjects were classified as having PPPD if their survey responses to the PPPD diagnostic criteria questions and combination of history and physical exam by a neurotologist both supported a diagnosis of PPPD and excluded other diagnoses as being more likely. Similarly, a diagnosis of migraine headache and vestibular migraine was made using a combination of responses to survey questions and a thorough history and physical exam by a neurotologist. Migraine headache without aura and vestibular migraine criteria were based on the International Classification of Headache Disorders (ICHD) 3rd edition published by the International Headache Society (IHS) (Table 2).5
Table 2.
Diagnostic criteria for migraine headache without aura and vestibular migraine as defined by the International Classification of Headache Disorders, 3rd edition (ICHD).
| Migraine headache without aura |
|
| Vestibular migraine |
| All five criteria (A-E) must be fulfilled to make the diagnosis: |
|
Demographics and prevalence of migraine headache features were compared between those with PPPD who met full migraine headache criteria and those who did not. Analysis utilizing chi-square or Fisher’s exact tests and independent sample t-test were performed to compare the variables between the two groups. SPSS 17.0 software (SPSS Inc., Chicago, IL, USA) was used for statistical analysis, with a P < 0.05 being considered statistically significant.
Results
Surveys were administered to all patients presenting with dizziness, of which 36 were diagnosed with PPPD. The mean age of PPPD subjects was 56 ± 16 years, with a female (72%) predominance. As outlined in Figure 1, a total of 19 (53%) patients met the ICHD criteria for migraine headache (13 female, 6 male). Of those with migraine headache, 6 (17% of total cohort) met the ICVD criteria for definite vestibular migraine. Of the PPPD patients who did not meet full migraine headache criteria, 6 (17%) patients met 4 of 5 criteria (probable vestibular migraine), and 5 (14%) patients met 3 of 5 criteria, for a total of 11 (31%) patients.
Figure 1.
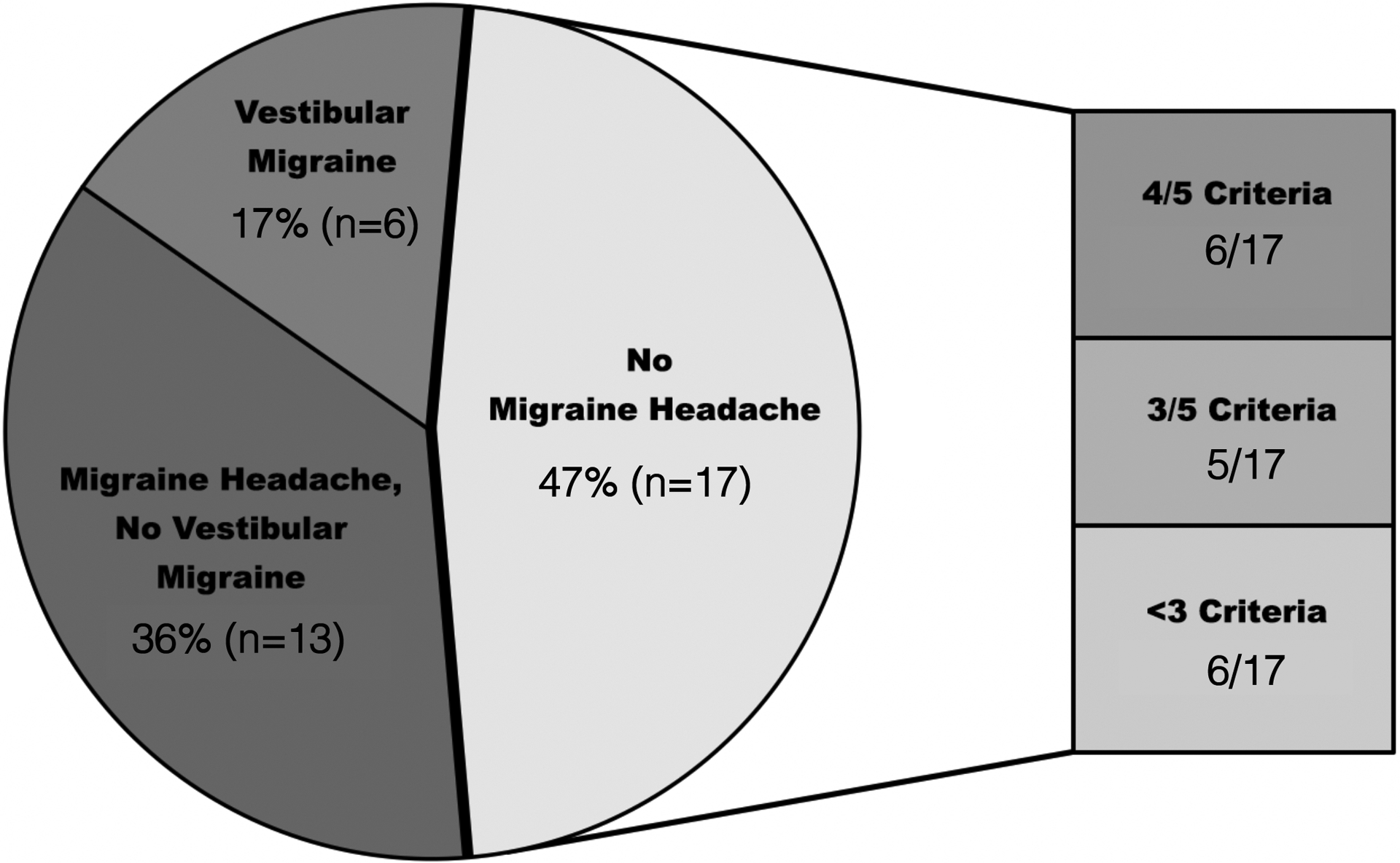
Percentage of persistent postural-perceptual dizziness subjects who met criteria for migraine headache (including vestibular migraine). Both ‘Migraine Headache, No Vestibular Migraine’ and ‘Vestibular Migraine’ patients meet full migraine headache criteria.
When comparing features of migraine between PPPD patients who fulfilled full migraine headache criteria and PPPD patients who did not, there was no significant difference between the percentage of those who experienced many migraine-related symptoms, such as sensitivity to light (73.7% vs. 41.2%, P = 0.09), sound (52.6% vs. 29.4%, P = 0.19), smells (26.3% vs. 11.8%, P = 0.41), and weather changes (31.6% vs. 5.9%, P = 0.09), feelings of sinus pressure or facial pain (57.9% vs. 35.3%, P = 0.20), feelings of mental fog or confusion (63.2% vs. 76.5%, P = 0.48), and family history of migraine (36.8% vs. 41.2%, P = 1.00) (Table 3). There was a significant difference between those who experienced nausea or vomiting during headache (63.2% vs. 11.8%, P = 0.005), relief of headaches with medication (68.4% vs. 94.1%, P = 0.02), headaches triggered by cold food or liquid (89.5% vs. 52.9%, P = 0.02), and ear pain (68.4% vs. 11.8%, P = 0.002).
Table 3.
Comparison of migraine features between persistent perceptual-postural dizziness (PPPD) patients who met full migraine headache criteria and those who did not meet full migraine headache criteria. A P < 0.05 was considered statistically significant.
| Feature | PPPD patients fulfilling migraine headache criteria (N=19) |
PPPD patients not fulfilling migraine headache criteria (N=17) |
P value |
|---|---|---|---|
| Sensitivity to light | 14 (73.7%) | 7 (41.2%) | 0.09 |
| Sensitivity to sound | 10 (52.6%) | 5 (29.4%) | 0.19 |
| Sensitivity to smells | 5 (26.3%) | 2 (11.8%) | 0.41 |
| Sensitivity to weather changes | 6 (31.6%) | 1 (5.9%) | 0.09 |
| Sinus pressure/facial pain | 11 (57.9%) | 6 (35.3%) | 0.20 |
| Mental fog/confusion | 12 (63.2%) | 13 (76.5%) | 0.48 |
| Family history of migraine | 7 (36.8%) | 7 (41.2%) | 1.00 |
| Family history of Meniere’s disease | 4 (21.1%) | 1 (5.9%) | 0.34 |
| Family history of motion sickness | 7 (36.8%) | 5 (29.4%) | 0.73 |
| Nausea/vomiting during headache | 12 (63.2%) | 2 (11.8%) | 0.005* |
| Relief of any headache with medications | 13 (68.4%) | 16 (94.1%) | 0.02* |
| Headache triggered by cold food or liquid | 17 (89.5%) | 9 (52.9%) | 0.02* |
| Ear pain | 13 (68.4%) | 2 (11.8%) | 0.002* |
Discussion
Despite PPPD being recently defined as a distinct clinical entity, its pathophysiology remains poorly understood. Nonetheless, data obtained from neuroimaging studies in patients with related disorders such as phobic postural vertigo and chronic subjective dizziness have provided a number of clues regarding the possible mechanisms underlying the complex disorder. The prevailing hypotheses include stiffened postural control, an imbalance in processing of visual stimuli over vestibular input, and neural dysfunction in regulating these two processes. In healthy individuals, the normal response to the onset of dizziness or vertigo is activation of high-risk postural control strategies such as shorter strides and more rigid stance when exposed to heights and slippery conditions. After the threat has subsided, these controls are abandoned. However, patients with PPPD experience failure to re-adapt quickly following postural imbalances due to deficiencies in higher cortical processes as well a behavioral maladaptation (often anxiety-driven) to natural postural control and spatial orientation.11
Our study found the prevalence of migraine headache in a population with PPPD to be 53%. This is much higher than the prevalence of migraine headache in the general population, which has been estimated to be about 8–13% in adults,12 and suggests an association between PPPD and migraine headache. This is also higher than the prevalence of migraine headache in those with PPPD investigated in other studies, which have found a prevalence of 26%4 and 16.5%.3 Various factors may account for this difference. In the study by Bittar and Lins,4 initially only women were treated in the clinic from which they included patient data before men were also included. In the study by Staab and Ruckenstein,3 patients with concomitant migraine headache and vestibular symptoms were excluded. When excluding patients who experienced vestibular migraine, the migraine headache prevalence in our study decreases to 36%; when men with migraine headache are excluded, the prevalence also decreases to 36%. This ultimately greater prevalence may potentially reflect a self-selective and differing patient population that presents to our tertiary care clinic and a comprehensive questionnaire that can assist in the migraine diagnosis.
While thought to be distinct disorders, migraine and PPPD share many characteristics that may help explain the high prevalence of migraine in our cohort of patients. Similar to the mechanisms described for PPPD, the pathophysiology of sensory phenomena during migraine auras can likely be attributed to cortical disturbances in the form of cortical spreading depression. Equally significant are the shared clinical features, particularly hypersensitivity to various sensory stimuli (e.g., visual motion, motion, light, sounds, smells) that may potentiate dizziness, motion sickness, and other vestibular symptoms experienced by migraine patients. For patients with concomitant PPPD, these same triggers that are responsible for migraine episodes likely serve to amplify the onset of PPPD and cause the vestibular symptoms to persist for even longer following termination of the inciting event. Given these observations, it appears that migraine itself may be considered a trigger and cause for the persistence of PPPD. For this reason, identification and effective management of underlying migraine disorder in patients can be reasonably attempted to help treat PPPD.
Our study additionally found a female predominance in both the entire cohort (72% female) and of migraine headache subgroup (68% female). Both PPPD and migraine headache tend to have more female sufferers.4,13,14 The increased prevalence of migraine headache in women is theorized to be related to the complex interplay of hormones, particularly estrogen, after menarche, during monthly cycles, and peri-menopause.15 In terms of PPPD, a personal or family history of anxiety has been identified as one risk factor for development of the condition;2,16,17 anxiety has also been found to be more common in women than in men.18 If an association between PPPD and migraine headache exists, then likely the combination of a higher risk of both migraine headache and of anxiety disorders may contribute to the female predominance of PPPD sufferers.
Interestingly, we identified a large group of individuals (31% of our cohort) who met three or four of the migraine headache criteria, although they did not meet all five criteria necessary to diagnose migraine headache. Similarly, there was no significant difference between the PPPD patients who met full migraine headache criteria and those who did not. This comparison was made for multiple migraine-associated symptoms that are not part of the diagnostic criteria, including sensitivity to smells and weather, feelings of mental fog, and sinus pressure or facial pain.19 This finding of no difference in migraine characteristics strongly suggests that multiple migraine features may be present in PPPD patients even when they do not fit all criteria for migraine headache or definite vestibular migraine. This may be especially poignant when it comes to management of PPPD.
Current treatments for PPPD include vestibular rehabilitation therapy, cognitive behavioral therapy, and medications including SSRIs and SNRIs.6–8 However, each treatment has varying efficacy according to current studies. Customized vestibular rehabilitation and cognitive behavioral therapy have both shown promise for improving and resolving symptoms.7,20,21 SSRIs and SNRIs, having previously been shown to help reduce vestibular symptoms in patients with chronic subjective dizziness, can also benefit PPPD patients and even those without psychiatric comorbidities. Unsurprisingly, PPPD patients with concomitant symptoms of depression and anxiety have also reported improvement in multiple open-label clinical trials. However, to date, only one randomized controlled trial has been conducted to study the efficacy of anti-depressants and compare the benefit of sertraline versus verapamil in patients with PPPD and vestibular migraine.11 In clinical practice, it has been recommended for clinicians to start with one SSRI (at half the dosage typically used in the treatment for depression) and to switch to a SNRI if the patient fails to tolerate or exhibit a clinical response even after trial with a second SSRI. Additionally, data from these trials have suggested that these medications take 8–12 weeks to produce the desired effects and patients who experience benefit should remain on treatment for at least 1 year.6
We have also found SSRIs and SNRIs to be effective in patients with vestibular migraine. It is possible that the success of these two classes of drugs may be related to its effectiveness in controlling migraine. The efficacy of these drugs may be through control of stress/anxiety/depression and sleep abnormalities which are significant migraine triggers. Although vestibular therapy can be helpful for PPPD, it can also worsen vestibular symptoms or slow improvement in the setting of active migraine.9 For this reason, it is imperative to identify PPPD patients who have comorbid migraine (headache or vestibular migraine) in order to implement an effective treatment plan. This is particularly critical because there may be an association between the two conditions, and treatment of migraine may reduce the severity of dizziness symptoms in PPPD.
This study has limitations that should be taken into consideration when interpreting the results. Its survey-based nature allows for the possibility of self-selection and recall bias. Furthermore, participants may not have full knowledge regarding their own family history. There is no objective diagnostic test for PPPD, and therefore, the amount of false positive diagnoses cannot be accurately quantified. These data were analyzed retrospectively, and randomized controlled trials which identify migraine symptoms and treat them alongside typical vestibular therapies would help elucidate the connection.
Conclusion
This study demonstrates that a majority of patients with PPPD fulfill criteria for migraine headache. A large proportion of PPPD patients who do not meet the full criteria for migraine headache still meet a majority of the migraine headache criteria and display features of migraine. PPPD may be part of the spectrum of otologic migraine, a spectrum of disorders where migraine can present with otologic complaints. This may suggest an association between the two conditions and underscores the importance of identifying when both conditions exist comorbidly, as treatment of only PPPD without addressing migraine may produce suboptimal improvement and treatment of both together may improve outcomes and the overall efficacy of treatment.
Financial Disclosure:
Mehdi Abouzari is supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant TL1TR001415.
Footnotes
Conflicts of Interest: Hamid R. Djalilian holds equity in MindSet Technologies and Cactus Medical LLC, and is on the advisory board of Novus Therapeutics.
Portion of this work has been presented orally at the AAO-HNSF 2020 Virtual Annual Meeting & OTO Experience on September 19, 2020.
References
- 1.Dieterich M, Staab JP. Functional dizziness: from phobic postural vertigo and chronic subjective dizziness to persistent postural-perceptual dizziness. Curr Opin Neurol 2017; 30:107–113. [DOI] [PubMed] [Google Scholar]
- 2.Staab JP, Eckhardt-Henn A, Horii Aet al. Diagnostic criteria for persistent postural-perceptual dizziness (PPPD): Consensus document of the committee for the Classification of Vestibular Disorders of the Barany Society. J Vestib Res 2017; 27:191–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Staab JP, Ruckenstein MJ. Expanding the differential diagnosis of chronic dizziness. Arch Otolaryngol Head Neck Surg 2007; 133:170–176. [DOI] [PubMed] [Google Scholar]
- 4.Bittar RS, Lins EM. Clinical characteristics of patients with persistent postural-perceptual dizziness. Braz J Otorhinolaryngol 2015; 81:276–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Headache Classification Committee of the International Headache S. The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia; 2013; 33:629–808. [DOI] [PubMed] [Google Scholar]
- 6.Popkirov S, Staab JP, Stone J. Persistent postural-perceptual dizziness (PPPD): a common, characteristic and treatable cause of chronic dizziness. Pract Neurol 2018; 18:5–13. [DOI] [PubMed] [Google Scholar]
- 7.Edelman S, Mahoney AE, Cremer PD. Cognitive behavior therapy for chronic subjective dizziness: a randomized, controlled trial. Am J Otolaryngol 2012; 33:395–401. [DOI] [PubMed] [Google Scholar]
- 8.Staab JP. Chronic subjective dizziness. Continuum (Minneap Minn) 2012; 18:1118–1141. [DOI] [PubMed] [Google Scholar]
- 9.Vitkovic J, Winoto A, Rance G, Dowell R, Paine M. Vestibular rehabilitation outcomes in patients with and without vestibular migraine. J Neurol 2013; 260:3039–3048. [DOI] [PubMed] [Google Scholar]
- 10.Seemungal BM, Passamonti L. Persistent postural-perceptual dizziness: a useful new syndrome. Pract Neurol 2018; 18:3–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Staab JP ES, Neff BA, Shepherd NT. Vestibular migraine and persistent postural-perceptual dizziness: results of a double-blind, parallel group, pharmacological dissection trial using verapamil and sertraline. Cephalgia 2015; 35:65. [Google Scholar]
- 12.Merikangas KR. Contributions of epidemiology to our understanding of migraine. Headache 2013; 53:230–246. [DOI] [PubMed] [Google Scholar]
- 13.Kalaydjian A, Merikangas K. Physical and mental comorbidity of headache in a nationally representative sample of US adults. Psychosom Med 2008; 70:773–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yan Z, Cui L, Yu T, Liang H, Wang Y, Chen C. Analysis of the characteristics of persistent postural-perceptual dizziness: A clinical-based study in China. Int J Audiol 2017; 56:33–37. [DOI] [PubMed] [Google Scholar]
- 15.Loder E, Rizzoli P, Golub J. Hormonal management of migraine associated with menses and the menopause: a clinical review. Headache 2007; 47:329–340. [DOI] [PubMed] [Google Scholar]
- 16.Staab JP, Rohe DE, Eggers SD, Shepard NT. Anxious, introverted personality traits in patients with chronic subjective dizziness. J Psychosom Res 2014; 76:80–83. [DOI] [PubMed] [Google Scholar]
- 17.Best C, Tschan R, Eckhardt-Henn A, Dieterich M. Who is at risk for ongoing dizziness and psychological strain after a vestibular disorder? Neuroscience 2009; 164:1579–1587. [DOI] [PubMed] [Google Scholar]
- 18.Remes O, Brayne C, van der Linde R, Lafortune L. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain Behav 2016; 6:e00497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghavami Y, Mahboubi H, Yau AY, Maducdoc M, Djalilian HR. Migraine features in patients with Meniere’s disease. Laryngoscope 2016; 126:163–168. [DOI] [PubMed] [Google Scholar]
- 20.Thompson KJ, Goetting JC, Staab JP, Shepard NT. Retrospective review and telephone follow-up to evaluate a physical therapy protocol for treating persistent postural-perceptual dizziness: A pilot study. J Vestib Res 2015; 25:97–103; quiz 103–104. [DOI] [PubMed] [Google Scholar]
- 21.A EJM, Edelman S, P DC. Cognitive behavior therapy for chronic subjective dizziness: longer-term gains and predictors of disability. Am J Otolaryngol 2013; 34:115–120. [DOI] [PubMed] [Google Scholar]


